Abstract
Brain parenchyma microvasculature is set in disarray in the presence of tumors, and malignant brain tumors are among the most vascularized neoplasms in humans. As microvessels can be easily identified in histologic specimens, quantification of microvascularity can be used alone or in combination with other histological features to increase the understanding of the dynamic behavior, diagnosis, and prognosis of brain tumors. Different brain tumors, and even subtypes of the same tumor, show specific microvascular patterns, as a kind of “microvascular fingerprint,” which is particular to each histotype. Reliable morphometric parameters are required for the qualitative and quantitative characterization of the neoplastic angioarchitecture, although the lack of standardization of a technique able to quantify the microvascular patterns in an objective way has limited the “morphometric approach” in neuro-oncology.
In this chapter we focus on the importance of the computational-based morphometrics, for the objective description of the tumoral microvascular fingerprinting. By also introducing the concept of “angio-space,” which is the tumoral space occupied by the microvessels, we here present fractal analysis as the most reliable computational tool able to offer objective parameters for the description of the microvascular networks.
The spectrum of different angioarchitectural configurations can be quantified by means of Euclidean and fractal-based parameters in a multiparametric analysis, aimed to offer surrogate biomarkers of cancer. Such parameters are here described from the methodological point of view (i.e., feature extraction) as well as from the clinical perspective (i.e., relation to underlying physiology), in order to offer new computational parameters to the clinicians with the final goal of improving diagnostic and prognostic power of patients affected by brain tumors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Angioarchitecture
- Brain tumor
- Fractal dimension
- Fractal analysis
- Glioblastoma multiforme
- Microvascularity
1 Introduction
The brain is among the most perfused organs of the human body, and in order to meet its high metabolic demand, it has one of the most complex vascular and microvascular systems. Different regions of the brain are characterized by specific microvascular networks [8, 22–24, 38] whose level of complexity most likely reflects the function related to that specific area [11]. Since tumors are supported by different patterns of vascularization [34], it is possible to speculate that tumorigenesis (i.e., the sequential accumulation of mutations within tissue cells) is related to the disarray of the physiological microvascular bed or even related to a programmed rearrangement of a new and specific microvascular network. The study of the neoplastic angioarchitecture seems to be of paramount importance not only for research purposes but for clinical applications as well since it has been shown that the “normalization” of the abnormal microvascular architecture of tumors by means of anti-angiogenic agents, for example, can reduce regional hypoxia and eventually increase the efficacy of therapies [32, 33]. According to this model, the imbalance between pro- and anti-angiogenic factors in a tumor disorganizes the angioarchitecture, which might be brought back from its irregular pathological state to a physiologic state and then “normalized.” Fractal analysis offers several tools for the quantification and temporal follow-up of such angiostructural changes [25, 44].
2 Brain Tumors and Vascularization
The latest available World Health Organization (WHO 2007Footnote 1) grading system classifies brain tumors according to histological features in a sort of benign-to-malignant gradient (from grade I to grade IV, with grade IV being the most malignant) [41]. The grading has diagnostic, prognostic, and therapeutic value, considering that grade I lesions have low proliferative and infiltrative potential, and can be virtually cured by means of surgery and/or radiosurgery alone, while grade IV cancer requires multimodal approaches (i.e., surgery followed by radio-chemotherapy) and has fatal prognosis.
Malignant brain tumors are among the most vascularized tumors in humans [41]. As microvessels can be easily identified in biopsy specimens, it has been suggested that quantification of microvascularity might be used alone or in combination with other histological features to increase the understanding of the dynamic behavior and prognosis of brain tumors, as well as for diagnostic purposes. However, microvascularity is not always considered a feature related to brain tumor grading. Microvascular proliferation is considered a histopathological hallmark of glioblastoma multiforme (GBM) [41], which is the most frequent and malignant glioma (WHO grade IV), but the differences in microvascularity between grade II and III gliomas, for example, are less clear and not used for grading. Also, meningiomas of different grades, as well as meningiomas in comparison to hemangiopericytomas, clearly display different vascular patterns (see Table 24.1), but other features are still used to differentiate the different grades and/or tumors [2]. This is also related to the lack of standardization of a technique able to quantify the microvascular patterns in an objective way.
The vascularization of malignant brain tumors is the target for anti-angiogenic treatment (such as bevacizumab), providing reasoning on the importance of the different methods in quantifying and assessing the changes in tumor microvascularity. On one hand, it is true that different brain tumors show different angiogenic patterns, but on the other it seems that single histotypes, such as GBM, show a very highly heterogeneous microangioarchitecture [5, 17, 18, 45]. We here summarize the concepts and methods related to microvascular detection and image analysis for the following morphometric analyses.
