Abstract
Chlamydia is a very common, curable sexually transmitted infection (STI) caused by the Chlamydia trachomatis bacteria. Chlamydia prevalence is higher in young women and is similar in some developed countries. Generally the infections are asymptomatic, resulting in a large reservoir of undetected, untreated infections. Untreated chlamydia infection may result in long-term sequelae in women including pelvic inflammatory disease (PID) and ectopic pregnancy. Detection of chlamydia has become easier with the recent introduction of rapid, sensitive, affordable, and non-invasive DNA tests. Treatment is also straightforward and inexpensive with doxycycline or azithromycin. Chlamydia screening therefore has been or is being implemented in various developed countries. However much of the epidemiology of chlamydia remains poorly understood and there are many questions regarding the long-term impact of interventions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Chlamydial infection is a major public health concern globally [1]. The World Health Organization (WHO) estimated the global prevalence of several sexually transmitted infections (STIs) among individuals aged 15–49 years every 5 years. The study presented a pooled prevalence for chlamydia worldwide in 2012 of 4.2% (95% UI: 3.7–4.7%) in women, with regional values ranging from 1.8% to 7.6%, and 2.7% (95% UI: 2.0–3.6%) in men, with regional values that ranged from 1.3% to 5.2%. Regions of the Americas and Western Pacific were the most affected areas [2].
Chlamydia is the most frequently reported infectious disease in the USA [3] and its estimated prevalence in Europe is statistically consistent with findings in other high income countries [4], despite the fact that most population based studies are considered at risk of participation bias [5].
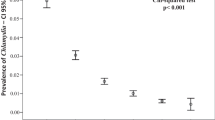
The main risk factors for acquisition of C. trachomatis infection are young age (individuals aged <25 years tend to have the highest prevalence of the infection) and behavioural factors such as prior C. trachomatis infection, inconsistent condom use, and new or multiple partners per year. A consistent association was found between socioeconomic disadvantage, race, ethnicity, residence in deprived areas, and chlamydia infection, due to lack of access to screening programmes, awareness on safe sex and condom use, and higher prevalence of substance use [6].
A statistically significant difference in prevalence between the two sexes is reported. In 2016, case rate in females was about two times the one in males, most probably due to the larger number of women screened for this infection. The increasing use of urinary highly sensitive nucleic acid amplification tests (NAATs) shows a larger number of men infected, even though many men are still not receiving a diagnosis of chlamydia or being reported [7]. Different studies demonstrated that >53% of couples in which at least one partner had chlamydia were concordant for the infection and that the concordance correlated with higher bacterial loads [8, 9].
Men who have sex with men are considered at high risk for STI. In 2016, the median site-specific prevalence of urogenital C. trachomatis among MSM tested at select STI clinics in the USA was 6% (range by site: 3–15%) [7].
Coinfections with C. trachomatis and other urogenital sexually transmitted pathogens have frequently been reported among high-risk men and women, especially Neisseria gonorrhoeae, Trichomoniasis, Mycoplasma genitalium, and HIV. Recent studies exhibited a possible role of C. trachomatis in enhancing the malignant potential of HPV, through the instauration of a chronic inflammatory environment [10, 11].
As asymptomatic infection is common among both men and women and immunity is short-lived, reinfection or persistent infection is also common.
2 Clinical Manifestations of Chlamydia trachomatis Infections
Chlamydia is known as a “silent” infection because most infected people are asymptomatic and lack abnormal physical examination findings. Estimates of the proportion of chlamydia-infected people who develop symptoms vary by setting and study methodology; two published studies that incorporated modelling techniques to address limitations of point prevalence surveys estimated that only about 10% of men and 5–30% of women with laboratory-confirmed chlamydial infection develop symptoms.
2.1 Clinical Syndromes in Women
2.1.1 Cervicitis
In women, the bacteria initially infect the cervix, where the infection may cause signs and symptoms of cervicitis such as:
-
Purulent or mucopurulent vaginal discharge and/or
-
Intermenstrual vaginal bleeding
-
Post-coital bleeding
-
Dyspareunia
-
Vulvovaginal irritation
-
Dysuria, urinary frequency
2.1.2 Urinary Symptoms
They are generally due to concomitant urethral infection, which occurs in approximately 15% of women with cervical chlamydia infection.
-
Dysuria
-
Urinary frequency
2.1.3 Pelvic Inflammatory Disease (PID)
Infection can spread from the cervix to the upper reproductive tract (i.e., uterus, fallopian tubes), causing pelvic inflammatory disease (PID), which encompasses a wide spectrum of clinical presentations.
-
Lower abdominal pain is the cardinal symptom.
The abdominal or pelvic pain is usually bilateral and rarely of more than 2 weeks’ duration [7]. The character of the pain is variable, and in some cases, may be quite subtle. The recent onset of pain that worsens during coitus or with jarring movement may be the only presenting symptom of PID. The onset of pain during or shortly after menses is particularly suggestive. On bimanual pelvic examination, physical examination, cervical motion tenderness or uterine tenderness or adnexal tenderness is the defining characteristic of acute symptomatic PID.
