Abstract
Based on clues from epidemiology, it has been proposed that low prenatal vitamin D may be a risk factor for schizophrenia. In order to explore this hypothesis, our group has undertaken an integrated research program linking analytic epidemiology and rodent experiments. There is consistent evidence from rodents that offspring exposed to low developmental vitamin D deficiency have altered brain structure and function as adults. This chapter provides a concise summary of the evidence linking vitamin D to brain development and function. In addition, the epidemiological evidence linking hypovitaminosis D and various neuropsychiatric disorders is outlined.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Key Words
1 Introduction
From an historical perspective, the links between vitamin D and neuropsychiatric disorders have only received attention in recent decades. The first indirect clue that vitamin D may play a role in brain development and function was when vitamin D and its metabolites were discovered in the cerebrospinal fluid of healthy adults (1). However, the work of Walter Stumpf catalysed the modern interest in the impact of vitamin D on brain function. Stumpf mapped 1,25-dihydroxyvitamin D [1,25(OH)2D] binding in rodent brains using radio-labelled 1,25(OH)2D and autoradiography (2, 3). The presence of this receptor in the central nervous system (CNS) provided the first real clues that vitamin D may have a role in brain function. Later studies using immunohistochemistry for the vitamin D receptor (VDR), in the neonatal and adult rat central nervous system, showed evidence for the VDR in multiple brain regions (e.g. temporal, orbital and cingulate cortices, thalamus, accumbens, amygdala, olfactory system and pyramidal neurons of the hippocampus), thus adding further weight to the hypothesis that vitamin D signalling is involved in brain function (4–6). The later discovery of 1-hydroxylase in the human brain suggests that the CNS can synthesise 1,25(OH)2D (the active form of vitamin D) from 25-hydroxyvitamin D [25(OH)D], which is the precursor inactive form (this is the “storage” form of vitamin D used to monitor serum levels). Thus, serum 25(OH)D levels may influence the autocrine and paracrine production of 1,25(OH)2D in the CNS (7–10), challenging the assumption that the brain is wholly reliant on circulating 25(OH)D crossing the blood–brain barrier (11, 12).
The chapter has two aims. We will provide a concise summary of the evidence linking vitamin D to brain development and brain function. Mostly, this evidence is based on animal experiments. In particular, we will focus on an animal model developed by the authors to explore the impact of transient low prenatal vitamin D on brain development. Finally, we will summarize the epidemiological clues that link vitamin D to adult neuropsychiatric disorders such as schizophrenia and depression.
2 Vitamin D And Brain Development
Expression of the VDR is temporally regulated in the developing rat CNS (4). The earliest expression of VDR in the developing brain is in neural epithelium from day 12 of gestation. The VDR continues to be expressed in differentiating areas of the brain throughout gestation (4). Specifically, the VDR emerges at days 19–21 in the pyramidal cells of the hippocampus, the same time at which the cells begin to cease division and commence differentiation in this brain region (4). There is also a strong correlation between the degree of VDR staining and the degree of mitotic activity seen in the developing neuroepithelium of the developing rat CNS (6). The temporal expression of VDR protein and messenger ribonucleic acid (mRNA) in the developing rat brain actually coincides with a decrease in mitotic activity and an increase in apoptosis, and this has led to the hypothesis that vitamin D could be regulating neuronal cell cycle events (6).
Given nerve growth factor (NGF) is essential for the growth and survival of cholinergic basal forebrain neurons which project to the hippocampus (13) and 1,25(OH)2D is a potent regulator of NGF (14, 15), it is possible that vitamin D can effect hippocampal development by modulating NGF production (4). The addition of 1,25(OH)2D has been shown to increase neurite outgrowth in embryonic hippocampal explant cultures, an effect which is most likely due to the induction of NGF (16). The addition of 1,25(OH)2D to cultured hippocampal neurons also reduces the number of mitotic cells present and increases the amount of free NGF protein produced (16). NGF is capable of binding to the neurotrophin receptor p75NTR (17). The promoter region of this receptor contains a vitamin D response element; hence, vitamin D can regulate the expression of the p75NTR receptor in glioma cells (18). NGF and p75NTR are essential for programmed cell death (19). As vitamin D regulates both proteins, it is possible that vitamin D could modulate neuronal survival and differentiation during development.
