Abstract
The knee joint, when properly aligned, can support several multiples of body weight during activity and do so reliably over a lifetime. When malaligned, however, the loads placed on the joint are improperly distributed and can lead to pain, debilitation, and premature degradation of the articular cartilage. The treatment of chondral defects, therefore, requires a thorough consideration of malalignment pathologies in all three primary planes: coronal, axial, and sagittal. Various radiographic, computed tomography (CT), and magnetic resonance imaging (MRI) views can be used to assess malalignment and plan corrective treatment whether in a staged setting or concomitantly with cartilage restoration. Accurate assessment and consideration of malalignment pathologies is essential to optimizing cartilage restoration outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The normal knee joint can support a lifetime of repetitive load, generally, without the development of degenerative changes. Excessive stress, which exceeds the tolerance of articular cartilage, disrupts articular homeostasis leading to deterioration of the articular cartilage. In physiological condition, the load applied to the knee joint is distributed across the compartments. Any deviation of the knee alignment, referred to as malalignment, negatively affects load distribution. Improper load distribution reduces the knee joint’s ability to accommodate physiological forces which may cause damage to the articular cartilage.
Cartilage lesions are one of the most challenging pathologies to manage successfully. When conservative treatment fails to relieve symptoms and recover functional limitations, surgery is usually recommended to treat both the cartilage defect and any underlying anatomic abnormalities. Despite these lesions being technically easily accessible, the analysis of concomitant pathologies is difficult; therefore, a rational approach to systematically evaluate and identify pathologic deviation of the knee alignment is required to plan specific treatment that addresses each pathologic component.
Imaging
Radiographic exams are the first step to evaluate knee alignment. A standard knee series includes a weight-bearing anteroposterior (AP) view in full extension, a posterior-anterior view in flexion (PA Rosenberg), full-length hip-to-ankle alignment radiograph, true lateral view, and axial view with 45° or 30° of flexion.
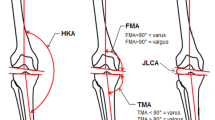
Standard weight-bearing AP and Rosenberg views allow evaluation of femorotibial pathology. A standing hip-to-ankle alignment radiograph is the most accurate method to evaluate mechanical axis of the lower extremity. In a neutrally aligned knee, it is defined as a line from the center of the femoral head to the center of the ankle joint, passing across the center of the knee joint. By definition, if the line is off-center at the knee toward the lateral compartment, it is valgus alignment, and if toward the medial compartment, it is varus alignment (Fig. 3.1).
True lateral view with superposition of both femoral condyles is usually taken with an angle of flexion of 20°. This incidence allows evaluation of tibial slope, patellar height (Insall-Salvati; Caton-Deschamps; Blackburne-Peel), patellar tilt, and trochlear morphology (Dejour classification).
Low flexion axial radiograph allows assessment of trochlea and patella morphology and the position of the patella relative to the trochlea. The difficulty with this technique is that images are not taken near full extension where the trochlea is most shallow. As the knee flexes, the trochlear groove deepens, and the patella slides medially, becoming more congruent with the femoral sulcus. Hence, trochlear dysplasia, patellar tilt, or subluxation are underestimated on the axial view due to the flexion required to obtain this incidence.
Computed tomography (CT) exam provides valuable information regarding the anatomy and kinematics of the knee joint, mainly the patellofemoral joint (PFJ). Allowing a true axial view of the PFJ, this exam can image in different degrees of flexion, letting one accurately define the anatomy and relationship between the patella and the femoral trochlea. Another important contribution of CT is the ability to create overlapping images, allowing assessment of torsional deformities, such as femoral anteversion (FA) and external tibial torsion, as well as measurements of tibial tubercle-trochlear groove (TT-TG) and/or tibial tubercle-posterior cruciate ligament (TT-PCL) distance.
Magnetic resonance imaging (MRI) is the most complete imaging technique. This exam allows for the simultaneous evaluation of all the structures that constitute the knee joint, distinguishing the different tissues. MRI exams can better evaluate articular morphology as well as meniscal and ligament tearing, chondral and osteochondral lesions, rotational deformities, and patellar alignment.
Table 3.1 summarizes clinical exams and imaging studies used to evaluate patellofemoral joint disorders and underlying comorbidities.