PID diagnostic criteria per CDC guidelines (2015) | |
|---|---|
Minimal criteriaa | Cervical motion tenderness |
Uterine tenderness | |
Adnexal tenderness | |
Additional criteriab | Oral temperature greater than 101 °F (38.3 °C) |
Abnormal cervical mucopurulent discharge or cervical friability | |
Abundant white blood cells on microscopic evaluation of vaginal fluid | |
Elevated erythrocyte sedimentation rate | |
Elevated C-reactive protein | |
Laboratory documentation of cervical infection with N. gonorrhoeae or C. trachomatis | |
Specific criteriac | Endometrial biopsy with histopathologic evidence of endometritis |
Transvaginal ultrasound or magnetic resonance imaging showing thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex, or Doppler studies suggesting pelvic infection | |
Laparoscopic findings consistent with PID | |
2.1.4 Perihepatitis (Fitz-Hugh–Curtis Syndrome)
Fitz-Hugh–Curtis syndrome is a rare disorder that occurs almost exclusively in women. It is characterized by inflammation of the membrane lining the stomach (peritoneum) and the tissues surrounding the liver (perihepatitis).
The syndrome is characterized by the onset of sudden, severe pain in the upper right area of the abdomen. Pain may spread to additional areas including the right shoulder and the inside of the right arm. Movement often increases pain. The upper right area may be extremely tender.
Additional symptoms may occur in some cases including fever, chills, night sweats, vomiting, and nausea. Some affected individuals may develop headaches, hiccupping, and a general feeling of poor health (malaise).
The pathogenesis of this entity is not fully understood but may involve either direct extension of infected material from the cul-de-sac through the peritoneum and/or lymphatics, or an immunologically mediated mechanism.
On laparoscopy or visual inspection, perihepatitis manifests as a patchy purulent and fibrinous exudate (“violin string” adhesions), most prominently affecting the anterior surfaces of the liver (not the liver parenchyma).
2.1.5 Tubo-Ovarian Abscess (TOA)
Tubo-ovarian abscess is usually a complication of PID. It is an inflammatory mass involving the fallopian tube, ovary, and, occasionally, other adjacent pelvic organs (e.g., bowel, bladder). This may manifest as a tubo-ovarian complex (an agglutination of those structures) or a collection of pus (tubo-ovarian abscess). These abscesses are found most commonly in reproductive age women and typically result from upper genital tract infection.
The classic presentation is the same as for PID alone, including acute lower abdominal pain, fever, chills, and vaginal discharge.
However, some cases of TOA differ from the classic scenario. Fever is not present in all patients and some patients report only low grade nocturnal fevers or chills. Also, not all women present in an acute fashion. These variations in clinical presentation were illustrated in one of the largest series of women with TOA (n = 175) [11]. As many as 40% of patients were afebrile upon presentation; 25% complained of chronic rather than acute abdominal pain; and 23% had normal white blood cell counts.
2.2 Clinical Syndromes in Men
2.2.1 Urethritis
C. trachomatis is the most common cause of nongonococcal urethritis in men. The proportion of cases that are asymptomatic vary by population and range from 40 to 96% [12,13,14]. When men do have symptoms, they typically present with a mucoid or watery urethral discharge, and dysuria is often a prominent complaint. The discharge is often clear and only seen upon milking the urethra. Sometimes the discharge is so scant that men only notice stained undergarments in the morning.
2.2.2 Epididymitis
Inflammation of the epididymis is known as epididymitis. C. trachomatis is one of the most frequent pathogens in epididymitis among sexually active men <35 years of age, along with N. gonorrhoeae.
Men with acute epididymitis typically have:
-
unilateral testicular pain and tenderness
-
hydrocele
-
palpable swelling of the epididymis.
On physical examination, the affected testis has a normal vertical lie; the scrotum may be red and parchment-like (although this is an uncommon finding); scrotal oedema is present in at least 50% of cases. Sometimes an inflammatory nodule is felt with an otherwise soft, nontender epididymis. In contrast to patients with testicular torsion, patients with epididymitis usually have a normal cremasteric reflex (if they have one under normal conditions). Patients with epididymitis may experience pain relief with elevation of the testis (Prehn sign), but this is not a reliable marker for epididymitis.
2.2.3 Prostatitis
C. trachomatis may be an aetiology in some cases of chronic prostatitis, although this attribution remains highly speculative. Symptoms in these men included:
-
dysuria
-
urinary dysfunction
-
pain with ejaculation
-
pelvic pain.
2.2.4 Proctitis
Chlamydial proctitis, defined as inflammation of the distal rectal mucosa, occurs primarily in men who have sex with men (MSM) who engage in receptive anal intercourse.
The clinical presentation of chlamydial proctitis depends on the infecting chlamydial serovars.
The L1, L2, and L3 serovars of C. trachomatis cause the disease known as lymphogranuloma venereum (LGV), which can present as anorectal disease and has been reported in outbreaks among European and North American MSM, particularly those who are HIV-infected [15].