2.1 Immunohistochemistry (IHC)
In histological specimens, microvessels can be detected by means of IHC. Several antibodies have been described for the immunodetection of the endothelium, each one with its own pros and cons, summarized in Table 24.2. The most commonly used are CD34 and CD31 (CD refers to “cluster of differentiation”), which are considered pan-endothelial markers, while CD105 and Endocan are more commonly used for newly formed vessels (i.e., in the process of angiogenesis). Factor VIII and Ulex europeus agglutinin I (UEAI) have almost fallen into disuse due to their multiple limitations. The ratios of CD34:CD105, CD34:Endocan, or CD31:Endocan immunoreactive vessels can provide the “angiogenic fraction” of the tumor [Di Ieva, unpublished results].
3 Morphometrics of Microvascularity
Qualitative rather than quantitative analyses have generally been used to describe the differences in the vascularization of the normal brain vs. brain tumors.
It has been suggested that vessel quantification can be added into the tumor classification system for grading as well as for prognostication. If the aim is to provide a morphometric biomarker (i.e., predicting patient prognosis, treatment response, etc.), the limitations are due to the lack of standardization of the proposed parameters. Morphometrics aims to reduce shapes to numbers, offering a reductionist approach to describe the geometrical complexity of natural objects. In pathology, morphometric analyses add a quantitative element to the qualitative description of the tissue [11], generating continuous variables, which can be used for statistical comparison.
Defining the “tumor-space” as the neoplastic volume, the “angio-space” refers to the proportion of microvessels filling such volume, not just in terms of quantity but also in terms of size, shape, and pattern of distribution [11].
Pathologists recognize distinct vascular angiogenic subtypes, described as palisades, glomeruloid vascular proliferation, vascular garlands, vascular clusters, and microvascular sprouting, and may also use semiquantitative scores to quantify the level of “clusterization” of the microvessels [20] (see Table 24.3). This seems to be relevant, especially when considering the relationship between vascular patterns and clinical outcomes, as different angiogenic protein expression associated with different angioarchitecture can respond in different ways to chemotherapy [5]. These descriptions lack standardization and some intra- and interobserver variability may be present.
Since the introduction of the use of the vessel density in 1972 [6], several other parameters have been proposed as potential “quantitators” of the microvascular system, used to quantify the angio-space (Tables 24.3 and 24.4).
We here classify these morphometric parameters in “Euclidean-based” and “fractal-based” parameters.
3.1 Euclidean-Based Parameters
One of the most used parameters is the microvessel density (MVD), based on the measure of the number of immunostained microvessels per square millimeter in the most densely vascularized area of the histological specimen (termed “hot spot”). Different techniques have been proposed for the MVD calculation, and several seminal papers have investigated its role in every human tumor (see review in [14]), including the brain and pituitary tumors (reviews in [13, 14]), but in conclusion it has been shown that it is not a valid measure for guiding and/or evaluating anti-angiogenic treatment [31], nor for distinguishing different grades of brain tumors. All the histological analyses are limited by the sampling, especially in GBMs, which show a very high histologic heterogeneity. The greatest limitation of the use of the MVD is the choice of the hot spot, due to (a) high inter- and intra-observer variability in its selection, (b) potential lack of representativity of the whole specimen, and (c) potential lack of representation of a complex 3D structure, such as the microvascular tree, in a 2D histological area [15, 18, 43].
Other Euclidean parameters can be computed on the histological specimens of brain tumors (see Table 24.3). Multiparametric analyses of combinations of such indices have shown microvascular morphometrics as a valid tool to differentiate different grades of brain tumors [18, 37, 45].
The greatest limitation of the described parameters is that Euclidean geometry can only quantify regular and smooth objects, and therefore can only offer approximations of the roughness expressed by natural objects, such as the microvascular trees. The complexity of vascular systems depends on (a) the number of vessels, (b) their size and shape, and (c) the pattern of the vessel distribution and the nonlinear, temporal, and spatial advance of the promotion, progress, mediation, and inhibition of angiogenesis generating the complex ramified network irregularly filling the environment surrounding the tumor, which can be described by Euclidean geometry only with great approximation [28].
Fractal geometry overcomes the limits of Euclidean parameters. The fractal-based parameters are described next.
3.2 Image Analysis
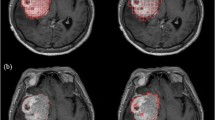
The first step to apply any morphometric analyses on the neoplastic angio-space is the choice of the technique to visualize the microvessels and the following image analysis, which should be standardized (see Chap. 12) (Fig. 24.1).
When the target of analysis is the microvascular network, several issues have to be considered, for example, whether the analysis is performed on the basis of the space-filling area of the vessels or on skeletonized representations of the microvessels.
