Abstract
Normal fetal growth can be altered by several pathological processes, including genetic diseases, infections, congenital anomalies, maternal hypoxia, and inadequate placental exchanges. The impossibility to reach the fetal genetic growth potential because of placental malfunction is defined intrauterine growth restriction (IUGR). IUGR causes slowing fetal growth, so that fetal biometry shifts from a higher to a significantly lower percentile during gestation, and it progressively leads to fetal hypoxia, acidemia, multiorgan damage, and death. Indeed, IUGR is associated with an excess of perinatal mortality and short- and long-term morbidity as well as metabolic syndrome in the adulthood. Prenatal diagnosis and appropriate timing of delivery improve neonatal outcomes.
When a fetus is found to be small for gestational age (SGA) at prenatal ultrasound, every effort has to be made to differentiate IUGR from other causes of impaired fetal growth. In case of IUGR, the clinical management is critically dependent on gestational age at onset. In early onset IUGR, the timing of delivery has to take into account the risks of prolonged intrauterine hypoxia versus the complications associated with preterm birth. In late onset IUGR, early induction of labor is probably the most cost-efficient method to prevent perinatal mortality and morbidity. In intermediate-onset IUGR there is a lack of clear evidence about the best tool to identify the fetuses that would benefit of timely delivery.
At birth, neonatal weight, length, and head circumference are indicators of the quality and quantity of intrauterine growth. SGA newborns, both preterm and term, have increased perinatal mortality risk and short-term complications such as birth asphyxia, infections, hypothermia, hypoglycemia, feeding difficulties, respiratory distress syndrome, bronchopulmonary dysplasia, retinopathy of prematurity, and necrotizing enterocolitis.
Even if most term children born SGA experience catch-up growth and achieve a normal adult height, approximately 10% of them remain shorter than peers born appropriate for gestational age. Preterm SGA infants can take four or more years to achieve heights in a normal range and the majority of them show a postnatal growth deficit at the time of hospital discharge (Extra Uterine Growth Restriction, EUGR).
Being born SGA is associated with long-term unfavorable outcomes such as learning difficulties, behavior problems, and development of metabolic syndrome.
The recognition of intrauterine malnutrition and the monitoring of early postnatal growth are of utmost importance for optimum survival and long-term outcomes of SGA infants.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Intrauterine Growth Restriction
- Postnatal Growth Deficit
- IUGR Fetuses
- Fetal Heart Rate Tracing
- Middle Cerebral Artery Doppler
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Salient Points
-
Normal fetal growth can be altered by several pathological processes, including inadequate placental exchanges determining intrauterine growth restriction (IUGR).
-
IUGR leads to fetal hypoxia, acidemia, multi-organ damage and death that can only be prevented by elective delivery.
-
At birth, weight, length and head circumference are indicators of the quality and quantity of intrauterine growth.
-
Small for gestational age (SGA) newborns, both preterm and term, have an increased perinatal mortality risk and a number of unfavorable short and long term consequences.
-
The recognition of any growth abnormalities and the monitoring of early postnatal growth are of utmost importance for optimum survival and long-term outcomes of SGA infants.
2 Normal and Abnormal Fetal Growth
Normal fetal growth is a complex process depending on cellular hyperplasia, prevailing during the first half of pregnancy, and cellular hypertrophy, being prevalent in the second half of pregnancy. Defects in fetal growth can therefore schematically be attributed to events that inhibit cellular mitosis (such as chromosomal or genetic diseases, infections or ischemia) or to events that restrict cellular metabolism (such as inadequate placental exchanges, maternal hypoxia due to respiratory, cardiac or hematologic diseases, maternal under-nutrition). The impossibility to reach the fetal genetic growth potential because of a pathologic event is defined intrauterine growth restriction (IUGR). In case of IUGR the limitation to maternal-fetal gas and metabolic exchanges progressively leads to fetal hypoxia and, when compensating mechanisms fail, to fetal acidemia, multi-organ damage and death. Such a cascade of events can only be interrupted by elective delivery of the fetus.
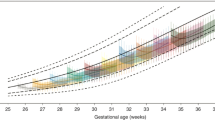
Based on the distribution of fetal and neonatal anthropometric parameters at each gestational age (GA) in the general population, every fetus and newborn can be defined as small for gestational age (SGA) if its biometric measures result below a pre-established threshold, large for gestational age (LGA) when they result above an upper threshold, or appropriate for gestational age (AGA) if they lay between these pre-defined limits of normality. However, a fetus that is SGA is not necessarily affected by IUGR, as it can be healthy but genetically determined to be smaller than the majority of the general population (constitutional SGA). On the contrary, an AGA fetus can actually be suffering from IUGR if its growth has slowed so that its biometry has shifted from a higher to a significantly lower percentile during gestation, but it has not fallen below the threshold of normality (Bardien et al. 2016) (Fig. 1).
Different patterns of fetal growth: (a) SGA fetus with IUGR: fetal abdominal circumference progressively shifts from the mean for GA to 2 standard deviations below the mean for GA, (b) SGA fetus without IUGR: fetal abdominal circumference is 2 standard deviations below the mean for GA, but it continues growing on the same trajectory throughout gestation; (c) AGA fetus with IUGR: fetal abdominal circumference progressively shifting from 2 standard deviations above the mean for GA to a lower percentile, without falling below the lower threshold of normality; (d) AGA fetus without IUGR: fetal abdominal circumference is between the limits of normality for GA and it continues growing on the same trajectory throughout gestation
IUGR is associated with a significant burden of perinatal mortality and neonatal morbidity (Garite et al. 2004; Aucott et al. 2004; Morsing et al. 2011) and impaired neurodevelopmental outcomes (Guellec et al. 2011), as well as the increased risk of hypertension, cardiovascular disease and type 2 diabetes in the adulthood (Barker and Osmond 1986; Barker 2006; Kanaka-Gantenbein 2010) due to epigenetic mechanisms influencing adaptation to the intrauterine environment (Hanson and Gluckman 2014). It has been demonstrated that prenatal identification of SGA fetuses (as a proxy of IUGR) improves neonatal outcomes (Lindqvist and Molin 2005), thus accurate diagnosis of IUGR is a primary goal of perinatal medicine.
Assessment of fetal growth in utero is performed by comparing fetal biometry with the normal value at that specific GA in the same population. To this purpose, three conditions are required:
-
1.
Exact knowledge of GA, i.e., accurate dating of pregnancy . As the date of conception is usually unknown, the beginning of the last menstrual period (LMP) is conventionally adopted as a surrogate in clinical practice, assuming that ovulation and conception, occur 2 weeks after LMP and that pregnancy extends on average 280 days (40 weeks) from LMP (Baskett and Nagele 2000). However, many women are not able to reliably report the date of LMP and, moreover, the interval from the beginning of LMP and conception is subject to considerable biologic variation (Nakling et al. 2005). The introduction of ultrasound allowed a more accurate estimate of GA, based on the fact that the velocity of embryonic growth shows a high degree of uniformity during early pregnancy (particularly during the first trimester) (Blaas et al. 1998). Indeed, between 9 and 13 weeks’ gestation, GA can be accurately estimated by the measure of crown-rump length (CRL) which growth is rapid and has a rather small inter-individual variability. Later, biparietal diameter is typically used for dating, as CRL can no longer be measured owing to curling of the growing fetus; however, variation is greater, which results in less accurate assessment of GA. For this reason, first-trimester ultrasound estimation of GA is recommended in clinical practice (Kalish et al. 2004). However, it must be noted that pathologic processes can influence intrauterine growth even in its earliest stages, including very early forms of IUGR (Morin et al. 2005; Thorsell et al. 2008).
-
2.
Availability of an adequate fetal growth chart. The classification of the biometry of an individual fetus as normal or abnormal for GA relies on the comparison with the normal value of each biometric variable at the same GA. Several charts have been published, including different populations and using different statistical methods; the choice of the chart has consequences on the sensitivity and specificity of the diagnosis of IUGR. Growth charts can be constructed retrospectively or prospectively (in the latter case quality data is improved by strict pre-defined protocols); they can be cross-sectional (every fetus in the study population contributes with only one observation; these studies can provide references for fetal size, but not for fetal growth velocity) or longitudinal (every fetus is measured serially over time and its growth velocity is assessed); they can include only healthy individuals (therefore providing standards of how fetuses should grow), or they can comprehend the general population (therefore describing references of how fetuses actually grow in that specific setting). Recently, international standards for fetal growth were published based on a prospective, multicenter, population-based study including 4321 women in optimal health and nutritional status, with singleton pregnancy, without major obstetric complications, from eight countries (Papageorghiou et al. 2014). Such approach is based on the assumption that when adequate health and nutritional conditions are met, other genetic and environmental factors do not have significant influence on intrauterine growth. Conversely, customized growth charts are founded on the hypothesis that few genetic and environmental variables (namely ethnic group, maternal height and body mass index, fetal sex and parity) can physiologically modulate fetal growth, so that the same fetal weight at the same gestational age would represent a different percentile if the fetus is Caucasian or African, female or male etc. (De Jong et al. 2000; Kase et al. 2012; Rizzo et al. 2016). Which approach is more efficient for the diagnosis of IUGR is still debated.
-
3.
Accurate measurement of relevant fetal biometric parameters.
