Abstract
Purpose
Coronal alignment of the knee is defined by the hip–knee–ankle angle (HKA), the femoral mechanical angle (FMA), the tibial mechanical angle (TMA), and the joint line convergence angle (JLCA). To date, there is still a lack of knowledge about the variability of native coronal knee alignment. The purpose of this paper is to present a systematic review of the current literature about the variability of coronal knee alignment (HKA, FMA, TMA, and JLCA) in non-osteoarthritic knees.
Methods
The electronic databases MEDLINE, EMBASE, and Google Scholar were searched from database inception to search date (November 1, 2018) and screened for relevant studies. The PRISMA guidelines were followed. Inclusion criteria were studies that reported the coronal alignment of the native, non-osteoarthritic knee.
Results
A total of 15 studies met the inclusion criteria. Thirteen studies performed the measurements on weight-bearing long-leg standing radiographs (LLR), one study used MRI, and one study used the EOS imaging system. The mean HKA ranged from 176.7° ± 2.8° (male) to 180.7° (female). The mean FMA ranged from 92.08° ± 1.78° (female) to 97.2° ± 2.7° (female). The mean TMA ranged from 84.6° ± 2.5° (female) to 89.6° (female). The mean JLCA ranged from − 0.47° ± 0.98° (male) to − 1.9° ± 1.4° (female).
Conclusion
This systematic review provides a detailed overview about the variability of the coronal knee alignment in non-osteoarthritic knees. The broad variability of all coronal alignment parameters highlights the necessity for a more anatomic and individualized approach in knee arthroplasty. It also offers the fundament to understand the changes in osteoarthritic knees.
Level of clinical evidence
Systematic review, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The coronal alignment of the knee is defined by the hip–knee–ankle angle (HKA) [18], and can be measured as the angle between the mechanical axes of the femur and the tibia [4, 9]. A mean native coronal knee alignment of 180° is regarded as physiological in non-osteoarthritic knees and referred to as being neutral [2, 30]. If the HKA is larger than 180°, the knee alignment is classified as valgus and lower than 180° as varus [3]. However, studies have shown that the mean HKA tends to be slightly in varus [2, 9, 18]. This raises the question whether an HKA of 180° really represents a “normal” knee alignment [2].
Another important factor of coronal alignment is the joint line orientation [10, 11]. The joint line of the femur can be measured by the angle between the mechanical axis of the femur and the tangent to the most distal part of the femoral condyles (femoral mechanical angle, FMA) and the joint line of the tibia can be measured by the angle between the mechanical axis of the tibia and the tangent to the tibial plateau (tibial mechanical angle, TMA) [18]. The joint line orientation is on average in 3° varus, which means that the articular surface of the femur is in 3° valgus, whereas the articular surface of the tibia is in 3° varus in relation to their mechanical axes. However, some authors reported substantial deviations from these values [1, 14, 20, 29].
Coronal laxity of the knee is mainly affected by the medial and lateral collateral ligaments (MCL, LCL) [5, 17]. Ligamentous laxity of either the MCL or LCL can result in a medial or lateral joint space opening, respectively. The joint space opening can be measured by the joint line convergence angle (JLCA), representing the angle between the joint lines of the femur and tibia. The summation of FMA, TMA, and JLCA adds up to the HKA [4].
Whereas the HKA can be approximately measured by a goniometer during physical examination, the TMA, FMA, and JLCA can only be measured by imaging modalities such as radiographs, EOS imaging, MRI, or CT [2, 21, 26].
However, to date, there is no sufficient evidence about the distribution and variability of coronal knee alignment in non-osteoarthritic knees with regards to all coronal alignment parameters.
The purpose of this paper is to present a systematic review of current literature about the variability of coronal knee alignment (HKA, FMA, TMA, and JLCA) in non-osteoarthritic knees.