In the image analysis, eventual artifacts related to the segmentation of immunoreactive vessels have to be considered. For example, nonspecific immunoreactivity can limit the automatic detection of the vessels, as in the case when antigens diffuse to other compartments (e.g., CD34 antigens which immunostain cell nuclei or necrotic areas rather than endothelial cells). In such cases, a pathologist is still required to identify any artifacts, which should be eliminated from the analysis.
Other digital image acquisition calibration parameters should be standardized as well, in terms of regulating the light intensity of the microscope, maintaining the same resolution over the whole series, and using an identical threshold to extract the immunoreactive vessels. A virtual microscope can be used to digitize the entire specimen rather than few areas selected manually. The vessels can be extracted as a whole from the specimen and organized in a vascular catalog, giving a snapshot on the number and shape of the microvessels within the specimen (Fig. 24.2).
4 Fractal-Based Morphometric Analyses of Microvessels
Fractal geometry provides a computer-aided method to describe and quantify the roughness and geometrical complexity of the microvessels distributed within the tumor, as it has been shown in a vast variety of neoplasia, including prostate, kidney, lung, colon, skin, and brain tumors as well. By concentrating on the irregularity of tumor growth rather than individual measure of size (such as diameter and volume or other Euclidean parameters), fractal geometry is well suited to quantify the morphological features that pathologists have long used to describe malignancies in a qualitative way (i.e., wrinkled borders within the host tissue, random microvascular patterns, etc.) [4]. Several researchers have demonstrated the fractality (or “semi-fractality”) and multifractality of the vascular and microvascular trees of many tissues and organs, in physiologic as well as pathologic states, including the human brain [1, 2, 4, 8–10, 26, 27, 29, 35, 40, 44, 47].
The main aim of computational fractal-based analysis of the microvascular patterns is the quantification of parameters, which can be used as surrogate biomarkers.
4.1 Microvascular Fractal Dimension (mvFD)
The most widely used parameter in fractal geometry is the fractal dimension (FD or D F), which describes the space-filling properties of irregularly shaped objects [3, 9, 10, 26]. FD has been shown to be the most robust estimator of vascular networks [36, 49]. Extending the use of FD to the quantification of microvessels, the microvascular fractal dimension (mvFD) quantifies the space-filling properties of the microvessels within a tissue; in the case of a tumor, mvFD quantifies the level of geometrical complexity of the microvessels embedded within the tumor. The mvFD adds a qualitative component to the parameterization of the angio-space, trying to answer the following question: assuming an equal number of vessels, what can be said about their shape, size, and pattern of distribution? This means that histological specimens of similar or different tissues can show the same value of MVD or total vascular area, for example, but a very different pattern of distribution, with different values of mvFD. Of course, it can also happen that histological tissues with same mvFD values differ for the Euclidean parameters, making the approaches complementary methods of quantification. Therefore, mvFD offers useful information about the tumoral space filled by microvessels. The parameter is computer aided, and its objective measure makes it a comparable parameter among different operators. If it is important to analyze the distribution of the vessels within the tissue, by means of FD, for example, it is equally important to analyze complementary parameters, the “vascular gappiness,” that is, the avascular spaces, by means of the lacunarity or other methods, like the distance maps [44].
In a 2D histological specimen, mvFD ranges from 0 to 2. For example, a tumor with a hypothetical mvFD value of 1.95 owns a microvascular network almost filling its area, like the Peano’s curve, with a very complex geometric and highly space-filling microvascular pattern (Fig. 24.3). This microvascular pattern virtually fills the whole tissue in which it is embedded, reducing the avascular spaces to the minimum (therefore increasing the lacunarity) [3] (Fig. 24.4). In the 3D space, such as in electron microscopy reconstructions of the microvascular trees in the 3D volume, FD trends toward a maximal value of 3 [44, 47].
