Abstract
Epigenetic therapy is a recognized central therapeutic strategy widely used in treatment of myelodysplatic syndrome (MDS). The approved agents, decitabine and azacytidine, are DNA hypomethylating agents that have been shown in randomized phase III trials to have clinical benefit in MDS patients. New research is investigating the use of these drugs in the setting of acute myeloid leukemia (AML) treatment, especially in older patients. Early studies are demonstrating promising results for the use of decitabine and azacytidine in treatment of AML. Other novel epigenetic/hypomethylating agents as well as chemotherapy combinations including hypomethylating agents represent an active area of research in treatment of AML patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
One of the first reports of methylation, specifically, hypermethylation, identifying this process as an important component of hematologic malignancies in humans, including acute myeloid leukemia (AML), was by Baylin et al. in the 1980s (Baylin et al. 1987; Jones and Baylin 2007). Since these early reports, it has become apparent that DNA methylation is a common event in myelodysplatic syndrome (MDS) (Garcia-Manero 2011) and that this so-called epigenetic aberrancy has the potential to be targeted for pharmacologic intervention with the hypomethylator agents (azacytidine, decitabine), now approved for MDS and being tested in AML settings (McDevitt 2012; Flotho et al. 2009). Indeed, it is the discovery of DNA methylation itself being one of the many fundamental methods by which the carcinogenesis of AML is possibly propagated, demonstrated by DNA methylation profiling and quantitative assays that is leading to many groups testing the hypothesis that hypomethylating agents in the clinic may be of clinical benefit to AML patients (Jain et al. 2009; Bullinger et al. 2010; Figueroa et al. 2010; Issa and Kantarjian 2009; Galm et al. 2005; Valk et al. 2004; Schoofs and Muller-Tidow 2011). This chapter will focus on the development of research efforts with regard to the clinical applications of hypomethylator therapy, with the two approved hypomethylating agents widely available today, decitabine and azacytidine, both approved for the treatment of MDS, and now being actively studied for use in patients with AML.
2 Decitabine in AML
2.1 Decitabine: Background
Decitabine (5-aza-2’-deoxycytidine, Dacogen, Eisai Inc, Astex Pharmaceauticals), is an analog of the DNA base cytidine . It is a DNA-hypomethylating agent, received its Food and Drug Administration (FDA) approval for use in MDS after studies including a large randomized phase III trial led by Kantarjian et al. demonstrated clinical activity in a wide range of MDS patients (Kantarjian et al. 2006). In this study, 170 patients with diagnosis of MDS experienced randomization to receive either decitabine 15 mg/m2 intravenously every 8 h for 3 days for every 6 weeks versus best supportive care. An overall response rate of 17 % in the decitabine arm, compared to 0 % in the supportive care arm (p < 0.001). Those treated in the decitabine arm had trend in direction of a longer median time to progression to AML or death when compared to those patients who received supportive care (12.1 months vs. 7.8 months, p = 0.16). Importantly, 18 % of the patients in this trial had bone marrow blasts 20–30 % at diagnosis, actually qualifying them as AML as per revised WHO classification, indicating possibility for activity among AML patient population of single agent decitabine.
With regard to investigating the antileukemic potential for decitabine, one of the original studies to demonstrate in vitro rationale was performed by Momparler et al. (1984) in which decitabine treatment resulted in more than 70 % inhibition of DNA methylation in leukemia cells suggesting that the process of DNA methylation inhibition to be the mechanism of action of decitiabine against leukemia cells .
Gattei et al. (1993) examined the in vitro sensitivity of blast progenitors to decitabine in nine AML patient samples clinically treated with decitabine, and demonstrated that the sensitivity of progenitor blasts in culture suspension correlated with the remission outcomes in AML patients.
Methylation profiling in AML patient samples has demonstrated a myriad of defects in methylation among AML patients. In one study, the frequency of hypermethylation of several genes, in particular, SDC4, GPR37, PITX2, and MYOD1 was high among AML patients (range 47–64%) in this study of 36 AML patient cases, suggesting that there might be a group of AML patients with potential to benefit from hypomethylating agents (Toyota et al. 2001) .
In addition to these data, accumulating evidence is showing that the mechanism of action of decitabine in AML may also involve antileukemia activity that is independent of methylation effects via microarray analysis assays (Schmelz et al. 2005). One such mechanism is via decitabine-induced caspase activation elaborating antileukemia activity (Tamm et al. 2005).
Further investigations of dectiabine as a single agent therapy in AML have included pharmacokinetic evaluation of the drug in MDS and AML. Cashen et al. demonstrated that decitabine, when dosed at 15 mg/m2 intravenous schedule every 8 h for 3 days, yielded a definable, tolerable side-effect profile in MDS/AML patients and that the pharmacokinetic (PK) value of decitabine measured over multiple cycles was unchanged and stable (Cashen et al. 2008). With demonstration of the low-dose schedule of decitabine and its overall safety and tolerable side-effect report in AML patients, it appears that decitabine might be especially promising for older or unfit patients with AML who are not candidates for intensive therapy (Bryan et al. 2011) .
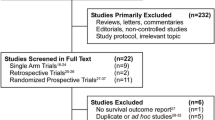
2.2 Clinical Trials of Decitabine in AML
2.2.1 Single-Agent Trials
Because of the relative dearth of therapeutically active agents available for the treatment of AML, especially among older patients, novel treatment strategies have been investigated, including promising early results of the hypomethylator agents such as decitabine in clinical trials (Kantarjian et al. 1996; Lubbert and Minden 2005) .
In the initial treatment designs incorporating decitabine into AML therapies, early investigators explored high doses of the hypomethylator drug in a similar approach to cytarabine-based strategies. Dosing schedules featuring total doses as high as 3000 mg/m2 were used in one of these initial studies (Richel et al. 1991).
One early study in 22 pediatric patients treated with decitabine with relapsed/refractory AML and acute lymphoblastic leukemia (ALL) demonstrated 14 % overall response (9% complete remission, CR, and 5 % partial remission, PR) (Rivard et al. 1981). Focusing on patients with AML, Momparler et al. treated a group of 27 patients with relapsed disease with decitabine 37–81 mg/m2 per cycle (over 36–60 h) and found an overall clinical response rate of 85 % (22 % CR, 15 % PR) (Momparler et al. 1985).
A key study involving patients with MDS, chronic myeloid leukemia (CML), and AML was an important early study to demonstrate the concept and feasibility of administering decitabine, over multiple cycles, in older patients (Pinto et al. 1989). In this study of 19 older-age patients (receiving total doses of 135–810 mg/m2), the overall response rate was found to be 70 % (15 % CR, 30 % PR) with median response duration of 12 months (range 6–> 58) and overall survival of 19 (7–> 64) months.