Material and methods
Search strategy
The electronic databases MEDLINE (PubMed), EMBASE, and Google Scholar were searched by two reviewers (LM and SH) from database inception to search date (November 1, 2018) and screened for relevant studies. The following keywords were used: (phenotypes OR morphology OR anatomy OR alignment) AND (coronal OR neutral OR varus OR valgus) AND (knee OR femur OR tibia) AND (healthy OR normal OR non-osteoarthritic OR native). Table 1 details the executed search strategy.
The search terms led to 1896 records. Their relevance was evaluated in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA).
Articles which reported the coronal alignment of native, non-osteoarthritic knees were included. Studies in English and German were considered.
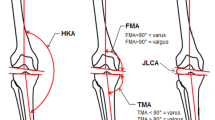
The following alignment angles were included: the HKA (medial angle between the mechanical axes of the femur and the tibia), the FMA (medial angle between the mechanical axis of the femur and the tangent to the distal femoral condyles), the TMA (medial angle between the mechanical axis of the tibia and the tangent to the tibial plateau), and the JLCA (the medial angle between the distal femoral joint line and the proximal tibial joint line in the coronal plane). Figure 1 illustrates the included angles.
Hip–knee–ankle angle (HKA, medial angle between the mechanical axes of the femur and the tibia), femoral mechanical angle (FMA, medial angle between the mechanical axis of the femur and a tangent to the distal femoral condyles), tibial mechanical angle (TMA, medial angle between the mechanical axis of the tibia and a tangent to the tibial plateau), and the joint line convergence angle (JLCA, the medial angle between the distal femoral joint line and the proximal tibial joint line)
Some authors used the same mechanical axes, but they measured the medial FMA instead of the lateral FMA and the lateral TMA, instead of the medial TMA. However, as the medial and lateral angles are complementary to each other and they add up to 180°, values were calculated for reasons of comparability and medial angles were used for reasons of consistency.
Exclusion criteria were the following: studies dealing with osteoarthritic patients, patients younger than 16 years and older than 45 years. Studies used different axes for reference than mentioned above.
Study screening
Two reviewers independently screened the titles, abstracts, and full texts of all retrieved articles (LM and SH). Discrepancies at the title and abstract stages were resolved by automatic inclusion to ensure thoroughness. Discrepancies at the full-text stage were resolved by consensus between the two reviewers. If a consensus could not be reached, a third, more senior reviewer (MTH) helped to resolve the discrepancy. The references of included studies were then screened to capture any articles that may have been missed.
A total of 511 duplicates were removed and 1332 studies were excluded by reading their titles and/or abstracts. Fifty-three full-text articles were assessed for eligibility, 31 articles did not measure HKA, FMA, TMA, or JLCA, and 7 articles included patients younger than 16 years and/or older than 45 years. This strategy left a total of 15 articles from which all relevant data were extracted. The detailed selection process can be seen in Fig. 2.
Finally, 15 studies were included in this systematic review, published between 1987 and 2017 (Table 2). Thirteen studies performed the measurements on weight-bearing long-leg standing radiographs (LLR), one study used magnetic resonance imaging (MRI), and one study the EOS imaging system. The study cohort ranged from 25 to 273 patients and the mean age ranged from 21 to 37 years.
Data extraction
Two reviewers (LM, SH) independently extracted relevant data from included articles and recorded these data in a Microsoft Excel (Microsoft Office Package, USA) spreadsheet designed a priori. Demographic information included author, year of publication, imaging modality, sample size, and patient demographics (i.e. sex, age, etc.).
Quality assessment of included studies
Since the studies used different imaging modalities and investigated a various study population, the authors were unable to compare their methods and levels of evidence using an established quality assessment standard.
Statistical analysis
Descriptive statistics, such as means, ranges, and measures of variance [e.g. standard deviations, 95% confidence intervals (CI)], are presented where applicable. No meta-analysis was performed, as there was high heterogeneity amongst the studies and multiple indirect comparisons.
