Abstract
How does immunotherapy affect the evolutionary dynamics of cancer cells? Can we enhance the anti-cancer efficacy of T cells by using different types of immune boosters in combination? Bearing these questions in mind, we present a mathematical model of cancer–immune competition under immunotherapy. The model consists of a system of structured equations for the dynamics of cancer cells and activated T cells. Simulations highlight the ability of the model to reproduce the emergence of cancer immunoediting, that is, the well-documented process by which the immune system guides the somatic evolution of tumors by eliminating highly immunogenic cancer cells. Furthermore, numerical results suggest that more effective immunotherapy protocols can be designed by using therapeutic agents that boost T cell proliferation in combination with boosters of immune memory.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
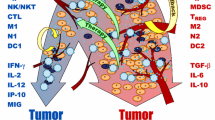
Immunotherapy is a type of treatment that can be used to boost or restore the ability of the immune system to fight cancer, infections or other form of disease. The molecular identification of human cancer antigens has allowed the development of different antigen-specific immunotherapy protocols. These include in vitro activation of autologous tumor T cells which are re-infused into patients after expansion, ex vivo expansion of autologous antigen-specific T cells which are then re-infused into patients, and vaccination with an antigen and an adjuvant to elicit therapeutic T cells [24, 28].
While T-cell-based therapies have been shown to boost the body’s ability to fight cancers such as leukemia, lymphoma and breast cancer, they have not improve the survival rates of patients with melanoma or lung cancer [29, 30]. However, current immunotherapy protocols have not resulted in durable clinical improvements, except in single patients [2, 13]. A possible reason for the limited ability of cytotoxic T cells to kill or to contain tumor growth is that they die quickly. In this scenario, the immune response is not sustained and cancer eventually returns. For this reason, current research trends include engineering cancer vaccines that induce both tumor-specific effector T cells, which can reduce the tumor mass, and tumor-specific memory T cells, which can control tumor relapse by providing the immune system with “memory” (i.e., they quickly expand becoming activated T cells upon re-exposure to their cognate antigen).
How does immunotherapy affect the evolutionary dynamics of cancer cells? Can we enhance the anti-cancer efficacy of T cells by using different types of immune boosters in combination? Bearing these questions in mind, we propose a structured population model that describes the dynamics of a well-mixed sample (i.e., space effects are, prima facie, kept aside) of cancer cells and activated T cells under immunotherapy. The immunotherapy we consider is based on the delivery of agents that boost the proliferation of T cells and immune memory. The model includes proliferation and death processes of both cancer cells and activated T cells. The mesoscopic formalism of the present model allows us to take into account microscopic features of cancer–immune competition, which is not possible in macroscopic models.
In spite of more complex mathematical models of cancer–immune competition [1–12, 14–20, 23, 25, 26], the one we present here relies on just a few parameters. In fact, as a first step of a long term project, this model is conceived as a tool to test different hypothetical scenarios, rather than to perform quantitative forecasts.
The reminder of the chapter is organized as follows. In Sect. 2, we describe the mathematical model and the related underlying assumptions. Section 3 introduces the general setup for numerical simulations and presents the results obtained under different parameter settings, which mimic different biological scenarios. We study the adaptation of the antigenic profile of cancer cells in response to the action exerted by activated T cells. We also analyze the evolution of the cancer cell density in the presence of T cell proliferation boosters and immune memory boosters. Finally, Sect. 4 contains the conclusions of this chapter and provides also ideas about future research perspectives.
2 The Model
As a reference system, we consider a population of cancer cells, structured by a non-negative real variable \(u \in U \subset \mathbb{R}_{+}\) that represents the antigenic expression, and a population of activated T cells, structured by a non-negative real variable v ∈ V ⊆ U that represents those antigens that T cells can effectively attack. For brevity, we refer to the variables u and v as traits of the cancer cells and T cells, respectively. Both cell populations are exposed to the action of two types of immunotherapies: one aimed at boosting the proliferation of activated T cells, and the other aimed at boosting immune memory. The local densities of cancer cells and T cells are modeled by the functions f C (t, u) ≥ 0 and f I (t, v) ≥ 0. The related total densities are computed as
We represent the infusion rates of therapeutic agents boosting proliferation and immune memory at time t ∈ [0, T] by the functions c P (t) ≥ 0 and c M (t) ≥ 0, respectively.
