Keypoints
-
1.
A detailed case history is required in all tinnitus patients in order to obtain the necessary information for deciding about the therapeutic management.
-
2.
Qualitative data can be best obtained by case history questionnaires or a structured interview.
-
3.
A case history should contain information about the history and descriptive characteristics of the tinnitus, about specific behavioral, social, interpersonal, and emotional consequences of tinnitus, about factors that may either exacerbate or reduce tinnitus severity, about previous tinnitus treatments, and about relevant comorbidities.
-
4.
Quantitative assessment of tinnitus severity is relevant for both clinical management and research applications.
-
5.
Various validated questionnaires are available for quantifying tinnitus distress, disability, or handicap.
-
6.
The selection of the questionnaire should be based not only on purpose (What should be assessed?) but also on psychometric data of the questionnaire and the availability of the questionnaire in a specific language.
-
7.
Numeric rating scales and visual analogue scales are easy applicable tools for quantifying different aspects of tinnitus (such as loudness or annoyance).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tinnitus
- Case history
- Questionnaire
- Structured interview
- Quantitative assessment
- Clinical management
- research applications
- Visual analogue scales
Introduction
Tinnitus has many forms and many characteristics. However, tinnitus is not readily apparent to others, and currently no objective procedures are yet established for diagnosis of tinnitus. The assessment of the perceptual aspects of tinnitus is difficult. Only by listening to the patient can one find out whether a patient has tinnitus and what form of tinnitus he/she has. The case history is of high importance for correct diagnosis in all areas of medicine; this is especially true for tinnitus, since it is fundamentally a self-report phenomenon. Moreover, the subjective nature of tinnitus is a challenge not only in the clinical management of the individual with tinnitus but also for research applications.
Therefore, in addition to an otologic (see Chap. 48) and audiologic assessment (see Chap. 49), a detailed case history is required in all tinnitus patients in order to obtain the necessary information for deciding about the therapeutic management (see Chap. 46). In many patients, a comprehensive diagnostic assessment including a detailed case history can be sufficient for tinnitus management. If a severe disorder (e.g., tumor or carotid dissection) can be excluded and the tinnitus is not perceived as a problem, no treatment is necessary. In all other cases, the detailed case history represents the first therapeutic step, since the patients can make their experience known, they see that their complaints are taken seriously and that the clinician is competent, caring, and understands the effects of tinnitus.
For the clinical management of the individual patient information about the perceptual characteristics of tinnitus (e.g., pulsatile or non pulsatile), its time course (e.g., recent onset or chronic), influencing factors (e.g., reduction by environmental sound), and associated symptoms (e.g., reduced sound tolerance) are important. These qualitative data can be best obtained by case history questionnaires or a structured interview.
Loudness of tinnitus can be evaluated quantitatively either by rating or by matching methods (see Chap. 49). In addition to details about the tinnitus percept, information about the perceived severity and the impact on an individual’s life also have to be assessed. Personality, comorbidities, or environmental circumstances contribute more to tinnitus-related distress, impairment, disability, and handicap than the perceptual characteristics of tinnitus [1, 2]. Therefore, the evaluation of tinnitus consequences on a person’s life needs to be multidimensional, taking into account psychological and social factors.
Screening tools allow an estimation of tinnitus severity based on a few questions, whereas for quantitative assessment of tinnitus severity, many psychometrically validated questionnaires are available. These questionnaires are helpful tools for quantifying disabling and handicapping effects of tinnitus, providing insight into how the tinnitus sensation generates a disability at a personal level and a handicap on the societal level. Responses on these questionnaires can be summed resulting in a total score or subscale scores. Based on the score, the tinnitus severity of an individual patient can be determined (e.g., in low, medium, moderate, or severe).
If a patient is moderately or severely impaired, additional assessment by a psychologist or a psychiatrist is frequently necessary. Psychological and psychiatric assessment involves the integration of information from multiple sources and tools, including the clinical interview, rating scales, questionnaires, and the observation of the patient’s behavior during the interview. It is not only what the patients say but also how they say it that is of relevance. Sometimes, interviews with significant others or reports from previous therapists or physicians provide further important information.
The clinician also needs to be aware that when people complaint about tinnitus, other problems may be contributing to any negative emotional state. For example, a coexistent hearing impairment or hyperacusis, balance problems, pain, anxiety, or depression may contribute to the person’s difficulties. Daily stressors or major life events may also have an impact on the person’s ability to cope with the tinnitus, and patients may attribute their feelings of depression and anxiety incorrectly to the tinnitus. An aim of the initial assessment may also be to disentangle causal connections between tinnitus distress, other stressors, and negative emotional states.
Another important area of investigation concerns the risk of suicide. Rather than avoiding asking questions about suicide, the clinician should address this issue directly. Patients may consider suicide as a means to escape from tinnitus or it may be concurrent to a depressive disorder (for more detailed information see Chap. 54). If results indicate the potential for self-harm, the clinician should manage for this or refer the patient to another specialist.
In addition to clinical applications, quantitative assessment by tinnitus questionnaires is an important tool for all kinds of different research applications.
This chapter reviews methods for obtaining qualitative and quantitative information about a condition, which is purely subjective in its nature, namely a patient’s tinnitus and its disabling and handicapping effects. It is our intent to provide a useful and practical reference for both clinicians and researchers seeking information about the availability of different methods. Also, the limitations of the different methods will be discussed in order to allow the readers to select the most appropriate method for their specific clinical or research application (see Table 47.1).
Case History
A detailed history and primary source of descriptive data of the patient’s tinnitus or tinnitus-related conditions can be obtained through the initial intake, either by a questionnaire or by structured interviews. The goal of the intake interview is to arrive at a thorough understanding of the nature of the tinnitus by exploring a broad range of inquiry, including causal, descriptive, and diagnostic variables. This information, together with otologic and audiological assessment, is the basis for further diagnostic and therapeutic management. In detail, the following areas should be explored comprehen sively:
-
(1)
The history and descriptive characteristics of the tinnitus;
-
(2)
Specific behavioral, social, interpersonal, and emotional consequences of tinnitus;
-
(3)
Factors that may either exacerbate or reduce tinnitus severity;
-
(4)
Previous tinnitus treatments;
-
(5)
Relevant comorbidities.
Many practitioners prefer questionnaires. Case history questionnaires offer advantages of standardized questions to provide reliable and complete information; furthermore, they require less clinician time than interviews. Detailed patient information can be especially important in medicolegal cases.
