Abstract
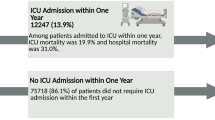
Immunocompromised children and adolescent patients who have hematologic or oncologic diseases represent a small percentage of patients treated in pediatric intensive care units (PICUs) but have a disproportionately high mortality rate. A single-center study of 1278 patients admitted to a pediatric hematology-oncology service over an 11-year period found an admission rate of 4.2% with an overall PICU mortality rate of 38.9% (Faraci et al. J Pediatr Hematol Oncol 36(7): e403–9, 2014). Risk factors for PICU admission included older age, diagnosis of nonmalignant disease, and treatment with HCT. A more recent retrospective multicenter cohort analysis of almost 250,000 consecutive PICU admissions using the Virtual PICU Systems database identified 10,365 patients diagnosed with a malignancy who were admitted to PICUs for reasons other than perioperative admissions during the study period (Zinter et al. Intensive Care Med 40(10): 1536–44, 2014). Children with any cancer accounted for 11.4% of all PICU deaths and had mortality of 6.8% (43% in those who were mechanically ventilated) compared to 2.4% in patients without malignancy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Immunocompromised children and adolescent patients who have hematologic or oncologic diseases represent a small percentage of patients treated in pediatric intensive care units (PICUs) but have a disproportionately high mortality rate. A single-center study of 1278 patients admitted to a pediatric hematology-oncology service over an 11-year period found an admission rate of 4.2% with an overall PICU mortality rate of 38.9% [1]. Risk factors for PICU admission included older age, diagnosis of nonmalignant disease, and treatment with HCT. A more recent retrospective multicenter cohort analysis of almost 250,000 consecutive PICU admissions using the Virtual PICU Systems database identified 10,365 patients diagnosed with a malignancy who were admitted to PICUs for reasons other than perioperative admissions during the study period [2]. Children with cancer accounted for 11.4% of all PICU deaths and had mortality of 6.8% (43% in those who were mechanically ventilated) compared to 2.4% in patients without malignancy.
Outcome data regarding patients admitted to PICUs who have nonmalignant hematologic or immunologic diseases is limited, with the exception of those treated with hematopoietic cell transplantation (HCT). Far more is known about patients with oncologic diagnoses, and the literature is most robust regarding those treated with HCT. The survival of children with hematologic and oncologic diseases has improved in recent years despite remaining higher than those of other patients treated in the PICU (Table 1.1). A meta-analysis of mortality trends of children treated in the PICU after HCT over time showed a significant decrease in mortality associated with the year of inclusion as did a large single-center study comparing outcomes over time [3, 4]. However, interpreting comparisons of mortality across multiple studies must be done with caution. The published literature is comprised almost exclusively of retrospective studies, and the inclusion criteria are not consistent across studies. Some studies include only those felt to be at highest risk for worst outcome, specifically HCT patients supported with mechanical ventilation, whereas others include patients with all oncology diagnoses and admitted to the PICU for all indications. There are multiple reasons for the improved outcomes including scientific advances in critical care, hematology, oncology, and HCT. Equally important have been advances in supportive care and infectious disease management.
The severity of illness of immunocompromised hematology and oncology patients admitted to PICUs is broad including planned postoperative admissions, semi-urgent admissions of patients with worsening illness, and the emergent transfer of rapidly decompensating children. Equally broad are the reasons for critical illness in this diverse population including infection, organ compromise, and complications of the primary disease. The management of critically ill immunocompromised children and adolescents must be guided by the primary disease and patient’s treatment. General principles of the initial management and stabilization of critically ill hematology and oncology patients, in most cases, can follow practices applied to other children. Thereafter, the management is strongly influenced not only by the reason for the need for critical care, but by the unique features of the underlying disease as well. For example, the early care of a child with sickle cell anemia experiencing acute respiratory dysfunction may mirror that of a patient with acute lymphoblastic leukemia or one with severe combined immune deficiency. After the primary stabilization of the patient, an understanding of the underlying disease is key to the next steps of diagnosis and management. In the example, one may consider acute chest syndrome as the cause of the respiratory distress in the patient with sickle cell anemia. Clearly this would not be on the list of potential etiologies in a child with leukemia in whom infection may be a chief concern. The therapy that the child receives to treat the primary disease is important as the critical illness may be a direct result or influenced heavily by the treatment. A clear example is that of children undergoing HCT who may have organ compromise, bleeding, infection, graft-versus-host disease, and other toxicities related to the recent and past therapy in addition to underlying comorbidities.
