Abstract
Orthoses are assistive devices that support joints through alignment, stabilization, or assisting weakened musculature. The cost associated with orthotic treatment is substantial, and the demand is outpacing the supply. Patient comfort and performance are influenced by orthosis fit (size or shape) as well as function (mechanical aspects). To achieve optimal performance outcomes, an orthosis must be customized to the individual patient. However, traditional fabrication methods do not readily support the objective prescription and manufacture of orthosis mechanical aspects. There is a need for processes that promote better patient outcomes. Here, we seek to identify promising approaches, contemporary methods, and existing gaps that may provide enhanced benefit and value to the orthotic user. This chapter examines the current state of patient care practices as well as cutting-edge research and technologies primarily associated with ankle-foot orthoses.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
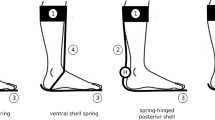
Orthoses are assistive devices that support joints through alignment, stabilization, or assisting weakened musculature. While prosthetic devices serve to replace a lost limb, the goal of an extremity orthosis is to restore the lost function of an impaired limb [1]. For the lower extremity, the three primary types of orthoses are foot orthoses (FOs), ankle-foot orthoses (AFOs), and knee-ankle-foot orthoses (KAFOs). There are orthoses that also span the hip and pelvis. Orthoses can be further categorized based on a variety of features including their power source (passive, semi-active, or active) and their design (solid or hinged) [2, 3].
In civilian and military populations, there are high rates of extremity and orthopedic injuries that result in limb impairments, which are often treated with orthotic interventions. According to the 2005 Americans with Disabilities report, approximately 27 million people over the age of 15 had a walking-related disability [4]. In the military population, 54% of combat wounds sustained in Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) from 2001 to 2005 were extremity injuries [5]. These injuries and associated disabilities limit function, often impeding the ability to work, perform activities of daily living, and return to active duty [6]. Orthopedic injuries are the leading cause of soldiers being deemed unfit for duty. Conditions of the foot, ankle, and lower extremity are three of the five most common orthopedic conditions leading to soldier disability in both peacetime and war [6]. Extremity injuries sustained during OIF and OEF accounted for 64% of service members determined to be unfit for duty [7]. The cost associated with orthotic treatment is substantial, and demand is outpacing supply. Disability costs associated with military extremity injuries are projected to be $170 million for a studied cohort of 1,566 injured subjects [7]. In 2010 alone, Medicare expenditures for prosthetic- and orthotic-related charges exceeded $580M [8]. By 2020, the Department of Education estimated that prosthetists and orthotists will be able to serve just 61% of the patients who need personalized rehabilitation devices [9].
Evidence suggests that many orthoses do not provide optimal benefit and value to those who wear them [10]. Characteristics related to fit (orthosis size or shape) and function (mechanical aspects) both influence comfort and performance. Fit and function must be customized to the individual patient to achieve optimal performance outcomes [1, 3]. Routinely, practitioners who prescribe orthoses apply subjective and sometimes contradictory approaches that have little evidence of efficacy [1, 11,12,13]. As a result, many patients experience suboptimal functional outcomes . Although orthoses appear to be relatively simple devices, the process of designing and objectively prescribing the fit and functional characteristics of an orthosis is remarkably complex. This complexity is reflected in the International Organization of Standardization (ISO) standards that have been developed to define orthotic terminology. These standards define terms relating to patient description, orthosis functional requirements, orthosis design, orthosis mechanical properties, and manufacturing (Fig. 6.1) [3]. They also indicate the importance of engaging an array of clinical, biomechanical, and engineering concepts in order to design and prescribe orthoses with ideal fit and function to promote optimal performance.
Established ISO standards for orthotic terminology . These standards, which define orthotic-related terms, range from patient assessment to orthosis characteristics to fabrication methods. (Figure originally published in Condie [3])
This chapter identifies contemporary methods, existing gaps, and promising approaches that may provide enhanced benefit and value to the orthotic user. Improved fabrication of orthoses would help to reduce costs associated with health care and disability claims. We consider the state of traditional patient care practices as well as cutting-edge research, technologies, and approaches primarily associated with ankle-foot orthoses. These advances have the potential for positive impact on patient outcomes and cost of care and, ultimately, the potential to transform the orthotic field.
Traditional Standards of Practice
Standards of practice for prescribing orthoses focus on three main categories: fit, function, and fabrication. These factors are considered when prescribing either a prefabricated or a customized orthosis. Prefabricated or off-the-shelf orthoses typically are available in a range of standard sizes and often include a footplate that is designed to be trimmed down to the individual user’s foot size [14,15,16]. Sometimes there is also the option to select functional characteristics such as the general strut or footplate stiffness, with options such as flexible, normal, or stiff [16].
Alternatively, the orthosis can be custom-made for the user. To make a customized orthosis, the orthotist traditionally begins by manually aligning the patient’s joint(s) based on knowledge of the relevant anatomy and then makes a cast of the patient’s limb in its corrected alignment [17]. This negative mold helps characterize the shape of the limb and serves as a guideline for fit customization of the orthosis. Plaster is poured into the negative mold to create a positive mold, and the orthotist forms plastic around the positive mold to craft the orthosis [17]. The orthotist then subjectively manipulates trimlines (material thickness) and shape to adjust the orthosis’ fit and function.
To customize orthosis function, the traditional prescription process typically begins with a patient assessment. This involves a combination of a physical evaluation, including manually tested strength and range-of-motion measurements, and a visual gait analysis in which the clinician watches the patient walk in real-time or by video recording [18]. Based on the findings of the assessment, the orthotist and physician prescribe the orthosis design and features appropriate to the patient [3]. Although effective treatment with orthoses requires an understanding of normal gait biomechanics, assessment of the patient’s biomechanical and functional abilities, and appropriate mechanical function [18], in a traditional clinical setting, these factors are typically considered qualitatively. Orthotists rely on their own judgment developed over years of professional experience and on qualitative descriptions provided by the orthotic manufacturer to represent how different orthosis designs are thought to affect gait biomechanics [19,20,21]. The functional characteristics of orthoses are rarely, if ever, quantified in a clinical setting. Thus it is difficult to objectively relate orthotic functional design characteristics to patient functional outcomes [1, 11,12,13].
