Abstract
Stress-induced alterations in sleep have been linked to the development of post-traumatic stress disorder (PTSD), and sleep complaints and disturbances in arousal are continuing symptoms in patients. PTSD-related changes in sleep have not been fully characterized but appear to involve persistent disturbances in both rapid eye movement (REM) and non-REM (NREM). Intense conditioned fear training, which may model PTSD in rodents, can produce reductions in REM without recovery as well as significant alterations in NREM that may vary with mouse and rat strains. These variants of conditioned fear paradigms and strain differences have not been fully exploited, but they appear to hold promise for modeling responses to stress that may provide insight into the role sleep plays in the neurobiology of PTSD. The amygdala and corticotropin-releasing hormone (CRH) play significant roles in regulating the stress response and have been implicated in PTSD. Recent work suggests that the amygdala and CRH may also play roles in regulating stress-induced changes in arousal and sleep. This chapter reviews the effects of stress on sleep with a specific emphasis on factors that may be important in modeling PTSD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Stress can have a significant, long-lasting negative impact on health (1), and severe stress has been linked to the genesis of post-traumatic stress disorder (PTSD) and other anxiety and mood disorders. However, stressors are commonly encountered in daily life without producing permanent or pathological changes. Even the traumatic life events that can give rise to PTSD do so in only a percentage of the population (2,3), whereas the majority may cope with similar situations with only transitory effects. The difference between successful and unsuccessful coping with stress and whether it has transitory or lasting effects can vary with characteristics of the stressful event, including its duration, intensity (4), predictability (5), and controllability (6). The effects also may involve individual differences in resilience and vulnerability to stressful events (7).
Stress-related conditioning processes are thought to play significant roles in the development of anxiety disorders (8,9) and thus provide a significant pathway by which traumatic events can produce lasting changes in behavior. Specifically, fear conditioning is thought to play a significant role in the development of PTSD (10,11). However, it is important to note that conditioned fear also can underlie adaptive behavior that typically is extinguished when the fear-inducing situation is removed. Fear “extinction” is considered a type of new learning that inhibits subsequent fear without erasing the original memory for fear conditioning (12). It is the failure of extinction that has been linked to persisting symptoms of PTSD (13).
Stress also has an impact on sleep, and traumatic life events virtually always produce at least temporary sleep disturbances that may include insomnia or subjective sleep problems (14). The persistence of sleep disturbances after a traumatic event may be predictive of future development of emotional and physical disorders (14). Sleep disturbances are also a core feature of PTSD, and insomnia is the most common grievance (15). PTSD also is characterized by disturbed REM, hypervigilance to unfamiliar stimuli, and stereotypical anxiety dreams (16,17). These factors suggest that disturbed sleep may be involved in the development of PTSD as well as being one of its persisting symptoms, and that determining how the sleep and arousal system are impacted by stressful events could lead to new avenues for understanding and treating stress-related disorders, including PTSD.
Our work over the last several years has focused on examining the effects of stress on sleep using a variety of stress paradigms but primarily aimed at understanding the effects of stress-related learning and stressful memories on sleep using variations of conditioned fear and other stress-motivated paradigms. We have also examined the role of the amygdala, a region strongly implicated in the regulation of stress and in PTSD, in regulating spontaneous and stress-induced alterations in arousal and sleep. In this chapter, we provide a general overview of the relationship between stress and sleep and its regulation by the amygdala, with a primary focus on our work and that of others examining the effects of fear conditioning on sleep. However, the relationship between stress and sleep as they relate to PTSD and other stress-related disorders is a significantly understudied problem, and current work, including our own, has a number of weaknesses in adequately modeling the effects of stress on sleep as it relates to the development of stress-related disorders. These are also discussed.
Sleep Disturbances in Post-Traumatic Stress Disorder
The nature of the sleep disturbance in patients with PTSD has been reviewed (16,17), and we only briefly address the topic here. Much of the work on sleep disturbances in PTSD has focused on REM, and some early polysomnographic studies reported a heightened tendency to enter and remain in REM in patients with PTSD. Among these studies, Greenberg, Pearlman, and Gampel (18) reported shortened REM latency (time from sleep onset to the first REM period) and increased REM density (number of rapid eye movements/total REM time) in Vietnam veterans with “war neurosis,” and van der Kolk, Blitz, Burr, Sherry, and Hartmann reported increased REM percentage (total REM time/total sleep time) in a group of elderly ex-prisoners of war with PTSD (19). Other early studies reported reduced REM in PTSD (e.g., 20).
Ross et al. (21,22) found abnormalities in the internal structure of REM rather than in the amount of REM in patients with combat-related PTSD. Tonic REM measures, indications of physiological processes that occur continuously throughout an REM period, showed internight variability and did not reliably discriminate PTSD patients from normal control subjects. However, measures of REM phasic events, exemplified by REM density, were elevated in PTSD compared to control subjects on the adaptation night and on two subsequent recording nights. Other researchers (e.g., 23,24) have observed increased REM density in PTSD patients; however, increased REM density was also found in patients with both PTSD and major depression and with depression alone compared to healthy controls.
Mellman et al. (25,26) have made the point that studies conducted months, years, or even decades after the traumatic event may be influenced by factors not related to the development of PTSD, and few studies have examined sleep in the initial stages of PTSD. One early polysomnographic study (20) of three patients hospitalized for “acute combat fatigue” reported that sleep was reduced in duration and consisted primarily of stage 2 sleep with an absence of stage 4 sleep. REM episodes were described as “rare and short.” The electromyograph (EMG) was reported as usually high, with numerous body movements and bursts of tachycardia occurring during the night. However, even this study was potentially influenced by other factors as the patients had experienced chronic partial sleep deprivation before they experienced a breakdown prior to the sleep studies being conducted (20).
Mellman and his colleagues (25,26) conducted more extensive polysomnographic studies within a month of the traumatic experience. These studies generally found a more fragmented pattern of REM characterized by shorter average duration REM episodes before shifting stage or awakening in PTSD patients compared to patients without PTSD and a nontraumatized comparison group. There was also a greater number of REM sleep episodes in the PTSD patients than in patients who experienced trauma without developing PTSD. These findings led Mellman et al. to speculate that intact REM may perform an adaptive function in aiding in the processing of the memory for trauma. We also have suggested that REM may play an adaptive function in recovery from stress in our work with animals (27).
The findings of changes in NREM in PTSD have also been emphasized. Specifically, both visually scored delta sleep and electroencephalographic (EEG) delta amplitude are reduced in patients with PTSD (reviewed in 16). Neylan, Otte, Yehuda, and Marmar (16) suggested that the changes in NREM and delta may involve persistent increases in corticotropin-releasing hormone (CRH) activity coupled with either enhanced negative feedback or downregulated CRH receptors. Taken together, the studies on sleep in PTSD patients suggest that that it will be important to determine alterations in REM and NREM as well as microarchitectural changes in each state to fully understand the changes in sleep that occur after traumatic stress.