Results
Fourteen studies [2, 3, 8, 9, 12, 13, 16, 18, 19, 23, 26,27,28,29] reported the mean HKA angle that ranged from 176.7° ± 2.8° (male) [16] to 180.7° (female) [29] (Table 3). Only three studies reported the range of the mean HKA [18, 23, 28]. However, the widest range was 16.1° from 167.7°–183.8° [23].
One study did not distinguish between male and female patients [27]. Three studies included only male patients [16, 18, 19] and one study included only female patients [26]. A closer look into HKA gender distribution reveals that gender differences do exist. Twelve studies [2, 3, 8, 9, 12, 13, 16, 18, 19, 23, 28, 29] investigated the HKA in male patients showing a mean HKA between 176.7° ± 2.8° [16] and 179.06° ± 0.42° [8], whereas ten studies [2, 3, 8, 9, 12, 13, 23, 26, 28, 29] showed a mean HKA in female patients between 177.8° ± 2.5 [28] to 180.7° [29]. These results support the current evidence that male knees are slightly more in varus than female knees. Furthermore, all studies that investigated the influence of gender on HKA found significant differences [2, 3, 8, 12, 23, 28].
Five studies [2, 3, 12, 19, 26] measured the mean FMA between 92.08° ± 1.78° (female) [2] and 97.2° ± 2.7° (female) [12] (Table 4). Three studies compared both genders [2, 3, 12], one study evaluated only male patients [19], and another study only female patients [26]. No study reported the range of the FMA.
Ten studies [2, 3, 13, 16, 18, 20, 23, 26, 28, and 29] evaluated the mean of TMA, which ranged from 84.6°± 2.5° (female) [28] to 89.6° [29] (Table 5). One studies did not distinguish between gender [23], six studies separated the results according to gender [2, 3, 13, 20, 28, 29] and two studies included only male patients [16, 18]. The widest range was 11.5° from 78° to 89.5° [28].
Four studies presented data on the JLCA [2, 3, 12, 20]. These ranged from − 0.47° ± 0.98° (male) [2] to − 1.9° ± 1.4° (female) [3] (Table 6). However, no study reported the range of JLCA. HKA, FMA, TMA, and JLCA according to gender are presented in Figs. 3, 4, 5, and 6.
Discussion
The most important findings of the present review are the following:
Restoration of a neutral mechanical alignment with an HKA of 180° is considered as one important factor for good outcome after TKA [22, 24, 25]. However, the variability of coronal alignment in native knees raises the question if an alignment of 180° really is “normal” and should be the target in TKA for all patients [2, 6]. Should patients with a non-neutral alignment (either varus or valgus) be aligned neutrally, even when it is not their native knee alignment? To answer this question, all coronal alignment parameters and not only the HKA need to be considered.
The mean FMA varied more than 5° from 92.08°±1.78° (female) [2] and 97.2° ± 2.7° (female) [12].The mean TMA varied 5° (from 84.6°±2.5° [28] to 89.6° [29]) showing a widest range of 12°. The mean JLCA varied more than 1° (from − 0.47° ± 0.98° [2] to − 1.9°±1.4° [3]). This clearly contradicts the assumption that the native joint lines of the femur and tibia are in 3° valgus (FMA of 93°) and 3° varus (TMA of 87°), respectively.
Gender differences are not unambiguously clear. Whereas Bellemans et al. reported an almost equal FMA, Cooke et al. and Jabalameli et al. found a higher FMA in female patients [2, 3, 12]. From the six studies investigating the TMA according to gender, two authors showed a higher angle for male patients [20, 28] and four studies reported higher angles for female patients [2, 4, 13, 29]. One study reported equal JLCA [20], two studies a higher JLCA for female knees [2, 4], and one study a higher JLCA for male knees [12].