Ultrasonographic measurement of fetal biometry is considered the gold standard for prenatal diagnosis of IUGR. However, ultrasound accuracy is limited by several factors related to the operator’s skills, technical characteristics of the ultrasound equipment, maternal body constitution, and dynamic nature of the pathology; under this regard, if ultrasound is performed late in pregnancy it has the potential to detect the majority of cases of abnormal growth, while it is going to miss a considerable proportion if it is performed earlier, when the deviation from normal growth is still mild or has not occurred yet. In a recent multicentric cohort study, universal ultrasound screening at 28 and 36 weeks of GA detected 57% of SGA fetuses with birthweight lower than the 10th percentile (vs. 20% of a policy of selective ultrasound when clinically indicated): even such an intensive protocol of monitoring (currently not feasible on the general population because of the limitation of resources even in high-income countries) is destined to miss nearly half of all SGA (Sovio et al. 2015). Not surprisingly, a series of papers from a prospective screening study in a single centre, found that ultrasonographic biometry, combined with maternal characteristics and medical history, can identify 44% of all SGA with birthweight lower than the 5th percentile born at term if it is performed at 19–24 weeks of GA, versus 58% if it is performed at 30–34 weeks of GA and 70% if it is performed at 35–37 weeks of GA (Lesmes et al. 2015; Bakalis et al. 2015; Fadigas et al. 2015). Of course, a program of screening by ultrasound late in pregnancy would miss the earliest and most severe cases.
3 Diagnosis of IUGR
As discussed above, every fetus can be defined as SGA if its biometric variables (usually abdominal circumference or estimated fetal weight) result below a pre-established lowest cut-off (e.g., 10th, 5th or 3rd percentile or 2 standard deviation below the mean for GA), LGA when they result above a highest cut-off (e.g., 90th, 95th, or 97th percentile or 2 standard deviation above the mean for GA), or AGA if they lay between the pre-defined limits of normality. However, such operation can only provide a cross-sectional measure of the size of the fetus: not all newborns falling below the cut-off are abnormally small because of growth restriction, as a proportion of them are representing the normal spectrum of fetal growth.
As growth is a dynamic process, the evaluation of fetal growth can only be obtained by a longitudinal sequence of biometric measurements during time. Accordingly, when fetal biometry shifts from a percentile to a significantly lower one, IUGR can be diagnosed, while the opposite passage, to a significantly higher percentile, allow the diagnosis of fetal growth acceleration.
However, ultrasound and Doppler velocimetry can provide several other clues to help differentiate a healthy, constitutional SGA fetus from one that is SGA because of IUGR, even when longitudinal assessment is not available:
-
(a)
Research for anatomical anomalies. A careful assessment of fetal anatomy can identify signs of congenital malformations, chromosomal or genetic diseases and intrauterine infections. This is particularly important when an SGA biometry is detected during the first half of pregnancy, a time when placental inadequacy to supply for fetal requirements is unlikely, and therefore the etiology of the growth defect has to be searched elsewhere. When anatomical anomalies are suspected, moreover, amniocentesis is indicated, for karyotyping, research for specific genetic mutations, or infectivologic analyses.
-
(b)
Uterine artery Doppler velocimetry. Doppler velocimetry tracings obtained from the uterine arteries reflect impedance to blood flow in the spiral arteries. These vessels are modified by trophoblastic invasion, producing vasodilatation, during the first half of pregnancy. Low resistance to flow and high diastolic velocities in the uterine arteries indicate normal trophoblastic invasion, while high resistance to flow and low diastolic velocities indicate shallow dilatation of the spiral arteries because of impaired placental invasion (Fig. 2). Therefore the finding of abnormally high resistance in the uterine arteries is strongly suggestive for a placental etiology (Olofsson et al. 1993; Lyall et al. 2013; Figueras and Gratacos 2014) and is associated with cesarean section for fetal distress, neonatal acidosis and neonatal hospitalization (Cruz-Martinez et al. 2015).
-
(c)
Umbilical artery Doppler velocimetry. Umbilical artery Doppler velocimetry reflects impedance to blood flow in the fetal side of placental circulation, i.e., in the villous tree. Abnormally high resistance in the umbilical arteries velocimetry are indicative of substantial placental pathology (McCowan et al. 1987; Todros et al. 1999). Indeed, elevated indices of resistance up to absent or reversed end-diastolic flow (ARED) in such vessels, correlate with worsening degrees of fetal hypoxia and acidosis and increased risk of perinatal mortality (Karsdorp et al. 1994; Nicolaides et al. 1988; Tyrrell et al. 1989) (Fig. 3). Hence the finding of elevated impedance in the umbilical arteries in an SGA fetus, is both diagnostic of IUGR of placental origin and prognostic, as its progression is indicative of worsening hypoxia, risk of fetal damage and intrauterine death and need for elective delivery.
-
(d)
Middle cerebral artery Doppler velocimetry . Vasodilatation in the cerebral circulation (most easily assessed in the middle cerebral artery – Fig. 4) is a sign of fetal hemodynamic adaptation to chronic hypoxia, which is thought to secure oxygenation to the brain, to the expense of other organs (brain sparing). Decreased impedance in the middle cerebral artery is particularly useful for the identification of late-onset IUGR, a subgroup of fetuses in which umbilical artery flow can be only mildly altered or even normal, but are still at risk of fetal distress during labor and suboptimal neurobehavioral outcomes (Oros et al. 2011; Eixarch et al. 2008).
-
(e)
Estimated fetal weight . Even when umbilical and middle cerebral artery Doppler assessment is normal, a very low estimated fetal weight (calculated by means of different algorithms on the basis of ultrasonographic biometry) is strongly predictive of adverse perinatal outcomes among SGA fetuses, and is therefore suggestive of IUGR (Savchev et al. 2012).
-
(f)
Pattern of growth. Since the introduction of fetal ultrasonographic biometry, obstetricians classify SGA fetuses as symmetrical (proportionately small head circumference, abdominal circumference ad femur length) and asymmetrical (substantial reduction in abdominal circumference with relatively preserved head circumference and femur length) with the believing that IUGR fetuses tend to adopt an asymmetric pattern of growth as a consequence of brain sparing, while constitutional SGA and fetuses with aneuploidies, congenital infections and malformations are preferentially symmetrical (Campbell and Thoms 1977). In contrast with this assumption, it has been shown that all SGA fetuses show some degree of asymmetry although such pattern is more common among IUGR (Todros et al. 1996; David et al. 1995). However, newborns with low weight and preserved length (also referred to as wasting), corresponding to asymmetrical SGA fetuses, show a stronger association with poor neonatal outcomes including admission to neonatal intensive care unit, respiratory distress syndrome, transient tachypnea and difficulty in oral feeding, compared to newborns with low weight and short length (also referred as stunting), corresponding to symmetrical SGA fetuses (Victora 2015). Therefore asymmetrical SGA fetuses should be considered at high risk of intrauterine damage.
4 Monitoring, Timing and Mode of Delivery
Clinical management of IUGR is critically dependent on gestational age at its onset. Early onset IUGR is more easily diagnosed because it tends to rapidly touch extreme degrees of alterations in terms of fetal biometry and oxygenation and because of its frequent association with maternal hypertensive diseases. However, the only available therapeutic intervention, i.e., interruption of pregnancy, is a serious clinical dilemma because it exposes the fetus to the risks of severe preterm birth. On the other hand, late onset IUGR, which is much more frequent, is more easily missed by antenatal care, because deviation from normal fetal growth and hemodynamic function are more subtle, while, in this case, the risks of anticipating delivery appear to be a safer option; however, in light of the growing evidence on the perinatal risks of late preterm birth, solid criteria to choose the timing of delivery are lacking.
Early onset IUGR. Early-onset IUGR (occurring before 34 weeks of gestation) is associated with a risk of perinatal mortality as high as 41%, depending on definition, study population and GA (Mari et al. 2007). Neonatal short- and long-term prognosis is mainly determined by three variables: fetal cardiovascular status, birthweight, and GA at birth (Baschat et al. 2007, 2009; Torrance et al. 2010).
The fetal cardiovascular status, as indicated by Doppler velocimetry of arterial and venous vessels and by fetal heart rate tracing, is strictly related to the fetal acid–base status: hence serial testing with Doppler ultrasound and fetal heart rate tracings allows to follow the transition from fetal normal oxygenation to hypoxemia, hypoxia and acidemia, which in turn appears to be the nearest fetal antecedent of perinatal mortality and infant neurodevelopmental delay (Soothill et al. 1992).
Birthweight is the expression of both GA at birth and the severity of fetal malnutrition and correlates with major neonatal morbidity (Baschat et al. 2007) and abnormal neurodevelopment in infancy and childhood independently of Doppler parameters (Baschat et al. 2009; Torrance et al. 2010).
