Abstract
Early and accurate diagnosis of pulmonary vascular disease is important given the high mortality of untreated pulmonary hypertension. The development of cardiopulmonary exercise testing (CPET) has allowed an early diagnosis of PAH in “at risk” patients or those with suggestive clinical findings. CPET can quantify the degree of exercise impairment, and rule out a pulmonary mechanical limit to exercise. It can also be used to monitor disease progression and response to treatment. CPET generally consists of an incremental symptom-limited cycling or treadmill exercise test with measurements of ventilation and pulmonary gas exchange. Noninvasive testing is done with continuous 12-lead ECG, cuff blood pressure monitoring and pulse oximetry. Invasive CPET adds arterial and pulmonary artery catheters for blood gas, pH and pressure measurements. CPET when used in the context of a diagnostic algorithm, can confirm the diagnosis of exercise-induced PH, distinguish between pulmonary arterial and venous hypertension, and rule out confounders such as impaired systemic O2 extraction. CPET may be used alone or combined with other modalities, such as transthoracic cardiac Doppler echo and MRI. Recent expert consensus statements suggest CPET is useful in the diagnosis, management and risk stratification of PH. This chapter provides an overview of the history of CPET, describes how measurements are obtained and interpreted, and discusses its use in diagnosis and monitoring of pulmonary hypertensive diseases including exercise-induced pulmonary hypertension and pulmonary hypertension associated heart and lung disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The timely and accurate diagnosis of PH is important given the high mortality if left untreated [1, 2], the availability of increasingly effective medical therapies [3] and a long wait for a donor lung at most transplant centers [4]. The development of cardiopulmonary exercise testing (CPET) has allowed an early diagnosis of PH in “at risk” patients or those with subtle suggestive clinical findings, affording the opportunity to treat patients most likely to benefit and to monitor their response.
PH carries a poor prognosis, with a mortality of about 15 % in 1 year despite modern therapy. The diagnosis of PH is often delayed; the average time from onset of symptoms to diagnosis is approximately 2 years [2]. The delay is due, in part from the nonspecific signs and symptoms of the disease, and the complex, extensive workup necessary to determine a cause of elevated pulmonary artery pressure. Traditional evaluation of resting pulmonary function and gas exchange is insensitive [5, 6], and further contributes to the diagnostic delay. Early PH generally does not cause symptoms at rest and stressing pulmonary vasculature with exercise may be necessary to demonstrate abnormal structure and function [2, 7–10]. An appropriate analogy might be that of coronary artery disease; a resting left heart catheterization identifies severe disease, but milder hemodynamically significant disease requires a functional study for its diagnosis.
Cardiopulmonary exercise testing (CPET) is such a functional test that may elicit early [7] and reproducible [11, 12] abnormalities suggestive of PH. CPET generally consists of an incremental symptom-limited cycling or treadmill exercise test with measurements of ventilation and pulmonary gas exchange [13, 14]. The first CPET done was in the Harvard Fatigue Lab in the 1920s (Fig. 11.1) where many of the basic tenets of normal human exercise physiology were described using measurements of ventilation, pulmonary gas exchange, arterial blood gases and pH as well as noninvasive estimates of cardiac output.
Currently, CPET is subdivided into noninvasive testing (niCPET), done with continuous 12-lead ECG, cuff blood pressure monitoring and pulse oximetry, and invasive CPET (iCPET), which adds arterial and pulmonary artery catheters for blood gas, pH and pressure measurements. CPET may be used alone or combined with other modalities, such as transthoracic cardiac Doppler echo and MRI. There is a rapidly growing body of evidence supporting its utility in patients with suspected or confirmed PH. Recent expert consensus statements suggest CPET’s is useful in the diagnosis, management and risk stratification of PH [15, 16]. CPET is safe even in established PH [17, 18] Severe PH with exertional syncopal episodes, cardiac arrhythmias, or acute right ventricular failure do, however, serve as contraindications to maximum exercise testing [13].
Noninvasive CPET
niCPET can be used as a screening test in the patient with unexplained exertional intolerance [14, 19] where a significant percentage of patients will ultimately be shown to have PH [7]. Such patients have generally undergone a time-honored history, physical examination, routine blood work, which are normal or, in the eyes of the clinician, show abnormalities insufficiently severe to explain symptoms. niCPET may also be appropriate in suspected PH, e.g., family members of Group 1 PH, or in “at risk” patients with for example connective tissue disease [20].
niCPET can quantify the degree of exercise impairment, rule in or out a pulmonary mechanical limit to exercise and suggest disorders manifested by abnormal O2 delivery or subsequent uptake and utilization, including PH. niCPET variables that are useful in assessing the presence and severity of PH are shown in Table 11.1. These variables largely reflect PH-related impairment of O2 delivery to the exercising muscle bed and ventilation-perfusion abnormalities in the lung [17, 21–25]. Additionally, niCPEt allows reproducible assessment of functional capacity and treatment efficacy in PH and can predict survival [11, 17, 22, 26–28].
Maximum Oxygen Uptake (VO2max)
Overall fitness is generally assessed by the VO2max, expressed as a percent of predicted for the patient’s age, gender and estimate of lean body mass, derived from height [29] VO2 increases linearly vs. work rate with a slope of approximately 10 mL/min/W in normal subjects [29]. This slope is not affected by age, gender, or training, but is shifted leftward in obese patients and may plateau in more severe heart failure (HF). In the obese patient, in the absence of pulmonary vascular disease, the VO2 max may be surprisingly well-preserved, but the external work performed on the cycle ergometer is compromised. This results from the oxygen cost of moving heavy legs or respiratory muscle work.
In established PH, VO2max decreases [7, 17, 23–25, 28, 30, 31]. Even milder exercise-induced PH depresses VO2max compared to normal [7, 10]. VO2max correlates inversely with resting pulmonary hemodynamics [17] and may improve with pulmonary vasodilator therapy [27, 32], but this is not uniformly observed [21], perhaps in part because of methodological concerns, but perhaps related to confounding deleterious effects of treatment.
VO2max is a powerful predictor of mortality in PAH [33, 34] and a peak VO2 below 10.4 mL/kg/min has been considered a key criterion for early mortality [22].
Ventilatory (VAT) or Gas Exchange “Anaerobic” Threshold (AT)
Heavy exercise increases blood lactate concentration, ventilation and VCO2 relative to VO2; the latter can be reliably detected noninvasively with CPET using an iterative least residual sum of the squares of a two-segment log–log plot [35]. For many years the lactic acidemia of exercise was assumed to be secondary to inadequate oxygen delivery to muscle with resultant increases in “anaerobic” glycolysis to produce ATP. However, skeletal muscle mitochondrial redox state is actually higher when working muscle is producing lactate than at rest, implying that oxygen supply is not the critical factor [36–38]. Likewise, the tight mechanistic link between LT and VAT has been under mined by the fact that the two may be uncoupled experimentally [39–41] and in McArdle’s disease [42] where ventilatory patterns during incremental exercise are normal in the absence of lactic acidemia. Nonetheless, the AT varies with cardiovascular fitness, correlates well with human performance in the field, and remains a useful clinical index.
The VAT occurs at greater than 40 % of the predicted VO2max in normal individuals, but earlier in cardiovascular disease including PH [17, 43, 44]. The AT correlates inversely with resting pulmonary hemodynamics [17] in established PH.
Ventilatory Reserve
Minute ventilation (VE) normally rises during incremental exercise as a result of a linear increase in breathing frequency and a hyperbolic increase in tidal volume (VT) [45]. VT reaches a plateau at approximately 50 % of the resting vital capacity, above which the elastic work of breathing is prohibitive [46]. The ratio of VE at peak exercise (VEmax) to the maximal voluntary ventilation (MVV) at rest has been termed the breathing reserve index [47]. A breathing reserve index of 0.70 can be sustained for 15 min in normal individuals, but values above 0.75 are usually not attained even at peak exercise [48].
Ventilation in patients with Group 1 PH may be excessive [49], but because the maximum voluntary ventilation is usually near-normal, relatively normal breathing reserve at peak exercise is usually found [17]. The niCPET can rule out a pulmonary mechanical limit to exercise by comparing VEmax to MVV. This is especially important in Group 3 PH where there are both pulmonary vascular and mechanical abnormalities limiting exercise. When an abnormal VAT precedes a BRI of 0.70, pulmonary vascular disease likely limits the patient’s activities of daily living. Conversely, when a BRI of 0.70 precedes the AT, pulmonary mechanics are thought to be rate limiting.
Ventilatory Efficiency
Normally, CO2 elimination by the lungs becomes more efficient during exercise [50]. Anatomic dead space increases because of a tethering effect on conducting airways at high VT. Conversely, during upright exercise, alveolar dead space decreases because of augmented blood flow to the lung apices, giving the net effect of a slight increase in total (physiologic) dead space (VD). However, this effect is more than offset by the increased VT, which produces a decrease in upright VD/VT from 0.45 at rest to less than 0.29 at maximum exercise [50]. Normally, the VE/VCO2 falls as a result to <37 at the ventilatory threshold [17].
Ventilatory inefficiency is one of the hallmarks of PH during exercise [7, 17, 23–25, 28, 30, 31, 51] and can be identified by an increased slope of the linear phase of VE/VCO2 or its absolute value at the ventilatory threshold. It has been suggested that the latter is preferable as the slope may be artificially flattened by hyperventilation at rest in anticipation of exercise.
