Abstract
Early detection of pulmonary hypertension (PH) is essential to ensure that patients receive timely and appropriate treatment for this progressive disease. Rest and exercise echocardiography has been used to screen patients in an attempt to identify early stage PH. However, current PH guidelines recommend against exercise tests because of the lack of evidence. We reviewed previous studies to discuss the current standpoint concerning rest and exercise echocardiography in PH. Around 20 exercise echocardiography studies were included to assess the cutoff value for exercise-induced pulmonary hypertension (EIPH). Approximately 40 exercise echocardiography studies were also included to evaluate the pulmonary artery pressure-flow relationship as assessed by the slope of the mean pulmonary artery pressure and cardiac output (ΔmPAP/ΔQ). There were several EIPH and ΔmPAP/ΔQ reference values in individuals with pulmonary vascular disease. We believed that assessing the ΔmPAP/ΔQ makes sense from a physiological standpoint, and the clinical value should be confirmed in future studies. Exercise echocardiography is an appealing alternative in PH. Further studies are needed to assess the prognostic value of the pulmonary artery pressure-flow relationship in high-risk subjects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary hypertension (PH) is a crucial hemodynamic state defined by a resting mean pulmonary artery pressure (mPAP) ≥25 mmHg regardless of the etiology. Current guidelines provide a classification system that categorizes PH into five groups with specific pathogeneses and clinical characteristics [1, 2]. Group 1 comprises pulmonary arterial hypertension (PAH) associated with idiopathic disease, connective tissue disease (CTD), congenital heart disease, and genetic disease. Group 2 includes PH caused by left heart failure, such as valvular heart disease or myocardial disease. Group 3 PH is caused by sleep-disordered breathing or lung disease such as chronic obstructive pulmonary disease (COPD). Group 4 includes chronic thromboembolisms (CTEPH), and group 5 indicates PH with unclear multifactorial mechanisms. Whatever the PH etiology, severe PH is a critical hemodynamic state. In PAH patients, severe PH is a leading cause of death, and several new treatments have been developed and provide benefits. In patients with left heart failure, PH is found in 15–60 % and is associated with a higher risk of cardiac events [3].
Poor PH outcomes might be explained not only by the severity of comorbidities but also by the delay in diagnosis. Thus, early detection of PH is essential to ensure that patients receive timely and appropriate treatment for this progressive disease. Current screening recommendations are based on several guidelines by the American College of Cardiology Foundation/American Heart Association (ACC/AHA) and the European Society of Cardiology/European Respiratory Society (ESC/ERS) [1, 2]. In the guidelines, transthoracic echocardiography is used to assess the pulmonary artery pressure (PAP) by Doppler measurements and should always be performed when PH is suspected. In addition, N-terminal pro-brain natriuretic peptide, as a marker of myocardial stress and a disproportionately reduced pulmonary diffusing capacity for carbon monoxide, is widely used. When remarkable findings are detected, right heart catheterization (RHC) is recommended. The diagnosis of PH is confirmed at RHC by an mPAP of ≥25 mmHg. The diagnostic criteria of PAH include a pulmonary capillary wedge pressure ≤15 mmHg and pulmonary vascular resistance >3 Wood units in the absence of other causes of precapillary PH, such as lung diseases or human immunodeficiency infection.
Early detection of PH remains a clinical challenge despite the development of several diagnostic tools. Because elevated PAP during exercise can be a cause of dyspnea and fatigue, exercise-induced pulmonary hypertension (EIPH) has been described as a potential useful indication for the early identification of patients at the risk of developing resting PH [4]. RHC is the gold standard for defining PAP during exercise. However, RHC is an invasive procedure, and we need noninvasive tests to screen for PH in all cohorts. Exercise echocardiography has been used to screen patients in an attempt to identify early stage PH with no remarkable echocardiographic findings at rest [5]. The American Society of Echocardiography (ASE) consensus had recommended that exercise Doppler echocardiography is a safe screening tool for detecting a pulmonary hypertensive response to exercise in high-risk patients [6]. However, the current PH guidelines (ACC/AHA and ESC/ERS) recommend against exercise echocardiography because there are relatively few published data [1, 2]. In addition, even in normal individuals, pulmonary pressure elevations will develop during exercise with increasing cardiac output. Evaluation of PH during exercise in the absence of knowledge of the cardiac output may be problematic. Several investigators showed that the exercise-induced increases in mPAP relative to cardiac output (ΔmPAP/ΔQ) were more likely to be useful for assessing the prognosis of PH [5]. The goal of this review is to clarify the current standpoint and future directions concerning exercise echocardiography for pulmonary hemodynamics in PH.