Several case history questionnaires have been published [3–5], but many clinicians and researchers have developed their own questionnaires in which they include those questions that they consider important and relevant. In the context of a consensus workshop on tinnitus assessment in Regensburg in July 2006, an “items list” for tinnitus case history questionnaires (see Table 47.2) has been compiled including items that are common to most questionnaires in current use and are considered important by experts in the field. This list consists of 14 essential (level A) items and 21 highly desirable (level B) items. Also, a case history questionnaire has been developed, which can be used as an example of how these items might be expressed (Tinnitus Sample Case History Questionnaire (TSCHQ), available in English, French, Spanish, Italian, German, Portuguese, Flemish, and Czech languages at http://www.tinnitusresearch.org [4]).
Depending on their individual background, some clinicians will consider additional items as relevant (e.g., a clinician with physiotherapeutic experience will be interested in more detailed information about postural complaints). The item list should therefore only be considered as a core list to which individual specializations should be added. In the following description, we want to give some examples about the relevance of the proposed items for further diagnostic or therapeutic procedures. A comprehensive description of the clinical characteristics of the different forms of tinnitus is found in Part V.
Demographic data, such as age, are of relevance since the causes of tinnitus are different in younger and older people. In elderly people, tinnitus is frequently associated with presbycusis [6]; other causal factors such as noise exposure may be more prominent in younger patients [7]. A positive family history of tinnitus complaints can point to a genetic form of hearing loss as an underlying disorder. There is also some suggestion that genetic factors may play a role for individual susceptibility to tinnitus [8] (see Chap. 7).
The duration of tinnitus is of high relevance for further diagnostic and therapeutic management. Whereas acute tinnitus, especially with abrupt onset, may be a sign of an acute dangerous disease, this is only very rarely the case in chronic tinnitus. Also, acute tinnitus requires an entirely different therapeutic management than chronic tinnitus. The circumstances under which tinnitus started are also important (e.g., onset of tinnitus related to neck trauma needs a different diagnostic work-up than tinnitus that started during a stressful live event).
Concerning the sound characteristics that patients report, the differentiation between pulsatile and non-pulsatile tinnitus is of greatest importance. In patients who describe pulsatile sounds, particularly if synchronous with the heartbeat, vascular origin should be suspected. Pulsatile tinnitus requires specific diagnostic procedures (see Chap. 46). Low-pitched tinnitus with intermittent occurrence may be a cue for the diagnosis of Ménière’s disease. Neurophysiologic differences have been suggested for tinnitus resembling “a pure tone” and “noise,” and response to specific therapeutic procedures may depend on this distinction [9, 10].
Tinnitus loudness can be assessed with numeric rating scales or visual analogue scales and gives an estimate of the subjectively perceived loudness of the patient’s tinnitus. The percentage of time patients are aware of their tinnitus varies enormously between “sometimes in quiet environments” and “always.” Also, there is a difference between the time patients are aware and the time patients are annoyed by their tinnitus. These factors are important for determining how intrusive the tinnitus may be in a specific patient.
Factors that improve or worsen tinnitus can be important predictors for treatment success (e.g., use of a sound generator if environmental sounds reduce tinnitus). Determination of therapies that have been trialed, successfully or not, can also provide useful information as to a future treatment choice. When therapies in the past have failed, it should be asked exactly how the therapy had been performed. Possible reasons for failing could be an inadequate performance or insufficient duration of a given treatment.
There are several health disorders, which are frequently associated with tinnitus, such as hearing loss, hyperacusis, neck or temporomandibular joint disorders, vertigo, insomnia, headache, anxiety, or depression. These comorbidities may be a cause or a consequence of tinnitus. In all cases, the co-occurrence of these disorders is of relevance for the therapeutic management. Irrespective of whether there is a causal relationship or not, successful treatment of tinnitus comorbidities can improve the patient’s quality of life enormously. This, in turn, may also improve the patient’s ability to cope with tinnitus, even if perceptual characteristics remain largely unchanged (see chapters in Part V for more details).
Although case history questionnaires are useful tools for obtaining information, they should not replace a thorough clinical intake interview. However, the use of a case history questionnaire can make the intake interview more efficient by providing an opportunity to discuss relevant items in detail. Patients should be encouraged to clarify questions when they are uncertain how to answer. The discussion allows patients to also describe in their own words aspects of special importance to them. The discussion of the different items helps establish rapport between the clinician and the patient. In this context, it is always helpful to ask patients what bothers them the most about their tinnitus. This varies from patient to patient and has implications for the therapeutic management. If, for example, a patient suffers mainly from the lack of control, this can be addressed by cognitive–behavioral therapy; if the main complaint is difficulty in sleeping, the treatment of the sleeping problem should also be the main focus. Furthermore, the impact of tinnitus on the person’s work, sleep (falling asleep and staying asleep), participation in enjoyable activities, social interaction (with friends, family, and partner), and the general lifestyle has to be examined. Reactions to tinnitus can be very different, and it is the patient’s reaction to tinnitus that causes problems rather than the sound by itself. If this message reaches the patient during the intake interview, a very important first step toward treatment has been achieved.
Quantitative Assessment of Tinnitus
Many people with tinnitus are neither bothered nor concerned about their tinnitus. There is also a group of patients who see a physician only because they are concerned that their tinnitus may be a sign of a serious ear or brain disease. Apart from those, all other people with tinnitus who seek medical attention are to some extent bothered by their tinnitus. However, there is a large variability in distress, ranging from those who have learned to cope but would welcome some relief from the sound, to those who have severe problems with tinnitus in their daily lives. It has been repeatedly shown that the loudness or the pitch of the tinnitus sensation does not predict suffering [1, 2, 11]. Methods that directly quantify tinnitus distress, disability, and handicap are more appropriate for assessing the amount of suffering. Screening tools allow an estimation of tinnitus severity based on a few questions, whereas for quantitative assessment of tinnitus severity several questionnaires are available.
Psychometric and Methodological Aspects
Different methodological aspects have to be considered in the use of quantitative measurement techniques.
Validity
Is there a specific questionnaire assessing disability, handicap, or coping styles? In general, the validity of an instrument is reflected by its ability to yield “truthful,” “correct,” or “real” information (see also Fig. 47.1). Validation strategies include content validity, criterion-related validity, and construct validity. Content validity demonstrates to which extent the items of the scale reflect the characteristics to be measured; criterion-related validity measures how well the instrument correlates with a “gold standard”; and construct validity reflects the degree to which an instrument purports to measure a theoretic construct of the characteristics to be assessed [12, 13].
Standardization and Norming
Can data assessed at place X at time X be compared to those at place Y and time Y?
Is there a specific score high or low as compared to most other patients?