A high VE/VCO2 during the submaximum domain of incremental exercise is explained by the alveolar ventilation equation:
-
\( \mathrm{V}\mathrm{E}/\mathrm{V}\mathrm{C}\mathrm{O}2=(k)/(\mathrm{PaCO}2\;\left(1-\mathrm{V}\mathrm{D}/\mathrm{V}\mathrm{T}\right) \). [17]
Hyperventilation during low-level exercise is common in PH and usually ascribed to a combination of stretch receptors in the RV and pulmonary outflow track, J receptor stimulation (in HF and interstitial lung disease) and hypoxemic stimulation of arterial chemoreceptors [52]. In addition, alveolar dead space fails to fall normally [17, 53, 54] because of blunted pulmonary vascular distention and recruitment, and, perhaps, pulmonary vasospasm [55].
Thus, the combined influence of two invasively measured variables, VD/VT and PaCO2 may make the noninvasive VE/VCO2 a powerful marker of the abnormal pulmonary vasculature. Using a stepwise regression model using PaCO2 and VD/VT at anaerobic threshold as independent variables suggested that variability in VE/VCO2 at anaerobic threshold was accounted for equally by both. In HFrEF we have demonstrated equal contributions of VD/VT and hyperventilation to ventilatory efficiency [56].
Reybrouck et al. [54] found that the VE/VCO2 slope was steeper in patients with PH than the slope in patients with normal mPAP, and a significant correlation between the slope and mPAP and the VD/VT. In PH, VE/VCO2 is inversely related to peak cardiac output [55], resting [17], and exercise [57] mPAP’s and overall exercise capacity [54, 58] A sudden rise may suggest dynamic opening of a PFO and right to left shunting during exercise [23].
Ventilatory inefficiency can predict adverse events [59] and is likely a better predictor of survival than VO2max [22, 34, 60]. Recent work suggests [60] ventilatory equivalent for carbon dioxide at anaerobic threshold >55 identifies patients with an over sevenfold increased risk of death within 24 months and better predicted the clinical outcome compared to VO2max < 10.4 ml/min/kg.
Ventilatory efficiency improves after therapy, including pulmonary vasodilators [27, 61] and lung transplantation [49] Interestingly VE/VCO2 slope’s change after treatment does not appear to influence survival [62].
Arterial O2 Desaturation
In the normal human during incremental exercise, arterial O2 saturation remains normal and the A-aDO2 widens due to hyperventilation and a rise in the RER. In PH, arterial O2 desaturation and/or exaggerated widening of the P(A − a)O2 is due both to V/Q mismatching and a diffusion defect induced by a rapid red cell transit time through a poorly compliant and recruitable pulmonary circulation. Prevalence of arterial O2 desaturation with exercise increases with PH severity [28].
Occasionally, a sudden fall in arterial oxygen saturation heralds the opening of a patent foramen ovale and increased right to left shunting due to elevation of right atrial pressure [23].
Exercise arterial O2 desaturation is not generally a feature of ambulatory HFpEF or HFrEF. Recent work suggests severe O2 desaturation is a negative prognosticator for PH [63].
End Tidal PCO2 (PETCO2)
The PETCO2 normally rises at the AT, reflecting increased VCO2 delivered to the pulmonary capillary which is disproportionately “sampled” at lower end-expiratory lung volumes. The negative Pa-ETCO2 gradient is dependent on normal exercise induced pulmonary vascular recruitment and distension.
As with ventilatory efficiency, pulmonary vascular remodeling or dysfunction impairs this response and alveolar dead space fails to fall normally, diluting the end tidal breath with room air [24, 64]. When PETCO2 at AT is <30 mmHg and especially <20 mmHg, in a patient with exertional dyspnea of unknown cause, PH should be considered as likely.
It has been shown that the PETCO2 [28] transition from rest to AT can distinguish between PH and left ventricular dysfunction; PETCO2 tends to decrease in PAH, whereas the PETCO2 tends to increase in LVD [20, 64].
Like ventilatory inefficiency, disease severity and survival are predicted by the pattern of change [22]. Oudiz et al. have shown higher PETCO2 at AT after treating PH after sildenafil [65].
O2 Uptake Efficiency Slope (OUES)
In 1996, Baba et al. proposed a hybrid measurement of oxygen transport and ventilation during exercise as a surrogate for VO2max in the pediatric population in whom the latter was difficult to reliably achieve [66]. The OUES is an objective, reproducible measure of cardiopulmonary reserve that does not require a maximal exercise effort. It integrates cardiovascular, musculoskeletal and respiratory function into a single index that is largely influenced by pulmonary dead space ventilation and exercise-induced lactic acidosis.
The OUES is derived from the relation between oxygen uptake (V.O2 [ml/min]) and minute ventilation (V.E [l/min]) during incremental exercise and is determined by:
-
V.O2 = a log V.E + b, where a = OUES (Fig. 11.2).
Fig. 11.2 O2 uptake efficiency slope, derived from the semi-log plot (panel b) of the rectilinear plot (panel a) of VO2 vs. VE during submaximum exercise [67]
Major factors that influence the OUES are: CO2 output (derived from muscle aerobic metabolism as well as from the pH buffering function of bicarbonate), arterial pCO2 set-point, and VD/VT.
A low OUES predicts poor survival in HF [68] and worse outcome in PH [69]. Ramos et al. performed an ROC curve analysis in PH (area under the curve = 0.688 [0.542–0.833], p < 0.01), indicating a best OUES cutoff for prognostication of 0.56 L/min/log.
Exercise Oscillatory Ventilation (EOV)
Cyclic fluctuations in minute ventilation during exercise, called exercise oscillatory ventilation (EOV), have been observed in 19–51 % of patients with HF [70–75]. Exercise oscillatory ventilation is a noninvasive parameter that is easily measurable (Fig. 11.3) during submaximum exercise.
Exercise oscillatory ventilation defined as ≥3 cyclic fluctuations of minute ventilation (V.E) during exercise with an amplitude >25 % of the mean trough-to-trough V.E during that interval. CL cycle length; Amp amplitude [76]
We recently examined iCPET data for EOV in 56 patients with HFrEF (mean ± SEM age, 59 ± 2 years; left ventricular ejection fraction, 30 ± 1 %) and 19 age-matched control subjects were studied with incremental cardiopulmonary exercise testing. We detected EOV in 45 % of HF (HF + EOV) patients and in none of the control subjects. The HF + EOV group did not differ from the HF patients without EOV (HF − EOV) in age, sex, body mass index, left ventricular ejection fraction, or origin of HF. Univariate predictors of the presence of EOV in HF, among measurements performed during exercise, included higher right atrial pressure and pulmonary capillary wedge pressure and lower cardiac index (CI) but not PACO2 or PAO2. Multivariate logistic regression identified that low exercise CI is the strongest predictor of EOV (odds ratio, 1.39 for each 1.0-L/min/m2 decrement in CI; 95 % confidence interval, 1.14–1.70; P = 0.001). Among HF patients with EOV, exercise CI was inversely related to EOV cycle length (R = −0.71) and amplitude (R = −0.60; both P < 0.001). In 11 HF + EOV subjects treated with 12 weeks of sildenafil, EOV cycle length and amplitude decreased proportionately to increases in CI. We conclude EOV is closely related to reduced CI, elevated filling pressures and impaired RV contractility (Fig. 11.4) during exercise and may be an important surrogate for exercise-induced hemodynamic impairment in HF patients.
Correlations between exercise oscillatory ventilation (EOV) parameters and cardiac performance; EOV amplitude is inversely related to cumulative cardiac index during exercise (Σcardiac index; a) and right ventricular ejection fraction (RVEF; c). In addition, EOV cycle length is inversely related to cumulative cardiac index during exercise (b) and RVEF (d)
Exercise oscillatory ventilation has emerged as a potent independent risk factor for adverse prognosis in HF [70, 72, 77]. To our knowledge this has not yet been determined for PAH and PH Groups 3–5.
Noninvasive CPET Diagnostic Algorithms for PH
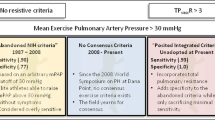
When used together, patterns of CPET variable changes may increase sensitivity and specificity of exercise testing for the diagnosis of PH [78–81]. Our laboratory validated a classic noninvasive CPET diagnostic algorithm for PH in a population of unexplained dyspnea with direct central hemodynamic measurements [26]. We evaluated 130 consecutive, clinically indicated iCPET’s whose phenotyping (see below) was performed to determine if PH were present at maximum exercise and limited exercise tolerance (pulmonary vascular limit (PVL) defined as a PVRmax >120 dyn s cm−5 and a maximum systemic oxygen delivery (DO2max) <80 % of predicted, in the absence of limiting abnormal pulmonary mechanics or poor effort). We evaluated the accuracy of a published diagnostic algorithm [78] (Fig. 11.5) and sequentially altered branch-point threshold values to maximize accuracy in diagnosing PVL. We based threshold values used at each branch point on the 95 % confidence intervals for healthy individuals during exercise [78]. Thus, for the diagnosis of PVL, branch-point values were adjusted in the following order: % predicted VO2max, anaerobic threshold as % predicted VO2max, breathing reserve maximum, and VE/VCO2 and anaerobic threshold.
Figure 11.6 shows the changing sensitivity, specificity, and accuracy for PVL when a representative branch point (VE/VCO2 at anaerobic threshold) was altered systematically. If consecutive branch-point values resulted in identical accuracy, we chose the median value.
In an identical fashion, we determined the utility of isolated peak exercise measurements of VD/V ̇T and PA-aO2 for PVL. We used upper limit of normal values for peak exercise VD/VT and PA-aO2 of 0.28 and 35 mmHg, respectively [78].
