Abstract
Fetal growth restriction (FGR) occurs when the fetus does not reach its intrauterine potential for growth and development as a result of compromise in placental function. FGR affects 5–10% of pregnancies and is the second leading cause of perinatal mortality, responsible for approximately 30% of stillbirths and for increasing the frequency of premature births and intrapartum asphyxia. Unfortunately, no effective therapy is currently available to reverse or at least interrupt the progressive course of placental insufficiency. Nutrition in early life and other exogenous factors like vitamin D and omega-3 have been recognized to play a key role in the pathogenesis of and predisposition to diseases, which seem to go on to subsequent generations. Bed rest in FGR has no benefits proven by scientific evidence and is inconvenient to patients and their families. Sildenafil, nitric oxide, and statins have emerged as treatment options to be implemented. Gene therapy with VEGF and nanotechnology may play a major part in the future with more and multicenter studies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
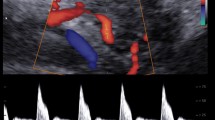
Fetal growth restriction (FGR) is a complication in which the fetal weight is below the 10th percentile. It affects 5–10% of pregnancies [1] and is the second leading cause of perinatal mortality , responsible for approximately 30% of stillbirths and for increasing the frequency of premature births and intrapartum asphyxia . It is also associated with neonatal complications, including meconium aspiration , metabolic and blood disorders , cognitive dysfunction , and cerebral palsy [2]. Hypoxia/acidemia is estimated to be present in 30% of fetuses with growth restriction at birth [3]. Unfortunately, no effective therapy is currently available to reverse or at least interrupt the progressive course of placental insufficiency . Follow-up comprises optimizing care and appropriately timing childbirth and balancing the risks inherent in prematurity and those arising from acidemia with intrauterine permanence. While obstetric expectant management is adopted, fetal well-being is monitored through examinations such as ultrasound, antepartum cardiotocography, Doppler velocimetry, and fetal biophysical profile [4].
Within this context, the use of omega-3 (ω-3) , vitamin D , sildenafil , statins , and nitric oxide has emerged as treatment options, in addition to bed rest and gene therapies, because of their ability to promote fetal development and growth.
Omega-3
Omega-3 (ω-3) fatty acids (FAs) are polyunsaturated carboxylic acids with the first double bond at the third carbon atom. FAs are carboxylic acids (-COOH) containing an aliphatic chain, and they are produced by the breakdown of fat molecules. Therefore, FAs are organic compounds (their molecules contain carbon and hydrogen) and are classified as monounsaturated , polyunsaturated , and saturated FAs [5, 6]. Saturated FAs are compounds in which the carbon atoms are linked by single bonds; these are mainly found in animal products in the solid form. Unsaturated FAs contain carbons linked by one or more double bonds; these mainly exist in vegetables in the liquid form. Such FAs can be either monounsaturated (with one carbon–carbon double bond) or polyunsaturated. Omega (ω) is a classification of unsaturated FAs according to the position number of the carbon linked by the first double bond (3, 6, or 9), counting from the methyl radical (Fig. 11.1). Thus, we have the following ω FAs: (1) ω-3, alpha-linolenic acid , eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) ; (2) ω-6, linoleic acid and arachidonic acid ; and (3) ω-9, oleic acid .
Some FAs are termed “essential” because they cannot be synthesized by the body and must be obtained through the diet (ω-6/ω-3 = 5:1). Western diets and diets consumed in industrialized countries are rich in ω-6 polyunsaturated FAs (PUFAs) because of the consumption of vegetable oils and saturated fats and low in ω-3 PUFAs because of the low consumption of fish. Western diets have a ω-6/ω-3 ratio of approximately 10–20:1. Omega-3 (ω-3) and ω-6 FAs compete with each other for the Δ-6-desaturase enzyme, which is a common key enzyme for both metabolic pathways. Thus, each type of FA can interfere with the metabolism of the other and create nutritional implications. Omega-3 (ω-3) and ω-6 FAs are also precursors for eicosanoids, which are mediators of the lipid origin that modulate inflammatory and immune responses (Fig. 11.2).