Effects of Stress on Sleep in Animals
Animal experiments have repeatedly demonstrated that stressful experiences during wakefulness can have a significant impact on subsequent sleep. Sleep has been recorded after a great number of stressors, including avoidable foot shock (28), restraint (29,30), water maze (31), exposure to novel objects (32), open field (33,34), ether exposure (35), cage change (33,34), and social stress (36). This work provides descriptive data of the effects of a variety of stressors on sleep and demonstrates that the extent of the changes in arousal and sleep varies with the type and intensity of stressor that is used. Exposure to these stressors typically induces a stress-induced period of arousal (37) followed by subsequent rebound sleep (increases in REM or NREM) that occur at various latencies after the stressor is removed. REM appears to be particularly susceptible to the effects of stress, and an initial decrease in REM is observed in response to all stressors (presented in the light-on sleep period) of which we are aware.
While there are many unanswered questions regarding the relationship between sleep and the development of PTSD in humans, the rebound REM or NREM found after various stressors is not consistent with the decreased REM and decreased delta sleep reported in PTSD patients after the initial traumatic stressor is no longer experienced. The rebound sleep also occurs in response to relatively mild stressors that animals may experience repeatedly, thus suggesting that this sleep response to a stressor is not indicative of developing pathology. An example of a repeated mild stressor is the routine cage changes that experimental animals experience as part of normal husbandry and that produce significant alterations in their sleeping and living environments. The stress induced by cage change may be related to fear and novelty (38), a view supported by behavioral and physiological observations, including increased rearing and grooming, increased exploratory behavior, and increased heart rate and blood pressure in rats after a cage change (38). These responses are consistent with recurring cage changes in animals on weekly change schedules, suggesting that the animals do not habituate over time (38).
Another example of a mild stressor is open-field exposure, which is thought to produce anxiety and an opportunity for exploration. Sleep after exposure to an open field also is characterized by an initial decrease followed by an increase in REM (33). We showed that the increases in REM are positively correlated to the amount of exploration in the open field in mice (33), which we have suggested may reflect an adaptive process of small rodents as they cope with potential challenges posed by a new environment (33). Thus, poststress increases in REM and sleep, in general, may play a positive functional role in responses to stressors that are experienced during wakefulness.
Stress, Sleep, and The Development of PTSD
The preceding discussion reveals some of the more significant problems in studying the effects of stress on sleep in animals with respect to modeling the development of PTSD. That is, there is a paucity of data describing the immediate and short-term effects of traumatic stress on sleep in humans, and the relationship of sleep disturbances to the development of PTSD is not fully known. It is also not known whether the initial stress-induced alterations in sleep are the same as those that occur in later stages of PTSD or how they may be modified over time by subsequent life experiences. In addition, work in animals has generally focused on acute stress manipulations and their immediate effects on sleep. Potential longer-term changes in sleep and their relationship to behaviors indicative of PTSD have received much less attention. These factors suggest that refinement is needed in the way that stress and sleep are studied if successful models are to be developed.
Stressors may be defined as stimuli that disrupt homeostasis (39), whereas the stress response is an attempt by the organism to restore homeostasis (37). In a review, Yehuda and LeDoux (2) emphasized that understanding the neurobiology of PTSD will require examining “atypical” responses to stress as well as determining individual differences in pre- and post-traumatic risk factors related to the genesis of PTSD and to the failure to restore physiological homeostasis. Obvious corollaries of these requirements are the need to understand normal responses to stressors as well as how the stress response may normally vary among individuals in order to identify those that are atypical.
We have suggested that the subsequent increases in sleep after many stressors may reflect restoration of homeostasis as the stress response follows its normal course (27). If this hypothesis is true, identifying either stressful situations or individual responses to those situations characterized by lack of recovery REM and abnormal changes in NREM compared to those reported after many stressors may reflect the failure of the stress response to restore homeostasis and may thus be a factor in the development of pathology. This also would be consistent with findings of decreased REM (20,25,26) and abnormalities in NREM (16) in PTSD patients.
Genetic differences are an important factor in the development of stress-related pathology as approximately 20–30% of individuals who experience traumatic events may develop PTSD, whereas others do not appear to suffer significant long-lasting effects (3,40). A few attempts to develop animal models that better represent individual differences in clinical populations have included selecting low and high responders to stressors in outbred rat strains (3,41). Examining individual differences has not often been considered in animal studies of stress and sleep or of sleep in general (42). An approach we have taken is to compare inbred strains, which are genetically identical within strain but that vary genetically and phenotypically across strain, to identify animals that vary in level of responsiveness to conditioned fear and other stressors. Our work in mice and rats has demonstrated that strains that exhibited greater anxiety-like behaviors in response to challenges in wakefulness exhibited correspondingly greater and longer duration alterations in sleep after training with inescapable shock and after fearful cues (43) and contexts (44). In general, more “anxious” mouse strains also showed greater decreases in sleep in situations with unlearned responses, including after exposure to an open field (33), after cage change, and after novel objects placed in the home cage (32). These findings led us to suggest that mouse strains that have greater emotional responses when faced with various types of environmental challenges also have greater reductions in subsequent sleep (32,33).
The following section describes work examining the effects of conditioned fear on sleep and some variants of the paradigm that show promise for producing alterations in sleep that differ from those seen with many of the stressors that have been examined.
Conditioned Fear and Alterations in Sleep
The conditioned fear paradigm is a classical conditioning procedure in which an association is formed between an explicit neutral stimulus (generally a light or auditory stimulus) or situational context and an aversive stimulus (usually foot shock). In typical experiments, the light or auditory stimulus serves as an initially emotionally neutral conditioned stimulus (CS) and the foot shock as an aversive unconditioned stimulus (US). Through pairing of the CS and US, an association is made, resulting in the previously neutral CS having fear-inducing qualities similar to those of the US and producing similar physiologic outcomes. Studies on conditioned fear have typically measured immediate responses to fearful cues or contexts or their effects on modifying responses to other stimuli. Thus, responses such as behavioral freezing (absence of all movement except respiration) (e.g., 45) and fear-potentiated startle amplitude are well established, as are the effects on a variety of physiological signals indicative of fear (reviewed in 46). The resemblance of the behavioral effects of fear conditioning to the symptoms of anxiety and other affective disorders has led to fear conditioning being an important model for examining how stressful and fearful memories can have an impact on behavior, and it is of particular interest as a factor in the development of anxiety disorders, including PTSD (1,6)
The effects of fear conditioning on sleep have received attention only in the last few years. A few studies have examined the relationship between conditioned fear and sleep, with the goal of understanding the potential role of sleep in fear memory consolidation. These studies have typically used training procedures with single, or at most a few, tone-shock or context-shock pairings as this type of paradigm may be more conducive to studies of memory consolidation (47). For example, with a single-shock presentation procedure, Graves, Heller, Pack, and Abel (47) found that total sleep deprivation performed by a gentle handling procedure impaired memory consolidation for contextual fear when sleep was deprived from 0 to 5 h after training but had no effect when sleep was deprived from 5 to 10 h after training. Cued fear was not altered by sleep deprivation in either time window. More recently, Hellman and Abel (48) found that NREM was increased by approximately 1 h over the 24 h after training in fear-conditioned mice compared to those exposed to conditioning stimuli without shock or to an immediate shock treatment that did not produce conditioned fear. In addition, mice experiencing conditioning stimuli alone had more delta power during NREM, whereas those receiving fear conditioning had less theta power during REM. An important point made by Hellman and Abel is that even a single trial of conditioned fear can produce alterations in sleep and EEG spectra that can persist for up to 24 h, whereas the behavioral effects (e.g., freezing) are much more transitory.