Even when modern technologies are applied as part of the process, the current clinical standard of practice for fabricating custom orthoses remains highly subjective. As an alternative to the traditional method of limb shape characterization via casting and positive molding, some practitioners capture the size and shape of a patient’s limb using digital scanning techniques [22]. By this method, the positive limb mold is created with the help of a computer-aided design (CAD) program and then modified by digitally extruding or carving the 3D scan image as deemed necessary by the orthotist or technician. However, after the initial digital design phase, the plastic orthosis is still formed manually over physical molds, which have been carved via computer-aided manufacturing (CAM) systems based on the digital positive mold [22].
While some practitioners have in-house orthotic fabricating capabilities for traditional and/or CAD-/CAM-based approaches, others have begun to outsource manufacturing to central fabricators. It is often cost-prohibitive to establish and maintain in-house fabrication systems; rapid treatment can be achieved by overnight shipping [22]. Despite these benefits, it was recently estimated that only 24% of prosthetists and orthotists use central fabricators [23]. The hesitancy to outsource fabrication may be due to the subjective nature of the manufacturing process itself, which can lead to wide variations in product quality [23]. However fabrication is approached, the process remains heavily qualitative and subjective, with the orthotist relying on experience and intuition to prescribe and fabricate the orthosis rather than measuring and quantitatively fine-tuning orthosis characteristics [3].
Orthosis Prescription Research
The prescription of customized orthoses can be divided into features that pertain to orthosis fit and features that pertain to orthosis function. In order to readily customize orthosis characteristics, objective prescription guidelines that relate patient assessment to orthosis fit and function must be established. Research is underway to develop this understanding and to establish methods for guideline implementation.
Characteristics of Fit
In order to customize the fit of an orthosis, the detailed shape of the individual’s limb must be recorded and replicated. Traditionally, this is done by the casting process previously described. Upon completion, customized fit is achieved by manually forming plastic around the limb cast [17]. While this approach is effective, it is also time-consuming, messy, and produces substantial material waste [17]. Furthermore, the subjective and manual nature of the process can introduce unwanted variability in fit and effectiveness [24].
As described briefly above, researchers are now working to develop 3D scanning technologies to capture a digital surface image of the limb [25,26,27]. The digitally captured surface image is then manually refined in a virtual environment, typically using smoothing and extruding functions. These modifications smooth the image to eliminate any gaps or inconsistencies from the scanning process and allow the practitioner to stretch and extrude specific areas of the image to relieve pressure or make room for padding introduced by the orthosis. These 3D scanning technologies have been implemented in some clinical service models to incrementally advance the field through central manufacture of physical limb models without the use of plaster [22].
In current research paradigms, the scanned surface model is used as the basis for creating a 3D CAD model of the orthosis [26, 28,29,30], which can then be fabricated by a variety of methods to be considered later in this chapter. In combination with advanced manufacturing approaches, the 3D scanning approach reduces the time needed for customization of the orthosis and eliminates the waste associated with traditional casting and manual fabrication processes [25]. Despite these benefits , 3D scanning techniques do not eliminate subjectivity or resulting variability [25, 27].
Some novel, objective approaches to the fit customization process have been proposed. As a concept to quantitatively fit-customize devices, Smith and Burgess described a “by the numbers approach” to the fitting of prosthetic sockets; this technique employs a standardized set of measurements (of the residual limb) to specify the size and shape of a prosthetic socket [22]. To our knowledge, this is the first introduction to the published literature of a quantitative method to customize the fit of a rehabilitation device.
We have proposed a novel approach to customizing the fit of AFOs. Rather than capturing the shape of a patient’s limb, we propose a biomechanically linked “shape conformance” process by which a fully parameterized AFO CAD model automatically conforms to the size and general shape of the limb [31]. The process employs discrete 3D measurements of a minimal set (n = 44) of biomechanically and anatomically relevant limb surface landmark locations. The discrete 3D measures are expected as input parameters in the fully parameterized CAD model, which automatically adapts its size and shape to conform to the patient’s limb when the values of the discrete 3D measures are updated [31, 32]. This unique process automatically conforms an AFO model to the patient’s limb, obviating the need to capture and reproduce limb size and shape and simultaneously eliminating the need for manual or subjective manipulation of the CAD model. By linking discrete landmarks directly to the CAD model via parameterization, this approach provides a quantifiable and repeatable method by which parameters of the orthosis CAD model are adjusted to digitally customize the virtual orthosis prior to function customization and fabrication. By linking the CAD model to joint centers and biomechanically based limb coordinate systems, this process also supports parameterized adjustments to important additional fit characteristics. For example, ankle joint alignment and AFO-surfaces-to-skin offset distances can be adjusted to accommodate various padding thicknesses [32].
Characteristics of Function
It is widely believed that in order to help patients achieve their highest functional potential, the functional characteristics of orthoses should be customized to meet each individual’s unique needs. However, there are no objective prescription guidelines available yet to support this goal. There are several obstacles to the development of such guidelines. First, the traditional manual approach to orthosis fabrication introduces substantial variability in function [33]. Because the functional characteristics of “crafted” braces are rarely quantified, there is a lack of evidence to support efficacy [1, 11,12,13]. Second, the majority of clinical studies do not report outcomes of patient assessments (e.g., muscle weakness) to quantify a patient’s capability or fail to report orthosis design information [34]. Deriving the relationship between patient assessment (capability), activity level (task demand), and orthosis function (level of device assistance) involves complex biomechanics and gait analysis [1, 18, 20]. Relevant factors involve the influence of the orthosis on the joint(s) it spans as well as interactions between limb segments and the foot’s interaction with the ground during activities of daily living [3, 35]. Lacking quantitative detail and evidence of efficacy , it is difficult to link patient capability and activity level to orthosis design and function, which in turn constrains development of an objective model for orthosis prescription. Years have been spent developing the technology necessary for advanced orthotic design, fit, and function, but the need persists for systematic research to quantify device and patient characteristics as well as their interaction during functional activity.
