Abstract
Hypermethylation of CpG islands near gene promoter regions is associated with transcriptional inactivation and represents an important mechanism of gene silencing in carcinogenesis. Such epigenetic phenomena can act alongside DNA mutations and deletions to disrupt tumor-suppressor gene function. The methylation status of the promoter-associated CpG islands from 11 well-characterized cancer-related genes was analyzed by methylation-specific polymerase chain reaction in 60 adult patients with acute myelogenous leukemia (AML) at diagnosis. The frequency of aberrant methylation among the patient samples was 45.0% (27/60) for suppressor of cytokine signaling-1, 31.7% (19/60) for p15, 20.0% (12/60) for retinoic acid receptor β2, 13.3% (8/60) for p73 and E-cadherin, 5.0% (3/60) for O6-methylguanine DNA methyltransferase, 3.3% (2/60) for death-associated protein kinase 1 and hMLH1, 1.7% (1/60) for p16, and 0% (0/60) for the tissue inhibitor of matrix metalloproteinases-3 and Ras association domain family 1A. Aberrant DNA methylation was found in AML of all French–American–British subtypes and throughout all cytogenetic risk groups. There appeared to be a trend towards a higher methylation frequency in AML patients with an unfavorable karyotype, but this difference was not statistically significant. Our data indicate that hypermethylation of multiple genes involving fundamental cellular pathways is a common event in AML, which varies greatly in frequency among the genes examined. The accumulation of epigenetic events affecting genes which are involved in regulating cell cycle inhibition, cell adhesion, growth factor signaling, and apoptosis may contribute to the malignant AML phenotype. The growing knowledge of the role of epigenetics in the aberrant silencing of cancer-related genes provides a rationale and molecular basis for targeted therapeutic approaches with demethylating agents in AML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myelogenous leukemia (AML) is a heterogeneous disease characterized by many different genetic defects. These aberrations include chromosomal translocations involving oncogenes and transcription factors, activation of signal transduction pathways, and alterations of growth factor receptors [4, 38]. Cytogenetic abnormalities are present in leukemic cells in the majority of AML patients and have been used to identify subgroups of AML with specific clinical behavior. The karyotype of the leukemic blasts has emerged as an important prognostic factor in AML [22].
In addition to genetic changes, epigenetic processes play a major role in carcinogenesis [30]. Aberrant methylation of CpG islands near gene promoter regions together with deacetylation and other modifications of histones are the most widely studied epigenetic abnormalities in human malignancies and are now established as important mechanisms for gene inactivation [14, 26, 31]. Protein complexes of methyl-CpG-binding proteins, transcriptional corepressors, chromatin-remodeling proteins, and histone deacetylases (HDACs) bind to hypermethylated DNA regions, resulting in a transcriptionally repressive chromatin state [11, 46]. As proposed in the two-hit hypothesis of Knudson [34], the disruption of the function of a tumor-suppressor gene generally requires a complete loss of function of both gene copies. In this context, abnormal methylation of CpG islands may exert the same effects as a mutation or deletion in the coding region in one copy of the gene and thus represents an alternative mechanism to contribute to the loss of function of one or both alleles [11, 26]. Genes involving fundamental cellular pathways have been shown to be affected by aberrant CpG island methylation in human cancer [13, 26].
There is now increasing evidence for the relevance of hypermethylation-associated gene silencing in the pathogenesis of myelodysplastic syndromes (MDS), AML, and other hematopoietic malignancies [7, 15, 16, 27, 43–45]. A growing number of genes that may become inactivated due to aberrant hypermethylation in cancer have been identified. This provides new insight into the biology of AML and may offer novel therapeutic opportunities [18, 28, 36]. Numerous in vitro experiments have shown that, in contrast to genetic aberrations, the hypermethylation-associated silencing of tumor-suppressor genes is a reversible phenomenon [1, 5, 42]. The therapeutic efficacy of the demethylating agents 5-aza-2′-deoxycytidine (decitabine) and 5-azacytidine (azacitidine, Vidaza) has been demonstrated in clinical trials in patients with MDS, AML, and chronic myelogenous leukemia [29, 32, 47, 50, 51].