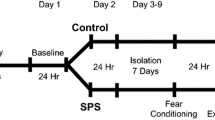
The studies described above suggested that sleep plays a role in the consolidation of fear memory. As conditioned fear typically extinguishes when the fear-inducing situation is removed, it is unlikely that brief, stressful experiences will produce the lasting changes necessary for the development of persisting changes in behavior. Indeed, the studies described above used training procedures with mild or brief foot shock stress and induced fear responses that typically are readily extinguishable with reexposure to the CS without reoccurrence of the US. By comparison, our own work is aimed at modeling and understanding how stress-related learning and memories can lead to persistent changes in behavior that are resistant to extinction and the potential role that stress-induced alterations in sleep play in those changes. As such, we have used training procedures with multiple-shock presentations and are beginning to examine the role of other stress parameters such as shock intensity and controllability in the persisting effects of stress. Thus, a distinction should be made between the procedures used in studies examining the relationship between sleep and fear memory consolidation and the procedures of studies aimed at understanding the lasting effects of traumatic stressors for which the memories are resistant to extinction.
The models we use have similarities to learned helplessness in that mice or rats are placed in a situation in which they repeatedly receive inescapable foot shock and cannot learn an adaptive response. In learned helplessness, rats exposed to inescapable foot shock later fail to learn an escape response in a situation for which their actions could let them avoid foot shock (reviewed in 49). These rats also may respond more anxiously in behavioral anxiety tests, and they may have greater responses to drugs of abuse. The training portion of the paradigm we use is essentially identical to training in learned helplessness with the difference that we usually do not test for performance on other tests. Instead, the animal is “reminded” of the shock situation in a manner similar to testing in cued or contextual fear; most importantly, we record the EEG and EMG as well as other physiological indicators across conditions. This gives a continual readout of changes in the animal's behavioral state after experiencing the stressor. This continual readout in the form of sleep and wake states and EEG spectra provides indicators of the longer-term effects of stress that may reflect the successful or unsuccessful resolution of the stress response and could ultimately provide predictors for changes in sleep involved in the development of PTSD.
Adrien, Dugovic, and Martin (50) provided the first report, of which we are aware, that examined the effects of learned helplessness training on sleep. In their study, rats were presented with 60 inescapable foot shocks of relatively high intensity (0.8 mA) and duration (15 s) over the course of 1 h. Compared to handling control rats that experienced the shock chamber without receiving foot shock, rats trained with inescapable shock showed greater REM latency, and during the first 3 h after training, shock-trained rats also showed reduced REM and increased light NREM compared to the control group and their own baseline sleep. Afterward, REM returned to control amounts, but no REM rebound was observed in recordings that night or the following day. Light NREM also was enhanced over the dark period recordings. This suggests that this paradigm results in significant differences in poststress sleep compared to most stressors described in the literature.
Our work with multitrial shock training procedures also has found significant posttraining alterations in sleep architecture in mice (43,44) and rats (27), although to date we have typically used less-intense shock of shorter duration. The most important outcome of this work has been the demonstration that cues and contexts associated with the foot shock can produce changes in sleep that are directionally similar to those produced when foot shock is presented. Thus, fear-conditioned stimuli (reminders of the shock) can produce significant changes in sleep similar to those when the foot shock stressor was presented just as they can produce the more immediate signs of fear that have been amply demonstrated.
In mice, multiple-shock training trials in both cued (43) and contextual (44) fear produced significant reductions in REM that can occur without recovery, and similar reductions without recovery can be seen with subsequent presentation of the fearful cue and fearful context. Hourly plots of NREM and REM amounts demonstrating this effect for cued fear in BALB/cJ mice are provided in (Fig. 11) Across studies, changes in NREM have been more variable, with some strains showing increases and some showing overall decreases compared to handling controls. Unfortunately, the EEG spectra across studies and strains have not been fully characterized, although there is some evidence that delta amplitude may vary as well, and we have found that NREM delta was relatively less in mice that showed greater reductions in REM (51). By comparison, NREM delta has been reported to be increased in rats after social stress (36) and after stress induced by a simulated predator (52). The decrease in delta sleep in patients with PTSD (reviewed in 16) suggests that it is important to determine stress-induced alterations in NREM as well as those in REM to understand the role sleep may play in the long-term effects of a traumatic event.
Non-rapid eye movement (NREM) and rapid eye movement (REM) sleep in BALB/cJ mice (n = 8) plotted hourly after shock training (left panels) and after the presentation of an auditory fearful cue (right panels) compared to baseline. For training, the mice received 15 tone-shock pairings (90-dB, 4.0-kHz, 5-s tone; 0.2-mA shock presented during the last 0.5 s). Testing with the fearful cue alone occurred 5 full days after shock training, and it was presented to the mice as they were otherwise undisturbed in their home cages. Note that 10 h of light period sleep were presented for the shock training day and 8 h of light period sleep were presented for the cue day due to a time difference between training and testing. Horizontal bar on the X-axis indicates the dark period. Base baseline, ST shock training, CUE fearful cue. Values are mean hourly total ± SEM, *p <.05 compared to baseline. (Adapted from Ref. 53)
The amount of training may also be an important factor as there appears to be a graded response in poststress sleep with greater or lesser numbers of pairings. For example, we found that the initial presentation of fearful cues after 4 days of training produced an 85% and a 55% reduction in REM and NREM, respectively, in the hour immediately after presentation (43). By comparison, the presentation of a fearful cue after a single day of training produced a 34% and a 19% reduction in REM and NREM, respectively, in the hour immediately after presentation (53). In contrast, REM and NREM mice trained with a single cue-shock pairing did not significantly differ from baseline levels after presentation of the cue. These differences also suggest variations in the relative strength of the association that was made between the cue and the shock across different amounts of training.
We have not fully replicated Adrien et al.'s (50) findings in rats; however, we have found reduced REM without rebound after multitrial training with a mild shock and reexposure to the fearful context (see Fig. 11), although there were differences among rat strains that may be related to differences in emotional reactivity as well as to differences in the stress axis (27). We have also found reductions in NREM after shock training and fearful contexts in some strains and not in others. Unfortunately, no one has conducted a full study of EEG spectra across rat strains and with different types of shock paradigms. Thus, while NREM amounts can be variable across studies, it remains to be seen whether there are differences in light and deep NREM or changes in EEG spectra in specific types of training paradigms that covary with the persistence of fearful behaviors.