These FAs influence cytokine production and the corresponding tissue response. In general, ω-3 FAs reduce systemic inflammatory response and ω-6 FAs increase it. Eicosanoids that result from the metabolism of ω-6 FAs are of the even-numbered series, 2-series prostaglandins, 4-series leukotrienes, and thromboxanes A2, and are important biochemical mediators involved in infection, inflammation, and tissue injury (↑PGE2). Eicosanoids of the odd-numbered series that result from the metabolism of ω-3 FAs, such as 3-series prostaglandins, 5-series leukotrienes, and thromboxanes A3, have a smaller inflammatory effect and a greater effect on the defense mechanism of the immune system (↓PGE2). Several benefits of ω-3 FAs have been described, including reducing triglyceride and LDL cholesterol levels, increasing HDL levels, playing an important role in allergies and inflammatory processes, increasing immune system protection, decreasing blood pressure and coronary artery diseases, rejuvenating skin, and improving depression and cognitive skills. Their use in obstetrics is controversial. Preterm labor prevention and intellectual development promotion have been reported [7,8,9]. Other researchers have reported that ω-3 supplementation does not influence the gestation period or fetal weight and have no effect on fetuses with growth restriction [10, 11]. Further studies must be conducted to demonstrate the real influence of ω-3 FAs on fetal growth and development.
Vitamin D
Vitamin D (Fig. 11.3), which promotes fetal development and growth, is an emerging treatment option for FGR. Vitamin D is a steroid that is involved in intestinal calcium absorption and calcium homeostasis regulation and is essential for the formation and maintenance of strong and healthy bones. Vitamin D deficiency can be caused by inadequate sun exposure, ineffective food intake, decreased absorption, abnormal metabolism, or resistance to vitamin D. Recently, several chronic diseases, such as cancer, hypertension, and osteoporosis, and several autoimmune diseases have been associated with vitamin D deficiency.
Humans have two sources of vitamin D: an exogenous source, provided by diet, in the forms of vitamin D2 and D3 and an endogenous source, in which cholecalciferol (D3), which is the main source of vitamin D, is synthesized in the skin when ultraviolet B (UVB) radiation causes the photolysis of 7-dehydrocholesterol and its conversion to vitamin D3. Exposure to sunlight or UVB radiation up to 18 IU/cm2 in 3 h is sufficient. This process has two stages. The first stage occurs in the dermis and comprises the photoconversion of 7-dehydrocholesterol to previtamin D3 or pre-cholecalciferol (Fig. 11.4). The second stage comprises a chemical isomerization that occurs depending on the body temperature, in which previtamin D slowly and progressively gets converted to vitamin D3, which has a high affinity for vitamin D-binding protein (DBP) , while previtamin D , which has a lower affinity, remains in the skin. When it reaches the skin capillary bed, vitamin D is bound to DBP and gets transported to the liver, where its metabolic transformation begins [12].
The two types of vitamin D undergo complex processing to become metabolically active. Initially, the prohormone undergoes 25th-carbon hydroxylation in the liver via the action of 25-vitamin D 1-hydroxylase (1-OHase) , which is a part of an enzymatic system dependent on cytochrome P-450 (CYP27B) , present in the liver microsomes and mitochondria. This reaction generates 25-hydroxyvitamin D [25(OH)D] , which is the most abundant circulating form of vitamin D, with an average blood concentration of 20–50 ng/ml (50–125 nmol/L) and a half-life of approximately 3–4 weeks. Its pool in the bloodstream is estimated to be in dynamic equilibrium with the reserves of 25(OH)D (muscles and adipose tissue). This makes the blood concentration a reliable measurement of vitamin D in the body. Under normal conditions, the percentage of conversion to 25(OH)D is low, with an almost 50% distribution in the fat and muscle compartments. If vitamin D ingestion is excessive, then most of it gets fixed in fat tissues [12]. Because of its low biological activity, 25(OH)D is transported to the kidneys, where it undergoes a second hydroxylation, resulting in the active forms calcitriol (1,25-dihydroxyvitamin D [1,25(OH)2D]) and calcitroic acid (24,25-dihydroxyvitamin D [24,25(OH)2D]) via the action of 1-OHase enzymes and vitamin D-24-hydroxylase (24-OHase) present in the mitochondria of cells of the proximal convoluted tubule. DBP and 25(OH)D are filtered by the glomerulus and absorbed in the proximal tubule by low-density lipoprotein receptors, which control the capture of the 25(OH)D–DBP complex within the cells of the tube and the subsequent hydroxylation of 1,25(OH)2D.
Several factors regulate 1,25(OH)2D levels, such as 1-OHase, the hydroxylation of which is activated by parathyroid hormone (PTH) , and calcitonin , which is inhibited by the plasma levels of calcium, phosphorus, and 1,25(OH)2D itself, whose half-life is 15 days. The blood concentration of phosphorus directly acts, without PTH intervention, and hypophosphatemia increases the production of 1,25(OH)2D [12] (Fig. 11.4).
