Abstract
The shape of any cell is defined and delimited by the shape of the outermost membrane of lipid. Whether a cell’s membrane is locally flat, protrusive, or invaginated at a given instant is often the resultant of forces generated by molecules within the cell as well as those attributable to external factors. For mammalian cells, major changes in cell shape are evident in processes that include cell spreading, migration, and cell division as well as differentiation and death. Such processes are illustrated here for blood cells, starting with stem cells in bone marrow plus the many different types of circulating cells, particularly RBCs whose membranes have been more deeply studied for decades compared to other mammalian cell types. A handful of the key proteins that apply or resist forces at the membrane are described here while focusing on the cortical protein meshworks that underlie membranes and contribute to properties and processes. Engulfment of particles and cells is one particular focus, with broad relevance to disease and therapy. Equally interesting is the frequently noted observation that changes in cell shape and orientation are also evident in shape and orientation changes of the cell's nucleus—which is again delimited by a membrane. A final section focuses on the physics of a sub-membranous lamina in the nucleus, which interfaces with the genome and provides insight into mechanosensing and cell fates.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
A cell’s shape is defined by how a cell’s plasma membrane is spatially arranged in its three-dimensional microenvironment. Sculpting a cell at any instant in time are the forces within a cell—including forces actively generated through energy consumption—as well as forces from outside a cell such as extracellular pressure and fluid shear. The resistance to shape change under force is variously referred to as stiffness, elasticity, rigidity, or plasticity; some deformations are of course fully reversible (i.e. elastic) while others are irrevesible (eg. plastic). Relatively stable cell shapes are achievable for just a few mammalian cells when isolated, and the red blood cell (RBC) with its symmetrically-dimpled “discocyte” shape is the best understood. Dynamic changes in the shapes of far more active cells are critical to cell functions that range from adhesion and migration to division, differentiation, and death. Understanding the mechanisms that underlie such essential cell processes requires clarifying the forces that locally shear, dilate, and bend membranes. This chapter seeks to introduce in broad terms a few of the basic cell biological processes that involve striking changes in cell shape, and in doing so we describe a small handful of the responsible proteins.
An overall view of the diversity of membrane shapes and their changes within a mammalian system is perhaps best achieved by focusing on the various types of human blood cells and their ongoing development in bone marrow (Fig. 1). Human bone marrow collectively generates red blood cells, platelets, and white blood cells, each at a rate of roughly 100,000 per second. Production is matched in steady state by cell death and removal from circulation, which occurs on average after ∼100 days for RBCs (red blood cells) in humans or just a few days to a week for platelets and some of the more abundant types of white blood cells. The longer life of the RBC thus explains why this is far more abundant than any other cell type in blood. The distinct multistep process by which an RBC is made and eventually destroyed provides many useful insights into biomembrane properties and forces that underlie remodeling of membrane shapes. Any terminally differentiated cell such as an RBC is derived from a less specialized cell referred to as a stem cell. Therefore, we begin by describing processes of the relevant bone marrow stem cell, focusing on the membrane and the stresses that control its shape—while. We also attempt to convey the importance of the cells and clinical motivations that every day save lives around the world.
1 Division: Fission Forces at the Membrane for Cell Differentiation
The long-term health of any tissue invariably requires that death or turnover of mature cells be balanced not only by differentiation from the relevant stem cell but also by self-renewal of the stem cell. These processes seem optimized in specialized tissue microenvironments called niches. Hematopoietic stem cells and progenitors (HSC/P) reside in bone marrow niches that are formed from extracellular matrix proteins and other cells. The latter include mesenchymal stem cells (MSCs) and MSC-derived lineages, namely, bone cells and fat cells [1]. Decades of clinical success in transplantation of HSC/Ps into patients [2] have motivated the exploration of mechanisms that underlie the balance between stem cell self-renewal, differentiation, and trafficking of mature cells from the marrow and into the blood circulation. Soluble factors and cell–cell contacts regulate these biological processes, but it is only recently appreciated that stem cells can generate and resist physical forces, while matrix stiffness and external stresses such as shear flow impact stem cell adhesion and intracellular signaling [3]. Structural proteins just below the cell membrane and even the nuclear membrane are major determinants.
Asymmetric division is one evolutionarily conserved mechanism that explains how stem cells both self-renew and differentiate [4]. A parent stem cell divides asymmetrically to give rise to one daughter cell that maintains stem cell characteristics and another that is committed to differentiation. Asymmetric segregation of proteins during division has been well documented in invertebrates [5], and in HSC/Ps these include integral membrane proteins such as CD34 (a “surface marker” that might not be crucial to function and simply helps identify these cells) as well as proteins that contribute to asymmetric division [3]. While extrinsic adhesive cues from neighboring cells have been implicated in asymmetric division of some white blood cells [6], the requisite polarization of a cell is inextricably linked to its cytoskeleton. In blood cells, the actin-myosin cytoskeleton is just below the plasma membrane as a cortex (Fig. 1), with its forces and/or crosslinking helping to break the symmetry of the doublet of daughter cells to induce a polarized distribution of molecules. Microtubules maintain the stability of the polarization [7], but the stiffness of microtubules could also feedback and help direct the contractile activity of the actin-myosin cytoskeleton [8].
Biophysical determinants of blood formation. Adhesion and contractile forces generated by MII are important in sensing matrix stiffness, which is heterogeneous in the BM microenvironment. During the cell division process, stem cells near the osteoblasts undergo asymmetric division to segregate MIIB into one daughter cell. Without MIIB, cells divide symmetrically. The other daughter cell becomes differentiated into three different lineages. Because MKs upregulate both lamin isoforms by endomitosis, they are too large to traffic through endothelial barriers. Instead, they undergo fragmentation into platelets. During erythroid differentiation, the nucleus shrinks in chromatin condensation. Condensed nuclei are too stiff to migrate through the endothelial barrier and are phagocytosed by macrophages, leading to enucleated RBCs. RBC red blood cell, WBC white blood cell, HSC/P hematopoietic stem cell/progenitor
Myosin-II (MII) proteins are ATP-consuming motor proteins that assemble into bipolar filaments and apply both contractile forces to and active crosslinking of actin filaments which, in turn, link to a diverse set of membrane proteins. In comparison to the non-muscle MII in blood cell types and other non-muscle cells, cardiac MII in heart muscle striates the cytoplasm of heart cells and contracts rhythmically to pump blood out of the heart. Skeletal muscle MII likewise striates the cytoplasm of elongated muscle cells, and its neuron-triggered, voluntary contractions drives body movements. Non-muscle MII is more closely related to the most evolutionary ancient form of MII that is found even in some single-cell organisms. Among its many cellular functions in non-muscle cells, MII confers the cell-intrinsic cortical tension that both stabilizes the plasma membrane [9, 10] and drives cell division (cytokinesis). The latter is achieved through a coordination of forces in the constriction ring and at the opposite poles of the daughter cells [11]. Cortical tension is also modulated at least locally by adhesion to stiff extracellular matrix [12, 13], which provides a mechanism by which MII regulates the ability of cells to sense physical properties of the matrix such as matrix elasticity, E. A simple intuition into mechanosensing is obtained by considering that actin polymerization drives cell spreading at a near constant rate, v polymer = A, whereas MII pulls back on the actin network at a rate v retract = B / (K + E) which is a hyperbolic decrease (with constants B, C) with resistance set by the extracellular load E (as with muscle, low speed at high loads). The extent of cell spreading relates to a steady state v polymer − v retract = A − B / (K + E) that yields minimal cell spreading for E ≪ K and maximal spreading for E ≫ K as observed for spreading cells [12]. A typical value of K ∼ 5 kPa [12], in units of stress or pressure, should be multiplied by a typical cell-generated strain of ∼5% [12] and then related through the well-known law of Laplace to an effective tension ∼ 0.1 mN/m in a typical protrusion curvature radius of ∼1 μm. A cortical tension of ∼ 0.1 mN/m has indeed been measured for HSC/Ps, and this tension decreases dramatically with MII inhibition [10].
For at least some stem cells, matrix mechanosensing can regulate cell differentiation [12, 13]; inhibition of MII also limits the proliferation of HSC/P when these cells adhere to a highly flexible or soft matrix [13]. However, in order for daughter cells to migrate away from each other, actin seems necessary while MII is not needed; such migration can help stretch and break a lipid tether or membrane nano-tubule that is often the final vestige of the cytokinetic furrow [8]. Other membrane factors in stem cells are also likely to contribute to cleavage and repair of the nano-tubule.