The sensitivity of the isolated peak exercise VD/VT for PVL was 20 %, with specificity of 85 % and accuracy of 56 %. Similarly, the isolated peak exercise PA-aO2 had sensitivity for PVL of 24 %, specificity of 92 %, and accuracy of 60 %.
The noninvasive algorithm’s sensitivity for PVL was 79 %, specificity was 75 %, and accuracy was 76 % (n = 93). Systematic alteration of branch-point values improved the algorithm’s specificity and accuracy to 88 % and 85 %, respectively. The greatest improvement in sensitivity for detecting pulmonary vascular limit resulted from a decrease in the threshold value for VE/VCO2 at anaerobic threshold; we applied a stepwise linear regression model to this branch point. When PaCO2 and VD/VT at anaerobic threshold were denoted as independent variables, the model assigned equal weight to both (standard coefficients = 0.59 and 0.57, respectively, p < 0.0001).
A recent study by [20] confirms the utility of a niCPEt algorithm for early detection of pulmonary vascular disease in an at risk population. The authors further suggest that one can distinguish right from left sided disease by the addition of PETCO2 changes from rest to AT.
A suggested niCPET for the diagnosis of PH is suggested (Fig. 11.7).
In summary, niCPET is a useful diagnostic modality that can suggest early or mild PH in at-risk patients or those with unexplained exertional intolerance. Confirmation of PH is almost always necessary through right heart catheterization. The remainder of this chapter focuses on combining CPET with RHC hemodynamic measurements.
Invasive CPET
Measurement of central hemodynamics during exercise has been performed for many years [82–84], but only more recently combined with CPET [85]. In our hands, an iCPET refers to niCPET with the addition of pulmonary and radial artery catheters for pressure measurements and blood sampling.
Methods
A detailed description of methods utilized in the BWH Advanced Cardiopulmonary Exercise Testing Facility has recently been published [86].
iCPET (Fig. 11.8) is best performed using a cycle ergometer to minimize upper body motion and a continuous ramp protocol to ensure a linear increment in work rate and resulting VO2. Upright positioning most closely mimics normal physical activity but either upright or supine exercise can be utilized to derive Ppa–flow relationships [87]. Radial arterial line placement allows precise systemic blood pressure measurement, as well as serial arterial blood gases, to assess important indicators of pulmonary vascular function, including dead space volume/tidal volume, alveolar–arterial gradient and direct Fick cardiac outputs when coupled with assessment of oxygen uptake and mixed venous saturation.
We use an ultrasound-guided internal jugular approach to PAC placement so cycling exercise is unimpeded. The optimal zero reference point for central pressures (approximating the right atrium) has recently been reviewed for supine RHC [88]. It has been suggested that in the upright position mid right atrial ZRP is well approximated by the fourth intercostal space at the junction with the sternum and is used by our laboratory. Pulmonary capillary wedge pressure (PCWP) should be verified based on characteristic waveforms, systemic oxygen saturation, and/or appearance on fluoroscopy. The critical extravascular closure pressure imposed by the lung parenchyma that contains the pulmonary vasculature is typically below that of the PCWP during exercise [89], and therefore PCWP can be used as the downstream pressure in order to determine transpulmonary pressure gradients (TPG = mPAP-PCWP) and pulmonary vascular resistance (PVR = TPG/CO). Care should be taken to maintain consistent upright posture relative to the leveled transducers throughout exercise. Serial measurements of mPAP, PCWP, and CO should be performed at regular intervals (i.e., every minute) during incremental exercise to characterize pressure–flow relationships.
Pleural pressure swings and their influence on pulmonary artery input and outflow pressures and beat-to-beat stroke volume deserve special discussion. For instance, the exaggerated end expiratory pressures seen in the obese patient and in COPD do likely contribute dynamically increased right heart afterload by compression of alveolar vessels, which may in turn contribute to the patient’s exertional intolerance. If, however, one assumes iCPET’s clinical role is in the detection of early pulmonary vasculopathy or HFpEF, one might wish to eliminate the confounding effects of respiratory pressure swings. The classic approach to the problem was to ignore it and take a mean PAP or PCWP through the respiratory cycle. In the 1980s, end-expiratory measures came into vogue, largely in the mechanically ventilated patient, when it was assumed zero airway flow at end expiration would result in the least contamination of PAC derived pressures and this has recently been recommended for supine, resting RHC [90] and utilized during exercise [91, 92].
When measuring hemodynamics during exercise in COPD, subtracting esophageal pressure (Pes), in order to acquire the true intra‐cavitary and thereby deriving actual transmural pressure which is critical in the detection of pulmonary vascular disease, is preferable [93]. The usefulness of the RAP waveform to estimate the pressure surrounding the heart was shown by Tyberg et al. [94]. This method assumes that pressure in the very compliant right atrium is predominantly dependent on pressure surrounding the heart (pericardial pressure, or in our case ITP), rather than by right atrial volume. We showed that this method was useful during exercise in COPD‐patients, as long as the lowest point of the RAP during expiration was used. This is explained by the fact that during the right atrial contraction dissociation between RAP and ITP is created. Therefore, only the pressure of an empty and relaxing right atrium is useful to estimate ITP. We found a small bias with mPAPtm and PCWPtm when RAPnadir was used to correct expiratory mPAP and PCWP, with a very reasonable 95 % CI. This method may not be useful in patients with more pronounced right heart failure, as this causes RAP to rise, even during relaxation.
We have recently examined the worst case scenario: moderate to severe COPD referred for evaluation of suspected PH with exercise [95]. Central hemodynamics were measured simultaneously with esophageal pressure during exercise in 30 COPD patients. mPAP and PCWP were assessed in four different manners:
-
1.
At end‐expiration.
-
2.
Averaged over the respiratory cycle.
-
3.
Corrected from the right atrial pressure (RAP) nadir.
-
4.
Corrected from the RAP respiratory swing and compared with the “gold standard” transmural mPAP and PCWP.
An example of a severe COPD patient’s PAP’s during exercise with and without correction for ITP is shown in Fig. 11.9. Maximum exercise cardiac output was 10.9 ± 3.8 L/min. The large swings in Peso were transduced into all central pressure; on average responsible for a difference between inspiratory values and expiratory values of about 20 mmHg. The expiratory Peso at maximal exercise ranged from +3 to + 25 mmHg. The mPAP/Q slope decreased from 6.4 ± 3.7–4.4 ± 3.2 mmHg/L (p < 0.001) after correction for ITP. Seven patients had a mPAP/Q slope >3 mmHg before correction which decreased to <3 mmHg after correction for the ITP. Twenty‐two patients had a PCWP recording. Nineteen patients of the 22 had a PCWP >20 mmHg with exercise without correction for ITP. Seven patients a had PCPWtm > 20; in three of them PCPWtm was between 20 and 25 mmHg.
Simultaneous measurement of RAP and esophageal pressure (Peso) at maximal exercise in the same patient as shown in Fig. 11.1. RAPnadir is the lowest point in RAP during expiration, which represents RAP during relaxation. Note that RAP falls towards Peso during relaxation. RAPswing was determined as the difference between inspiratory RAP and expiratory RAP [95]
“Gold standard” mPAPtm and PCWPtm at maximum exercise were 47 ± 15 and 17 ± 8 mmHg respectively (Fig. 11.10). The average mPAP values at maximal exercise of the four methods were; mPAPend‐exp: 59 ± 14, mPAPaveraged: 50 ± 14, mPAPrap‐nadir: 44 ± 15, and mPAPrap_swing: 38 ± 15 mmHg. The average PCWP values at maximum exercise of the four methods were; PCWPend‐exp: 27 ± 9, PCWPaveraged: 20 ± 8, PCWPrap‐nadir: 15 ± 7, and PCWPswing: 11 ± 8 mmHg.
Example of pulmonary artery pressure before (PAP) and after (PAPtm) continuous correction for esophageal pressure (Peso) at maximal exercise in a patient with severe COPD (FEV1: 30 % of predicted) [95]
Bland‐Altman analyses showed the best agreement of mPAP (Fig. 11.11) averaged over the respiratory cycle (bias: 2.5 mmHg, limits‐of‐agreement (−6.0 to 11.8) and when corrected with the nadir of RAP (bias: −3.6 mmHg, limits: −11.2 to 3.9). Measuring mPAP at end‐expiration (bias: 10.3 mmHg, limits: 0.5–20.3) and mPAP corrected with the RAP‐swing (bias: −9.3 mmHg, limits: −19.8 to 2.1) resulted in lower levels of agreement (Fig. 11.12). Bland‐Altman plots of the four methods of PCWP measurements during exercise were similar and are shown in Fig. 11.13; both are summarized in Table 11.2.
