Abstract
Proximal hamstring injuries can be a debilitating injury in active individuals. In some patients, nonoperative treatment can result in poor functional outcomes and inability to return to pre-injury levels of activity. Recent studies suggest that surgical repair of proximal hamstring injuries can improve functional outcomes and increase the chances of successful return to sporting activities. Prompt recognition and sound surgical technique are critical in achieving optimal outcomes. This chapter reviews the treatment algorithm for patients with proximal hamstring injuries and includes a focus on the surgical anatomy of the proximal hamstring, ischial tuberosity, and sciatic nerve. While the mainstay of treatment remains open surgical technique, a brief review of the endoscopic technique is included as well.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Rupture of the proximal origin of the hamstring tendons is a relatively uncommon injury classically described as a waterskier injury that occurs with violent eccentric contraction of the hamstring in a position of knee extension and hip flexion [1]. While hamstring strains at the muscle belly or myotendinous junction account for 25–30 % of all strains and, in fact, are the most commonly strained muscle group in the athlete [2, 3], true proximal hamstring ruptures account for just 9–12 % of all hamstring injuries [4]. It is important to recognize these proximal injuries promptly as delays in diagnosis can affect the overall outcome.
The mechanism of injury in acute ruptures most commonly involves a sudden and unexpected flexion of the hip with the knee in an extended position. Proximal hamstring injuries were coined as the “waterskier injury” as the novice water skier was pulled suddenly by the tow rope leading to a rapid flexion moment at the hip with the knees locked in an extended position, while the waterskis provided tremendous counterforce to the pull of the boat. One could imagine how the proximal hamstring may rupture under such tremendous tension and load.
While water skiing certainly accounts for many of these injuries, in reality, a wide variety of activities can result in proximal hamstring rupture (Fig. 33.1). The most common mechanism of injury in our clinic involves the patient’s foot slipping on a wet surface. The patient’s stable leg remains anchored in one position, while the unstable leg juts violently in front of the body creating an inadvertent “splits” maneuver resulting in damage to the proximal hamstring complex.
Oftentimes, the patient reports a history of a “pop” or a series of “pops” and when asked to localize the pain points to the proximal lower gluteus and proximal posterior thigh. Initially the injury can seem innocuous, and the inexperienced clinician may falsely diagnose these injuries as a hamstring muscle strain. However, with a suspicious mechanism of injury, such as a slip on a wet floor and a history of a pop, the clinician should error on the side of caution and order an MRI to assess the level and severity of the injury.
Usually within 48–72 h, a significant ecchymosis is apparent in the midthigh region, which quickly darkens and extends distally sometimes all the way to the foot (Fig. 33.2). While some mild ecchymosis may occur in a mid hamstring muscle strain, it is nowhere near the severity and size of the ecchymotic changes seen in a proximal hamstring avulsion injury.
Although hamstring strains reliably heal after a period of rest and dedicated physiotherapy, nonoperative management of complete ruptures and high-grade partial ruptures may result in low return to sports, persistent pain, weakness, and instability [5–9]. While the natural history of partial tears is not clearly defined, certain partial tears, particularly those with retraction greater than 2 cm and tendinous detachment greater than 50 %, have also been shown to do poorly with nonoperative management [9–11].
Given the unreliable results with nonoperative management, the trend has been toward open repair with suture anchor fixation as the surgical method of choice [2, 5, 9, 10, 12–17]. This can be performed through either a transverse or vertical incision. Whereas open repair leads to high rates of good and excellent outcomes in both the acute and chronic setting [18, 19]; complications include wound dehiscence 2.4 % [20], wound infection 1–2.4 % [16, 20, 21], seroma 2.4 % [20], posterior cutaneous neuralgia 9.8–40 % [15, 20], hypertrophic scar formation 2.0 % [16], wound fistula 1.1 % [11], incisional numbness 60.9 % [12], and cosmetic deformity 60.9 % [12].
Arthroscopic and endoscopic techniques have been used throughout sports medicine in an effort to minimize surgical incisions, decrease morbidity, and speed recovery. In an effort to mitigate the potential morbidity of an open repair, advanced surgical techniques have allowed us to endoscopically treat some of these injuries to the proximal hamstring. Here we present a case example of one of our patients treated with endoscopic repair of a proximal hamstring injury.