Vitamin D may also indirectly influence neuronal development by altering neurotrophic factor production by non-neuronal cells. The addition of 1,25(OH)2D to rat primary glial cell cultures has been shown to increase the synthesis of NGF mRNA and protein (14), neurotrophin-3 (NT-3) mRNA (20) and down-regulate neurotrophin-4 (NT-4) mRNA (20). The addition of 1,25(OH)2D can also increase the synthesis of glial cell line-derived neurotrophin factor (GDNF) mRNA in C6 glioma cells (21) but does not regulate GDNF production in primary glial cell cultures (22). While GDNF is produced by non-neuronal cells, it is integral to the development of the dopaminergic (23) and noradrenergic systems (24). This evidence therefore suggests that vitamin D could directly alter cellular development in the brain (both neuronal and non-neuronal).
Further evidence that vitamin D can effect brain development comes from studies on non-neuronal cell lines. 1,25(OH)2D is able to induce cell death pathways in rat and human gliomas (25) and this effect extends to multiple glioma cell lines and primary cultures from surgical specimens (26). Microglial astrocytes also respond to 1,25(OH)2D in models of lipopolysaccharide (LPS)-induced brain inflammation and experimental autoimmune encephalitis (EAE) (27, 28). Finally, it has been shown in vitro that activated microglia can metabolise 25(OH)D and produce biologically active 1,25(OH)2D (29). This evidence, taken in light of the evidence that the enzyme 1 α-hydroxylase is present in glial (9), suggests that non-neuronal cells could synthesise vitamin D locally within the brain.
3 Brain Development In The Developmental Vitamin D (Dvd)-Deficient Rodent
In order to explore the impact of transient hypovitaminosis D on brain development and subsequent adult brain structure and function, the authors have developed the developmental vitamin D (DVD) deficiency model. To obtain vitamin D depletion, female Sprague-Dawley rats are kept on a vitamin D-deficient diet. Animals are housed on a 12-h light/dark cycle (lights on at 06:00 h) using incandescent lighting to avoid ultraviolet radiation within the vitamin D action spectrum. These conditions are maintained for 6 weeks prior to mating and throughout gestation. Control animals are kept under similar conditions except they receive a vitamin D-replete diet and are housed under standard lighting conditions. After the dams have littered, all dams (and corresponding litters) are placed on vitamin D-replete diet. The vitamin D-deficient dams and DVD-deficient offspring remain normocalcemic (i.e. neither the dams nor their offspring have the rickets-like phenotype that would result from more chronic vitamin D depletion). It is important to stress that this is only a developmental exposure, because from birth all maternal animals and offspring receive a diet containing normal levels of vitamin D. Offspring are vitamin D replete by 2 weeks of age (30), and vitamin D levels, calcium, and parathyroid hormone (PTH) levels are all normal when the animals are tested as adults (i.e. 10 weeks).
As neonates, the DVD-deficient offspring have a number of anatomical changes in the developing brain, including an increase in brain and lateral ventricle size and a decrease in thickness of the neocortex (31). There are also other changes in markers of neuronal development, as DVD-deficient rats showed increased numbers of mitotic cells and decreased levels of p75 protein (31). Further studies confirmed that cellular differentiation was profoundly altered in the DVD-deficient developing brain (32). The level of apoptosis in the developing brains of DVD-deficient rats follows a different trajectory compared to controls; at embryonic day 19 (E19) there was no difference; however, at E21 and birth DVD-deficient rats had fewer apoptotic cells than controls (32). This difference was normalised by post-natal day 7 (P7) (32). It should be noted, however, that these rats were maintained on a vitamin D-deficient diet until being tested at P7. In line with a previous study (31), DVD-deficient rats also showed increased rates of mitosis at significant pre- and post-natal time points (E19, E21, P0 and P7) (32). More recently the VDR was shown to be present in neurospheres cultured from the subventricular zone (SVZ) of neonatal rats (33). When neurosphere cultures are made from the brains of DVD-deficient neonates, neurosphere number was increased, suggesting greater cellular division (33). This same study also revealed that the addition of 1,25(OH)2D decreased neurosphere number. Thus, both the presence and the absence of vitamin D are capable of manipulating cellular proliferation in developing brain cells.