Average pressure flow relations before and after correction for esophageal pressure. mPAP mean pulmonary artery pressure, mPAPtm transmural mPAP (calculated as mPAP‐Peso), PCWP pulmonary capillary wedge pressure, PCWPtm transmural PCWP (calculated as PCWP‐Peso). **p < 0.01, ***p > 0.001 [95]
Bland‐Altman analyses of the difference between pulmonary artery pressure (mPAP) and transmural mean pulmonary artery pressure (mPAPtm) plotted vs. the mPAPtm. (a) mPAP measured at end expiration, (b) mPAP averaged over the respiratory cycle (c) mPAP corrected with the lowest point of RAP during expiration (RAP‐nadir) and (d) mPAP corrected with the swing in RAP (RAP‐swing). Dotted lines represent the 95 % coincidence intervals [95]
Bland‐Altman analyses of the difference between pulmonary capillary wedge pressure (PCWP) and transmural pulmonary capillary wedge pressure (PCWPtm) plotted vs. the PCWPtm. (a) PCWP measured at end expiration, (b) PCWP averaged over the respiratory cycle (c) PCWP corrected with the lowest point of RAP during expiration (RAP‐nadir) and (d) PCWP corrected with the swing in RAP (RAP‐swing). Dotted lines represent the 95 % coincidence intervals [95]
Our findings support the use of mPAP and PCWP averaged over 2–3 respiratory cycles in order to acquire more accurate assessment of the transmural values of mPAP and PCWP during exercise in COPD‐patients. The patients in the present study showed a wide range of expiratory Peso at exercise, reaching to as high as 25 mmHg, which is consistent with previous studies on pulmonary mechanics. In these studies, as well as the present study, the positive excursion of Peso during expiration is at least as large as the negative excursion during inspiration. It is therefore not surprising that mPAP averaged over the respiratory cycle is a more realistic measure of intravascular pressure. Albeit more accurate than mPAPend‐exp, mPAPaveraged was still a slight overestimation, which can be explained by the increased expiratory time.
Lastly, we showed that the swings in mPAP, PCWP and RAP were similar (r 2 = 0.82, slope: 0.95 ± 0.1) (Fig. 11.14). This has several convenient implications. The consequence of an identical effect of ITP swing on mPAP and PCWP is that the difference between the two, the transpulmonary pressure gradient is unaffected by the swing in ITP. This only holds when both the mPAP and PCWP being recorded at the same time point in the respiratory cycle. So, although individually, mPAP and PCWP are overestimations of intravascular pressure, the mPAPend‐expand PCWPend‐exp combined lead to the correct transpulmonary pressure gradient or PVR (transpulmonary gradient/CO). It underscores the importance of PVR as part of the suggested definition of exercise induced pulmonary arterial hypertension [7], as it prevents patients being diagnosed simply because of an increased ITP.
Illustrates the relation between mPAPswing and PWCPswing. The swing in mPAP and PCWP did not differ (mean difference 0.9 mmHg, p = 0.35). There was a strict relation between RAPswing and PCWPswing (r 2 = 0.9, p < 0.001) with a slope 1.02 and no significant difference between RAPswing and PCWPswing (mean difference 0.7 mmHg, p = 0.28) [95]
The similar effect of ITP swings in RAP and PCWP also has a potential implication in evaluating exercise hemodynamics. The increase in PCWP calculated as a ratio to the increase in RAP (∆PCWP/∆RAP), as previously suggested [25, 96], is unaffected by ITP swings. This ratio might therefore be of potential help in the difficult situation of a high PCWP with exercise in the presence of ITP‐ swings. This would be especially helpful in diagnosing exercise‐induced HFpEF [97].
We conclude central hemodynamics measured at end‐expiration leads to an overestimation of intravascular pressures in exercising COPD‐patients. More reliable data are generated by averaging pressures over the respiratory cycle or using the RAP waveform to correct for intrathoracic pressure. Assessment of the pulmonary gradient is unaffected by respiratory swings. The patients in the study of Boerrigter et al. had at least moderate airflow limitation, likely a worst‐case scenario for the influence of ITP on central pressure measurements. We can only speculated to what extent our findings can be extrapolated to patients with less severe airflow limitation such as PH. Pulmonary vascular pressure therefore should be averaged over 2–3 respiratory cycles not only in COPD [7, 8, 28] but also healthy subjects [98, 99]. Whether an averaged mPAP is a more accurate estimate of the intravascular pressure at maximal exercise in PH without parenchymal lung disease remains unknown and depends on the amplitude and the length of the inspiratory and expiratory excursions in ITP.
We have recently adopted a slow-breathing maneuver to avoid respirophasic change in pulmonary vascular pressures. Fig. 11.15 shows respirophasic change of PAP during moderate exercise; at the arrow, the patient is asked to “relax and miss a breath or two”. Over 90 % of our patients coached in this manner, with a brief practice while at rest on cycle ergometer, can successfully perform the maneuver. The same maneuver results in a stable PCWP measurement (Fig. 11.16).
iCPET Variables
In a manner similar to niCPET, certain variables (Table 11.3) obtained by niCPET plus radial or arterial catheter pressure and blood gas measurements help confirm the presence of PH and differentiate PH with a TPG vs Group 2 without (pulmonary arterial vs. venous hypertension).
Cardiac Output (Qt)
The Fick Principle and conservation of mass dictate that in the steady-state, VO2 = Qt × (CaO2 − CvO2) where Qt = cardiac output and (CaO2 − CvO2) is the difference in O2 content (ml/L) between arterial and mixed venous blood. Thus during iCPET continuous breath-by breath measurement of VO2 and simultaneous blood gas sampling from the distal PA port and radial artery catheter every minute allow the calculation of a Direct Fick cardiac output. Dividing predicted absolute VO2max (ml/min) for a given patient by an expected peak (Ca − vO2(ml/L)) = [Hb] × 10 yields an estimated Qtmax predicted.
Cardiac output generally limits VO2max in healthy adults. Maximal cardiac output, which facilitates transport of oxygen from the alveolus to skeletal muscle, determines the maximal oxygen uptake and aerobic capacity to a large degree. Maintenance of CaO2 and depression of CvO2 during exercise are also circulatory functions, requiring exquisite matching of blood flow to ventilation and tissue metabolism, respectively. Cardiac output normally increases by approximately 5 mL/min for every 1 mL/min increase in VO2 [100]. This slope is not altered by training, but maximum cardiac output improves with conditioning to four to five times resting values (up to levels of approximately 25 L/min in a young healthy individual). Maximum cardiac outputs above 40 L/min have been reported in elite athletes, and elite athletes may exhaust their breathing reserve before attaining maximal cardiac output [101].
Stroke volume (SV) increases in a hyperbolic fashion vs. VO2, and maximum values can be augmented by up to 50 % with training [100, 102, 103]. The rise in SV during exercise is mediated in part by increased contractility, reflected by a 0.10 increase in left ventricular ejection fraction (LVEF) from rest to peak exercise [104]. Left ventricular end-diastolic volume (LVEDV) also increases by 20–40 %, augmenting SV by the Frank-Starling mechanism [105]. LV filling is enhanced during exercise by capacitance venoconstriction, greater negative intrathoracic pressures, and the pumping action of exercising limbs [106]. In a heart with normal lusitropic properties, LV end-diastolic pressure increases to approximately 20 mmHg at maximum exercise [87]. In PH, variable contributions of increased right heart afterload and decreased contractility blunt Qtmax and, in turn, VO2max [7].
Pulmonary Artery Pressure
Pulmonary arterial pressure responses to exercise were first characterized over 60 years ago [82]. Pulmonary hypertension was previously defined in United States and European guidelines as a mean PAP (mPAP) >25 mmHg at rest or >30 mmHg during exercise [107, 108]. In 2008, the Working Group on Diagnosis and Assessment of Pulmonary Arterial Hypertension from the Fourth World Symposium on PH (Dana Point, CA) concluded that mPAP >30 mmHg should be abandoned as a diagnostic criteria for PH whose decision has remained controversial [8, 9, 109, 110]. This decision was based on the age-dependent nature of exercise mPAP and limited data on normal subjects derived from heterogeneous levels, types, and postures during exercise testing [111]. The key paper was a meta-analysis of 47 studies describing 72 populations of healthy volunteers who underwent RHC with invasive measurement of mPAP at rest and during exercise [112]. Data were stratified by gender, age, type of exercise (i.e., cycle ergometry, treadmill exercise), body position (upright vs supine), and exercise levels (slight, submaximal, and maximal). For all subjects at maximal exercise, the ULN was 37 (supine) and 35 mmHg (upright). However, during supine exercise Ppa was significantly higher in subjects aged >50 years (29.4 + 8.4 mmHg) compared to those aged 30–50 years (20.0 + 4.7 mmHg) and 30 years (18.2 + 5.1 mmHg). The upper limit of normal for mPAP in subjects aged <50 years was 29.0 mmHg vs. 46.2 mmHg in subjects aged >50 years. Of note this analysis included TM exercise which is associated with mPAP 8–13 % higher than cycle ergometry and did not report how respiratory pressure swings were controlled for. Moreover, the PCWP and upper limit of PVR were not analyzed.
Pulmonary Vascular Resistance
In the normal human increases in cardiac output exceed the increase in TPG and PVR falls. The PVR fall during exercise is a consequence of both passive distention of a compliant circulation and active vasodilation mediated in part by NO [113]. Pulmonary capillary wedge pressure increases about 1.4 mmHg for every 1.0 mmHg increase in right atrial pressure, suggesting interdependence of right and left ventricular filling [7, 96].