A pilot study by Petti et al. showed promise for decitabine in treatment of AML, especially for treatment possibilities in older or unfit patients (Petti et al. 1993). In this trial, the goal was to observe the efficacy and toxicity of decitabine in AML patients with particularly poor prognosis. The investigators evaluated 12 patients with AML; all received decitabine at dosing 90–120 mg/m2 intravenously every 8 h for 3 days for every 4–6 weeks. With 10 out of 12 of these patients evaluable for response, it was demonstrated that CR occurred in 3 patients and PR in 1 patient. As demonstrated by laboratory correlative work (immunophenotype testing and kinetic of remission studies), achievement of CR and PR with decitabine may have resulted via induction of leukemia cell differentiation .
In a phase I trial, Issa et al. studied decitabine administered in low dose, repeated dosing schedule in a cohort of relapsed and refractory leukemia patients. Out of 50 patients, 44 had MDS/AML. The dosing schedule that resulted in most responses was 15 mg/m2 for 10 days (11 of 17 patients, 65 %) (Issa et al. 2004).
A retrospective study by Ravandi et al. suggested that therapy with hypomethylating agents (decitabine or azacytidine) improved the outcomes of an especially poor cytogenetic group, high-risk MDS and AML patients with abnormalities of chromosome 5 and 7 (Ravandi et al. 2009). In this study, 81 patients with either high-risk MDS (54 %) or AML (46 %) received hypomethylator therapy and overall survival was favorable in those treated with hypomethylator as compared to a similar group who received intensive chemotherapy (p = 0.019) .
2.2.2 Phase II Trials: Decitabine in AML
Three separate phase II clinical trials of decitabine in AML patients have been recently reported, one study featuring a 5-day dosing schedule and the other a 10-day dosing schedule .
In the first phase II trial, a multicenter effort by Cashen et al. reported on a single-arm, open label, phase II trial of older AML patients (age greater than or equal to 60) receiving front-line therapy with decitabine (Cashen et al. 2010). A dosing schedule of 20 mg/m2 intravenously over 5 days every 4 weeks was utilized. Median of three cycles with range of 1–25 cycles was administered. Out of 55 AML patients with a mean age of 74 years, and median bone marrow blasts at presentation of 50 % (range 0–99), the reported overall response rate was 25 % (CR 24 %), even in patients with particularly poor/high-risk disease status such as antecedent MDS or high-risk cytogenetic groups. In this study, the overall survival was found to be 7.7 months (range 5.7–11.6 months); median survival for those patients achieving CR or a CRi reached 14 months. The most commonly occurring side effects in this trial were myelosuppression (100 %), neutropenic fever (29 %) and fatigue (26 %). Based on these promising phase II results, the authors suggested that a phase III study would be warranted to continue to study decitabine in the treatment of older AML patients .
In the other phase II trial, a single center study by Blum et al. (2010), exploration of a 10-day dosing schema (given as 20 mg/m2, intravenously, over 1 h, on 10 consecutive days, days 1–10 of each cycle) of decitabine in AML patients was conducted. With a median age of 74 years (range 60–85), investigators evaluated 53 AML patients for treatment with single-agent decitabine in the frontline setting. Median number of four cycles was administered. Overall response rate was 64 % (25 patients (47 %) achieved CR and 9 patients CRi). As in the Cashen study, responses were noted across subgroup types, including poor prognostic subgroups of antecedent MDS and high-risk cytogenetics. Besides myelosuppression, neutropenic fever and infection were most common side effects with 31 patients (58 %) experiencing a grade 3 or greater infection event in the first two cycles of the therapy. Laboratory correlatives were performed in this study, including the measurement of mir-29b expression. Among 23 patients who had samples prior to treatment available for analysis, investigators in this study found that 11 of these patients had achieved CR. The analysis demonstrated that those patients with response to therapy with decitabine had a higher pre-therapy level of mir-29b than those patients who did not respond (p = 0.02) .
In the third phase II trial, Lubbert et al. (2012) evaluated 227 frontline AML patients with high-risk features and median 72 years treated with decitabine alone (although, notably, this trial did include administration of all-trans retinoic acid (ATRA) given to 100 patients in course 2 of therapy). CR was found to be 26 %, and even patients with high-risk features had responses (e.g., monosomal karyotype) with this approach, and median overall survival was 5.5 months (range 0–> 57.5). On the basis of the promising results of these phase II trials, investigators have sought to further evaluate in the phase III setting .
2.2.3 Phase III Trials: Decitabine in AML
Two large phase III trials with AML patients receiving decitabine in the upfront setting have been recently reported .
In the trial led by Kantarjian et al. (2012), a randomized phase III trial was conducted at multiple sites in which comparison was studied between decitabine versus best supportive care or low-dose cytarabine in untreated AML patients age 65 or older. The investigators evaluated 485 patients in a 1:1 randomization schema of one arm with decitabine 20 mg/m2 daily for 5 days every 28 days versus an arm with either best supportive care (including blood product transfusions) or low-dose cytarabine given at 20 mg/m2 subcutaneous injection for 10 days every 28 days. Primary endpoint of the clinical study was overall survival. With a median age of 73 years (range 64–91 years), and 36 % with poor risk cytogenetics, the authors demonstrated a significantly higher remission rate (CR/CRp) in the decitabine treated arm versus the non-dectiabine treated arm (17.8 vs. 7.8 %, respectively, with p = 0.001) and a median overall survival of 7.7 months in the decitabine treated arm and 5 months in the non-decitabine treatment arm (the p value was not significant). Patients in this trial received a median of four cycles of therapy with over 26.5 % of the patients receiving nine or more cycles .
In another large phase III study, Lubbert et al. (2011) tested decitabine compared to best supportive care in older patients with MDS (high-risk disease). Decitabine was administered at low dosing schedule (15 mg/m2 intravenously, three times a day for 3 days, during 6-week cycles). Importantly, in this clinical trial, 32 % of the patients met criteria for AML by WHO classification (equal to or greater than 20 % blasts). The trial was open for enrollment to patients aged 60 or greater. With 233 patients evaluated, median age was 70 years (range 60–90 years). Notably, 53 % had poor risk cytogenetics. The investigators demonstrated that PFS was significantly increased for decitabine arm compared to best supportive care arm (median PFS = 6.6 months compared to 3.0 months, p = 0.004); in addition, the risk of AML transformation at 1 year timepoint was also significantly lowered in decitabine arm (p = 0.036). In terms of overall survival, there was no significant difference between the two groups (10.1 months for decitabine arm, 8.5 months for best supportive care arm) .