Prematurity (as a result of iatrogenic preterm delivery of fetuses considered to be at high risk of intrauterine acidemia and demise) is also an independent predictor of neonatal mortality and severe neonatal complications associated with abnormal neurodevelopmental outcomes in IUGR fetuses (Baschat et al. 2007, 2009; Torrance et al. 2010; Soothill et al. 1992; Lees et al. 2013). A multicenter cohort trial conducted between 2000 and 2006 in 12 centers of perinatal medicine in USA and Europe, reports neonatal outcomes of 604 singleton liveborn with IUGR delivered between 24 and 32 weeks + 6 days. Mortality within 28 days of life was 20% while incidence of severe morbidity was 36%; however, the rate of neonatal death decreased by 2% per each day of pregnancy prolongation between 24 and 27 weeks of GA. In contrast, after this threshold Doppler velocimetry of the venous circulation and arterial pH were the only independent variables predictive of neonatal mortality, while GA at delivery was not a determinant of neonatal survival. Similarly, GA was the main predictor of severe neonatal morbidity until 29 weeks, but it was replaced by venous Doppler between 29 and 33 weeks (Baschat et al. 2007).
More favorable data on neonatal mortality and morbidity are reported by the Trial of Umbilical and Fetal Flow in Europe (TRUFFLE). This is a randomized clinical trial conducted between 2005 and 2010 in 20 European centers, in which 503 fetuses with early-onset IUGR (diagnosed between 26 weeks and 31 weeks + 6 days of GA) were randomly allocated to be delivered according to one of three criteria: (1) fetal heart rate criteria (namely reduced short term variation); (2) early abnormalities in the Doppler velocimetry of the ductus venosus (reduced velocities during atrial contraction); (3) late abnormalities in the ductus venosus (absent or reversed velocities during atrial contraction) (Fig. 5). When the short-term outcomes of the whole cohort, regardless of the arm of randomization, were analyzed, neonatal mortality before discharge from hospital was 5.5% of all live born, and severe morbidity was 24%. Besides GA and birthweight, the major determinant of poor outcome was the occurrence of maternal hypertensive disease, which shortened the interval between diagnosis of IUGR and delivery (Lees et al. 2013).
Doppler velocimetry tracing of the ductus venosus in the third trimester of pregnancy with: (a) normal positive velocities during atrial contraction; (b) reduced velocities during atrial contraction; (c) reversed velocities during atrial contraction. Arrows indicate velocities during atrial contraction
In summary, the aim of clinical management of early-onset IUGR fetuses is focused on optimizing the timing of delivery in order to balance the risks of prolonged intrauterine hypoxia versus the complications associated with preterm birth. Unfortunately, there is no single test indicating the break point, in spite many tests reflecting fetal conditions and their deterioration have been developed in the last decades: fetal arterial and venous Doppler velocimetry, fetal heart rate tracing with computerized analysis of short term variability, ultrasound for assessment of fetal growth and amniotic fluid. The results of the TRUFFLE study recently demonstrated that the best neurodevelopmental outcome at 2 years in surviving fetuses is obtained when timing of delivery is based on the integration of results of ductus venosus Doppler and fetal heart rate (Lees et al. 2015).
Late onset IUGR. Late-onset IUGR is not a minor clinical issue, because most infants with intrauterine growth restriction are born at term (Clausson et al. 1998). Even when diagnosed late in gestation, IUGR is associated with increased risk of perinatal mortality and morbidity, such as fetal distress, hypoglycemia, seizures, behavioral problems, cerebral palsy, and cardiovascular disease (Jarvis et al. 2003; Pulver et al. 2009; Boulet et al. 2006; Dijxhoorn et al. 1987). Moreover growing evidence suggests that growth failure occurring around term is associated with a poorer mental and psychomotor development (Skuse et al. 1994). Early delivery by induction of labor might prevent the detrimental effects of inadequate nutrition and oxygenation, and indeed it is the common clinical practice; however, the excess of mortality and morbidity associated with late preterm (between 34 an 36 weeks) and early term (between 37 and 38 weeks) birth is increasingly recognized (Shapiro-Mendoza et al. 2008; Hansen et al. 2008; Engle 2011).
A multicenter randomized clinical trial (the Disproportionate Intrauterine Growth Intervention Trial At Term, DIGITAT) compared the effect of induction of labor and expectant management on a population of 650 women with prenatal diagnosis of IUGR after 36 weeks of GA and did not find any significant difference in terms of adverse neonatal outcomes (Boers et al. 2010, 2012), caesarean sections (Boers et al. 2010), and developmental and behavioral outcomes at two years of age (van Wyk et al. 2012). However, expectant management was associated with a higher chance of being born with severe IUGR, which is a major predicting factor for neurodevelopmental disturbances. On the other hand, early induction was associated with a higher rate of neonatal admission to intermediate care, but such excess of neonatal admissions seemed to be related to protocols of clinical management for late prematurity and not to specific neonatal complications (Boers et al. 2012). Evidence is still lacking regarding the best monitoring tool to identify those fetuses that would benefit from early induction of labor (Tajik et al. 2014). Therefore, in case of IUGR after 36 weeks of GA, it appears more reasonable to choose induction of labor in order to prevent fetal mortality and neonatal morbidity and in order to save the resources needed for intensive fetal monitoring.
Intermediate onset IUGR . The time interval between 34 and 36 weeks of GA is the source of the greatest uncertainty in the clinical management of pregnancies complicated by IUGR, as evidence is lacking about risks of chronic intrauterine hypoxia and preterm birth and the most efficient tools for identifying fetuses at highest risk of intrauterine compromise. As umbilical artery Doppler is frequently normal in this population, the middle cerebral artery velocimetry could be the best marker for impending fetal hypoxia and could be used for timing delivery. At the moment there is a need for clinical research on the subject.
5 Auxological Evaluation of the Newborn
Weight, length, and head circumference at birth are indicators of the quality and quantity of growth. These variables must be evaluated using standardized instruments and following the techniques required for accurate measurements as described by Cameron (2004).
In order to identify intrauterine malnutrition, some anthropometric indexes have been proposed. They compare variables, such as body length and head circumference, which are less influenced in cases of malnutrition, to those variables which are more compromised such as body weight.
The most well known is the Rörher ponderal index [PI = body weight (grams) × 100/length (centimeters)3] whose normal value in a full-term newborn lies between 2.2 and 3 (3rd and 97th percentile) (Miller 1985). This neonatal body proportionality index corresponds to the Body Mass Index (BMI) used in children and adults [BMI= body weight (kg)/length (m)2], and it is an indirect measure of soft tissue and inferentially of fat accumulation.
At birth, recognition of any growth abnormalities or intrauterine malnutrition is of utmost importance for prognostic purposes and in clinical practice. The so-called neonatal anthropometric charts or curves are used whereby graphs represent, at various gestational ages, either the percentile values or the mean and standard deviation of anthropometric variables considered which are computed on a reference population. A recent commentary defines the characteristics that a reliable anthropometric chart should possess to be of both epidemiological and clinical use (Table 1) (Bertino et al. 2007).
The neonatal anthropometric charts enable the classification of newborns at different gestational ages based on weight as follows:
-
SGA – Small for Gestational Age: weight below the 10th centile for GA
-
AGA – Appropriate for Gestational Age: weight between 10th and 90th centile for GA
-
LGA – Large for Gestational Age: weight above 90th centile for GA
Some authors set down a cut-off of the 3rd and 97th centile among AGA, SGA, LGA newborns or equivalent limits of mean ± 2 SD (Clayton et al. 2007).
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (The American Academy of Pediatrics and the American College of Obstetricians and Gynecologist 2007) recognize three groups of GA and define neonates as follows:
-
Preterm: born before 37 completed weeks (less than 259 days)
-
Full term: born between 37 and 41 weeks + 6 days (from 259 to 293 days)
-
Postterm: born 42 weeks of GA (294 or more days)
As a consequence, nine different classes of newborns can be defined.
The definition of small, appropriate, and large newborn for GA is based on weight. However, similar classes may be defined considering body length and head circumference, so that at every GA, newborns can be defined as having small, appropriate, and large body length or head circumference.
Consideration of weight, body length, and head circumference traditionally allows identification, among the heterogeneous group of SGA newborns, those infants who are symmetrical (or proportionate) or asymmetrical (or disproportionate) (Brar and Rutherford 1988).
Symmetrical SGA newborns have reduced weight, body length, and head circumference. The insult leading to reduced growth occurs early in pregnancy, during the phase of growth primarily characterized by cellular hyperplasia, with consequent reduction in cell number (hypoplasia) that may limit the subsequent catch-up of organ and tissue growth (Vrachnis et al. 2006; Singer et al. 1991).
Asymmetrical SGA newborns have reduced weight, with normal or less reduced body length and head circumference. The insult, leading to reduced growth occurs later, interfering with the delivery of oxygen and nutrition during the phase of prevalent cellular hypertrophy, resulting in reduced cell size (hypotrophy), with the possibility of subsequent catch-up growth (Vrachnis et al. 2006; Singer et al. 1991). The weight deficit is principally due to a reduction in fat deposition, particularly during the third trimester of pregnancy. The disproportion is due to the redistribution of the blood flow, which occurs in these cases in the fetus, with preferential perfusion of the brain, heart, and adrenal glands to the detriment of other organs, such as the liver, spleen, kidneys, thymus, and adipose tissue, whose growth is more compromised not only as regards the brain but also body length (Barker and Hanson 2004). In the case of late noxa, the biggest reduction in fetal weight growth compared to body length may also be explained by the different dynamics of their intrauterine growth: the velocity peak of length growth, about the 20th week, occurs earlier than the peak of weight growth (Tanner 1989; Bertino et al. 1996). At six months of pregnancy the fetus reaches 70% of its full-term length but only 25% of its weight.