Standardization means that data are always assessed and performed in the same standardized way. Relevant issues can be whether a questionnaire is completed as an electronic version or as a paper version, or whether it is completed before or after the first consultation. Only a standardized way of assessment allows comparison across individuals, time, and clinical settings. Norming means obtaining information about the distribution of measures in a target population in the form of means, standard deviations, or percentiles. Normative data allow placement of the score of an individual in context of a target population.
Reliability
Does the tinnitus questionnaire have high test–retest reliability and stability?
Reliability describes the precision of the instrument and includes internal consistency but also reproducibility. Internal consistency reflects the inter-item consistency of a scale or subscales. It is expected that several items that assess the same construct (e.g., tinnitus handicap) correlate with each other. The statistical measure of this internal consistency is Cronbach’s α.
Reproducibility can be differentiated in short- and long-term reproducibility. Short-term reproducibility may reflect effects of day-to-day fluctuations; long-term reproducibility describes stability over longer time intervals. This is of relevance when a questionnaire is used for evaluating effects of a specific intervention. If there is a lack of knowledge about the changes in a questionnaire score over time occurring without any treatment intervention, one cannot rely on uncontrolled observations of treatment effects. Documented changes in tinnitus scores may not be due to the treatment, per se, but rather due to measurement error of the questionnaire used for assessing treatment outcome.
Responsiveness
Is the questionnaire sensitive for treatment-induced changes?
Responsiveness reflects the ability of a questionnaire to register changes following an individual’s response to a treatment intervention. This is especially required when an instrument is used as treatment outcome measure. This aspect of measurement instruments has also been characterized as evaluative [14, 15]. Variables that are stable over time and reflect, for example, the individual’s personality are called trait parameters, whereas variables that reflect mainly the actual condition are called state variables.
From an evaluative questionnaire, one would expect that it samples mainly state variables that are likely to change under treatment. A large amount of change-insensitive trait variables are useless for detecting treatment effects and may even obscure them. In contrast, the inclusion of trait parameters can be useful for an instrument designed for diagnostic use (e.g., for discriminating between individuals with severe vs. mild tinnitus, see Table 47.5).
Another factor related to the responsiveness of a questionnaire is the number of response options for each item. A questionnaire, which consists of items that can only be answered with two or three levels (e.g., yes and no), is, in general, less sensitive to changes than a questionnaire with five or more answer options per item.
It should be noted that the currently available tinnitus questionnaires have not been specifically designed for evaluating treatment-related changes, but most of them have been used as outcome measurers in clinical trials. New questionnaires specifically designed to evaluate treatment-related changes will emerge in the near future [15].
Feasability
Is the questionnaire easily applicable?
Feasibility reflects the property of an instrument to be practically applicable in a real-world context. As an example, in order to be applicable in a busy clinical practice, tinnitus questionnaires should be brief and easy to administer, understand, score, and interpret.
Cultural and Language Bias
Questionnaires designed and tested in one population and language are not necessarily equally applicable in another. Questionnaires developed in one culture do not necessarily measure the same factors in another, even if the language is the same [16]. Likewise, translation from one language to another can introduce changes in meaning. One way of addressing these variations is to validate the questionnaire in each language and setting. This may lead to some items from the original questionnaire being moved into a different factor or rejected as invalid. While this approach has merit in optimizing the questionnaire for a particular population, there are at least two significant downsides: (1) considerable time is required to validate the questionnaire in each setting and (2) cross-population comparisons become difficult. The latter of these two issues is most troublesome for researchers who might want to compare outcomes from two populations using the “same” questionnaire. For example, a questionnaire developed in the US but optimized for New Zealand might omit questions [16]. If two treatments are compared between these countries and found to have the same questionnaire scores, it cannot be assumed that the treatments are equally effective because they actually do not ask the same questions. On the other hand, if the original questionnaire is used in its original form in both countries, cultural idiosyncrasies mean that they still measure different factors. This paradox is a limitation of questionnaires. Any “worldwide” standard should retain as many of its original items and factor structure when validated in different populations. Researchers should recognize the potential for population differences when using questionnaires.
Screening of Tinnitus Severity
In the daily routine of an audiological or otolaryngologic clinic, there is a high need for fast and reliable classification of tinnitus patients according to their severity. Those who suffer from tinnitus require an entirely different management than those who simply experience tinnitus, but are only slightly impaired by it. Here, a screening tool is presented that consists of three questions and allows screening for tinnitus severity in an objective and economic way (B-Scale; [17]; Table 47.3).
Another possibility of a single, global measure of the impact of tinnitus on individuals is the following global item [15]:
How much of a problem is your tinnitus?
Not a problem | 0 |
A small problem | 1 |
A moderate problem | 2 |
A big problem | 3 |
A very big problem | 4 |
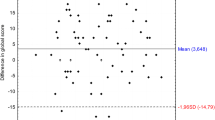
Preliminary data from the tinnitus clinic in Regensburg show that this five-level response scale correlates highly with the score of the tinnitus questionnaire (see Fig. 47.2), indicating that it is a reliable, well-functioning global item for screening patients.
Correlation between the screening question “How much of a problem is your tinnitus?” and the score in the Tinnitus Questionnaire [30] (N: 281; r = 0.70)
Tinnitus Questionnaires
Different questionnaires are available to assess specific aspects of patients with tinnitus (see Table 47.4). These questionnaires are score driven, which means that the responses to single items are scored and then summed or averaged. Thus, total scores or subscale scores can be calculated.
There are specific questionnaires for assessing tinnitus-related cognitions (TCQ) or coping styles (TCSQ). The other questionnaires mainly aim to quantify tinnitus distress, disability, or handicap. Items of the different scales largely overlap. Accordingly, there is a relatively high correlation between the total scores of the different tinnitus severity and handicap questionnaires.
In addition to clinical applications, quantitative assessment by tinnitus questionnaires allows research applications. For example, tinnitus questionnaires have been successfully used for investigating the relationship between personality and psychopathology and their impact on tinnitus severity [18]. Furthermore, tinnitus questionnaires provide a method for researchers to quantify tinnitus severity as a criterion for subject selection. That is, self-report measures allow investigators to select only those patients indicating a certain degree of tinnitus severity to be included in a particular study. Minimum and maximum values of the individual’s tinnitus score are defined in the research protocol as inclusion criterion, if it is expected that the treatment under study shows best effects in patients with specific tinnitus severity (see Chap. 22). Furthermore, self-report measures can be used to evaluate the effectiveness of a particular experimental treatment. Even if none of the currently available questionnaires has been specifically designed to be sensitive to treatment-related changes, there is general consensus that questionnaire scores are the best available measures of tinnitus consequence and should be used as primary outcome variables in randomized clinical trials for tinnitus treatment [4, 19].