Cell force generators have evolved to be fine-tuned by slightly more specialized molecules, which has come to reveal how important the proper forces and dynamics need to be for cell function. In particular, humans express three myosin-II genes (MIIA, MIIB, and MIC) with different properties. MIIB appears especially key to asymmetric division of HSC/Ps [3]. MIIB motors make notably stable assemblies with actin filaments and can be seen to polarize within cells due to external stiffness or perhaps stresses such as fluid shear [3]. The latter forces could be relevant to triggering blood formation in early embryos [14]. Soft microenvironments do not sustain or transmit high stress, which limits myosin-IIB forces and polarization, and since bone marrow is very soft compared to rigid bone, polarization is more likely on the latter. External cues and spontaneous intracellular fluctuations in the cell cortex [15] could cause polarization during cell division of adult HSC/Ps, but it is very clear that MIIB segregates asymmetrically to the cortex of the one daughter cell that maintains stemness (i.e., CD34 high cells). The other nucleated daughter cell with less MIIB is thereby differentiated, and MIIB is similarly reduced per division in differentiation—at least in differentiation toward white blood cells and cells called megakaryocytes that make platelets. Asymmetric segregation of MIIB likely establishes an asymmetric cortical tension that drives differentiation, although physical differences still need to be measured.
As MIIB is downregulated in differentiating cells, MIIA is activated by dephosphorylation. This change favors MIIA assembly into filaments that again localize to the cortex. However, soft matrix favors MIIA phosphorylation. Soft microenvironments thus maintain early HSC/Ps by suppressing a switch of myosin-II’s from high to low levels of MIIB and from deactivated to activated MIIA. Stiff microenvironments that resist stress have the opposite effect and initiate asymmetric division and differentiation.
RBCs have much higher levels of MIIB than platelets and white blood cells. Although myosin-II’s in mature RBCs are probably vestigial in not contributing greatly to discocyte-shaped RBCs, they do contribute to the loss of nuclei during formation of RBCs. In particular, MIIB helps to polarize the nucleated RBC progenitor (called an erythroblast) and to expel the cell’s nucleus in a final step of asymmetric division [16]. The expelled nucleus is rigid [3] compared to the nascent RBC, which is called a reticulocyte. As in cytokinesis, the nucleus remains tethered by a membrane nano-tubule to the reticulocyte [17]. Eventually, the tether is severed as the nucleus is engulfed by white blood cells called macrophages that reside in bone marrow as well as all other tissues [18]. Engulfment might be accompanied by macrophage-facilitated expulsion of the reticulocyte from the marrow into the blood vessels flowing through the marrow. The latter speculation is based on an absence of any data showing that reticulocytes can move or crawl. Megakaryocytes serve as a useful comparison since they actively extend pseudopods into the bloodstream via membrane-protrusive polymerization of actin and microtubules (as myosin is phospho-inhibited). The pseudopods then fragment under shear to make pre/pro-platelets [19] that are about half the size of a mature RBC. Once in the circulation, these giant pre/pro-platelets divide to make the small and abundant platelets, and division uses MIIA that is normally activated by fluid shear unless mutations in MIIA keep it aggregated [20]. The latter mutations give rise to MYH9-related diseases (i.e., MIIA related diseases) that lead to “macro-thrombo-cytopenia,” which refers to giant platelets that are few in number. RBCs appear relatively normal in number and shape in these patients even though a recent study of mature RBCs [21] concluded that pharmacological inhibition of myosin-II could generate a very small fraction of `elliptocytic' RBCs. Platelet maturation thus finishes within the circulation to a much greater extent than with RBCs. What remains in the marrow from the megakaryocytes after production of many pre/pro-platelets is just a giant nucleus unable to cross the small micro-pores into the sinusoids. This nucleus that is stuck in the marrow is engulfed by macrophages. The same occurs with RBC nuclei after generation of a reticulocyte.
As with platelets, RBC maturation also finishes within the circulation: the reticulocyte sheds membrane and volume (15% and 10%, respectively [22]) within hours to become the discocyte-shaped RBC. In this final remodeling, more lipid is observed to be lost than cortical cytoskeleton, and this cytoskeleton is particularly enriched in the actin-crosslinking protein spectrin which forms a two-dimensional spectrin-actin network that attaches below the lipid bilayer. The relative loss of lipid thus increases the overall stoichiometry of 2D cytoskeleton to 2D lipid membrane. The spectrin network has been observed to dilate strongly at the tip of an RBC projection that is aspirated into a micropipette (Fig. 2) [23, 24], but in the absence of such external forces the state of stress in the “at rest” spectrin-actin network remains a matter of uncertainty. The cortical network could be under constant tension and tending to pull away from the bilayer [25], or the network could be stress free or else compressed. The cited loss of lipid relative to cytoskeleton is consistent with the network being compressed by the more limited overlying lipid bilayer, and in this case the lipid bilayer is under an equal and opposite tension which smooths and suppresses fluctuations of the lipid bilayer. Such a balance of membrane forces does not set global cell shape as the forces are too weak. Rather, the flaccid discocyte shape results from volume regulation and the relatively fixed cell area set by the near incompressibility of the lipid bilayer.
(a) Simulation of a near full-scale RBC under aspiration. The surface of the cell is triangulated with 6110 vertex nodes that represent the spectrin-actin junction complexes of the erythrocyte cytoskeleton. Mouse RBCs have about two-thirds the surface area of human RBCs and are estimated to have about 18,000 spectrin-actin nodes, so that the simulation is about one-third scale. The volume of the cell is 0.6 times the fully inflated volume, and the snapshot is from simulation of a stress-free meshwork. (b) AFM indentation in a continuum calculation of an axisymmetric shape with isotropic tension and elastic dilation of the membrane, but no bending resistance. (c) With increasing velocity, v, of the AFM tip, the lytic force, f c, needed to penetrate the tensed RBC membrane increases exponentially as does the indentation depth until lysis. (d) On mouse RBC membranes, the membrane protein Band 3 appears largely connected to the cytoskeleton, whereas another membrane protein Cd47 appears completely mobile, squeezing out to the tip of the aspirated membrane. Lipid is uniformly distributed with equal entrance and cap intensities
The RBC cytoplasm lacks all other organelles and is predominantly a highly concentrated fluid of hemoglobin protein (with chelated iron that makes RBCs red) plus many other macromolecules and counterions that cannot permeate the lipid bilayer. Water readily permeates the few-nanometer-thick bilayer, despite the oiliness of the core of the lipid bilayer, so that the entrapped solutes attract and retain hydrating water in strict relation to the osmotic pressure outside the cell. Thus, to first approximation, RBC volume is not regulated by membrane physical properties but could affect membrane state—such as rupture and lysis in hypo-osmotic media. Importantly, the shear resilience of an increasingly compressed spectrin-actin network would tend to resist further rapid fragmentation of the RBC, so that a cell circulates for another ∼100 days after quickly shedding 15% of its initial plasma membrane and losing a smaller fraction of its cytoplasmic solutes and membrane skeleton. Old RBCs have ∼3–6% less hemoglobin mass relative to the bulk population [26], which indicates that the membranes of these cells rarely rupture under shear or else they rapidly reseal. Regardless, old RBCs are removed from circulation as they are engulfed or “phagocytosed” by macrophages located near slit-like blood vessels within the spleen.
Some additional physical aspects of the prototypical RBC membrane should be highlighted before proceeding to the next section on phagocytosis, with a focus on membrane-mediated interactions and cytoskeleton-driven adhesion. First, the simplicity of the RBC membrane has lent itself to a rapidly increasing number of molecular and multiscale simulations that increasingly capture the fine structure and 2D elastic properties of the spectrin network as well as the resistance of the bilayer to both dilation and bending. One such free energy expression used in whole cell simulation (Fig. 2) has employed a “Hamiltonian” for a triangulated meshwork of spectrin chains that have both steric exclusion (as ∼c / Area for each triangle, with c being a constant) and worm-like chain stretching energy of the spectrin chains (as fraction x of the maximum contour length):
where k quantifies spectrin’s stiffness when stretched. A change in position of a node in a triangle due to a thermal fluctuation or external force such as aspiration into a micropipette or fluid shear costs energy, which should—as a goal—reach a global minimum for the discocyte shape under stress [27]. As a function of pressure, a linear increase in length of aspirated membrane for a flaccid RBC reveals the apparent shear elastic modulus of the spectrin-actin network, which is in the range of 0.006–0.009 mN/m. This is tenfold softer than the MII-dependent cortical tension of ∼0.1 mN/m typically measured for cells including HSC/Ps [10].