Harlaar and colleagues proposed that objective, evidence-based prescription guidelines should be based on (a) assessment of a patient’s activity level and gait function and (b) specification of the mechanical characteristics of the orthosis [1]. Prescription guidelines must apply these factors to match the orthosis specifically to the patient’s individual needs [1] (Fig. 6.2). Additionally, Brehm and colleagues proposed quantitative performance measures of patient activity to evaluate the efficacy of orthoses [11]. To develop evidence-based prescription guidelines in combination with these measurements, they proposed a core set of outcome parameters, which include measures of joint, bone, and muscle [11].
A proposed conceptual prescription model for ankle-foot orthoses . This prescription model highlights two important factors in customizing and prescribing ankle-foot orthoses. (Figure originally published in Harlaar et al. [1])
Bending stiffness , or the resistance to bending of a passive-dynamic orthosis, is one of the primary functional characteristics that many research and practitioners believe should be customized for individuals to achieve optimal function [1, 10, 36, 37]. To adjust orthosis stiffness, orthotists usually modify material thickness or trimlines. Numerous approaches have been proposed to measure orthosis bending resistance [38], but these methods are seldom employed in a clinical setting. Thus, no objective criteria exist for selecting or prescribing orthosis stiffness.
Researchers are using experimental and computational techniques in the effort to develop prescription guidelines for orthosis stiffness, primarily for AFOs. AFOs can provide dorsiflexor assistance by providing plantar flexion resistance or plantar flexor assistance by providing dorsiflexion resistance. AFOs that assist the dorsiflexors are commonly prescribed for individuals with foot drop. While it is fairly straightforward to create an AFO that can hold the ankle in a neutral position during swing, it is important not to make the orthosis so stiff that it restricts ankle motion during stance [10]. Kobayashi and colleagues employed an experimental AFO with quantifiable and adjustable stiffness to investigate the influence of AFO stiffness on gait [39]. Their findings demonstrate that too much plantar flexion resistance can induce undesired knee flexion in early stance, thereby emphasizing the need to customize AFO stiffness to provide the proper amount of assistance required [40]. However, comprehensive patient assessment measures were not reported, thus limiting the ability to relate AFO stiffness to patient functional outcome. Although it seems clear that stiffness should be related to the patient’s individual strength and functional ability, specific guidelines have yet to be determined.
For individuals with weakened plantar flexors , AFOs should provide dorsiflexion resistance to supplement weakened ankle plantar flexion activity to control shank progression during the stance phase of gait [41]. Restoring ankle moments to normal levels may be critical to restoring functional gait. This was demonstrated in a controlled perturbation study which showed that healthy individuals maintained invariant ankle moments during gait when an ankle exoskeleton provided supplemental plantar flexion torque [42], and similar findings have been documented in other studies [43]. It has been shown that in patients with plantar flexor weakness, AFOs can provide supplemental plantar flexion moments [44,45,46] as well as additional benefits including tibial advancement control, supplemental ankle power, and longer strides. However, only one of those studies, which was a pilot study, reported AFO bending stiffness [46]. The magnitude of the AFO stiffness is important, as is the timing energy returned by the AFO [47] and the AFO’s work about the ankle [48].
The studies referenced above demonstrate the benefits of resistive plantar flexion and dorsiflexion AFO stiffness and suggest important parameters that can be targeted to improve gait. Still missing, however, is a method by which to determine optimal device stiffness in relationship to patient weakness, functional ability, and outcomes. Recent efforts to quantifiably customize the stiffness of AFOs have used finite element analysis to establish the bending stiffness of virtual orthoses [49, 50]. In these studies, finite element analysis of orthosis computer models was used to predict strains under a given load to estimate stiffness. Orthosis shape characteristics could then be adjusted to tune the bending stiffness of the AFO. Thus, finite element analysis enables the stiffness of an orthosis to be predicted and adjusted (tuned) prior to manufacturing.
Although not yet used in clinical practice, many researchers have developed other techniques to experimentally quantify the stiffness of already manufactured AFOs [38]. Notably, one group has developed a novel, clinically applicable device to test the stiffness and neutral angle of AFOs [51]. The Biarticular Reciprocating Universal Compliance Estimator (BRUCE) measures stiffness of an AFO and/or AFO-shoe combination about the ankle and metatarsal joints across a functional sagittal plane ankle range of motion. It accommodates a wide range of AFO sizes and shapes because it measures angles and moments in the same manner as a traditional gait analysis and applies boundary conditions that mimic conditions during AFO use. BRUCE can also be operated in a clinical setting (Fig. 6.3). Other techniques have been tested to measure AFO stiffness, but many do not apply appropriate boundary conditions. This is potentially problematic because AFOs are very sensitive to loading conditions [52].
Design of an ankle-foot orthosis stiffness testing device . The novel Biarticular Reciprocating Universal Compliance Estimator (BRUCE) design provides an excellent example of a clinically viable device that provides valuable quantifications of orthosis bending stiffness. (Figure originally published in Bregman et al. [51])
In addition to stiffness, other important characteristics have been identified as necessary for customized orthoses. For example, footplate design and orthosis joint alignment are two components that can be customized to improve gait function by facilitating foot-to-floor motion and controlling kinematics of the entire lower extremity. A footplate creates a lever arm for the rest of the orthosis to rotate, so it is important for at least a portion of the footplate to be rigid [1]. Additionally, it has been noted that footplate length should be prescribed either to limit or to preserve joint motion, depending on the patient’s impairment profile, with the overall goal to facilitate functional gait and stability [12]. As an addition or alternative to customizing footplate length, rocker bottom shoes or rockers built into the footplate may reduce plantar pressures and pain [53]. Finally, footplate design can influence the dynamics of the entire lower extremity. For example, a case study with a patient with hemiplegia demonstrated that tuning the AFO in combination with footwear improved knee kinematics [54].
In conjunction with footplate design , orthosis joint alignment should be customized by considering the alignment of all lower-extremity joints. For example, in a rigid AFO, the unloaded AFO ankle joint angle influences the position of the tibia and therefore of knee and hip net joint moments. All of these parameters should be taken into account when prescribing the AFO ankle joint alignment [1]. Limb segment kinematics must also be considered [35]. Malas noted that the prescription and design of AFOs must consider the shank angle to the floor, which is influenced by AFO design and by the interaction between the AFO and footwear [12]. It has been suggested that the AFO shank-to-floor angle should stabilize the proximal lower-extremity joints and properly align the patient’s posture. Depending on the patient’s impairment profile, orthoses were found to be set with a shank-to-floor angle anywhere between 7° and 15°, although 10–12° is most common [12].