Case Description
The patient is a very active 53-year-old female who presented 6 weeks months after sustaining an injury to her right hamstring while sprinting during a soccer match. She attempted rest and rehabilitation but complained of persistent pain, weakness, and inability to return to explosive acceleration required in sports that she enjoyed including recreational soccer. The exertional symptoms included cramping of the mid-substance hamstring musculature as well as sharp pain and sitting intolerance at the ischial tuberosity region. On physical examination, she had tenderness over the ischial tuberosity with a small palpable defect over the proximal hamstring origin. She had pain with resisted knee flexion and slightly decreased sensation in the sciatic nerve distribution. MRI revealed a high-grade partial avulsion with approximately 2 cm of retraction (Fig. 33.3a, b). Given that she had failed conservative management and desired to return to soccer, she elected to undergo proximal hamstring repair, and an endoscopic approach was discussed as an option.
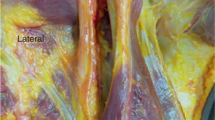
Under general endotracheal tube anesthesia, the patient was placed in the prone position with the gluteal and posterior thigh prepped and draped. The first portal, the direct posterior portal, was made in the gluteal crease over the proximal hamstrings. The arthroscope was placed into the subgluteal space and, using a low-pressure pump, the space was insufflated with fluid; the subgluteal is defined as the space between the gluteus maximus and proximal hamstring fascia. Under direct visualization, a second portal, the posterolateral portal, was made in the gluteal crease just lateral to the first portal, directly over the lateral facet of the ischial tuberosity. An arthroscopic shaver was carefully used to debride the ischial bursa and develop the subgluteal space (Fig. 33.4). Working laterally, the shaver was used bluntly to identify the sciatic nerve. Several adhesions were bluntly dissected from the sciatic nerve. Care was taken to avoid damage to the sciatic nerve throughout the remainder of the case. Next, the ischial tuberosity and proximal hamstring ruptured fibers were visualized (Fig. 33.5). Approximately 60 % of the tendon footprint was detached and retracted. All scar tissues were debrided. The torn and retracted fibers were thoroughly debrided and “freshened” in an effort to enhance healing upon refixation. A combination of clear cannulas and Passport cannulas was placed into each of the portals. The dissection using the motorized shaver was carried distally 4–5 cm which was helpful in mobilizing the tendon stump and would allow easier reduction to the footprint. An arthroscopic grasper was used to assess mobilization of the tendon (Fig. 33.6). Next, a single 4.5 mm double-loaded poly-ether-ether-ketone (PEEK) corkscrew anchor was used (Arthrex, Naples, FL), and sutures were passed using a combination of angled crescent suture passers and the Scorpion Fastpass suture passer device (Arthrex, Naples, FL). A horizontal mattress configuration was made. A second anchor was placed, and similar suture passing through the proximal hamstring tendon was performed. With the knee flexed, the tendon was easily reduced to the bone using standard arthroscopic suture technique and then tied in place (Fig. 33.7). Solid reduction and fixation were confirmed while flexing and extending the knee.
The patient was discharged home the same day. Aspirin 325 mg was used for 1 month for DVT prophylaxis. A hinged knee brace initially locked in 70° of flexion was progressively brought into full extension over the next 10–14 days. The patient was kept non-weight bearing until full extension was achieved. Weight bearing was then gradually progressed to full by 6 weeks, and crutches were abandoned. Physical therapy and range of motion exercises were initiated at this point. Strengthening exercises began at 12 weeks with progressive return to sport at 4–6 months. Final follow-up was 1 year after the surgery. The patient had normal muscular contour, full strength, and range of motion and had returned to competitive recreational soccer at the same level as prior to the injury. The numbness that was experienced preoperatively had resolved.
Discussion Points
Anatomic Considerations of the Proximal Hamstring Region
The anatomy of the proximal hamstring is important to review as it has significant implications particularly when attempting surgical intervention whether in an acute or chronic setting. The two most important anatomic considerations involve the sciatic nerve and the true anatomic footprint of the proximal hamstring tendon.