2.2.4 Combination Studies
Early studies showed promising results with possibilities for decitabine to be used in combination with other agents in treatment of AML patients. One approach of these earlier trials focused on combination of decitabine with either amsacrine or an anthracycline in relapsed/refractory acute leukemia patients (Richel et al. 1991; Willemze et al. 1993; Schwartsmann et al. 1997; Willemze et al. 1997) and these promising results suggested that decitabine had a more tolerable toxicity profile than Ara-C and that combination studies should be further studied.
More recently, there has been interest in combining hypomethylator agents with histone deacetylase inhibitors for AML patients. In a phase I/II trial conducted by Garcia-Manero et al. (Garcia-Manero et al. 2006), both untreated (older, unfit) and relapsed/refractory AML patients were treated with the combination of decitabine and valproic acid. Out of 54 patients evaluated, the investigators found 10 CRs (19 %) and 2 CRp (3 %) with remission duration of 7.2 months and overall survival of 15.3 months in responding patients, suggesting that this combined epigenetic chemotherapy approach was feasible. In another phase I study, Blum et al. (2007) also evaluated the combination of decitabine and valproic acid in an AML population. Out of 25 patients with median age of 70 years, 13 patients had relapsed AML. In this phase I study designed to find the optimal biologic dose of decitabine in this population and the maximum tolerated dose (MTD) of the valproic acid in combination with decitabine, the investigators reported a response rate of 44 %, 4 with CR, 4 with CRi, 3 PR. Importantly, the authors concluded that the addition of valproic acid led to observed encephalopathy at even low doses and that the drug and dose to be studied further could be decitabine at 20 mg/m2 per day for 10 days alone,with the possibility of another histone deacetylatalse agent. .
Many other decitabine-based combinations are continuing to be tested in clinical trials. One study reviewed the combination of decitabine with gemtuzumab ozogamicin , and found among 12 AML patients treated with this combination, 5 (42%) attained CR and went on to SCT with overall good side-effect profile (Chowdhury et al. 2009). Another combination approach featured clofarabine with addition of low dose Ara-C alternating with decitabine in older AML patients (Faderl et al. 2012). In this trial, Faderl et al. (2012) evaluated 60 newly diagnosed AML patients with median age of 70 years. In this strategy, patients were allowed to receive up to 17 cycles of consolidation therapy that included decitabine. CR was achieved in 58 %, median overall survival 12.7 months and mortality during induction was 7 % at 8 weeks with tolerable side-effect profile, suggesting a combined cytotoxic chemotherapy/hypomethylator approach could be utilized in an older AML patient population. Yet another combination approach was recently reported by Blum et al. with decitabine combined with bortezomib (Blum et al. 2012). The authors studied this combination in 19 AML patients determined to be higher-risk AML, with median age of 70 years; decitabine was given as 20 mg/m2 with 10-day dosing days 1–10 and bortezomib was added at escalating doses to 1.3 mg/m2 goal dose on days 5, 8, 12, and 15. The authors found five of ten patients (50 %) with untreated AML had CR/CRi. Of interest, researchers found that bortezomib contributed to downregulation of FLT3 at the end of cycle one as a pharmacodynamic endpoint .
2.3 Decitabine in AML and SCT
Several early studies have explored the possibility of utilizing decitabine for treatment of AML in the stem cell transplant (SCT) treatment setting. Giralt et al. (1997) performed two studies that sought to evaluate the safety and efficacy of decitabine in both the post-transplant leukemia relapse setting and with decitabine as a component of conditioning therapy regimen prior to SCT. In one small study, the authors examined three leukemia patients (two with AML) treated in the post-SCT relapse setting; treatment was with decitabine as a single agent at 1000 mg/m2 total dose. This study demonstrated median time to relapse of 7 months. In another small study, the authors demonstrated that four leukemia patients (one with AML) were able to successfully tolerate decitabine as part of an SCT conditioning regimen.
In addition, a phase I study showed encouraging data that decitabine (doses of 100–150 mg/m2 every 12 h for 5 days) plus a donor stem cell infusion from original donor in the post-SCT setting was a tolerable and feasible approach (Ravandi et al. 2001).
The combination of decitabine with cyclophosphamide and busulfan, to form a novel conditioning regimen for leukemia patients undergoing allogeneic SCT was investigated by de Lima et al. (2003). In this study, 12 AML patients were included out of 23 total leukemia patients evaluated. The authors described no instances of rate limiting toxicity from the decitabine and demonstrated 26 % of the patients still alive at 3.3 years after SCT.
To further explore the idea of utilizing decitabine in the SCT setting especially in older MDS and AML patients, Lubbert et al. (2009) evaluated 15 MDS/AML patients. With a median age of 69 years (range 60–75 years), 5 of 15 patients had AML. The total group showed a very tolerable side-effect profile with use of decitabine in the frontline treatment setting, which was followed by conditioning chemotherapy in preparation for SCT. The authors suggested that decitabine-based approaches could be considered as a treatment option in those MDS/AML patients who are not candidates for intensive chemotherapy.
2.4 Future Directions
2.4.1 Epigenetic Priming
One promising approach to AML patients is the concept of epigenetic priming therapy. In this treatment strategy, investigators administer a hypomethylating agent prior to administration of cytotoxic chemotherapy. Recently, Scandura et al. (2011) reported early results of this approach in which they tested in phase I setting, decitabine (in two different dose schedules) followed by standard cytotoxic chemotherapy program of anthracyline (daunorubicin 60 mg/m2 for three doses) and ARA-C (100 mg/m2 for 7 days). Investigators found that 90 % of patients had a response to therapy (27 patients) with 17 CR and 10 PR. These promising early results suggest that epigenetic priming therapy warrants further investigation in the AML setting.
2.4.2 Decitabine as Maintenance Therapy
The role for hypomethylator agents in the maintenance setting for AML patients is actively being tested . One such study featured a treatment approach with AML patients in CR or subsequent CR being randomized to maintenance with conventional care versus decitabine up to 12 cycles (Boumber et al. 2012). Among 50 patients enrolled with median age 57 years, this trial showed feasibility of the notion for decitabine as a potential maintenance strategy in AML patients in CR, with a trend to less patients relapsing in the decitabine treated group versus conventional care, although the difference was not reported to be statistically significant. Further studies will be warranted to investigate the use of hypomethylating drugs in the AML maintenance setting.