Table 47.4 gives an overview about the most widely used quantitative tinnitus questionnaires in the English language. In the following discussion, each of these questionnaires is presented in detail. A description of the questionnaire is followed by a short explanation of how the questionnaire is scored and interpreted. Psychometric characteristics of the questionnaire are presented, strengths and weaknesses of the instrument are discussed, and finally it is indicated whether validated translations for the questionnaire are available.
Even if self-report questionnaires have been proven to be useful tools both in the clinical management of tinnitus and in research applications, some caution is advised in their use and interpretation. First, completing a questionnaire might not only measure specific aspects of a patient’s tinnitus but also influence the patient’s tinnitus. Especially, catastrophizing statements may induce or reinforce maladaptive coping strategies (e.g., statements about suicide). Also, statements such as, “I cannot sleep because of my tinnitus,” may induce incorrect attributions. A patient, who repeatedly reads such a statement, may become convinced that his insomnia may be a caused by his tinnitus, which is not necessarily true and might result in incorrect beliefs such as, “as long as I have my tinnitus I will never be able to sleep well.”
Second, it should be considered that self-report questionnaires can be subject to dissimulation or aggravation. Thus, just as a low score cannot exclude a significant impact of the tinnitus on a patient’s life, a high score is not proof of severe suffering. Therefore, questionnaire results always have to be evaluated in the context of the clinical impression and the patient’s tinnitus-related behavior.
Tinnitus Severity Scale (TSS) [20]
The tinnitus severity scale (TSS) aims at quantifying individuals’ cognitive and behavioral responses to tinnitus. The 15 items are categorized under the factors intrusiveness (four items), distress (six items), hearing loss (three items), sleep disturbance (one item), and medication (one item). Responses refer to the past week and range in score from 1 (no impact) to 4 (most impact). Each item is weighted from 1 to 3 points (total weight score = 39 points). The total score is calculated by multiplying each item’s score by its weight and summing these products, resulting in a range between 39 points (39 weighting points × 1-point item score) and 156 points (39 weighting points × 4-point item score). The TSS has acceptable test–retest reliability (r = 0.86). No other psychometric data are available, limiting clinical and research applications. Validated translations of the English scale into other languages are not published.
Subjective Tinnitus Severity Scale (STSS) [21]
The 16-item subjective tinnitus severity scale (STSS) was developed to provide a simple questionnaire to assess tinnitus severity. Each question is answered with either a “yes” or a “no” response. Ten of the 16 items earn a point if the response is “yes” (e.g., “Are you almost always aware of your tinnitus?”), whereas the other six items earn a point if the response is “no” (e.g., “When you are busy, do you quite often forget about your tinnitus?”), summing up to scores between 0 and 16 with higher scores reflecting greater overall severity. A Cronbach’s α of 0.84 indicates high consistency reliability. The validity was established in a sample of 30 patients, where mean STSS scores were found to correlate highly with two independent clinical ratings of severity.
The STSS is extremely simple to administer and score. The lack of a classification scheme for the total score limits its diagnostic use. Furthermore, no data about test–retest reliability are available, limiting its applicability for measuring treatment outcome.
The original questionnaire is in the English language, validated translations in Dutch [22] and French [23] have been published.
Tinnitus Questionnaire (TQ) [24]
The 52-item Tinnitus Questionnaire (TQ) developed by Hallam and colleagues has been designed to measure several dimensions of patients’ tinnitus complaints, namely emotional distress, auditory perceptual difficulties, and sleep disturbance. Questions either relate to the “noises” in the ear as the major cause of distress or reflect lack of coping skills.
Individuals indicate their level of agreement to each statement using one of the three response alternatives: true (2 points), partly true (1 point), or not true (0 points). Affirmative responses to an item (indicated by true) are identified as complaints about tinnitus, with the exception of the items 1, 7, 32, 40, 44, and 49, which are reverse scored because they are considered positive statements. Possible scores range from 0 to 104 points, with higher scores reflecting greater tinnitus complaints.
The TQ instrument has been found to have high internal consistency reliability (Cronbach’s α =.91–.95) and high test–retest reliability (r = .91–.94) [25, 26]. The high test–retest reliability suggests good stability over time.
High correlations were also found between the TQ and measures of tinnitus handicap (Tinnitus Handicap Questionnaire (THQ) [27], tinnitus handicap inventory (THI) [28], and tinnitus distress (TRQ) [29]. Factor analyses conducted in separate populations were consistent with the factors originally identified by Hallam and colleagues in the United Kingdom supporting the instrument’s validity.
The TQ has been found to measure a number of different dimensions of tinnitus complaints and is a stable measure over time. In this connection, the TQ would be useful as an outcome measure in determining the effectiveness of treatment. However, the responsiveness of the TQ to changes has not been evaluated, and no data are available to assist the clinician in determining what is considered a statistically significant or clinically relevant change in scores following intervention for a given patient.
The TQ has been translated into the German language and extensively validated [30–32]. Factor analysis of the German translation of the TQ revealed that the dimensions of emotional and cognitive distress, intrusiveness, auditory perceptual difficulties, sleep disturbances, and somatic complaints can be differentiated [32]. This validation also resulted in a different scoring system, where some items were not used at all and others loaded in two factors, resulting in a maximum score of 84 points. Further translations in Dutch and French are based on the German version [33]. Recently, a Chinese version of the TQ has been validated [34]. Also, a short version of the TQ has been presented in the German language (Mini TQ, [31]), which has also been validated in Portuguese [35]. Furthermore, official translations of the Mini TQ in most European languages are available at http://www.eutinnitus.com/country-selection.php.
Tinnitus Handicap/Support Scale (TH/SS) [36]
The 28-item tinnitus handicap/support scale (TH/SS) assesses the attitudes of significant others toward the person with tinnitus. Three factors were identified, including perceived attitudes or reactions of others (factor 1; 9 items), social support (factor 2; 10 items), and personal and social handicaps (factor 3; 9 items). Each statement on the scale is scored from 1 (strongly disagree) to 5 (strongly agree). The reliability of the TH/SS has not been examined. Construct validity of the TH/SS was assessed using a 10-item Tinnitus Severity Questionnaire (TSQ). This is the only questionnaire that has been designed to assess the influence of significant others in the overall management process, which can be helpful for counseling. The lack of retest reliability data limits both its clinical and its scientific use.
The questionnaire is in the English language and has not been validated in any other language.
Tinnitus Handicap Questionnaire (THQ) [27]
The Tinnitus Handicap Questionnaire (THQ) description has been developed to be broad in scope but sensitive to patients’ perceived degree of tinnitus handicap. By factor analysis, three factors have been differentiated. Factor 1 (15 items) reflects the physical, emotional, and social consequences of tinnitus; factor 2 (8 items) assesses the effects of tinnitus and hearing; and factor 3 (4 items) explores the patient’s view on tinnitus.