Membrane proteins bind to the spectrin network, so that dilation of the deformed spectrin meshwork that is evident in simulation is also seen in experiments to cause a similar density gradient of attached membrane proteins (e.g., Band 3). The steric bulk of such proteins excludes mobile membrane proteins (e.g., mouse-CD47), whereas lipid remains uniform [23]. In this way at least, the local membrane density of both mobile and immobile membrane proteins is mechanosensitive. Futhermore, unfolding of the spectrin protein when stretched has been demonstrated in intact RBC membranes [28], which provides a means for the ubiquitous spectrin network to contribute to membrane mechanosensitivity of many cell types.
Beyond the small elastic dilation limits of the bilayer, poration of RBCs with loss of hemoglobin can occur physically as well as upon addition of various chemicals that insert and disrupt the lipid membrane. Even a simple tool such as the sharpened tip of an atomic force microscope cantilever can indent adhesively attached RBCs to stress the membrane and rupture it [29, 30]. Differential geometry is useful for calculating the continuous, equilibrium shape of an indented cell up to rupture. Regardless, the rate dependence of such a process is an expected signature of stochastics in failure[31].
2 Phagocytosis and Adhesion: Microbes, Colloids, and Key Molecular Pathways for “Self” Cells
Phagocytosis was already mentioned above as important to both the removal of nuclei from the progenitor cells that make RBCs or platelets and also the clearance from circulation of old RBCs (platelets, and other cells also). Biophysical factors and molecular factors both determine whether a macrophage engulfs an entire cell or just a nucleus. A “macro phage” is a large cell that devours, with principal “targets” for engulfment being microbes that constantly cross beach tissue barriers. The occasional serious pathogen might include malaria parasites which are notable for having a blood stage in which this microbe enters an RBC to digest hemoglobin and replicate. Additional targets of phagocytosis are now well appreciated to include all types of injected colloids, including nanoparticles, and also dying cells (or nuclei) in the same tissue, but there are also exciting efforts to make macrophages eat cancer cells. Multiple features of a target influence eating by a macrophage, including surface molecules that promote adhesion and eating, but also at least one molecule that inhibits eating as elaborated below. In addition, physical properties such as target shape and target rigidity impact phagocytosis efficiency of the target.
Phagocytosis is undoubtedly an ancient evolutionary development that provided sustenance to some of the first amoeboid cells. With soft plasma membranes rather than the rigid cell walls of bacteria, ancient amoeba (like modern amoeba typified by Dictyostelium) could wrap around their target to engulf it and digest it within a phagosome [32]. Fast forward eons to organisms like humans that gain nutrition through a highly differentiated and multicellular digestive tract, and we find that phagocytosis within humans is a highly efficient process used primarily by specialized white blood cells of the mononuclear phagocyte system. Microbes (in and on us) remain major targets as they not only outnumber and outproliferate our own cells but also invade through any and all compromised tissue barriers [33]. Principal cell types of the mononuclear phagocyte system are macrophages which reside in every tissue and monocytes that circulate out of the bone marrow to enter a tissue and differentiate to macrophages [34]. These cells as well as the highly phagocytic neutrophils must—for the health of the organism—choose to devour “foreign” targets rather than devour human “self” cells or extracellular matrix that generally surrounds the phagocytic cell. Phagocytosis thus evolved for engulfment and destruction of “foreign” strictly for protection of the organism.
A variety of molecular cues and sensor assemblies must be used by our phagocytic cells to distinguish and destroy “foreign” amidst “self.” Many decades of work have elaborated a list of biochemical entities, soluble and/or surface bound, which activate macrophages (we will hereafter ignore the distinction from monocytes) to initiate engulfment of a target. One of the most important classes of molecules that is described below in context are immunoglobulin-G (IgG) antibodies which diffuse and bind to a target surface so that when a macrophage contacts the target, the constant fragment (Fc) of the IgG binds the macrophage membrane receptor FcγR and (for some classes of FcγR) activates the macrophage to eat the opsonized target (Fig. 3). Importantly, while it is commonly presumed that our “self” cells simply lack such surface “opsonization” by activating molecules such as IgG, it is now clear that “self” recognition is not simply the absence of a “foreign” signal. Instead, a dominating and passivating interaction occurs between a “Marker of Self” CD47 membrane protein on a candidate target and the macrophage membrane receptor CD172a (also known as SIRPA, signal-regulatory protein alpha). Controlling the balance of “eat me” cues (e.g., IgG-FcγR interaction) and “don’t eat me” signals (CD47-SIRPA) is currently an active area of translation to the clinic for anticancer therapy [35] and has begun to be exploited on nanoparticles in preclinical models [36]. However, the decision-making process within the macrophage remains a topic in need of deeper insight.
(a) On both rigid and native flexible RBCs, SIRPA binds CD47. Downstream of FcgR binding of IgG, kinases phosphorylate multiple cytoskeletal proteins, including myosin-II, which drive assembly of the phagocytic cup and promote uptake. CD47-SIRPA signaling leads to activation of SHP-1 phosphatase that can deactivate myosin-II. Because substrate rigidity initiates assembly and polarization of myosin-II in many cell types, phagocytic target rigidity is expected to counterbalance CD47-mediated inhibition of the motor. Our working hypothesis is that with flexible self-cells (left), CD47-initiated inhibition can overcome myosin-II activation, whereas with rigid self-cells (right), the myosin-II driven cytoskeleton is not diminished by CD47-SIRPA self signals. (b) Phagocytic uptake of opsonized RBCs is faster with CD47 inhibition but fastest for rigid RBCs. Human-derived THP-1 macrophages were incubated with human RBCs that were opsonized with anti-hRBC antiserum and also blocked with anti-CD47, native RBCs with active CD471, or rigidified as GA discocytes. Time-lapse imaging in DIC and phase contrast begins with initial adhesion between macrophage and RBC targets and ends on complete engulfment (scale bar, 8 μm). At the right of each time-lapse series, silhouettes of the target RBC clarify the changes in RBC morphology over the course of engulfment and RBC position relative to the macrophage boundaries, as indicated by the sketched lines
An explosion of efforts to make a broad range of injectable and implantable particles or devices for therapy and diagnostics has also revealed phagocytes to be a major impediment to delivery. Make a nanoparticle, inject it into the bloodstream of a mouse or man, and one invariably finds that most of the particles have been eaten by macrophages of the spleen and of the liver (the latter are called Kupffer cells). Based on several decades of work on a diversity of nanoparticles, such clearance can be delayed but never eliminated [37,38,39,40]. Studies of macrophages in conventional static culture where nanoparticle diffusion and buoyancy can dominate have questioned whether evident uptake of small nanoparticles occurs by phagocytosis [36] or not [41]. In vivo, however, blood-borne nanoparticles flow into contact with macrophages that line the spleen and liver vasculature, where these cells constantly and actively filter out dying and energy-depleted blood cells (e.g., after blood storage) to maintain blood homeostasis. A leaky vasculature at a site of injury or disease such as an infarct in the heart or a tumor can allow sufficiently small particles to permeate tissue and perhaps be retained [42]. However, when macrophages in damaged and disease sites are examined, they prove to be major consumers of permeating nanoparticles [43]. Macrophages are indeed resident if distinct in every tissue in the body [34], and at damaged and disease sites they will at least be involved in clearing dead and dying tissue. A large implant (or even a splinter) also damages tissue and causes a “foreign body response” that starts with serum protein deposition and soon recruits phagocytes to the site, but phagocytosis is frustrated for large implants and somehow triggers macrophage–macrophage fusion to a “foreign body giant cell” that encases the implant [44]. Physical size is thus a factor in macrophage function, but the focus below is on targets including cells that are cell-sized or smaller, with attention to additional properties such as target rigidity and shape as well as surface signaling (Fig. 3). Despite the decades of work on synthetics, there is nothing more biocompatible than a properly matched blood transfusion, but the reasons why continue to be elaborated.