Encompassing all of these concepts, Elaine Owen proposes a prescription algorithm prescribing a combined orthosis-footwear system based on shank kinematics in a clinical gait assessment [35] (Fig. 6.4). Nonetheless, there is still a lack of quantitative evidence to identify the net influence of these parameters on patient kinematics and kinetics. As a result, orthotists are left with a clinical decision tree by which to select and customize AFO and other footwear characteristics [55].
A clinical decision tree for selecting and customizing ankle-foot orthosis and footwear characteristics . This clinical prescription model serves as an excellent basis for developing and implementing objective prescription model s for customizing orthosis characteristics. (Figure originally published in Owen [5])
Devices in Development with Customizable Function
To meet the increasingly important need to provide highly customized functional aspects of orthoses, researchers are exploring various orthotic design approaches ranging from passive dynamic (springlike) to active dynamic (powered) [2, 31]. Passive orthoses use material properties or mechanical elements such as springs to generate mechanical characteristics. They can control joint motion and provide torque assistance; however, they have a limited capability to adapt their function for different tasks (e.g., walking, running, stair ascending) or even within a single task (e.g., stance vs. swing of gait). Power-harvesting passive orthoses contain elements that harvest power through motion, such as oil dampers or pneumatic components. Semi-active orthoses use a variety of technologies that store and release energy; these devices often include some type of control scheme but cannot feed energy into the system. Active orthoses contain a power source that puts energy into the system and actuators that run by a control scheme. Active orthoses have a greater capability for dynamic adaptability but see limited use in the traditional clinical setting due to their costs and complexities (weight, size, power sources, and control schemes) [2].
Incorporating many of the fit and function customization concepts into its design and prescription, the Intrepid Dynamic Exoskeletal Orthosis (IDEO) is a customized carbon fiber passive-dynamic orthosis that has helped limb-salvage wounded warriors achieve high levels of function [56, 57] (Fig. 6.5). This novel design provides dramatic improvements in functional gains over other orthoses currently available. However, the IDEO still relies on traditional fabrication methods for customization of fit and function. The footplate and cuff are handcrafted using traditional limb shape replication methods, and a trial-and-error method is used to converge on the proper off-the-shelf strut stiffness; there is limited ability to objectively prescribe the IDEO’s bending stiffness.
Novel fit- and function-customized passive-dynamic ankle-foot orthosis design . The Intrepid Dynamic Exoskeletal Orthosis (IDEO) demonstrates the importance of fit and function customization and can be used as a basis to establish a powerful, objective design and prescription method for orthoses. (Figure originally published in Patzkowski [57])
To improve the customization of stiffness , orthotic joints have been developed with variable impedance for use in both ankle [58, 59] and knee [60] applications. These efforts aim to enable regulation of joint stiffness throughout the gait cycle. If successful, such joints could provide resistance to control segment or joint motion when necessary and reduce resistance to allow for greater range of motion when needed.
Alternatively, pneumatically powered, myoelectrically controlled AFOs and KAFOs are being developed to provide assistive torques about a joint [61, 62]. These orthoses have the potential to promote more natural gait [45], although to date use of these orthoses has been limited to the research laboratory. Finally, harnessing passive-dynamic properties, Ingimundarson and colleagues have designed a footplate with varying and tunable stiffness throughout its length to facilitate functional foot-to-floor motion and promote natural segment kinematics [63].
Devices have also been developed to address joint and segment alignment and kinematics. The primary feature of such devices is their ability to selectively lock or unlock the orthosis joint throughout the gait cycle, based on the phase of gait. The locking mechanism may be controlled by feedback from weight or pressure sensors [64], a pneumatic circuit connected to a pump embedded in the sole of the shoe [65], or an actuator with active control [66], in each case allowing it to integrate with passive or active devices. Customizing the alignment of the orthosis joint is important to customize its function. Pallari and colleagues have designed a pivot joint with customizable axis and a framework for integrating the joint into a customized subject-specific orthosis [67]. The pivot joint allows the axis of rotation to be customized to better mimic the rotation of an individual’s natural joint.
Takemura and colleagues are working to develop an AFO to control and measure ankle motion [68]. Their “Stewart Platform-Type” device has an adjustable rotation axis to better mimic natural ankle dynamics. While not yet translated to clinical practice, this orthosis design focuses on an important concept: the dynamic nature of joints. Joints naturally and automatically adjust their characteristics, such as location and orientation rotation axis, during a single activity (e.g., throughout the gait cycle) and between activities (e.g., walking vs. running). However, the dynamic nature of human joints is rarely captured in prosthetic and orthotic devices. Thus, the wide range of settings and adaptability of the Stewart Platform-Type orthosis in development holds great potential for enabling users to achieve high levels of function across a range of activities.
Orthoses Fabrication
Efforts to advance orthosis fabrication techniques focus on frameworks capable of rapid and cost-effective manufacturing. Because each prescribed device is unique – it is also important to improve key aspects of customized fit and function – the emphasis in the majority of these frameworks has been utilization of additive manufacturing.
Additive manufacturing, also referred to as 3D printing, uses a layer-by-layer approach by which material is additively joined to create a 3D component [69]. An array of additive manufacturing methods and materials are available. Recently, advancements in additive manufacturing now enable parts to be manufactured directly from CAD models and used in functional applications, not merely as prototypes [70, 71]. This new capability holds great promise for the manufacture of objectively customized orthotic devices and may simultaneously reduce time and cost associated with current methods. Additive manufacturing technology can be used to manufacture individual fit-customized components that are connected, via passive or active mechanical parts, to complete the function customization of the orthosis. An alternative is to use additive manufacturing to create fully fit- and function-customized passive-dynamic single-part orthoses [28,29,30,31].
Additive manufacturing requires the development of a CAD model of the customized orthosis. Traditional size and shape data are obtained to define the limb and are applied to drive the fit of a custom, patient-specific CAD model. These data first must be captured by the clinician through 3D scanning or 3D digitizing techniques, discussed previously in this chapter. Once developed, the geometry of the CAD model can be manually adjusted to customize its function. Often, finite element analysis is used to predict the mechanical properties of the device, and the CAD model geometry is then modified, iteratively or through an optimization scheme, until targeted mechanical properties are achieved [49, 50].