Symptoms occur in the vast majority of cases. These include:
-
anorectal pain
-
discharge
-
tenesmus
-
rectal bleeding
-
constipation
Systemic symptoms of fever and malaise are also often present. Left untreated, rectal infection with the L1, L2, and L3 serovars can lead to rectal fistulae and strictures.
The non-LGV serovars that cause genital infection (serovars D through K) can also cause infection of the rectum, particularly in MSM, but in contrast to LGV, these infections are usually asymptomatic.
2.2.5 Reactive Arthritis/Reactive Arthritis Triad (RAT)
Approximately 1% of men with urethritis develop reactive arthritis, and approximately one-third of these patients have the complete reactive arthritis triad (RAT) formerly referred to as Reiter syndrome (arthritis, uveitis, and urethritis).
Patients with reactive arthritis typically present with an asymmetric oligoarthritis, usually 1–4 weeks following the inciting infection. The several types of clinical manifestations of reactive arthritis include:
-
Symptoms of preceding enteric or genitourinary infection (diarrhoea or urethritis)
-
Musculoskeletal signs and symptoms:
-
Arthritis: acute-onset asymmetric oligoarthritis, often affecting the lower extremities
-
Enthesitis: inflammation around the enthesis (site of insertion of ligaments, tendons, joint capsule, or fascia to bone). Common sites of heel involvement are at the insertions of the Achilles tendon and of the plantar fascia on the calcaneus. Pain, swelling, and local tenderness are suggestive clinical features. Estimates of the frequency of enthesitis in patients with reactive arthritis have ranged from 20 to 90%
-
-
Extraarticular signs and symptoms
-
Conjunctivitis,
-
Genitourinary tract symptoms, such as dysuria, pelvic pain, urethritis, prostatitis
-
Oral lesions, including mucosal ulcers
-
Cutaneous eruptions and other skin changes, such as keratoderma blennorrhagica (hyperkeratotic skin lesions on soles and palms) and erythema nodosum
-
Nail changes that resemble those seen in psoriasis
-
Genital lesions such as circinate balanitis
-
Cardiac manifestations, which are uncommon, include valve disease, particularly aortic insufficiency, with greater chronicity of illness. Pericarditis has been reported very rarely.
-
3 Screening in Adult Men and Women
Detecting chlamydial infections among asymptomatic individuals is an important public health tool. Its main rationale is to identify and treat the infection to avoid complications, particularly in women, and to prevent transmission and reinfection among sex partners.
Women: As CT shows its highest prevalence in young women, an annual screening of all sexually active women aged <25 years is recommended, as well as screening of all women with behavioural risk factors such as new or multiple sex partners, a sex partner with concurrent partners, or a sex partner who has a sexually transmitted infection. The main advantage of chlamydia screening programs is to reduce the rates of PID in women [16], whereas their effect on prevalence in the general population is uncertain [17].
Modern approach to women screening for chlamydia includes endocervical or vaginal swabs or first-catch urine samples. Nucleic acid amplification tests (NAAT), specific for nucleic acid (DNA or RNA), are considered the gold standard for the detection of C. trachomatis because of their high sensitiveness, specificity, and speed, thus replacing less-sensitive methods, such as isolation in cell culture or identification by direct fluorescence assays (DFA) [4, 18]. Serologic tests that detect a systemic immune response to infection are not recommended because of the lack of precision for the detection of an active infection. The test can be run on endocervical swabs collected during a vaginal speculum examination or on vaginal swabs or urine samples. The CDC considers vaginal swab to be the preferred specimen type for its efficacy and ease of collection [19]. A recent review on ten studies involving 10,479 participants showed that home-based specimen collection can be a valid alternative to clinic-based collection, encouraging more people to be tested and reducing costs, discomfort, and time of a clinical consultation [20]. A first-catch urine specimen is also acceptable but less sensitive.
According to CDC guidelines, a routine screening for chlamydia should be offered at the first prenatal visit to all pregnant women aged <25 years at increased risk. Retest during the third trimester is supposed to prevent maternal postnatal complications and neonatal infection. Positive women should undergo NAAT 3–4 weeks after treatment to assess eradication and be retested within 3 months [3].
Screening for chlamydia in the rectum and pharynx with the use of laboratory validated assays can be considered in persons who are at risk for infection at those sites, even if no definitive data on the group of women to screen or the harm of infection in these sites are available [21].
Men: Targeted chlamydia screening in men aims to reduce infection, reinfection, and transmission among sex partners and should only be considered when prevalence is high. Efficacy and cost-effectiveness of routine screening for C. trachomatis in sexually active young men are not clear [18]. However, it must be proposed in specific clinical settings with a high prevalence of infection such as adolescent clinics, correctional facilities, and STD clinics.