For each item, the individual responds with a number between 0 and 100 indicating how much he or she disagrees (0 = strongly disagrees) or agrees (100 = strongly agrees) with the statement. After inverting scores obtained on items 25 and 26 by subtracting them from 100, mean scores can be calculated for the total or for each of the three factors. Higher scores indicate greater handicap.
The THQ demonstrated high internal consistency and reliability for the total scale (Cronbach’s α = 0.95), factor 1 (0.95), and factor 2 (0.88). Factor 3 yielded a low alpha (0.47), which may be due to the small number of items comprising this factor. A similar factor structure has been obtained in Australian [26] and New Zealand [37] samples.
Adequate construct validity of the THQ was documented by relative high correlations (r > 0.50) with perceived tinnitus loudness, life satisfaction, hearing threshold, depression, and general health status. High test–retest correlations have been obtained assessed over a 6-week period for the total score (r = 0.89), factor 1 (r = 0.89), and factor 2 (r = 0.90), whereas factor 3 yielded inadequate retest reliability (r = .50) [38]. Normative data for the THQ are available [27]. The percentile ranking allows determining severity for an individual patient relative to other patients with tinnitus. Comparison of the scores for Factor 1 (emotional and social effects) and Factor 2 (hearing) has been used to guide clinicians in treatment selection (high Factor 1, greater psychological management; high Factor 2, hearing aids [39]).
The 100-point response scale may be relatively sensitive for changes [40], but it may be somewhat problematic, especially for items, dealing with subjective strength of belief.
According to their authors, the THQ is among the most widely used questionnaires [40]. A French translation of the THQ has been validated [41]; official (unvalidated) translations in various languages are available at http://www.uihealthcare.com/depts/med/otolaryngology/clinics/tinnitus/questionnaires/index.html.
Tinnitus Handicap Inventory (THI) [42]
The 25-item Tinnitus Handicap Inventory consists of three subscales. The functional subscale (11 items) evaluates role limitations, the emotional subscale (nine items) reflects affective responses to tinnitus, and the catastrophic subscale (five items) probes the most severe reactions to tinnitus. However, the distinctness of the subscales has been questioned, and the use of only the total score was recommended [43].
For each item of the inventory, the patient responds with “yes” (4 points), “sometimes” (2 points), or “no” (0 points). The responses are summed, with a total score ranging from 0 to 100 points. Higher scores represent greater perceived handicap. Handicap severity categories (0–16: no; 18–36: mild; 38–56: moderate; 58–100: severe) have been developed based on quartiles calculated for the total THI score [44].
The THI has very good internal consistency reliability (Cronbach’s α = 0.93) and high test–retest reliability for the total score (r = 0.92), as well as the subscales (ranging from 0.84 to 0.94). Test–retest reliability assessed on average 20 days after the initial administration was also high for the total score and the three subscales. A 95% confidence interval of 20 points for the total scale suggests that in an individual, a difference of 20 points or more between pre- and post-treatment administration can be considered statistically significant. Convergent validity was assessed using the THQ, whereas construct validity was assessed using the Beck Depression Inventory, Modified Somatic Perception Questionnaire, symptom rating scales (e.g., sleep disturbance, annoyance), and perceived tinnitus pitch and loudness. High convergent validity with the TQ has been demonstrated recently [28].
The THI is briefly and easily administered and scored. It assesses the domains of function that are addressed by many available treatment interventions.
The test–retest data allow clinicians to judge effects of treatment interventions. Further data about retest stability over longer time intervals are desirable in order to evaluate changes in perceived handicap over the medium and long term.
The THI is the most widely used tinnitus questionnaire, as evidenced by the number of citations. Validated translations are published in Danish [45], Spanish [46], Korean [47], Portuguese [48, 49], German [50], Italian [51], and Chinese [52].
In a consensus meeting, the (additional) use of the THI has been recommended for clinical studies in order to facilitate comparability between studies [4].
Tinnitus Reaction Questionnaire (TRQ) [29]
The Tinnitus Reaction Questionnaire has been developed for quantifying the psychological distress associated with tinnitus [29]. The 26 items of the TRQ relate to distress consequences such as anger, confusion, annoyance, helplessness, activity avoidance, and panic.
Each item on the TRQ is scored on a 5-point scale, ranging from 0 to 4 points. The scores are summed with the total score ranging from 0 to 104 points, with higher scores reflecting greater distress.
The TRQ has high internal consistency reliability (Cronbach’s α = .96), as well as test–retest reliability (r =.88). Concerning construct validity, there are moderate to high correlations between the TRQ and clinician ratings and self-reported measures of anxiety and depression. A factor analysis revealed the factor’s general distress, interference, severity, and avoidance.
The TRQ represents an easy clinical tool for assessing tinnitus distress. However, no cut-off values for severity categories are available. High test–retest reliability over a period ranging from 3 days to 3 weeks indicates short-term stability of the TRQ and its usefulness in quantifying treatment outcome, at least for short interventions. However, no data are available about what is considered a statistically significant or a clinically relevant change of the score. A French translation of the TRQ has been validated [23] and compared with the English version, demonstrating only minor effects of language [53].
The Tinnitus Severity Index
The Tinnitus Severity Index is a 12-item questionnaire that measures the effect of tinnitus on work and social activities and overall quality of life [54]. The 12 items of the TSI are totaled for a single severity index. This is one of the shorter tinnitus questionnaires that has been published. There have been two versions of the TSI, the original [54] using 3- and 4-point scales and a modified version using primarily a 5-point scale, with two 4-point questions and one 3-point question [55]. The TSI has had limited use outside of the US, but the original version has been normed in New Zealand as well [37]. The TSI has good internal consistency in both US and NZ (Cronbach’s α > 0.87) populations. The TSI has been found to correlate to the subjective rating of tinnitus loudness but not hearing loss [37]. The TSI and THQ are correlated (r = 0.77, p < 0.05), suggesting that each questionnaire is measuring similar, but not exactly the same, elements of tinnitus [37]. The TSI scores have been shown to improve following comprehensive audiology-based tinnitus management programs [56, 57], and use of SSRIs has improved scores [58]. Persons with tinnitus following head injuries have greater TSI scores than those whose tinnitus develops from other injuries [59].