The sciatic nerve courses in close approximation to the proximal hamstring origin at the ischial tuberosity. The sciatic nerve is located just lateral to the proximal hamstring and proceeds to course distally before arborizing and sending branches to each of the muscle bellies of the hamstring complex. The sciatic nerve has two distinct bundles at the proximal level called the tibial branch and the peroneal branch. The tibial branch supplies innervation to the three main muscles of the hamstring complex including the semimembranosus, semitendinosus, and the long head of the biceps femoris. The short head of the biceps femoris muscle is innervated by the peroneal branch of the sciatic nerve, but it is important to note that the short head of the biceps femoris does not contribute to the proximal hamstring tendon.
Important neurovascular structures lurk proximally as well. The inferior gluteal neurovascular bundle lies just 5.0 cm proximal to the inferior border of the ischial tuberosity [22]. Whether the approach to the area is performed endoscopically or in an open fashion, care must be taken not to place retractors or instruments into this zone.
Proximally the sciatic nerve also gives off a purely sensory branch called the posterior femoral cutaneous nerve (PFCN). This nerve branch supplies sensation to a large portion of the posterior thigh skin. It takes off from the sciatic nerve just proximal to the level of the ischium and darts superficially through the gluteus maximus and into the subcutaneous layer of the skin of the posterior thigh. The PFCN is particularly vulnerable to injury when making the approach to the proximal hamstring. Injury can occur as a direct transection of the PFCN or one of its branches or more commonly as a neuropraxia while retracting the gluteus maximus muscle.
The sciatic nerve is at risk during the surgical dissection and approach to the proximal hamstring region. In its native state, the sciatic nerve lies in close approximation to the ischial footprint of the proximal hamstring attachment. In an injured state following rupture, the disrupted hamstring fibers are avulsed violently and retract distally away from the bone and oftentimes come to rest in even closer apposition to the course of the sciatic nerve. As part of the normal healing response, scar tissue formation inevitably occurs between the ruptured tendinous fibers and the sciatic nerve. Patients may develop a significant sciatic neuritis, which can become a chronic situation in some instances. The typical complaints of sciatica occur with attempted contraction of the hamstring musculature; as the muscle contracts, if the sciatic nerve is tethered to the contracting musculotendinous complex, the result is a painful tug on the nerve resulting in sciatic pain. One of the arguments for early proximal hamstring repair is to ensure that the proximal hamstring tendon is carefully dissected away from the nearby sciatic nerve, thus mitigating the risk of future sciatic neuritis.
Review of Literature of Proximal Hamstring Repair
Excellent results can be expected with open repair of proximal hamstring tendon avulsions. Sarimo et al. [20] reported on 41 patients (average age, 46 years) with complete ruptures of the proximal hamstring. Seventy-one percent had good-to-excellent results with repair. Those with moderate-to-poor results had a mean time to surgery of 11.7 months, suggesting that early surgical intervention is ideal.
Birmingham et al. [12] followed 23 patients with an average age of 46 years who underwent surgical repair for complete rupture of the proximal hamstring. Ninety-one percent returned to their sport at the same level within 10 months. Isokinetic testing revealed hamstring strength of 90 % compared to the contralateral side.
Wood et al. [9] reported on 72 proximal hamstring ruptures with an average age of 40 years that underwent surgical repair. Forty cases, including seven incomplete ruptures, were chronic cases that had failed nonoperative management. Postoperative hamstring strength and endurance were 84 % and 89 %, respectively, compared to the contralateral extremity. Patients with preoperative sciatic nerve symptoms from retracted ruptures were significantly weaker than those without. Eighty percent of patients returned to sport at their pre-injury level by 6 months.
Lempainan et al. [16] reported their results on surgical repair of 48 partial tears of the proximal hamstring tendons. Forty-two patients had failed conservative management. All patients were athletes (average age, 33 years) including 13 professional and 15 competitive athletes. Eight-eight percent had a good-to-excellent outcome and returned to pre-injury level of sports after an average of 5 months.
While results with open repair of the proximal hamstring ruptures are good, complications have been described. Wound complications include dehiscence, infection, fistula, seroma, hypertrophic scar formation, and cosmetic deformity. Neurologic complications include posterior cutaneous nerve numbness or hyperesthesia, neuroma, and incisional numbness [11, 12, 15, 16, 20].
Additionally, while the open technique is straightforward, gluteus maximus retraction can be difficult, particularly with larger or more muscular individuals. Care must be taken with prolonged retraction as the inferior gluteal neurovascular bundle lies just 5.0 cm proximal to the inferior border of the ischial tuberosity [22]. Deep retractors and a head lamp are necessary as are 1–2 assistants, thus making this procedure cumbersome in general.