The timing of the reintroduction of vitamin D appears to be important in the persistence of these developmental changes into adulthood (34). The enlarged lateral ventricles seen in the DVD-deficient neonates (31) only persist into adulthood if the introduction of the vitamin D-replete diet is delayed until weaning. Thus, re-addition of vitamin D to the diet from birth appears to partially ameliorate the lateral ventricle changes in DVD-deficient rats (34).
The adult DVD-deficient rats also have altered brain expression of genes involved in cytoskeleton maintenance (MAP2, NF-L) and neurotransmission (GABA-Aα4) (34). Gene array and proteomics analysis have been used to explore gene expression in the whole brain and protein expression in the prefrontal cortex and hippocampus of adult DVD-deficient rats (35, 36). These studies found that DVD deficiency resulted in significantly altered expression of 36 proteins and 74 genes involved with cytoskeleton maintenance, calcium homeostasis, synaptic plasticity and neurotransmission, oxidative phosphorylation, redox balance, protein transport, chaperoning, cell cycle control and post-translational modifications (35, 36). A recent study has examined protein expression in the nucleus accumbens in the DVD rat (37). While this study found small fold-changes, it identified significant alterations in several proteins involved in calcium binding proteins (calbindin1, calbindin2 and hippocalcin). Other proteins associated with DVD deficiency related to mitochondrial function and the dynamin-like proteins.
4 Behaviour In The Dvd-Deficient Rat And Mouse
By adulthood, male DVD-deficient rats show a complex behavioural phenotype. DVD-deficient rats have disrupted latent inhibition (38); however, they have normal pre-pulse inhibition (39) and working memory (38). In the open field, DVD-deficient rats display a novelty-induced hyperlocomotion (40) that can be abated by injection or restraint (39, 41), even though they display a normal stress response in the hypothalamic pituitary axis (42). Adult, male DVD-deficient rats also exhibit a sensitivity to the N-methyl-d-aspartic acid receptor (NMDA-R) antagonist MK-801 (39). Treatment with MK-801 induces hyperlocomotion in the open field in control rats, and DVD-deficient rats responded with an even greater enhancement in locomotor activity (39). The later period of gestation appeared to be most relevant for this later effect (30), because rats experiencing a DVD deficiency during late gestation also showed this effect, whereas DVD-deficient rats exposed during early gestation did not (30).
A mouse model of DVD deficiency has also recently been produced in two strains of mice (129/SvJ and C57BL/6 J) (43). As with the rat model, one strain exhibited spontaneous hyperlocomotion in the open field arena (43). However, both strains demonstrated increased frequency of head dips in a hold board arena, indicative of increased exploratory behaviour (43). This is in contrast to findings from DVD-deficient rats on the hole board test (38). DVD-deficient mice were also assessed on a comprehensive screen of behavioural tests, including the elevated plus maze, forced swim test, pre-pulse inhibition and social interaction test (43). There was no effect of maternal diet or strain on performance in any of these four tests (43).
5 Vitamin D And Neuropsychiatric Disorders: Clues From Epidemiology
Based on clues from epidemiology, it has been proposed that low prenatal vitamin D may be associated with an increased risk of several adult-onset disorders. For example, McGrath (12) drew attention to diseases such as multiple sclerosis and schizophrenia that had both season of birth effects (e.g. those born in winter and spring have an increased risk of developing schizophrenia) and latitude effects (e.g. the prevalence of schizophrenia and multiple sclerosis is higher at higher latitudes).