These newborns, once defined “dysmature,” often seem to have clinical signs of intrauterine malnutrition, an “old man” appearance, wrinkled and hypoelastic skin, easily liftable and pliable skinfolds, poorly represented subcutaneous tissue, hypotrophic muscular mass, and thin umbilical cord. When meconium is passed in utero, there is a yellow-green staining of fingernails, skin, and umbilical cord (Fig. 6). Thanks to better prenatal diagnosis and management of fetal growth restriction, the newborns with all these features are uncommon nowadays. The main differences between symmetrical and asymmetrical SGA newborns are presented in Table 2.
Some studies have reassessed the distinction between proportionate and disproportionate SGA newborns. It has been suggested that these two classes represent a continuum rather than distinct classes (Todros et al. 1996; Kramer et al. 1989) and that both disproportionate and proportionate fetal growth restriction may start early in pregnancy (17–19 weeks of gestation) (Rasmussen et al. 2006). These observations lead to a partial reconsideration of causes, timing, and risk of symmetric or asymmetric IUGR. Of course recognizing specific underlying causes of reduced fetal growth may be more important than evaluating body proportionality at birth in predicting short- and long-term outcomes of SGA children.
In contrast with the usual assessment based solely on weight, a recent paper suggests to classify newborns as proportionately or disproportionately developed and infants as stunted (short length for age, reflecting linear growth restriction) or wasted (low weight for length, or low BMI for age, often reflecting recent weight loss). Although newborn stunting and wasting share some common determinants, they are distinct phenotypes with their own risk factors and neonatal prognoses. This distinction could help to prioritize preventive interventions and focus the management of fetal undernutrition (Victora 2015).
Growth of the fetus relative to the placenta also seems to be important. Babies born small but with a relatively large placenta are less likely to show catch-up growth in the 18 months after birth and have an increased risk of hypertension in adult life (Casey 2008).
6 Neonatal Outcome
6.1 Mortality
Small for gestational age newborns, both preterm and term, have an increased perinatal mortality risk (Pallotto and Kilbride 2006; Vashevnik et al. 2007). A recent paper has demonstrated that the increased risk of neonatal and infant mortality observed in late preterm (34–36 weeks) and early term (37–38 weeks) SGA infants persists even when infants dying of congenital anomalies are excluded. In addition to congenital conditions, birth asphyxia and infections have a relevant role in neonatal mortality whereas sudden infant death syndrome contributes to infant mortality (Pulver et al. 2009). Some other data have indicated that birth weight is the predominant factor independently affecting neonatal mortality as well as risk for low Apgar score and neonatal sepsis during NICU stay (Mamopoulos et al. 2015).
A higher mortality rate is reported in SGA preterm infants with abnormal (absent or reversed end-diastolic flow) umbilical artery Doppler velocimetry (Shand et al. 2009).
6.2 Asphyxia
Transient diminished placental blood flow during labor is poorly tolerated by growth-restricted fetuses. Intrauterine chronic hypoxia and limited carbohydrate reserves as a consequence of placental insufficiency predispose to perinatal asphyxia SGA neonates more than AGA newborns. As a result, there is also an increased risk of all clinical sequelae of perinatal asphyxia (Rosenberg 2008).
6.3 Infections
Recent studies suggest possible interactions between immunological function and nutritional status. Thymic atrophy and prolonged impairment of cell immunity have been found in SGA infants and animal models of intrauterine growth retardation. These subjects also have a more pronounced hypogammaglobulinemia compared with AGA infants (Bartels et al. 2007). Neutropenia occurs frequently in infants born to mothers with preeclampsia (Snijders et al. 1993). In a recent paper, lower counts of leukocytes, total neutrophils, immature neutrophils, lymphocytes, and monocytes were detected in SGA infants not related to maternal preeclampsia (median birthweight 583 g) suggesting that IUGR may act as an independent factor for lower counts of different leukocytes in very immature preterm infants (Wirbelauer et al. 2010). All these aspects result in an increased risk of neonatal infections.
6.4 Coagulation Disorders
The hepatic dysfunction that results from chronic intrauterine hypoxia may lead to a reduction in vitamin-K dependent factors and thrombocytopenia. Such disorders are usually transient and easily corrected. Only occasionally severe bleeding, such as pulmonary hemorrhage, has been reported (Halliday 2009). In a recent study, prolonged PT and INR were observed in full-term healthy SGA neonates, indicating a predisposition to hemorrhagic events. However, the newborns included in the study did not appear to have any clinical symptoms of altered hemostasis (Mitsiakos et al. 2009).
6.5 Thermoregulation
SGA infants are at increased risk of hypothermia as a consequence of their higher brain weight and body surface area in relation to weight as well as to their lower subcutaneous adipose tissue stores, including depleted brown fat reserves (Yu and Upadhyay 2004).
6.6 Hypoglycemia
Reduced hepatic and skeleton muscle glycogen stores (the predominant source of glucose in the first hours after birth) and impaired glycogenolysis and gluconeogenesis are the main causes of hypoglycemia in IUGR infants. In addition, growth-restricted infants have limited fat stores and do not effectively oxidize free fatty acids and triglycerides (Sabel et al. 1982). The risk of hypoglycemia is greater during the first few days of life when the newborn must adapt to extrauterine life without the placental source of nutrients, but in some cases it may persist for weeks (Halliday 2009; Pallotto et al. 2004; Rozance 2014).
6.7 Polycytemia
Chronic fetal hypoxia results in increased erythropoietin production and release by the fetal kidney, with consequent excessive blood red cells production. Besides, a shift of blood from the placental compartment to the fetus during labour or a period of fetal asphyxia constitutes important causes of polycythemia in IUGR fetuses (Sarkar and Rosenkrantz 2008). Polycythemia contributes to the increased risk of pathologies such as hypoglycemia, hyperbilirubinemia, and NEC.
7 Respiratory Distress Syndrome (RDS) and Bronchopulmonary Dysplasia (BPD)
The common opinion that the intrauterine stress associated with IUGR enhances lung maturation has been challenged in some papers reporting that the incidence of RDS is inversely correlated with birth weight and gestational age (McIntire et al. 1999) and that growth-restricted infants may have the same (Piper et al. 1996) or a higher (McIntire et al. 1999; Bernstein et al. 2000; Peacock et al. 2013) incidence of RDS than AGA newborns of the same gestational age.
A higher BPD incidence has also been reported in IUGR preterm infants (Aucott et al. 2004; Gortner et al. 1999; Lal et al. 2003; Regev et al. 2003; Sharma et al. 2004; Soudée et al. 2014). BPD has a multifactorial etiology, and there are several hypotheses about its physiopathology in SGA including abnormal intrauterine lung development (Lal et al. 2003), oxidative injury in utero, more severe early lung disease with subsequent ventilator-induced lung injury, and fetal or neonatal systemic inflammatory response due to chronic hypoxia (Soudée et al. 2014; Kinsella et al. 2006).
7.1 Retinopathy of Prematurity (ROP)
It has been reported that SGA infants have an increased risk of developing ROP (Dhaliwal et al. 2009; Lundgren et al. 2014).
Changes in organ development due to fetal hypoxemia, nutrient restriction, and alterated endocrine environment can all contribute to the pathogenesis (McMillen et al. 2001). SGA infants are often sicker than their AGA peers, requiring more intensive and prolonged hospital care (Yu and Upadhyay 2004). They are therefore more likely to require supplementary oxygen, which is a well-documented risk factor for ROP. A lower serum concentration of insulin-like growth factor 1, documented in SGA infants, may as well play a role (Smith 2005).
7.2 Necrotizing Enterocolitis (NEC)
Infants who are growth-restricted in utero are considered as having a higher risk of developing NEC, especially if there has been antenatal detection of absent or reversed end-diastolic flow velocities in Doppler studies of fetal aorta or umbilical artery (Dorling et al. 2005; Ree et al. 2014). The underlying mechanism is unclear, but increasing thoracic aorta and umbilical artery resistance may be associated with alterations in blood flow in the viscera, particularly in the intestine and in the liver. Abnormalities of bowel blood flow persist postnatally, with some recovery during the first week of life, providing justification for a delayed and careful introduction of enteral feeding (Dorling et al. 2005). Early postnatal evaluation of superior mesenteric artery blood flow may also be used to identify infants at increased risk of developing NEC (Murdoch et al. 2006; Bora et al. 2009; Bozzetti et al. 2013).
It is common practice in neonatal intensive care units to delay enteral feeding administration for these infants. Recent trials, however, have shown that early enteral feeding in IUGR infants is safe and that human milk exerts a protective role against NEC.
8 Long-Term Outcome
8.1 Postnatal Growth Impairment
Most term children born SGA experience catch-up growth and achieve a normal adult height, above −2 SD. Approximately 10% of them remain shorter than peers born AGA (Clayton et al. 2007; Simon et al. 2008). Catch-up growth is typically an early postnatal process. Term SGA infants usually experience a period of accelerated linear growth during the first 12 months of life (Saenger et al. 2007) and in most cases catch-up growth is complete by two years of age (Clayton et al. 2007; Saenger et al. 2007). It is has been suggested that SGA children aged 2–4 years with no evidence of catch-up growth and heights less than −2.5 SD should be referred for endocrinological evaluation and could be eligible for GH treatment (Clayton et al. 2007). The preterm SGA infants can take 4 or more years to achieve heights in a normal range (Gibson et al. 2000).