Echocardiographic assessment of pulmonary hypertension at rest
The guidelines clearly describe echocardiographic assessments of right heart function in PH [7]. The most important measurement of PH assessment is the estimation of the systolic PAP (sPAP). The estimation of sPAP is based on the tricuspid regurgitation pressure gradient (TR-PG) according to the simplified Bernoulli equation, taking into account the estimated right atrial pressure in the absence of right ventricular outflow tract obstruction. The mPAP can be estimated by the following simple formula: mPAP = 0.61 × SPAP + 2 mmHg [7]. Figure 1a shows measurement of the TR-PG. Previous studies have shown modest to good correlations between the estimated PAP and invasively measured pressures. Concerning limitations, sPAP has a wide limit of agreement in Bland-Altman analysis (−19 to 18 mmHg) [8], and there are many formulas for calculating the mPAP. We should use this index to guide clinical decision-making, not to diagnose PH.
Conventional and new echocardiographic parameters for the assessment of PH. a Elevated pulmonary artery pressure by the tricuspid regurgitant pressure gradient (TR-PG). b M-mode recording through the lateral tricuspid valve annulus to measure the tricuspid annular plane systolic excursion (TAPSE). c Two-dimensional image demonstrating dilated right ventricular size caused by elevated pulmonary artery pressure. Right ventricular fractional area change (RVFAC) is measured by the following formula: (RV end diastolic area − RV end systolic area)/RV end diastolic area. d Tissue Doppler image of the lateral tricuspid valve annulus. Peak systolic annular motion velocity of the RV free wall (RVS’) impaired in PH. e Speckle-tracking analysis of a patient with severely reduced myocardial defamation of the right ventricular (RV strain). RA right atrium
There are several parameters of echocardiographic right ventricular (RV) function for assessing the disease state in PH. Patients with PH have gradually reduced exercise capacity related to decreasing RV function. Thus, the progression of PH is determined by the severity of the increase in the resting PAP and RV function. An increased RV afterload may cause RV dysfunction, which leads to advanced RV failure and cardiac death. Although RV dysfunction is closely associated with elevated PAP, RV impairment can be observed in patients with relatively normal PAP because of other underlying factors. Therefore, detection of RV dysfunction in the development of PH might be useful in clinical follow-up.
Assessment of RV morphology is also often challenging, and the assessment of the RV by conventional echocardiography remains difficult because of the complex shape of the chamber. Tricuspid annular plane systolic excursion (TAPSE) has been previously reported to have good predictive value for RV failure, and it is simple and easy to measure (Fig. 1b). RV fractional area change (RVFAC) is also measured by two-dimensional echocardiograms in the RV focused view by the following formula: (RV end diastolic area − RV end systolic area)/RV end diastolic area (Fig. 1c). TAPSE <17 mm or RVFAC <35 % should be considered a marker of RV dysfunction from the reference values according to the guideline [7]. Doppler tissue imaging of the basal tricuspid annular motion has been applied to assess RV function in several cardiac diseases including PH. According to the guideline, the systolic annular motion velocity of the RV free wall (RVS’) <10 cm/s is a reference value (Fig. 1d). The RV strain analysis by two-dimensional speckle-tracking echocardiogram has been proposed to allow the quantification of RV myocardial deformation (Fig. 1e). The speckle-tracking technique is angle independent, which enables an assessment of the RV myocardial strain from a two-dimensional speckle-tracking echocardiogram. Analysis of the RV strain may provide prognostic information and could help in the stratification of patients with PH. Recently, three-dimensional speckle-tracking echocardiography (3D-STE) was developed in the clinical setting. Some investigators suggested that the strain and RV ejection fraction (EF) measured by 3D-STE may help risk stratify patients with PH and guide clinical management [9]. However, the limitations of 3D-STE are the low temporal and spatial resolution and limited acoustic windows. Thus, it has been recommended to combine various RV echocardiographic parameters to assess the RV function in PH.