The upper limit for PVRmax in healthy humans remains poorly defined. Reeves et al. [87] calculated that in young, healthy subjects, the upper limit of a normal PVRmax is 56 dyn s cm−5 (O.7 Wood units). Granath et al. [98] studied 27 healthy, older men (aged 71 + 6 years) and found an upper 95 % confidence interval for PVRmax of 120 dyn s cm−5 (1.5 Wood units). Kovacs et al. recently described the changes in PVR in healthy individuals primarily during supine exercise. The data were stratified by sex, age, type of exercise (i.e., cycle ergometry and treadmill exercise), body position (upright vs. supine), and exercise level (slight, submaximum and maximum). The authors concluded that a decline in PVR is seen during the exercise response in healthy normal subjects. A limitation of the study was the paucity of individuals aged >50 years; subjects aged 51–69 years were limited to only 13 and 4 patients in supine and upright positions, respectively. Of these, PVR was available for only 8 (47 %) subjects. Kovacs focused on changes of PVR from rest to exercise, but did not emphasize absolute exercise values. Of note for those subjects ages 51–70 who performed two levels of (supine) exercise, mPAPex was 28.0 ± 7.6 mmHg and PVRex 57 + 27 dyn s cm−5. If one calculates an ULN for both mPAPex is 43.4 mmHg but PVRex is only 111 dyn s cm−5. The latter is in accord with the ULN for PVRmax described by Granath et al. [98]. We suggest a dual definition of exercise PH include both an ULN of mPAPmax and an ULN for PVRmax. Until further studies are done in the aged population, 120 dyn s cm−5 represents a reasonable ULN for PVRmax.
Pressure–Flow Relationships
It has recently been suggested that patterns of change of mPAP vs. cardiac output (ΔmPAP/ΔQt) during exercise may identify a pulmonary vasculopathy without maximally stressing the patient. Reeves et al. [87] performed exercise measurements in 63 healthy young adults at rest and at least two levels of exercise and determined average ΔmPAP/ΔQt <1 mmHg/min/L. Kovacs et al. {Kovacs, 2012 #1942} reported a normal ΔmPAP/ΔQt <1.06 mmHg/min/L. Our 16 normals showed a ΔPpa/ΔQt of 1.4 [7]. ΔmPAP/ΔQt increases as a function of age with an ULN of about 3.0 [9].
A steep ΔmPAP/ΔQt relation is seen in Groups 1 and 2 PH. Fig. 11.17 shows ΔmPAP/ΔQt in scleroderma, PAH compared to the normal.
It can be concluded that the compliant pulmonary vasculature can accommodate large increases in blood flow during exercise with a proportionate modest increment in mPAP and a fall in PVR. When assessing mPAP, it is critical to account for Qt augmentation; therefore, determination of ΔmPAP/ΔQt or PVR is preferable to mPAP alone.
iCPET Diagnostic Algorithms
Once a central cardiac limit is established based on a low VO2max, early AT, and a depressed Qtmax, left heart disease can be differentiated from the right using PAC-derived hemodynamics. This allows a direct Fick cardiac output (VO2 = Qt × (CaO2 − CvO2)) and one can determine whether VO2max is decreased because of a blunted peak cardiac output (a true cardiac limit) or failure to systemically extract O2 (e.g., a Mt myopathy). iCPET can be used as an initial test where PH is strongly suspected, when resting RHC numbers are borderline or when the noninvasive test is either suggestive of PH or unrevealing in a symptomatic patient. It is useful to differentiate a pulmonary mechanical from a pulmonary vascular limit in a patient with suspected Group 3 PH [64].
Patients with exercise-induced PAH, which is discussed further below, have normal cardiopulmonary hemodynamics at rest, but on iCPET demonstrate increased mean pulmonary artery pressure >30 mmHg and pulmonary vascular resistance >80–120 dyn s cm5 [7, 96, 98]. In patients with normal biventricular function, an increased mean PCWP >20 mmHg [96] at peak exercise in the absence of elevations to pulmonary vascular resistance suggests exercise-induced HFpEF. Exertional intolerance may be associated with preload-dependent limitations to stroke volume and cardiac output [114]. In this patient population, failure to augment right atrial pressure on exercise is observed despite abnormally decreased cardiac output. Finally, impaired systemic O2 extraction (Ca-vO2 < [Hb]) indicates left to right shunting or a Mt myopathy [115].
An iCPET diagnostic algorithm is suggested Fig. 11.18. Using this approach we recently reviewed the iCPET diagnoses made at one institution over a 1-year period (Fig. 11.19).
Exercise Induced Pulmonary Arterial Hypertension (eiPAH)
Our group has studied a subset of patients with unexplained exertional intolerance, and depressed VO2max whose sole explanation is an abnormal rise in mPAP and blunted fall of PVR during incremental exercise. An example is shown in Fig. 11.20.
We systematically reviewed results of 406 sequential patients undergoing iCPET to evaluate dyspnea “eiPAH” was defined as resting mPAP <25 mmHg coupled with exercise mPAP >30 mmHg, and PVR >80 dyn s cm−5 and PCWP <20 mmHg [7]. Patients with eiPAH (n = 78) were compared to patients with normal exercise capacity and hemodynamics (n = 16) and patients with resting PAH (mPAP >25 mmHg, PCWP <15 mmHg, n = 15). We found VO2max % predicted was lowest in resting PAH (55.8 ± 20.3 %), intermediate in eiPAH (66.5 ± 16.3 %), and highest in normals (91.7 ± 13.7 %), whereas peak mPAP (48 ± 11 vs. 37 ± 6 vs. 27 + 4 mmHg) and PVR (294 ± 158 vs. 161 ± 60 vs. 62 ± 20 dyn s cm−5, respectively; all P < 0.05) followed an opposite pattern [7].
Within the eiPAH group, mPAP response to exercise followed one of two patterns. eiPAH patients with “takeoff” physiology demonstrate significantly higher VO2max and Qtmax than “plateau” eiPAH (Fig. 11.21). The “takeoff” physiology seen in the exercise induced PAH patients resemble normal/detrained “takeoff” physiology while the “plateau” physiology resembles the physiology seen in those with resting PAH. These data suggest that eiPAH is an intermediate exercise phenotype between normal subjects and those with resting PAH and that abnormal central hemodynamics during exercise substantively contribute to exertional symptoms and impairment.
Subsequent studies have provided further evidence of the functional significance of exercise-induced elevations in PAP in “at-risk populations” for PAH [10, 116–118]. Fowler et al. [10] described 17 subjects eiPAH patients with reduced VO2max (1.2 ± 0.4 vs. 1.7 ± 0.5 L min, P < 0.05), in turn related to decreased peak exercise cardiac output (72 ± 19 % predicted). She and her colleagues also demonstrated elevated ventilatory equivalent for carbon dioxide (41.0 ± 7.3 vs. 31.0 ± 2.9, P < 0.05) and reduced end-tidal carbon dioxide tension (32.6 ± 3.6 vs. 39.4 ± 2.7 mmHg, P < 0.05) at the anaerobic threshold. Kovacs et al. showed that a higher exercise mPAP and PVR in patients with “borderline” resting mPAP was associated with reduced 6-min walk distance and reduced peak workload [117].
Whyte et al. [119], examined the hemodynamic response to exercise in “at risk” patients aged <50 years with normal resting mPAP. They showed that individuals who increased mPAP >30 mmHg (24 out of 38) tended to have a higher resting mPAP and PVR. In particular, 88 % of patients with “borderline” resting mPAP of 21–24 mmHg developed mPAP >30 mmHg on mild-to-moderate exercise tended to have a lower 6-min walk test compared to the remaining 14 patients.
Whether exercise-induced elevations in mPAP and PVR provide a window into the diagnosis of early, potentially more treatable forms of PAH is uncertain [108, 120, 121]. Tolle et al. [7] described five subjects with eiPAH who underwent a repeat clinically indicated iCPET. The time to retest was 29.8 + 10.7 months. Both underlying diagnoses and treatment regimens were heterogeneous. At peak exercise, there was a nonsignificant decrease in VO2max (69.8 + 20.2 to 61.2 + 21.9 % predicted) that was associated with a similar change in Qtmax (86.4 + 25.6 to 80.0 + 23.8 % predicted, p > 0.05 for both), but with no change in central hemodynamics (mPAP: 38.4 + 4.3 to 37.2 + 7.5 mmHg; PVR: 175 + 79 to 131 + 29 dyn s/cm5, p > 0.05 for both). Saggar et al. described 3/11 eiPAH SSc patients developing resting PAH over 24 weeks of open label ambrisentan [122]. Condliffe et al. found that 19 % of patients with scleroderma with eiPAH develop resting pulmonary hypertension after 2.3 years [123]. Long-term follow-up is needed, preferably as part of RCT’s.
We conclude eiPAH is a clinically relevant entity whose abnormal central hemodynamics cause symptoms and substantively impair exercise tolerance. A standardized approach to its diagnosis and definition is needed. Long term prognosis, relationship to resting PH and optimal treatment need to be better defined.
Exercise-Induced HFpEF
niCPET has been used extensively in the diagnosis and management of HFpEF [124, 125] quantifying the exercise impairment and ruling out a pulmonary mechanical limit. Guazzi et al. has also shown that niCPET variables such as peak VO2, VE/VCO2 slope, rest and peak end tidal CO2 (PETCO2) are correlated with diastolic function in HFpEF patients [125]. Although VO2max is an important prognostic factor in HFrEF, this association is not as clearly established for HFpEF patients [125].
iCPET has been used to investigate the central hemodynamics [126] and relative contributions of Qt and systemic O2 extraction in HFpEF [97, 127, 128] iCPET has been suggested as a useful diagnostic modality in the diagnosis of eiHFpEF [129]. Borlaug et al. [97, 130] reported hemodynamic responses to exercise in 55 patients with exertional dyspnea and normal resting hemodynamic measurements. Exercise-induced changes in PCWP and PAP in patients with HFpEF were significantly higher than those in patients with noncardiac dyspnea. Kitzman et al. similarly found that compensated outpatients with HFpEF had normal resting PCWP but marked increases in exercise PCWP, suggesting that HFpEF may initially manifest with only intermittent elevations in cardiac filling pressures [130].