Tibiofemoral Alignment and Cartilage Lesions
During a normal gait, knee reaction forces reach three times the body weight, increasing to six times the body weight during higher activity levels. In a normally aligned knee, approximately 60% of the weight-bearing force is transmitted through the medial compartment, the adduction moment being the primary contributing factor to an increased medial joint reaction force [1]. Biomechanical studies have demonstrated that varus and valgus alignment increase medial and lateral load, respectively [2, 3]. Accordingly, malalignment has been recognized as an independent risk factor for development and progression of knee osteoarthritis (OA) [4, 5]. After 18 months of follow-up, a valgus-aligned knee was five times more likely to present progression of lateral compartment OA compared with knees of neutral alignment; similarly, a varus-aligned knee increases risk of medial OA progression by a factor of 4.
Patellofemoral Alignment and Cartilage Lesions
Clinically, extensor mechanism alignment can be assessed measuring Q angle. Described as the direction of the quadriceps force and the patellar tendon reaction force, this angle determines the lateral vector of the extensor mechanism force. Despite the widely discussed potential for inaccuracy of the clinical measurement of the Q angle, a theoretical understanding of the influence of extensor mechanism alignment is crucial to comprehend the influence of anatomical abnormalities on patellofemoral contact forces.
Patellofemoral malalignment is a complex pathology with a wide spectrum of clinical presentation. Several features can influence the Q angle and, consequently, the PF reaction forces. No single factor may be the sole defining etiology, as patellofemoral malalignment is most frequently the result of an association of anatomic abnormalities. Therefore, a global understanding of the pathology is crucial to tailor the most suitable approach in each case.
Coronal Alignment
Both valgus and varus alignment may contribute to modification of the contact stresses in the PFJ [6, 7]. Valgus alignment increases the Q angle, which leads to an increment increase in the lateral vector of the quadriceps force, thereby overloading the lateral side of the PFJ. Conversely, varus alignment tends to reduce the Q angle, shifting the quadriceps force medially, therefore, increasing the contact stress on the medial side of the PFJ [8]. Cahue et al. prospectively showed that valgus alignment was associated with lateral PF OA progression; likewise, varus alignment increased the risk for medial PF OA progression [9].
Axial Alignment
Evaluation of the patellofemoral alignment in the axial plane can be challenging and should be evaluated carefully to understand the true source of abnormality. The tibial tubercle-trochlear groove (TT-TG) distance is one of the most used parameters for the measurement of patellofemoral alignment, being largely correlated with Q angle [10, 11]. This measurement assesses the mediolateral distance between the center of the patellar tendon insertion at the tibial tubercle and the deepest point of the trochlear groove (Fig. 3.2). The TT-TG distance can be measured with ease using both MRI and CT; however, the values resultant from these two techniques may not be interchangeable. Due to discrepancies in knee flexion during image acquisition, MRI exams tend to underestimate the TT-TG distance when compared with CT and should be taken into consideration during surgical planning [12].
TT-TG measurement . Images from the trochlear groove and tibial tubercle are superimposed. Trochlear groove location is determined at the level where the posterior cortex of the femoral condyles is well defined. The trochlear line is drawn perpendicular to the posterior condylar axis, tangential to the posterior femoral condyles (dFCL), and passing through the deepest point of the trochlear groove (TG). Tibial tubercle image is selected at the level of the most anterior point of the tibial tuberosity. A line crossing through the center of the tibial tubercle (TT) is drawn perpendicular to the posterior femoral axis. The distance between these two parallel lines is the TT-TG distance. (Copyright © 2012 American Orthopaedic Society for Sports Medicine. Reprinted from Seitlinger et al. [15] with permission from SAGE publications)
Traditionally, a TT-TG distance of greater than 20 mm is considered pathologic, representing an excessive lateral position of the TT in relation to the trochlea, and has been accepted as the threshold for recommendation of distal realignment [13]. However, a large TT-TG must be interpreted carefully. Other conditions such as trochlear dysplasia, distal femoral internal rotation, or tibial external rotation may lead to increased TT-TG distance; each should be evaluated to determine the site of potential treatment [14, 15]. Tensho et al., compared the influence of trochlea medialization, tibial tubercle lateralization, and knee rotation, and found that knee rotation is the most important factor influencing TT-TG distance [16].
Tibial tubercle-posterior cruciate ligament (TT-PCL) distance was introduced as an adjunct measurement to evaluate the TT position [15]. This parameter is assessed by measuring the distance between the medial margin of the PCL and the midpoint of the TT at the level of the patellar tendon attachment (Fig. 3.3), normal values being less than 24 mm. As it is referenced to the tibia, this parameter is independent of trochlear morphology and femoral rotation. Therefore, femoral rotation abnormalities should be investigated in patients with a TT-TG distance more than 20 mm and normal TT-PCL distance.