Exercise-induced pulmonary hypertension (EIPH)
In pulmonary hemodynamics, the large reserve of the pulmonary circulation indicates that PH is usually diagnosed late in its course, with an asymptomatic stage preceding onset. Therefore, patients with early PH may present with almost normal resting PAP, but an abnormal exercise PAP, with an increase in pulmonary blood flow. Several investigators showed abnormal PAP elevation during exercise in patients with high-risk PH, including CTD. This is referred to as EIPH. Previous papers suggested that EIPH is a marker for the risk of developing resting PH [10]. However, there are several exercise protocols and many cutoff values to assess the EIPH. An overview of the studies of exercise echocardiography for detecting EIPH in a high-risk population is presented in Table 1. The PAP cutoff value affects the accuracy of the detection of PH by Doppler echocardiography. Low PAP leads to false-positive results, and high PAP leads to false-negative results. In patients with CTD including mainly systemic sclerosis (SSc), abnormal responses were defined by an sPAP greater than 30–35 mmHg during exercise or a post-exercise increase in sPAP by >20 mmHg. Recent studies generally showed that abnormal responses were defined by an sPAP >50 mmHg during exercise in order to exclude false-positive results in the screening tests [11–22]. In group 2 PH, the PAP cutoff value was variable and depended on the specific diseases [23–30]. The cutoff values should be taken into consideration in each patient. The other specific limitation is that several stress methods are widely used in the clinical setting (Fig. 2). Exercise data during ergometer exercise should not be applied to post-treadmill or other exercises because each protocol is characterized by different loading conditions.
Representative EIPH case
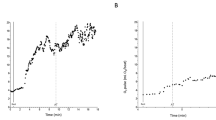
A 50-year-old female was referred to a clinic for SSc 5 years ago (Fig. 3). She was admitted to our hospital to check the PAP with dyspnea. Echocardiography showed a TR-PG of 22 mmHg at rest, indicating normal sPAP, and the 6-min walk distance was 510 m, indicating an almost normal exercise capacity (the 6-min walk test is equivalent to the ergometer test with 90 % workload) [31]. However, the TR-PG just after the 6-min walk test was elevated to 36 mmHg, indicating a poor pulmonary vascular response (Fig. 3a). Oxygen saturation was slightly decreased from 97 to 94 % by exercise. Supine ergometer exercise echocardiography was performed to assess the details of EIPH. TR-PG at baseline was 23 mmHg and increased in severity at 25 and 50 W of exercise (Fig. 3b). During exercise, the peak TR-PG was elevated to 58 mmHg. In our experience, the PAP increase with the 6-min walk test was similar to a 25-W workload with a supine ergometer. We suspected EIPH and transferred this patient to the catheter laboratory. RHC at rest showed an mPAP of 24 mmHg and PCWP of 11 mmHg, which did not meet the criteria of PH with normal left ventricular EF and no coronary artery stenosis. Then, during exercise using a supine ergometer, the mPAP was significantly elevated (25 W: mPAP = 41 mmHg; 50 W: mPAP = 55 mmHg) with remarkable dyspnea (Fig. 3c). PVR was also elevated during exercise (at baseline: PVR = 3.2 Wood units, 25 W: PVR = 4.2 Wood units; 50 W: PVR = 4.7 Wood units). This case clearly showed significant changes in PAP developed even with mild exercise with a spine ergometer.
Invasive and noninvasive parameters of the 6-min walk test and spine ergometer test: a representative case. TR-PG tricuspid regurgitant pressure gradient, BP blood pressure, HR heart rate, Q cardiac output, mPAP mean pulmonary artery pressure, TPG transpulmonary gradient, PVR pulmonary vascular resistance
Pulmonary artery pressure-flow relationship
One concern of previous EIPH criteria is the lack of cardiac output when considering the pulmonary circulation because PAP is a flow-dependent variable. Several investigators have reported the upper limits of sPAP in healthy individuals from exercise echocardiography are 40–45 mmHg. However, the upper limits are 55–60 mmHg with significantly increasing cardiac output in top athletes. In addition, some investigators showed that a PAP increase during exercise might be a marker of a good RV contractile reserve and prognosis in patients with moderate to severe impairment of PH [23]. They stated that a greater increase in pressure allows a higher stroke volume, and the contractile reserve can be defined by the increase in pressure. Therefore, in the evaluation of PH, cardiac output should be given, and the multipoint pressure-flow response of the pulmonary circulation may be a useful method.