Researchers have demonstrated the feasibility of using additive manufacturing – in particular, selective laser sintering or fused deposition modeling – for foot and ankle-foot orthoses [28,29,30, 50, 72]. These studies created orthoses with targeted mechanical properties that mimicked commercially available devices [29] and foot orthoses with a range of stiffness values that had sufficient differences in mechanical properties to induce changes in subjects’ lower-extremity dynamics [72]. Others report work to characterize the properties of parts manufactured by selective laser sintering to derive accurate material properties for use in finite element modeling and thus to better predict and tune the functional characteristics of ankle-foot orthoses [71].
Despite the promise of additive manufacturing , the orthotic industry has yet to embrace this technology. One reason may be that many believe it is essential to use a hands-on approach to assess patients and align them for casting. Many of the approaches described above attempt to replicate hands-on assessment and alignment in a virtual CAD environment. These frameworks do require the subjective formation and development of a unique CAD model for each orthosis. Outsourcing the CAD modeling may be a cost-effective option [23], but many orthotists may prefer to work the design themselves.
To facilitate the use of CAD tools and rapid manufacturing for non-experts, one group developed a CAD support tool, which defined design constraints based on rapid manufacturing requirements and capabilities [70]. Alternatively, the process introduced by Schrank and Stanhope relies on shape conformance of a single, fully parameterized CAD model. Under this framework, the clinician digitally obtains and inputs a set of numerical parameters, indicating selections for fit and functional characteristics into a computerized form or spreadsheet. This triggers the CAD model to automatically adapt its size and shape to customize the orthosis [31]. Approaches such as these, which enable clinicians to objectively control orthosis fit and function without CAD expertise, appear promising but require additional substantial technological development. For instance, it is a substantial task to develop a fully parameterized CAD model with the complex geometry of an AFO that can self-adjust (without editing the model) to a wide range of sizes and shapes based on a minimal number of external instructions (parameters).
Orthosis Delivery Frameworks
Recognizing the importance of integrating objective prescription with advanced manufacturing methods, several research groups have proposed system of service frameworks to execute the full customization and fabrication process. Focusing on foot orthotics, Lowe eliminated the need for casting by using sensor pads to capture static and dynamic 3D data about the shape of the patient’s foot [73]. The data are then analyzed and quantified to determine specifications for orthosis customization. Use of software for analysis and quantification provides automation capabilities, which expedites the process and minimizes the need for practitioner input that could introduce subjectivity and variability into the process. The customized device design can then be sent directly to a manufacturing terminal.
Providing a firmer link between biomechanical assessment and orthosis design for athletes, Crabtree and colleagues present a system for the design and manufacture of personalized, symptom-specific sport insoles [74]. This framework describes how results from biomechanical assessments, ideally performed using reliable and repeatable methods, should be used to drive prescription (fit and function of the insole). The model is integrated with CAD technology (for customization of design and material) and CAM systems or other manufacturing methods for rapid and objective fabrication (Fig. 6.6). This framework encompasses the important concepts for objective customization and manufacture, including patient assessment, task demand, and device design, and so holds great potential to facilitate high levels of user function.
A proposed framework for designing and manufacturing customized foot orthoses . One of the most comprehensive frameworks currently presented in the literature, this framework conceptually links biomechanical patient assessment to orthosis design as well as incorporates a method for designing and objectively manufacturing the customized orthoses. (Figure originally published in Crabtree et al. [74])
Several frameworks have also been proposed for the objective customization and rapid fabricate of ankle-foot orthoses [26, 31, 50, 75]. In general, these frameworks focus on methods to (a) capture information pertaining to fit, (b) use computer modeling to design and customize orthosis function, and (c) fabricate the device using additive manufacturing technologies. The method proposed several years ago by Mavroids, Sivak, and colleagues used 3D laser scanning to capture shape characteristics of the patient’s ankle-foot complex. The digital data were then manually manipulated to create a customized computer model of the AFO [26, 75]. While effectively eliminating the process of producing a physical model of limb shape, the proposed framework relied on scanning techniques and manual manipulation of the virtual scan to customize the AFO computer model. These subjective steps introduce sources of potential variability in the process and make customizations difficult to repeat with precision.
Described previously in this chapter, the framework developed by Schrank and Stanhope uses a novel approach [31, 32], introducing an automated orthosis design and manufacturing framework (Fig. 6.7) whereby a fully parameterized CAD model automatically customizes its fit and functional characteristics based on prescription parameters and discrete 3D measurements of landmark locations. This eliminates the need for subjective manipulation of the computer model to customize design. Next, a parameterized optimization process and finite element analysis are used to modify the dimensions of functional components, thereby predicting and adjusting the bending stiffness of the fabricated AFO. This represents a powerful automated design and centralized manufacturing framework capable of objective functional design, but further research is needed to enhance the set of fabrication materials, add additional parameterized customizations, and – as is needed for all frameworks – define a prescription model that can drive orthosis function customization toward optimal functional outcomes .
A proposed framework for the automated design and rapid manufacture of orthotic devices. This framework combined with an objective prescription model that links patient assessment to orthosis design characteristic settings holds great potential for establishing a system of service to objectively and rapidly customize and manufacture orthoses that are optimally designed for every individual. (Figure originally published in Schrank and Stanhope [31])
Summary and Conclusions
Orthoses are traditionally prescribed and fabricated through a subjective process based primarily on qualitative guidelines and orthotist experience. While select clinical groups are making advances toward more objective design , the clinical field remains primarily craft based, relying on the knowledge, skills, and abilities of well-trained and experienced practitioners. The industry as a whole has not yet fully embraced modern technological capabilities for use in customized prescription of orthosis fit, function, and fabrication.