2.4.3 SGI-110
The development of novel DNA hypomethylating agents represents a new area of research in the field of MDS and AML. One such agent is SGI-110 (Astex Pharmaceuticals), which is a decitabine-guanosine dinucleotide that is linked by a phosphodiester linker. The pharmacokinetics are different that decitabine, in that its subcutaneous administration and slower release of its active metabolite (decitabine) has the potential to result in longer exposure to active drug. This agent is currently being tested in an ongoing multi-center phase I/II study testing different dose schedules of SGI-110 in relapsed/refractory AML patients.
3 Azacytidine in AML
3.1 Background: Azacytidine
5-azacytidine (azacytidine, Vidaza, Celgene) is a DNA-hypomethylating agent approved by the FDA for the treatment of MDS . This approval was based on the results of two large phase III studies, the CALGB 9221 trial (Silverman et al. 2002), and the AZA-001 trial, a large randomized phase III trial (Fenaux et al. 2009; Keating 2012). In the AZA-001 trial, Fenaux et al. (2009) evaluated 358 patients and demonstrated an increased overall survival in high-risk MDS patients receiving azacytidine versus other conventional care regimens (azacytidine cohort median overall survival 24.5 months vs. 15.0 months for conventional care cohort, p = 0.0001). In the CALGB 9221 study, Silverman et al. (2002) randomized 191 MDS patients to evaluate azacytidine versus supportive care. In this trial, it was shown that overall response rates were higher in the azacytidine arm, along with landmark analysis at 6 months (performed to account for crossover confounding effects) demonstrating median overall survival of 18 months in azacytidine arm versus 11 months in supportive care arm (p = 0.03) .
3.2 Clinical Trials in AML
3.2.1 Phase I/II Clinical Trials, Single-Agent Azacytidine in AML
With regard to the development of azacytidine in the field of AML, the earliest clinical reports of this specific use are from Hrodek and Vesely (1972) in the 1970s, in which the first signal of azacytidine’s potential antileukemic activity was demonstrated in pediatric leukemia patients (Santini et al. 2001) . Building on these early results, Karon et al. and McCreadie et al. conducted clinical trials both published in 1973. In the trial by Karon et al., in which 37 pediatric patients (ages 2–17 years), with acute leukemias who have failed treatment with standard Ara-C based chemotherapy, were given 5-azacytidine (days 1–5 every 2 weeks). Among AML patients, the authors demonstrated that 6 out of 14 (43 %) patients achieved remission status in the bone marrow (Karon et al. 1973). In the trial by McCredie et al. (1973), a total of 28 patients with acute leukemias were treated with 5 days intravenous administration of azacytidine, demonstrating an overall response rate of 28 % . Both of these early studies suggested activity for azacytidine as an antileukemic drug even in Ara-C refractory patients. Further studies in the mid- and late-1970s contributed to mounting interest and evidence in azacytidine-based AML therapy with larger studies of larger number of patients continuing to show safety, feasibility, and tolerability in addition to high response rates and even CRs with this chemotherapeutic approach in AML patients (Von Hoff et al. 1976; Vogler et al. 1976; Saiki et al. 1978).
In the 1980s, one of the notable trials in this field was led by Saiki et al. (1981). In this trial, the authors analyzed 154 relapsed/refractory acute leukemia patients who were treated with azacytidine. The authors focused on evaluating different dosing schedules. Overall, CR was achieved in nine patients in this study. The authors concluded that there was clinical benefit and less toxicity profile with lower dose, continuous infusion dose schedules with duration of 5, 7, and 10 days .
A retrospective review of 20 AML patients (by WHO) with low blast count (21–38 %) and who were found to be poor candidates for intensive chemotherapy, were given therapy with azacytidine. This study reported four CR and an overall response rate of 60 % and the drug was administered safely overall in an outpatient setting with infection being the most common toxicity noted in eight patients (Sudan et al. 2006). A larger study of 82 AML patients treated with azacytidine (as first therapy (n = 35) or salvage (n = 47) was analyzed by Maurillo et al. (2012). In this study, investigators found a median age of 72 years with a third of the patients having secondary AML. The analysis demonstrated an overall response rate of 32 % with 12 CRs, 4 CRi, and 10 PR, with greater occurrence of these responses occurring in the frontline treatment group. Based on these promising results, the authors suggested that single-agent azacytidine could be a treatment approach for older AML patients. .
A multicenter phase I/II study was undertaken to further study this concept. Al-Ali et al. (2012) analyzed 40 older AML patients treated with azacytidine. The median age of the cohort was 72 years. The overall response rate was reported as 50 % in the frontline treated patients and 10 % in the relapsed/refractory group (p = 0.008), signaling the safety and feasibility of single-agent azacytidine in an older AML patient population, including newly diagnosed patients .
3.2.2 Phase III Clinical Trials, Single-Agent Azacytidine in AML
With the reclassification of blast percent in MDS and AML by the WHO from the FAB system, Fenaux et al. were interested to analyze the results from the AZA-001 trial with treatment for intermediate risk and high-risk MDS patients with azacytidine (Font 2011) . In their analysis, Fenaux et al. found that one third of the patients treated were, in fact, now classified as AML (i.e., those patients had 21–30 % blasts) (Fenaux et al. 2010). The analysis compared azacytidine -treated patients to those in the other arms of the trial (best supportive care, low-dose ARA-C, or intensive chemotherapy). The authors demonstrated that treatment with azacytidine resulted in overall survival benefit for low blast count AML compared with conventional care regimens (24.5 months vs. 16.0 months p = 0.005). Further evidence supporting this finding is from the previously reported Silverman et al. study which analyzed the results of a smaller number of AML patients (n = 27) that were treated in three CALGB [A-Za-z_-’&;]{3,20} (8421, 8921, 9221) and this study had also seen benefit with azacytidine therapy with median overall survival of 19.3 months. Taken together, the subgroup analysis of these large phase III trials that originally treated MDS patients and included low blast count AML as classified by WHO, leads to the promise of azacytidine as a therapy consideration for AML patients, especially older AML patients and those unfit for intensive chemotherapy .
3.3 Azacytidine in Stem Cell Transplant
The promise of the application of azacytidine in treatment of patients with AML has included its potential for use in the SCT setting . In one early study, Zittoun et al. (1989) utilized azacytidine as one part of a multidrug post-remission AML treatment plan (with or without addition of SCT). Among a large cohort of patients, 60 of these patients ultimately underwent SCT (43 were allogeneic SCT, 17 autologous). The authors concluded that further studies were needed to help determine the effectiveness of multidrug consolidation, and various types of SCTs should be further studied.