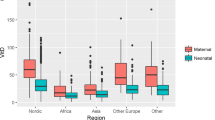
Many studies have shown that those born in winter and spring have a significantly increased risk of developing schizophrenia (44) and that those born at higher latitudes are also at increased risk (45), with both the incidence and the prevalence of schizophrenia being significantly greater in sites from higher latitudes (46). Furthermore, based on data from cold climates, the incidence of schizophrenia is significantly higher in dark-skinned migrants compared to the native born (47). Given that hypovitaminosis D is more common (a) during winter and spring, (b) at high latitudes and (c) in dark-skinned individuals (48), low prenatal vitamin D “fits” these key environmental features. Preliminary evidence from analytical epidemiology studies also links low prenatal vitamin D with schizophrenia risk. For example, vitamin D supplements in the first year of life significantly reduced the risk of schizophrenia in males in a large Finnish Birth Cohort (49). In addition, 25(OH)D serum levels in 26 mothers whose children developed schizophrenia were numerically (but not significantly) lower than that of 51 control mothers whose children did not develop the disease (50). There was a trend-level association between low maternal vitamin D levels and schizophrenia in a subgroup of children of African-American mothers (50), who would be at greatest risk of vitamin D deficiency because of their increased skin pigmentation.
There is some epidemiological data linking developmental vitamin D status and MS. The concordance rate of MS in monozygotic twins is only 30%, indicating a strong environmental influence on the development of the disease. Two northern hemisphere studies have described a season of birth effect for MS. A small Danish study described an excess of MS births in spring (51), and a pooled analysis of patients from Canada, Britain, Denmark and Sweden described an increase in the percentage of people with MS born in May (spring) and a decrease in the percentage born in November (autumn) (52). Other epidemiological links between vitamin D and multiple sclerosis are covered elsewhere in this book.
There is a growing body of evidence linking hypovitaminosis D and depression. First, the higher prevalence of seasonal affective disorder in high latitudes was noted by Stumpf (53); however, results of randomized controlled trials of vitamin D supplements in this group have been mixed (54–57). There is some evidence linking 25(OH)D levels to scores on mood scales (55, 56), and hypotheses have been outlined linking vitamin D to neurotransmitters implicated in depression (58). Observational studies suggest an association between low 25(OH)D levels and depression. Two studies designed primarily to examining 25(OH)D levels and performance on cognitive function have also reported an association between low 25(OH)D levels and depressed mood (59, 60). However, neither of these studies included adjustments for physical activity; thus, any apparent association between 25(OH)D and mood may simply reflect that depressed individuals are less likely to go outside and thus access ultraviolet radiation.
These issues have been examined in a larger observation study (61). Based on 1,283 community-based elderly residents (65–95 years), it was reported that 25(OH)D levels were 14% lower in 169 persons with minor depression and 14% lower in 26 persons with major depressive disorder compared with levels in 1,087 control individuals. Depression severity was significantly associated with decreased serum 25(OH)D levels and increased serum PTH levels. These associations persisted when controlled for activity levels. Adequately powered randomized controlled trials will be required to progress this interesting research field.
With respect to vitamin D and cognition, the results are also mixed. Several clinical studies have examined 25(OH)D levels and performance on neurocognitive measures using case–control samples. Based on patients with secondary hyperparathyroidism (n = 21) and matched controls (n = 63), Jorde and colleagues reported no significant association between 25(OH)D levels and various cognitive measures (59). Another study, based on a mixed sample of 80 elderly individuals (60 years or older; half with mild Alzheimer’s disease), reported no association between 25(OH)D levels and performance on a factor score derived from a large battery of neurocognitive tests (60). Finally, a study based on a sample of 80 elderly individuals referred to a memory clinic reported a significant positive correlation between 25(OH)D levels and performance on the Mini Mental State Examination (62). However, these studies lacked sufficient power to confidently detect small effect sizes, were not community-based and were not able to address the important potential confound of reverse causality (i.e. those with impaired cognitive ability may be less likely to go outside, and thus may develop hypovitaminosis D as a consequence of impaired cognition).