“Eat me” signals can be weak or strong but are unavoidable. IgGs are well known for high-affinity interactions (∼nano-Molar) between epitopes and their antibody fragment (Fab) domains, but they are also large glycoproteins of ∼150,000 Daltons with considerable surface area to mediate nonspecific interactions. They are among the most abundant proteins in normal serum at ∼100 μM. Antibodies and other serum proteins physisorb in vivo to red blood cells (RBCs) [45, 46], to viruses [47], and even to particles coated with PEG (polyethylene glycol) which otherwise delays adsorption and in vivo clearance from minutes to many hours [48, 49]. Autologous IgG binding to autologous RBCs in humans and dogs in vivo increases up to sevenfold toward the end of the cell’s ∼100-day life span. Aged human RBCs lack additional “eat me” signals such as exposure of the negatively charged lipid phosphatidylserine [46, 50]. IgG opsonization is increased in blood diseases including sickle cell anemia and malaria among other conditions, where phagocytosis and cell clearance are also increased (tabulated recently in [51]). When IgG-opsonized RBCs and particles are phagocytosed in vitro, uptake is hyperbolic and saturable versus IgG, which is consistent with specific activation of the FcγR phagocytosis pathway. Because macrophages and phagocytic dendritic cells can also function as antigen-presenting cells to the white blood cells of the “acquired immune system,” it seems sensible that engulfment can promote immunogenicity in vivo even to foreign polymers [52].
Binding of the IgG’s Fc domain to the macrophage FcγR receptor triggers phagocytic cup formation in a coordinated process of adhesion, pseudopod extension, and eventual internalization with phagosome closure. The surface interactions initiate Src family kinase phosphorylation of immunoreceptor tyrosine-based activating motifs (ITAMs) that then propagate a phosphorylation cascade [53]. Phosphopaxillin and F-actin [54, 55] accumulate in minutes or less together with other structural components at this dynamic phagocytic synapse. The process is highly analogous to adhesion formation upon integrin binding to rigid extracellular matrices, wherein the nascent adhesion matures to a focal adhesion only when the F-actin cytoskeleton is mechanically organized through pulling by non-muscle myosin-II (MII) phospho-protein [56, 57]. At the phagocytic synapse, MIIA accumulates to greatly help with pulling targets into a macrophage, including IgG-opsonized targets as small as 100 nm nanoparticles (perhaps smaller) and at least as large as opsonized RBCs [36, 58, 59]. Engulfment of such targets is greatly decreased by inhibiting MIIA motor activity with the drug blebbistatin which also blocks MII localization without affecting F-actin or phosphopaxillin. Uptake increases linearly with MII activity based on its knockdown and overexpression [58]. At least above a low baseline level of uptake in vitro, MII makes phaogocytosis efficient for our macrophages if not for ancient amoeba like Dictyostelium [32].
As an IgG-opsonized target contacts a macrophage and adheres intimately via FcγR, the parallel presence on the target of an appropriate form of CD47 can lead to binding to the macrophage phagocytosis inhibitory receptor SIRPA, which accumulates in the synapse [59]. The latter complex somehow phosphorylates SIRPA’s cytoplasmic immunoreceptor tyrosine-based activating motifs (ITIMs), which activates the immunomodulatory phosphatase SHP-1 (Src homology region 2 domain-containing phosphatase-1) [60] to regulate multiple proteins by dephosphorylation [61], including deactivation of MIIA [36, 58]. SIRPA-null macrophages engulf IgG-opsonized mouse RBCs more readily than wild-type macrophages [61] and show no major differences in phospho-FcγR nor the downstream effectors phospho-Syk or phosho-Cbl, which suggests that regulation of proteins even further downstream is key. Inhibition of downstream actomyosin contractility at the phagocytic synapse [36, 58] could indeed explain various observations that CD47 partially blocks engulfment of not only mouse RBCs—which started the expanding “Marker of Self” field [62] but maybe also cancer cells [63,64,65] and opsonized polystyrene beads (100 nm to 6 μm) that display CD47’s binding domain in parallel with IgG [36, 58]. The effectiveness of CD47 with small nanobeads is surprising because pulling in large particles with MII forces seems more understandable than pulling in small particles. Nonetheless, CD47's mechanism of inhibition is ultimately: just don’t pull it in!
CD47 and SIRPA arose in evolution at the same time in amniotes and are not found even in amphibians [66]. CD47 and SIRPA are thus more recent inventions than the ancient actomyosin cytoskeleton found even in amoeba such as Dictyostelium. CD47 is found on all cells in man and mouse while the expression of SIRPA is more restricted. CD47 knockout mice have one-quarter to one-half the life spans of normal mice (at least for some strains) and also show evidence of anti-RBC antibodies as well as anemia [67]. This is consistent with the idea that a modest level of opsonization exists in vivo, which tilts the balance toward engulfment and possibly even an acquired immune response with antibody generation.
Saturable binding of SIRPA, CD47, and/or CD47-derived “Self” peptide to beads as well as to living cells shows that an intermediate strength interaction (sub-micro-Molar) has evolved to be largely species specific [36, 58, 68]. The molecules also differ between strains of mice. NOD-SCID strains of mice uniquely express a SIRPA variant that binds human CD47 with similar affinity as human SIRPA, which partially explains why these are the best mouse choice for engraftment of human stem cells [69]. Species specificity in vivo is a critically important issue because human-specific blocking antibodies have been injected intravenously together with opsonizing IgG to impede growth and even shrink tumors of human cancer cell lines in mice. As emphasized by others [70,71,72], injection of any reagent that binds human-CD47 would bind to every cell membrane in the body, even if cancer cells have severalfold more of this ubiquitous protein [73, 74]. On the other hand, CD47 is far from the most abundant protein on cells (∼250 molecules/μm2 on RBCs which is 10–20-fold less than Glycophorin-A), so that blocking CD47 even with IgG is not expected to drive strong phagocytosis unless an additional and far more abundant “eat me” cue is also bound to a candidate target. The half-max density for inhibition by CD47 on beads is independent of particle size and is ∼20 molecules/μm2, which is consistent with the minimum density of CD47 on circulating RBCs from patients with anemia [36, 58]. For senescing neutrophils, CD47 is somehow downregulated from the surface and the needed cue to drive macrophage engulfment seems to be surface-exposed calreticulin (from the endoplasmic reticulum) rather than IgG [75]. Some of the above ideas are currently being put to the test in the clinic [35]. Safety is of course the first question of concern for systemic injection of any entity that limits macrophages from recognizing “self”, and loss of RBCs from circulation is readily expected to be observed when patients are injected with anti-humanCD47 IgG.
Rigid cells and particles drive phagocytosis, but shape and size of a target can also frustrate engulfment. A relatively new principle in cell biology that applies to many cell types is that adhesion-induced activation of myosin-II is maximized by adhesion to a substrate that is rigid (like glass or plastic) rather than flexible like most soft tissues [12]. Bacteria such as E. coli and fungi such as yeast have cell walls as rigid as some plastics [76]. For the RBC precursor erythroblasts that interact with macrophages, the effective cell stiffness relative to mature RBCs has been measured by micropipette aspiration to be 50-fold higher, and senescence is also higher in senescence and in diseases ranging from inherited anemias to malaria (tabulated in [51]). With spherical microparticles made of hydrogels and opsonized by IgG, engulfment is proportional to stiffness, which was also shown to drive focal adhesion protein assembly at the synapse [77]. Cell stiffness changes occur with cancer and with chemotherapy [78, 79]. Soft cancer cells might thus escape anticancer efforts aimed at inhibiting CD47–SIRPA interactions [63, 64]. However, a clear relation of cell or particle stiffness to CD47 signaling and to cells with more complicated shapes had been untested until recently.
With normal human RBCs, controlled stiffening could be achieved within seconds by the addition of a protein crosslinker (divalent and covalent) that does not compromise binding of CD47 to SIRPA [22]. Measurements showed that RBC Stiffness ∼ exp(crosslinker concentration/a). The stiffened RBCs that were highly opsonized by IgG were engulfed faster and in greater number according to “Self” Phagocytosis ∼exp(crosslinker concentration/b). A ratio (a/b) ∼ 0.5 was determined so that we can eliminate crosslinker concentration to arrive at:
which is a power law typical of mechanosensitive pathways dependent on myosin-II [80]. When CD47 is not on the target as is typical in past studies of polymer beads [77], estimates of bead stiffness based on the amount of crosslinker used (per [12]) suggest a stronger exponent of ∼1 in Eq. (2) that is generally consistent with “Self” inhibition of phagocytosis.
Rigid RBCs showed active myosin-II at the synapse [51], which suggests that CD47 cannot signal effectively even though it binds SIRPA. As expected, the MII inhibitor blebbistatin blocked MII accumulation and RBC engulfment. Injection of rigid RBC discocytes into the circulation of a mouse also confirmed equal clearance by splenic macrophages independent of whether CD47 was blocked or not with antibody. Synthetic polymer discs resembling RBCs and that lacked any CD47 or other RBC proteins were also shown to be removed from circulating blood far more rapidly when they were stiff rather than soft [81]. Mechanistically, stiff cells and particles become stuck in narrow splenic slits [82], which could facilitate probing and clearance by splenic macrophages [83].