One key study in this field was performed by de Lima et al. in the maintenance setting post-SCT (Lima and Thall 2010). In this study, the authors tested the hypothesis and potential for hypomethylator therapy with azacytidine to help reduce the rate of relapse in AML patients undergoing allogeneic SCT. Among 45 AML patients analyzed and with median age of 60 years, investigators began treatment with azacytidine at D + 40 from SCT date for post-SCT maintenance schedule. They found that four cycles of azacytidine given days 1–5 on a 30-day cycle at dose 32 mg/m2 per cycle was the best dose schedule/combination out of several tested in a relapsed/refractory MDS/AML population, with possibility for this approach yielding improvements in overall and event-free survival, with further exploration of dosing/scheduling/duration (Lima and Thall 2010) .
Building on this concept, Platzbecker et al. also studied administration of azacytidine in the post-SCT setting but in this study, they focused their efforts on those patients exhibiting minimal residual disease positivity (MRD+) (Platzbecker et al. 2012). A goal of four cycles of azacytidine was to be given to 20 MDS/AML patients with MRD+ status while still in CR; 16 of these patients (80 %) had responses as defined by either a rising CD34+ donor chimerism to greater than or equal to 80 % or stabilization, with no evidence of overt relapse of the disease. Thirteen patients ultimately experienced hematologic relapse (65 %); the authors found this occurrence was delayed to a median of 231 days after the initial decrease of CD34+ donor chimerism to less than or equal to 80 % was originally noted, suggesting that the administration of azacytidine in the setting of complete remission but with MRD+ status was able to effectively help to delay the occurrence of overt relapse of the patients’ underlying MDS/AML and this approach could be safe and feasible in the MDS/AML population in the post-SCT setting. Future studies in SCT setting will aim to explore further the mechanism of action by which azacytidine elaborates its benefit, especially in the post-SCT setting; one such study in this regard hypothesized that azacytidine enhances the graft versus leukemia effect without actually increased graft versus host disease in AML patients post-SCT treated with azacytidine in the post-SCT setting (Goodyear et al. 2012) .
3.4 Combination Clinical Trials and Future Directions
3.4.1 Combination Therapies
A number of combination chemotherapy clinical trials have been undertaken including azacytidine in the treatment of AML patients. One of the earliest of these efforts was undertaken by Winton and the SWOG in 1985 in which investigators demonstrated the clinical activity of sequentially administered azacytidine with amsacrine in a relapsed/refractory group of 128 patients, suggesting that drug combinations with azacytidine might be promising (Winton et al. 1985). Other early and more recent studies continued to test the drug combination hypothesis in both post-induction strategies of azacytidine combined with other drugs (Volger et al. 1995; Rees et al. 1996), and in relapsed settings with various other chemotherapeutic agents including mitoxantrone (Goldberg et al. 1993) amsacrine and etoposide (Steuber et al. 1996), hydroxyurea and gemtuzumab (Nand et al. 2008), thalidomide (Raza et al. 2008), Ara-C (Borthakur et al. 2010) all suggesting a possible role for azacytidine in various AML treatment settings.
One key azacytidine-based combination to highlight is with combination of valproic acid, a histone deacetylase inhibitor. The pairing of these two agents has led to observation of synergistic activity both in vitro and in vivo (Braiteh et al. 2008). Braiteh et al. demonstrated the feasibility of this combination in phase I setting in various advanced malignancies. A phase I/II study by Soriano et al. (2007) aimed to assess the safety of the combination of azacytidine and valproic acid, with the addition of ATRA specifically in MDS/AML patients. In this trial, 53 patients were analyzed with median age of 69 years. There was neurotoxicity established as the dose limiting toxicity (DLT) and overall response rate was reported as 42 %, suggesting safety of the three drug combination and suggestion for further study. A phase 2 trial led by Raffoux et al. (2010) was then undertaken, further studying the three drug combination (azacytidine, valproic acid, ATRA). Out of 65 MDS/AML patients with median age of 72 years, 13 patients were relapsed/refractory. The investigators found 14 CRs and 3 PRs and median overall survival of 12.4 months. Another study assessing the combination of DNA hypomethylation and histone deacetylase inhibition was conducted by Kuendgen et al. (2011). In this trial, the authors tested only the combination of azacytidine and valproic acid, leaving off the ATRA that had been included in the previous two trials. Among 24 patients that received the combination therapy, 17 patients had AML. A total of 7 patients were found to have CR with another two patients in PR. The authors concluded that there was indeed clinical benefit to the two-drug combination and that prospective clinical trials would be warranted to further assess this therapeutic approach.
3.4.2 Future Directions
There are many exciting applications, concepts, and drug combinations in the area of azacytidine research for patients in AML. This section will highlight a few of these promising ongoing approaches.
Oral Azacytidine
In a pilot pharmacologic study, Garcia-Manero et al. evaluated a newly reformulated version of oral azacytidine (Garcia-Manero et al. 2008) . In this feasibility study, investigators demonstrated that the possibility of an oral version of this SQ/iv drug was indeed feasible and has adequate bioavailability in humans. This led Garcia-Manero et al. (2011) to conduct and report on a phase I clinical trial of oral azacytidine in treatment of MDS/AML. In this study, the authors evaluated the safety of this approach in 41 patients (AML, n = 8), who received one cycle of SQ administration followed by oral drug. Diarrhea was found to be most common grade 3 and 4 event. An overall response rate of 35 % was reported in relapsed/refractory patients and 73 % rate in frontline patients. The oral formulation was found to have adequate bioavailability and clinical activity in MDS/AML patients and further trials are being planned to study this novel approach .
Azacytidine in Combination with Lenalidomide
A phase I study was conducted to evaluate the safety of a novel sequential therapy in treatment of AML patients with azacytidine and lenalidomide in older AML patients (Pollyea et al. 2012) . The approach was executed as sequential treatment in a cohort of 18 older, untreated AML patients. Results showed no maximum tolerated dose being reached and rate of CR/CRi to be 7/16 patients (44 %) with median response duration of 6.2 months. These promising data have led multiple groups to further explore this therapy combination in both MDS and AML patients including Garcia-Manero et al. (2011) as presented at ASH 2011.