Recent studies have emphasized on the importance of the nontraditional roles of vitamin D in pregnancy and in the placenta and have reported an association of vitamin D deficiency in pregnancy with preeclampsia, insulin resistance, gestational diabetes, bacterial vaginosis, increased prematurity, and placental abruption, as well as FGR. Currently, nutrition in early life and other exogenous factors have been recognized to play a key role in the pathogenesis of and predisposition to diseases, which seem to go on to subsequent generations. Epigenetic changes establish a connection with the nutritional status during the critical periods of development and cause changes in gene expression that can lead to the development of disease phenotypes. However, whether vitamin D influences fetal growth, particularly in cases of growth restriction, remains unclear. Further, maternal vitamin D deficiency has been linked to numerous adverse health outcomes, but its association with FGR remains unclear. Population-based studies have confirmed that vitamin D deficiency is considered a public health problem worldwide, particularly in the developing countries, which affects all age groups and has more concerning effects on pregnant women.
In 2010, Bodnar et al. [13] tried to elucidate the association of maternal serum concentrations of 25-hydroxyvitamin D [25(OH)D] in early pregnancy with the risk of small-for-gestational-age (SGA) size and to explore the association between single-nucleotide maternal polymorphisms in the vitamin D receptor gene. Serum 25(OH)D was related to the risk of SGA among white mothers but not among black mothers. The findings suggest that vitamin D has a complex relationship with fetal growth that can vary according to ethnicity. In 2011, Robinson et al. [14] conducted a study aimed at identifying the association of vitamin D levels with the occurrence of SGA in patients with severe and early-onset preeclampsia. They found that vitamin D deficiency was associated with an increased risk of preeclampsia and its diagnosis in the severe and early clinical manifestations. Vitamin D levels were lower among patients with SGA and those with a diagnosis of severe, early-onset preeclampsia than among those without growth restriction. Thus, the authors suspected that vitamin D impacts fetal growth via placental mechanisms [14]. In 2013, Gernand et al. [15] confirmed the association of maternal vitamin D deficiency with FGR, but the mechanisms involved were unclear. They tested the hypothesis that maternal 25(OH)D was associated with an increased risk of placental insufficiency. The result was that the relationship between 25(OH)D and vascular damage was modified by the child’s sex. No association was observed between maternal 25(OH)D and vascular disorder in mothers with female fetuses. Therefore, the findings suggested complex relationships among vitamin D, placental vascular damage, and birth weight, which differed according to the child’s sex. Maternal vitamin D status may be beneficial for male and female descendants through different mechanisms. In 2014, Gernand et al. [16] examined the association of maternal serum concentrations of 25(OH)D with the risk of SGA newborns. The mean 25(OH)D concentration was lower in women with SGA newborns than in those with newborns with an adequate weight. Maternal obesity and ethnicity influenced this relationship. Maternal vitamin D status in the second trimester is associated with the risk of SGA in all women and in the subgroups of white and nonobese women.
In 2015, Khalessi et al. [17] found that maternal hypovitaminosis D harms fetal growth and causes adverse results in pregnancy, including FGR and low birth weight . The mean maternal vitamin D level was lower for newborns with low birth weight than for those with an adequate birth weight. All mothers of newborns with a head circumference of ≤33 cm also had vitamin D deficiency . In 2016, Miliku et al. [18] examined maternal vitamin D concentrations during pregnancy, fetal growth patterns, and the risk of adverse outcomes at birth and reported an association of low maternal 25(OH)D concentrations with FGR and with an increased risk of preterm birth and SGA size at birth. Further studies are needed to investigate the causality of these associations and the potential for public health interventions. In 2017, Wookey et al. [19] investigated whether DBP expression is altered in placental dysfunction associated with FGR. Their results showed significantly reduced placental DBP levels, which were strongly associated with idiopathic FGR. Thus, DBP may be a factor in unexplained placental dysfunction associated with idiopathic FGR and can potentially serve as a biomarker for this disease [19].
Sildenafil
Recently, one of the most widely studied treatments has been sildenafil , which is a phosphodiesterase type 5 inhibitor; it blocks the enzyme phosphodiesterase, preventing the degradation of cyclic guanosine monophosphate (cGMP) and potentializing the action of nitric oxide [20]. Maternal spiral arteries that have not undergone complete remodeling in the beginning of pregnancy present muscle layers that are still responsive to nitric oxide and can go through vasodilation, leading to an increased blood flow [21].
In November 2017, a meta-analysis by Paauw et al. [22] evaluated 24 studies on sildenafil and FGR published before November 2016. Of these, 22 were conducted using animal models, such as mice, rats, rabbits, sheep, and pigs, and the two studies with humans were randomized clinical trials. The meta-analysis found a significant increase in the fetal weight gain in the group that presented FGR and preeclampsia but not in the pregnancies without any complication. The maximum weight gain was approximately 10% [22]. Furthermore, it showed that differences between the studies, such as different medication dosages and administration methods, did not significantly influence the treatment effectiveness. However, a trend for a better effect was observed when the drug was orally and continuously administered and administered throughout the pregnancy [22]. Finally, the authors warned that few studies have evaluated the safety of using sildenafil during pregnancy because this medication crosses the placental barrier and may cause embryotoxicity at high doses. Further, adverse maternal effects such as intense headaches can occur.