In this study, we examined the methylation status of 11 well-characterized cancer-related genes in samples of 60 adult patients with AML at diagnosis and explored possible correlations between methylation patterns and clinical parameters. Methylation was analyzed using the methylation-specific polymerase chain reaction (MSP) technique [24]. This assay entails the initial modification of genomic DNA by sodium bisulfite, converting all unmethylated cytosines to uracils but leaving the methylated cytosines unchanged. Subsequently, the DNA region of interest is amplified in two separate polymerase chain reactions (PCRs) with primer pairs specific to either the methylated or the unmethylated sequence. The list of candidate genes comprises the cell cycle regulators p15, p16, and p73, the tissue inhibitor of matrix metalloproteinases-3 (TIMP-3), E-cadherin, the DNA repair genes O6-methylguanine DNA methyltransferase (MGMT) and hMLH1, retinoic acid receptor β2 (RARβ2), death-associated protein kinase 1 (DAPK), Ras association domain family 1A (RASSF1A), and the cytokine regulator suppressor of cytokine signaling-1 (SOCS-1). It has been shown previously that the expression of each of these genes may be affected by aberrant CpG island methylation in association with transcriptional silencing in various human malignancies [1, 3, 6, 8, 12, 20, 25, 33, 41, 49, 52].
Materials and methods
Human tissue samples
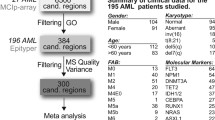
After informed consent was obtained, bone marrow (BM) and peripheral blood (PB) specimens (32 BM and 28 PB) were collected at diagnosis during routine clinical assessment of 60 adult patients with AML that presented at the University Hospital Aachen, Germany, between 1995 and 2004. AML diagnosis was made in accordance with revised French–American–British (FAB) classification criteria [2]. Cytogenetic data were also available in 53/60 patients. The main clinical and laboratory features of the patient cohort are summarized in Table 1. PB samples from healthy volunteers were used as controls. Mononuclear cells from BM and PB were separated by density gradient centrifugation prior to analysis.
Methylation-specific polymerase chain reaction
The methylation status of the 11 candidate genes was analyzed by MSP [24]. Genomic DNA was isolated using a commercially available kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. Approximately 1 μg of DNA was sodium-bisulfite-modified and subjected to MSP as described previously [24]. A detailed list of MSP primers that specifically recognize either unmethylated (U) or methylated (M) gene sequences is given in Table 2. Reactions were hot-started at 95°C for 5 min and held at 80°C before addition of 0.625 U of Taq polymerase (Sigma, Munich, Germany). PCR conditions for all genes except TIMP-3 were as follows: 35 cycles of 95°C for 30 s, 60°C for 30 s, and 72°C for 30 s, followed by 1 cycle of 72°C for 5 min. For TIMP-3 analysis, conditions were 35 cycles of 95°C for 30 s, 59°C for 30 s, and 72°C for 30 s, followed by 1 cycle of 72°C for 5 min. PCR products were separated on 2.5% agarose gels and visualized by ethidium bromide staining.
Statistical methods
Correlations between variables were analyzed using the Fisher's exact two-sided test and the two-tailed Mann–Whitney test. Overall Kaplan–Meier survival curves were compared using the log-rank test. Survival was calculated from the date of diagnosis until the patients' death or last visit. All calculations were performed using the SAS statistical software (Version 9.1, SAS Institute, Cary, NC, USA).
Results
Methylation patterns in acute myelogenous leukemia
Representative MSP results are shown in Fig. 1. The frequency of hypermethylated genes among the AML patient samples was 45.0% (27/60) for SOCS-1, 31.7% (19/60) for p15, 20.0% (12/60) for RARβ2, 13.3% (8/60) for p73 and E-cadherin, 5.0% (3/60) for MGMT, 3.3% (2/60) for DAPK and hMLH1, 1.7% (1/60) for p16, and 0% (0/60) for TIMP-3 and RASSF1A (Fig. 2a). We have previously demonstrated that none of these 11 cancer-related genes showed aberrant CpG island hypermethylation in 20 nonmalignant BM samples [17]. An overview of the methylation status of the 60 AML samples is given in Table 3. The majority of the AML patients exhibited aberrant CpG island methylation. At least one hypermethylated gene promoter region was found in 70.0% (42/60) of the primary patient samples, while 41.7% (25/60) harbored two or more hypermethylated genes (Fig. 2b).