In recent years, the research and manufacturing communities have made great efforts to advance the field of orthotic devices. While the introduction of new technologies into the fitting process has been positive, gains have been incremental with limited integration into traditional clinical settings. Efforts to develop objective prescription guidelines to customize the function of orthoses are also underway but have proved equally challenging. Numerous important functional characteristics have been identified, including orthosis bending stiffness, footplate design, and alignment, and experimental devices have been designed to apply them. However, we have not yet achieved a comprehensive understanding of the interplay among the many factors that determine a patient’s level of impairment and those that promote desired functional outcomes. An improved understanding of that interplay is essential to the construction of objective fit and function prescription guidelines. Finally, novel technologies have been developed to manufacture custom orthoses rapidly with precisely tuned fit and functional characteristics, but use of these technologies remains limited by the strength, durability, and cost of available materials.
Frameworks have been proposed for the objective prescription and fabrication of orthoses whose fit and functional characteristics advance functional outcomes, but these have yet to be fully realized in practice. Innovative design and fabrication frameworks hold great potential to rapidly and objectively customize and manufacture orthoses. However, new frameworks need to be refined, tested, and integrated into clinical settings before they can be adopted as service models.
While research efforts are well on the way to establishing significant technological capabilities , the challenge lies in clinical implementation of these technological capabilities. Current reimbursement models , which drive the clinical orthotic field, do not support the use of the most advanced instrumentation in standard clinical settings. The most advanced technological capabilities are costly and not yet supported by adequate data to establish reliably improved outcomes. Quantitative evidence to demonstrate enhanced outcomes may provide the necessary incentive for third-party payers to increase reimbursement. It has been documented that patients who achieve high levels of function are more active, which in turn reduces the incidence of chronic health conditions. This is an important objective not just for those who use orthoses and prostheses but also for the broader population of citizens whose insurance premiums and taxes are applied to cover costs associated with health care generally. According to the Centers for Disease Control, 75% of all health-care costs in 2009 were due to chronic health conditions [76] and in 2011 amounted to a cost of approximately two trillion dollars [77].
Data are needed to demonstrate improved outcomes, associated long-term health benefits, and potential cost savings. Such an effort would likely require support through a large-scale consortium that links individual care system such as the US Department of Veterans Affairs (VA) and Department of Defense (DoD) medical treatment facilities with industry and academic centers of excellence. Without the constraints of current reimbursement models , the objective would be to access and use advanced instrumentation with relevant clinical populations to demonstrate and document evidence of impact. Within this same consortium model, research can continue in parallel to advance and optimize technologic capabilities, reduce costs, and streamline processes for implementation in the insurance-dependent civilian population. Ideally, results from coordinated basic and clinical research can pave the way to reimbursement for care that allows patients to live happier and healthier lives while also reducing the lifetime cost of health care.
Abbreviations
- AFOs:
-
Ankle-foot orthoses
- BRUCE:
-
Biarticular Reciprocating Universal Compliance Estimator
- CAD:
-
Computer-aided design
- CAM:
-
Computer-aided manufacturing
- IDEO:
-
Intrepid Dynamic Exoskeletal Orthosis
- FOs:
-
Foot orthoses
- KAFOS:
-
Knee-ankle-foot orthoses
- OEF:
-
Operation Enduring Freedom
- OIF:
-
Operation Iraqi Freedom
References
Harlaar J, Brehm M, Becher JG, Bregman DJJ, Buurke J, Holtkamp F, De Groot V, Nollet F. Studies examining the efficacy of ankle foot orthoses should report activity level and mechanical evidence. Prosthetics Orthot Int. 2010;34:327–35.
Shorter KA, Xia J, Hsiao-Wecksler ET, Durfee WK, Kogler GF. Technologies for powered ankle-foot orthotic systems: possibilities and challenges. IEEE/ASME Trans Mechatron. 2013;18:337–47.
Condie DN. The modern era of orthotics. Prosthetics Orthot Int. 2008;32:313–23.
Brault MW. Americans with disabilities: 2005. Curr Popul Rep US Census Bur. 2008:70–117.
Owens BD, Kragh JF, Macaitis J, Svoboda SJ, Wenke JC. Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma. 2007;21:254–7.
Patzkowski JC, Rivera JC, Ficke JR, Wenke JC. The changing face of disability in the US Army: the Operation Enduring Freedom and Operation Iraqi Freedom effect. J Am Acad Orthop Surg. 2012;20(Suppl 1):S23–30.
Masini BD, Waterman SM, Wenke JC, Owens BD, Hsu JR, Ficke JR. Resource utilization and disability outcome assessment of combat casualties from Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma. 2009;23:261–6.
(2010) Part B national summary data file.
Nielson CC. The future demand for orthotists and prosthetists: update 2002. Natl Comm Orthotic Prosthet Educ. 2002:1–27.
Bregman DJJ, De Groot V, Van Diggele P, Meulman H, Houdijk H, Harlaar J. Polypropylene ankle foot orthoses to overcome drop-foot gait in central neurological patients: a mechanical and functional evaluation. Prosthetics Orthot Int. 2010;34:239–304.
Brehm M, Bus SA, Harlaar J, Nollet F. A candidate core set of outcome measures based on the International Classification of Functioning, Disability and Health for clinical studies on lower limb orthoses. Prosthetics Orthot Int. 2011;35:269–77.
Malas BS. What variables influence the ability of an AFO to improve function and when are they indicated? Clin Orthop Relat Res. 2011;469:1308–14.
Ball KA, Afheldt MJ. Evolution of foot orthotics—part 2: research reshapes long-standing theory. J Manip Physiol Ther. 2002;25:125–34.
Ossur (2013) AFO dynamic. Foothill Ranch, California.
Ottobock (2013) WalkOn ® family of AFOs. Minneapolis, Minnesota.
(2013) Noodle AFO. Lutz, Florida.
Doxey GE. Clinical use and fabrication of molded thermoplastic foot orthotic devices. Suggestion from the field. Phys Ther. 1985;65:1679–82.
Bedotto RA. Biomechanical assessment and treatment in lower extremity prosthetics and orthotics: a clinical perspective. Phys Med Rehabil Clin N Am. 2006;17:203–43.
Pomeranz B. Prosthetics and orthotics for older adult with a physical disability. Clin Geriartic Med. 2006;22:377–94.
Perry J, Clark D. Biomechanical abnormalities of post-polio patients and the implications for orthotic management. NeuroRehabilitation. 1997;8:119–38.