A goal of this textbook is to provide an understanding of the specific aspects of different diagnoses and therapies that impact the critical care of immunocompromised hematology and oncology patients. It is unrealistic to expect PICU providers to have a comprehensive understanding of all the diseases and therapies used in this population and for hematologists-oncologists to fully understand advances in ICU care. This is particularly true given the rapidly changing landscape of pediatric hematologic and oncologic care. Recent years have seen the development and expanded use of molecularly targeted medications, chimeric antigen receptor T-cell (CAR-T) therapy, and gene therapy. Each of these and other emerging therapies carry unique risks. Because of the complexity of diagnoses and treatment, a collaborative relationship between the PICU and the disease-specific teams is important to the care of these patients. Different models for cooperative care are addressed later in this text.
Multiple research consortia including the Pediatric Acute Lung Injury and Sepsis Investigators and Pediatric Blood and Marrow Transplant Consortium have focused on the care of immunocompromised hematology and oncology patients. The work of these and other groups is important as the community works to improve the survival of these vulnerable patients.
References
Faraci M, Bagnasco F, Giardino S, Conte M, Micalizzi C, Castagnola E, et al. Intensive care unit admission in children with malignant or nonmalignant disease: incidence, outcome, and prognostic factors: a single-center experience. J Pediatr Hematol Oncol. 2014;36(7):e403–9. https://doi.org/10.1097/MPH.0000000000000048.
Zinter MS, DuBois SG, Spicer A, Matthay K, Sapru A. Pediatric cancer type predicts infection rate, need for critical care intervention, and mortality in the pediatric intensive care unit. Intensive Care Med. 2014;40(10):1536–44. https://doi.org/10.1007/s00134-014-3389-2.
van Gestel JP, Bollen CW, van der Tweel I, Boelens JJ, van Vught AJ. Intensive care unit mortality trends in children after hematopoietic stem cell transplantation: a meta-regression analysis. Crit Care Med. 2008;36(10):2898–904. https://doi.org/10.1097/CCM.0b013e318186a34a.
Tamburro RF, Barfield RC, Shaffer ML, Rajasekaran S, Woodard P, Morrison RR, et al. Changes in outcomes (1996–2004) for pediatric oncology and hematopoietic stem cell transplant patients requiring invasive mechanical ventilation. Pediatr Crit Care Med. 2008;9(3):270–7. https://doi.org/10.1097/PCC.0b013e31816c7260.
Hayes C, Lush RJ, Cornish JM, Foot AM, Henderson J, Jenkins I, et al. The outcome of children requiring admission to an intensive care unit following bone marrow transplantation. Br J Haematol. 1998;102(3):666–70.
Hallahan AR, Shaw PJ, Rowell G, O’Connell A, Schell D, Gillis J. Improved outcomes of children with malignancy admitted to a pediatric intensive care unit. Crit Care Med. 2000;28(11):3718–21.
Diaz de Heredia C, Moreno A, Olive T, Iglesias J, Ortega JJ. Role of the intensive care unit in children undergoing bone marrow transplantation with life-threatening complications. Bone Marrow Transplant. 1999;24(2):163–8. https://doi.org/10.1038/sj.bmt.1701874.
Lamas A, Otheo E, Ros P, Vazquez JL, Maldonado MS, Munoz A, et al. Prognosis of child recipients of hematopoietic stem cell transplantation requiring intensive care. Intensive Care Med. 2003;29(1):91–6. https://doi.org/10.1007/s00134-002-1549-2.
Kache S, Weiss IK, Moore TB. Changing outcomes for children requiring intensive care following hematopoietic stem cell transplantation. Pediatr Transplant. 2006;10(3):299–303. https://doi.org/10.1111/j.1399-3046.2005.00453.x.
Cheuk DK, Ha SY, Lee SL, Chan GC, Tsoi NS, Lau YL. Prognostic factors in children requiring admission to an intensive care unit after hematopoietic stem cell transplant. Hematol Oncol. 2004;22(1):1–9. https://doi.org/10.1002/hon.724.