Representative MSP analysis of AML patient samples. Lanes U: amplified products with primers recognizing the unmethylated gene sequence. Lanes M: amplified products with primers recognizing the methylated gene sequence. Peripheral blood (PB) from healthy volunteers, in vitro methylated DNA (IVD), and water served as controls for each MSP reaction
Correlation of methylation data with clinical parameters
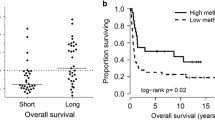
Possible correlations between methylation patterns and clinical and laboratory parameters were investigated in all 60 AML patients. Aberrant methylation occurred in all AML FAB subtypes (Table 3). No correlation could be found between methylation status and overall survival for any of the 11 CpG islands analyzed and no association with white blood cell counts (WBC) or serum lactate dehydrogenase (LDH) levels. Furthermore, there was no correlation between patient age and the number of hypermethylated genes (Fig. 3a). There was no association of the number of hypermethylated genes with overall survival.
a Correlation between age and aberrant CpG island methylation. For each individual patient, the age at diagnosis is plotted vs. the number of hypermethylated genes. b Average number of hypermethylated genes in AML patients according to cytogenetic risk group (error bars indicate standard error of the mean)
Seventeen of the 60 patients (28.3%) had a history of MDS or other antecedent hematologic disorders at diagnosis of AML. The average number of hypermethylated genes in these 17 samples did not differ significantly from the other (i.e., de novo) AML patients (1.41 vs. 1.34 genes).
Associations between aberrant methylation and cytogenetic data
Cytogenetic data were available from 53/60 (88.3%) AML patients. Risk stratification was performed according to cytogenetically defined prognostic groups [22]. The favorable cytogenetic risk group (n=13) included two cases with chromosomal translocation t(8;21), three patients with t(15;17), and eight patients with inversion inv(16). The intermediate risk group included 32 patients, and the adverse risk group was comprised of five patients with monosomy 7, two patients with deletion del(5q), and one patient with a complex karyotype. Aberrant CpG island methylation in AML was a common event throughout all cytogenetic risk groups. There appeared to be a trend towards a higher methylation frequency in AML patients with an adverse karyotype (Fig. 3b). However, this difference was not statistically significant and thus may possibly be related to the limited number of patients.
Discussion
In the present study, the methylation status of 11 candidate genes in a cohort of 60 adult AML patients was examined at diagnosis. Our data confirm that a variety of genes regulating fundamental cellular pathways may be simultaneously affected by hypermethylation in AML. Aberrant CpG island methylation of multiple cancer-related genes appears to be a common event in adult AML occurring in all FAB subtypes and throughout all cytogenetic risk groups.
There have been several previous reports describing DNA hypermethylation in AML. Melki et al. [40] determined the methylation status of eight CpG-rich candidate genes in 20 AML patients by bisulfite sequencing. Aberrant methylation was detected in 19/20 samples, while 15/20 samples carried two or more hypermethylated genes. However, in this small patient cohort, association with clinical parameters was not analyzed. Another study investigated the methylation status of 14 promoter-associated CpG islands in 36 AML patients using bisulfite PCR [48]. In that study, an inverse correlation was seen between patient age and frequency of CpG island methylation in AML. However, this was based on a group of patients with a comparatively young age (median 39 years), which may not be representative of the general AML population.
In our larger patient cohort, with a median age of 60 years, 70% had at least one methylated gene at diagnosis. Our results thus provide further evidence of the important role of epigenetic changes in leukemogenesis. The distribution of genes affected by aberrant methylation in AML differs from solid tumors and other hematopoietic malignancies [13, 17, 45], with SOCS-1, p15, RARβ2, p73, and E-cadherin most frequently methylated in AML. Hypermethylation of MGMT, DAPK, hMLH1, and p16 were rare events, and there was no methylation of TIMP-3 and RASSF1A. While these genes are not frequently methylated in AML, they have been found to be commonly methylated in other forms of malignancy [13].
Epigenetic aberrations affecting these genes regulating cell cycle inhibition, cell adhesion, growth factor signaling, and regulation of apoptosis may, in addition to genetic alterations [19, 38], contribute to the multistep process of cellular transformation in leukemogenesis.
Understanding the impact of gene hypermethylation on the pathogenesis of AML may not only lead to the development of novel biomarkers [35] but also help to determine candidate patients for epigenetically targeted therapies [18, 28, 36]. The demethylating agents decitabine and azacitidine act primarily through inhibition of DNA methyltransferases (DNMTs), enzymes that are responsible for establishing and maintaining DNA methylation patterns [39]. Clinical trials using DNA methylation inhibitors have recently yielded promising results in MDS patients [47, 50].