Values of the fractal dimension (FD) on a 2D plane, comparing two fractal objects with the microvasculature (endothelial CD34 immunostaining) of a pituitary adenoma (lower image) with the specimen of a normal pituitary gland. The lower image on the left shows the Koch’s curve (“snowflake”), with FD = 1.26. FD increases in more space-filling objects, namely, in the Peano’s curve (higher image on the left, with FD ≈ 2) and in the microvasculature of the normal pituitary gland, which is more homogeneously distributed within the parenchyma of the gland
Specimens of three cases of GBM, showing different microvasculature (microvessels detected by using antibodies raised against CD34 with brown coloration). The angio-space of each tumor can be described by means of several parameters (TVA total vascular area, mvFD microvascular fractal dimension, loc bcD local box-counting dimension. See Table 24.4)
In several kinds of tissues, it has been shown that FD and lacunarity values differ in the physiological and pathological vascular networks [3, 19, 25]. This means that the disarray of the microvascular network, which extends from the normal tissue (e.g., the brain) to the tumor, can be quantified by means of fractal analysis, in a kind of gradient of morphometric differences between tissues. Based on the evidence that the neoplastic microvascular network is abnormal, it has been experimentally shown that the “normalization” of such disarray can be used for therapeutic purposes, as previously quoted, and the FD can be used as a surrogate biomarker for diagnosis and/or treatment follow-up [3, 25]. By means of 2D and 3D analyses, FD values of normal brain microvasculature have been found to be higher than that of neoplastic regions, meaning that the normal brain is better suited to more space-occupying microvasculature [3, 25, 47]. However, due to the use of different methods and techniques, these results are controversial. For example, in one experimental study, the vascular FD values of primate and rat brain tumors have been found to be higher than those of normal brain parenchyma, thus indicating a greater metabolic supply and bigger surface area for gas exchange within the tumors [44]. In numerical terms, fractal-based demonstration that tumoral and normal vascular networks are intrinsically different; Baish et al. introduced a complementary metric to the FD, the tortuosity, defined as the ratio between the minimum vascular path joining two points and their geometric distance from each other [3]. A greater tortuosity has been correlated with a worse response to drugs, confirming again the importance of the analysis of the angiostructure from the therapeutic perspective.
Among several reasons, including their relative simplicity and the speed to be computed, the most used methods to compute mvFD are the box-counting and the sandbox methods (see Chap. 2). These methods have been applied to whole histological specimens of brain tumors as well as on selected spots. The choice of the “hot spot” can be performed manually (i.e., the pathologist chooses the area subjectively considered to be the most vascularized and representative of the microvascular network of the tumor) or by computer-aided methods (e.g., the spot with the highest vascular area, as calculated by the computer). The first method is biased by the introduction of the operator-dependent choice of the hot spot, while the second method can be biased by the operator-dependent choice of the threshold to automatically extract the immunoreactive vessels from the specimen or from manually erasing artifacts outside the region of interest. An ideal method should be objective and reproducible, without any operator-dependent biases. Moreover, as it often happens in pathology, the analysis can be biased by the choice of the specimen itself (the problem of sampling, which could not be representative of the whole tumor, like a sample resembling a WHO grade II glioma within a grade III tumor). To limit this problem, other parameters have been introduced.
4.2 Local Fractal Dimension and Local Box-Counting Dimension
In order to avoid the sampling of nonrepresentative areas of the tumors such as necrotic areas, the local fractal dimension considers FD in the hot spot. The subjective selection of the hot spot would limit the objective reproducibility of such parameters in the same way as with the MVD. In order to avoid such limitations, the hot spot can be automatically chosen, for example, by computing the vascular area for each 1 mm2 area on a grid drawn on the specimen (Fig. 24.5) and extracting the spot with the highest ratio (immunoreactive surface of vessels/tumoral area). Once selected, the 1 mm2 spot with the highest vascular area becomes the hot spot for the following analysis (Figs. 24.5 and 24.6). On such a spot, the local mvFD can be computed. A previous analysis showed that a monofractal behavior was found considering a two orders of magnitude window, that is, between 1 and 100 μm [20]. Assuming an average microvessel diameter between 5 and 10 μm, such a fractal window considers the smallest features of the microvessels (i.e., the roughness of the outline), as well as the agglomerate of micro-clusters of vessels (at the magnitude of 100 μm). As shown, this was considered insufficient to cover the entirety of the histopathological features of the microvessels, such as the macro-agglomerates in large clusters (like the garland-like vascular structures). A fractal window ranging between 1 μm and 1 mm, that is, covering three orders of magnitude, was considered significant to cover all of the mean histopathological characteristics of the microvessels, including the intrinsic morphologic features and their clustering properties. Applying the box-counting method in such a range, a monofractal behavior was not confirmed (see Fig. 24.6), although a similar slope of the curve was found across all the analyzed specimens. The several power laws showed that glioma microvascularity clearly demonstrates a multifractal distribution of geometrical complexity of the glioma’s microvessels when observed at various scales of magnification. The slope of a straight line interpolating the points on the log-log graphs was considered as the mean value expressing the space-filling properties of the microvessels in the hot spot, and the value was indicated as the local box-counting dimension (local bcD) [20]. Both mvFD and local bcD express, in a single variable, the ability of the microvessels to fill the space in which they are embedded (i.e., the tumor), which is a characteristic intrinsically correlated to their number, size, shape, and distribution pattern.