Strong evidences support the relevance of screening in populations at risk, such as men who have sex with men (MSM) [4, 22]. Since CT infections are often asymptomatic, accurate early diagnosis through an annual test in MSM is critical to hinder the transmission and to reduce the risk of acquiring HIV infection. Nucleic acid amplification tests (NAAT) are now recommended by international guidelines to screen also MSM for extra-genital CT infections. Rectal prevalence in MSM for chlamydia is estimated 8.9%, with a pharyngeal prevalence of 1.6% and 5.3%, respectively. Oropharyngeal chlamydia screening could be useful to detect infections in this site, which would have been missed and not treated with just urogenital test. However, it is still unclear whether oropharyngeal chlamydia contributes to the overall prevalence of chlamydia in MSM [23].
3.1 Diagnostic Considerations
Diagnostic techniques for C. trachomatis infection have been ever developing during the last decades; NAAT replaced other classical methods such as culture, antigen detection, and genetic probes.
Nucleic acid amplification—NAAT methodology consists of amplifying C. trachomatis DNA or RNA sequences using polymerase chain reaction (PCR), transcription-mediated amplification (TMA), or strand displacement amplification (SDA). It is nowadays considered the benchmark for diagnosis, due to its superior sensitivity, specificity, and ease to collect specimens [24]. It can be performed on either endocervical, vaginal, or urethral swabs with a plastic or wire shaft and a rayon, dacron, or cytobrush tip [20]. Diagnosis of C. trachomatis urethral infection in men can be made by testing a urethral swab or first-catch urine specimen, which is preferred as non-invasive. In women, a swab of vaginal fluid is the preferred approach for diagnosing chlamydial infection, as this specimen provides the highest sensitivity [25]. First-catch urine can also be used with sensitivity and specificity of non-invasive testing comparable to invasive testing. Urine sample should be collected from the initial stream (approximately the first 10 mL) without pre-cleansing of the genital areas. Purulent material or blood does not affect the performance of the test. Commercially available NAATs are not yet licensed by FDA for the diagnosis of extra-genital (rectal or oropharyngeal) samples but have shown to be more reliable than culture for detection of chlamydial infection in persons engaging in receptive anal or oral intercourse. For this reason, chlamydia infection might be detected in a single specimen in the occasion of gonorrhoea testing. Self-collection of rectal specimens is considered as reliable as clinic-based collection [3].
Liquid-based cytology specimens collected for Pap smears have been tested for NAAT, with the aim of running different tests on the same specimen collected for HPV screening, which is offered by most states worldwide. Recently, the Chlamydia trachomatis Qx Amplified DNA Assay (CTQ) has been FDA-cleared for the detection of C. trachomatis in liquid-based preparations. Test sensitivity has shown to be lower than on cervical or vaginal swab specimens. A confirmatory test is recommended in a population with a low prevalence of chlamydial infection to minimize the number of false positives [3, 20, 26].
Rapid tests for chlamydia—rapid point-of-care diagnostic tests (RDTs) are particularly valuable as they allow immediate diagnosis and treatment. RDTs are useful to reach high-risk individuals marginalized from the healthcare system or for patients who have problems in returning to the clinic for the results. Most RDTs are immune chromatographic tests based on lateral-flow-technology and detect chlamydia LPS antigen in genital swabs or urine. They cannot be recommended as screening tests due to lack of sensitivity. Currently available near-point-of-care NAATs have acceptable performance characteristics and results for chlamydia (and gonorrhoea) can be provided within 90 min. This test is approved in the USA for use on endocervical or vaginal swabs and urine. European CDC suggests caution in the use of the actual available tests [4]. Several immunoassay-based and PCR-based tests are in development. These rapid tests provide results within 30 min of testing and are less expensive to perform and easy to interpret [27].
Culture—culture methods used to be the gold standard for C. trachomatis detection. Their use is today limited to research due to the expense and technical difficulties.
Serology—C. trachomatis serology needs complement fixation titres >1:64. It can support the diagnosis of chlamydia in pelvic chronic and invasive infections (PID, LGV) but it is useless in cutaneous and early manifestations. It may also not perform as well in diagnosing rectal infections in men as it does upper genital tract infection in women.
Antigen detection—Antigen detection requires invasive testing using a swab from the cervix or urethra. The sensitivity of this method is 80–95% compared with culture.
Genetic probe methods—probe methods require invasive testing using a direct swab from the cervix or urethra. The sensitivity of this assay is approximately 80% compared with culture. The main advantage of these tests is their low cost; however, because their sensitivity is considerably lower than NAAT and because NAAT became more cost-competitive, these tests are not used as frequently as in the past.
European guidelines establish clear indication about whom should be tested for chlamydia infection.
Asymptomatic people who present risk factors for C. trachomatis and/or other STI (age <25 years, new sexual contact in the last year, more than one partner in the last year, receptive anal intercourses, MSM, sexually active HIV-infected individuals) should undergo routine screening.
Any sexually active individual with symptoms or signs consistent with risk of chlamydia infection such as urethritis, acute epididymo-orchitis in men, cervical or vaginal discharge, acute pelvic pain and/or symptoms or signs of PID or purulent conjunctivitis need to be diagnosed and treated.