Hijmans JM, Geertzen JHB. Development of clinical guidelines for the prescription of orthoses in patients with neurological disorders in The Netherlands. Prosthetics Orthot Int. 2006;30:35–43.
Smith DG, Burgess EM. The use of CAD/CAM technology in prosthetics and orthotics – current clinical models and a view to the future. J Rehabil Res Dev. 2001;38:327–34.
Sanders JE, Severance MR, Myers TR, Ciol MA. Central fabrication: carved positive assessment. Prosthetics Orthot Int. 2011;35:81–9.
Convery P, Greig RJ, Ross RS, Sockalingam S. A three centre study of the variability of ankle foot orthoses due to fabrication and grade of polypropylene. Prosthetics Orthot Int. 2004;28:175–82.
Telfer S, Woodburn J. The use of 3D surface scanning for the measurement and assessment of the human foot. J Foot Ankle Res. 2010;3:19.
Mavroidis C, Ranky RG, Sivak ML, et al. Patient specific ankle-foot orthoses using rapid prototyping. J Neuroeng Rehabil. 2011;8:1.
Telfer S, Gibson KS, Hennessy K, Steultjens MP, Woodburn J. Computer-aided design of customized foot orthoses: reproducibility and effect of method used to obtain foot shape. Arch Phys Med Rehabil. 2012;93:863–70.
Telfer S, Pallari J, Munguia J, Dalgarno K, McGeough M, Woodburn J. Embracing additive manufacture: implications for foot and ankle orthosis design. BMC Musculoskelet Disord. 2012;13:84.
Faustini MC, Neptune RR, Crawford RH, Stanhope SJ. Manufacture of passive dynamic ankle-foot orthoses using selective laser sintering. IEEE Trans Biomed Eng. 2008;55:784–90.
Pallari JHP, Dalgarno KW, Woodburn J. Mass customization of foot orthoses for rheumatoid arthritis using selective laser sintering. IEEE Trans Biomed Eng. 2010;57:1750–6.
Schrank ES, Stanhope SJ. Dimensional accuracy of ankle-foot orthoses constructed by rapid customization and manufacturing framework. J Rehabil Res Dev. 2011;48:31–42.
Stanhope SJ, Schrank ES. Process and System for Manufacturing a Customized Orthosis. Patent: United States Patent No. 8,538,570, 2013.
Chevalier TL, Chockalingam N. Effects of foot orthoses: how important is the practitioner? Gait Posture. 2011;35:383–8.
Ridgewell E, Dobson F, Bach T, Baker R. A systematic review to determine best practice reporting guidelines for AFO interventions in studies involving children with cerebral palsy. Prosthetics Orthot Int. 2010;34:129–45.
Owen E. The importance of being earnest about shank and thigh kinematics especially when using ankle-foot orthoses. Prosthetics Orthot Int. 2010;34:254–69.
Miyazaki S, Yamamoto S, Kubota T, Kubota T. Effect of ankle-foot orthosis on active ankle moment in patients with hemiparesis. Med Biol Eng Comput. 1997;35:381–5.
Sumiya T, Suzuki Y, Kasahara T. Stiffness control in posterior-type plastic ankle-foot orthoses: effect of ankle trimline Part 2: orthosis characteristics and orthosis/patient matching. Prosthetics Orthot Int. 1996;20:132–7.
Kobayashi T, Leung AKL, Hutchins SW. Techniques to measure rigidity of ankle-foot orthosis: a review. J Rehabil Res Dev. 2011;48:565–76.
Kobayashi T, Leung AKL, Akazawa Y, Hutchins SW. Design of a stiffness-adjustable ankle-foot orthosis and its effect on ankle joint kinematics in patients with stroke. Gait Posture. 2011;33:721–3.
Kobayashi T, Leung AKL, Akazawa Y, Hutchins SW. The effect of varying the plantarflexion resistance of an ankle-foot orthosis on knee joint kinematics in patients with stroke. Gait Posture. 2013;37:457–9.
Hansen AH, Childress DS, Miff SC, Gard SA, Mesplay KP. The human ankle during walking: implications for design of biomimetic ankle prostheses. J Biomech. 2004;37:1467–74.
Kao P-C, Lewis CL, Ferris DP. Invariant ankle moment patterns when walking with and without a robotic ankle exoskeleton. J Biomech. 2010;43:203–9.
Arch ES, Stanhope SJ. Passive-dynamic ankle-foot orthoses substitute for ankle strength while causing adaptive gait strategies: a feasibility study. Ann Biomed Eng. 2015;43:442–50.
Bartonek A, Eriksson M, Gutierrez-Farewik EM. A new carbon fibre spring orthosis for children with plantarflexor weakness. Gait Posture. 2007;25:652–6.
Takahashi KZ, Lewek MD, Sawicki GS. A neuromechanics-based powered ankle exoskeleton to assist walking post-stroke: a feasibility study. J Neuroeng Rehabil. 2015;12:1–13.
Arch ES, Reisman DS, Sniffen ZB, Stanhope SJ. A strength enhancement paradigm for prescription of passive-dynamic ankle-foot orthoses for individuals post-stroke. World Congr. Biomech. 2014;3(2):442–50.
Bregman DJJ, van der Krogt MM, de Groot V, Harlaar J, Wisse M, Collins SH. The effect of ankle foot orthosis stiffness on the energy cost of walking: a simulation study. Clin Biomech. 2011;26:955–61.
Bregman DJJ, Harlaar J, Meskers CGM, De Groot V, de Groot V. Spring-like ankle foot orthoses reduce the energy cost of walking by taking over ankle work. Gait Posture. 2012;35:148–53.
Ramsey JAA. Development of a method for fabricating polypropylene non-articulated dorsiflexion assist ankle foot orthoses with predetermined stiffness. Prosthetics Orthot Int. 2011;35:54–69.
Schrank ES, Hitch L, Wallace K, Moore R, Stanhope SJ. Assessment of a virtual functional prototyping process for the rapid manufacture of passive-dynamic ankle-foot orthoses. J Biomech Eng. 2013;135:101011–7.
Bregman DJJ, Rozumalski A, Koops D, de Groot V, Schwartz M, Harlaar J. A new method for evaluating ankle foot orthosis characteristics: BRUCE. Gait Posture. 2009;30:144–9.