A study including five placebo-controlled randomized multicenter clinical trials on the use of sildenafil and the prognosis for early-onset FGR (STRIDER) is in progress [23], encompassing Australia and New Zealand, the Netherlands, the United Kingdom, Ireland, and Canada. Pregnant women between 18 and 30 weeks with a diagnosis of early-onset, severe FGR are included. Each patient receives a 25 mg dose of sildenafil or a matching placebo thrice a day until 32 weeks of pregnancy. Although each center presents an autonomous clinical trial with a few differences expected between results, it is believed that the multicenter character of STRIDER may help elucidate the role of sildenafil on fetal growth and its safety and efficacy for use in clinical practice.
Nitric Oxide
Nitric oxide has been considered an important bioregulatory molecule acting on vascular tone [24]. It causes vasodilation, relaxes smooth muscle, and inhibits platelet aggregation and leukocyte adhesion. In pregnancies without any disease, uterine arteries increase the endothelial nitric oxide synthase activity and its protein expression, thereby improving uterine perfusion. This enzyme is also expressed in the placenta and the umbilical artery endothelium, where nitric oxide production contributes to a low resistance in fetal–placental circulation [24].
The exogenous administration of nitric oxide can present an important role in pregnancies with preeclampsia or FGR by increasing uteroplacental perfusion [25]. A randomized clinical trial, published in 2017, used nitroglycerin patches and placebo in pregnant women with FGR. The patches released 10 mg every 24 h and were used for 3 consecutive days. The result was decreased uterine and umbilical arteries resistance and pulsatility. Another study from the same year compared nitric oxide plus maternal plasma expansion with placebo in pregnant women with FGR. Glyceryl trinitrate transdermal patches releasing 5 mg every 24 h were used only 12 h a day to prevent tolerance. Fluid intake was increased to 2.5 l of water per day. After 2 weeks, a decrease in the systemic vascular resistance and an increase in the cardiac output were noticed in the group receiving the treatment. At birth, newborns from the medication group were at a greater weight percentile [26].
New technologies are being tested, such as using a vasodilator (SE175) that also releases nitric oxide combined with a peptide that would act only on the uterine and placental region, thereby minimizing tolerance and side effects. The group responsible for this research already has promising results in animals, with increased weight percentiles and decreased vascular resistance, showing that this may be a part of clinical practice in the coming years [27].
Bed Rest
Bed rest at the hospital or at home is widely prescribed for several obstetric complications, including preterm labor, hemorrhagic syndromes, multiple gestation, pregnancy hypertension, and FGR [28]. It is estimated that 700,000 patients are prescribed bed rest every year in the United States [29]. Patients with FGR are routinely advised to rest in an attempt to improve uteroplacental perfusion . Bed rest supposedly decreases the peripheral blood flow and inferior vena cava compression and improves the venous return and cardiac output, thereby increasing the uteroplacental circulation [30]. Furthermore, several patients are hospitalized for a stricter control of fetal well-being [28]. However, prolonged bed rest can be harmful to patients and may be associated with an increased risk of thromboembolism [31], muscle atrophy, constipation, and stress, as well as higher costs for the health system [30, 32].
A 2004 study with 104 high-risk patients in bed rest at a hospital showed maternal weekly weight gain to be less than the recommended gain and fetal weight at birth to be lower than the average weight (compared with newborns of the same gestational age, ethnicity, and sex). The study suggested that maternal weight loss associated with bed rest is related to a lower birth weight and an increased risk of FGR [29]. A Cochrane systematic review was conducted to evaluate the effects of bed rest in the hospital on patients with FGR. Only one study, with 107 patients, comparing hospital bed rest with outpatient management (with medical leave from work) was included in the review [33]. No statistically significant differences were observed in weight, gestational age at birth, and neonatal prognosis. The review concluded that there is not enough evidence for prescribing bed rest in the hospital for patients with FGR but pointed out that studies are too scarce to exclude any benefit with a reasonable degree of certainty. Although widely practiced, hospitalization for bed rest in FGR has no benefits proven by scientific evidence and is inconvenient to patients and their families, in addition to the increasing costs [28].