TT-PCL measurement. Proximal tibia (below the joint and above the head of the fibula) and patellar tendon insertion (most inferior slice in which the ligament could still be clearly identified) images are superimposed. The TT-PCL distance is the mediolateral distance between the medial border of the posterior cruciate ligament (PCL) and the center of the insertion of the patellar tendon. Both lines are drawn perpendicular to a posterior tibial condyles reference line (dTCL), tangential to the proximal tibia below the joint and above the head of the fibula. (Copyright © 2012 American Orthopaedic Society for Sports Medicine. Reprinted from Seitlinger et al. [15] with permission from SAGE publications)
The Q angle is also influenced by the rotational interaction between the femur and tibia. Lateral rotation of the tibia in relation to the femur moves the tibial tubercle (TT) laterally, resulting in an increase in the Q angle [17, 18]. Similarly, increased femoral anteversion leads to internal rotation of the distal femur, moving the patella medially, thereby, increasing the Q angle [19, 20].
During normal gait, the knee joint axis rotates externally, in relation to the pelvis, during the swing phase, and moves internally during the stance phase. The increment of the femoral anteversion leads to an abnormal internally rotated gait. While the body is moving forward, the knee joint axis is pointing medially. This leads to an increased internal rotation of the knee joint axis during stance phase, causing excessive lateral forces on the patella. This excessive lateralization increases tension on the MPFL and pressure on the lateral side of the patellofemoral joint while unloading the medial side. Hence, increased FA results in abnormal lateral patellofemoral pressure and the tendency for lateral subluxation.
Several techniques have been described to assess rotational alignment of the inferior limb. Femoral, tibial, and knee torsion can be assessed by overlapping axial cuts from the femoral head, base of the femoral neck or lesser trochanter, the knee joint (either tangent to the posterior condyles or between the medial and lateral epicondyles), the proximal tibia at the joint, and the ankle joint. Either CT or MRI studies can provide similar measurements. Femoral anteversion can be measured by drawing a line from the center of the femoral neck to the femoral head and distally either along the transepicondylar axis (mean value 7.4°) or the tangent of the posterior femoral condyles (mean value 13.1°). These values differ by about 6°, with a range of 11° of retroversion to 22° of anteversion (Fig. 3.4) [21].
Numerous studies have highlighted the importance of tibial torsion on patellar tracking [17, 22]. There is no consensus concerning the measurement techniques to determine the tibial torsion. Thus, the lack of a standardized method to measure tibial torsion is a major stumbling block to determining a pathologic threshold for this abnormality. Both MRI and CT studies have been demonstrated as reliable reproducible methods to assess tibial torsion [23, 24]. The measurement is taken from two superimposed axial images: one of the proximal tibial epiphysis right above the proximal end of the fibula and the other tangent to the talar dome. This is the angle between the line tangent to the posterior tibial plateau rim and the bimalleolar axis as drawn through the centers of the anteroposterior aspect of the lateral and medial malleoli [24, 25].
Biomechanical studies have shown the influence of both tibial and femoral rotation on patellofemoral contact pressure. Lee et al. demonstrated that increased external tibial rotation resulted in a lateral shift of the patella, thus increasing the pressure on the lateral facet [17]. A comparison of patients with chronic patellofemoral symptoms and asymptomatic controls showed that symptomatic patients presented significant increased external tibial torsion compared to controls [22]. Moreover, a biomechanical study analyzing PF contact pressures demonstrated that if a torsional and an angular deformity coexist, the rotatory component causes greater PF changes [26]. Takai et al. have evaluated femoral and tibial torsion in patients with unicompartmental PF arthrosis and demonstrated the high correlation between PF arthrosis and increased femoral anteversion (23° of femoral anteversion in the PF OA group versus 9° of anteversion in the control group) [27]. Similarly, Lerat has found an increased risk for patellar chondropathy in patients with increased internal femoral torsion [28].
Patellar tilt and subluxation are additional factors that indicate PF malalignment and have been associated with deterioration of PF cartilage laterally. Patellar position can be easily assessed using axial radiographs or axial images from MRI or CT; however, the source of this incongruence is multifactorial and requires a deeper evaluation. In addition to the rotational deviation described earlier, a laxity or weakness of medial soft tissue restraints, such as the MPFL and vastus medialis, and/or a lateral tethering lead to an overload of the lateral facet. In this case, physical evaluation demonstrates a decrease in medial-lateral patellar translation.