Microvascular map for the automatic selection of the hot spot. Over-imposing a grid of 1 mm2 boxes on the entire specimen, the vascular area can be computed on each box and a color map can be associated to the different ratios. In this example, the yellow boxes represent the regions of the specimen with the highest vascular area. Raw data show also the value of the vascular area for each box, and the one with the highest value is automatically chosen as hot spot for the following computational analyses (software by Carlo Russo)
Computer-aided technique for fractal analysis of the microvasculature in histological specimens. Estimation of the morphometric fractal parameter in the whole section and in the hot spot region of specimens of brain gliomas; detection of microvessels using antibodies raised against CD34. The extraction of the whole specimen and the segmentation of the immunoreactive vessels (a, b) allow the automatic measurement of the morphometric parameters listed in Table 24.4. Moreover, a grid of boxes measuring 1 mm to a side length is superimposed on the whole histological section. For each box, the ratio between the local vascular area and the local neoplastic area is calculated [local A(%)]; the box with the highest local A(%) is automatically selected and extracted to be used as the “hot spot” representative of the whole specimen (c). (d) Hot spot of the specimen, automatically extracted. (e) Selection of the RGB threshold to automatically extract the CD34+ vessels. (f) Box-counting method: superimposition on the image of grids with boxes of different lengths, from a minimum size (ε min ) to a maximum size (ε max ), in the preselected scaling window. (g) A monofractal behavior was found by limiting the scaling window to a range of two orders of magnitude (ε min = 1 μm – ε max = 100 μm). The slope of the obtained curve is the microvascular fractal dimension (mvFD) [Axes of the log-log graph (box-counting method): X-axis = Box size (mm); Y-axis = N Boxes]. (h) Considering that a maximum size of the box of 100 μm does not cover the complete hot spot, a wider scaling window was also applied (Reproduced from Di Ieva et al. [20])
5 Fractal-Based Analysis of the Angio-Space in Brain Pathology
We define the concept of “angio-space” as the set of parameters quantifying the microvasculature within a tumor or the tumoral space occupied by its own angioarchitecture (Di Ieva [19] and unpublished data). According to the speculation that different tumors, or even different subtypes of the same tumor have a specific “microvascular fingerprint” [19], it has been speculated that a gradient of geometrical representation (and then of fractal angioarchitectural parameters, including FD) exists between physiological and pathological tissues, as well as different states of the same tissues. The pituitary gland is an exemplary model: Euclidean-based approaches (i.e., vascular area and MVD) and fractal-based analyses have clearly shown that it is not only more vascularized but also exhibits a higher microvascular heterogeneity and geometrical complexity in the comparison of the pituitary adenomas [13, 16, 21]. Regarding the different subtypes of pituitary adenomas, analyses of the MVD have shown very discordant results [13], with some preliminary fractal-based analyses not showing any statistically significant differences in the angioarchitecture of micro- vs. macro-adenomas, for example [Di Ieva, unpublished results]. The pituitary gland is a simple model from which to extend the fractal analysis of the microvasculature to the study of brain tumors, by analyzing histological specimens treated with antibodies raised against the endothelium (in the whole specimen and/or hot spots), or volumetric reconstructions of histological tissues and/or radiological images (see Chaps. 19, 20, 21, 22, and 23). If the pituitary gland shows a relatively low variability of the microvascular patterns (meaning that the vascular network is quite homogeneous) [12], malignant brain tumors show very high microvascular heterogeneity. By analyzing 114 GBM specimens, a mean mvFD value of about 1.44 (ranging 1.06–1.87) was found, with a coefficient of variation (CV, standard deviation divided by the mean) of 44 % [18]. For comparison, the CV of pituitary adenomas was found less than 10 % [12]. This very high variability in the space-filling properties of microvascularity of GBM reflects the very high angioarchitectural heterogeneity shown by this malignant tumor. The microvascular networks of GBM can be represented in a very broad and continuous spectrum of possible geometric configurations; this was the first mathematical demonstration that GBM is multiforme (from the Latin meaning “multi-shapes”) also in relation to its microvascularity [18].
Morphometric and computational fractal-based analyses also showed that grade II gliomas have different angio-spaces in comparison to grade III gliomas (Fig. 24.7). Among several morphometric parameters, the local mvFD and especially the local bcD were shown to be the most reliable quantitative indicators of the neoplastic microvasculature, making them potential surrogate biomarkers [20]. The histopathological grading of gliomas can be challenging in some cases, especially in grade II vs. grade III gliomas, and the erroneous diagnosis can result in patients’ over- or undertreatment [48]. For this reason, computational methods, which can help in differential diagnosis, are more than welcome to be added in the pathologists’ and clinicians’ armamentarium.