Maternal Gene Therapy with Vascular Endothelial Growth Factor (VEGF)
Inadequate trophoblast invasion results in an incomplete spiral artery remodeling and high-resistance, low-flow circulation [34, 35]. This mechanism leads to reduced placental perfusion, oxidative stress, and an imbalance between the angiogenic factors, such as VEGF and placental growth factor , and the anti-angiogenic factors, such as soluble fms-like tyrosine kinase-1 (sFlT-1) and soluble endoglin [36, 37]. A possible approach for the treatment of FGR would be increasing the VEGF levels in the uterine arteries, leading to vasodilation and an increase in angiogenesis. This can be accomplished by injecting the uterine arteries with adenovirus vectors coding for VEGF through interventional radiology, leading to a short-term increase in VEGF expression [21].
A study in normal sheep pregnancies, published in 2008, showed an increased flow in the uterine arteries due to decreased vasoconstriction. This effect was noticed 4–7 days after injecting the vector, and the increased flow was sustained for up to 6 weeks (until the end of sheep pregnancies) probably because of neovascularization and the modification of vascular reactivity [38, 39]. In 2014, a study in sheep afflicted by FGR and treated using gene therapy with VEGF showed an increase in the growth rate and a decrease in the brain-sparing effect (assessed using the BPD/AC or brain weight/liver weight ratio) in comparison with the group treated with placebo [40]. A 2016 study on Guinea pigs with induced FGR (the placental physiology of Guinea pigs is more similar to the human one than that of other animals) concluded that the treatment led to an increase in the growth rate and fewer fetuses were affected by severe FGR at birth [41]. Animal model studies have not shown evidence that the vector crosses the placental barrier or that VEGF is expressed in fetal tissues [38].
A multicenter clinical trial termed “Does vascular endothelial growth factor gene therapy safely improve outcome in severe early-onset fetal growth restriction?” (EVERREST) is being conducted since 2013 aiming to evaluate the safety and effectiveness of maternal gene therapy with VEGF in severe early-onset FGR [42]. At the moment, the group is conducting a prospective observational study in pregnancies with severe early-onset FGR to define the inclusion criteria, probably pregnant women with severe early-onset FGR with greater risks of fetal and neonatal death [43].
Although the method is invasive, no ethical or legal objections to the use of this therapy in clinical studies in pregnant women were found because the disease still lacks effective treatment and gene therapy with VEGF has the potential to cause vasodilation in maternal uteroplacental circulation [44].
Nanotechnology and Treatment Strategies Targeted at Uteroplacental Circulation
Numerous studies have focused on treatment strategies that may locally act on uteroplacental circulation or on trophoblastic tissue to improve placental function and increase uterine circulation [21].
Peptide sequences that selectively bind to the placenta and, therefore, do not interfere with the normal development can be used to carry proteins such as insulin-like growth factor type 2 specifically to the placental tissue. Insulin-like growth factors stimulate cell proliferation in the placenta and promote a greater placental supply of glucose and amino acids [45, 46]. Studies in mice have shown an increase in the placental and fetal weights [47]. Another treatment currently under study uses microRNA inhibitors , particularly miR145-3 and miR675, that have been identified as placental growth inhibitors. In rats, an increase in the placental and fetal weights was found when compared with controls. Tests with human trophoblastic tissue have also been conducted in the first trimester, decreasing miR145 expression and increasing cytotrophoblast proliferation [48]. Although these new treatment strategies seem promising, all of them require further studies to prove their safety and effectiveness.
Statins
Statins inhibit 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMG-CoA reductase) , which is known for its cardioprotective effect by acting on lipids. However, statins also have anti-inflammatory and antioxidant effects, making them potentially beneficial for inadequate placentation [49]. Statins were classified into Food and Drug Administration (FDA) pregnancy category X in the 1980s. This happened mostly because, at that moment, there were no benefits justifying their use in pregnancy [50]. However, records of exposure to pravastatin in the United States (20 cases) and Canada (288 cases) show no association with fetal malformations [51, 52]. In addition, a prospective observational study conducted in Canada with 64 patients found no greater incidence of fetal malformations resulting from the exposure to pravastatin in the first trimester [53]. If studies with pravastatin show benefits during pregnancy, then this classification will probably be reviewed [54].
A study, published in 2013, on rats with reduced uteroplacental perfusion showed that rats treated with pravastatin improved maternal hypertension , decreased sFlt-1, and increased VEGF and fetal weight compared with controls [55]. In a study on 21 patients with antiphospholipid antibody syndrome treated with aspirin and low-molecular-weight heparin, 11 of these patients were also treated with pravastatin after developing preeclampsia or FGR. The results revealed an increase in the gestational age at delivery and an apparent improvement in the perinatal prognosis in patients who received pravastatin [56].