Previous studies have described abnormal cardiac output responses for increments of mPAP as having the potential to assess the disease state and functional class in PH. When we gathered a sufficient number of ΔmPAP/ΔQ data, we think it became possible to identify a reference value of this slope in each disease. In any type of PH, specific cutoff values of ΔmPAP/ΔQ can be presented. In normal individuals, invasive and noninvasive studies have clearly showed the slope of the linearized mPAP-Q relationship should not exceed 3 mmHg/l/min. The average of ΔmPAP/ΔQ is 1.2 mmHg/l/min as calculated from 11 previous studies in normal control studies (Fig. 4a).
Pulmonary artery pressure-flow relationships. a On 11 normal studies [27, 35–44]. b On 5 pulmonary arterial hypertension (PAH) studies [45–49]. c On 7 connective tissue disease (CTD) studies [4, 19, 20, 32, 50–52]. d Prediction for development of pulmonary hypertension (PH) in our study [33]. e On 8 left heart failure studies [26, 28, 30, 53–56]. f On 8 chronic obstructive pulmonary disease (COPD) studies [57–62]
PAH is associated with remodeling of the small pulmonary arteries and leads to an increase in pulmonary vascular resistance with right heart failure. The pulmonary vascular bed is severely damaged, and ΔmPAP/ΔQ is significantly increased. According to five previous studies, the average ΔmPAP/ΔQ is 8.6 mmHg/l/min in PAH patients (Fig. 4b). Patients with CTD are also considered a high-risk group for developing PH, and SSc is the highest risk group within CTD. Estimation of the lifetime risk of developing PAH is 10–15 %. PAH is associated with 30 % of all deaths in SSc [32]. In this type of disease, the pulmonary circulation depends mainly on the inability of the pulmonary vascular bed to dilate under stress and consequently reflects the abnormally stiff vascular system characteristics. In seven previous studies with subjects without PH at rest, the average ΔmPAP/ΔQ was 4.5 mmHg/l/min in CTD (Fig. 4c). This cutoff value is significantly higher than the upper limit of the reference value. Recently, our institute developed 6-min walk stress echocardiography to detect the early stage of PH in CTD [33]. We demonstrated that ΔmPAP/ΔQ obtained by 6-min walk stress echocardiography was a predictor of the future development of PH in patients with CTD and was independent of the 6-min walk distance. In the Fig. 4d, the ΔmPAP/ΔQ in patients with events (development of overt PH) was significantly higher than in patients without events (6.1 vs. 2.6 mmHg/l/min; p < 0.001). Using a receiver-operating characteristic curve, the best cutoff value of ΔmPAP/ΔQ for predicting the development of PH was >3.3 mmHg/l/min. CTD patients with greater increases in PAP relative to cardiac output are at increased risk of developing PH during long-term follow-up. Figure 5 shows the case of one representative patient with CTD who underwent 6-min walk stress echocardiography. TR-PG by echocardiography and cardiac output by electric cardiometry were increased post 6-min walk test. We can calculate the pulmonary artery pressure-cardiac output relationships as ΔmPAP divided by ΔQ (ΔmPAP/ΔQ). To our knowledge, this is the first report to combine measures of the change in the pressure-flow relationship and long-term outcomes for the development of PH in CTD. Exercise echocardiography has been described as a safe and valuable screening tool for detecting an abnormal response of pulmonary artery pressure in high-risk patients such as those with CTD, but it remains technically difficult and requires experience.
PH at rest or during exercise is associated with an adverse outcome in patients with left heart failure (group 2 PH). The presence of PH at rest or during exercise has also been included in the risk assessment of valve surgery. Patients with normal or mildly elevated PAP at rest may develop severe PH during exercise in the left heart failure group. In eight previous studies with left heart failure, the average ΔmPAP/ΔQ was 6.1 mmHg/l/min (Fig. 4e). In COPD patients (group 3 PH), the prevalence of PH was from 30 to 70 %, and PH was significantly correlated with a decrease in the exercise capacity and mortality. A relationship between the pulmonary circulation and severity of hypoxemia suggested that hypoxia causes pulmonary vascular remodeling in COPD. In eight previous studies with COPD, the average ΔmPAP/ΔQ was 5.2 mmHg/l/min (Fig. 4f). Therefore, there were several reference values of EIPH and ΔmPAP/ΔQ in individuals with pulmonary vascular disease.