Non-rapid eye movement (NREM) (left panel) and rapid eye movement (REM) (right panel) in Wistar rats (n = 8) plotted hourly after a handling and nonfearful, context control condition (Ctrl), after shock training (ST), and after reexposure to the shock training context without shock (context). For training, the rats were presented with 20 foot shocks (0.2 mA, 0.5-s duration) at 1.0-min intervals over the course of 20 min on two separate days (day 2 of training is plotted). For testing, they were placed back into the shock context for an equivalent period without receiving shock. Horizontal bar on the X-axis indicates the dark period. Values are mean ± SEM. S and C above the Ctrl line indicate significant differences compared for ST and Context, respectively. (Adapted from Ref. 27)
Morrison, Ross, and their colleagues (11,54,55) have focused primarily on the changes in REM that occur within the first 4 h after relatively mild fear training and subsequent presentation of fearful cues or contexts. These studies have also examined the recordings for the relative occurrence of sequential (<3 min between) and single (>3 min between) REM episodes based on findings that stressors like thermal load (56) and immobilization stress (30) have differential effects on sequential and single-REM episodes. In a study of cued fear, these authors (11) reported that the decrease in REM after presentation of the fearful cue was due to fewer single-REM episodes, whereas rats trained with an unpaired cue showed an increase in REM characterized by an increase in the number of sequential REM episodes. In a more recent study (55), they reported reduced sequential REM and increased single-REM episodes after presenting fear-inducing cues on day 14 after shock training. They also found significantly increased myoclonic twitches during REM, an important finding because increased phasic muscle activity during REM has been reported in veterans with PTSD (21,24). These studies indicate that determining simple changes in REM amounts will not be sufficient to fully understand the effects of stressors. It also remains to be determined how these conditioned changes in REM compare to those induced by other stressors.
Learning is often associated with increases in REM (57), and one might have predicted increased REM following fear conditioning. Rats (57) and mice (58) do exhibit increased REM (and rats also have more clusters of ponto-geniculo-occipital (PGO) waves, a signature characteristic of REM (57)) at various latencies after shock avoidance training in a shuttlebox. In the avoidance paradigm, animals are signaled of imminent shock and can learn to jump to safety without shock ever being delivered. The increases in REM have typically been viewed in the context of learning and interpreted as indicating a role for REM in memory consolidation. However, performance in this paradigm is motivated by foot shock and could involve significant stress.
While the reason for the difference between the two training procedures is unknown, the clearest difference is that shuttlebox training allows the animal to learn to avoid shock, whereas in fear conditioning the foot shock is inescapable. The fact that animals can learn to avoid shock in shuttlebox training implies that the animals have some control over the situation. By comparison, in fear conditioning, the animal has no control over whether it receives shock, although its occurrence may be predictable. Thus, there are significant differences in sleep after uncontrollable shock compared to after controllable shock, suggesting that understanding these differences may provide clues regarding the role poststress sleep may play in deterring or promoting the development of stress-related pathology. Intensity (4), predictability (5), and controllability (6) are important factors in the influence of stressors on behavior and physiology, and stressor intensity (4) and lack of controllability (6) have been suggested to be factors in the development of PTSD.
While the research on conditioned fear and sleep is not yet conclusive, work to date suggests that variations of this paradigm may provide models that have significant parallels to sleep in the development of PTSD as well as in the persisting alterations in sleep and arousal and may provide models that lead to better understanding of the underlying neurobiology. This work is also consistent with the suggestion of Yehuda and LeDoux (2) that understanding the neurobiology of PTSD will require identifying and characterizing atypical responses to stressors. This will likely require determining the relevant stressor qualities as well as determining individual differences in stress-induced changes in sleep that predict long-term changes in behavior in either inbred or outbred animals.
Fear Extinction and Sleep
Conditioned fear responses produced by fearful cues and contexts can typically be blocked through extended presentations of either type of stimuli without the reoccurrence of foot shock. This fear extinction is considered a type of new learning that inhibits subsequent fear without erasing the original memory for fear conditioning (12). The failure of extinction is thought to be a significant factor in persisting fear responses and anxiety (13), and extinction based therapy is used to treat PTSD patients (59). However, even though sleep disturbances are a significant complaint in PTSD, and several studies have demonstrated the effects of conditioned fear on sleep in animals, the relationship of fear extinction to subsequent sleep is not yet known.
Silvestri (60) trained rats for cued fear conditioning with light-shock pairings followed by 6 h of REM deprivation produced by the inverted flowerpot method. On extinction trials when the light alone was presented, compared to controls, REM-deprived rats showed greater overall freezing and less decrease in freezing across presentations of the light. The groups did not differ in freezing on a second session when the light alone was presented. No significant difference was found between REM-deprived and control rats in extinction to contextual fear. By comparison, Fu et al. (61) trained rats using an auditory cue to signal shock and found that 6 h of REM deprivation immediately after training did not alter extinction learning compared to control rats; however, REM-deprived rats did show greater spontaneous recovery of freezing on a second day with presentation of the fearful cue alone. REM deprivation performed from 7 to 12 h after shock training had no significant effects. There are a number of procedural differences in the studies that may be linked to relative differences in results in these two studies. However, both studies found effects for extinction of cued fear, and neither found that REM deprivation significantly altered contextual fear extinction learning or spontaneous recovery of freezing on a second day of testing (60,61). A limitation of these studies is that they were conducted without recording sleep and thus do not provide information regarding the relationship between electrophysiologically determined sleep and extinction.
We completed the first study that we are aware of to determine whether fear extinction is followed by different patterns of sleep compared to those after continued fear (62). We trained two groups of rats in contextual fear using a foot shock stressor and then reexposed both groups to the fearful context alone. One group was removed from the context before extinction occurred, and the other was allowed to remain in the fearful context until behavioral signs of fear (freezing) had completely subsided. This allowed comparison of sleep in rats with extinguished fear behavior to that in rats that continued to show fear. We also examined both groups for similarities and differences in freezing during shock training and on reexposure to the context. Figure 11 demonstrates increased sleep (both NREM and REM) following extinction to levels indicative of normal sleep, whereas rats that continued to show freezing in the fearful context exhibited reductions in REM similar to those previously reported (11,27). All rats experienced the same stressor; afterward, all were returned to the safety of their home cages. Animals that experienced identical handling and time in the context compared to the rats that exhibited continued fear or extinguished fear but never received shock sleep did not show significant differences in sleep. Thus, rats that were allowed to extinguish fear in the shock context showed different sleep than those that continued to show fear in the shock chamber, even though all were returned to the safety of their home cage. These data complement findings demonstrating fear-conditioned alterations in sleep and further suggest that poststress sleep is an important reflection of how the fear was processed. While this issue has not been examined in humans, these data also suggest that exposure therapy in PTSD patients may not only decrease their behavioral symptoms but also could play a role in alleviating their sleep disturbances as well (62).