The Tinnitus Handicap Questionnaire (Tinnitus Beeinträchtigungs Fragebogen; TBF-12)
Based on the Tinnitus Handicap Inventory (THI) [42], a short version in German language has been developed [60]. The number of items was reduced based on rigorous psychometrical testings. The final German version encompasses 12 items and distinguishes between the factors emotional cognitive (items 3, 4, 6, 8, 10, 11, and 12) and functional communicative impairments (items 1, 2, 5, 7, 9).
The internal consistency reliability of the TBF is high (Cronbach’s α = 0.90). The TBF-12 is easy to understand and administer, psychometrically robust, and well suitable as a screening instrument in primary care. The TBF-12 is currently used as the primary outcome measure for evaluation of the efficacy of a pharmacologic compound in phase III trials. In case the trials will be positive and the compound will be approved by the Food and Drug Administration (FDA) or the European Agency for the Evaluation of Medical Products (EMEA), it will set a standard for further drugs to be approved. In the context of the phase III trial, the questionnaire has been translated and linguistically evaluated in Spanish, Dutch, French, Portuguese, Czech, Spanish, Polish, and English, as well as in African languages.
Tinnitus Cognitions Questionnaire (TCQ) [61]
In contrast to the scales assessing distress, disability, or handicap, the Tinnitus Cognitions Questionnaire (TCQ) focuses on the patient’s reaction to tinnitus from a cognitive perspective. The 26 items assess positive and negative thoughts associated with tinnitus [61], especially important in the context of the psychological management of tinnitus. The TCQ consists of 13 negative items and 13 positive items, which are clearly separated. Each of the items is rated on a five-point scale (0–4). The negative items (1–13) are scored 0–4, whereas the positive items (14–26) are reverse scored, 4–0. The addition of the item scores reveals the total TCQ score, which can range from 0 to 104, with higher scores reflecting a tendency toward more negative and less positive thoughts in response to tinnitus.
The TCQ yielded both good test–retest reliability (r = .88) and internal consistency
reliability (Cronbach’s α = .91). A factor analysis revealed that the negative and positive cognitions represent independent factors. Construct and convergent validity was assessed between the TCQ-total, TCQ-positive, and TCQ-negative scores, as well as other measures of tinnitus-specific symptomatology (e.g., distress, handicap, complaint behavior), depression, automatic thoughts, and loss of control. The TCQ showed moderate correlations with other tinnitus-related measures (i.e., TRQ, THQ, and TQ), with the TCQ-negative subscale demonstrating higher correlations with each of the tinnitus- and non-tinnitus measures.
The TCQ is different from other questionnaires by focusing on cognitive responses in individuals with tinnitus. The information gleaned from the TCQ responses is especially useful in the context of cognitive–behavioral therapy for screening or stratifying patients, but also for outcome measurement. However, the latter requires data about test–retest reliability. It has to be considered that reporting about cognitions or thoughts may not be identical to engaging in these thoughts. No validated translations of the instrument have been published.
Tinnitus Coping Style Questionnaire (TCSQ) [62]
The Tinnitus Coping Style Questionnaire (TCSQ) is a 33-item scale developed to assess adaptive and coping strategies and consists of two factors [62]. Eighteen items comprise the maladaptive coping factor; the other fifteen items comprise the effective coping subscale.
For each item, the patient indicates how frequently he/she employs each of the coping strategies on a1 (“never”) to 7 (“always”) scale. Higher scores on the maladaptive coping subscale reflect poorer coping skills, whereas higher scores on the effective coping dimension are characterized by better acceptance of the tinnitus and use of a broad range of adaptive coping skills.
The internal consistency reliability values for the maladaptive coping and effectiveness coping subscales were 0.90 and 0.89, respectively. The two subscales were not significantly correlated (r = 0.13). Maladaptive coping strategies were significantly associated with measures of tinnitus severity, depression, and anxiety. In contrast, effective coping was not correlated with any of the tinnitus adjustment measures [62].
The TCSQ is specifically focused on coping strategies used by tinnitus sufferers. Information obtained with the TCSQ is fundamental in developing a cognitive–behavioral therapy program. After probing test–retest reliability of the instrument, the TSCQ might also be suitable for monitoring changes during cognitive– behavioral therapy.
Other Questionnaires
Beside tinnitus-related questionnaires, several other instruments referring to different comorbid conditions may be useful as part of a broad assessment of the patient and their problems. A large variety of self-report questionnaires are available for assessing depression, anxiety, sleep disorders, or health-related quality of life. A detailed description of these questionnaires is beyond the scope of this chapter. In general, these instruments are not necessary for basis assessment in every patient but may be helpful in specific cases.
VAS Scales
Rating scales (visual analogue scales or Likert-type scales/numerical rating scales) can be used for assessing different characteristics of tinnitus, such as loudness or annoyance. Examples for such scales are given in Fig. 47.3. Rating scales are easy to understand, but sometimes patients report difficulties, because generally the maximum end of the scale is only very vaguely defined.
Apart from loudness and annoyance, other qualitative features of tinnitus can also be easily assessed with rating scales (e.g., intrusiveness or ability to ignore tinnitus). This can provide an opportunity to understand what the most important problem is for a given patient and may lead to the use of more individually tailored assessment and monitoring tool, such as tinnitus diaries or tinnitus protocols.
A big advantage of rating scales is that they are fast to perform and can be repeated easily, e.g., in the form of tinnitus protocols. Unfortunately, there is limited psychometric data for visual analogue and numeric rating scales. One recent study shows that in individuals with tinnitus who do not seek medical attention, loudness rating scores are much lower than in those who seek help for their tinnitus [63]. It has also been shown that results of visual analogue loudness scale correlate with the THI scores (r = 0.56) [64].
Tinnitus Protocols
Tinnitus protocols are self-report instruments for assessing different aspects of tinnitus over time. As an example, tinnitus loudness, annoyance, mood, and stress can be assessed daily, and results can be displayed in a diagram (see Fig. 47.4).
A tinnitus protocol can be an appropriate tool to examine changes of different tinnitus aspects over time, and correlations between intensity of tinnitus (e.g., loudness, annoyance) and different psychobehavioral factors such as mood or stress. This allows, for example, the detection of triggers or rhythmic changes over time. As shown in the example in Fig. 47.3, such a protocol can reveal that mood and stress are correlated closer to tinnitus annoyance than loudness. By monitoring different parameters over a certain period of time, the patient can learn that it is not just the noise that borders them but other emotional, cognitive, and behavioral factors that influence tinnitus perception and reaction. This can be helpful to motivate patients for cognitive–behavioral therapy.