Takahashi K, Stanhope SJ. Estimates of stiffness for ankle-foot orthoses are sensitive to loading conditions. J Prosthetics Orthot. 2010;22:211–9.
Fong DT-P, Pang K-Y, Chung MM-L, Hung AS-L, Chan K-M. Evaluation of combined prescription of rocker sole shoes and custom-made foot orthoses for the treatment of plantar fasciitis. Clin Biomech (Bristol, Avon). 2012;27:1072–7.
Jagadamma KC, Owen E, Coutts FJ, Herman J, Yirrell J, Mercer TH, Van Der Linden ML. The effects of tuning an ankle-foot orthosis footwear combination on kinematics and kinetics of the knee joint of an adult with hemiplegia. Prosthetics Orthot Int. 2010;34:270–6.
Eddison N, Chockalingam N. The effect of tuning ankle foot orthoses-footwear combination on the gait parameters of children with cerebral palsy. Prosthetics Orthot Int. 2013;37:95–107.
Patzkowski JC, Blanck RV, Owens JG, Wilken JM, Blair JA, Hsu JR. Can an ankle-foot orthosis change hearts and minds? J Surg Orthop Adv. 2011;20:8–18.
Patzkowski JC, Blanck RV, Owens JG, Wilken JM, Kirk KL, Wenke JC, Hsu JR. Comparative effect of orthosis design on functional performance. J bone Jt Surg. 2012;94:507–15.
Blaya JA, Herr H. Adaptive control of a variable-impedance ankle-foot orthosis to assist drop-foot gait. IEEE Trans Neural Syst Rehabil Eng. 2004;12:24–31.
Herr H, Blaya JA, Pratt GA. Active Ankle foot orthosis. Patent: United States Patent No. 8,075,633, 2011.
Bulea TC, Member S, Kobetic R, To CS, Audu ML, Schnellenberger JR, Triolo RJ. A variable impedance knee mechanism for controlled stance flexion during pathological gait. IEEE/ASME Trans Mechatron. 2012;17:822–32.
Gordon KE, Ferris DP. Learning to walk with a robotic ankle exoskeleton. J Biomech. 2007;40:2636–44.
Sawicki GS, Ferris DP. A pneumatically powered knee-ankle-foot orthosis (KAFO) with myoelectric activation and inhibition. J Neuroeng Rehabil. 2009;6:23.
Ingimundarson AT, de Roy K. Ankle-foot orthosis having an orthotic footplate. 2009. https://www.google.com/patents/US7513880.
Campbell JH, Zalinski N, Naft JM, Newman WS. Orthosis knee joint and sensor. 2008. https://www.google.tl/patents/US7410471.
Chin R, Hsiao-wecksler ET, Loth E, Kogler G, Manwaring SD, Tyson SN, Shorter KA, Gilmer JN. A pneumatic power harvesting ankle-foot orthosis to prevent foot-drop. J Neuroeng Rehabil. 2009;6:1–11.
Jonsson H, Clausen AV, Ingimarsson G, Lecomte C, Sigfusson L, Ragnarsdottir HG. Actuator assembly for prosthetic or orthotic joint. 2016. https://www.google.com/patents/US9351854.
Pallari JHP, Jens RW-S. Artificial exoskeleton device or an orthotic device comprising an integrated hinge structure. 2011. https://www.google.com/patents/US20110009787.
Takemura H, Onodera T, Ming D, Mizoguchi H. Design and control of a wearable Stewart Platform-type ankle-foot assistive device. Int J Adv Robot Syst. 2012;9:1–7.
Kim GD, Oh YT. A benchmark study on rapid prototyping processes and machines: quantitative comparisons of mechanical properties, accuracy, roughness, speed, and material cost. Proc Inst Mech Eng Part B J Eng Manuf. 2008;222:201–15.
Smith PC, Rennie AEW. A computer aided design (CAD) support tool for parametric design of products from rapid manufacture (RM). In: Bartolo P, editor. Innovative developments in design and manufacturing advanced research in virtual and rapid prototyping – Proceedings of VRP4. CRC Press; 2009. p. 95–100. http://www.crcnetbase.com/doi/10.1201/9780203859476.ch13, https://www.routledge.com/Innovative-Developments-in-Design-and-Manufacturing-Advanced-Research/Silva-Bartolo-Artur-Jorge-da-Conceicao-Batista-Almeida-Matias-Correia-Vasco-Gaspar-Correia-Andre- Alves-Novo-Goncalves-Martinho-Carvalho/p/book/9780415873079.
Muraru L, Pallari JHP, Creylman V, Vander Sloten J, Peeraer L. SLS nylon 12 characterization through tensile testing and digital image correlation for finite element modeling of foot and ankle-foot orthoses. Proc Solid Free Fabr Symp. 2010. p. 828–833.
Toon D, Vinet A, Pain MTG, Caine MP. A methodology to investigate the relationship between lower-limb dynamics and shoe stiffness using custom-built footwear. Proc Inst Mech Eng Part P J Sport Eng Technol. 2011;225:32–7.
Lowe CE. System and method for creating Orthtoics. 2007. https://google.com/patents/WO2005086857A3?cl=sv.
Crabtree P, Dhokia VG, Newman ST, Ansell MP. Manufacturing methodology for personalised symptom-specific sports insoles. Robot Comput Integr Manuf. 2009;25:972–9.
Sivak ML, Ranky RG, DiPisa JA, Caddle AL, Gilhooly KL, Govoni LC, Sivak SJ, Lancia M, Bonato P, Mavroidis C. Patient specific ankle-foot orthotic device. 2009.
National Center for Chronic Disease Prevention and Health Promotion. Chronic diseases the power to prevent, the call to control. 2009
Centers for Medicare & Medicaid Services. National health expenditures 2001 highlights. 2011
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media LLC
About this chapter
Cite this chapter
Arch, E.S., Stanhope, S.J. (2017). Orthotic Device Research. In: Tepe, V., Peterson, C. (eds) Full Stride. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-7247-0_6
Download citation
DOI: https://doi.org/10.1007/978-1-4939-7247-0_6
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-7245-6
Online ISBN: 978-1-4939-7247-0
eBook Packages: MedicineMedicine (R0)