In England, a randomized double-blind clinical trial is being conducted in patients with early-onset preeclampsia between 24 weeks and 31 weeks and 6 days. The study will measure sFlt-1 levels 48 h after randomization and evaluate neonatal morbidity and mortality [49]. Another randomized double-blind clinical trial is being conducted in the United States with pregnant women between 12 weeks and 16 weeks and 6 days with a history of preeclampsia in prior pregnancies to evaluate the safety and pharmacokinetics of pravastatin in preeclampsia and FGR [57].
Conclusion
Since FGR is diagnosed, there are no proven effective therapies to reverse or at least interrupt the progressive course of placental insufficiency . Fetal surveillance and decision time to delivery are still the main strategies in the management of these fetuses. Some recommendations, like bed rest, despite widely prescribed, are not established to be benefic. Several studies with potential new possibilities of therapies are done, but we have to wait for the results before implementing these treatments in clinical practice.
References
Froen JF, Gardosi JO, Thurmann A, Francis A, Stray-Pedersen B. Restricted fetal growth in sudden intrauterine unexplained death. Acta Obstet Gynecol Scand. 2004;83:801–7.
Barker DJP, Gluckman PD, Godfrey KM. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993;341:938–41.
Mandruzzato GP, Bogatti P, Fisher L, Gigli C. The clinical significance of absent or reverse end diastolic flow in the fetal aorta and umbilical artery. Ultrasound Obstet Gynecol. 1991;1:192–6.
Nardozza LM, Caetano AC, Zamarian AC, Mazzola JB, Silva CP, Marçal VM, et al. Fetal growth restriction: current knowledge. Arch Gynecol Obstet. 2017;295:1061–77.
Waitzberg DL, Garla P. Contribution of omega-3 fatty acids for memory and cognitive function. Nutr Hosp. 2014;30:467–77.
Agostoni C, Marangoni F, Stival G, Gatelli I, Pinto F, Risé P, et al. Whole blood fatty acid composition differs in term versus mildly preterm infants: small versus matched appropriate for gestational age. Pediatr Res. 2008;64:298–302.
Brantsæter AL, Birgisdottir BE, Meltzer HM, Kvalem HE, Alexander J, Magnus P, et al. Maternal seafood consumption and infant birth weight, length and head circumference in the Norwegian Mother and Child Cohort Study. Br J Nutr. 2012;107:436–44.
Gaete MG, Atalah ES. Niveles de LC-PUFA n-3 en la leche maternal despues de incentivar el consumo de valimentosx marinos. Rev Chil Pediatr. 2003;74:158–65.
Olsen SF, Sørensen JD, Secher NJ, Hedegaard M, Henriksen TB, Hansen HS, et al. Randomised controlled trial of effect of fish-oil supplementation on pregnancy duration. Lancet. 1992;25:1003–7.
Saccone G, Berghella V, Maruotti GM, Sarno L, Martinelli P. Omega-3 supplementation during pregnancy to prevent recurrent intrauterine growth restriction: systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet Gynecol. 2015;46:659–64.
Saccone G, Saccone I, Berghella V. Omega-3 long-chain polyunsaturated fatty acids and fish oil supplementation during pregnancy: which evidence? J Matern Fetal Neonatal Med. 2016;29:2389–97.
Urrutia-Pereira M, Sole D. Vitamin D deficiency in pregnancy and its impact on the fetus, the newborn, and in childhood. Rev Paul Pediatr. 2015;33:104–13.
Bodnar LM, Catov JM, Zmuda JM, Cooper ME, Parrott MS, Roberts JM, et al. Maternal serum 25-hydroxyvitamin D concentrations are associated with small-for-gestational age births in white women. J Nutr. 2010;140:999–1006.
Robinson CJ, Wagner CL, Hollis BW, Baatz JE, Johnson DD. Maternal vitamin D and fetal growth in early-onset severe preeclampsia. Am J Obstet Gynecol. 2011;204:556.e1–4.
Gernand AD, Bodnar LM, Klebanoff MA, Parks WT, Simhan HN. Maternal serum 25-hydroxyvitamin D and placental vascular pathology in a multicenter US cohort. Am J Clin Nutr. 2013;98:383–8.
Gernand AD, Simhan HN, Caritis S, Bodnar LM. Maternal vitamin D status and small-for-gestational-age offspring in women at high risk for preeclampsia. Obstet Gynecol. 2014;123:40–8.
Khalessi N, Kalani M, Araghi M, Farahani Z. The relationship between maternal vitamin D deficiency and low birth weight neonates. J Family Reprod Health. 2015;9:113–7.