Future directions
In high-risk patients (e.g., those with SSc, left heart failure with valve disease, COPD, and CTEPH), the ΔmPAP/ΔQ according to exercise echocardiography as a marker of pulmonary circulation can be a useful measurement of the disease state of PH. However, the clinical utility of ΔmPAP/ΔQ has only been supported by small and cross-sectional studies. The clinical implication was also limited because of the absence of longitudinal data with medical treatment. Well-controlled multicenter studies in large cohorts of high-risk patients are needed to validate exercise echocardiographic data including ΔmPAP/ΔQ. Therapeutic strategies for EIPH have not been described in the recent guidelines. Patients with EIPH according to echocardiography need to have the actual pressure confirmed by RHC individually. In addition, a small study reported that endothelin receptor antagonists have been used for early stage PH [34].
Conclusions
From our comprehensive review, we suggest that multipoint assessment of mPAP relative to Q during exercise should be taken into consideration for the assessment of the pulmonary circulation. ΔmPAP/ΔQ >3 mmHg/l/min represents an abnormal pulmonary vascular response to exercise. We believe that this index makes sense from a physiological standpoint, and the clinical worth should be confirmed in the future studies. Exercise echocardiography is an appealing alternative in PH. Further studies are needed to assess the prognostic value of the pulmonary artery pressure-flow relationship in high-risk subjects.
References
Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62:D42–50.
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2015; ehv317.
Magne J, Pibarot P, Sengupta PP, et al. Pulmonary hypertension in valvular disease. JACC Cardiovasc Imaging. 2015;8:83–99.
Codullo V, Caporali R, Cuomo G, et al. Stress Doppler echocardiography in systemic sclerosis: evidence for a role in the prediction of pulmonary hypertension. Arthritis Rheum. 2013;65:2403–11.
Lewis GD, Bossone E, Naeije R, et al. Pulmonary vascular hemodynamic response to exercise in cardiopulmonary diseases. Circulation. 2013;128:1470–9.
Bossone E, D’Andrea A, D’Alto M, et al. Echocardiography in pulmonary arterial hypertension: from diagnosis to prognosis. J Am Soc Echocardiogr. 2013;26:1–14.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1–39):e14.
D'Alto M, Romeo E, Argiento P et al. Accuracy and precision of echocardiography versus right heart catheterization for the assessment of pulmonary hypertension. Int J Cardiol 2013;168:4058–62.
Smith BC, Dobson G, Dawson D, et al. Three-dimensional speckle tracking of the right ventricle: toward optimal quantification of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol. 2014;64:41–51.
Coghlan JG, Denton CP, Grunig E et al. Evidence-based detection of pulmonary arterial hypertension in systemic sclerosis: the DETECT study. Ann Rheum Dis 2014;73:1340–9.
Alkotob ML. Reduced exercise capacity and stress-induced pulmonary hypertension in patients with scleroderma. Chest. 2006;130:176–81.
Collins N, Bastian B, Quiqueree L, et al. Abnormal pulmonary vascular responses in patients registered with a systemic autoimmunity database: pulmonary hypertension assessment and screening evaluation using stress echocardiography (PHASE-I). Eur J Echocardiogr. 2006;7:439–46.
Huez S, Roufosse F, Vachiery JL, et al. Isolated right ventricular dysfunction in systemic sclerosis: latent pulmonary hypertension? Eur Respir J. 2007;30:928–36.
Steen V. Exercise-induced pulmonary arterial hypertension in patients with systemic sclerosis. Chest. 2008;134:146.
Kovacs G, Maier R, Aberer E, et al. Borderline pulmonary arterial pressure is associated with decreased exercise capacity in scleroderma. Am J Respir Crit Care Med. 2009;180:881–6.
Kovacs G. Assessment of pulmonary arterial pressure during exercise in collagen vascular disease. Chest. 2010;138:270.
D’Alto M, Ghio S, D’Andrea A, et al. Inappropriate exercise-induced increase in pulmonary artery pressure in patients with systemic sclerosis. Heart. 2011;97:112–7.
Suzuki K, Akashi YJ, Manabe M, et al. Simple exercise echocardiography using a master’s two-step test for early detection of pulmonary arterial hypertension. J Cardiol. 2013;62:176–82.
Saggar R, Khanna D, Furst DE, et al. Exercise-induced pulmonary hypertension associated with systemic sclerosis: four distinct entities. Arthritis Rheum. 2010;62:3741–50.