Sagittal Alignment
The position of the patella in the sagittal axis is an additional factor influencing patellofemoral tracking. Essentially, patella alta or infera must be evaluated using an identified index. The main indexes currently used in the literature are Insall-Salvati, Caton-Deschamps, and Blackburne-Peel. All imaging techniques (lateral view radiographs, MRI, and CT) have demonstrated reliable and reproducible methods for measurement and can be interchangeable when assessing patellar height [29]. Mehl et al., in a case control study comparing patients with cartilage defects and normal controls, found that 67% of patients with a chondral lesion showed a pathologic Insall-Salvati index of >1.2, while this ratio was only 25.6% of the control group [30]. Additionally, an observational study of patients with osteoarthritis showed a significant association between patellar alignment and cartilage loss in both lateral and medial sides [31].
Patellofemoral Geometry
In addition to patellofemoral alignment, but no less significant, the contour of the trochlea and the patella is an important contributor to the patellofemoral contact force and consequently a risk factor for patellofemoral cartilage lesions. The geometry of the trochlea has been recognized as a risk factor for the development of cartilage lesions of the PF joint. Several studies have correlated patellofemoral cartilage loss with flat or shallow trochlea [31,32,33]. Historically, trochlea morphology was mainly assessed using axial radiography or CT using bone landmarks. However, bone reference may not reproduce the articular cartilage surface, and investigation with MRI is advisable [34].
Summary
In conclusion, identification and correction of underlying abnormal patellofemoral alignment is crucial for successful cartilage repair in the patellofemoral joint. Patients with full-thickness cartilage defects of the patella frequently demonstrate a high number of co-pathologies in association. Therefore, these pathologies must be identified accurately and considered carefully when planning surgical treatment of patellofemoral cartilage defects.
References
Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–27.
Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25(3):367–77.
McKellop HA, Llinás A, Sarmiento A. Effects of tibial malalignment on the knee and ankle. Orthop Clin North Am. 1994;25(3):415–23.
Sharma L, Chmiel JS, Almagor O, Felson D, Guermazi A, Roemer F, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M. The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis. 2013;72(2):235–40. https://doi.org/10.1136/annrheumdis-2011-201070.
Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61(4):459–67. https://doi.org/10.1002/art.24336.
Weinberg DS, Tucker BJ, Drain JP, Wang DM, Gilmore A, Liu RW. A cadaveric investigation into the demographic and bony alignment properties associated with osteoarthritis of the patellofemoral joint. Knee. 2016;23(3):350–6. https://doi.org/10.1016/j.knee.2016.02.016.
McWalter EJ, Cibere J, MacIntyre NJ, Nicolaou S, Schulzer M, Wilson DR. Relationship between varus-valgus alignment and patellar kinematics in individuals with knee osteoarthritis. J Bone Joint Surg Am. 2007;89(12):2723–31. https://doi.org/10.2106/JBJS.F.01016.
Schön SN, Afifi FK, Rasch H, Amsler F, Friederich NG, Arnold MP, Hirschmann MT. Assessment of in vivo loading history of the patellofemoral joint: a study combining patellar position, tilt, alignment and bone SPECT/CT. Knee Surg Sports Traumatol Arthrosc. 2013;22(12):3039–46. https://doi.org/10.1007/s00167-013-2698-2.
Cahue S, Dunlop D, Hayes K, Song J, Torres L, Sharma L. Varus-valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum. 2004;50(7):2184–90. https://doi.org/10.1002/art.20348.
Ho CP, James EW, Surowiec RK, Gatlin CC, Ellman MB, Cram TR, Dornan GJ, LaPrade RF. Systematic technique-dependent differences in CT versus MRI measurement of the tibial tubercle-trochlear groove distance. Am J Sports Med. 2015;43(3):675–82. https://doi.org/10.1177/0363546514563690.
Dickschas J, Harrer J, Bayer T, Schwitulla J, Strecker W. Correlation of the tibial tuberosity–trochlear groove distance with the Q-angle. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):915–20. https://doi.org/10.1007/s00167-014-3426-2.
Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS, Dahm DL. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41(8):1835–40. https://doi.org/10.1177/0363546513484895.
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26.
Daynes J, Hinckel B, Farr J. Tibial tuberosity—posterior cruciate ligament distance. J Knee Surg. 2016;29(06):471–7. https://doi.org/10.1055/s-0035-1564732.
Seitlinger G, Scheurecker G, Hogler R, Labey L, Innocenti B, Hofmann S. Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012;40(5):1119–25. https://doi.org/10.1177/0363546512438762.
Tensho K, Akaoka Y, Shimodaira H, Takanashi S, Ikegami s KH, Saito N. What components comprise the measurement of the tibial tuberosity-trochlear groove distance in a patellar dislocation population? J Bone Joint Surg Am. 2015;97(17):1441–8. https://doi.org/10.2106/JBJS.N.01313.