The results which show rigid RBC discocytes are engulfed independent of CD47 present a paradox for the field in that rigid, spherical beads that display CD47 are reproducibly capable of signaling self and thereby impeding engulfment both in vitro and in vivo [36, 58]. Shape is an additional target factor that also modulates phagocytosis and resolves the apparent paradox. Polystyrene microbeads distorted into diverse shapes are always equally rigid but have been shown to be engulfed more readily as spheres than as non-spheres when IgG opsonized [84]. In many studies of other cell types, the topography of a substrate affects cell attachment and is sometimes referred to as “contact guidance.” For macrophage engulfment, the dependence on target shape seems relevant to the diverse shapes of bacteria and fungi that are invariably rigid as noted above. Flexible PEG-based filaments also persist in the in vivo circulation many days longer than spherical particles of the same type of polymer, with particles always eventually cleared by spleen and liver macrophages [38].
With normal human RBCs, the rapid and controlled stiffening approach [51] was used to make rounded, cup-shaped RBC “stomatocytes” that signal “self” much better than rigid RBC discocytes. The problem with a discocyte is that its rigid concavities cannot contact and signal “self” to the macrophage which builds up a high cortical tension when activated by IgG via Fc receptor. In the same studies, native and flexible human-RBC discocytes with the requisite IgG opsonization were seen in video microscopy to be greatly distended by the human macrophage, with myosin-II turned off by CD47 signaling but actin polymerization driving protrusions as if pushing the cell away in recognition of “self.” Thus, since rigid but rounded cells do signal “self”—even if not as efficiently as flexible RBC—one can ultimately understand the success in delaying clearance of CD47-nanobeads that then enable better tumor imaging and drug delivery. However, it seems that a greater advantage might be achieved with flexible beads that avoid the intrinsic activation of myosin-II.
There are some important implications of phagocytic interactions for the production of RBCs within bone marrow. RBC stiffness is one among many factors including shape that changes in erythropoiesis. A plausible mechanism is that the macrophage senses both a rigid nucleus and a soft nascent reticulocyte, which is a cue for the macrophage to help pull the erythroblast apart provided that CD47 on the reticulocyte effectively signals “self.” Target size (e.g., small nucleus versus large retic) does not affect uptake provided molecular densities are properly calculated [36], but additional polarized “eat me” factors might signal the macrophage to pull on a nucleus for its rapid engulfment. With mouse erythroblast nuclei, phosphatidylserine (PS) flips within minutes to the outer leaflet to promote engulfment, although PS flipped only “when cultures were subjected to weak physical stress” [85]. CD47 might be present at low levels on nuclei isolated from erythroblast cultures [86], and we had shown CD47 levels as low as ∼10% of levels on RBCs still impede eating, consistent with the lowest levels of CD47 on RBCs reported in the human population [59]. Nuclear rigidity thus seems a major “eat me” cue.
3 Nuclear Membrane Properties and Mechanosensing in Brief
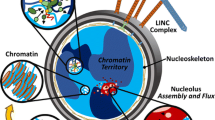
Although mammalian RBCs have only the outer plasma membrane, the RBC progenitor has abundant internal membrane systems, including endoplasmic reticulum which is continuous with the double bilayer of the nuclear envelope. A meshwork of proteins again forms as a sub-membranous cortical layer or lamina, and an understanding of the complex physical properties of this nuclear lamina is just emerging. Unlike the actin filaments and actin-crosslinking proteins spectrin and myosin-II that are main constituents of plasma membrane cortices discussed above for RBCs and the other hematopoietic cells, the nuclear lamina meshwork is formed from self-assembling intermediate filament proteins, called lamins. The lamina lies just inside the nuclear envelope and interacts at least indirectly with chromatin, but the lamina also has protein linkages to nuclear membrane proteins that interact with the cytoskeleton outside the nucleus. The nucleus is thus embedded within and also linked to the stress-generating cytoskeleton, which deforms the nucleus, perhaps affecting gene expression as well as genome integrity. As suggested by the various types of differentiated cells sketched in Fig. 1, nuclear shape and orientation tend to track with cell shape and orientation—which has long been noticed in various nucleated cells (e.g. marrow derived MSCs [87]).
In humans and mice, the main forms of lamin protein are expressed from three genes: lamin-A, lamin-B1, and lamin-B2. Like other intermediate filament proteins, such as keratin in skin, fingernails, and horns, the lamins form coiled coil parallel dimers that assemble into higher-order filamentous structures that fulfill important structural roles [88]. The B-type lamins are distinct in being permanently modified by a greasy farnesyl group that promotes avid interactions of these filaments with the innermost leaflet of the nucleus’ double lipid bilayer and these lamins also interact with lamin-B receptor, which is a transmembrane protein [89]. Such interactions will tend to act as effective physical crosslinks of a meshwork of lamin-B filaments, even though there no reported lamin crosslinker proteins.
Lamin-A was found in a proteomic study of diverse tissues to be almost unique among hundreds of abundant proteins of the cytoskeleton and nucleus, in that lamin-A concentration increased 30-fold as a function of increasing stiffness of tissue, E tissue, from soft bone marrow and brain tissue to stiff muscle and rigid bone [80, 90]. Tissue stiffness is defined of course by how resistant the tissue is to stress and thus relates to the stress in functional tissue: bone sustains and resists high mechanical stress whereas marrow is protected by bone from stress, as is brain, and both shear very easily. Such mechanical differences between tissues are largely attributable to the amount of collagen fiber in the extracellular matrix, which is abundant in bone and minimal in marrow and brain [80]. The finding for lamin-A thus suggests that the nucleus adjusts its levels of this protein to the mean stress σ in most cells and their nuclei in a given tissue, whereas B-type lamins remain nearly constant. Importantly, the stress σ likely tracks the active (and passive) stiffness of a cell, especially contractile activity of myosin-II inside a cell that increases with matrix stiffness In terms of the tissue-type dependent stoichiometry (A:B), an experimental correlation emerges from measurements of composition and mechanics:
As a relevant aside given this chapter’s broad focus on the sculpting of cell membrane shapes, the only other protein discovered in the same proteomic study to exhibit such a strong and clear scaling relationship across diverse tissues is a membrane-interacting protein called cavin-1. Cavin-1 is known to regulate the morphology of mechanosensitive plasma membrane invaginations called caveolae [91, 92]. Such a scaling relationship with stress is an indicator of mechanosensing by such proteins, and since lamin-A is also a filament-forming structural protein, it should directly affect nuclear mechanics.
Micropipette aspiration has once again been used to quantify and clarify the rate-dependent deformation of nuclei under controlled pressures [93, 94]. Because of the log range in lamin-A:B stoichiometry, the characteristic contributions of A- and B-type lamins to nuclear properties have become reasonably clear, with nuclei having low lamin-A:B responding in seconds, whereas nuclei having high lamin-A:B take many minutes to deform when similarly stressed. The B-type lamin filaments that strongly associate with the nucleus’ inner lipid bilayer (via lamin-B farnesylation) understandably contribute mostly to the elastic response of the nucleus, whereas lamin-A contributes most strongly to nuclear viscosity consistent with the flow physics of filamentous polymers [90, 95, 96]. Thus, when lamin-A dominates, the nucleus response is akin to a balloon filled with honey, whereas when lamin-A is very low the nucleus behaves merely as a balloon filled with water. While the importance of A-type lamins in maintaining nuclear structural integrity and cell viability has been appreciated for a long time [94, 97], the influence of lamin-A on cell motility has been more recent. A rate-limiting role for the nucleus and its lamina in migration of a given cell type through small pores is now clear for cancer cells invading nearby tissue [95] and also for hematopoietic cells that either remain within the marrow or else escape from it through small micro-pores in the endothelial lining that separates marrow from blood (Fig. 1).