Comparison of non-rapid eye movement (NREM) and rapid eye movement (REM) sleep recorded in Wistar rats after exposure to a fearful context without fear extinction (top panels) as indicated by continued freezing and with fear extinction (bottom panels) as indicated by cessation of freezing. NREM and REM sleep are plotted in two 4-h blocks (B1 and B2) and the entire 8-h light period (LIGHT). BL baseline sleep, ST shock training, FR (n = 7) 30-min context reexposure that did not produce extinction, EXT (n = 7) 60-min context reexposure that did produce extinction, R retest of both with a second fearful context exposure. For training, the rats were presented with 20 foot shocks (0.8 mA, 0.5-s duration) at 1.0-min intervals on a single day. Values are mean ± SEM. Differences relative to BL: +, p ≤.05; differences relative to ST: *, p ≤.05. (Adapted from Ref. 62)
Role of The Amygdala in Modulating The Effects of Stress on Sleep
The role of the amygdala in identifying aversive stimuli, mediating conditioned fear responses, and storing fearful memories has long been recognized (46,63). The amygdala also is a critical region for mediating the effects of stress, and it has been implicated in the psychopathology of PTSD (64). Several lines of research demonstrate that the amygdala plays a significant role in regulating sleep and arousal, and it is likely to play a role in regulating changes in arousal induced by stress.
The majority of research on the role of the amygdala in regulating sleep has been focused on its influence on REM; however, a number of studies indicated that the amygdala may be able to influence all sleep-wakefulness states. Evidence also indicates that inhibition of the central nucleus of the amygdala (CNA) suppresses REM, and that activation of CNA can promote REM in some situations. Functional inactivation of CNA with microinjections of the γ-aminobutyric acid A (GABAA) agonist muscimol produces a relatively selective decrease in REM, whereas blocking GABA-ergic inhibition with the GABAA antagonist bicuculline enhances REM. Functional lesions of the CNA by tetrodotoxin (TTX), which inactivates both cell bodies and fibers of passage, also decrease REM and reduce arousal (65). The decrease in REM can occur without recovery (see Fig. 11), a finding also seen with training with inescapable shock and fearful cues and contexts. In addition, putative inhibition of CNA by microinjections of serotonin terminate ongoing REM episodes (66), and electrical stimulation of the serotonergic dorsal raphé nucleus inhibits REM-on neurons in CNA (11). By comparison, electrical stimulation of CNA promotes REM in rats (67). In cats, microinjections of vasoactive intestinal peptide (68) and the cholinergic agonist carbachol (68) into CNA and basal amygdaloid nuclei can increase REM and related phenomena, although acetylcholine appears to play a role in reducing REM in rats (69).
Non-rapid eye movement (NREM) (left panel) and rapid eye movement (REM) (right panel) sleep in Wistar rats (n = 9) plotted hourly after microinjection of saline (SAL: 0.2 μL) and tetrodotoxin (TTX; 5.0 ng/0.2 μL) bilaterally into the central nucleus of the amygdala. Horizontal bar under X-axis indicates dark period. Error bars indicate SEM. *, p <.05 differences between SAL and TTX. (Adapted from Ref. 65)
Some of the effect of TTX may involve blocking fibers from the basal amygdala (BA) that pass through CNA to the bed nucleus of the stria terminalis (63). TTX inactivation of CNA, including fibers of passage, prior to dark onset shortened sleep latency, increased NREM time, decreased REM time, and decreased activity in rats (70). The effects of TTX inactivation on dark period sleep amounts are shown in Fig. 11. The involvement of BA also is suggested by reports that bilateral electrolytic and chemical lesions of the basolateral amygdala (BLA) increase NREM and total sleep time in rats (71) and that bilateral chemical lesions of the amygdala produce more consolidated sleep in chair-restrained Rhesus monkeys (72). In contrast, electrical and chemical stimulation of the BLA increased low-voltage, high-frequency activity in the cortical EEG and decreased NREM and total sleep time, respectively (71). An early study reported that electrical stimulation of the dorsal and ventral regions of BLA desynchronized and synchronized the EEG, respectively (73).
Dark period non-rapid eye movement (NREM) (left panel) and rapid eye movement (REM) (right panel) sleep in Wistar rats (n = 8) plotted in 2-h intervals after microinjections of saline (SAL: 0.2 μL) and two volumes of tetrodotoxin (TTXL: 2.5 ng/0.1 μL; TTXH: 5.0 ng/0.2 μL) to the central nucleus of the amygdala. Error bars indicate SEM. L and H indicate significant differences for TTXL and TTXH, respectively, compared to SAL (Tukey test, p <.05). (Adapted from Ref. 70)
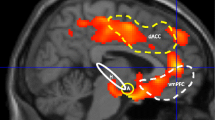
The human PTSD literature generally considers the amygdala as a single structure whose activation is important in PTSD symptoms. Indeed, neuroimaging studies have reported increased activation in the amygdala of PTSD patients in response to threat stimuli compared to nontrauma controls and trauma-exposed people who did not develop PTSD (reviewed in 74). However activation of the amygdala has also been found in association with REM in humans (e.g., 75). This suggests a refinement is needed regarding how the amygdala is viewed in regulating arousal state. This may be found in animal work that indicates that regions of the amygdala may be differentially involved in modulating different sleep states. For example, consistent with microinjection data, training with inescapable shock produced increased Fos activation in several regions of the amygdala (e.g., medial amygdala, cortical amygdala, BA, lateral amygdala, and amygdalostriatal transition region), but not in CNA (76), where muscimol and TTX microinjections decreased REM. This suggests that the probable role of the amygdala in influencing poststress sleep may involve differential activation and inactivation in various nuclei, and that multiple regions of the amygdala can be activated at the same time that REM is reduced.
CRH, Stress, and Alterations in Sleep
CRH has a major role in mediating central nervous system as well behavioral, autonomic, and physiological responses to stressors (77). It thus has been of significant interest as a factor in anxiety and mood disorders. Elevated levels of CRH have been found in the cerebrospinal fluid (78) and plasma (79) of PTSD patients, and elevated CRH has been hypothesized to play a role in the reduced delta sleep found in patients with PTSD (16).
Also, CRH has been implicated in stress-induced alterations in sleep, particularly in the control of REM (80). For example, administration of CRH antagonists have been reported to eliminate REM rebound after immobilization stress (80) and to decrease REM rebound after sleep deprivation (29). In the absence of stressors, CRH may contribute to the regulation of spontaneous waking (81), as evidenced by findings that the intracerebroventricular administration of CRH increases wakefulness in rats (82). The enhancement of wakefulness by CRH may occur at dosages too low to stimulate the hypothalamic-pituitary-adrenal (HPA) axis or produce behavioral effects (83). These findings indicate that CRH may produce changes in arousal and sleep in otherwise undisturbed conditions.