Any patient affected from gonorrhoea or other STI should be tested for Chlamydia trachomatis.
After sexual contact with persons with a potential or known STI or PID, American College of Obstetricians and Gynaecologists supports the use of expedited partner therapy as a method of preventing gonorrhoea and chlamydial reinfection when a patient’s partners are unable or unwilling to seek medical care. Patients should be instructed to abstain from sexual intercourse for 7 days after they and their sexual partners have completed treatment [28, 29].
Women undergoing any intrauterine interventions or manipulations should be tested for chlamydia to lower risk of PID.
Recurrent symptoms after initial resolution represent an indicator of reinfection. For that, evaluation for chlamydia should be repeated with NAAT. It is important to investigate whether sex partner has been appropriately treated and to counsel the patient about safe sex opportunities. Repeated testing in 3–6 months should be offered to young women and men (<25 years of age) who test positive for C. trachomatis [4]. A recent RCT suggests that invitation for retesting 8 weeks after initial treatment would be the optimal management for both younger and older than 25 to detect new infections [30]. However, this point is still controversial, and more evidence is needed.
4 New Evidence Based Treatment Approach
Treating urogenital C. trachomatis infection prevents complications (PID, chronic pelvic pain, infertility, ectopic pregnancy) and decreases the rate of sexual and vertical transmission. Treating sex partners is critical to avoid reinfection and spreading of the infection.
Chlamydia should be diagnosed early, and people resulted positive should be treated promptly; treatment delays have been associated with complications.
-
Treatment of uncomplicated urogenital chlamydia (urethritis in men, urethritis and cervicitis in women)
-
Recommended Regimens
-
Azithromycin 1 g orally in a single dose OR
-
Doxycycline 100 mg orally twice a day for 7 days
-
-
All the world most important centres for diseases control state that azithromycin and doxycycline are the first line in CT treatment. Cure rates with these two regimens are similar and exceed 95%. Some authors suggest that doxycycline might be superior in terms of efficacy to azithromycin [31, 32], but the relevance of this finding in clinical scenario is still not clear [33]. The drug choice in different settings results from cost, quality, and equity considerations. Azithromycin is preferred for its convenience in administration and excellent tissue and intracellular penetration, doxycycline reduces costs of treatment, but a 7-day compliance is needed and it is contraindicated in pregnancy.
-
Alternative Regimens
Erythromycin and penicillin are inferior in their cure rates but are useful in pregnant patients who cannot tolerate azithromycin. The use of these drugs requires a test of cure to ensure microbiologic eradication.
Fluoroquinolones are highly effective against chlamydia and are recognized by CDC as alternative therapies. As drawbacks, they require compliance to a week-therapy; are more expensive; and are contraindicated in pregnancy, lactation, and children. They were used in the past for coinfections from Chlamydia and Neisseria gonorrhoeae, but are no more considerate adequate as Neisseria has developed drug resistance.
-
Treatment of other chlamydia infections
-
Coinfections with gonorrhoea: empiric therapy for gonorrhoea is not indicated routinely in all patients diagnosed with Chlamydia. Men should be treated for both if intracellular gram-negative diplococci are detected on a Gram stain of urethral discharge. Women should be treated in accordance to risk factors for gonorrhoea or high local prevalence of this infection, as presence of non-pathogen endocervical Neisseria makes Gram stain less useful [3].
-
Proctitis and lymphogranuloma venereum: A meta-analysis of observational studies showed higher cure rates of rectal chlamydia after doxycycline therapy than after azithromycin therapy [33]. However, these studies have limitations, and prospective clinical trials comparing azithromycin versus doxycycline regimens for rectal C. trachomatis infection are needed. Due to high prevalence of coinfection in patients with acute proctitis, empiric therapy for both chlamydia and gonorrhoea is indicated. It should be started immediately if symptoms are highly suggestive or polymorphonuclear leukocytes are found on anorectal exudate sample. The recommended regimen includes ceftriaxone 250 mg IM in a single dose plus doxycycline 100 mg orally twice a day for 7 days. MSM with acute proctitis and either a positive rectal chlamydia NAAT or HIV infection with bloody discharge, perianal ulcers, or mucosal ulcers should be empirically treated for LGV with doxycycline 100 mg twice daily orally for 3 weeks [3, 34].
-
Epididymitis: CDC guidelines recommended regimens for acute epididymitis most likely caused by sexually transmitted chlamydia and gonorrhoea include ceftriaxone 250 mg IM in a single dose plus doxycycline 100 mg orally twice a day for 10 days. In case of risk factors for enteric organisms, such as insertive anal sex, ceftriaxone 250 mg IM in a single dose plus levofloxacin 500 mg orally once a day for 10 days or ofloxacin 300 mg orally twice a day for 10 days are preferred [3].
-
Pelvic inflammatory disease: [3, 35] All patients diagnosed with PID should be tested for Chlamydia, gonorrhoea, M. genitalium, syphilis, and HIV. Delayed treatment should be avoided for the increase of risk of long-term sequelae. Regimens should be adjusted by the changing spectrum of antimicrobial resistance over time and in different geographical areas.