The first study to show that the clinical history of MDS may be altered using a nonintensive drug treatment resulting in improved quality of life was reported by Silverman et al. [47]. A randomized controlled phase III trial compared the subcutaneous application of azacitidine vs best supportive care, resulting in significant prolongation of median survival and a delay of time to leukemic transformation in the azacitidine arm.
A pivotal phase II trial [50] of low-dose intravenous decitabine resulted in an overall response rate of 49% in MDS patients and a response rate of 64% in the high-risk subgroup stratified according to the International Prognostic Scoring System [21]. Hypermethylation of the cell cycle inhibitor p15 was shown to be reversed in MDS patients who responded to treatment with decitabine, implicating pharmacologically induced demethylation as mechanism which may contribute to treatment response [9].
In the normal clinical course, MDS may eventually progress to AML [23]. It has been shown previously that methylation of the p15 gene in MDS is associated with a higher percentage of BM blasts. Furthermore, the frequency of aberrant p15 methylation increased with disease evolution towards AML [43]. In our patient cohort, methylation patterns in AML patients with evidence of preceding MDS or other antecedent hematologic disorders were similar to those of de novo AML patients, supporting the close biological relationship between advanced MDS and AML.
A trend towards a higher methylation frequency and therefore potentially higher degree of gene silencing was observed in AML patients with an adverse karyotype, indicating possible links between genetic and epigenetic aberrations in AML. Experimental evidence suggests that in AML subtypes carrying the translocations t(15;17) and t(8;21), the corresponding fusion proteins (PML/RARα and AML1/ETO) associate with HDACs and also recruit DNMTs, resulting in the transcriptional repression of target genes [10, 37]. Thus, there may be a mechanistic role of AML-associated fusion proteins in establishing specific DNA methylation patterns in AML. Furthermore, there is in vitro evidence for synergistic effects of pharmacologic demethylation and HDAC inhibition on reexpression of epigenetically silenced genes [5]. Based on these findings, therapeutic strategies that incorporate the combination of demethylating agents and HDAC inhibitors in the treatment of AML are being developed [18].
In summary, we have demonstrated that aberrant CpG island methylation affecting genes involved in fundamental cellular pathways is a common phenomenon in adult AML. There is now a growing list of candidate genes that may be used for monitoring the in vivo effects of DNA methylation inhibitors. This present study has focused on 11 well-characterized cancer-related genes, but there may be other genes that may undergo inactivation due to CpG island hypermethylation. Our results provide insight into the changes to the complex epigenetic status that occur during leukemogenesis and help to provide a molecular rationale for developing epigenetically targeted therapeutic approaches. To further explore possible links between genetic and epigenetic events in the evolution of AML, future studies are needed to examine a broad spectrum of methylation changes as well as genetic alterations in MDS and AML at diagnosis and during follow-up. Prospective analysis of a larger patient series is necessary to determine whether methylation patterns may be predictive of response to treatment with epigenetically targeted therapies. The discovery of novel molecular targets for demethylating agents is important for the development of future therapeutic strategies and tools to monitor the in vivo effects of those drugs.
References
Bachman KE, Herman JG, Corn PG, Merlo A, Costello JF, Cavenee WK, Baylin SB, Graff JR (1999) Methylation-associated silencing of the tissue inhibitor of metalloproteinase-3 gene suggest a suppressor role in kidney, brain, and other human cancers. Cancer Res 59:798–802
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C (1985) Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French–American–British cooperative group. Ann Intern Med 103:620–625