4 Conclusions
In terms of future directions, a deeper understanding of the biophysical similarities and differences between a nucleus and an RBC should be pursued. Indeed, one caveat to the analyses above is that it undoubtedly applies to a flaccid nucleus in which the chromatin is highly hydrated within a relative nuclear volume that is roughly similar to that of an RBC discocyte (e.g., Fig. 2). The ∼2 meters of DNA folded as chromatin inside each and every nucleus contributes most clearly to nuclear rigidity only when the genome becomes condensed with loss of water and nuclear volume [94]. Mobile nuclear proteins including DNA repair factors and transcription factors might be lost or have limited access to dense DNA [98], thereby suppressing gene expression, but the high nuclear rigidity of such a dehydrated nucleus will also tend to stimulate local contractility of myosin-II (especially MIIB) in driving an asymmetric process of “cytokinesis” or nuclear expulsion (per erythropoiesis in Fig. 1). The rigidity of an expelled nucleus will also tend to favor its phagocytosis by bone marrow macrophages regardless of whether the “Self” marker CD47 is present or not (Fig. 3), whereas the nascent RBC reticulocyte is highly flexible in being filled with a solution of hemoglobin. Severing of the lipid membrane tether between nucleus and reticulocyte and loss of lipid membrane blebs in maturation to an RBC also raise issues of limits on nuclear membrane integrity. This is an exciting topic with increasing evidence of curvature-dependent rupture of the lamin-B meshwork that is somehow modulated by lamin-A and followed by loss of integrity of the double bilayer [99]. Within the marrow, such a stepwise process of nuclear rigidification, gene expression shutdown, nuclear expulsion, and engulfment with severing of the tether between nucleus and flexible reticulocyte are the final stages in the marrow for generating an RBC—with rich biophysics to be perturbed and more deeply understood.
References
Morrison SJ, Scadden DT (2014) The bone marrow niche for haematopoietic stem cells. Nature 505:327–334
Thomas ED, Lochte HL Jr, Lu WC, Ferrebee JW (1957) Intravenous infusion of bone marrow in patients receiving radiation and chemotherapy. N Engl J Med 257:491–496
Shin JW, Buxboim A, Spinler KR, Swift J et al (2014) Contractile forces sustain and polarize hematopoiesis from stem and progenitor cells. Cell Stem Cell 14:81–93
Betschinger J, Knoblich JA (2004) Dare to be different: asymmetric cell division in Drosophila, C. elegans and vertebrates. Curr Biol 14:R674–R685
Rhyu MS, Jan LY, Jan YN (1994) Asymmetric distribution of numb protein during division of the sensory organ precursor cell confers distinct fates to daughter cells. Cell 76:477–491
Chang JT, Palanivel VR, Kinjyo I, Schambach F et al (2007) Asymmetric T lymphocyte division in the initiation of adaptive immune responses. Science 315:1687–1691
Li R, Gundersen GG (2008) Beyond polymer polarity: how the cytoskeleton builds a polarized cell. Nat Rev Mol Cell Biol 9:860–873
Raab M, Discher DE (2016) Matrix rigidity regulates the microtubule network polarization in migration. Cytoskeleton (Hoboken) 74(3):114–124. https://doi.org/10.1002/cm.21349
Merkel R, Simson R, Simson DA, Hohenadl M et al (2000) A micromechanic study of cell polarity and plasma membrane cell body coupling in Dictyostelium. Biophys J 79:707–719
Shin JW, Swift J, Spinler KR, Discher DE (2011) Myosin-II inhibition and soft 2D matrix maximize multinucleation and cellular projections typical of platelet-producing megakaryocytes. Proc Natl Acad Sci 108(28):11458–11463
Sedzinski J, Biro M, Oswald A, Tinevez JY, Salbreux G, Paluch E (2011) Polar actomyosin contractility destabilizes the position of the cytokinetic furrow. Nature 476:462–466
Engler AJ, Sen S, Sweeney HL, Discher DE (2006) Matrix elasticity directs stem cell lineage specification. Cell 126:677–689
Holst J, Watson S, Lord MS, Eamegdool SS, Bax DV, Nivison-Smith LB, Kondyurin A, Ma L, Oberhauser AF, Weiss AS, Rasko JE (2010) Substrate elasticity provides mechanical signals for the expansion of hemopoietic stem and progenitor cells. Nat Biotechnol 28(10):1123–1128
Adamo L, Naveiras O, Wenzel PL, McKinney-Freeman S, Mack PJ, Gracia-Sancho J, Suchy-Dicey A, Yoshimoto M, Lensch MW, Yoder MC, García-Cardeña G, Daley GQ (2009) Biomechanical forces promote embryonic haematopoiesis. Nature 459(7250):1131–1135
Shin ME, He Y, Li D, Na S, Chowdhury F, Poh YC, Collin O, Su P, de Lanerolle P, Schwartz MA, Wang N, Wang F (2010) Spatiotemporal organization, regulation, and functions of tractions during neutrophil chemotaxis. Blood 116:3297–3310
Ubukawa K, Guo YM, Takahashi M, Hirokawa M, Michishita Y, Nara M, Tagawa H, Takahashi N, Komatsuda A, Nunomura W, Takakuwa Y, Sawada K (2012) Enucleation of human erythroblasts involves non-muscle myosin IIB. Blood 119(4):1036–1044
Hebiguchi M, Hirokawa M, Guo YM, Saito K, Wakui H, Komatsuda A, Fujishima N, Takahashi N, Takahashi T, Sasaki T, Nunomura W, Takakuwa Y, Sawada K (2008) Dynamics of human erythroblast enucleation. Int J Hematol 88(5):498–507
Chasis JA, Mohandas N (2008) Erythroblastic islands: niches for erythropoiesis. Blood 112(3):470–478
Junt T, Schulze H, Chen Z, Massberg S, Goerge T, Krueger A, Wagner DD, Graf T, Italiano JE Jr, Shivdasani RA, von Andrian UH (2007) Dynamic visualization of thrombopoiesis within bone marrow. Science 317:1767–1770
Spinler KR, Shin JW, Lambert MP, Discher DE (2015) Myosin-II repression favors pre/proplatelets but shear activation generates platelets and fails in macrothrombocytopenia. Blood 125(3):525–533
Smith AS, Nowak RB, Zhou S, Giannetto M, Gokhin DS, Papoin J, Ghiran IC, Blanc L, Wan J, Fowler VM (2018 May 8) Myosin IIA interacts with the spectrin-actin membrane skeleton to control red blood cell membrane curvature and deformability. Proc Natl Acad Sci USA 115(19):E4377–E4385
Waugh RE, McKenney JB, Bauserman RG, Brooks DM, Valeri CR, Snyder LM (1997) Surface area and volume changes during maturation of reticulocytes in the circulation of the baboon. J Lab Clin Med 129(5):527–535
Discher DE, Mohandas N, Evans EA (1994) Molecular maps of red cell deformation: hidden elasticity and in situ connectivity. Science 266:1032–1035
Subramanian S, Tsai R, Sen S, Dahl KN, Discher DE (2006) Membrane mobility and clustering of Integrin Associated Protein (IAP, CD47)—Major differences between mouse and man and implications for signaling. Blood Cells Mol Dis 36(3):364–372
Schmidt CF, Svoboda K, Lei N, Petsche IB, Berman LE, Safinya CR, Grest GS (1993) Existence of a flat phase in red cell membrane skeletons. Science 259(5097):952–955
Gifford SC, Derganc J, Shevkoplyas SS, Yoshida T, Bitensky MW (2006) A detailed study of time-dependent changes in human red blood cells: from reticulocyte maturation to erythrocyte senescence. Br J Haematol 135(3):395–404
Discher DE, Boal DH, Boey SK (1998) Simulations of the erythrocyte cytoskeleton at large deformation II: micropipette aspiration. Biophys J 75(3):1584–1597
Johnson CP, Tang HY, Carag C, Speicher DW, Discher DE (2007) Forced unfolding of proteins within cells. Science 317:663–666
Sen S, Subramanian S, Discher DE (2005) Indentation and adhesive probing of a cell membrane with AFM: model and experiments. Biophys J 89:3202–3213
Hategan A, Law R, Kahn S, Discher DE (2003) Adhesively tensed erythrocyte membrane: lysis dynamics and AFM probing. Biophys J 85:2746–2759