-
Outpatient regimens include
-
ceftriaxone 500 mg single dose followed by oral doxycycline 100 mg twice daily plus metronidazole 500 mg twice daily for 14 days or
-
oral ofloxacin 400 mg twice daily plus oral metronidazole 500 mg twice daily for 14 days or
-
oral moxifloxacin 400 mg once daily for 14 days.
If severe sign, tubo-ovarian abscess or pregnancy are verified, inpatient regimens are preferred:
-
i.v./i.m. ceftriaxone 1 g once daily plus i.v. doxycycline 100 mg twice daily followed by oral doxycycline 100 mg twice daily plus oral metronidazole 500 mg twice daily to complete 14 days or
-
i.v. clindamycin 900 mg three times daily plus i.m./i.v. gentamicin 3–6 mg/kg as a single daily dose with renal monitoring followed by either oral clindamycin 450 mg four times daily to complete 14 days or oral doxycycline 100 mg twice daily plus oral metronidazole 500 mg twice daily to complete 14 days.
Alternative regimens
-
i.v. ofloxacin 400 mg twice daily plus i.v. metronidazole 500 mg three times daily for 14 days
-
i.m. ceftriaxone 500 mg single dose plus oral azithromycin 1 g single dose followed by a second dose of oral azithromycin 1 g after 1 week
-
Oropharyngeal infection: it is still uncertain the clinical significance of oropharyngeal C. trachomatis infection and therefore routine oropharyngeal screening for CT is not recommended. However, evidence suggests oropharyngeal C. trachomatis can be sexually transmitted to genital sites [36, 37]; therefore, detection of C. trachomatis from an oropharyngeal specimen should be treated with azithromycin or doxycycline. The efficacy of alternative antimicrobial regimens in oropharyngeal chlamydia infection remains unknown.
-
Treatment of chlamydia infection during pregnancy: [3, 4, 24] treatment of chlamydia infection in pregnancy is critical to avoid transmission to the newborn.
-
Recommended regimen
-
Oral azithromycin 1 g as a single dose is considered the first line, as it is effective and safe, while doxycycline is contraindicated in the second and third trimesters of pregnancy
-
-
Alternative Regimens
-
Amoxicillin 500 mg orally three times a day for 7 days OR
-
Erythromycin base 500 mg orally four times a day for 7 days OR erythromycin base 250 mg orally four times a day for 14 days OR
-
Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR erythromycin ethylsuccinate 400 mg orally four times a day for 14 days
-
-
Amoxicillin is safe and it used to be a first-line drug, but data suggest that it might cause persistence in culture at physiologically relevant concentrations [38], erythromycin is safe but compliance is reduced by gastrointestinal side effects.
Test-of-cure to document chlamydial eradication (preferably by NAAT) 3–4 weeks after completion of therapy is needed to assess infection eradication. In addition, all pregnant women who have chlamydial infection diagnosed should be retested 3 months after treatment.
5 Follow-Up Strategies [3, 4]
Testing for chlamydia after treatment is critical to assess the eradication of infection and avoid mis-known recurrence or persistence and spread of infection among sex partners. After-treatment strategies include “test of cure” (TOC) and “retesting.”
TOC is a diagnostic testing with the aim of assessing whether the pathogen has been eradicated by the antibiotic strategy used. It is performed 3–4 weeks after treatment is completed. NAAT method is the first choice and it is not reliable if done earlier for the risk of testing false-positive for the presence of dead microorganisms [20, 38]. It is not recommended to perform TOC routinely in patients treated with recommended first-line regimens, unless therapeutic adherence is in question, symptoms persist, or reinfection is suspected. Indications for TOC include pregnancy, complicated infections, persistence of symptoms, use of second-line or third-line regimens such as erythromycin or amoxicillin. It should also be considered in extra-genital infections, particularly when azithromycin 1 g stat has been administered for treatment of rectal infections. TOC of asymptomatic MSM with rectal chlamydia after treatment for uncomplicated chlamydial infection (azithromycin 1 g single oral dose or doxycycline 100 mg, 7 days) should be considered to ensure that any LGV infection is not missed.
Retesting is performed approximately 3 months after treatment of infection, or if this is not possible, at the first visit thereafter within 12 months of treatment. This is necessary because most post-treatment infections result from reinfection due to lack of notification and treatment of sex partners or the initiation of sexual relation with a new infected partner. International guidelines assert that young women and men (<25 years of age) who test positive for C. trachomatis should be retested, regardless of whether they believe that their sex partners were treated. A recent RCT suggests that invitation for retesting 8 weeks after initial treatment would be the optimal management for both younger and older than 25 to detect new infections [30]. However, this point is still controversial, and more evidence is needed. Beyond testing, persistence or recurrence of symptoms must be monitored.