Azacytidine combination with FLT3 Inhibitor
Yet another approach in treatment of AML is the combination of a hypomethylator agent with an inhibitor of the FLT3 inhibitor. FLT3, or FMS-like 3, is mutated in approximately 30% AML patients (Pemmaraju et al. 2011) and in the setting of potential therapeutic targeting, Sato et al. have shown that traditional cytotoxic chemotherapy might lead to FLT3 ligand levels actually being increased and thus leading to FLT3 resistance (Sato et al. 2011) . It is precisely in this setting that novel approaches involving azacytidine combined with a FLT3 inhibitor have been undertaken. One such study, an ongoing phase II clinical trial reported by Alattar et al. (ASCO 2012 Abstract 6558) evaluated the combination of azacytidine with sorafenib (an FDA-approved drug for treatment of advanced renal cell cancer and hepatocellular cancer, which is a multi-kinase inhibitor with targets including FLT3) has enrolled 32 patients (median age 61 years) with relapsed/refractory AML. FLT3-ITD mutation was positive in 30/32 patients. The reported CR/CRi is 50 % with median duration of the CR/CRi lasting 3 months and three patients ultimately going onto SCT. In another phase I/II study, Nazha et al. (ASCO 2012 Abstract 6589) studied another FLT3 inhibitor, PKC-412, in combination with azacytidine. In this study, investigators enrolled 14 patients thus far, with overall response rate reported as 3/13 (21 %), including two CRi. One out of four patients with FLT3-ITD was able to demonstrate a CRi. The authors of both studies concluded that the safety and efficacy of the combination of azacytidine with a FLT3 inhibitor appeared to be promising and the further, larger prospective trials would be useful to continue to study this approach .
4 Conclusion
Outcomes in AML, especially older patients, remain overall poor. The backbone of traditional cytotoxic therapy, generally consisting of an anthracycline combined with Ara-C, is not able to be utilized in a large amount of AML patients due to age, co-morbidities, and toxicity profile, and novel therapies are warranted in treatment of these patients. Epigenetic therapy , including hypomethylating agents (decitabine, azacytidine) and investigational agents in this field represent an exciting new era in treatment of AML patients and offers patients opportunity for treatment with potentially less toxic alternatives to traditional cytotoxic therapy. Future work in this field will include better delineation of biomarkers for prediction of response of these agents and further studies utilizing these agents in combination with other chemotherapeutic therapies.
References
Al-Ali HK, Jaekel N, Junghanss C et al (2012) Azacitidine in patients with acute myeloid leukemia medically unfit for or resistant to chemotherapy: a multicenter phase I/II study. Leuk Lymphoma 53:110–117
Baylin SB, Fearon ER, Vogelstein B et al (1987) Hypermethylation of the 5′ region of the calcitonin gene is a property of human lymphoid and acute myeloid malignancies. Blood 70:412–417
Blum W, Klisovic RB, Hackanson B et al (2007) Phase I study of decitabine alone or in combination with valproic acid in acute myeloid leukemia. J Clin Oncol 25:3884–3891
Blum W, Garzon R, Klisovic RB et al (2010) Clinical response and miR-29b predictive significance in older AML patients treated with a 10-day schedule of decitabine. Proc Natl Acad Sci U S A 107:7473–7478
Blum W, Schwind S, Tarighat SS et al (2012) Clinical and pharmacodynamic activity of bortezomib and decitabine in acute myeloid leukemia. Blood 119:6025–6031
Borthakur G, Huang X, Kantarjian H et al (2010) Report of a phase 1/2 study of a combination of azacitidine and cytarabine in acute myelogenous leukemia and high-risk myelodysplastic syndromes. Leuk Lymphoma 51:73–78
Boumber Y, Kantarjian H, Jorgensen J et al (Jun 5 2012) A randomized study of decitabine versus conventional care for maintenance therapy in patients with acute myeloid leukemia in complete remission. Leukemia 26(11):2428–2431
Braiteh F, Soriano AO, Garcia-Manero G et al (2008) Phase I study of epigenetic modulation with 5-azacytidine and valproic acid in patients with advanced cancers. Clin Cancer Res 14:6296–6301
Bryan J, Kantarjian H, Garcia-Manero G, Jabbour E (2011) Pharmacokinetic evaluation of decitabine for the treatment of leukemia. Expert Opin Drug Metab Toxicol 7:661–672
Bullinger L, Ehrich M, Dohner K et al (2010) Quantitative DNA methylation predicts survival in adult acute myeloid leukemia. Blood 115:636–642
Cashen AF, Shah AK, Todt L, Fisher N, DiPersio J (2008) Pharmacokinetics of decitabine administered as a 3-h infusion to patients with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS). Cancer Chemother Pharmacol 61:759–766
Cashen AF, Schiller GJ, O’Donnell MR, DiPersio JF (2010) Multicenter, phase II study of decitabine for the first-line treatment of older patients with acute myeloid leukemia. J Clin Oncol 28:556–561
Chowdhury S, Seropian S, Marks PW (2009) Decitabine combined with fractionated gemtuzumab ozogamicin therapy in patients with relapsed or refractory acute myeloid leukemia. Am J Hematol 84:599–600
de Lima M, Ravandi, Shahjahan M et al (2003) Long-term follow-up of a phase I study of high-dose decitabine, busulfan, and cyclophosphamide plus allogeneic transplantation for the treatment of patients with leukemias. Cancer 97:1242–1247
de Lima M, Giralt, Thall PF et al (2010) Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer 116:5420–5431
Faderl S, Ravandi F, Huang X et al (26 Jan 2012) Clofarabine plus low-dose cytarabine followed by clofarabine plus low-dose cytarabine alternating with decitabine in acute myeloid leukemia frontline therapy for older patients. Cancer 118(18):4471–4477
Fenaux P, Mufti GJ, Hellstrom-Lindberg E et al (2009) Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 10:223–232
Fenaux P, Mufti GJ, Hellstrom-Lindberg E et al (2010) Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J Clin Oncol 28:562–569
Figueroa ME, Lugthart S, Li Y et al (2010) DNA methylation signatures identify biologically distinct subtypes in acute myeloid leukemia. Cancer Cell 17:13–27