Conclusion
There are different forms of tinnitus that require specific management. The intake interview is of highest importance for obtaining comprehensive information about the patient’s tinnitus in order to be able to make an exact diagnosis. Collected information from the interview, observation of the patient, and the various self-report scales should enable the clinician to formulate a view about the nature of the tinnitus, its time course, its perceptual characteristics, its comorbidities, the difficulties experienced by the patient, the person’s coping strategies, loudness the consequences of the tinnitus for the person’s life. Based on all these information, a specific treatment program may be developed, which is likely to be effective for an individual patient.
References
Meikle, MB, Vernon, J, Johnson, RM. The perceived severity of tinnitus Some observations concerning a large population of tinnitus clinic patients. Otolaryngol Head Neck Surg, 1984;92(6):689–96
Jakes, SC, Hallam, RS, Chambers, C, Hinchcliffe, R. A factor analytical study of tinnitus complaint behaviour. Audiology, 1985;24(3):195–206
Stouffer, JL, Tyler, RS. Characterization of tinnitus by tinnitus patients. J Speech Hear Disord, 1990;55(3):439–53
Langguth, B, Goodey, R, Azevedo, A, Bjorne, A, Cacace, A, Crocetti, A, et al. Consensus for tinnitus patient assessment and treatment outcome measurement: Tinnitus Research Initiative Meeting, Regensburg, 2006. Prog Brain Res, 2007;166:525–36
Henry, JA, Jastreboff, MM, Jastreboff, PJ, Schechter, MA, Fausti, SA. Assessment of patients for treatment with tinnitus retraining therapy. J Am Acad Audiol, 2002;13(10):523–44
Hoffman HJ, Reed GW. Epidemiology of tinnitus. In: Snow JB, editor. Tinnitus: Theory and Management. London: BC Ker, 2004;16–41
Coelho, CB, Sanchez, TG, Tyler, RS. Tinnitus in children and associated risk factors. Prog Brain Res, 2007;166:179–91
Sand, PG, Langguth, B, Kleing, T, Eichhammer. Genetics of chronic tinnitus. Prog Brain Res, 2007;166:159–68
De Ridder, D, van der Loo, E, Van der Kelen, K, Mesky, T, Van de Heyning, P, Møller, A. Do tonic and burst TMS modulate the lemniscal and extralemniscal system differentially? Int J Med Sci, 2007;4(5):242–6
De Ridder, D, van der Loo, E, Van der Kelen, K, Mesky, T, Van de Heyning, P, Møller, A. Theta, alpha and beta burst transcranial magnetic stimulation: brain modulation in tinnitus. Int J Med Sci, 2007;4(5):237–41
Hiller, W, Goebel, G. Factors influencing tinnitus loudness and annoyance. Arch Otolaryngol Head Neck Surg, 2006;132(12):1323–30
Hyde, ML. Reasonable psychometric standards for self-report outcome measures in audiological rehabilitation. Ear Hear, 2000;21(4 Suppl):24 S–36 S
Ventry IM, Schiavetti N. Evaluating Research in Speech Pathology and Audiology. Reading, MA: Addison Wesley, 1980
Kirshner, B, Guyatt, G. A methodological framework for assessing health indices. J Chronic Dis, 1985;38(1):27–36
Meikle, MB, Stewart, BJ, Griest, SE, Tin, WH, Henry, JA, Abrams, HB, et al. Assessment of tinnitus: measurement of treatment outcomes. Prog Brain Res, 2007;166:511–21
Searchfield GD, Jerram C. Tinnitus assessment. In: Searchfield GD, Goodey R, editors. Tinnitus Discovery: Asia Pacific Tinnitus Symposium, 2010
Biesinger, E, Heiden, C, Greimel, V, Lendle, T, Hoing, R, Albegger, K. Strategies in ambulatory treatment of tinnitus. HNO, 1998;46(2):157–69
Langguth, B, Kleing, T, Fischer, B, Hajak, G, Eichhammer, P, Sand, PG. Tinnitus severity, depression, and the big five personality traits. Prog Brain Res, 2007;166:221-5
Dobie, RA. A review of randomized clinical trials in tinnitus. Laryngoscope, 1999;109:1202–11
Sweetow, RW, Levy, MC. Tinnitus severity scaling for diagnostic/therapeutic use. Hear Instrum, 2009;41:20–46
Halford, JB, Anderson, SD. Tinnitus severity measured by a subjective scale, audiometry and clinical judgement. J Laryngol Otol, 1991;105(2):89–93
van Veen, ED, Jacobs, JB, Bensing, JM. Assessment of distress associated with tinnitus. J Laryngol Otol, 1998;112(3):258–63
Meric, C, Pham, E, Chery-Croze, S. Validation of French translation of the “Tinnitus Reaction Questionnaire”, Wilson et al 1991. Encephale, 1997;23(6):442–6
Hallam, RS, Jakes, SC, Hinchcliffe, R. Cognitive variables in tinnitus annoyance. Br J Clin Psychol, 1988;27(Pt 3): 213–22
Hallam RS. Manual of the Tinnitus Questionnaire. London: The Psychological Corporation/Harcourt Brace, 1996
Henry, JL, Wilson, PH. The psychometric properties of two measures of tinnitus complaint and handicap. Int Tinnitus J, 1998;4(2):114–21
Kuk, FK, Tyler, RS, Russell, D, Jordan, H. The psychometric properties of a tinnitus handicap questionnaire. Ear Hear, 1990;11(6):434–45
Baguley, DM, Humphriss, RL, Hodgson, CA. Convergent validity of the tinnitus handicap inventory and the tinnitus questionnaire. J Laryngol Otol, 2000;114(11):840–3
Wilson, PH, Henry, J, Bowen, M, Haralambous, G. Tinnitus reaction questionnaire: psychometric properties of a measure of distress associated with tinnitus. J Speech Hear Res, 1991;34(1):197–201
Goebel, G, Hiller, W. The tinnitus questionnaire A standard instrument for grading the degree of tinnitus. Results of a multicenter study with the tinnitus questionnaire. HNO, 1994;42:166–72
Hiller, W, Goebel, G, Rief, W. Reliability of self-rated tinnitus distress and association with psychological symptom patterns. Br J Clin Psychol 1994;33(Pt 2):231–9
Hiller, W, Goebel, G. A psychometric study of complaints in chronic tinnitus. J Psychosom Res, 1992;36(4):337–48
Meeus, O, Blaivie, C, Van de, HP. Validation of the Dutch and the French version of the Tinnitus Questionnaire. B-ENT, 2007;3(Suppl 7):11–7