The majority of preterm infants show a postnatal growth deficit at the time of hospital discharge, the so-called Extra Uterine Growth Restriction (EUGR). There is no consensus among neonatologists regarding the best way to define EUGR. At present, a definition based on the negative change of SDS from birth to term corrected age is probably the most appropriate because age at discharge could be biased by different discharge policies over time and between centers. The EUGR is largely due to inadequate postnatal nutrient intake as well as postnatal morbidities, and it increases with the decrease of gestational age at birth (Wit et al. 2006; Bertino et al. 2009). Studies demonstrate that premature infants with EUGR also have metabolic abnormalities similar to those observed in term SGA children and these occur irrespectively of whether they are SGA or AGA at birth (Hofman et al. 2006). Approximately 10% of very preterm children have heights below −2 SD at 4–5 years of age. This percentage is similar to that of term SGA infants who do not show postnatal catch-up growth (Wit et al. 2006) (Fig. 7). SGA term infants suffer from an adverse fetal environment during the last trimester of pregnancy, whereas very preterm infants suffer from an adverse postnatal environment during the first three months, a time biologically equivalent to the third trimester of fetal life. Considering these similarities, an expert group has recently suggested that the indication of GH therapy should be expanded to preterm children with EUGR who failed to normalize over time (Wit et al. 2006). Several common comorbidities of prematurity are significantly associated with postnatal growth restriction including medical or surgical NEC, gastrointestinal perforation, and severe retinopathy of prematurity. These results should help clinicians to identify those infants at highest risk of adverse growth outcomes and work to further improve these outcomes (Griffin et al. 2015).
8.2 Neurological Outcome
There is an increasing evidence that being born SGA is independently associated with mild to moderate learning difficulties in childhood and adolescence, lower psychological and intellectual performance in young adulthood, low social competence and behavior problems when compared with AGA infants of the same gestational age (Lundgren and Tuvemo 2008; Walker and Marlow 2008; Levine et al. 2015).
A recent review suggests the association between cerebral redistribution based on middle cerebral artery Doppler indices and poorer neurodevelopmental outcome supporting the growing evidence that there is a need to reevaluate whether cerebral redistribution should be used as a criterion for delivering late preterm and term SGA or growth restricted babies, even in the absence of abnormal Umbilical artery Doppler (Meher et al. 2015). The most important predictor of subnormal performance is the absence of catch-up growth in height and/or head circumference (Clayton et al. 2007; Rosenberg 2008). SGA children who developed catch-up growth were shown to have completed successfully higher school grades and to get higher mean intelligence quotiens scores compared to those who fail to develop catch-up growth or to those with steady growth or to children with early catch-down (Varella and Moss 2015).
Long-term exclusive breastfeeding could help to prevent some of the neurological sequelae of being born SGA. Overfeeding with enriched formula could accelerate growth, but it does not seem to be an advantage for the intellectual development and could be a drawback in terms of metabolic and cardiovascular risks (Morley et al. 2004; Agostoni 2005). It has been suggested that GH treatment may improve IQ in short SGA children, but additional data are required (Clayton et al. 2007; Lundgren and Tuvemo 2008).
The association between cerebral palsy and IUGR which has been observed in both term and preterm infants may be due to placental insufficiency: reduced oxygen or nutrient delivery to the fetus may have adverse effects on brain development and differentiation (Halliday 2009; Lundgren and Tuvemo 2008).
8.3 Metabolic Risk
Since the late 1980s, epidemiological studies have shown that impaired intrauterine growth is associated with later development of the metabolic syndrome or one of its components (insulin resistance, hyperinsulinemia, impaired glucose tolerance or diabetes mellitus type 2, dyslipidemia, arterial hypertension, and obesity). Additionally, some other morbidities have been connected with the syndrome, such as hypercoagulability, nonalcoholic fatty liver disease, renal dysfunction (micro- or macroalbuminuria), polycystic ovary syndrome, endothelial dysfunction, and atherosclerosis leading to increased cardiovascular morbidity and mortality (Varda and Gregoric 2009).
A number of mechanisms for the development of metabolic syndrome have been proposed. One hypothesis is that the fetus adapts to an adverse intrauterine environment “reprogramming” the endocrine-metabolic status, with short-term survival benefits. This process consists mainly of insulin resistance and of reduced insulin secretion due to impaired development of beta cells. As a result, blood glucose concentration can be maintained for the benefit of brain development at the expense of less glucose transported to peripheral tissue (e.g., muscle and fat) (Barker et al. 2005). This reprogramming is adequate to maintaining gluco-homeostasis in the short term, when intrauterine nutrient supply is deficient, but it predisposes the child to metabolic syndrome in later life, when nutrient supplies are adequate (Halliday 2009; Saenger et al. 2007). Moreover, SGA newborns show postnatal accelerated growth with rapid weight gain, associated with later obesity, which is per se associated with the metabolic syndrome (Maiorana et al. 2007; Nobili et al. 2008). Overweight former SGA children have an increased risk of metabolic syndrome compared with overweight former AGA children (Reinehr et al. 2009). On the other hand, it is known that poor postnatal growth is associated with later poor neurocognitive outcome (Yeung 2006).
The challenge of neonatal nutrition is the achievement of a “healthy catch-up growth” of IUGR subjects, based on a nutritional strategy that improves neurodevelopmental outcome while minimizing long-term metabolic and cardiovascular adverse effects (Nobili et al. 2008).
8.4 Chronic Kidney Disease
As previously described, when resources in utero are restricted their allocation to the development of the kidney is restricted to guarantee appropriate development of the brain and heart (Barker and Hanson 2004). The result is a diminished number of nephrons which predisposes these subjects to albuminuria and to the risk of developing chronic kidney disease, as well as of hypertension. In parallel, metabolic syndrome and type 2 diabetes may contribute to renal complications (Koleganova et al. 2009).
8.5 Puberty and Reproductive Function
In girls born SGA most studies have shown an increased risk of earlier pubertal development or normal timing, but with rapid progression (Hernández and Mericq 2008). These aberrations may result in reduced adult stature. Today there are insufficient data to define the risk of ovarian dysfunction, reduced fertility, or early menopause in females born SGA. On the contrary, most boys born SGA have normal pubertal timing, but often heights below the target (Hernández and Mericq 2008) Information about the influence of fetal growth on gonadal function is scarce, but most studies have shown that low birth weight is a common risk factor for testicular cancer, hypospadia, and cryptorchidism (Main et al. 2006).