Burbee DG, Forgacs E, Zochbauer-Muller S, Shivakumar L, Fong K, Gao B, Randle D, Kondo M, Virmani A, Bader S, Sekido Y, Latif F, Milchgrub S, Toyooka S, Gazdar AF, Lerman MI, Zabarovsky E, White M, Minna JD (2001) Epigenetic inactivation of RASSF1A in lung and breast cancers and malignant phenotype suppression. J Natl Cancer Inst 93:691–699
Caligiuri MA, Strout MP, Gilliland DG (1997) Molecular biology of acute myeloid leukemia. Semin Oncol 24:32–44
Cameron EE, Bachman KE, Myohanen S, Herman JG, Baylin SB (1999) Synergy of demethylation and histone deacetylase inhibition in the re-expression of genes silenced in cancer. Nat Genet 21:103–107
Cameron EE, Baylin SB, Herman JG (1999) p15(INK4B) CpG island methylation in primary acute leukemia is heterogeneous and suggests density as a critical factor for transcriptional silencing. Blood 94:2445–2451
Claus R, Lubbert M (2003) Epigenetic targets in hematopoietic malignancies. Oncogene 22:6489–6496
Corn PG, Kuerbitz SJ, van Noesel MM, Esteller M, Compitello N, Baylin SB, Herman JG (1999) Transcriptional silencing of the p73 gene in acute lymphoblastic leukemia and Burkitt's lymphoma is associated with 5′ CpG island methylation. Cancer Res 59:3352–3356
Daskalakis M, Nguyen TT, Nguyen C, Guldberg P, Kohler G, Wijermans P, Jones PA, Lubbert M (2002) Demethylation of a hypermethylated P15/INK4B gene in patients with myelodysplastic syndrome by 5-Aza-2′-deoxycytidine (decitabine) treatment. Blood 100:2957–2964
Di Croce L, Raker VA, Corsaro M, Fazi F, Fanelli M, Faretta M, Fuks F, Lo Coco F, Kouzarides T, Nervi C, Minucci S, Pelicci PG (2002) Methyltransferase recruitment and DNA hypermethylation of target promoters by an oncogenic transcription factor. Science 295:1079–1082
Egger G, Liang G, Aparicio A, Jones PA (2004) Epigenetics in human disease and prospects for epigenetic therapy. Nature 429:457–463
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG (1999) Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59:793–797
Esteller M, Corn PG, Baylin SB, Herman JG (2001) A gene hypermethylation profile of human cancer. Cancer Res 61:3225–3229
Esteller M (2002) CpG island hypermethylation and tumor suppressor genes: a booming present, a brighter future. Oncogene 21:5427–5440
Esteller M (2003) Profiling aberrant DNA methylation in hematologic neoplasms: a view from the tip of the iceberg. Clin Immunol 109:80–88
Galm O, Esteller M (2004) Beyond genetics—the emerging role of epigenetic changes in hematopoietic malignancies. Int J Hematol 80:120–127
Galm O, Wilop S, Reichelt J, Jost E, Gehbauer G, Herman JG, Osieka R (2004) DNA methylation changes in multiple myeloma. Leukemia 18:1687–1692
Gilbert J, Gore SD, Herman JG, Carducci MA (2004) The clinical application of targeting cancer through histone acetylation and hypomethylation. Clin Cancer Res 10:4589–4596
Gilliland DG, Griffin JD (2002) The roles of FLT3 in hematopoiesis and leukemia. Blood 100:1532–1542
Graff JR, Herman JG, Lapidus RG, Chopra H, Xu R, Jarrard DF, Isaacs WB, Pitha PM, Davidson NE, Baylin SB (1995) E-cadherin expression is silenced by DNA hypermethylation in human breast and prostate carcinomas. Cancer Res 55:5195–5199
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, Ohyashiki K, Toyama K, Aul C, Mufti G, Bennett J (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89:2079–2088
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A (1998) The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood 92:2322–2333
Heaney ML, Golde DW (1999) Myelodysplasia. N Engl J Med 340:1649–1660
Herman JG, Graff JR, Myohanen S, Nelkin BD, Baylin SB (1996) Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci U S A 93:9821–9826
Herman JG, Umar A, Polyak K, Graff JR, Ahuja N, Issa JP, Markowitz S, Willson JK, Hamilton SR, Kinzler KW, Kane MF, Kolodner RD, Vogelstein B, Kunkel TA, Baylin SB (1998) Incidence and functional consequences of hMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci U S A 95:6870–6875
Herman JG, Baylin SB (2003) Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med 349:2042–2054