Some of these issues were addressed in a recently published study based on the large population-based NHANES III survey. The study examined the association between 25(OH)D levels and several different neurocognitive measures (including measures of attention and memory) in an adolescent group (n = 1676, age range 12–17 years), adult group (n = 4747, 20–60 years) and elderly group (n = 4809, 60–90 years). The study controlled for physical activity, as a proxy measure related to outdoor activity and possible ultraviolet light exposure. However, in the adolescent and adult groups, none of the psychometric measures were associated with 25(OH)D levels. In the elderly group there was a significant difference between 25(OH)D quintiles performance on a learning and memory task; however, paradoxically those with the highest quintile of 25(OH)D were most impaired on the task, contrary to the hypotheses. Lower 25(OH)D levels were not associated with impaired performance on various psychometric measures. While this cross-sectional study indicates that 25(OH)D levels are not associated with neurocognitive performance, it remains to be seen if chronic exposure to low 25(OH)D levels alters brain function in the long term. Curiously, in vitro experiments have clearly shown that vitamin D has neuroprotective qualities (63–67). For example, pretreatment with 1,25(OH)2D reduces the impact of glucocorticoid-induced neuronal changes (68). Thus, it may be feasible that low vitamin D reduces the ability of the brain to recover after various adverse events (e.g. hypoxia, infection/inflammation, high glucocorticoid levels related to stress). Chronic hypovitaminosis D may exacerbate the resultant neuropsychiatric impairment. A longitudinal, prospective study would be better suited to exploring this hypothesis. While the animal experimental data supports an association between low developmental vitamin D and altered brain development, the impact of hypovitaminosis D during adulthood on brain function remains to be clarified. Recently, a detailed narrative review of the field reached similar conclusions (69). More animal experimental work should help clarify the role of vitamin D on adult brain function; however, more focussed analytic epidemiological experiments are also required.
6 Conclusions
The list of neuropsychiatric disorders with possible links to vitamin D continues to grow. Recently, developmental vitamin D deficiency has also been linked to autism spectrum disorders (70). While the results from the DVD-deficient animal experiments indicate that brain structure and function is altered in rodents, it remains to be seen if this deficiency is associated with schizophrenia in humans. How vitamin D links to cognition and depression also warrants further scrutiny. Much work remains to be done in order to understand how developmental vitamin D can influence brain development.
REFERENCES
Balabanova S, Richter HP, Antoniadis G, Homoki J, Kremmer N et al (1984) 25-Hydroxyvitamin D, 24, 25-dihydroxyvitamin D and 1,25-dihydroxyvitamin D in human cerebrospinal fluid. Klin Wochenschr 62:1086–1090
Stumpf WE, Bidmon HJ, Li L, Pilgrim C, Bartke A et al (1992) Nuclear receptor sites for vitamin D-soltriol in midbrain and hindbrain of Siberian hamster (Phodopus sungorus) assessed by autoradiography. Histochemistry 98:155–164
Stumpf WE, O’Brien LP (1987) 1,25 (OH)2 vitamin D3 sites of action in the brain. An Autoradiographic Study. Histochemistry 87:393–406
Veenstra TD, Prufer K, Koenigsberger C, Brimijoin SW, Grande JP et al (1998) 1,25-Dihydroxyvitamin D3 receptors in the central nervous system of the rat embryo. Brain Res 804:193–205
Prufer K, Veenstra TD, Jirikowski GF, Kumar R (1999) Distribution of 1,25-dihydroxyvitamin D3 receptor immunoreactivity in the rat brain and spinal cord. J Chem Neuroanat 16:135–145