The biological phenomena of interest are modeled according to the assumptions and the strategies summarized below. Mathematical details are similar to those previously introduced in [6], apart from those which concern the modeling of immunotherapies:
Cancer Cell Proliferation and Competition for Resources In order to mimic cancer growth, we introduce a parameter κ C > 0, which models the average rate of cell proliferation net of apoptosis. Furthermore, since cellular proliferation is hampered by the competition for resources, we assume that interactions can lead cancer cells to die at an average rate μ C > 0.
Clonal Expansion of T Cells and Homeostatic Regulation In order to enhance the efficacy of immune response, T cells undergo a rapid in situ clonal expansion. We account for this process by including binary interactions between cancer cells with trait u and activated T cells with trait v, that occur at a rate described by the function
and lead to the proliferation of T cells. In order to model the selectivity of clonal expansion, the interaction rate is defined as a symmetric and decreasing function of the distance between the traits of the interacting cells. Parameter θ E > 0 measures, on average, the selectivity of the interactions. Moreover, due to the limited availability of nutrients, and homeostatic regulation mechanisms as well, T cells cannot proliferate in an unbounded way. As a consequence, we assume that they can die at an average rate μ I > 0 due to interactions with other cells of the same population.
Action of T Cells Against Cancer Cells T cells are able to target and kill cancer cells that express their cognate antigen. Therefore, we also include binary interactions between cancer cells with trait u and activated T cells with trait v, that occur at a rate described by function
and lead to the destruction of cancer cells. Considerations analogous to those drawn about function \(\eta _{\theta _{ E}}\) hold. It is worth noting that \(\eta _{\theta _{I}}(\cdot )\) may be different from \(\eta _{\theta _{E}}(\cdot )\), namely because clonal expansion and immune competition can be characterized by different levels of selectively.
Boosting of T Cell Proliferation and Immune Memory The effect of therapeutic agents that enhance the proliferation of T cells are modeled through an increase in the proliferation rate of T cells by parameter κ P > 0. On the other hand, the action of therapeutic agents that boost immune memory is modeled through a reduction in the death rate related to homeostatic regulation by parameter μ M > 0.
Therefore, we describe the dynamics of the two cell populations through the following system of structured equations
where R C and R I model the net proliferation rates of cancer cells and T cells, respectively,
Remark 1.
Since we assume a well-mixed cell sample, the current model does not account for any spatial dynamics. However, we note that the formalism at hand would allow us to incorporate spatial effects of the two cell populations. This could be namely done by integrating the modeling strategies presented in [22] with the considerations made in [8].
3 Numerical Results
In this section, we study the evolution of cancer cells under the effects of immunotherapy in the framework of the model presented in the previous section. In particular, our simulations
-
1.
analyze how cancer cells adapt to the immune response exerted by activated T cells, in the presence of therapeutic agents that boost the proliferation of activated T cells and immune memory;
-
2.
verify the existence of suitable infusion schemes that enhance the efficacy of immunotherapy protocols.
We assume \(U = V:= [0,1]\), while as a time domain we select the interval [0, T = 120]. Time is in units of the average cell cycle. We choose the initial conditions
where χ V is the characteristic function of the set V and the factors \(C_{C,I} \in \mathbb{R}_{+}\) are such that
These conditions mimic a biological scenario where, at the beginning of observations, the cancer cell population is almost monomorphic (i.e., most of the cancer cells are characterized by the same antigenic expression). Concurrently, the distribution of activated T cells over the possible antigenic expressions is assumed to be uniform.
In order to perform numerical simulations, we select a uniform grid with N = 400 points on the segment [0, 1]. We denote by f C (t k , u n ) ≥ 0 and f I (t k , v n ) ≥ 0 the numerical solutions at grid points u n = n Δ u and v n = n Δ v (space steps \(\varDelta u =\varDelta v = 1/N\)) and time t k = k Δ t (time step Δ t = 0. 1). Therefore,
We implement in Matlab the following implicit–explicit finite difference scheme, see e.g. [21],
where R C, I +(t k , u n ) and R C, I −(t k , v n ) denote, respectively, the positive and negative parts of the numerical approximations for R C (t, u) and R I (t, v).