In HFpEF peak oxygen uptake may be additionally affected by impaired systemic O2 extraction [131, 132] as demonstrated by a reduced peak arterial–venous oxygen during iCPET.
Mixed eiPH
A significant percentage of HFpEF patients demonstrate a reactive increase in pulmonary vascular resistance (PVR) which is recognized at resting RHC, which is likely associated with worse outcome [133]. Tailored therapy of exercise-induced mixed PH, phenotyped by iCPET, shows more promise than larger clinical trials of heterogeneous, noninvasively defined HFpEF patients.
iCPET in Established Heart and Lung Disease
Pulmonary Arterial Hypertension
While exercise hemodynamic measurements are not necessary to confirm the diagnosis of established resting PH, they may aid in probing the compensatory capacity of the RV-pulmonary vascular unit. mPAP usually worsens during exercise when compared to rest [134]. With increased temporal resolution (e.g., q 1-min Fick Qt determinations), established PH shows a plateau in mPAP relative VO2 during maximum incremental exercise [7, 135] which may be indicative of dynamic RV dysfunction.
HFrEF
Likewise, iCPET is not necessary for the diagnosis of decompensated HF, but the pulmonary vascular response to exercise yields important mechanistic and prognostic information. For instance, Lam et al. [136] studied 60 consecutive patients with HFrEF (age 60 ± 12 years, left ventricular ejection fraction 0.31 ± 0.07, mean ± SD) and 19 controls with iCPET. During low-level exercise (30 W), LVSD subjects, compared with controls, had greater augmentation in mean PAPs (15 ± 1 vs. 5 ± 1 mmHg), transpulmonary gradients (5 ± 1 vs. 1 ± 1 mmHg), and effective pulmonary artery elastance (0.05 ± 0.02 vs. −0.03 ± 0.01 mmHg/mL, P < 0.0001 for all). A linear increment in PAP relative to work (0.28 ± 0.12 mmHg/W) was observed in 65 % of LVSD patients, which exceeded that observed in controls (0.07 ± 0.02 mmHg/W, P < 0.0001). Exercise capacity and survival was worse in patients with a PAP/W slope above the median than in patients with a lower slope. In the remaining 35 % of LVSD patients, exercise induced a steep initial increment in PAP (0.41 ± 0.16 mmHg/W) followed by a plateau. The plateau pattern, compared with a linear pattern, was associated with reduced VO2max (10.6 ± 2.6 vs. 13.1 ± 4.0 mL/kg/min, P = 0.005), lower right ventricular stroke work index augmentation with exercise (5.7 ± 3.8 vs. 9.7 ± 5.0 g/m2, P = 0.002), and increased mortality (hazard ratio 8.1, 95 % CI 2.7–23.8, P < 0.001).A steep increment in PAP during exercise and failure to augment PAP throughout exercise are associated with decreased exercise capacity and survival in patients with LVSD, and may therefore represent therapeutic targets (Fig. 11.22).
(Left panel) Mean pulmonary arterial pressures (PAP) relative to cardiac outputs during incremental exercise in patients with LVSD. (Right panels) Transpulmonary gradient (TPG) and pulmonary capillary wedge pressure (PCWP) responses to exercise relative to cardiac output augmentation in patients with LVSD. *P < 0.005 for the comparison of pressure changes in patients with LVSD with pressure changes in controls [136]
Chronic Obstructive Pulmonary Disease
As noted above niCPET can differentiate between a pulmonary vascular and mechanical limit to exercise. iCPET can confirm resting or eiPH in chronic obstructive pulmonary disease (COPD). Per the discussion above [95], care must be taken to average input and outflow pressures through several respiratory cycles and to measure mPAP and PCWP for TPG at the same point of the respiratory cycle. Exercise stroke volume appears to be limited by PH in COPD [137] A recent study suggested a high prevalence of eiPH in COPD [92]. We have used iCPET to determine the relative contributions of cardiac output and systemic O2 extraction to the exercise limit in COPD [138, 139].
Conclusions
Cardiopulmonary exercise testing is an important diagnostic tool in the evaluation of the patient with suspected PH. Noninvasive testing is an appropriate screening test for unexplained exertional intolerance or the patient “at risk” for PH. It and can quantify the degree of impairment, and rule out a pulmonary mechanical limit to exercise. Noninvasive parameters, especially ventilatory inefficiency and PETCO2 changes with exercise, especially when used in the context of a niCPET diagnostic algorithm, show reasonable diagnostic accuracy. niCPET can confirm the diagnosis of exercise-induced PH, distinguish between pulmonary arterial and venous hypertension, and rule out confounders such as impaired systemic O2 extraction.
Abbreviations
- 6MWT:
-
6-min walk test
- A-sDO2 :
-
Alveolar–arterial oxygen tension difference
- AT:
-
Anaerobic threshold
- BRI:
-
Breathing reserve index
- CaO2 :
-
Oxygen content of arterial blood
- CO:
-
Cardiac output
- CPET:
-
Cardiopulmonary exercise test
- CvO2 :
-
Oxygen content of venous blood
- DO2 :
-
Oxygen delivery
- DO2max:
-
Maximum systemic oxygen delivery
- eiPAH:
-
Exercise-induced pulmonary hypertension
- EOV:
-
Exercise oscillatory ventilation
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduce ejection fraction
- ITP:
-
Intrathoracic pressure
- IVS:
-
Interventricular septum
- LT:
-
Lactate threshold
- LV:
-
Left ventricle
- LVEF:
-
Left ventricular ejection fraction
- mPAP:
-
Mean pulmonary artery pressure
- MVV:
-
Maximum voluntary ventilation
- OUES:
-
O2 uptake efficiency slope
- PAH:
-
Pulmonary arterial hypertension
- PAP:
-
Pulmonary artery pressure
- PASP:
-
Pulmonary artery systolic pressure
- PCWP:
-
Pulmonary capillary wedge pressure
- PETCO2 :
-
End tidal PCO2
- PFO:
-
Patent foramen ovale
- PH:
-
Pulmonary hypertension
- PVD:
-
Pulmonary vascular disease
- PVL:
-
Pulmonary vascular limit
- PVR:
-
Pulmonary vascular resistance
- RA:
-
Right atrium
- RAP:
-
Right atrial pressure
- RER:
-
Respiratory exchange ratio
- RHC:
-
Right heart catheterization
- ROC:
-
Receiver operating characteristic
- RV:
-
Right ventricle
- RVSP:
-
Right ventricular systolic pressure
- SVR:
-
Systemic vascular resistance
- TPG:
-
Transpulmonary gradient
- ULN:
-
Upper limit of normal
- VAT:
-
Ventilatory anaerobic threshold
- VCO2 :
-
Carbon dioxide production
- VE:
-
Minute ventilation
- VEmax:
-
Minute ventilation at peak exercise
- VO2 :
-
Oxygen uptake
- VO2max:
-
Maximum oxygen uptake
- VT:
-
Tidal volume
- WHO:
-
World Health Organization
References
Thenappan T, et al. A USA-based registry for pulmonary arterial hypertension: 1982–2006. Eur Respir J. 2007;30(6):1103–10.
Whyte K. Towards early detection of pulmonary hypertension: a call to arms. Eur Respir J. 2014;43(1):16–9.
Pullamsetti SS, et al. Novel and emerging therapies for pulmonary hypertension. Am J Respir Crit Care Med. 2014;189(4):394–400.
Norfolk SG, Lederer DJ, Tapson VF. Lung transplantation and atrial septostomy in pulmonary arterial hypertension. Clin Chest Med. 2013;34(4):857–65.
Moser KM, et al. Chronic thromboembolic pulmonary hypertension: clinical picture and surgical treatment. Eur Respir J. 1992;5(3):334–42.
Mohsenifar Z, et al. Lack of sensitivity of measurements of Vd/Vt at rest and during exercise in detection of hemodynamically significant pulmonary vascular abnormalities in collagen vascular disease. Am Rev Respir Dis. 1981;123(5):508–12.
Tolle JJ, et al. Exercise-induced pulmonary arterial hypertension. Circulation. 2008;118(21):2183–9.
Saggar R, et al. Pulmonary vascular responses to exercise: a haemodynamic observation. Eur Respir J. 2012;39(2):231–4.
Naeije R, et al. Exercise-induced pulmonary hypertension: physiological basis and methodological concerns. Am J Respir Crit Care Med. 2013;187(6):576–83.
Fowler RM, et al. Implications of exercise-induced pulmonary arterial hypertension. Med Sci Sports Exerc. 2011;43(6):983–9.
Hansen JE, et al. Reproducibility of cardiopulmonary exercise measurements in patients with pulmonary arterial hypertension. Chest. 2004;126(3):816–24.
Barron A, et al. Test-retest repeatability of cardiopulmonary exercise test variables in patients with cardiac or respiratory disease. Eur J Prev Cardiol. 2014;7:7.
American Thoracic Society. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211–77.
Balady GJ, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191–225.
Grünig E, et al. Non-invasive diagnosis of pulmonary hypertension: ESC/ERS Guidelines with Updated Commentary of the Cologne Consensus Conference 2011. Int J Cardiol. 2011;154 Suppl 1:S3–12.
Committee W, et al. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur Heart J. 2012;33(23):2917–27.
Sun XG, et al. Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation. 2001;104(4):429–35.
Smith G, et al. Safety of maximal cardiopulmonary exercise testing in pediatric patients with pulmonary hypertension. Chest. 2009;135(5):1209–14.