In a landmark study, Bellemans et al. investigated the incidence of constitutional varus in 250 patients (m:f 125:125; age between 20 and 27 years) on full-leg standing digital radiographs [2]. They defined a neutral alignment of ± 3°, constitutional varus < 177°, and constitutional valgus > 183°. They found that 80 (32%) male knees and 43 (17.2%) female knees had a constitutional varus. Only five (2%) and seven (2.8%) of the male and female knees had a constitutional valgus. Consequently, two other authors also investigated the incidence of constitutional varus in their population using the same definition as Bellemans et al. [23, 26]. Shetty et al. investigated a mixed Indian and Korean population having 40% of the male knees in varus and 28% of the female knees in varus [23]. Song et al. only examined female Korean knees and found less knees in varus (20.34%) [26].
The mean HKA in Bellemans et al. was significantly smaller in the male knees (178.23° ± 2.42°) than in the female ones (179.21° ± 2.13°) (p < 0.0001). As most significant contributing factors to a constitutional varus the TMA (40.8%) and the FMA (29.4%) were identified. Whereas the TMA significantly differed between male and female knees (86.50°± 2.17°:87.58° ± 1.82°), no significant differences were observed for the FMA (87.88° ± 1.70°: 87.92° ± 1.78°) and JLCA (0.47° ± 0.98°:0.56° ± 1.12°).
The present systematic review has a considerable number of limitations. First, the studies included in this systematic review used different imaging and measurement methodologies. Most of the studies investigated the alignment on plain long-leg radiographs (n = 13) [2, 3, 9, 12, 13, 16, 18,19,20, 23, 26,27,28], one study used EOS imaging [29] devices, and only one author used MRI [8]. Although some authors used CT for measurements on osteoarthritic knees [15, 31], there are, to date, no data of 3D-reconstructed CT scans in non-osteoarthritic knees. However, 3D-CT represents the technique with the highest accuracy in determining anatomical landmarks and should be used for exact alignment measurements [7].
Second, many authors did not report the range of their results. This would have been of particular interest for this review. However, the variability can be sufficiently evaluated using the different mean values and their standard deviations.
Third, some studies did not distinguish between male and female patients. However, our review showed that great differences between genders exist.
Despite the above-mentioned weaknesses, this review is the first to comprehensively show the variability of all coronal alignment parameters in non-osteoarthritic knees. A further systematic review of osteoarthritic knees would help to assess the possible changes of coronal alignment in osteoarthritic knees.
Conclusion
This systematic review provides a detailed overview about the variability of the coronal knee alignment in non-osteoarthritic knees. The broad variability of all coronal alignment parameters highlights the necessity for a more individualized approach in knee arthroplasty. It also offers the fundament to understand the changes in osteoarthritic knees.
Abbreviations
- HKA:
-
Hip–knee–ankle angle
- FMA:
-
Femoral mechanical angle
- TMA:
-
Tibial mechanical angle
- JLCA:
-
Joint line convergence angle
- LLR:
-
Long-leg radiographs
- MRI:
-
Magnet resonance imaging
- CT:
-
Computed tomography
References
Altman RD, Fries JF, Bloch DA, Carstens J, Cooke TD, Genant H et al (1987) Radiographic assessment of progression in osteoarthritis. Arthritis Rheum 30:1214–1225
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P (1997) Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage 5:39–47
Cooke TD, Li J, Scudamore RA (1994) Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am 25:387–393
Deep K (2014) Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 472:3426–3431
Hirschmann MT, Behrend H (2018) Functional knee phenotypes: a call for a more personalised and individualised approach to total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4973-8
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Jt Surg Br 93:629–633
Hovinga KR, Lerner AL (2009) Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J Orthop Res 27:1191–1196
Hsu RW, Himeno S, Coventry MB, Chao EY (1990) Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res 255:215–227
Hungerford DS, Krackow KA (1985) Total joint arthroplasty of the knee. Clin Orthop Relat Res 192:23–33