Abbreviations
- AGA:
-
Appropriate for gestational age
- BMI:
-
Body mass index
- BPD:
-
Broncopulmonary displasia
- EUGR:
-
Extra uterine growth restriction
- GA:
-
Gestational age
- GH:
-
Growth hormone
- INR:
-
International mormalized ratio
- IUGR:
-
Intrauterine growth restriction
- LGA:
-
Large for gestational age
- NEC:
-
Necrotizing enterocolitis
- PI:
-
Ponderal index
- PT:
-
Protrombin time
- RDS:
-
Respiratory distress syndrome
- ROP:
-
Retinopathy of prematurity
- SD:
-
Standard deviation
- SGA:
-
Small for gestational age
References
Agostoni C (2005) Small-for-gestational-age infants need dietary quality more than quantity for their development: the role of human milk. Acta Paediatr 94:827–829
Aucott SW, Donohue PK, Northington FJ (2004) Increased morbidity in severe early intrauterine growth restriction. J Perinatol 24:435–440
Bakalis S, Silva M, Akolekar R, Poon LC, Nicolaides KH (2015) Prediction of small-for-gestational-age neonates: screening by fetal biometry at 30–34 weeks. Ultrasound Obstet Gynecol 45:551–558
Bardien N, Whitehead CL, Tong S, Ugoni A, McDonald S, Walker SP (2016) Placental insufficiency in fetuses that slow in growth but are born appropriate for gestational age: a prospective longitudinal study. PLoS One 11:e0142788
Barker DJP (2006) Adult consequences of fetal growth restriction. Clin Obstet Gynecol 49:270–283
Barker DJ, Hanson MA (2004) Altered regional blood flow in the fetus: the origins of cardiovascular disease? Acta Paediatr 93:1559–1560
Barker DJ, Osmond C (1986) Infant mortality, childhood nutrition, and ischaemic heart disease in England and Wales. Lancet 1:1077–1081
Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG (2005) Trajectories of growth among children who have coronary events as adults. N Engl J Med 353:1802–1809
Bartels DB, Schwab F, Geffers C, Poets CF, Gastmeier P (2007) Nosocomial infection in small for gestational age newborns with birth weight <1500 g: a multicentre analysis. Arch Dis Child Fetal Neonatal Ed 92:F449–F453
Baschat AA, Cosmi E, Bilardo CM, Wolf H, Berg C, Rigano S, Germer U, Moyano D, Turan S, Hartung J, Bhide A, Müller T, Bower S, Nicolaides KH, Thilaganathan B, Gembruch U, Ferrazzi E, Hecher K, Galan HL, Harman CR (2007) Predictors of neonatal outcome in early-onset placental dysfunction. Obstet Gynecol 109:253–261
Baschat AA, Viscardi RM, Hussey-Gardner B, Hashmi N, Harman C (2009) Infant neurodevelopment following fetal growth restriction: relationship with antepartum surveillance parameters. Ultrasound Obstet Gynecol 33:44–50
Baskett TF, Nagele F (2000) Naegele’s rule: a reappraisal. BJOG 107:1433–1435
Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A (2000) Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol 182:198e206
Bertino E, Di Battista E, Bossi A, Pagliano M, Fabris C, Aicardi G, Milani S (1996) Fetal growth velocity: kinetic, clinical, and biological aspects. Arch Dis Child 74:F10–F15
Bertino E, Milani S, Fabris C, De Curtis M (2007) Neonatal anthropometric charts: what they are, what they are not. Arch Dis Child Fetal Neonatal Ed 92:7–10
Bertino E, Coscia A, Boni L, Rossi C, Martano C, Giuliani F, Fabris C, Spada E, Zolin A, Milani S (2009) Weight growth velocity of very low birth weight infants: role of gender, gestational age and major morbidities. Early Hum Dev 85:339–347
Blaas HG, Eik-Nes SH, Bremnes JB (1998) The growth of the human embryo. A longitudinal biometric assessment from 7 to 12 weeks of gestation. Ultrasound Obstet Gynecol 12:346–354
Boers KE, Vijgen SM, Bijlenga D, van der Post JA, Bekedam DJ, Kwee A, van der Salm PC, van Pampus MG, Spaanderman ME, de Boer K, Duvekot JJ, Bremer HA, Hasaart TH, Delemarre FM, Bloemenkamp KW, van Meir CA, Willekes C, Wijnen EJ, Rijken M, le Cessie S, Roumen FJ, Thornton JG, van Lith JM, Mol BW, Scherjon SA, DIGITAT study group (2010) Induction versus expectant monitoring for intrauterine growth restriction at term: randomized equivalence trial (DIGITAT). BMJ 341:c7087
Boers KE, van Wyk L, van der Post JA, Kwee A, van Pampus MG, Spaanderdam ME, Duvekot JJ, Bremer HA, Delemarre FM, Bloemenkamp KW, de Groot CJ, Willekes C, Rijken M, Roumen FJ, Thornton JG, van Lith JM, Mol BW, le Cessie S, Scherjon SA, DIGITAT Study Group (2012) Neonatal morbidity after induction vs expectant monitoring in intrauterine growth restriction at term: a subanalysis of the DIGITAT RCT. Am J Obstet Gynecol 206:344 e1–344 e7
Bora R, Mukhopadhyay K, Saxena AK, Jain V, Narang A (2009) Prediction of feed intolerance and necrotizing enterocolitis in neonates with absent end diastolic flow in umbilical artery and the correlation of feed intolerance with postnatal superior mesenteric artery flow. J Matern Fetal Neonatal Med 22:1092–1096
Boulet SL, Alexander GR, Salihu HM, Kirby RS, Carlo WA (2006) Fetal growth risk curves: defining levels of fetal growth restriction by neonatal death risk. Am J Obstet Gynecol 195:1571–1577
Bozzetti V, Tagliabue PE, Visser GH, van Bel F, Gazzolo D (2013) Feeding issues in IUGR preterm infants. Early Hum Dev 89(S2):S21–S23
Brar HS, Rutherford SE (1988) Classification of intrauterine growth retardation. Semin Perinatol 12:2–10
Cameron N (2004) Measuring techniques and instruments. In: Nicoletti I, Benso L, Gilli G (eds) Physiological and pathological auxology. Edizioni Centro Studi Auxologici, Firenze, pp 117–159
Campbell S, Thoms A (1977) Ultrasound measurement of the fetal head to abdomen circumference ratio in the assessment of growth retardation. Br J Obstet Gynaecol 84:165–174
Casey PH (2008) Growth of low birth weight preterm children. Semin Perinatol 32:20–27
Clausson B, Cnattingius S, Axelsson O (1998) Preterm and term births of small for gestational age infants: a population-based study of risk factors among nulliparous women. Br J Obstet Gynaecol 105(9):1011–1017
Clayton PE, Cianfarani S, Czernichow P, Johannsson G, Rapaport R, Rogol A (2007) Management of the child born small for gestational age through to adulthood: a consensus statement of the International Societies of Pediatric ndocrinology and the Growth Hormone Research Society. J Clin Endocrinol Metab 92:804–810
Cruz-Martinez R, Savchev S, Cruz-Lemini M, Mendez A, Gratacos E, Figueras F (2015) Clinical utility of third-trimester uterine artery Doppler in the prediction of brain hemodynamic deterioration and adverse perinatal outcome in small-for-gestational-age fetuses. Ultrasound Obstet Gynecol 45:273–278
David C, Gabrielli S, Pilu G, Bovicelli L (1995) The head-to-abdomen circumference ratio: a reappraisal. Ultrasound Obstet Gynecol 5:256–259
De Jong CL, Francis A, Van Geijn HP, Gardosi J (2000) Customized fetal weight limits for antenatal detection of fetal growth restriction. Ultrasound Obstet Gynecol 15:36–40
Dhaliwal CA, Fleck BW, Wright E, Graham C, McIntosh N (2009) Retinopathy of premature in small- for gestational age infants compared with those of appropriate size for gestational age. Arch Dis Child Fetal Neonatal Ed 94:F193–F195
Dijxhoorn MJ, Visser GH, Touwen BC, Huisjes HJ (1987) Apgar score, meconium and acidaemia at birth in small-for-gestational age infants born at term, and their relation to neonatal neurological morbidity. Br J Obstet Gynaecol 94:873–879
Dorling J, Kempley S, Leaf A (2005) Feeding growth restricted preterm infants with abnormal antenatal Doppler results. Arch Dis Child Fetal Neonatal Ed 90:F359–F363
Eixarch E, Meler E, Iraola A, Illa M, Crispi F, Hernandez-Andrade E, Gratacos E, Figueras F (2008) Neurodevelopmental outcome in 2-year-old infants who were small-for-gestational-age term fetuses with cerebral blood flow redistribution. Ultrasound Obstet Gynecol 32:894–899
Engle WA (2011) Morbidity and mortality in late preterm and early term newborns: a continuum. Clin Perinatol 38:493–516
Fadigas C, Saiid Y, Gonzalez R, Poon LC, Nicolaides KH (2015) Prediction of small-for-gestational-age neonates: screening by fetal biometry at 35–37 weeks. Ultrasound Obstet Gynecol 45:559–565
Figueras F, Gratacos E (2014) Stage-based approach to the management of fetal growth restriction. Prenat Diagn 34:655–659
Garite TJ, Clark R, Thorp JA (2004) Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am J Obstet Gynecol 191:481–487
Gibson AT, Carney S, Cavazzoni E, Wales JK (2000) Neonatal and postnatal growth. Horm Res 53:42–49
Gortner L, Wauer RR, Stock GJ, Reiter HL, Reiss I, Jorch G, Hentschel R, Hieronimi G (1999) Neonatal outcome in small for gestational age infants: do they really better? J Perinat Med 27:484e9
Griffin IJ, Tancredi DJ, Bertino E, Lee HC, Profit J (2015) Postnatal growth failure in very low birthweight infants born between 2005 and 2012. Arch Dis Child Fetal Neonatal Ed 101:F1–F6
Guellec I, Lapillonne A, Renolleau S, Charlaluk ML, Roze JC, Marret S, Vieux R, Monique K, Ancel PY, EPIPAGE Study Group (2011) Neurologic outcomes at school age in very preterm infants born with severe or mild growth restriction. Pediatrics 127:e883–e891