Opp and his colleagues have conducted an extensive series of studies examining the role of CRH in modulating arousal. These studies demonstrated that rat strains differing in the synthesis and secretion of CRH and in basal plasma concentrations of corticosterone show significant differences in amounts of sleep (83). Specifically, Lewis strain rats have a deficiency in the synthesis and secretion of hypothalamic CRH. These rats exhibit less wakefulness and more NREM than genetically related inbred Fischer 344 rats, outbred Spague-Dawley rats (33,83), or Wistar strain rats (33). Opp's laboratory also found that rats recorded in their home cages under well-habituated conditions, and without the presence of stressors, showed selective increases in wakefulness and decreases in NREM but no significant changes in REM after the intracerebroventricular administration of CRH (84). In addition, in rats in nonstressful conditions, the intracerebroventricular administration of CRH enhanced wakefulness when given at the beginning of either the light or the dark period, whereas intracerebroventricular administration of the nonspecific CRH antagonists astressin and αHelCRH (α-helical CRH9–41) reduced wakefulness and increased NREM only when administered in the dark period (84).
We examined the effects of CRH and astressin on wakefulness and sleep using two mouse strains with differential responsiveness to stress to determine whether CRH might also differentially affect undisturbed sleep and activity (85). Less-reactive C57BL/6J and high-reactive BALB/cJ mice were implanted with transmitters for determining sleep via telemetry and with guide cannulae for delivering drug into the lateral ventricles. In C57BL/6J mice, REM was significantly decreased after microinjections of 0.2 μg CRH and 0.4 μg CRH, and NREM and total sleep were decreased after microinjection of 0.4 μg CRH. Astressin did not significantly change wakefulness or sleep. In BALB/cJ mice, 0.4 μg CRH increased wakefulness and decreased NREM, REM, and total sleep. Astressin decreased active wakefulness and significantly increased REM at the low and high dosages. These strain differences in the effects of CRH and astressin may be linked to the relative responsiveness of C57BL/6J and BALB/cJ mice to stressors and to underlying differences in the CRH system.
The amygdala is a critical region for the central effects of CRH, and it appears to mediate a number of its anxiogenic effects, as evidenced by intra-amygdala microinjections of CRH agonists and antagonists (reviewed in 63). There has been very little work with respect to the effects on sleep of local application of CRH compounds into the brain; however, microinjections of 1.0-ng dosage of CRH into CNA of rats decreased average amount of REM over 4 h postinjection (11). Ongoing work in our lab conducted in rats also suggests that the CRH system in the amygdala can influence fear-induced alterations in sleep. For instance, microinjections of the relatively specific CRH receptor 1 antagonist antalarmin into CNA of rats attenuated reductions in REM and NREM that occur after exposure to a fearful context (86). While preliminary, these data indicate that the amygdala could be an important site for the influence of CRH on arousal and sleep in stressful conditions, and that it could be involved in potential effects on sleep produced by enhanced central CRH in PTSD patients. Recent in vitro work has implicated CRH in the modulation of excitatory glutamatergic synaptic transmission in CNA, with CRH1 and CRH2 receptors apparently playing inhibitory and facilitatory roles, respectively (87), a finding consistent with studies demonstrating that inactivation of CNA decreases REM.
Summary
Stress-induced alterations in sleep have been linked to the development of PTSD in humans, and sleep complaints and disturbances in arousal are continuing symptoms in patients. Stress-induced changes in sleep related to PTSD have not been fully characterized but appear to involve persisting changes in both REM and NREM. A number of animal models of stress are characterized by initial decreases in sleep followed by recovery sleep, which may indicate a restoration of homeostasis and successful resolution of the stress response. By comparison, intense conditioned fear training can produce reductions in REM without recovery as well as significant alterations in NREM that may vary with mouse and rat strains. These variants of conditioned fear paradigms and strain differences have not been fully exploited, but they appear to hold promise for modeling responses to stress that may provide insight into the role sleep plays in the neurobiology of PTSD. The amygdala and CRH have been implicated in PTSD and play significant roles in regulating the stress response that most likely includes regulating stress-induced changes in arousal and sleep. Determining normal and atypical responses to stress, including poststress sleep, may lead to the development of significantly improved models for examining how stress produces long-term alterations in behavior.
References
Shalev, A. Y. (2000) Biological responses to disasters. Psychiatric Q 71, 277–88.
Yehuda, R., and LeDoux, J. (2007) Response variation following trauma: a translational neuroscience approach to understanding PTSD. Neuron 56, 19–32.
Cohen, H., Zohar, J., and Matar, M. (2003) The relevance of differential response to trauma in an animal model of posttraumatic stress disorder. Biol Psychiatry 53, 463–73.
Buydens-Branchey, L., Noumair, D., and Branchey, M. (1990) Duration and intensity of combat exposure and posttraumatic stress disorder in Vietnam veterans. J Nerv Ment Dis 178, 582–87.
Abbott, B. B., Schoen, L. S., and Badia, P. (1984) Predictable and unpredictable shock: behavioral measures of aversion and physiological measures of stress. Psychol Bull 96, 45–71.
Foa, E. B., Zinbarg, R., and Rothbaum, B. O. (1992) Uncontrollability and unpredictability in post-traumatic stress disorder: an animal model. Psychol Bull 112, 218–38.
Yehuda, R., Flory, J. D., Southwick, S., and Charney, D. S. (2006) Developing an agenda for translational studies of resilience and vulnerability following trauma exposure. Ann N Y Acad Sci 1071, 379–96.
Rauch, S. L., Shin, L. M., and Phelps, E. A. (2006) Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research—past, present, and future. Biol Psychiatry 60, 376–82.
Charney, D., and Deutch, A. (1996) A functional neuroanatomy of anxiety and fear: implications for the pathophysiology and treatment of anxiety disorders. Crit Rev Neurobiol 10, 419–46.
Pynoos, R., Ritzmann, R., Steinberg, A., Goenjian, A., and Prisecaru, I. (1996) A behavioral animal model of posttraumatic stress disorder featuring repeated exposure to situational reminders. Biol Psychiatry 39, 129–34.
Jha, S. K., Brennan, F. X., Pawlyk, A. C., Ross, R. J., and Morrison, A. R. (2005) REM sleep: a sensitive index of fear conditioning in rats. Eur J Neurosci 21, 1077–80.
Bouton, M. E. (2004) Context and behavioral processes in extinction. Learn Mem 11, 485–94.
Myers, K. M., and Davis, M. (2007) Mechanisms of fear extinction. Mol Psychiatry 12, 120–50.
Lavie, P. (2001) Sleep disturbances in the wake of traumatic events. N Engl J Med 345, 1825–32.
Harvey, A. G., Jones, C., and Schmidt, D. A. (2003) Sleep and posttraumatic stress disorder: a review. Clin Psychol Rev 23, 377–407.
Neylan, T. C., Otte, C., Yehuda, R., and Marmar, C. R. (2006) Neuroendocrine regulation of sleep disturbances in PTSD. Ann N Y Acad Sci 1071, 203–15.
Germain, A., Buysse, D. J., and Nofzinger, E. (2007) Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev 12, 185–95.
Greenberg, R., Pearlman, C. A., and Gampel, D. (1972) War neuroses and the adaptive function of REM sleep. Br J Med Psychol 45, 27–33.
van der Kolk, B., Blitz, R., Burr, W., Sherry, S., and Hartmann, E. (1984) Nightmares and trauma: a comparison of nightmares after combat with lifelong nightmares in veterans. Am J Psychiatry 141, 187–90.