Burkert R, McGrath J, Eyles D (2003) Vitamin D receptor expression in the embryonic rat brain. Neurosci Res Commun 33:63–71
Hosseinpour F, Wikvall K (2000) Porcine microsomal vitamin D(3) 25-hydroxylase (CYP2D25). Catalytic properties, tissue distribution, and comparison with human CYP2D6. J Biol Chem 275:34650–34655
Zehnder D, Bland R, Williams MC, McNinch RW, Howie AJ et al (2001) Extrarenal expression of 25-hydroxyvitamin d(3)-1 alpha-hydroxylase. J Clin Endocrinol Metab 86:888–894
Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ (2005) Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat 29:21–30
Sutherland MK, Somerville MJ, Yoong LK, Bergeron C, Haussler MR et al (1992) Reduction of vitamin D hormone receptor mRNA levels in Alzheimer as compared to Huntington hippocampus: correlation with calbindin-28 k mRNA levels. Brain Res Mol Brain Res 13:239–250
Gascon-Barre M, Huet PM (1983) Apparent [3H]1,25-dihydroxyvitamin D3 uptake by canine and rodent brain. Am J Physiol 244:E266–E271
McGrath J (2001) Does ‘imprinting’ with low prenatal vitamin D contribute to the risk of various adult disorders? Med Hypotheses 56:367–371
Korsching S, Auburger G, Heumann R, Scott J, Thoenen H (1985) Levels of nerve growth factor and its mRNA in the central nervous system of the rat correlate with cholinergic innervation. Embo J 4:1389–1393
Neveu I, Naveilhan P, Jehan F, Baudet C, Wion D et al (1994) 1,25-dihydroxyvitamin D3 regulates the synthesis of nerve growth factor in primary cultures of glial cells. Brain Res Mol Brain Res 24:70–76
Wion D, MacGrogan D, Neveu I, Jehan F, Houlgatte R et al (1991) 1,25-Dihydroxyvitamin D3 is a potent inducer of nerve growth factor synthesis. J Neurosci Res 28:110–114
Brown J, Bianco JI, McGrath JJ, Eyles DW (2003) 1,25-dihydroxyvitamin D3 induces nerve growth factor, promotes neurite outgrowth and inhibits mitosis in embryonic rat hippocampal neurons. Neurosci Lett 343:139–143
Chao MV, Hempstead BL (1995) p75 and Trk: a two-receptor system. Trends Neurosci 18:321–326
Naveilhan P, Neveu I, Baudet C, Funakoshi H, Wion D et al (1996) 1,25-Dihydroxyvitamin D3 regulates the expression of the low-affinity neurotrophin receptor. Brain Res Mol Brain Res 41:259–268
Chao MV (1994) The p75 neurotrophin receptor. J Neurobiol 25:1373–1385
Neveu I, Naveilhan P, Baudet C, Brachet P, Metsis M (1994) 1,25-dihydroxyvitamin D3 regulates NT-3, NT-4 but not BDNF mRNA in astrocytes. Neuroreport 6:124–126
Naveilhan P, Neveu I, Wion D, Brachet P (1996) 1,25-Dihydroxyvitamin D3, an inducer of glial cell line-derived neurotrophic factor. Neuroreport 7:2171–2175
Remy S, Naveilhan P, Brachet P, Neveu I (2001) Differential regulation of GDNF, neurturin, and their receptors in primary cultures of rat glial cells. J Neurosci Res 64:242–251
Granholm AC, Reyland M, Albeck D, Sanders L, Gerhardt G et al (2000) Glial cell line-derived neurotrophic factor is essential for postnatal survival of midbrain dopamine neurons. J Neurosci 20:3182–3190
Quintero EM, Willis LM, Zaman V, Lee J, Boger HA et al (2004) Glial cell line-derived neurotrophic factor is essential for neuronal survival in the locus coeruleus-hippocampal noradrenergic pathway. Neuroscience 124:137–146
Naveilhan P, Berger F, Haddad K, Barbot N, Benabid AL et al (1994) Induction of glioma cell death by 1,25(OH)2 vitamin D3: towards an endocrine therapy of brain tumors? J Neurosci Res 37:271–277
Zou J, Landy H, Feun L, Xu R, Lampidis T et al (2000) Correlation of a unique 220-kDa protein with vitamin D sensitivity in glioma cells. Biochem Pharmacol 60:1361–1365
Garcion E, Sindji L, Montero-Menei C, Andre C, Brachet P et al (1998) Expression of inducible nitric oxide synthase during rat brain inflammation: regulation by 1,25-dihydroxyvitamin D3. Glia 22:282–294