Diaz MA, Vicent MG, Prudencio M, Rodriguez F, Marin C, Serrano A, et al. Predicting factors for admission to an intensive care unit and clinical outcome in pediatric patients receiving hematopoietic stem cell transplantation. Haematologica. 2002;87(3):292–8.
Jacobe SJ, Hassan A, Veys P, Mok Q. Outcome of children requiring admission to an intensive care unit after bone marrow transplantation. Crit Care Med. 2003;31(5):1299–305. https://doi.org/10.1097/01.CCM.0000060011.88230.C8.
Heying R, Schneider DT, Korholz D, Stannigel H, Lemburg P, Gobel U. Efficacy and outcome of intensive care in pediatric oncologic patients. Crit Care Med. 2001;29(12):2276–80.
Tomaske M, Bosk A, Eyrich M, Bader P, Niethammer D. Risks of mortality in children admitted to the paediatric intensive care unit after haematopoietic stem cell transplantation. Br J Haematol. 2003;121(6):886–91.
Gonzalez-Vicent M, Marin C, Madero L, Sevilla J, Diaz MA. Risk score for pediatric intensive care unit admission in children undergoing hematopoietic stem cell transplantation and analysis of predictive factors for survival. J Pediatr Hematol Oncol. 2005;27(10):526–31.
Hassan NE, Mageed AS, Sanfilippo DJ, Reischman D, Duffner UA, Rajasekaran S. Risk factors associated with pediatric intensive care unit admission and mortality after pediatric stem cell transplant: possible role of renal involvement. World J Pediatr. 2013;9(2):140–5. https://doi.org/10.1007/s12519-012-0391-z.
Aspesberro F, Guthrie KA, Woolfrey AE, Brogan TV, Roberts JS. Outcome of pediatric hematopoietic stem cell transplant recipients requiring mechanical ventilation. J Intensive Care Med. 2014;29(1):31–7. https://doi.org/10.1177/0885066612457343.
Bartram JL, Thein SL, Gardner K, Egberongbe Y, D’Silva P, Height SE, et al. Outcome of children with sickle cell disease admitted to intensive care – a single institution experience. Br J Haematol. 2010;150(5):614–7. https://doi.org/10.1111/j.1365-2141.2010.08272.x.
Chima RS, Daniels RC, Kim MO, Li D, Wheeler DS, Davies SM, et al. Improved outcomes for stem cell transplant recipients requiring pediatric intensive care. Pediatric Crit Care Med. 2012;13(6):e336–42. https://doi.org/10.1097/PCC.0b013e318253c945.
Duncan CN, Lehmann LE, Cheifetz IM, Greathouse K, Haight AE, Hall MW, et al. Clinical outcomes of children receiving intensive cardiopulmonary support during hematopoietic stem cell transplant. Pediatr Crit Care Med. 2013;14(3):261–7. https://doi.org/10.1097/PCC.0b013e3182720601.
Zinter MS, Dvorak CC, Spicer A, Cowan MJ, Sapru A. New insights into multicenter PICU mortality among pediatric hematopoietic stem cell transplant patients. Crit Care Med. 2015;43(9):1986–94. https://doi.org/10.1097/CCM.0000000000001085.
Rowan CM, Gertz SJ, McArthur J, Fitzgerald JC, Nitu ME, Loomis A, et al. Invasive mechanical ventilation and mortality in pediatric hematopoietic stem cell transplantation: a multicenter study. Pediatr Crit Care Med. 2016;17(4):294–302. https://doi.org/10.1097/PCC.0000000000000673.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing
About this chapter
Cite this chapter
Duncan, C.N. (2019). The Changing Landscape of the Critical Care of Pediatric Immunocompromised Hematology and Oncology Patients. In: Duncan, C., Talano, JA., McArthur, J. (eds) Critical Care of the Pediatric Immunocompromised Hematology/Oncology Patient. Springer, Cham. https://doi.org/10.1007/978-3-030-01322-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-01322-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-01321-9
Online ISBN: 978-3-030-01322-6
eBook Packages: MedicineMedicine (R0)