Schlosberg, A., and Benjamin, M. (1978) Sleep patterns in three acute combat fatigue cases. J Clin Psychiatry 39, 546–49.
Ross, R. J., Ball, W. A., Dinges, D. F., et al. (1994) Rapid eye movement sleep disturbance in posttraumatic stress disorder. Biol Psychiatry 35, 195–202.
Ross, R. J., Ball, W. A., Sanford, L. D., et al. (1999) Rapid eye movement sleep changes during the adaptation night in combat veterans with posttraumatic stress disorder. Biol Psychiatry 45, 938–41.
Dow, B. M., Kelsoe, J. R., Jr, and Gillin, J. C. (1996) Sleep and dreams in Vietnam PTSD and depression. Biol Psychiatry 39, 42–50.
Mellman, T. A., Nolan, B., Hebding, J., Kulick-Bell, R., and Dominguez, R. (1997) A polysomnographic comparison of veterans with combat-related PTSD, depressed men, and non-ill controls. Sleep (abstract suppl) 20, 46–51.
Mellman, T. A., Bustamante, V., Fins, A. I., Pigeon, W. R., and Nolan, B. (2002) REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatry 159, 1696–1701.
Mellman, T. A., Pigeon, W. R., Nowell, P. D., and Nolan, B. (2007) Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma. J Trauma Stress 20, 893–901.
Tang, X., Yang, L., and Sanford, L. D. (2005) Rat strain differences in freezing and sleep alterations associated with contextual fear. Sleep 28, 1235–44.
Sanford, L. D., Xiao, J., Liu, X., Yang, L., and Tang, X. (2005) Influence of avoidance training (AT) and AT cues on sleep in C57BL/6J (B6) and BALB/cJ (C) mice. Sleep (abstract suppl) 28, A6.
Gonzalez, M. M., Debilly, G., Valatx, J. L., and Jouvet, M. (1995) Sleep increase after immobilization stress: role of the noradrenergic locus coeruleus system in the rat. Neurosci Lett 202, 5–8.
Dewasmes, G., Loos, N., Delanaud, S., Dewasmes, D., and Ramadan, W. (2004) Pattern of rapid-eye movement sleep episode occurrence after an immobilization stress in the rat. Neurosci Lett 355, 17–20.
Smith, C. (1995) Sleep states and memory processes. Behav Brain Res 69, 137–45.
Tang, X., Xiao, J., Parris, B. S., Fang, J., and Sanford, L. D. (2005) Differential effects of two types of environmental novelty on activity and sleep in BALB/cJ and C57BL/J mice. Physiol Behav 85, 419–29.
Tang, X., Xiao, J., Liu, X., and Sanford, L. D. (2004) Strain differences in the influence of open field exposure on sleep in mice. Behav Brain Res 154, 137–47.
Tang, X., Liu, X., Yang, L., and Sanford, L. D. (2005) Rat strain differences in sleep after acute mild stressors and short-term sleep loss. Behav Brain Res 160, 60–71.
Bodosi, B., Obal, F., Jr, Gardi, J., Komlodi, J., Fang, J., and Krueger, J. M. (2000) An ether stressor increases REM sleep in rats: possible role of prolactin. Am J Physiol Regul Integr Comp Physiol 279, R1590–98.
Meerlo, P., Pragt, B. J., and Daan, S. (1997) Social stress induces high intensity sleep in rats. Neurosci Lett 225, 41–44.
Chrousos, G. P. (1998) Stressors, stress, and neuroendocrine integration of the adaptive response. Ann N Y Acad Sci 851, 311–35.
Duke, J. L., Zammit, T. G., and Lawson, D. M. (2001) The effects of routine cage-changing on cardiovascular and behavioral parameters in male Sprague-Dawley rats. Contemp Top Lab Anim Sci 40, 17–20.
Pacak, K., and Palkovits, M. (2001) Stressor specificity of central neuroendocrine responses: implications for stress-related disorders. Endocr Rev 22, 502–48.
Kerns, J. G., Cohen, J. D., MacDonald, A. W., 3rd, Cho, R. Y., Stenger, V. A., and Carter, C. S. (2004) Anterior cingulate conflict monitoring and adjustments in control. Science 303, 1023–26.
Bush, D. E., Sotres-Bayon, F., and LeDoux, J. E. (2007) Individual differences in fear: isolating fear reactivity and fear recovery phenotypes. J Trauma Stress 20, 413–22.
Tang, X., Yang, L., and Sanford, L. D. (2007) Individual variation in sleep and motor activity in rats. Behav Brain Res 180, 62–68.
Sanford, L. D., Tang, X., Ross, R. J., and Morrison, A. R. (2003) Influence of shock training and explicit fear-conditioned cues on sleep architecture in mice: strain comparison. Behav Genet 33, 43–58.
Sanford, L. D., Yang, L., and Tang, X. (2003) Influence of contextual fear on sleep in mice: a strain comparison. Sleep 26, 527–40.
Blanchard, R. J., and Blanchard, D. C. (1969) Crouching as an index of fear. J Comp Physiol Psychol 67, 370–75.
Davis, M. (1992) The role of the amygdala in conditioned fear. In: Aggleton, J., ed. The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. New York: Wiley-Liss; 255–305.
Graves, L. A., Heller, E. A., Pack, A. I., and Abel, T. (2003) Sleep deprivation selectively impairs memory consolidation for contextual fear conditioning. Learn Mem 10, 168–76.
Hellman, K., and Abel, T. (2007) Fear conditioning increases NREM sleep. Behav Neurosci 121, 310–23.
Maier, S. F., Amat, J., Baratta, M. V., Paul, E., and Watkins, L. R. (2006) Behavioral control, the medial prefrontal cortex, and resilience. Dialogues Clin Neurosci 8, 397–406.
Adrien, J., Dugovic, C., and Martin, P. (1991) Sleep-wakefulness patterns in the helpless rat. Physiol Behav 49, 257–62.
Tang, X., Yang, L., and Sanford, L. D. (2006) Spectral EEG power after uncontrollable shock (US) and fearful context (FC): variability amongst mouse strains. Sleep 29, A11.
Lesku, J. A., Bark, R. J., Martinez-Gonzalez, D., Rattenborg, N. C., Amlaner, C. J., and Lima, S. L. (2008) Predator-induced plasticity in sleep architecture in wild-caught Norway rats (Rattus norvegicus). Behav Brain Res 189, 298–305.
Sanford, L. D., Fang, J., and Tang, X. (2003) Sleep after differing amounts of conditioned fear training in BALB/cJ mice. Behav Brain Res 147, 193–202.
Pawlyk, A. C., Jha, S. K., Brennan, F. X., Morrison, A. R., and Ross, R. J. (2005) A rodent model of sleep disturbances in posttraumatic stress disorder: the role of context after fear conditioning. Biol Psychiatry 57, 268–77.
Madan, V., Brennan, F. X., Mann, G. L., et al. (2008) Long-term effect of cued fear conditioning on REM sleep microarchitecture in rats. Sleep (abstract suppl) 31, 497–305.