Gargani L, Pignone A, Agoston G, et al. Clinical and echocardiographic correlations of exercise-induced pulmonary hypertension in systemic sclerosis: a multicenter study. Am Heart J. 2013;165:200–7.
Voilliot D, Magne J, Dulgheru R, et al. Determinants of exercise-induced pulmonary arterial hypertension in systemic sclerosis. Int J Cardiol. 2014;173:373–9.
Suzuki K, Izumo M, Kamijima R, et al. Influence of pulmonary vascular reserve on exercise-induced pulmonary hypertension in patients with systemic sclerosis. Echocardiography. 2015;32:428–35.
Grunig E, Janssen B, Mereles D, et al. Abnormal pulmonary artery pressure response in asymptomatic carriers of primary pulmonary hypertension gene. Circulation. 2000;102:1145–50.
Grunig E, Weissmann S, Ehlken N, et al. Stress doppler echocardiography in relatives of patients with idiopathic and familial pulmonary arterial hypertension: results of a multicenter european analysis of pulmonary artery pressure response to exercise and hypoxia. Circulation. 2009;119:1747–57.
Grunig E, Tiede H, Enyimayew EO, et al. Assessment and prognostic relevance of right ventricular contractile reserve in patients with severe pulmonary hypertension. Circulation. 2013;128:2005–15.
Grunig E, Mereles D, Hildebrandt W, et al. Stress Doppler echocardiography for identification of susceptibility to high altitude pulmonary edema. J Am Coll Cardiol. 2000;35:980–7.
Möller T, Brun H, Fredriksen PM, et al. Right ventricular systolic pressure response during exercise in adolescents born with atrial or ventricular septal defect. Am J Cardiol. 2010;105:1610–6.
Kusunose K, Popovic ZB, Motoki H, et al. Prognostic significance of exercise-induced right ventricular dysfunction in asymptomatic degenerative mitral regurgitation. Circ Cardiovasc Imaging. 2013;6:167–76.
Tolle JJ, Waxman AB, Van Horn TL, et al. Exercise-induced pulmonary arterial hypertension. Circulation. 2008;118:2183–9.
Kusunose K, Agarwal S, Marwick TH, et al. Decision making in asymptomatic aortic regurgitation in the era of guidelines: incremental values of resting and exercise cardiac dysfunction. Circ Cardiovasc Imaging. 2014;7:352–62.
Hill K, Dolmage TE, Woon L, et al. Comparing peak and submaximal cardiorespiratory responses during field walking tests with incremental cycle ergometry in COPD. Respirology. 2012;17:278–84.
Pope JE, Lee P, Baron M et al. Prevalence of elevated pulmonary arterial pressures measured by echocardiography in a multicenter study of patients with systemic sclerosis. J Rheumatol 2005;32:1273–8.
Kusunose K, Yamada H, Hotchi J, et al. Prediction of future overt pulmonary hypertension by 6-min walk stress echocardiography in patients with connective tissue disease. J Am Coll Cardiol. 2015;66:376–84.
Galie N, Rubin LJ, Hoeper M, et al. Treatment of patients with mildly symptomatic pulmonary arterial hypertension with bosentan (EARLY study): a double-blind, randomised controlled trial. Lancet 2008;371:2093–100.
Hickam JB, Cargill WH. Effect of exercise on cardiac output and pulmonary arterial pressure in normal persons and in patients with cardiovascular disease and pulmonary emphysema. J Clin Invest. 1948;27:10–23.
Lonsdorfer-Wolf E, Richard R, Doutreleau S, et al. Pulmonary hemodynamics during a strenuous intermittent exercise in healthy subjects. Med Sci Sports Exerc. 2003;35:1866–74.
Degre S, de Coster A, Messin R, et al. Normal pulmonary pressure-flow relationship during exercise in the sitting position. Int Z Angew Physiol. 1972;31:53–9.
Slonim NB, Ravin A, Balchum OJ, et al. The effect of mild exercise in the supine position on the pulmonary arterial pressure of five normal human subjects. J Clin Invest. 1954;33:1022–30.
Wagner PD, Gale GE, Moon RE, et al. Pulmonary gas exchange in humans exercising at sea level and simulated altitude. J Appl Physiol. 1985;1986(61):260–70.
Damato AN, Galante JG, Smith WM. Hemodynamic response to treadmill exercise in normal subjects. J Appl Physiol. 1966;21:959–66.