Miliku K, Vinkhuyzen A, Blanken LM, McGrath JJ, Eyles DW, Burne TH, et al. Maternal vitamin D concentrations during pregnancy, fetal growth patterns, and risks of adverse birth outcomes. Am J Clin Nutr. 2016;103:1514–22.
Wookey AF, Chollangi T, Yong HE, Kalionis B, Brennecke SP, Murthi P, et al. Placental vitamin D-binding protein expression in human idiopathic fetal growth restriction. J Pregnancy. 2017;2017:5120267.
El-Sayed MA, Saleh SA, Maher MA, Khidre AM. Utero-placental perfusion Doppler indices in growth restricted fetuses: effect of sildenafil citrate. J Mater Fetal Neonatal Med. 2018;31:1045–50.
Gromm KM, David AL. The role of aspirin, heparin, and other interventions in the prevention and treatment of fetal growth restriction. Am J Obstet Gynecol. 2018;218:S829–40.
Paauw ND, Terstappen F, Ganzevoort W, Joles JA, Gremmels H, Lely AT. Sildenafil during pregnancy a preclinical meta-analysis on fetal growth and maternal blood pressure. Hypertension. 2017;70:998–1006.
Pels A, Kenny LC, Alfirevic Z, Baker PN, von Dadelszen P, Gluud C, et al. STRIDER (Sildenafil The Rapy in dismal prognosis early onset fetal growth restriction): an international consortium of randomised placebo-controlled trials. BMC Pregnancy Childbirth. 2017;17:440.
Sladek SM, Magness RR, Conrad KP. Nitric oxide and pregnancy. Am J Phsyiol. 1997;272:441–63.
Gupta S, Chauhan M, Sen J, Nanda S. Effect of transdermal nitroglycerine on Doppler velocity waveforms of the uterine, umbilical and fetal middle cerebral arteries in patients with chronic placental insufficiency: a prospective RCT. J Clin Diagn Res. 2017;11:QC13–7.
Tiralongo GM, Pisani I, Vasapollo B, Khalil A, Thilaganathan B, Valensise H. Effect of a nitric oxide donor on maternal hemodynamics in fetal growth restriction. Ultrasound Obstet Gynecol. 2018;51:514–8.
Cureton N, Korotkova I, Baker B, Greenwood S, Wareing M, Kotamraju VR, et al. Selective targeting of a novel vasodilator to the uterine vasculature to treat impaired uteroplacental perfusion in pregnancy. Theranostics. 2017;7:3715–31.
Say L, Gülmezoglu AM, Hofmeyr GJ. Bed rest in hospital for suspected impaired fetal growth. Cochrane Database Syst Rev. 2000;2:CD000034.
Maloni JA, Alexander GR, Schluchter MD, Shah DM, Park S. Antepartum bed rest: maternal weight change and infant birth weight. Biol Res Nurs. 2004;5:177–86.
Figueroa R, Maulik D. Prenatal therapy for fetal growth restriction. Clin Obstet Gynecol. 2006;49:308–19.
Kovacevich GJ, Gaich SA, Lavin JP, Hopkins MP, Crane SS, Stewart J, et al. The prevalence of thromboembolic events among women with extended bed rest prescribed as part of the treatment for premature labor or preterm premature rupture of membranes. Am J Obstet Gynecol. 2000;182:1089–92.
Heaman M, Gupton A. Perceptions of bed rest by women with high-risk pregnancies: a comparison between home and hospital. Birth. 1998;25:252–8.
Laurin J, Persson PH. The effect of bed rest in hospital on fetal outcome in pregnancies complicated by intra-uterine growth retardation. Acta Obstet Gynecol Scand. 1987;66:407–11.
Brosens JJ, Pijnenborg R, Brosens IA. The myometrial junctional zone spiral arteries in normal and abnormal pregnancies: a review of the literature. Am J Obstet Gynecol. 2002;187:1416–23.
Brosens IA, Robertson WB, Dixon HG. The role of the spiral arteries in the pathogenesis of preeclampsia. Obstet Gynecol Annu. 1972;1:177–91.
Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355:992–1005.
Benton SJ, McCowan LM, Heazell AE, Grynspan D, Hutcheon JA, Senger C, et al. Placental growth factor as a marker of fetal growth restriction caused by placental dysfunction. Placenta. 2016;42:1–8.
David AL, Torondel B, Zachary I, Wigley V, Abi-Nader K, Mehta V, et al. Local delivery of VEGF adenovirus to the uterine artery increases vasorelaxation and uterine blood flow in the pregnant sheep. Gene Ther. 2008;15:1344–50.
Mehta V, Abi-Nader KN, Peebles DM, Benjamin E, Wigley V, Torondel B, et al. Long-term increase in uterine blood flow is achieved by local overexpression of VEGFA(165) in the uterine arteries of pregnant sheep. Gene Ther. 2012;19:925–35.