Evans E, Ritchie K (1999) Strength of a weak bond connecting flexible polymer chains. Biophys J 76(5):2439–2447
Shu S, Liu X, Korn ED (2005) Blebbistatin and blebbistatin-inactivated myosin II inhibit myosin II-independent processes in dictyostelium. Proc Natl Acad Sci USA 102:1472–1477
Skoczek DA, Walczysko P, Horn N, Parris A, Clare S, Williams MR, Sobolewski A (2014) Luminal microbes promote monocyte-stem cell interactions across a healthy colonic epithelium. J Immunol 193:439–451
Yonit L, Deborah W, Ronnie BG, David E, Keren SH, Merad M, Jung S, Amit I (2014) Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment. Cell 159:1312–1326
Alvey C, Discher DE (2017 July) Engineering macrophages to eat cancer: from “marker of self” CD47 and phagocytosis to differentiation. J Leukoc Biol 102(1):31–40
Rodriguez PL, Harada T, Christian DA, Pantano DA, Tsai RK, Discher DE (2013) Minimal “self” peptides that inhibit phagocytic clearance and enhance delivery of nanoparticles. Science 339:971–975
Hu CM, Zhang L, Aryal S, Cheung C, Fang RH, Zhang L (2011) Erythrocyte membrane-camouflaged polymeric nanoparticles as a biomimetic delivery platform. Proc Natl Acad Sci USA 108:10980–10985
Geng Y, Dalhaimer P, Cai S, Tsai R, Tewari M, Minko T, Discher DE (2007) Shape effects of filaments versus spherical particles in flow and drug delivery. Nat Nanotechnol 2:249–255
Chambers E, Mitragotri S (2007) Long circulating nanoparticles via adhesion on red blood cells: Mechanism and extended circulation. Exp Biol Med (Maywood) 232:958–966
Bartlett DW, Su H, Hildebrandt IJ, Weber WA, Davis ME (2007) Impact of tumor-specific targeting on the biodistribution and efficacy of siRNA nanoparticles measured by multimodality in vivo imaging. Proc Natl Acad Sci USA 104:15549
Swanson JA, Hoppe AD (2004) The coordination of signaling during Fc receptor-mediated phagocytosis. J Leukoc Biol 76:1093
Wong C, Stylianopoulos T, Cui J, Martin J, Chauhan VP, Jiang W, Popovic Z, Jain RK, Bawendi MG, Fukumura D (2011) Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc Natl Acad Sci USA 108:2426–2431
Turk MJ, Waters DJ, Low PS (2004) Folate-conjugated liposomes preferentially target macrophages associated with ovarian carcinoma. Cancer Lett 213:165–172
Rhee I, Davidson D, Souza CM, Vacher J, Veillette A (2013) Macrophage fusion is controlled by the cytoplasmic protein tyrosine phosphatase PTP-PEST/PTPN12. Mol Cell Biol 33:2458–2469
Turrini F, Arese P, Yuan J, Low PS (1991) Clustering of integral membrane proteins of the human erythrocyte membrane stimulates autologous IgG binding, complement deposition, and phagocytosis. J Biol Chem 266:23611–23617
Franco RS, Puchulu-Campanella ME, Barber LA, Palascak MB, Joiner CH, Low PS, Cohen RM (2013) Changes in the properties of normal human red blood cells during in vivo aging. Am J Hematol 88:44–51
Wilflingseder D, Banki Z, Garcia E, Pruenster M, Pfister G, Muellauer B, Nikolic DS, Gassner C, Ammann CG, Dierich MP, Piguet V, Stoiber H (2007) IgG opsonization of HIV impedes provirus formation in and infection of dendritic cells and subsequent long-term transfer to T cells. J Immunol 178:7840
Discher DE, Ortiz V, Srinivas G, Klein ML, Kim Y, Christian D, Cai S, Photos P, Ahmed F (2007) Emerging applications of polymersomes in delivery: from molecular dynamics to shrinkage of tumors. Prog Polym Sci 32:838–857
Lundqvist M, Stigler J, Elia G, Lynch I, Cedervall T, Dawson KA (2008) Nanoparticle size and surface properties determine the protein corona with possible implications for biological impacts. Proc Natl Acad Sci USA 105:14265
Rettig MP, Low PS, Gimm JA, Mohandas N, Wang J, Christian JA (1999) Evaluation of biochemical changes during in vivo erythrocyte senescence in the dog. Blood 93:376–384
Sosale NG, Rouhiparkouhi T, Bradshaw AM, Dimova R, Lipowsky R, Discher DE (2015) Cell rigidity and shape override CD47’s “self”-signaling in phagocytosis by hyperactivating myosin-II. Blood 125:542–552
JK A, Hempel G, Koling S, Chan LS, Fisher T, Meiselman HJ, Garratty G (2007) Antibody against poly (ethylene glycol) adversely affects PEG-asparaginase therapy in acute lymphoblastic leukemia patients. Cancer 110:103–111
Cox D, Greenberg S (2001) Phagocytic signaling strategies. Fc (gamma) receptor-mediated phagocytosis as a model system. Semin Immunol 13:339–345
Greenberg S, Chang P, Silverstein SV (1994) Tyrosine phosphorylation of the gamma subunit of Fc gamma receptors, p72syk, and paxillin during Fc receptor-mediated phagocytosis in macrophages. J Biol Chem 269:3897–3902
Aderem A, Underhill BM (1999) Mechanisms of phagocytosis in macrophages. Annu Rev Immunol 17:593–623
Wolfenson H, Bershadsky A, Henis YI, Geiger B (2011) Actomyosin-generated tension controls the molecular kinetics of focal adhesions. J Cell Sci 124:1425–1432
Raab M, Swift J, Dingal D, Shah P, Shin JW, Discher DE (2012) Crawling from soft to stiff matrix polarizes the cytoskeleton and phosphoregulates myosin-II heavy chain. J Cell Biol 199:669–683
Tsai RK, Discher DE (2008) Inhibition of “self” engulfment through deactivation of myosin-II at the phagocytic synapse between human cells. J Cell Biol 180:989–1003
Tsai RK, Rodriguez PL, Discher DE (2010) Self inhibition of phagocytosis: The affinity of ‘marker of self’ CD47 for SIRP alpha dictates potency of inhibition but only at low expression levels. Blood Cells Mol Dis 45:67–74
Murata Y, Saito Y, Kaneko T, Kotani T, Kaneko Y, Ohnishi H, Matozaki T (2014) Autoimmune animal models in the analysis of the CD47-SIRP alpha signaling pathway. Methods 65:254–259
Okazawa H, Motegi S, Ohyama N, Ohnishi H, Tomizawa T, Kaneko Y, Oldenborg PA, Ishikawa O, Matozaki T (2005) Negative regulation of phagocytosis in macrophages by the CD47-SHPS-1 system. J Immunol 174:2004–2011
Oldenborg PA, Zheleznyak A, Fang YF, Lagenaur CF, Gresham HD, Lindberg FP (2000) Role of CD47 as a marker of self on red blood cells. Science 288:2051–2054
Willingham SB, Volkmer JP, Gentles AJ, Sahoo D, Dalerba P, Mitra SS, Wang J, Contreras-Trujillo H, Martin R, Cohen JD, Lovelace P, Scheeren FA, Chao MP, Weiskopf K, Tang C, Volkmer AK, Naik TJ, Storm TA, Mosley AR, Edris B, Schmid SM, Sun CK, Chua MS, Murillo O, Rajendran P, Cha AC, Chin RK, Kim D, Adorno M, Raveh T, Tseng D, Jaiswal S, Enger PØ, Steinberg GK, Li G, So SK, Majeti R, Harsh GR, van de Rijn M, Teng NN, Sunwoo JB, Alizadeh AA, Clarke MF, Weissman IL (2012) The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc Natl Acad Sci USA 109:6662
Horrigan SK (2017) Replication study: the CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. eLife 6:e18173. https://doi.org/10.7554/eLife.18173
Alvey CM, Spinler KR, Irianto J, Pfeifer CR, Hayes B, Xia Y, Cho S, Dingal PCPD, Hsu J, Smith L, Tewari M, Discher DE (2017 July 24) SIRPA-inhibited, marrow-derived macrophages engorge, accumulate, and differentiate in antibody-targeted regression of solid tumors. Curr Biol 27(14):2065–2077
Bentley AA, Adams JC (2010) The evolution of thrombospondins and their ligand-binding activities. Mol Biol Evol 9:2187–2197
Oldenborg P-A, Gresham HD, Chen Y, Izui S, Lindberg FP (2002) Lethal autoimmune hemolytic anemia in CD47-deficient nonobese diabetic (NOD) mice. Blood 99:3500–3504
Subramanian S, Parthasarathy R, Sen S, Boder ET, Discher DE (2006) Species- and cell type-specific interactions between CD47 and human SIRPalpha. Blood 107:2548–2556