For all simulations, the functions \(\eta _{\theta _{E}}\) and \(\eta _{\theta _{I}}\) are defined as
and the other parameters of the model are set as
The above functions and the related parameters are chosen to be simple and offering clear illustrations of the generic properties (2) and (3).
Definitions of functions c P and c M are selected case by case to mimic different infusion schedules. At first, we study the dynamics of cancer cells without immunotherapies, that is, when
Figure 1 shows the “chase-and-escape” dynamics of activated T cells and cancer cells, i.e.,
-
1.
clonal expansion leads to a rapid proliferation of those T cells that can effectively attack the antigens mostly expressed by the cancer cell population;
-
2.
the selective pressure exerted by activated T cells causes the selection of the cancer cells that are actually able to evade immune predation.
This cause the emergence of oscillations in the total densities of cancer cells and T cells (see the right panel of Fig. 1).
From the evolutionary perspective, let us note that immune competition pushes the monomorphic cancer cell population to become, in succession, dimorphic, trimorphic and then tetramorphic (i.e., most of the cells are characterized by two, three or four given antigenic expressions, respectively). In turn, the same pattern of evolution is followed by activated T cells with a certain delay, which is due to the time required to adapt to the antigenic distribution of cancer cells (see the left and center panels of Fig. 1). In the framework of our model, these evolutionary patterns can be seen as the result of cancer immunoediting, that is, the well-documented process by which the immune system guides the somatic evolution of tumors by eliminating highly immunogenic cancer cells [4, 9].
Cell dynamics without immune boosters. Evolution of f C (t, u) (left panel), f I (t, v) (center panel), ρ C (t) (right panel, solid line) and ρ I (t) (right panel, dashed line). Clonal expansion leads to a rapid proliferation of the T cells that can effectively attack the antigens mostly expressed by the cancer cell population. The selective pressure exerted by activated T cells causes, in turn, the selection of those cancer cells that are able to evade immune predation
Next we analyze the evolution of cancer cells under three different immunotherapy regimes:
-
1.
T cell proliferation boosters only, i.e.,
$$\displaystyle{ c_{P}(t):= C\mathop{sgn}\nolimits (\sin (\omega t))^{+},\qquad c_{ M}(t):= 0; }$$(7) -
2.
immune memory boosters only, i.e.,
$$\displaystyle{ c_{P}(t):= 0,\qquad c_{M}(t):= C\mathop{sgn}\nolimits (\sin (\omega t))^{+}; }$$(8) -
3.
simultaneous delivery of both boosters, i.e.,
$$\displaystyle{ c_{P}(t):= \frac{C} {2} \mathop{sgn}\nolimits (\sin (\omega t))^{+},\qquad c_{ M}(t):= \frac{C} {2} \mathop{sgn}\nolimits (\sin (\omega t))^{+}. }$$(9)
During simulations, we choose \(\omega = 10\pi /T\) and we test three different instances of infusion, which are characterized by picks of different height (see the center panels of Figs. 2, 3, 4), i.e., we set alternatively C = 4, C = 6 or C = 8. Provided that the same value of parameter C is selected, the integral
does not change under definitions (7)–(9), that is, the total delivered dose is kept the same in the three cases at hand. This is actually of primary importance to make a consistent comparison between the protocols under study.
At first, we study the effects of immunotherapy protocols that rely on the delivery of T cell proliferation boosters only, i.e., we perform simulations under definitions (7). The results presented in the left panels of Fig. 2 support the idea that boosters of T cell proliferation may only allow a temporary reduction in the total density of cancer cells, which is then followed by a relapse.
Next, we analyze the efficacy of immunotherapy protocols that make use of immune memory boosters only, i.e., we perform simulations under definitions (8). After a comparison between the results shown by the left panels of Fig. 3 and those presented in the right panel of Fig. 1, we are led to conclude that the dynamics of the cancer cell density is left almost unaltered with respect to the case without therapies. The addition of oscillations seems to be the only significant effect.