The current literature regarding endoscopic proximal hamstring is limited. A technical report on endoscopic proximal hamstring technique including a case presentation was published by Domb and Gerhardt [23]. Another case report on endoscopic proximal hamstring repair was published by Guanche et al. [24] There are no current studies comparing open versus endoscopic proximal hamstring repair.
Despite the lack of comparative studies, it appears that endoscopic repair of proximal hamstring rupture provides potential advantages over the traditional open technique. Endoscopic repair avoids larger incisions, avoids risk of excessive gluteus maximus retraction, and inflicts minimal disruption of normal anatomy. This may result in decreased incidence of neurovascular complications.
Visualization can prove challenging in the open approach, and this can lead to a nonanatomic repair. Sitting pain is a known side effect following open proximal hamstring repair, and it is likely secondary to imprecise attachment of the tendon to the incorrect region of the ischial footprint. The endoscopic approach clearly allows for superior visualization of the ischial tuberosity, which is crucial for anatomic recreation of the proximal hamstring footprint on the lateral facet of the ischium.
Endoscopy also allows for improved evaluation of partial thickness tears; this becomes increasingly valuable as evidence mounts on the poor outcomes seen with nonoperative management of partial tears.
While these factors may lead to decreased complications, faster recovery, and improved results, endoscopic proximal hamstring repair is technically challenging. The sciatic nerve must be respected during portal placement and endoscopic dissection. Operative times can be longer than the open approach, particularly at the beginning of the learning curve. Due to the endoscopic nature of the procedure, the authors recommend working in a low-pressure environment to minimize the risk of extravasation into the local soft tissue planes. If significant swelling occurs at any point, it is recommended that conversion to a traditional open approach be performed to complete the repair. In our experience, conversion to an open procedure after a failed endoscopic attempt causes no deleterious effects in outcomes and therefore a low threshold to conversion if any untoward events occur during attempted endoscopic repair.
References
Blasier RB, Morawa LG. Complete rupture of the hamstring origin from a water skiing injury. Am J Sports Med. 1990;18:435–7.
Chalal J, Bush-Joseph CA, Chow A, Zelazny A, Mather RC, Lin E, Gupta D, Verma NN. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures. Does the tendon heal? Am J Sports Med. 2012;40:2325–30.
Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237–48.
Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582–9.
Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures—a systematic review. Int J Sports Med. 2011;32:490–5.
Kurosawa H, Nakasita K, Nakasita H, Sasaki S, Takeda S. Complete avulsion of the hamstring tendons from the ischial tuberosity: a report of two cases sustained in judo. Br J Sports Med. 1996;30:72–4.
Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23:702–5.
Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996;24:130–6.
Wood DG, et al. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90:2365–74.
Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350–5.
Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009;37:727–34.
Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93:1819–26.
Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13:411–8.
Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30:742–7.
Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34:119–23.
Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40:688–91.
Miller SL, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A surgical technique. J Bone Joint Surg Am. 2008;90 Suppl 2(Part 1):108–16.
Folsom GJ, Larson CM. Surgical treatment of acute versus chronic proximal hamstring ruptures. Am J Sports Med. 2008;36:104–9.
Sallay PJ, et al. Subjective and functional outcome following surgical repair of complete ruptures of the proximal hamstring complex. Orthopedics. 2008;31:1092.
Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36:1110–5.
Carmichael F, et al. Avulsion of the proximal hamstring origin: surgical technique. J Bone Joint Surg Am. 2009;91 Suppl 2:250–6.
Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A cadaveric study. J Bone Joint Surg Am. 2007;89:44–8.
Domb BG, Linder D, Sharp KG, Sadik A, Gerhardt MB. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013;2(1): e35–9.
Dierckman BD, Guanche CA. Endoscopic proximal hamstring repair and ischial bursectomy. Arthrosc Tech. 2012;1(2):e201–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Gerhardt, M.B., Schub, D.L. (2015). Proximal Hamstring Pathology and Endoscopic Management. In: Brockmeier, S. (eds) MRI-Arthroscopy Correlations. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2645-9_33
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2645-9_33
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2644-2
Online ISBN: 978-1-4939-2645-9
eBook Packages: MedicineMedicine (R0)