Kwong LS, Brown MH, Barclay AN, Hatherley D (2014) Signal-regulatory protein alpha from the NOD mouse binds human CD47 with an exceptionally high affinity—implications for engraftment of human cells. Immunology 143:61–67
Soto-Pantoja DR, Miller TW, Frazier WA, Roberts DD (2012) Inhibitory signaling through signal regulatory protein-alpha is not sufficient to explain the antitumor activities of CD47 antibodies. Proc Natl Acad Sci USA 109:2842–2842
Zhao XW, Matlung HL, Kuijpers TW, van den Berg TK (2012) On the mechanism of CD47 targeting in cancer. Proc Natl Acad Sci USA 109:2843–2843
SB W, Volkmer JP, Gentles AJ, Sahoo D, Dalerba P, Mitra SS, Wang J, Contreras-Trujillo H, Martin R, Cohen JD, Lovelace P, Scheeren FA, Chao MP, Weiskopf K, Tang C, Volkmer AK, Naik TJ, Storm TA, Mosley AR, Edris B, Schmid SM, Sun CK, Chua MS, Murillo O, Rajendran P, Cha AC, Chin RK, Kim D, Adorno M, Raveh T, Tseng D, Jaiswal S, Enger PØ, Steinberg GK, Li G, So SK, Majeti R, Harsh GR, van de Rijn M, Teng NN, Sunwoo JB, Alizadeh AA, Clarke MF, Weissman IL (2012) The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc Natl Acad Sci USA 109(17):6662–6667
Jaiswal S, Jamieson CH, Pang WW, Park CY, Chao MP, Majeti R, Traver D, van Rooijen N, Weissman IL (2009) CD47 is upregulated on circulating hematopoietic stem cells and leukemia cells to avoid phagocytosis. Cell 138:271–285
Lindberg FP, Lublin DM, Telen MJ, Veile RA, Miller YE, Donis-Keller H, Brown EJ (1994) Rh-related antigen CD47 is the signal-transducer integrin-associated protein. J Biol Chem 269:1567–1570
Gardai SJ, McPhillips KA, Frasch SC, Janssen WJ, Starefeldt A, Murphy-Ullrich JE, Bratton DL, Oldenborg PA, Michalak M, Henson PM (2005) Cell-surface calreticulin initiates clearance of viable or apoptotic cells through trans-activation of LRP on the phagocyte. Cell 123:321–334
Arfsten J, Leupold S, Bradtmoeller C, Kampen I, Kwade A (2010) Atomic force microscopy studies on the nanomechanical properties of Saccharomyces cerevisiae. Colloid Surf B 79:284–290
Beningo KA, Wang YL (2002) Fc-receptor-mediated phagocytosis is regulated by mechanical properties of the target. J Cell Sci 115:849–856
Lam WA, Rosenbluth MJ, Fletcher DA (2007) Chemotherapy exposure increases leukemia cell stiffness. Blood 109:3505–3508
Cross SE, Jin YS, Rao J, Gimzewski JK (2007) Nanomechanical analysis of cells from cancer patients. Nat Nanotechnol 2:780–783
Swift J, Ivanovska IL, Buxboim A, Harada T, Dingal PC, Pinter J, Pajerowski JD, Spinler KR, Shin JW, Tewari M, Rehfeldt F, Speicher DW, Discher DE (2013) Nuclear lamin-A scales with tissue stiffness and enhances matrix-directed differentiation. Science 341(6149):1240104
Merkel TJ, Jones SW, Herlihy KP, Kersey FR, Shields AR, Napier M, Luft JC, Wu H, Zamboni WC, Wang AZ, Bear JE, DeSimone JM (2011) Using mechanobiological mimicry of red blood cells to extend circulation times of hydrogel microparticles. Proc Natl Acad Sci USA 108:586–591
Mebius RE, Kraal G (2005) Structure and function of the spleen. Nat Rev Immunol 5:606–616
Deplaine G, Safeukui I, Jeddi F, Lacoste F, Brousse V, Perrot S, Biliqui S, Guillotte M, Guitton C, Dokmak S, Aussilhou B, Sauvanet A, Cazals Hatem D, Paye F, Thellier M, Mazier D, Milon G, Mohandas N, Mercereau-Puijalon O, David PH, Buffet PA (2011) The sensing of poorly deformable red blood cells by the human spleen can be mimicked in vitro. Blood 117:88–95
Champion JA, Mitragotri S (2006) Role of target geometry in phagocytosis. Proc Natl Acad Sci USA 103:4930–4934
Yoshida H, Kawane K, Koike M, Mori Y, Uchiyama Y, Nagata S (2005) Phosphatidylserine-dependent engulfment by macrophages of nuclei from erythroid precursor cells. Nature 437(7059):754–758
Bell AJ, Satchwell TJ, Heesom KJ, Hawley BR, Kupzig S, Hazell M, Mushens R, Herman A, Toye AM (2013) Protein distribution during human erythroblast enucleation in vitro. PLoS One 8(4):e60300
Buxboim A, Irianto J, Swift J, Athirasala A, Shin JW, Rehfeldt F, Discher DE (2017 Nov 7) Coordinated increase of nuclear tension and lamin-A with matrix stiffness outcompetes lamin-B receptor that favors soft tissue phenotypes. Mol Biol Cell 28(23):3333–3348
Herrmann H, Strelkov SV, Burkhard P, Aebi U (2009) Intermediate filaments: primary determinants of cell architecture and plasticity. J Clin Invest 119:1772–1783
Dechat T, Adam SA, Taimen P, Shimi T, Goldman RD (2010) Nuclear lamins. Cold Spring Harb Perspect Biol 2:a000547
Buxboim A, Swift J, Irianto J, Spinler KR, Dingal PC, Athirasala A, Kao YR, Cho S, Harada T, Shin JW, Discher DE (2014) Matrix elasticity regulates lamin-AC phosphorylation and turnover with feedback to actomyosin. Curr Biol 24(16):1909–1917
Echarri A, Del Pozo MA (2015 Aug 1) Caveolae - mechanosensitive membrane invaginations linked to actin filaments. J Cell Sci 128(15):2747–2758
Sinha B, Köster D, Ruez R, Gonnord P, Bastiani M, Abankwa D, Stan RV, Butler-Browne G, Vedie B, Johannes L, Morone N, Parton RG, Raposo G, Sens P, Lamaze C, Nassoy P (2011 Feb 4) Cells respond to mechanical stress by rapid disassembly of caveolae. Cell. 144(3):402–413
Dahl KN, Engler AJ, Pajerowski JD, Discher DE (2005) Power-law rheology of isolated nuclei with deformation mapping of nuclear substructures. Biophys J 89:2855–2864
Pajerowski JD, Dahl KN, Zhong FL, Sammak PJ, Discher DE (2007) Physical plasticity of the nucleus in stem cell differentiation. Proc Natl Acad Sci USA 104:15619–15624
Harada T, Swift J, Irianto J, Shin JW, Spinler KR, Athirasala A, Diegmiller R, Dingal PC, Ivanovska IL, Discher DE (2014) Nuclear lamin stiffness is a barrier to 3D migration, but softness can limit survival. J Cell Biol 204:669–682
Shin JW, Spinler KR, Swift J, Chasis JA, Mohandas N, Discher DE (2013) Lamins regulate cell trafficking and lineage maturation of adult human hematopoietic cells. Proc Natl Acad Sci USA 110(47):18892–18897
Broers JL, Peeters EA, Kuijpers HJ, Endert J, Bouten CV, Oomens CW, Baaijens FP, Ramaekers FC (2004) Decreased mechanical stiffness in LMNA−/− cells is caused by defective nucleo-cytoskeletal integrity: implications for the development of laminopathies. Hum Mol Genet 13:2567–2580
Irianto J, Pfeifer CR, Bennett RR, Xia Y, Ivanovska IL, Liu AJ, Greenberg RA, Discher DE (2016) Nuclear constriction segregates mobile nuclear proteins away from chromatin. Mol Biol Cell 27(25):4011–4020
Xia Y, Ivanovska IL, Zhu K, Smith L, Irianto J, Pfeifer CR, Alvey CM, Ji J, Liu D, Cho S, Bennett RR, Liu AJ, Greenberg RA, Discher DE (2018 Aug 31) Nuclear rupture at sites of high curvature compromises retention of DNA repair factors. J Cell Biol pii: jcb.201711161
Acknowledgements
The author gratefully acknowledges support of the National Institutes of Health, including National Heart, Lung & Blood Institute (R01 HL124106, R21 HL128187) and National Cancer Institute under Physical Sciences Oncology Center Award U54 CA193417, a Human Frontiers Sciences Program grant RGP0024, and the US–Israel Binational Science Foundation, National Science Foundation grant agreement CMMI 15-48571.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Discher, D.E. (2018). Biomembrane Mechanical Properties Direct Diverse Cell Functions. In: Bassereau, P., Sens, P. (eds) Physics of Biological Membranes. Springer, Cham. https://doi.org/10.1007/978-3-030-00630-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-00630-3_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00628-0
Online ISBN: 978-3-030-00630-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)