Cell dynamics with boosters of immune memory. Evolution of ρ C (t), ρ I (t) and c M (t) for C = 4 (dotted lines), C = 6 (dashed lines) and C = 8 (solid lines). Immune memory boosters leave the qualitative dynamics of the cancer cell density almost unaltered with respect to the case without therapies (to be compared with the right panel of Fig. 1), apart from the addition of oscillations in the total density of cancer cells
Finally, we consider the case where the two types of immune boosters are used in combination, i.e., we perform simulations under definitions (9). The results shown by the lower left panel of Fig. 4 support the idea that if the two types of immune boosters considered are used in combination, then there exists certain doses that make it possible to push the cancer cell population toward extinction, and effectively control tumor relapse. This may be due to the fact that the simultaneous delivery of T cell proliferation boosters and boosters of immune memory at sufficiently high doses allows the total density of immune cells to attain higher values (compare the center panel of Fig. 4 with the center panels of Figs. 2 and 3).
Cell dynamics with boosters of T cell proliferation in combination with boosters of immune memory. Evolution of ρ C (t), ρ I (t) and c P (t) + c M (t) for C = 4 (dotted lines), C = 6 (dashed lines) and C = 8 (solid lines). If the two types of immune boosters considered are used in combination, then there exists certain doses that allow to achieve the complete eradication of cancer cells
The qualitative properties of the results presented in Figs. 2, 3, 4 are left unaltered by variations of the parameter values (6), within reasonable ranges. Furthermore, let us note that we have developed additional simulations (data not shown) under the following definitions of functions c P and c M
with \(\omega = 10\pi /T\). The obtained results highlight how protocols that rely on the alternate delivery of T cell proliferation boosters and boosters of immune memory do not allow to eradicate the cancer cell population.
These results lead us to conclude that, with the doses used in our tests, more effective immunotherapy protocols can be designed by using combinations of therapeutic agents that boost T cell proliferation and immune memory. This is in agreement with the ideas presented in [11, 27].
4 Conclusions and Perspectives
In this chapter, we have presented a structured population model that describes the dynamics of a well-mixed sample of cancer cells and activated T cells under immunotherapy. The immunotherapy we consider is based on the delivery of agents that boost the proliferation of T cells and immune memory. The model includes proliferation and death processes of both cancer cells and activated T cells, as well as clonal expansion of T cells and their action against cancer cells.
In spite of more complex mathematical models of cancer–immune competition, the one we have presented here relies on just a few parameters and it is conceived as a tool to test different hypothetical scenarios, rather than to perform quantitative forecasts. In the framework of this model, we have studied, through numerical simulations, the adaptation of the antigenic profile of cancer cells in response to the action exerted by activated T cells. We have also analyzed the evolution of cancer cell density in the presence of T cell proliferation boosters only, immune memory boosters only, and combination of them.
Despite its simplicity, the model seems able reproduce the emergence of the “chase-and-escape” dynamics involving activated T cells and cancer cells. Furthermore, the results presented here support the idea that, ceteris paribus, more effective immunotherapy protocols can be designed by using suitable combinations of therapeutic agents that boost both T cell proliferation and immune memory.
Future research will be focussing on refining the modeling strategies of the evolutionary dynamics of cancer cells. For instance, a natural improvement of the model would be to include an additional structuring variable, let us say w, related to the proliferative potential of cancer cells, and replace the parameter κ C with an increasing function of this variable. Furthermore, since cell proliferation implies resource reallocation (i.e., redistribution of energetic resources from competition-oriented tasks toward development and maintenance of proliferative potential), it might also be worth replacing parameter μ C and function \(\eta _{\theta _{ I}}\) with some functions μ C (w) and \(\eta _{\theta _{I}}(\vert u - v\vert,w)\).
From a mathematical standpoint, it could be interesting to provide a detailed characterization of the oscillations that arise in the total densities of the two cell populations. Namely the techniques applied in [21] may prove to be useful to show that the evolution equations for ρ C, I (t) can resemble a kind of Lotka–Volterra system, under a proper time rescaling together with suitable assumptions on the functions and parameters of the model.