6 Management of Sex Partners
Reinfection among asymptomatic sex partners is the most frequent cause of recurrence of chlamydia infection. The only way to avoid it is to assess and treat people who had sexual intercourses with the patient within the last 60 days preceding the onset of symptoms or chlamydia diagnosis, or the most recent sex partner. As most people are unwilling to be tested and counselled, a strategy termed expedited partner therapy has been proposed. Expedited partner therapy enables the obstetrician–gynaecologist or other provider to give prescriptions or medications to patients to take to their partners without first examining them. Compared with standard patient referral of partners, this approach to therapy has been associated with decreased rates of persistent or recurrent chlamydia [39]. Despite the effectiveness of expedited partner therapy, numerous legal, medical, practical, and administrative barriers hinder its routine use by obstetrician–gynaecologists [28]. EPT is not routinely recommended for MSM with chlamydia because of a high risk for coexisting infections (especially undiagnosed HIV) among their partners, and because data are limited regarding the effectiveness of this approach in reducing persistent or recurrent chlamydia among MSM [4]. To avoid reinfection, sex partners should be instructed to abstain from sexual intercourse until they and their sex partners have been adequately treated (i.e., for 7 days after a single-dose regimen or after completion of a 7-day regimen) and have resolved any symptoms [28].
7 Conclusions
C. trachomatis is the leading cause of bacterial sexually transmitted diseases and it is responsible for cervicitis, salpingitis, and endometritis. Nowadays, C. trachomatis infection continues to be an important public health problem worldwide because of its increasing incidence [1]. Many infections are asymptomatic and result in delayed diagnosis and uninterrupted transmission. Targeted screening, opportunistic testing for asymptomatic infections, contact tracing, and mandatory notification could be prerequisites to improve the knowledge and the diffusion of this important infection.
References
World Health Organization. Global incidence and prevalence of selected curable sexually transmitted infections-2008. Geneva: WHO; 2012. p. 1–28.
Newman L, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS ONE. 2015;10(12):e0143304.
Workowski KA, Bolan GA, CDC (Centers for Disease Control, Prevention). Sexually transmitted diseases treatment guidelines, 2015. Morb Mortal Wkly Rep. 2015;64(RR3):1–137.
Lanjouw E, Ouburg S, de Vries HJ, Stary A, Radcliffe K, Unemo M. 2015 European guideline on the management of Chlamydia trachomatis infections. Int J STD AIDS. 2016;27(5):333–48.
Redmond SM, et al. Genital chlamydia prevalence in Europe and non-European high income countries: systematic review and meta-analysis. PLoS One. 2015;10(1):e0115753.
Crichton J, Hickman M, Campbell R, Batista-Ferrer H, Macleod J. Socioeconomic factors and other sources of variation in the prevalence of genital chlamydia infections: a systematic review and meta-analysis. BMC Public Health. 2015;15(1):729.
CDC. Sexually transmitted disease surveillance 2016. U.S Dep. Heal. Hum. Serv. 2017.
Schillinger JA, et al. Genotype-specific concordance of chlamydia trachomatis genital infection within heterosexual partnerships. Sex Transm Dis. 2016;43(12):741–9.
Quinn TC, et al. Epidemiologic and microbiologic correlates of Chlamydia trachomatis infection in sexual partnerships. JAMA. 1996;276(21):1737–42.
Bellaminutti S, Seraceni S, de Seta F, Gheit T, Tommasino M, Comar M. HPV and Chlamydia trachomatis co-detection in young asymptomatic women from high incidence area for cervical cancer. J Med Virol. 2014;86(11):1920–5.
Landers DV, Sweet RL. Tubo-ovarian abscess: contemporary approach to management. Rev Infect Dis. 1983;5(5):876–84.
Detels R, Green AM, Klausner JD, Katzenstein D, Gaydos C, Handsfield H, Pequegnat W, Mayer K, Hartwell TD, Quinn TC. The incidence and correlates of symptomatic and asymptomatic Chlamydia trachomatis and Neisseria gonorrhoeae infections in selected populations in five countries. Sex Transm Dis. 2011;38(6):503–9.
Kent CK, Chaw JK, Wong W, Liska S, Gibson S, Hubbard G, Klausner JD. Prevalence of rectal, urethral, and pharyngeal chlamydia and gonorrhea detected in 2 clinical settings among men who have sex with men: San Francisco, California, 2003. Clin Infect Dis. 2005;41(1):67.
Cecil JA, Howell MR, Tawes JJ, Gaydos JC, McKee KT Jr, Quinn TC, Gaydos CA. Features of Chlamydia trachomatis and Neisseria gonorrhoeae infection in male Army recruits. J Infect Dis. 2001;184(9):1216–9.
Martin-Iguacel R, Llibre JM, Nielsen H, Heras E, Matas L, Lugo R, Clotet B, Sirera G. Lymphogranuloma venereum proctocolitis: a silent endemic disease in men who have sex with men in industrialised countries. Eur J Clin Microbiol Infect Dis. 2010;29(8):917–25.
Karim S, Souho T, Benlemlih M, Bennani B. Cervical cancer induction enhancement potential of Chlamydia trachomatis: a systematic review. Curr Microbiol. 2018;75(12):1667–74.