Correlation between the fractal angiomorphometric parameters and the level of clustering of the microvessels. Schema showing the correlation between the angioscore assigned by the neuropathologist to each specimen and the fractal-based variables [local box-counting dimension (loc bcD) and microvascular fractal dimension (mvFD)]. The value reported for each angioarchitectural group is the mean value of loc bcD ± standard deviation. The yellow line indicates the increasing grade of malignancy of the tumor. The fractal parameters assigned nearly 75 % of the gliomas to the correct histological grade and angioscore (Reproduced from Di Ieva et al. [20])
6 Limitations
If fractal-based angioarchitectural classification of brain tumors can be useful for diagnostic and prognostic purposes, there are still some limitations to acknowledge. For a description of the limitation of image and fractal analysis, see Chaps. 1 and 12. Below, we summarize some main points. First of all, according to the basic principles of fractal geometry, it does not mean that objects owning the same mvFD, for example, show the same microvascular pattern. As previously stated, this means that fractal indexes should be analyzed as complementary to other morphometric parameters in a multiparametric analysis.
When the analysis is performed on histological specimens, the sampling problem can limit its benefit. The analysis of the whole specimen or of the computationally chosen most representative spot of the specimen tends to decrease the limitations of other analyses, like the MVD-based ones, but a histological sample still often does not represent anything more than a very small fraction of the whole tumor, and this should be taken into consideration. The estimation of a 2D representation of the microvascular tree could not reflect the real 3D complexity of the microvascular network, because 2D methods performed on histological specimens are length related rather than mass related, and this can underestimate the true 3D complexity of the tree in the space [7, 42]. This issue can be limited by using volumetric analyses and 3D reconstructions of tissues. The effect of geometrical deformation (e.g., cracks) during the process of sample preparations, and other artifacts such as nonhomogeneity of staining, may also have some impact on the accuracy of the fractal analysis. For this reason, also the sampling, immunostaining and preparation of the histological specimen should be standardized.
Moreover, the histological section represents a “snapshot” in time, a “frozen photo” of the tumor at the moment of the surgical operation, and each quantification refers to that specific moment, not taking in account the dynamic process on the temporal trend of the tumor. For this reason, the temporal changes of tumors should also be considered by means of neuroradiological and/or nuclear medicine findings over time (such as perfusion parameters or methionine uptake in PET, positron emission tomography) [17].
As previously stated, the value of FD and other fractal-based parameters is highly dependent on the image analysis parameters (and “pixel related”, according to the resolution). Several research inquiries have considered different tissues (brain cortex, tumors) in different models (humans, rats), visualized in different ways after undergoing different treatments. When comparing the several values found in the published research, a plethora of results show contrasting findings, and this could be avoided only by a standardization of techniques, materials, and methods.
The standardization ought to be done also in the analytical analysis of the fractal parameters. It is in fact known that biological fractals, such as microvascular networks, are statistically self-similar only within a specific scaling window (i.e., covering at least two orders of magnitude) [40]. The choice of different windows may give different results, and such choice should be standardized as well or at least justified: if a window ranging 1–100 μm, for example, considers a FD that reflects the organization of the vessels in micro-clusters and their roughness, on the other hand, a range of 100–10,000 μm does not take into account the roughness of the single vessels but rather the distribution of vascular clusters on a larger scale [14]. The lack of standardization of all these elements could produce results no more comparable between different laboratories. Last but not least, microvessels cannot be real fractals, as pointed out, and the “fractalization” of such natural objects can be a mathematical idealization limited by computational manipulation. In order to avoid the several definitions expressed in the very thick related literature on fractality, quasi-fractality, pseudo-fractality, or multifractality of microvessels [27, 39, 46, 50, 51], it is here enough to say that fractal analysis, far from being an infallible and universal method, is still able to offer several reliable parameters for an objective, reproducible, and realistic description and quantification of the microvascularity in normal as well as pathological tissues.
7 Future Perspectives and Conclusion
As the architectural pattern of each tumor seems to be its specific microvascular fingerprinting, objective and reproducible morphometric biomarkers are required to describe and quantify the so-called angio-space. Such indexes should be (a) able to quantify what pathologists describe in a qualitative way on the histological specimens of tumors, (b) objective, that is, not affected by intra- and interobserver variability, and (c) clinically meaningful, having prognostic and/or predictive value [20]. Fractal analysis offers several parameters that are promising candidates for such purposes.
In addition, the methodological phase of testing morphometric parameters should be followed by clinically oriented research; to be tested as a potential biomarker, in fact, the morphometric fractal-based parameters should be analyzed in the same way that new oncologic therapies are introduced into clinical practice, in step-by-step successive phases of study [30]. Although the translation of the concept of “fractal microvascularity” into clinical practice (i.e., from “bench to bedside”) is still difficult to be realized [11], it should be emphasized that the research in the field of microvessel morphometrics should run alongside research focused on tumoral angiogenesis (research on molecular biomarkers, such as vascular endothelial growth factor, hypoxia-induced factor, etc.), in order to offer a holistic view on the effects of structure and function on the environment and viability of brain tumors. This means that the morphometric analyses should run alongside the biological approach. Moreover, morphometric analyses should be integrated into in vivo techniques (neuroimaging and nuclear medicine methods) to follow-up brain tumors and response to treatment.