Amici, R., Zamboni, G., Perez, E., Jones, C. A., and Parmeggiani, P. L. (1998) The influence of a heavy thermal load on REM sleep in the rat. Brain Res 781, 252–58.
Datta, S. (2000) Avoidance task training potentiates phasic pontine-wave density in the rat: a mechanism for sleep-dependent plasticity. J Neurosci 20, 8607–13.
Smith, C., Kitahama, K., Valatx, J. L., and Jouvet, M. (1974) Increased paradoxical sleep in mice during acquisition of a shock avoidance task. Brain Res 77, 221–30.
Pitman, R. K., Shin, L. M., and Rauch, S. L. (2001) Investigating the pathogenesis of posttraumatic stress disorder with neuroimaging. J Clin Psychiatry 62, 47–54.
Silvestri, A. J. (2005) REM sleep deprivation affects extinction of cued but not contextual fear conditioning. Physiol Behav 84, 343–49.
Fu, J., Li, P., Ouyang, X., et al. (2007) Rapid eye movement sleep deprivation selectively impairs recall of fear extinction in hippocampus-independent tasks in rats. Neuroscience 144, 1186–92.
Wellman, L. L., Holbrook, B. D., Yang, L., Tang, X., and Sanford, L. D. (2008) Contextual fear extinction eliminates sleep disturbances found following fear conditioning in rats. Sleep 31, 1035–42.
Davis, M., and Whalen, P. J. (2001) The amygdala: vigilance and emotion. Mol Psychiatry 6, 13–34.
Bremner, J. D. (2005) Effects of traumatic stress on brain structure and function: relevance to early responses to trauma. J Trauma Dissociation 6, 51–68.
Tang, X., Yang, L., Liu, X., and Sanford, L. D. (2005) Influence of tetrodotoxin inactivation of the central nucleus of the amygdala on sleep and arousal. Sleep 28, 923–30.
Sanford, L. D., Tejani-Butt, S. M., Ross, R. J., and Morrison, A. R. (1995) Amygdaloid control of alerting and behavioral arousal in rats: involvement of serotonergic mechanisms. Arch Ital Biol 134, 81–99.
Smith, C. T., and Miskiman, D. E. (1975) Increases in paradoxical sleep as a result of amygdaloid stimulation. Physiol Behav 15, 17–19.
Calvo, J., Simón-Arceo, K., and Fernández-Mas, R. (1996 ) Prolonged enhancement of REM sleep produced by carbachol microinjection into the amygdala. NeuroRep 7, 577–80.
Sanford, L. D., Yang, L., Tang, X., Dong, E., Ross, R. J., and Morrison, A. R. (2006) Cholinergic regulation of the central nucleus of the amygdala in rats: effects of local microinjections of cholinomimetics and cholinergic antagonists on arousal and sleep. Neuroscience 141, 2167–76.
Sanford, L. D., Yang, L., Liu, X., and Tang, X. (2006) Effects of tetrodotoxin (TTX) inactivation of the central nucleus of the amygdala (CNA) on dark period sleep and activity. Brain Res 1084, 80–88.
Zhu, G. Q., Zhong, M. K., Zhang, J. X., et al. (1998) [Role of basolateral amygdaloid nuclei in sleep and wakeful state regulation]. Sheng Li Xue Bao 50, 688–92.
Benca, R. M., Obermeyer, W. H., Shelton, S. E., Droster, J., and Kalin, N. H. (2000) Effects of amygdala lesions on sleep in rhesus monkeys. Brain Res 879, 130–38.
Kreindler, A., and Steriade, M. (1964) EEG patterns of arousal and sleep induced by stimulating various amygdaloid levels in the cat. Arch Ital Biol 102, 576–86.
Shin, L. M., Rauch, S. L., and Pitman, R. K. (2006) Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann N Y Acad Sci 1071, 67–79.
Maquet, P., Peters, J., Aerts, J., et al. (1996) Functional neuroanatomy of human rapid-eye-movement sleep and dreaming. Nature 383, 163–66.
Liu, X., Tang, X., and Sanford, L. D. (2003) Fear-conditioned suppression of REM sleep: relationship to Fos expression patterns in limbic and brainstem regions in BALB/cJ mice. Brain Res 991, 1–17.
Koob, G. F. (1999) Corticotropin-releasing factor, norepinephrine, and stress. Biol Psychiatry 46, 1167–80.
Bremner, J. D., Licinio, J., Darnell, A., et al. (1997) Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am J Psychiatry 154, 624–29.
de Kloet, C. S., Vermetten, E., Geuze, E., et al. (2007) Elevated plasma corticotrophin-releasing hormone levels in veterans with posttraumatic stress disorder. Prog Brain Res 167, 287–91.
Gonzalez, M. M., and Valatx, J. L. (1997) Effect of intracerebroventricular administration of alpha-helical CRH (9–41) on the sleep/waking cycle in rats under normal conditions or after subjection to an acute stressful stimulus. J Sleep Res 6, 164–70.
Chang, F. C., and Opp, M. R. (2001) Corticotropin-releasing hormone (CRH) as a regulator of waking. Neurosci Biobehav Rev 25, 445–53.
Ehlers, C. L., Reed, T. K., and Henriksen, S. J. (1986) Effects of corticotropin-releasing factor and growth hormone-releasing factor on sleep and activity in rats. Neuroendocrinology 42, 467–74.
Opp, M. R. (1997) Rat strain differences suggest a role for corticotropin-releasing hormone in modulating sleep. Physiol Behav 63, 67–74.
Chang, F. C., and Opp, M. R. (1998) Blockade of corticotropin-releasing hormone receptors reduces spontaneous waking in the rat. Am J Physiol 275, R793–R802.
Sanford, L. D., Yang, L., Wellman, L. L., Dong, E., and Tang, X. (2008) Mouse strain differences in the effects of corticotropin releasing hormone (CRH) on sleep and wakefulness. Brain Res 1190, 94–104.
Liu, X., Dong, E., Yang, L., Tang, X., and Sanford, L. D. (2008) Antagonizing corticotropin releasing hormone (CRH) 1 receptors in the central nucleus of the amygdala (CNA) attenuates fear-induced reductions in sleep. Sleep (abstract suppl) 31, A16.
Liu, J., Yu, B., Neugebauer, V., et al. (2004) Corticotropin-releasing factor and Urocortin I modulate excitatory glutamatergic synaptic transmission. J Neurosci 24, 4020–29.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Humana Press, a part of Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Sanford, L., Tang, X. (2009). Effect of Stress on Sleep and Its Relationship to Post-Traumatic Stress Disorder. In: LeDoux, J., Keane, T., Shiromani, P. (eds) Post-Traumatic Stress Disorder. Humana Press. https://doi.org/10.1007/978-1-60327-329-9_11
Download citation
DOI: https://doi.org/10.1007/978-1-60327-329-9_11
Published:
Publisher Name: Humana Press
Print ISBN: 978-1-60327-328-2
Online ISBN: 978-1-60327-329-9
eBook Packages: MedicineMedicine (R0)