Flotho C, Claus R, Batz C et al (2009) The DNA methyltransferase inhibitors azacitidine, decitabine and zebularine exert differential effects on cancer gene expression in acute myeloid leukemia cells. Leukemia 23:1019–1028
Font P (2011) Azacitidine for the treatment of patients with acute myeloid leukemia with 20%–30% blasts and multilineage dysplasia. Adv Ther 28(3):1–9
Galm O, Wilop S, Luders C et al (2005) Clinical implications of aberrant DNA methylation patterns in acute myelogenous leukemia. Ann Hematol 84(1):39–46
Garcia-Manero G (2011) Treatment of higher-risk myelodysplastic syndrome. Semin Oncol 38:673–681
Garcia-Manero G, Kantarjian HM, Sanchez-Gonzalez B et al (2006) Phase 1/2 study of the combination of 5-aza-2′-deoxycytidine with valproic acid in patients with leukemia. Blood 108:3271–3279
Garcia-Manero G, Stoltz ML, Ward MR, Kantarjian H, Sharma S (2008) A pilot pharmacokinetic study of oral azacitidine. Leukemia 22:1680–1684
Garcia-Manero G, Daver NG, Borthakur G et al (2011) Phase I Study of the Combination of 5-Azacitidine Sequentially with High-Dose Lenalidomide in Higher-Risk Myelodysplastic Syndrome (MDS) and Acute Myelogenous Leukemia (AML). ASH Annual Meeting Abstracts 118:2613 December 10–13, 2001
Garcia-Manero G, Gore SD, Cogle C et al. (2011) Phase I study of oral azacitidine in myelodysplastic syndromes, chronic myelomonocytic leukemia, and acute myeloid leukemia. J Clin Oncol 29:2521–2527
Gattei V, Aldinucci D, Petti MC, Da Ponte A, Zagonel V, Pinto A (1993) In vitro and in vivo effects of 5-aza-2′-deoxycytidine (Decitabine) on clonogenic cells from acute myeloid leukemia patients. Leukemia 7(1):42–48
Giralt S, Davis M, O’Brien S et al (1997) Studies of decitabine with allogeneic progenitor cell transplantation. Leukemia 11(1):S32–34
Goldberg J, Gryn J, Raza A et al (1993) Mitoxantrone and 5-azacytidine for refractory/relapsed ANLL or CML in blast crisis: a leukemia intergroup study. Am J Hematol 43:286–290
Goodyear OC, Dennis M, Jilani NY et al (2012) Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood 119:3361–3369
Hrodek O, Vesely J (1971) 5-azacytidine in childhood leukemia. Neoplasma 18:493–503
Issa JP, Kantarjian HM (2009) Targeting DNA methylation. Clin Cancer Res 15:3938–3946
Issa JP, Garcia-Manero G, Giles FJ et al (2004) Phase 1 study of low-dose prolonged exposure schedules of the hypomethylating agent 5-aza-2′-deoxycytidine (decitabine) in hematopoietic malignancies. Blood 103:1635–1640
Jain N, Rossi A, Garcia-Manero G (2009) Epigenetic therapy of leukemia: An update. Int J Biochem Cell Biol 41:72–80
Jones PA, Baylin SB (2007) The epigenomics of cancer. Cell 128:683–692
Kantarjian HM, Estey EH, Keating MA (1996) New chemotherapeutic agents in acute myeloid leukemia. Leukemia 10(1):S4–6
Kantarjian H, Issa JP, Rosenfeld CS et al (2006) Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer 106:1794–1803
Kantarjian HM, Thomas XG, Dmoszynska A et al (2012) Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol 30:2670–2677
Karon M, Sieger L, Leimbrock S, Finklestein JZ, Nesbit ME, Swaney JJ (1973) 5-Azacytidine: a new active agent for the treatment of acute leukemia. Blood 42:359–365
Keating GM (2012) Azacitidine: a review of its use in the management of myelodysplastic syndromes/acute myeloid leukaemia. Drugs 72:1111–1136
Kuendgen A, Bug G, Ottmann OG et al (2011) Treatment of poor-risk myelodysplastic syndromes and acute myeloid leukemia with a combination of 5-azacytidine and valproic acid. Clin Epigenetics 2:389–399
Lubbert M, Minden M (2005) Decitabine in acute myeloid leukemia. Semin Hematol 42:S38–42
Lubbert M, Bertz H, Ruter B et al (2009) Non-intensive treatment with low-dose 5-aza-2′-deoxycytidine (DAC) prior to allogeneic blood SCT of older MDS/AML patients. Bone Marrow Transplant 44:585–588
Lubbert M, Suciu S, Baila L et al (2011) Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol 29:1987–1996
Lubbert M, Ruter BH, Claus R et al (2012) A multicenter phase II trial of decitabine as first-line treatment for older patients with acute myeloid leukemia judged unfit for induction chemotherapy. Haematologica 97:393–401
Maurillo L, Venditti A, Spagnoli A et al (2012) Azacitidine for the treatment of patients with acute myeloid leukemia: report of 82 patients enrolled in an Italian Compassionate Program. Cancer 118:1014–1022
McCredie KB, Bodey GP, Burgess MA et al (1973) Treatment of acute leukemia with 5-azacytidine (NSC-102816). Cancer Chemother Rep 57:319–323
McDevitt MA (2012) Clinical applications of epigenetic markers and epigenetic profiling in myeloid malignancies. Semin Oncol 39:109–122
Momparler RL, Bouchard J, Onetto N, Rivard GE (1984) 5-aza-2′-deoxycytidine therapy in patients with acute leukemia inhibits DNA methylation. Leuk Res 8:181–185
Momparler RL, Rivard GE, Gyger M (1985) Clinical trial on 5-aza-2′-deoxycytidine in patients with acute leukemia. Pharmacol Ther 30:277–286
Nand S, Godwin J, Smith S et al (2008) Hydroxyurea, azacitidine and gemtuzumab ozogamicin therapy in patients with previously untreated non-M3 acute myeloid leukemia and high-risk myelodysplastic syndromes in the elderly: results from a pilot trial. Leuk Lymphoma 49:2141–2147
Pemmaraju N, Kantarjian H, Ravandi F, Cortes J (2011) FLT3 inhibitors in the treatment of acute myeloid leukemia: the start of an era? Cancer 117:3293–3304
Petti MC, Mandelli F, Zagonel V et al (1993) Pilot study of 5-aza-2′-deoxycytidine (Decitabine) in the treatment of poor prognosis acute myelogenous leukemia patients: preliminary results. Leukemia 7(1):36–41
Pinto A, Zagonel V, Attadia V et al (1989) 5-Aza-2′-deoxycytidine as a differentiation inducer in acute myeloid leukaemias and myelodysplastic syndromes of the elderly. Bone Marrow Transplant 4(3):28–32
Platzbecker U, Wermke M, Radke J et al (2012) Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: results of the RELAZA trial. Leukemia 26:381–389
Pollyea DA, Kohrt HE, Gallegos L et al (2012) Safety, efficacy and biological predictors of response to sequential azacitidine and lenalidomide for elderly patients with acute myeloid leukemia. Leukemia 26:893–901