Kam, AC, Cheung, AP, Chan, PY, Leung, EK, Wong, TK, Tong, MC, et al. Psychometric properties of a Chinese (Cantonese) version of the Tinnitus Questionnaire. Int J Audiol, 2009;48(8):568–75
Cerejeira, R, Cerejeira, J, Paiva, S, Goncalves, P, Firmino, H, Quartilho, M, et al. The Portuguese version of Mini-Tinnitus Questionnaire: brief screening test for assessment of tinnitus-induced stress. Otol Neurotol, 2009;30(1):112–5
Erlandsson, SI, Hallberg, LR, Axelsson, A. Psychological and audiological correlates of perceived tinnitus severity. Audiology, 1992;31(3):168–79
Searchfield, GD, Jerram, C, Wise, K, Raymond, S. The impact of hearing loss on tinnitus severity Australian and New Zealand. J Audiol 2007;29:67–76
Newman, CW, Wharton, JA, Jacobson, GP. Retest stability of the tinnitus handicap questionnaire. Ann Otol Rhinol Laryngol, 1995;104(9 Pt 1):718–23
Searchfield GD. Hearing aids and tinnitus. In: Tyler R, editor. Tinnitus: Treatment. New York: Thieme, 2007;161–75
Tyler, RS, Oleson, J, Noble, W, Coelho, C, Ji, H. Clinical trials for tinnitus: study populations, designs, measurement variables, and data analysis. Prog Brain Res, 2007;166:499–509
Meric, C, Pham, E, Chery-Croze, S. Translation and validation of the questionnaire Tinnitus Handicap Questionnaire, 1990. J Otolaryngol, 1997;26(3):167–70
Newman, CW, Jacobson, GP, Spitzer, JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg, 1996;122(2):143–8
Baguley, DM, Andersson, G. Factor analysis of the Tinnitus Handicap Inventory. Am J Audiol, 2003;12(1):31–4
Newman, CW, Sandridge, SA, Jacobson, GP. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am Acad Audiol, 1998; 9(2):153–60
Zachariae, R, Mirz, F, Johansen, LV, Andersen, SE, Bjerring, P, Pedersen, CB, Reliability and validity of a Danish adaptation of the Tinnitus Handicap Inventory, Scand Audiol, 2000;29(1):37–43
Herraiz, C, Hernandez, CJ, Plaza, G, Tapia, MC, de los, SG. Disability evaluation in patients with tinnitus. Acta Otorrinolaringol Esp, 2001;52(6):534–8
Kim, JH, Lee, SY, Kim, CH, Lim, SL, Shin, JN, Chung, WH, et al. Reliability and validity of a Korean adaptation of the Tinnitus Handicap Inventory. Korean J Otholaryngol, 2002;45:328–34
Paula Erika, AF, Cunha, F, Onishi, ET, Branco-Barreiro, FC, Gananca, FF. Tinnitus Handicap Inventory: cross-cultural adaptation to Brazilian Portuguese. Pro Fono, 2005;17(3):303–10
Dias, A, Cordeiro, R, Corrente, JE. Tinnitus annoyance assessed by the tinnitus handicap inventory. Rev Saude Publica, 2006;40(4):706–11
Kleing, T, Fischer, B, Langguth, B, Sand, PG, Hajak, G, Dvorakova, J, et al. Validation of the German-Version Tinnitus Handicap Inventory (THI). Psychiatr Prax, 2007;34(S1):140–2
Monzani, D, Geese, E, rara, A, Gherpelli, C, Pingani, L, Forghieri, M, et al. Validity of the Italian adaptation of the Tinnitus Handicap Inventory; focus on quality of life and psychological distress in tinnitus-sufferers. Acta Otorhinolaryngol Ital, 2008;28(3):126–34
Kam, AC, Cheung, AP, Chan, PY, Leung, EK, Wong, TK, van Hasselt, CA, et al. Psychometric properties of the Chinese (Cantonese) Tinnitus Handicap Inventory. Clin Otolaryngol, 2009;34(4):309–15
Meric, C, Pham, E, Chery-Croze, S. Validation assessment of a French version of the tinnitus reaction questionnaire: a comparison between data from English and French versions. J Speech Lang Hear Res, 2000;43(1):184–90
Meikle, MB, Griest, S, Stewart, BJ, Press, LS. Measuring the negative impact of tinnitus: A brief severity index. Abstr Midwinter Res Meet Assoc Res Otolaryngol, 1995;18:167
Folmer, RL, Carroll, JR. Long-term effectiveness of ear-level devices for tinnitus. Otolaryngol Head Neck Surg, 2006;134(1):132–7
Folmer, RL. Long-term reductions in tinnitus severity. BMC Ear Nose Throat Disord, 2002;2(1):3
Henry, JA, Schechter, MA, Zg, TL, Griest, S, Jastreboff, PJ, Vernon, JA, et al. Outcomes of clinical trial: tinnitus masking versus tinnitus retraining therapy. J Am Acad Audiol, 2006;17(2):104–32
Folmer, RL, Shi, YB. SSRI use by tinnitus patients: interactions between depression and tinnitus severity. Ear Nose Throat J, 2004;83(2):107–8, 110, 112
Folmer, RL, Griest, SE. Chronic tinnitus resulting from head or neck injuries. Laryngoscope, 2003;113(5):821–7
Greimel, KV, Leibetseder, M, Unterrainer, J, Albegger, K. Can tinnitus be measured? Methods for assessment of tinnitus-specific disability and presentation of the Tinnitus Disability Questionnaire. HNO, 1999;47(3):196–201
Wilson, PH, Henry, JL. Tinnitus cognitions questionnaire: development and psychometric properties of a measure of dysfunctional cognitions associated with tinnitus. Int Tinnitus J, 1998;4(1):23–30
Budd, RJ, Pugh, R. Tinnitus coping style and its relationship to tinnitus severity and emotional distress. J Psychosom Res, 1996;41(4):327–35
Demeester, K, Van, WA, Hendrickx, JJ, Topsakal, V, Fransen, E, Van, LL, et al. Prevalence of tinnitus and audiometric shape. B-ENT, 2007;3(Suppl 7):37–49
Figueiredo, RR, Azevedo, AA, Oliveira, PM. Correlation analysis of the visual-analogue scale and the Tinnitus Handicap Inventory in tinnitus patients. Braz J Otorhinolaryngol, 2009; 75(1):76–9
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Langguth, B., Searchfield, G.D., Biesinger, E., Greimel, K.V. (2011). History and Questionnaires. In: Møller, A.R., Langguth, B., De Ridder, D., Kleinjung, T. (eds) Textbook of Tinnitus. Springer, New York, NY. https://doi.org/10.1007/978-1-60761-145-5_47
Download citation
DOI: https://doi.org/10.1007/978-1-60761-145-5_47
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-60761-144-8
Online ISBN: 978-1-60761-145-5
eBook Packages: MedicineMedicine (R0)