In light of the speculations and findings that have been illustrated in this chapter, computational fractal-based and multiparameter morphometric analyses will ultimately find its place in the oncologist’s toolbox as a conventional diagnostic procedure.
Notes
- 1.
At the time of the chapter writing, the WHO classification system for brain tumors published in 2016 was not available yet.
References
Al-Kadi OS. Texture measures combination for improved meningioma classification of histopathological images. Pattern Recog. 2010;43:2043–53.
Al-Kadi OS. A multiresolution clinical decision support system based on fractal model design for classification of histological brain tumours. Comput Med Imaging Graph. 2015;41:67–79.
Baish JW, Gazit Y, Berk DA, et al. Role of tumor vascular architecture in nutrient and drug delivery: an invasion percolation-based network model. Microvasc Res. 1996;51:327–46.
Baish JW, Jain RK. Fractals and cancer. Cancer Res. 2000;60:3683–8.
Birner P, Piribauer M, Fischer I, et al. Vascular patterns in glioblastoma influence clinical outcome and associate with variable expression of angiogenic proteins: Evidence for distinct angiogenic subtypes. Brain Pathol. 2003;13:133–43.
Brem S, Cotran R, Folkman J. Tumor angiogenesis: a quantitative method for histologic grading. J Natl Cancer Inst. 1972;48:347–56.
Caserta F, Eldred WD, Fernandez E, et al. Determination of fractal dimension of physiologically characterized neurons in two and three dimensions. J Neurosci Methods. 1995;56:133–44.
Cassot F, Lauwers F, Fouard C, et al. A novel three-dimensional computer-assisted method for a quantitative study of microvascular networks of the human cerebral cortex. Microcirculation. 2006;13:1–18.
Cross SS, Start RD, Silcocks PB, et al. Quantitation of the renal arterial tree by fractal analysis. J Pathol. 1993;170:479–84.
Cross SS. The application of fractal geometric analysis to microscopic images. Micron. 1994;25:101–13.
Di Ieva A, Tschabitscher M. Fractal-based classification of brain tumors angioarchitecture. In: Murray SR, Mitchell EW, editors. Classification and applications of fractals: new research. New York: Nova Science Publishers; 2012. p. 205–16.
Di Ieva A, Grizzi F, Ceva-Grimaldi G, et al. Fractal dimension as a quantitator of the microvasculature of normal and adenomatous pituitary tissue. J Anat. 2007;211:673–80.
Di Ieva A, Grizzi F, Gaetani P, et al. Euclidean and fractal geometry of microvascular networks in normal and neoplastic pituitary tissue. Neurosurg Rev. 2008;31:271–81.
Di Ieva A. Angioarchitectural morphometrics of brain tumors: are there any potential histopathological biomarkers? Microvasc Res. 2010;80:522–33.
Di Ieva A, Grizzi F. Microvessel density. J Neurosurg Pediatr. 2010;6:304–6; author reply 306.
Di Ieva A, Grizzi F, Ceva-Grimaldi G, et al. The microvascular network of the pituitary gland: a model for the application of fractal geometry to the analysis of angioarchitecture and angiogenesis of brain tumors. J Neurosurg Sci. 2010;54:49–54.
Di Ieva A, Grizzi F, Tschabitscher M, et al. Correlation of microvascular fractal dimension with positron emission tomography [(11)C]-methionine uptake in glioblastoma multiforme: preliminary findings. Microvasc Res. 2010;80:267–73.
Di Ieva A, Grizzi F, Sherif C, et al. Angioarchitectural heterogeneity in human glioblastoma multiforme: a fractal-based histopathological assessment. Microvasc Res. 2011;81:222–30.
Di Ieva A. Fractal analysis of microvascular networks in malignant brain tumors. Clin Neuropathol. 2012;31:342–51.
Di Ieva A, Bruner E, Widhalm G, et al. Computer-assisted and fractal-based morphometric assessment of microvascularity in histological specimens of gliomas. Sci Rep. 2012;2:429.
Di Ieva A, Weckman A, Di Michele J, et al. Microvascular morphometrics of the hypophysis and pituitary tumors: from bench to operating theatre. Microvasc Res. 2013;89:7–14.
Duvernoy HM, Delon S, Vannson JL. Cortical blood vessels of the human brain. Brain Res Bull. 1981;7:519–79.
Duvernoy HM. Vascularization of the cerebral cortex. Rev Neurol (Paris). 1999;155:684–7.