Arena R, et al. Cardiopulmonary exercise testing in the assessment of pulmonary hypertension. Expert Rev Respir Med. 2011;5(2):281–93.
Dumitrescu D, et al. Developing pulmonary vasculopathy in systemic sclerosis, detected with non-invasive cardiopulmonary exercise testing. PLoS One. 2010;5(12):e14293.
Oudiz R, Barst R, Hansen J. Cardiopulmonary exercise testing and six-minute walk correlations in pulmonary arterial hypertension. Am J Cardiol. 2006;97:123–6.
Wensel R, Opitz C, Anker S. Assessment of survival in patients with primary pulmonary hypertension. Importance of cardiopulmonary exercise testing. Circulation. 2002;106:319–24.
Sun X, et al. Gas exchange detection of exercise-induced right-to-left shunt in patients with primary pulmonary hypertension. Circulation. 2002;105:54–60.
Riley M, et al. Gas exchange responses to continuous incremental cycle ergometry exercise in primary pulmonary hypertension in humans. Eur J Appl Physiol. 2000;83:63–70.
Miyamoto S, Nagaya N, Satoh T. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000;161:487–92.
Markowitz DH, Systrom DM. Diagnosis of pulmonary vascular limit to exercise by cardiopulmonary exercise testing. J Heart Lung Transplant. 2004;23(1):88–95.
Nagaya N, Shimizu Y, Satoh T. Oral beraprost sodium improves exercise capacity and ventilatory efficiency in patients with primary or thromboembolic pulmonary hypertension. Heart. 2002;87:340–5.
Yasunobu Y, et al. End-tidal pco2 abnormality and exercise limitation in patients with primary pulmonary hypertension. Chest. 2005;127(5):1637–46.
Hansen JE, Sue DY, Wasserman K. Predicted values for clinical exercise testing. Am Rev Respir Dis. 1984;129(2 Pt 2):S49–55.
D’Alonzo GE, et al. Comparison of progressive exercise performance of normal subjects and patients with primary pulmonary hypertension. Chest. 1987;92(1):57–62.
Gläser S, et al. Impact of pulmonary hypertension on gas exchange and exercise capacity in patients with pulmonary fibrosis. Respir Med. 2009;103(2):317–24.
Wax D, Garofano R, Barst RJ. Effects of long-term infusion of prostacyclin on exercise performance in patients with primary pulmonary hypertension. Chest. 1999;116(4):914–20.
Humbert M, McLaughlin V. Proceedings of the 4th World Symposium on Pulmonary Hypertension. J Am Coll Cardiol. 2009;54:S1–116.
Groepenhoff H, et al. Exercise testing to estimate survival in pulmonary hypertension. Med Sci Sports Exerc. 2008;40(10):1725–32.
Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol. 1986;60(6):2020–7.
Putman CT, et al. Skeletal muscle pyruvate dehydrogenase activity during maximal exercise in humans. Am J Physiol. 1995;269(3 Pt 1):E458–68.
Stainsby WN, et al. Oxidation/reduction state of cytochrome oxidase during repetitive contractions. J Appl Physiol. 1989;67(5):2158–62.
Graham TE, Saltin B. Estimation of the mitochondrial redox state in human skeletal muscle during exercise. J Appl Physiol. 1989;66:561–6.
Poole DC, Gaesser GA. Response of ventilatory and lactate thresholds to continuous and interval training. J Appl Physiol. 1985;58:1115–21.
Gaesser GA, Poole DC. Lactate and ventilatory thresholds: disparity in time course of adaptations to training. J Appl Physiol. 1986;61:99–1004.
Phillips SM, et al. Effects of training duration on substrate turnover and oxidation during exercise. J Appl Physiol. 1996;81(5):2182–91.
Hagberg JM, et al. Exercise and recovery ventilatory and VO2 responses of patients with McArdle’s disease. J Appl Physiol. 1990;68:1393–8.
Sue DY, Hansen JE. Normal values in adults during exercise testing. Clin Chest Med. 1984;5:89–98.
Wasserman K, McIlroy MB. Detecting the threshold of anaerobic metabolism in cardiac patients during exercise. Am J Cardiol. 1964;14:844–52.
Wasserman K, Whipp BJ. Exercise physiology in health and disease. Am Rev Respir Dis. 1975;112:219–49.
Hey EN, et al. Effects of various respiratory stimuli on the depth and frequency of breathing in man. Respir Physiol. 1966;1:193–205.
Medoff BD, et al. Breathing reserve at the lactate threshold to differentiate a pulmonary mechanical from cardiovascular limit to exercise. Chest. 1998;113(4):913–8.
Rochester DF. Tests of respiratory muscle function. Clin Chest Med. 1988;9:249–61.
Theodore J, et al. Augmented ventilatory response to exercise in pulmonary hypertension. Chest. 1986;89(1):39–44.
Jones NL. Normal values for pulmonary gas exchange during exercise. Am Rev Respir Dis. 1984;129(Suppl):S44–6.
Kleber FX, et al. Impairment of ventilatory efficiency in heart failure: prognostic impact. Circulation. 2000;101(24):2803–9.
Habedank D, et al. Ventilatory efficiency and exercise tolerance in 101 healthy volunteers. Eur J Appl Physiol. 1998;77:412–26.
Fukuchi K, Hayashida K, Nakanishi N. Quantitative analysis of lung perfusion in patients with primary pulmonary hypertension. J Nucl Med. 2002;43:757–61.
Reybrouck T, Mertens L, Schulze-Neick I. Ventilatory inefficiency for carbon dioxide during exercise in patients with pulmonary hypertension. Clin Physiol. 2008;28:337–44.
Reindl I, Wernecke K, Opitz C. Impaired ventilatory efficiency in chronic heart failure: possible role of pulmonary vasoconstriction. Am Heart J. 1998;136:778–85.
Lewis GD, et al. Determinants of ventilatory efficiency in heart failure: the role of right ventricular performance and pulmonary vascular tone. Circ Heart Fail. 2008;1(4):227–33.
Raeside DA, et al. Pulmonary artery pressure measurement during exercise testing in patients with suspected pulmonary hypertension. Eur Respir J. 2000;16(2):282–7.
Mitani R, Haraguchi M, Takata S. Excessive ventilatory response during exercise in patients with non-hypoxic pulmonary hypertension. Circ J. 2002;66:453–6.
Yetman AT, et al. Utility of cardiopulmonary stress testing in assessing disease severity in children with pulmonary arterial hypertension. Am J Cardiol. 2005;95(5):697–9.
Schwaiblmair M, et al. Ventilatory efficiency testing as prognostic value in patients with pulmonary hypertension. BMC Pulm Med. 2012;12(1):23.
Wensel R, et al. Effects of iloprost inhalation on exercise capacity and ventilatory efficiency in patients with primary pulmonary hypertension. Circulation. 2000;101(20):2388–92.
Groepenhoff H, et al. Prognostic relevance of changes in exercise test variables in pulmonary arterial hypertension. PLoS One. 2013;8(9):e72013.
Paciocco G, et al. Oxygen desaturation on the six-minute walk test and mortality in untreated primary pulmonary hypertension. Eur Respir J. 2001;17(4):647–52.
Hansen JE, et al. Mixed-expired and end-tidal CO2 distinguish between ventilation and perfusion defects during exercise testing in patients with lung and heart diseases. Chest. 2007;132(3):977–83.
Oudiz RJ, et al. Effect of sildenafil on ventilatory efficiency and exercise tolerance in pulmonary hypertension. Eur J Heart Fail. 2007;9(9):917–21.
Baba R, et al. Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol. 1996;28(6):1567–72.
Hollenberg M, Tager IB. Oxygen uptake efficiency slope: an index of exercise performance and cardiopulmonary reserve requiring only submaximal exercise. J Am Coll Cardiol. 2000;36(1):194–201.
Sun XG, Hansen JE, Stringer WW. Oxygen uptake efficiency plateau best predicts early death in heart failure. Chest. 2012;141(5):1284–94.
Ramos RP, et al. Exercise oxygen uptake efficiency slope independently predicts poor outcome in PAH. Eur Respir J. 2013;5:5.
Corra U, et al. Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence. Circulation. 2006;113(1):44–50.
Kremser CB, O’Toole MF, Leff AR. Oscillatory hyperventilation in severe congestive heart failure secondary to idiopathic dilated cardiomyopathy or to ischemic cardiomyopathy. Am J Cardiol. 1987;59(8):900–5.
Sun XG, et al. Oscillatory breathing and exercise gas exchange abnormalities prognosticate early mortality and morbidity in heart failure. J Am Coll Cardiol. 2010;55(17):1814–23.
Guazzi M, Raimondo R, Vicenzi M. Exercise oscillatory ventilation may predict sudden cardiac death in heart failure patients. J Am Coll Cardiol. 2007;50:299–308.
Guazzi M, et al. Exercise oscillatory breathing in diastolic heart failure: prevalence and prognostic insights. Eur Heart J. 2008;29(22):2751–9.
Arena R, et al. Prognostic value of timing and duration characteristics of exercise oscillatory ventilation in patients with heart failure. J Heart Lung Transplant. 2008;27(3):341–7.
Murphy RM, et al. Exercise oscillatory ventilation in systolic heart failure: an indicator of impaired hemodynamic response to exercise. Circulation. 2011;124(13):1442–51.
Leite JJ, et al. Periodic breathing during incremental exercise predicts mortality in patients with chronic heart failure evaluated for cardiac transplantation. J Am Coll Cardiol. 2003;41(12):2175–81.