Gottlieb SL, Xu F, Brunham RC. Screening and treating Chlamydia trachomatis genital infection to prevent pelvic inflammatory disease: interpretation of findings from randomized controlled trials. Sex Transm Dis. 2013;40(2):97–102.
Low N, et al. Screening for genital chlamydia infection. Cochrane Database Syst Rev. 2016;2016(9):CD010866.
Wiesenfeld HC. Screening for Chlamydia trachomatis infections in women. N Engl J Med. 2017;376(8):765–73.
Centers for Disease Control and Prevention. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae--2014. MMWR Recomm Rep. 2014;63(2):1–19.
Dombrowski JC. Do women need screening for extragenital gonococcal and chlamydial infections? Sex Transm Dis. 2015;42(5):240–2.
Coll J, et al. Early detection of HIV infection and of asymptomatic sexually transmitted infections among men who have sex with men. Clin Microbiol Infect. 2018;24(5):540–5.
Ong JJ, et al. Should asymptomatic men who have sex with men be screened for oropharyngeal Chlamydia? Clinical outcomes from a cross-sectional study. Sex Transm Dis. 2018;45(2):103–6.
Reyburn H. WHO guidelines for the treatment of Chlamydia trachomatis. Geneva: WHO; 2016.
Luisa F-B, et al. Home-based versus clinic-based specimen collection in the management of Chlamydia trachomatis and Neisseria gonorrhoeae infections SO. Cochrane Database Syst Rev. 2015;9:CD011317.
Levi AW, Beckman D, Hui P, Schofield K, Harigopal M, Chhieng DC. Comparing two methods of detection for Chlamydia trachomatis in liquid-based papanicolaou tests. Am J Clin Pathol. 2012;138(2):236–40.
Kelly H, et al. Systematic reviews of point-of-care tests for the diagnosis of urogenital Chlamydia trachomatis infections. Sex Transm Infect. 2017;93(S4):S22–30.
Committee on Obstetric Practice. Committee opinion. Am J Obstet Gynecol. 2015;654:1–4.
van Aar F, van Benthem BHB, van den Broek IVF, Götz HM. STIs in sex partners notified for chlamydia exposure: implications for expedited partner therapy. Sex Transm Infect. 2018;94(8):619–21.
van der Helm JJ, Koekenbier RH, van Rooijen MS, Schim van der Loeff MF, de Vries HJC. What is the optimal time to retest patients with a urogenital Chlamydia infection? A randomized controlled trial. Sex Transm Dis. 2018;45(2):132–7.
Geisler WM, et al. Azithromycin versus doxycycline for urogenital Chlamydia trachomatis infection. N Engl J Med. 2015;373(26):2512–21.
Kissinger PJ, et al. Azithromycin treatment failure for chlamydia trachomatis among heterosexual men with nongonococcal urethritis. Sex Transm Dis. 2016;43(10):599–602.
Kong FYS, et al. Azithromycin versus doxycycline for the treatment of genital chlamydia infection: A meta-analysis of randomized controlled trials. Clin Infect Dis. 2014;59(2):193–205.
Williams JA, Ofner S, Batteiger BE, Fortenberry JD, Van Der Pol B. Duration of polymerase chain reaction-detectable DNA after treatment of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis infections in women. Sex Transm Dis. 2014;41(3):215–9.
Gannon-Loew KE, Holland-Hall C, Bonny AE. A review of expedited partner therapy for the management of sexually transmitted infections in adolescents. J Pediatr Adolesc Gynecol. 2017;30(3):341–8.
Barbee LA, Khosropour CM, Dombrowski JC, Manhart LE, Golden MR. An estimate of the proportion of symptomatic gonococcal, chlamydial and non-gonococcal nonchlamydial urethritis attributable to oral sex among men who have sex with men: a case-control study. Sex Transm Infect. 2016;92(2):155–60.
Marcus JL, Kohn RP, Barry PM, Philip SS, Bernstein KT. Chlamydia trachomatis and Neisseria gonorrhoeae transmission from the female oropharynx to the male urethra. Sex Transm Dis. 2011;38(5):372–3.
Kintner J, Lajoie D, Hall J, Whittimore J, Schoborg RV. Commonly prescribed beta-lactam antibiotics induce C. trachomatis persistence/stress in culture at physiologically relevant concentrations. Front Cell Infect Microbiol. 2014;4(April):1–10.
Ross J, Guaschino S, Cusini M, Jensen J. 2017 European guideline for the management of pelvic inflammatory disease. Int J STD AIDS. 2018;29(2):108–14.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
De Seta, F., Comar, M., De Santo, D., Larsen, B., Zito, G. (2020). Novel Approach to Chlamydia trachomatis Infections in Female and Male. In: Cristaudo, A., Giuliani, M. (eds) Sexually Transmitted Infections . Springer, Cham. https://doi.org/10.1007/978-3-030-02200-6_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-02200-6_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-02199-3
Online ISBN: 978-3-030-02200-6
eBook Packages: MedicineMedicine (R0)