Halliday HL (2009) Neonatal management and long-term sequelae. Best Pract Res Clin Obstet Gynaecol 23:871–880
Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB (2008) Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ 336:85–87
Hanson MA, Gluckman PD (2014) Early developmental conditioning of later health and disease: physiology or pathophysiology? Physiol Rev 94:1027–1076
Hernández MI, Mericq V (2008) Impact of being born small for gestational age on onset and progression of puberty. Best Pract Res Clin Endocrinol Metab 22:463–476
Hofman PL, Regan F, Cutfield WS (2006) Prematurity-another example of perinatal metabolic programming? Horm Res 66:33–39
Jarvis S, Glinianaia SV, Torrioli MG, Platt MJ, Miceli M, Jouk PS, Johnson A, Hutton J, Hemming K, Hagberg G, Dolk H, Chalmers J, Surveillance of Cerebral Palsy in Europe (SCPE) collaboration of European Cerebral Palsy Registers (2003) Cerebral palsy and intrauterine growth in single births: European collaborative study. Lancet 362:1106–1111
Kalish RB, Thaler HT, Chasen ST, Gupta M, Berman SJ, Rosenwaks Z, Chervenak FA (2004) First- and second-trimester ultrasound assessment of gestational age. Am J Obstet Gynecol 191:975–978
Kanaka-Gantenbein C (2010) Fetal origins of adult diabetes. Ann N Y Acad Sci 1205:99–105
Karsdorp VH, van Vugt JM, van Geijn HP, Kostense PJ, Arduini D, Montenegro N, Todros T (1994) Clinical significance of absent or reversed end-diastolic velocity waveforms in umbilical artery. Lancet 344:1664–1668
Kase BA, Carreno CA, Blackwell SC (2012) Customized estimated fetal weight: a novel antenatal tool to diagnose abnormal fetal growth. Am J Obstet Gynecol 207:218.e1–218.e5
Kinsella JP, Greenough A, Abman SH (2006) Bronchopulmonary dysplasia. Lancet 367:1421–1431
Koleganova N, Piecha G, Ritz E (2009) Prenatal causes of kidney disease. Blood Purif 27:48–52
Kramer MS, Mc Lean FH, Olivier M, Willis DM, Usher RH (1989) Body proportionality and head and length “sparing” in growth-retarded neonates: a critical reappraisal. Pediatrics 84:717–723
Lal MK, Manktelow BN, Draper ES, Field DJ (2003) Chronic lung disease of prematurity and intrauterine growth retardation: a population-based study. Pediatrics 111:483–487
Lees C, Marlow N, Arabin B, Bilardo CM, Brezinka C, Derks JB, Duvekot J, Frusca T, Diemert A, Ferrazzi E, Ganzevoort W, Hecher K, Martinelli P, Ostermayer E, Papageorghiou AT, Schlembach D, Schneider KT, Thilaganathan B, Todros T, van Wassenaer-Leemhuis A, Valcamonico A, Visser GH, Wolf H, TRUFFLE Group (2013) Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet Gynecol 42:400–408
Lees C, Marlow N, van Wassenaer-Leemhuis A, Arabin B, Bilardo CM, Brezinka C, Calvert S, Derks JB, Diemert A, Duvekot JJ, Ferrazzi E, Frusca T, Ganzevoort W, Hecher K, Martinelli P, Ostermayer E, Papageorghiou AT, Schlembach D, Schneider KTM, Thilaganathan B, Todros T, Valcamonico A, Visser GHA, Wolf H, on behalf of the TRUFFLE Group (2015) The Trial of Randomized Umbilical and Fetal Flow in Europe (TRUFFLE) study: two year neurodevelopmental and intermediate perinatal outcomes. Lancet 385:2162–2172
Lesmes C, Gallo DM, Panaiotova J, Poon LC, Nicolaides KH (2015) Prediction of small-for-gestational-age neonates: screening by fetal biometry at 19–24 weeks. Ultrasound Obstet Gynecol 46:198–207
Levine TA, Grunau RE, McAuliffe FM, Pinnamaneni R, Foran A, Alderdice FA (2015) Early childhood neurodevelopment after intrauterine growth restriction: a systematic review. Pediatrics 135:126–141
Lindqvist PG, Molin J (2005) Does antenatal identification of small-for-gestational age fetuses significantly improve their outcome? Ultrasound Obstet Gynecol 25:258–264
Lundgren EM, Tuvemo T (2008) Effects of being born small for gestational age on long-term intellectual performance. Best Pract Res Clin Endocrinol Metab 22:477–488
Lundgren P, Kistner A, Andersson EM, Hansen Pupp I, Holmström G, Ley D, Niklasson A, Smith LE, Wu C, Hellström A, Löfqvist C (2014) Low birth weight is a risk factor for severe retinopathy of prematurity depending on gestational age. PLoS One 9:e109460
Lyall F, Robson SC, Bulmer JN (2013) Spiral artery remodeling and trophoblast invasion in preeclampsia and fetal growth restriction: relationship to clinical outcome. Hypertension 62:1046–1054
Main KM, Jensen RB, Asklund C, Høi-Hansen CE, Skakkebaek NE (2006) Low birth weight and male reproductive function. Horm Res 65:116–122
Maiorana A, Del Bianco C, Cianfarani S (2007) Adipose tissue: a metabolic regulator. Potential implications for the metabolic outcome of subjects born Small for Gestational Age (SGA). Rev Diabet Stud 4:134–146
Mamopoulos A, Petousis S, Tsimpanakos J, Masouridou S, Kountourelli K, Margioula-Siarkou C, Papouli M, Rousso D (2015) Birth weight independently affects morbidity and mortality of extremely preterm neonates. J Clin Med Res 7:511–516
Mari G, Hanif F, Treadwell MC, Kruger M (2007) Gestational age at delivery and Doppler waveforms in very preterm intrauterine growth-restricted fetuses as predictors of perinatal mortality. J Ultrasound Med 26:555–559
McCowan LM, Mullen BM, Ritchie K (1987) Umbilical artery flow velocity waveforms and the placental vascular bed. Am J Obstet Gynecol 157:900–902
McIntire DD, Bloom SL, Casey BM, Leveno KJ (1999) Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med 340:1234–1238
McMillen I, Adams M, Ross J, Coulter CL, Simonetta G, Owens JA, Robinson JS, Edwards LJ (2001) Fetal growth restriction: adaptation and consequences. Reproduction 122:195–204
Meher S, Hernandez-Andrade E, Basheer SN, Lees C (2015) Impact of cerebral redistribution on neurodevelopmental outcome in small for gestational age or growth restricted babies: a systematic review. Ultrasound Obstet Gynecol 46:398–404
Miller HC (1985) Prenatal factors affecting intrauterine growth retardation. Clin Perinatol 12:307–318
Mitsiakos G, Papaioannou G, Papadakis E, Chatziioannidis E, Giougi E, Karagianni P, Evdoridou J, Malindretos P, Athanasiou M, Athanassiadou F, Nikolaidis N (2009) Haemostatic profile of full-term, healthy, small for gestational age neonates. Thromb Res 124:288–291
Morin I, Morin L, Zhang X, Platt RW, Blondel B, Bréart G, Usher R, Kramer MS (2005) Determinants and consequences of discrepancies in menstrual and ultrasonographic gestational age estimates. BJOG 112:145–152
Morley R, Fewtrell MS, Abbott RA, Stephenson T, MacFadyen U, Lucas A (2004) Neurodevelopment in children born small for gestational age: a randomized trial of nutrient-enriched versus standard formula and comparison with a reference breastfed group. Pediatrics 113:515–521
Morsing E, Asard M, Ley D, Stjernqvist K, Marsál K (2011) Cognitive function after intrauterine growth restriction and very preterm birth. Pediatrics 127:e874–e882
Murdoch EM, Sinha AK, Shanmugalingam ST, Smith GC, Kempley ST (2006) Doppler flow velocimetry in the superior mesenteric artery on the first day of life in preterm infants and the risk of neonatal necrotizing enterocolitis. Pediatrics 118:1999–2003
Nakling J, Buhaug H, Backe B (2005) The biologic error in gestational length related to the use of the first day of last menstrual period as a proxy for the start of pregnancy. Early Hum Dev 81:833–839
Nicolaides KH, Bilardo CM, Soothill PW, Campbell S (1988) Absence of end diastolic frequencies in umbilical artery: a sign of fetal hypoxia and acidosis. BMJ 297:1026
Nobili V, Alisi A, Panera N, Agostoni C (2008) Low birth weight and catch-up-growth associated with metabolic syndrome: a ten year systematic review. Pediatr Endocrinol Rev 6:241–247
Olofsson P, Laurini RN, Marsál K (1993) A high uterine artery pulsatility index reflects a defective development of placental bed spiral arteries in pregnancies complicated by hypertension and fetal growth retardation. Eur J Obstet Gynecol Reprod Biol 49:161–168
Oros D, Figueras F, Cruz-Martinez R, Meler E, Munmany M, Gratacos E (2011) Longitudinal changes in uterine, umbilical and fetal cerebral Doppler indices in late-onset small-for-gestational age fetuses. Ultrasound Obstet Gynecol 37:191–195
Pallotto EK, Kilbride HW (2006) Perinatal outcome and later implications of intrauterine growth restriction. Clin Obstet Gynecol 49:257–269
Pallotto EK, Woelnerhanssen B, Putt M (2004) Incidence and risk factors for prolonged hypoglycemia in small for gestational age infants. Abstract, Society for Pediatric and Perinatal Epidemiology
Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Cheikh Ismail L, Lambert A, Jaffer YA, Bertino E, Gravett MG, Purwar M, Noble JA, Pang R, Victora CG, Barros FC, Carvalho M, Salomon LJ, Bhutta ZA, Kennedy SH, Villar J, International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) (2014) International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet 384:869–879
Peacock JL, Lo JW, D’Costa W, Calvert S, Marlow N, Greenough A (2013) Respiratory morbidity at follow-up of small-for-gestational age infants born very prematurely. Pediatr Res 73:457–463