Duvernoy HM. Comments on the microvascularization of the brain. Cerebrovasc Dis. 2006;21:423–4.
Gazit Y, Baish JW, Safabakhsh N, et al. Fractal characteristics of tumor vascular architecture during tumor growth and regression. Microcirculation. 1997;4:395–402.
Goldberger AL, West BJ. Fractals in physiology and medicine. Yale J Biol Med. 1987;60:421–35.
Grasman J, Brascamp JW, Van Leeuwen JL, et al. The multifractal structure of arterial trees. J Theor Biol. 2003;220:75–82.
Grizzi F, Russo C, Colombo P, et al. Quantitative evaluation and modeling of two-dimensional neovascular network complexity: the surface fractal dimension. BMC Cancer. 2005;5:14.
Grizzi F, Colombo P, Taverna G, et al. Geometry of human vascular system: is it an obstacle for quantifying antiangiogenic therapies? Appl Immunohistochem Mol Morphol. 2007;15:134–9.
Hainfellner JA, Heinzl H. Neuropathological biomarker candidates in brain tumors: key issues for translational efficiency. Clin Neuropathol. 2010;29:41–54.
Hlatky L, Hahnfeldt P, Folkman J. Clinical application of antiangiogenic therapy: microvessel density, what it does and doesn’t tell us. J Natl Cancer Inst. 2002;94:883–93.
Jain RK. Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med. 2001;7:987–9.
Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62.
Jain RK, di Tomaso E, Duda DG, et al. Angiogenesis in brain tumours. Nat Rev Neurosci. 2007;8:610–22.
Kedzia A, Rybaczuk M, Andrzejak R. Fractal dimensions of human brain cortex vessels during the fetal period. Med Sci Monit. 2002;8:MT46–51.
Kirchner LM, Schmidt SP, Gruber BS. Quantitation of angiogenesis in the chick chorioallantoic membrane model using fractal analysis. Microvasc Res. 1996;51:2–14.
Korkolopoulou P, Patsouris E, Kavantzas N, et al. Prognostic implications of microvessel morphometry in diffuse astrocytic neoplasms. Neuropathol Appl Neurobiol. 2002;28:57–66.
Lauwers F, Cassot F, Lauwers-Cances V, et al. Morphometry of the human cerebral cortex microcirculation: general characteristics and space-related profiles. Neuroimage. 2008;39:936–48.
Lorthois S, Cassot F. Fractal analysis of vascular networks: insights from morphogenesis. J Theor Biol. 2010;262:614–33.
Losa GA. The fractal geometry of life. Riv Biol. 2009;102:29–59.
Louis DN, Ohgaki H, Wiestler OD, et al. WHO classification of tumours of the central nervous system. Lyon: International Agency for Research on Cancer (IARC); 2007.
Mandelbrot BB. The fractal geometry of nature. New York: W.H. Freeman; 1982.
Preusser M, Heinzl H, Gelpi E, et al. Histopathologic assessment of hot-spot microvessel density and vascular patterns in glioblastoma: poor observer agreement limits clinical utility as prognostic factors: a translational research project of the European organization for research and treatment of cancer brain tumor group. Cancer. 2006;107:162–70.
Risser L, Plouraboue F, Steyer A, et al. From homogeneous to fractal normal and tumorous microvascular networks in the brain. J Cereb Blood Flow Metab. 2007;27:293–303.
Sharma S, Sharma MC, Gupta DK, et al. Angiogenic patterns and their quantitation in high grade astrocytic tumors. J Neurooncol. 2006;79:19–30.
Takahashi T. Microcirculation in fractal branching networks. Tokyo: Springer; 2014.
Vakoc BJ, Lanning RM, Tyrrell JA, et al. Three-dimensional microscopy of the tumor microenvironment in vivo using optical frequency domain imaging. Nat Med. 2009;15:1219–23.
van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician’s perspective. Acta Neuropathol. 2010;120:297–304.
Vico PG, Kyriacos S, Heymans O, et al. Dynamic study of the extraembryonic vascular network of the chick embryo by fractal analysis. J Theor Biol. 1998;195:525–32.
Zamir M. On fractal properties of arterial trees. J Theor Biol. 1999;197:517–26.
Zamir M. Fractal dimensions and multifractility in vascular branching. J Theor Biol. 2001;212:183–90.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Di Ieva, A., Al-Kadi, O.S. (2016). Computational Fractal-Based Analysis of Brain Tumor Microvascular Networks. In: Di Ieva, A. (eds) The Fractal Geometry of the Brain. Springer Series in Computational Neuroscience. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3995-4_24
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3995-4_24
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3993-0
Online ISBN: 978-1-4939-3995-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)