References
Agliari, E., Barra, A., Guerra, F., Moauro, F.: A thermodynamical perspective of immune capabilities. J. Theor. Biol. 287, 48–63 (2010)
Brichard, V., Dréno, B., Tessier, M.H., Rankin, E., Parmiani, G., Arienti, F., Humblet, Y., Bourlond, A., Vanwijck, R., Liénard, D., Beauduin, M., Dietrich, P.Y., Russo, V., Kerger, J., Masucci, G., Jäger, E., De Greve, J., Atzpodien, J., Brasseur, F., Coulie, P.G., van der Bruggen, P., Boon, T.: Tumor regressions observed in patients with metastatic melanoma treated with an antigenic peptide encoded by gene MAGE-3 and presented by HLA-A1. Int. J. Cancer 80, 219–230 (1999)
Bunimovich-Mendrazitsky, S., Byrne, H., Stone, L.: Mathematical model of pulsed immunotherapy for superficial bladder cancer. Bull. Math. Biol. 70, 2055–2076 (2008)
Burgess, D.J.: Tumour immunogenicity: editorial selection demystified. Nat. Rev. Cancer 12, 227 (2012)
Calvez, V., Korobeinikov, A., Maini, P.K.: Cluster formation for multi-strain infections with cross-immunity. J. Theor. Biol. 233, 75–83 (2005)
Delitala, M., Lorenzi, T.: Recognition and learning in a mathematical model for immune response against cancer. Discrete Contin. Dyn. Syst. Ser. B 18, 891–914 (2013)
De Pillis, L.G., Radunskaya, A.E., Wiseman, C.L.: A validated mathematical model of cell-mediated immune response to tumor growth. Cancer Res. 65, 7950–7958 (2005)
De Pillis, L.G., Mallet, D.G., Radunskaya, A.E.: Spatial tumor-immune modeling. Comput. Math. Meth. Med. 7, 159–176 (2006)
DuPage, M., Mazumdar, C., Schmidt, L.M., Cheung, A.F., Jacks, T.: Expression of tumour-specific antigens underlies cancer immunoediting. Nature 482, 405–409 (2012)
Eftimie, R., Bramson, J.L., Earn, D.J.: Interactions between the immune system and cancer: a brief review of non-spatial mathematical models. Bull. Math. Biol. 73, 2–32 (2011)
Guloglu, F.B., Ellis, J.S., Wan, X., Dhakal, M., Hoeman, C.M., Cascio, J.A., Zaghouani, H.: Antigen-free adjuvant assists late effector CD4 T cells to transit to memory in lymphopenic hosts. J. Immunol. 191, 1126–1135 (2013)
Hillen, T., Enderling, H., Hahnfeld, P.: The tumor growth paradox and immune system-mediated selection for cancer stem cells. Bull. Math. Biol. 75, 161–184 (2013)
Jäeger, E., Bernhard, H., Romero, P., Ringhoffer, M., Arand, M., Karbach, J., Ilsemann, C., Hagedorn, M., Knuth, A.: Generation of cytotoxic T-cell responses with synthetic melanoma-associated peptides in vivo: implications for tumor vaccines with melanoma-associated antigens. Int. J. Cancer 66, 162–169 (1996)
Kim, P., Lee, P., Peter, P.: Dynamics and potential impact of the immune response to chronic myelogenous leukemia. PLoS Comput. Biol. 4, e1000095 (2008)
Kim, P., Lee, P., Levy, D.: A theory of immunodominance and adaptive regulation. Bull. Math. Biol. 73, 1645–1665 (2011)
Komarova, N., Barnes, E., Klenerman, P., Wodarz, D.: Boosting immunity by anti-viral drug therapy: a simple relationship between timing, efficacy and success. Proc. Natl. Acad. Sci. 100, 1855–1860 (2008)
Kolev, M., Kozlowska, E., Lachowicz, M.: A mathematical model for single cell cancer-immune system dynamics. Math. Comput. Model. 41, 1083–1095 (2005)
Kzhyshkowska, J., Marciniak-Czochra, A., Gratchev, A.: Perspectives of mathematical modelling for understanding of macrophage function. Immunobiology 212, 813–825 (2007)