Piper JM, Xenakis EM, McFarland M, Elliott BD, Berkus MD, Langer O (1996) Do growth-retarded premature infants have different rates of perinatal morbidity and mortality than appropriately grown premature infants? Obstet Gynecol 87:169–174
Pulver LS, Guest-Warnick G, Stoddard GJ, Byington CL, Young PC (2009) Weight for gestational age affects the mortality of late preterm infants. Pediatrics 123:e1072–e1077
Rasmussen S, Kiserud T, Albrechtsen S (2006) Foetal size and body proportion at 17–19 weeks of gestation and neonatal size, proportion, and outcome. Early Hum Dev 82:683–690
Ree IM, Smits-Wintjens VE, Rijntjes-Jacobs EG, Pelsma IC, Steggerda SJ, Walther FJ, Lopriore E (2014) Necrotizing enterocolitis in small-for-gestational-age neonates: a matched case–control study. Neonatology 105:74–78
Regev RH, Lusky A, Dolfin T, Litmanovitz I, Arnon S, Reichman B, Network IN (2003) Excess mortality and morbidity among small-for-gestational-age premature infants: a population-based study. J Pediatr 143:186–191
Reinehr T, Kleber M, Toschke AM (2009) Small for gestational age status is associated with metabolic syndrome in overweight children. Eur J Endocrinol 160:579–584
Rizzo G, Prefumo F, Ferrazzi E, Zanardini C, Di Martino D, Boito S, Aiello E, Ghi T, SIEOG working group on fetal biometric charts (2016) The effect of fetal sex on customized fetal growth charts. J Matern Fetal Neonatal Med 3:1–8
Rosenberg A (2008) The IUGR newborn. Semin Perinatol 32:219–224
Rozance PJ (2014) Update on neonatal hypoglycemia. Curr Opin Endocrinol Diabetes Obes 21:45–50
Sabel KG, Olegard R, Mellander M, Hildingsson K (1982) Interrelation between fatty acid oxidation and control of gluconeogenic substrates in small for gestational age (SGA) infants with hypoglycemia and with normoglycemia. Acta Paediatr Scand 71:53–61
Saenger P, Czernichow P, Hughes I, Reiter EO (2007) Small for gestational age: short stature and beyond. Endocr Rev 28:219–251
Sarkar S, Rosenkrantz TS (2008) Neonatal polycythemia and hyperviscosity. Semin Fetal Neonatal Med 13:248–255
Savchev S, Figueras F, Cruz-Martinez R, Illa M, Botet F, Gratacos E (2012) Estimated weight centile as a predictor of perinatal outcome in small-for-gestational-age pregnancies with normal fetal and maternal Doppler indices. Ultrasound Obstet Gynecol 39:299–303
Shand AW, Hornbuckle J, Nathan E, Dickinson JE, French NP (2009) Small for gestational age preterm infants and relationship of abnormal umbilical artery Doppler blood flow to perinatal mortality and neurodevelopmental outcomes. Aust N Z J Obstet Gynaecol 49:52–58
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J, Declercq E (2008) Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics 121:e223–e232
Sharma P, McKay K, Rosenkrantz TS, Hussain N (2004) Comparisons of mortality and pre-discharge respiratory outcomes in small-for-gestational-age and appropriate-for-gestational-age premature infants. BMC Pediatr 4:9
Simon D, Léger J, Carel JC (2008) Optimal use of growth hormone therapy for maximizing adult height in children born small for gestational age. Best Pract Res Clin Endocrinol Metab 22:525–537
Singer DB, Sung CJ, Wigglesworth JS (1991) Fetal growth and maturation with standards for body and organ development. In: Wigglesworth JS, Singer DB (eds) Textbook of fetal and perinatal pathology. Blackwell, London, pp 11–47
Skuse D, Pickles A, Wolke D, Reilly S (1994) Postnatal growth and mental development: evidence for a “sensitive period”. J Child Psychol Psychiatry 35:521–545
Smith LE (2005) IGF-1 and retinopathy of prematurity in the preterm infant. Biol Neonate 88:237–244
Snijders RJ, Abbas A, Melby O, Ireland RM, Nicolaides KH (1993) Fetal plasma erythropoietin concentration in severe growth retardation. Am J Obstet Gynecol 168:615–619
Soothill PW, Ajayi RA, Campbell S, Ross EM, Candy DC, Snijders RM, Nicolaides KH (1992) Relationship between fetal acidemia at cordocentesis and subsequent neurodevelopment. Ultrasound Obstet Gynecol 2:80–83
Soudée S, Vuillemin L, Alberti C, Mohamed D, Becquet O, Farnoux C, Biran V, Baud O (2014) Fetal growth restriction is worse than extreme prematurity for the developing lung. Neonatology 106:304–310
Sovio U, White IR, Dacey A, Pasupathy D, Smith GC (2015) Screening for fetal growth restriction with universal third trimester ultrasonography in nulliparous women in the Pregnancy Outcome Prediction (POP) study: a prospective cohort study. Lancet 386:2089–2097
Tajik P, van Wyk L, Boers KE, le Cessie S, Zafarmand MH, Roumen F, van der Post JA, Porath M, van Pampus MG, Spaanderdam ME, Kwee A, Duvekot JJ, Bremer HA, Delemarre FM, Bloemenkamp KW, de Groot CJ, Willekes C, van Lith JM, Bossuyt PM, Mol BW, Scherjon SA, DIGITAT Study Group (2014) Which intrauterine growth restricted fetuses at term benefit from early labour induction? A secondary analysis of the DIGITAT randomised trial. Eur J Obstet Gynecol Reprod Biol 172:20–25
Tanner JM (1989) Foetus into man, 2nd edn. Castlemead Publication, Welwyn Garden City
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologist (2007) Standard terminology for reporting of reproductive health statistics in the United States. In: Guideline for prenatal care. American Academy of Pediatrics, Elk Grove Village
Thorsell M, Kaijser M, Almström H, Andolf E (2008) Expected day of delivery from ultrasound dating versus last menstrual period–obstetric outcome when dates mismatch. BJOG 115:585–589
Todros T, Plazzotta C, Pastorin L (1996) Body proportionality of the small-for-date fetus: is it related to aetiological factors? Early Hum Dev 45:1–9
Todros T, Sciarrone A, Piccoli E, Guiot C, Kaufmann P, Kingdom J (1999) Umbilical Doppler waveforms and placental villous angiogenesis in pregnancies complicated by fetal growth restriction. Obstet Gynecol 93:499–503
Torrance HL, Bloemen MC, Mulder EJ, Nikkels PG, Derks JB, de Vries LS, Visser GH (2010) Predictors of outcome at 2 years of age after early intrauterine growth restriction. Ultrasound Obstet Gynecol 36:171–177
Tyrrell S, Obaid AH, Lilford RJ (1989) Umbilical artery Doppler velocimetry as a predictor of fetal hypoxia and acidosis at birth. Obstet Gynecol 74:332–337
van Wyk L, Boers KE, van der Post JA, van Pampus MG, van Wassenaer AG, van Baar AL, Spaanderdam ME, Becker JH, Kwee A, Duvekot JJ, Bremer HA, Delemarre FM, Bloemenkamp KW, de Groot CJ, Willekes C, Roumen FJ, van Lith JM, Mol BW, le Cessie S, Scherjon SA, DIGITAT Study Group (2012) Effects on (neuro developmental and behavioral outcome at 2 years of age of induced labor compared with expectant management in intrauterine growth-restricted infants: long-term outcomes of the DIGITAT trial. Am J Obstet Gynecol 206:406 e1–406 e7
Varda NM, Gregoric A (2009) Metabolic syndrome in the pediatric population: a short overview. Pediatric Rev 1:e1
Varella MH, Moss WJ (2015) Early growth patterns are associated with intelligence quotient scores in children born small-for-gestational age. Early Hum Dev 91:491–497
Vashevnik S, Walker S, Permezel M (2007) Stillbirths and neonatal deaths in appropriate, small and large birthweight for gestational age fetuses. Aust N Z J Obstet Gynaecol 47:302–306
Victora CG (2015) Anthropometric characterization of impaired fetal growth. Risk factors for and prognosis of newborns with stunting or wasting. JAMA Pediatr 169(7):e151431
Vrachnis N, Botsis D, Iliodromiti Z (2006) The fetus that is small for gestationel age. N Y Acad Sci 1092:304–309
Walker DM, Marlow N (2008) Neurocognitive outcome following fetal growth restriction. Arch Dis Child Fetal Neonatal Ed 93:F322–F325
Wirbelauer J, Thomas W, Rieger L, Speer CP (2010) Intrauterine growth retardation in preterm infants ≤32 weeks of gestation is associated with low white blood cell counts. Am J Perinatol 27(10):819–824
Wit JM, Finken MJ, Rijken M, de Zegher F (2006) Preterm growth restraint: a paradigm that unifies intrauterine growth retardation and preterm extrauterine growth retardation and has implications for the small-for-gestational-age indication in growth hormone therapy. Pediatrics 117:e793–e795
Yeung MY (2006) Postnatal growth, neurodevelopment and altered adiposity after preterm birth–from a clinical nutrition perspective. Acta Paediatr 95:909–917
Yu V, Upadhyay A (2004) Neonatal management of the growth-restricted infant. Semin Fetal Neonatal Med 9:403–409
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this entry
Cite this entry
Bertino, E., Oggè, G., Di Nicola, P., Giuliani, F., Coscia, A., Todros, T. (2018). Intrauterine Growth Restriction: Obstetric and Neonatal Aspects. Intervention Strategies. In: Buonocore, G., Bracci, R., Weindling, M. (eds) Neonatology. Springer, Cham. https://doi.org/10.1007/978-3-319-29489-6_158
Download citation
DOI: https://doi.org/10.1007/978-3-319-29489-6_158
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29487-2
Online ISBN: 978-3-319-29489-6
eBook Packages: MedicineReference Module Medicine