Carr DJ, Wallace JM, Aitken RP, Milne JS, Mehta V, Martin JF, et al. Uteroplacental adenovirus vascular endothelial growth factor gene therapy increases fetal growth velocity in growth-restricted sheep pregnancies. Hum Gene Ther. 2014;25:375–84.
Swanson AM, Rossi CA, Ofir K, Mehta V, Boyd M, Barker H, et al. Maternal therapy with Ad.VEGF-A165 increases fetal weight at term in a guinea-pig model of fetal growth restriction. Hum Gene Ther. 2016;27:997–1007.
Gancberg D, Hoeveler A, Draghia-Akli R. Introduction: gene therapy and gene transfer projects of the 7th Framework Programme for Research and Technological Development of the European Union (second part). Hum Gene Ther Clin Dev. 2015;26:77.
Spencer R, Ambler G, Brodszki J, Diemert A, Figueras F, Gratacós E, et al. EVERREST prospective study: a 6-year prospective study to define the clinical and biological characteristics of pregnancies affected by severe early onset fetal growth restriction. BMC Pregnancy Childbirth. 2017;17:43.
Sheppard M, Spencer RN, Ashcroft R, David AL, EVERREST Consortium. Ethics and social acceptability of a proposed clinical trial using maternal gene therapy to treat severe early-onset fetal growth restriction. Ultrasound Obstet Gynecol. 2016;47:484–91.
Harris LK. Could peptide-decorated nanoparticles provide an improved approach for treating pregnancy complications? Nanomedicine. 2016;11(17):2235–8.
Constancia M, Hemberger M, Hughes J, Dean W, Ferguson-Smith A, Fundele R, et al. Placental-specific IGF-II is a major modulator of placental and fetal growth. Nature. 2002;417:945–8.
King A, Ndifon C, Lui S, Widdows K, Kotamraju VR, Agemy L, et al. Tumor-homing peptides as tools for targeted delivery of payloads to the placenta. Sci Adv. 2016;2:e1600349.
Beards F, Jones LE, Charnock J, Forbes K, Harris LK. Placental homing peptide-microRNA inhibitor conjugates for targeted enhancement of intrinsic placental growth signaling. Theranostics. 2017;7:2940–55.
Spencer R, Carr D, David A. Treatment of poor placentation and the prevention of associated adverse outcomes – what does the future hold? Prenat Diagn. 2014;34:677–84.
U.S. Food and Drug Administration Drug bulletin. Fed Reg. 1980;44:37434–67.
Edison R, Muenke M. Mechanistic and epidemiologic considerations in the evaluation of adverse birth outcomes following gestational exposure to statins. Am J Med Genet. 2004;131A:287.
Ofori B, Rey E, Berard A. Risk of congenital anomalies in pregnant users of statin drugs. Br J Clin Pharmacol. 2007;64:496.
Taguchi N, Rubin ET, Hosokawa A. Prenatal exposure to HMG-CoA reductase inhibitor: effects on fetal and neonatal outcomes. Repro Tox. 2008;26:175.
Taguchi N, Rubin ET, Hosokawa A, Choi J, Ying AY, Moretti ME, Koren G, Ito S. Prenatal exposure to HMG-CoA reductase inhibitors: effects on fetal and neonatal outcomes. Reprod Toxicol. 2008;26:175–7.
Bauer AJ, Banek CT, Needham K, Gillham H, Capoccia S, Regal JF, et al. Pravastatin attenuates hypertension, oxidative stress and angiogenic imbalance in rat model of placental ischemia-induced hypertension. Hypertension. 2013;61:1103–10.
Lefkou E, Mamopoulos A, Dagklis T, Vosnakis C, Rousso D, Girardi G. Pravastatin improves pregnancy outcomes in obstetric antiphospholipid syndrome refractory to antithrombotic therapy. J Clin Invest. 2016;126:2933–40.
Costantine M, Cleary K, Eunice Kennedy Shriver National Institute of Child Health and Human Development Obstetric – Fetal Pharmacology Research Units Network. Pravastatin for the prevention of preeclampsia in high-risk pregnant women. Obstet Gynecol. 2013;121:349–53.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Nardozza, L.M.M., Caetano, A.C.R., Zamarian, A.C.P. (2019). Clinical Treatment. In: Nardozza, L., Araujo Júnior, E., Rizzo, G., Deter, R. (eds) Fetal Growth Restriction. Springer, Cham. https://doi.org/10.1007/978-3-030-00051-6_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-00051-6_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00050-9
Online ISBN: 978-3-030-00051-6
eBook Packages: MedicineMedicine (R0)