Lee TQ, Yang BY, Sandusky MD, McMahon PJ. The effects of tibial rotation on the patellofemoral joint: assessment of the changes in in situ strain in the peripatellar retinaculum and the patellofemoral contact pressures and areas. J Rehabil Res Dev. 2001;38(5):463–9.
Hefzy MS, Jackson WT, Saddemi SR. Effects of tibial rotations on patellar tracking and patello-femoral contact areas. J Biomed Eng. 1992;14(4):329–43.
Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res. 1994;302:69–74.
van Kampen A, Huiskes R. The three-dimensional tracking pattern of the human patella. J Orthop Res. 1990;8(3):372–82. https://doi.org/10.1002/jor.1100080309.
Yoshioka Y, Cooke TDV. Femoral anteversion: assessment based on function axes. J Orthop Res. 1987;5(1):86–91. https://doi.org/10.1002/jor.1100050111.
Cooke TDV, Price N, Fisher B, Hedden D. The inwardly pointing knee. An unrecognized problem of external rotational malalignment. Clin Orthop Relat Res. 1990;260:56–60. https://doi.org/10.1097/00003086-199011000-00011.
Basaran SH, Ercin E, Bayrak A, Cumen H, Bilgili MG, Inci E, Avkan MC. The measurement of tibial torsion by magnetic resonance imaging in children: the comparison of three different methods. Eur J Orthop Surg Traumatol. 2015;25(8):1327–32. https://doi.org/10.1007/s00590-015-1694-2.
Folinais D, Thelen P, Delin C, Radier C, Catonne Y, Lazennec JY. Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop Traumatol Surg Res. 2013;99(5):509–16. https://doi.org/10.1016/j.otsr.2012.12.023.
Reikerås O, Høiseth A. Torsion of the leg determined by computed tomography. Acta Orthop Scand. 1989;60(3):330–3.
Fujikawa K, Seedhom BB, Wright V. Biomechanics of the patello-femoral joint. Part I: a study of the contact and the congruity of the patello-femoral compartment and movement of the patella. Eng Med. 1983;12(1):3–11.
Takai S, Sakakida K, Yamashita F, Suzu F, Izuta F. Rotational alignment of the lower limb in osteoarthritis of the knee. Int Orthop. 1985;9(3):209–15.
Lerat JL, Moyen B, Bochu M, Galland O. Femoropatellar pathology and rotational and torsional abnormalities of the inferior limbs: the use of CT scan. In: Müller W, Hackenbruch W, editors. Surgery and arthroscopy of the knee. Berlin: Springer; 1988. p. 61–5. https://doi.org/10.1007/978-3-642-72782-5_11.
Lee PP, Chalian M, Carrino JA, Eng J, Chhabra A. Multimodality correlations of patellar height measurement on X-ray, CT, and MRI. Skelet Radiol. 2012;41(10):1309–14. https://doi.org/10.1007/s00256-012-1396-3.
Mehl J, Feucht MJ, Bode G, Dovi-Akue D, Südkamp NP, Niemeyer P. Association between patellar cartilage defects and patellofemoral geometry: a matched-pair MRI comparison of patients with and without isolated patellar cartilage defects. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):838–46. https://doi.org/10.1007/s00167-014-3385-7.
Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Felson DT, Hunter D. The association between patellar alignment and patellofemoral joint osteoarthritis features an MRI study. Rheumatology. 2007;46(8):1303–8. https://doi.org/10.1093/rheumatology/kem095.
Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol. 2010;194(3):721–7. https://doi.org/10.2214/AJR.09.3008.
Tsavalas N, Katonis P, Karantanas AH. Knee joint anterior malalignment and patellofemoral osteoarthritis: an MRI study. Eur Radiol. 2012;22(2):418–28. https://doi.org/10.1007/s00330-011-2275-3.
Salzmann GM, Weber TS, Spang JT, Imhoff AB, Schöttle PB. Comparison of native axial radiographs with axial MR imaging for determination of the trochlear morphology in patients with trochlear dysplasia. Arch Orthop Trauma Surg. 2009;130(3):335–40. https://doi.org/10.1007/s00402-009-0912-y.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ambra, L.F., Gomoll, A.H., Farr, J. (2019). Coronal and Axial Alignment: The Effects of Malalignment. In: Yanke, A., Cole, B. (eds) Joint Preservation of the Knee. Springer, Cham. https://doi.org/10.1007/978-3-030-01491-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-01491-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-01490-2
Online ISBN: 978-3-030-01491-9
eBook Packages: MedicineMedicine (R0)