Nataf S, Garcion E, Darcy F, Chabannes D, Muller JY et al (1996) 1,25 Dihydroxyvitamin D3 exerts regional effects in the central nervous system during experimental allergic encephalomyelitis. J Neuropathol Exp Neurol 55:904–914
Neveu I, Naveilhan P, Menaa C, Wion D, Brachet P et al (1994) Synthesis of 1,25-dihydroxyvitamin D3 by rat brain macrophages in vitro. J Neurosci Res 38:214–220
O’Loan J, Eyles DW, Kesby J, Ko P, McGrath JJ et al (2007) Vitamin D deficiency during various stages of pregnancy in the rat; its impact on development and behaviour in adult offspring. Psychoneuroendocrinology 32:227–234
Eyles D, Brown J, Mackay-Sim A, McGrath J, Feron F (2003) Vitamin D3 and brain development. Neuroscience 118:641–653
Ko P, Burkert R, McGrath J, Eyles D (2004) Maternal vitamin D3 deprivation and the regulation of apoptosis and cell cycle during rat brain development. Brain Res Dev Brain Res 153:61–68
Cui X, McGrath JJ, Burne TH, Mackay-Sim A, Eyles DW (2007) Maternal vitamin D depletion alters neurogenesis in the developing rat brain. Int J Dev Neurosci 25:227–232
Feron F, Burne TH, Brown J, Smith E, McGrath JJ et al (2005) Developmental Vitamin D3 deficiency alters the adult rat brain. Brain Res Bull 65:141–148
Almeras L, Eyles D, Benech P, Laffite D, Villard C et al (2007) Developmental vitamin D deficiency alters brain protein expression in the adult rat: implications for neuropsychiatric disorders. Proteomics 7:769–780
Eyles D, Almeras L, Benech P, Patatian A, Mackay-Sim A et al (2007) Developmental vitamin D deficiency alters the expression of genes encoding mitochondrial, cytoskeletal and synaptic proteins in the adult rat brain. J Steroid Biochem Mol Biol 103:538–545
McGrath J, Iwazaki T, Eyles D, Burne T, Cui X et al (2008) Protein expression in the nucleus accumbens of rats exposed to developmental vitamin D deficiency. PLoS One 3(6):e2383
Becker A, Eyles DW, McGrath JJ, Grecksch G (2005) Transient prenatal vitamin D deficiency is associated with subtle alterations in learning and memory functions in adult rats. Behav Brain Res 161:306–312
Kesby JP, Burne TH, McGrath JJ, Eyles DW (2006) Developmental vitamin D deficiency alters MK 801-induced hyperlocomotion in the adult rat: an animal model of schizophrenia. Biol Psychiatry 60:591–596
Burne TH, Becker A, Brown J, Eyles DW, Mackay-Sim A et al (2004) Transient prenatal Vitamin D deficiency is associated with hyperlocomotion in adult rats. Behav Brain Res 154:549–555
Burne TH, O’Loan J, McGrath JJ, Eyles DW (2006) Hyperlocomotion associated with transient prenatal vitamin D deficiency is ameliorated by acute restraint. Behav Brain Res 174:119–124
Eyles DW, Rogers F, Buller K, McGrath JJ, Ko P et al (2006) Developmental vitamin D (DVD) deficiency in the rat alters adult behaviour independently of HPA function. Psychoneuroendocrinology 31:958–964
Harms LR, Eyles DW, McGrath JJ, Mackay-Sim A, Burne TH (2007) Developmental vitamin D deficiency alters adult behaviour in 129/SvJ and C57BL/6 J mice. Behav Brain Res 187(2):343–350
Torrey EF, Miller J, Rawlings R, Yolken RH (1997) Seasonality of births in schizophrenia and bipolar disorder: a review of the literature. Schizophr Res 28:1–38
Saha S, Chant DC, Welham JL, McGrath JJ (2006) The incidence and prevalence of schizophrenia varies with latitude. Acta Psychiatr Scand 114:36–39
Davies G, Welham J, Chant D, Torrey EF, McGrath J (2003) A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophr Bull 29:587–593
Cantor-Graae E, Selten JP (2005) Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry 162:12–24
Holick MF (1995) Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr 61:638S–645S
McGrath J, Saari K, Hakko H, Jokelainen J, Jones P et al (2004) Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr Res 67:237–245
McGrath J, Eyles D, Mowry B, Yolken R, Buka S (2003) Low maternal vitamin D as a risk factor for schizophrenia: a pilot study using banked sera. Schizophr Res 63:73–78