Reeves JT, Groves BM, Sutton JR, et al. Operation Everest II: preservation of cardiac function at extreme altitude. J Appl Physiol. 1985;1987(63):531–9.
Argiento P, Chesler N, Mule M, et al. Exercise stress echocardiography for the study of the pulmonary circulation. Eur Respir J. 2010;35:1273–8.
Kovacs G, Berghold A, Scheidl S, et al. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34:888–94.
Argiento P, Vanderpool RR, Mule M, et al. Exercise stress echocardiography of the pulmonary circulation: limits of normal and sex differences. Chest. 2012;142:1158–65.
Janicki JS, Weber KT, Likoff MJ, et al. The pressure-flow response of the pulmonary circulation in patients with heart failure and pulmonary vascular disease. Circulation. 1985;72:1270–8.
Blumberg FC, Riegger GA, Pfeifer M. Hemodynamic effects of aerosolized iloprost in pulmonary hypertension at rest and during exercise. Chest. 2002;121:1566–71.
Domingo E, Grignola JC, Aguilar R, et al. Impairment of pulmonary vascular reserve and right ventricular systolic reserve in pulmonary arterial hypertension. BMC Pulm Med. 2014;14:69.
Lau EM, Vanderpool RR, Choudhary P, et al. Dobutamine stress echocardiography for the assessment of pressure-flow relationships of the pulmonary circulation. Chest. 2014;146:959–66.
Lau EM, Manes A, Celermajer DS, et al. Early detection of pulmonary vascular disease in pulmonary arterial hypertension: time to move forward. Eur Heart J. 2011;32:2489–98.
Saggar R, Khanna D, Shapiro S, et al. Brief report: effect of ambrisentan treatment on exercise-induced pulmonary hypertension in systemic sclerosis: a prospective single-center, open-label pilot study. Arthritis Rheum. 2012;64:4072–7.
Hager WD, Collins I, Tate JP, et al. Exercise during cardiac catheterization distinguishes between pulmonary and left ventricular causes of dyspnea in systemic sclerosis patients. Clin Respir J. 2013;7:227–36.
Nagel C, Henn P, Ehlken N, et al. Stress Doppler echocardiography for early detection of systemic sclerosis-associated pulmonary arterial hypertension. Arthritis Res Ther. 2015;17:165.
Lewis GD, Lachmann J, Camuso J, et al. Sildenafil improves exercise hemodynamics and oxygen uptake in patients with systolic heart failure. Circulation. 2007;115:59–66.
Lewis GD, Murphy RM, Shah RV, et al. Pulmonary vascular response patterns during exercise in left ventricular systolic dysfunction predict exercise capacity and outcomes. Circ Heart Fail. 2011;4:276–85.
Mancini D, Katz S, Donchez L, et al. Coupling of hemodynamic measurements with oxygen consumption during exercise does not improve risk stratification in patients with heart failure. Circulation. 1996;94:2492–6.
Borlaug BA, Nishimura RA, Sorajja P, et al. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3:588–95.
Saito S, Miyamoto K, Nishimura M, et al. Effects of inhaled bronchodilators on pulmonary hemodynamics at rest and during exercise in patients with COPD. Chest. 1999;115:376–82.
Blanco I, Gimeno E, Munoz PA, et al. Hemodynamic and gas exchange effects of sildenafil in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Am J Respir Crit Care Med. 2010;181:270–8.
Maltais F, Jobin J, Sullivan MJ, et al. Metabolic and hemodynamic responses of lower limb during exercise in patients with COPD. J Appl Physiol. 1985;1998(84):1573–80.
Portillo K, Torralba Y, Blanco I, et al. Pulmonary hemodynamic profile in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1313–20.
Hilde JM, Skjorten I, Hansteen V, et al. Haemodynamic responses to exercise in patients with COPD. Eur Respir J. 2013;41:1031–41.
Hilde JM, Skjorten I, Grotta OJ, et al. Right ventricular dysfunction and remodeling in chronic obstructive pulmonary disease without pulmonary hypertension. J Am Coll Cardiol. 2013;62:1103–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Kenya Kusunose and Hirotsugu Yamada declare that they have no conflict of interest.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revisions. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Kusunose, K., Yamada, H. Rest and exercise echocardiography for early detection of pulmonary hypertension. J Echocardiogr 14, 2–12 (2016). https://doi.org/10.1007/s12574-015-0268-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-015-0268-y