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Jabalameli M, Moghimi J, Yeganeh A, Nojomi M (2015) Parameters of lower extremities alignment view in Iranian adult population. Acta Med Iran 53:293–296
Khattak MJ, Umer M, Davis ET, Habib M, Ahmed M (2010) Lower-limb alignment and posterior tibial slope in Pakistanis: a radiographic study. J Orthop Surg (Hong Kong) 18:22–25
Lampart M, Behrend H, Moser LB, Hirschmann MT (2018) Due to great variability fixed HKS angle for alignment of the distal cut leads to a significant error in coronal TKA orientation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5041-0
Luyckx T, Zambianchi F, Catani F, Bellemans J, Victor J (2013) Coronal alignment is a predictor of the rotational geometry of the distal femur in the osteo-arthritic knee. Knee Surg Sports Traumatol Arthrosc 21:2331–2337
Maini L, Singh S, Kushwaha NS, Saini A, Rohilla S, Sharma H et al (2015) Radiographic analysis of the axial alignment of the lower extremity in Indian adult males. J Arthrosc Jt Surg 2:128–131
Markolf KL, Mensch JS, Amstutz HC (1976) Stiffness and laxity of the knee–the contributions of the supporting structures. A quantitative in vitro study. J Bone Jt Surg Am 58:583–594
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Mullaji AB, Marawar SV, Mittal V (2009) A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J Arthroplasty 24:861–867
Nakano N, Matsumoto T, Hashimura M, Takayama K, Ishida K, Araki D et al (2016) Coronal lower limb alignment in normal knees–a radiographic analysis of 797 normal knee subjects. Knee 23:209–213
Nam D, Shah RR, Nunley RM, Barrack RL (2014) Evaluation of the 3-dimensional, weight-bearing orientation of the normal adult knee. J Arthroplasty 29:906–911
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Shetty GM, Mullaji A, Bhayde S, Nha KW, Oh HK (2014) Factors contributing to inherent varus alignment of lower limb in normal Asian adults: role of tibial plateau inclination. Knee 21:544–548
Slevin O, Hirschmann A, Schiapparelli FF, Amsler F, Huegli RW, Hirschmann MT (2018) Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc 26:1602–1609
Slevin O, Schmid FA, Schiapparelli FF, Rasch H, Amsler F, Hirschmann MT (2017) Coronal femoral TKA position significantly influences in vivo patellar loading in unresurfaced patellae after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3605–3610
Song MH, Yoo SH, Kang SW, Kim YJ, Park GT, Pyeun YS (2015) Coronal alignment of the lower limb and the incidence of constitutional varus knee in korean females. Knee Surg Relat Res 27:49–55
Tanaka T, Takayama K, Hashimoto S, Kanzaki N, Hayashi S, Kuroda R et al (2017) Radiographic analysis of the lower limbs using the hip-calcaneus line in healthy individuals and in patients with varus knee osteoarthritis. Knee 24:1146–1152
Tang WM, Zhu YH, Chiu KY (2000) Axial alignment of the lower extremity in Chinese adults. J Bone Jt Surg Am 82-A:1603–1608
Than P, Szuper K, Somoskeoy S, Warta V, Illes T (2012) Geometrical values of the normal and arthritic hip and knee detected with the EOS imaging system. Int Orthop 36:1291–1297
Thienpont E, Schwab PE, Cornu O, Bellemans J, Victor J (2017) Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg 137:393–400
Thienpont E, Schwab PE, Paternostre F, Koch P (2014) Rotational alignment of the distal femur: anthropometric measurements with CT-based patient-specific instruments planning show high variability of the posterior condylar angle. Knee Surg Sports Traumatol Arthrosc 22:2995–3002
Funding
There was no financial conflict of interest with regards to this study.
Author information
Authors and Affiliations
Contributions
LBM participated in study design, literature review, data collection, figures and tables, and manuscript writing. SH participated in literature review, data collection, and manuscript editing. FA participated in study design and manuscript editing. HB participated in study design and manuscript editing. MTH participated in study design and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was not required as this is a pure review of the literature not involving humans nor animals.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moser, L.B., Hess, S., Amsler, F. et al. Native non-osteoarthritic knees have a highly variable coronal alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 27, 1359–1367 (2019). https://doi.org/10.1007/s00167-019-05417-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05417-2