Templer DI, Trent NH, Spencer DA, Trent A, Corgiat MD et al (1992) Season of birth in multiple sclerosis. Acta Neurol Scand 85:107–109
Willer CJ, Dyment DA, Sadovnick AD, Rothwell PM, Murray TJ et al (2005) Timing of birth and risk of multiple sclerosis: population based study. BMJ 330:120
Stumpf WE, Privette TH (1989) Light, vitamin D and psychiatry. Role of 1,25 dihydroxyvitamin D3 (soltriol) in etiology and therapy of seasonal affective disorder and other mental processes. Psychopharmacology (Berl) 97:285–294
Dumville JC, Miles JN, Porthouse J, Cockayne S, Saxon L et al (2006) Can vitamin D supplementation prevent winter-time blues? A randomised trial among older women. J Nutr Health Aging 10:151–153
Gloth FM 3rd, Alam W, Hollis B (1999) Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging 3:5–7
Lansdowne AT, Provost SC (1998) Vitamin D3 enhances mood in healthy subjects during winter. Psychopharmacology (Berl) 135:319–323
Partonen T, Vakkuri O, Lamberg-Allardt C, Lonnqvist J (1996) Effects of bright light on sleepiness, melatonin, and 25-hydroxyvitamin D(3) in winter seasonal affective disorder. Biol Psychiatry 39:865–872
Berk M, Sanders KM, Pasco JA, Jacka FN, Williams LJ et al (2007) Vitamin D deficiency may play a role in depression. Med Hypotheses 69:1316–1319
Jorde R, Waterloo K, Saleh F, Haug E, Svartberg J (2006) Neuropsychological function in relation to serum parathyroid hormone and serum 25-hydroxyvitamin D levels : The Tromso study. J Neurol 253:464–470
Wilkins CH, Sheline YI, Roe CM, Birge SJ, Morris JC (2006) Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. Am J Geriatr Psychiatry 14:1032–1040
Hoogendijk WJ, Lips P, Dik MG, Deeg DJ, Beekman AT et al (2008) Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry 65:508–512
Przybelski RJ, Binkley NC (2007) Is vitamin D important for preserving cognition? A positive correlation of serum 25-hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys 460(2):202–205
Oermann E, Bidmon HJ, Witte OW, Zilles K (2004) Effects of 1alpha,25 dihydroxyvitamin D3 on the expression of HO-1 and GFAP in glial cells of the photothrombotically lesioned cerebral cortex. J Chem Neuroanat 28:225–238
Wang JY, Wu JN, Cherng TL, Hoffer BJ, Chen HH et al (2001) Vitamin D(3) attenuates 6-hydroxydopamine-induced neurotoxicity in rats. Brain Res 904:67–75
Brewer LD, Thibault V, Chen KC, Langub MC, Landfield PW et al (2001) Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons. J Neurosci 21:98–108
Moore ME, Piazza A, McCartney Y, Lynch MA (2005) Evidence that vitamin D3 reverses age-related inflammatory changes in the rat hippocampus. Biochem Soc Trans 33:573–577
Losem-Heinrichs E, Gorg B, Redecker C, Schleicher A, Witte OW et al (2005) 1alpha,25-dihydroxy-vitamin D3 in combination with 17beta-estradiol lowers the cortical expression of heat shock protein-27 following experimentally induced focal cortical ischemia in rats. Arch Biochem Biophys 439:70–79
Obradovic D, Gronemeyer H, Lutz B, Rein T (2006) Cross-talk of vitamin D and glucocorticoids in hippocampal cells. J Neurochem 96:500–509
McCann JC, Ames BN (2008) Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction? FASEB J 22:982–1001
Cannell JJ (2008) Autism and vitamin D. Med Hypotheses 70:750–759
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Harvey, L., Burne, T., Cui, X., Mackay-Sim, A., Eyles, D., McGrath, J. (2010). Vitamin D and the Brain: A Neuropsychiatric Perspective. In: Holick, M. (eds) Vitamin D. Nutrition and Health. Humana Press. https://doi.org/10.1007/978-1-60327-303-9_16
Download citation
DOI: https://doi.org/10.1007/978-1-60327-303-9_16
Published:
Publisher Name: Humana Press
Print ISBN: 978-1-60327-300-8
Online ISBN: 978-1-60327-303-9
eBook Packages: MedicineMedicine (R0)