Raffoux E, Cras A, Recher C et al (2010) Phase 2 clinical trial of 5-azacitidine, valproic acid, and all-trans retinoic acid in patients with high-risk acute myeloid leukemia or myelodysplastic syndrome. Oncotarget 1:34–42
Ravandi F, Kantarjian H, Cohen A et al (2001) Decitabine with allogeneic peripheral blood stem cell transplantation in the therapy of leukemia relapse following a prior transplant: results of a phase I study. Bone Marrow Transplant 27:1221–1225
Ravandi F, Issa JP, Garcia-Manero G et al (2009) Superior outcome with hypomethylating therapy in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome and chromosome 5 and 7 abnormalities. Cancer 115:5746–5751
Raza A, Mehdi M, Mumtaz M, Ali F, Lascher S, Galili N (2008) Combination of 5-azacytidine and thalidomide for the treatment of myelodysplastic syndromes and acute myeloid leukemia. Cancer 113:1596–1604
Rees JK, Gray RG, Wheatley K (1996) Dose intensification in acute myeloid leukaemia: greater effectiveness at lower cost. Principal report of the Medical Research Council’s AML9 study. MRC Leukaemia in Adults Working Party. Br J Haematol 94:89–98
Richel DJ, Colly LP, Kluin-Nelemans JC, Willemze R (1991) The antileukaemic activity of 5-Aza-2 deoxycytidine (Aza-dC) in patients with relapsed and resistant leukaemia. Br J Cancer 64:144–148
Rivard GE, Momparler RL, Demers J et al (1981) Phase I study on 5-aza-2′-deoxycytidine in children with acute leukemia. Leuk Res 5:453–462
Saiki JH, McCredie KB, Vietti TJ et al (1978) 5-azacytidine in acute leukemia. Cancer 42:2111–2114
Saiki JH, Bodey GP, Hewlett JS et al (1981) Effect of schedule on activity and toxicity of 5-azacytidine in acute leukemia: a Southwest Oncology Group Study. Cancer 47:1739–1742
Santini V, Kantarjian HM, Issa JP (2001) Changes in DNA methylation in neoplasia: pathophysiology and therapeutic implications. Ann Intern Med 134:573–586
Sato T, Yang X, Knapper S et al (2011) FLT3 ligand impedes the efficacy of FLT3 inhibitors in vitro and in vivo. Blood 117:3286–3293
Scandura JM, Roboz GJ, Moh M et al (2011) Phase 1 study of epigenetic priming with decitabine prior to standard induction chemotherapy for patients with AML. Blood 118:1472–1480
Schmelz K, Sattler N, Wagner M, Lubbert M, Dorken B, Tamm I (2005) Induction of gene expression by 5-Aza-2′-deoxycytidine in acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) but not epithelial cells by DNA-methylation-dependent and -independent mechanisms. Leukemia 19:103–111
Schoofs T, Muller-Tidow C (2011) DNA methylation as a pathogenic event and as a therapeutic target in AML. Cancer Treat Rev 37(1):13–18
Schwartsmann G, Fernandes MS, Schaan MD et al (1997) Decitabine (5-Aza-2′-deoxycytidine; DAC) plus daunorubicin as a first line treatment in patients with acute myeloid leukemia: preliminary observations. Leukemia 11(1):S28–31
Silverman LR, Demakos EP, Peterson BL et al (2002) Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol 20:2429–2440
Soriano AO, Yang H, Faderl S et al (2007) Safety and clinical activity of the combination of 5-azacytidine, valproic acid, and all-trans retinoic acid in acute myeloid leukemia and myelodysplastic syndrome. Blood 110:2302–2308
Steuber CP, Krischer J, Holbrook T et al (1996) Therapy of refractory or recurrent childhood acute myeloid leukemia using amsacrine and etoposide with or without azacitidine: a Pediatric Oncology Group randomized phase II study. J Clin Oncol 14:1521–1525
Sudan N, Rossetti JM, Shadduck RK et al (2006) Treatment of acute myelogenous leukemia with outpatient azacitidine. Cancer 107:1839–1843
Tamm I, Wagner M, Schmelz K (2005) Decitabine activates specific caspases downstream of p73 in myeloid leukemia. Ann Hematol 84(1):47–53
Toyota M, Kopecky KJ, Toyota MO, Jair KW, Willman CL, Issa JP (2001) Methylation profiling in acute myeloid leukemia. Blood 97:2823–2829
Valk PJ, Verhaak RG, Beijen MA et al (2004) Prognostically useful gene-expression profiles in acute myeloid leukemia. N Engl J Med 350:1617–1628
Vogler WR, Miller DS, Keller JW (1976) 5-Azacytidine (NSC 102816): a new drug for the treatment of myeloblastic leukemia. Blood 48:331–7
Volger WR, Weiner RS, Moore JO, Omura GA, Bartolucci AA, Stagg M (1995) Long-term follow-up of a randomized post-induction therapy trial in acute myelogenous leukemia (a Southeastern Cancer Study Group trial). Leukemia 9:1456–1460
Von Hoff DD, Slavik M, Muggia FM (1976) 5-Azacytidine. A new anticancer drug with effectiveness in acute myelogenous leukemia. Ann Intern Med 85:237–245
Willemze R, Archimbaud E, Muus P (1993) Preliminary results with 5-aza-2′-deoxycytidine (DAC)-containing chemotherapy in patients with relapsed or refractory acute leukemia. The EORTC Leukemia Cooperative Group. Leukemia 7(1):49–50
Willemze R, Suciu S, Archimbaud E et al (1997) A randomized phase II study on the effects of 5-Aza-2′-deoxycytidine combined with either amsacrine or idarubicin in patients with relapsed acute leukemia: an EORTC Leukemia Cooperative Group phase II study (06893). Leukemia 11(1):S24–27
Winton EF, Hearn EB, Martelo O et al (1985) Sequentially administered 5-azacitidine and amsacrine in refractory adult acute leukemia: a phase I-II trial of the Southeastern Cancer Study Group. Cancer Treat Rep 69:807–811
Zittoun R, Jehn U, Fiere D et al (1989) Alternating v repeated postremission treatment in adult acute myelogenous leukemia: a randomized phase III study (AML6) of the EORTC Leukemia Cooperative Group. Blood 73:896–906
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag New York
About this chapter
Cite this chapter
Pemmaraju, N., Garcia-Manero, G., Ravandi, F. (2015). Methylation in AML: Clinical Applications. In: Andreeff, M. (eds) Targeted Therapy of Acute Myeloid Leukemia. Current Cancer Research. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1393-0_22
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1393-0_22
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1392-3
Online ISBN: 978-1-4939-1393-0
eBook Packages: MedicineMedicine (R0)