Ledzewicz, U., d’Onofrio, A., Schattler, H.: Tumor development under combination treatments with anti-angiogenic therapies. Mathematical methods and models in biomedicine. Lecture Notes on Mathematical Modelling in the Life Sciences, pp. 311–337. Springer, New York (2013)
Lollini, P.L., Palladini, A., Pappalardo, F., Motta, S.: Predictive models in tumor immunology. In: Bellomo, N., De Angelis, E. (eds.) Selected Topics in Cancer Modeling, vol. 4, pp. 363–384. Birkhäuser, Boston (2008)
Lorenzi, T., Lorz, A., Restori, G.: Asymptotic dynamics in populations structured by sensitivity to global warming and habitat shrinking. Acta Appl. Math. (2013). doi:10.1007/s10440-013-9849-9
Lorz, A., Lorenzi, T., Clairambault, J., Escargueil, A., Perthame, B.: Effects of space structure and combination therapies on phenotypic heterogeneity and drug resistance in solid tumors (2013, preprint)
Matzavinos, A., Chaplain, M.A.J., Kuznetsov, V.A.: Mathematical modelling of the spatio-temporal response of cytotoxic T-lymphocytes to a solid tumor. Math. Med. Biol. 21, 1–34 (2004)
Palucka, K., Banchereau, J.: Cancer immunotherapy via dendritic cells. Nat. Rev. Cancer 12, 265–277 (2012)
Perelson, A., Weisbuch, G.: Immunology for physicists. Rev. Mod. Phys. 69, 1219–1268 (1997)
Plesa, A., Ciuperca, G., Genieys, S., Louvet, V., Pujo-Menjouet, L., Dumontet, C., Volpert, V.: Diagnostics of the AML with immunophenotypical data. Math. Mod. Nat. Phen. 2, 104–123 (2006)
Ravkov, E.V., Williams, M.A.: The magnitude of CD4+ T cell recall responses is controlled by the duration of the secondary stimulus. J. Immunol. 183, 2382–2389 (2009)
Ricupito, A., Grioni, M., Calcinotto, A., Hess Michelini, R., Longhi, R., Mondino, A., Bellone, M.: Booster vaccinations against cancer are critical in prophylactic but detrimental in therapeutic settings. Cancer Res. 73, 3545–3554 (2013)
Rosenberg, S.A., Yannelli, J.R., Yang, J.C., Topalian, S.L., Schwartzentruber, D.J., Weber, S.J., Parkinson, D.R., Seipp, C.A., Einhorn, J.H., White, D.E.: Treatment of patients with metastatic melanoma with autologous tumorinfiltrating lymphocytes and interleukin 2. J. Natl. Cancer Inst. 86, 1159–1166 (1994)
Semino, C., Martini, L., Queirolo, P., Cangemi, G., Costa, R., Alloisio, A., Ferlazzo, G., Sertoli, M.R., Reali, U.M., Ratto, G.B., Melioli, G.: Adoptive immunotherapy of advanced solid tumors: an eight year clinical experience. Anticancer Res. 19, 5645–5649 (1999)
Acknowledgements
This work has been partially supported by the FIRB project—RBID08PP3J, the Fondation Sciences Mathématiques de Paris (FSMP) and by a public grant overseen by the French National Research Agency (ANR) as part of the “Investissements d’Avenir” program (reference: ANR-10-LABX-0098).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this paper
Cite this paper
Delitala, M., Lorenzi, T., Melensi, M. (2014). A Structured Population Model of Competition Between Cancer Cells and T Cells Under Immunotherapy. In: Eladdadi, A., Kim, P., Mallet, D. (eds) Mathematical Models of Tumor-Immune System Dynamics. Springer Proceedings in Mathematics & Statistics, vol 107. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1793-8_3
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1793-8_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1792-1
Online ISBN: 978-1-4939-1793-8
eBook Packages: Mathematics and StatisticsMathematics and Statistics (R0)