Wasserman K, Hansen JE, Sue DY, Casaburi R, Whipp BJ. Principles of exercise testing and interpretation. 3rd ed. Baltimore, MD: Lipincott Williams & Wilkins; 1999. p. 193.
Weisman IM, Zeballos RJ. An integrated approach to the interpretation of cardiopulmonary exercise testing. Clin Chest Med. 1994;15(2):421–45.
Eschenbacher WL, Mannina A. An algorithm for the interpretation of cardiopulmonary exercise tests. Chest. 1990;97(2):263–7.
Ramos RP, et al. Clinical usefulness of response profiles to rapidly incremental cardiopulmonary exercise testing. Pulm Med. 2013;359021(10):12.
Hickam JB, Cargill WH. Effect of exercise on cardiac output and pulmonary arterial pressure in normal persons and in patients with cardiovascular disease and pulmonary emphysema. J Clin Invest. 1948;27(1):10–23.
Slonim NB, et al. The effect of mild exercise in the supine position on the pulmonary arterial pressure of five normal human subjects. J Clin Invest. 1954;33(7):1022–30.
Damato AN, Galante JG, Smith WM. Hemodynamic response to treadmill exercise in normal subjects. J Appl Physiol. 1966;21(3):959–66.
Janicki JS, et al. The pressure-flow response of the pulmonary circulation in patients with heart failure and pulmonary vascular disease. Circulation. 1985;72(6):1270–8.
Maron BA, et al. The Invasive Cardiopulmonary Exercise Test. Circulation. 2013;127(10):1157–64.
Reeves JT, et al. Increased wedge pressure facilitates decreased lung vascular resistance during upright exercise. Chest. 1988;93(Suppl):97S–9.
Kovacs G, et al. Zero reference level for right heart catheterisation. Eur Respir J. 2013;42(6):1586–94.
Fowler NO. The normal pulmonary arterial pressure-flow relationships during exercise. Am J Med. 1969;47(1):1–6.
Champion HC, Michelakis ED, Hassoun PM. Comprehensive invasive and noninvasive approach to the right ventricle-pulmonary circulation unit: state of the art and clinical and research implications. Circulation. 2009;120(11):992–1007.
Blanco I, et al. Hemodynamic and gas exchange effects of sildenafil in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Am J Respir Crit Care Med. 2010;181(3):270–8.
Hilde JM, et al. Haemodynamic responses to exercise in patients with COPD. Eur Respir J. 2013;41(5):1031–41.
Lockhart A, et al. Elevated pulmonary artery wedge pressure at rest and during exercise in chronic bronchitis: fact or fancy. Clin Sci. 1969;37(2):503–17.
Tyberg JV, et al. The relationship between pericardial pressure and right atrial pressure: an intraoperative study. Circulation. 1986;73(3):428–32.
Boerrigter BG, et al. Measuring central pulmonary pressures during exercise in COPD: how to cope with respiratory effects? Eur Respir J. 2013;43(5):1316–25.
Reeves JT, et al. Operation Everest II: cardiac filling pressures during cycle exercise at sea level. Respir Physiol. 1990;80:147–54.
Borlaug BA, et al. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3(5):588–95.
Granath A, Jonsson B, Strandell T. Circulation in healthy old men, studied by right heart catheterization at rest and during exercise in supine and sitting position. Acta Med Scand. 1964;176:425–46.
Groves BM, et al. Operation Everest II: elevated high-altitude pulmonary resistance unresponsive to oxygen. J Appl Physiol. 1987;63(2):521–30.
Weber KT, Janicki JS. Cardiopulmonary exercise testing: physiologic principles and clinical applications. Philadelphia: WB Saunders; 1986.
Dempsey JA. Is the lung built for exercise? Med Sci Sports Exerc. 1986;18:143–55.
Weber KT, Janicki JS. Cardiopulmonary exercise testing for evaluation of chronic cardiac failure. Am J Cardiol. 1985;55:22A–31.
Blomqvist CG, Saltin B. Cardiovascular adaptations to physical training. Annu Rev Physiol. 1983;45:169–89.
Mahler DA, et al. Volumetric responses of right and left ventricles during upright exercise in normal subjects. J Appl Physiol. 1985;58:1818–22.
Manyari DE, Kostuk WJ. Left and right ventricular function at rest and during bicycle exercise in the supine and sitting positions in normal subjects and patients with coronary artery disease: assessment by radionuclide ventriculography. Am J Cardiol. 1983;51:36–42.
Shepherd JT. Circulatory response to exercise in health. Circulation. 1987;76(Suppl V):VI3–10.
Galie N, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J. 2004;25(24):2243–78.
McGoon M, et al. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP Evidence-Based Clinical Practice Guidelines. Chest. 2004;126(1_suppl):14S–34.
Hoeper MM, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25, Suppl):D42–50.
Lewis GD, et al. Pulmonary vascular hemodynamic response to exercise in cardiopulmonary diseases. Circulation. 2013;128(13):1470–9.
Badesch DB, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54(1 Suppl):S55–66.
Kovacs G, et al. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34(4):888–94.
Kane DW, et al. Exercise-induced pulmonary vasoconstriction during combined blockade of nitric oxide synthase and beta adrenergic receptors. J Clin Investig. 1994;93(2):677–83.
Fu Q, et al. Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol. 2010;55(25):2858–68.
Taivassalo T, et al. The spectrum of exercise tolerance in mitochondrial myopathies: a study of 40 patients. Brain. 2003;126(2):413–23.
Fowler RM, Gain KR, Gabbay E. Exercise intolerance in pulmonary arterial hypertension. Pulm Med. 2012;2012:359204.
Kovacs G, et al. Borderline pulmonary arterial pressure is associated with decreased exercise capacity in scleroderma. Am J Respir Crit Care Med. 2009;180(9):881–6.
Steen V, et al. Exercise induced pulmonary arterial hypertension in patients with systemic sclerosis. Chest. 2008;134(1):146–51.
Whyte K, et al. The association between resting and mild-to-moderate exercise pulmonary artery pressure. Eur Respir J. 2012;39(2):313–8.
Proudman SM, et al. Pulmonary arterial hypertension in systemic sclerosis: the need for early detection and treatment. Intern Med J. 2007;37(7):485–94.
Raeside DA, et al. Pulmonary artery pressure variation in patients with connective tissue disease: 24 hour ambulatory pulmonary artery pressure monitoring. Thorax. 1998;53(10):857–62.
Saggar R, et al. Brief report: effect of ambrisentan treatment on exercise-induced pulmonary hypertension in systemic sclerosis: a prospective single-center, open-label pilot study. Arthritis Rheum. 2012;64(12):4072–7.
Condliffe R, et al. Connective tissue disease-associated pulmonary arterial hypertension in the modern treatment era. Am J Respir Crit Care Med. 2009;179(2):151–7.
Guazzi M, Cahalin LP, Arena R. Cardiopulmonary exercise testing as a diagnostic tool for the detection of left-sided pulmonary hypertension in heart failure. J Card Fail. 2013;19(7):461–7.
Guazzi M, Myers J, Arena R. Cardiopulmonary exercise testing in the clinical and prognostic assessment of diastolic heart failure. J Am Coll Cardiol. 2005;46(10):1883–90.
Bhella PS, et al. Abnormal haemodynamic response to exercise in heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13(12):1296–304.
Borlaug BA. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction. Circ J. 2013;78(1):20–32.
Abudiab MM, et al. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail. 2013;15(7):776–85.
van Empel VPM, Kaye DM. Integration of exercise evaluation into the algorithm for evaluation of patients with suspected heart failure with preserved ejection fraction. Int J Cardiol. 2013;168(2):716–22.
Kitzman DW, et al. Exercise intolerance in patients with heart failure and preserved left ventricular systolic function: failure of the Frank-Starling mechanism. J Am Coll Cardiol. 1991;17(5):1065–72.
Tolle J, Waxman A, Systrom D. Impaired systemic oxygen extraction at maximum exercise in pulmonary hypertension. Med Sci Sports Exerc. 2008;40(1):3–8.
Haykowsky MJ, et al. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. J Am Coll Cardiol. 2011;58(3):265–74.
Lam CS, et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53(13):1119–26.
Laskey WK, et al. Pulmonary artery hemodynamics in primary pulmonary hypertension. J Am Coll Cardiol. 1993;21(2):406–12.
Wonisch M, et al. Continuous haemodynamic monitoring during exercise in patients with pulmonary hypertension. Int J Cardiol. 2005;101(3):415–20.
Lewis GD, et al. Pulmonary vascular response patterns during exercise in left ventricular systolic dysfunction predict exercise capacity and outcomes. Circ Heart Fail. 2011;4(3):276–85.
Holverda S, et al. Stroke volume increase to exercise in chronic obstructive pulmonary disease is limited by increased pulmonary artery pressure. Heart. 2009;95(2):137–41.
Oelberg DA, et al. Ventilatory and cardiovascular responses to inspired He-O2 during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158(6):1876–82.
Oelberg DA, et al. Systemic oxygen extraction during incremental exercise in patients with severe chronic obstructive pulmonary disease. Eur J Appl Physiol Occup Physiol. 1998;78(3):201–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Systrom, D.M., Waxman, A.B. (2015). Cardiopulmonary Exercise Testing in Pulmonary Hypertension. In: Klinger, J., Frantz, R. (eds) Diagnosis and Management of Pulmonary Hypertension. Respiratory Medicine, vol 12. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-2636-7_11
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2636-7_11
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-2635-0
Online ISBN: 978-1-4939-2636-7
eBook Packages: MedicineMedicine (R0)