Issa JP, Baylin SB, Herman JG (1997) DNA methylation changes in hematologic malignancies: biologic and clinical implications. Leukemia 11(Suppl 1):S7–S11
Issa JP (2003) Decitabine. Curr Opin Oncol 15:446–451
Issa JP, Garcia-Manero G, Giles FJ, Mannari R, Thomas D, Faderl S, Bayar E, Lyons J, Rosenfeld CS, Cortes J, Kantarjian HM (2004) Phase 1 study of low-dose prolonged exposure schedules of the hypomethylating agent 5-aza-2′-deoxycytidine (decitabine) in hematopoietic malignancies. Blood 103:1635–1640
Jones PA, Laird PW (1999) Cancer epigenetics comes of age. Nat Genet 21:163–167
Jones PA, Baylin SB (2002) The fundamental role of epigenetic events in cancer. Nat Rev Genet 3:415–428
Kantarjian HM, O'Brien S, Cortes J, Giles FJ, Faderl S, Issa JP, Garcia-Manero G, Rios MB, Shan J, Andreeff M, Keating M, Talpaz M (2003) Results of decitabine (5-aza-2′deoxycytidine) therapy in 130 patients with chronic myelogenous leukemia. Cancer 98:522–528
Katzenellenbogen RA, Baylin SB, Herman JG (1999) Hypermethylation of the DAP-kinase CpG island is a common alteration in B-cell malignancies. Blood 93:4347–4353
Knudson AG (2001) Two genetic hits (more or less) to cancer. Nat Rev Cancer 1:157–162
Laird PW (2003) Early detection: the power and the promise of DNA methylation markers. Nat Rev Cancer 3:253–266
Leone G, Teofili L, Voso MT, Lubbert M (2002) DNA methylation and demethylating drugs in myelodysplastic syndromes and secondary leukemias. Haematologica 87:1324–1341
Liu S, Shen T, Rush LJ, Becknel B, Klisovic MI, Whitman SP, Vukosavljevic T, Byrd JC, Plass C, Marcucci G (2003) AML1/ETO associates with DNA methyltransferase I (DNMT1) in inducing transcriptional repression of the AML1-target gene interleukin-3 (IL-3). Blood 102:218a
Lowenberg B, Downing JR, Burnett A (1999) Acute myeloid leukemia. N Engl J Med 341:1051–1062
Lubbert M (2000) DNA methylation inhibitors in the treatment of leukemias, myelodysplastic syndromes and hemoglobinopathies: clinical results and possible mechanisms of action. Curr Top Microbiol Immunol 249:135–164
Melki JR, Vincent PC, Clark SJ (1999) Concurrent DNA hypermethylation of multiple genes in acute myeloid leukemia. Cancer Res 59:3730–3740
Merlo A, Herman JG, Mao L, Lee DJ, Gabrielson E, Burger PC, Baylin SB, Sidransky D (1995) 5′ CpG island methylation is associated with transcriptional silencing of the tumour suppressor p16/CDKN2/MTS1 in human cancers. Nat Med 1:686–692
Paz MF, Fraga MF, Avila S, Guo M, Pollan M, Herman JG, Esteller M (2003) A systematic profile of DNA methylation in human cancer cell lines. Cancer Res 63:1114–1121
Quesnel B, Guillerm G, Vereecque R, Wattel E, Preudhomme C, Bauters F, Vanrumbeke M, Fenaux P (1998) Methylation of the p15(INK4b) gene in myelodysplastic syndromes is frequent and acquired during disease progression. Blood 91:2985–2990
Roman-Gomez J, Jimenez-Velasco A, Castillejo JA, Agirre X, Barrios M, Navarro G, Molina FJ, Calasanz MJ, Prosper F, Heiniger A, Torres A (2004) Promoter hypermethylation of cancer-related genes: a strong independent prognostic factor in acute lymphoblastic leukemia. Blood 104:2492–2498
Rossi D, Capello D, Gloghini A, Franceschetti S, Paulli M, Bhatia K, Saglio G, Vitolo U, Pileri SA, Esteller M, Carbone A, Gaidano G (2004) Aberrant promoter methylation of multiple genes throughout the clinico-pathologic spectrum of B-cell neoplasia. Haematologica 89:154–164
Rountree MR, Bachman KE, Herman JG, Baylin SB (2001) DNA methylation, chromatin inheritance, and cancer. Oncogene 20:3156–3165
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, Stone RM, Nelson D, Powell BL, DeCastro CM, Ellerton J, Larson RA, Schiffer CA, Holland JF (2002) Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol 20:2429–2440
Toyota M, Kopecky KJ, Toyota MO, Jair KW, Willman CL, Issa JP (2001) Methylation profiling in acute myeloid leukemia. Blood 97:2823–2829
Virmani AK, Rathi A, Zochbauer-Muller S, Sacchi N, Fukuyama Y, Bryant D, Maitra A, Heda S, Fong KM, Thunnissen F, Minna JD, Gazdar AF (2000) Promoter methylation and silencing of the retinoic acid receptor-beta gene in lung carcinomas. J Natl Cancer Inst 92:1303–1307
Wijermans P, Lubbert M, Verhoef G, Bosly A, Ravoet C, Andre M, Ferrant A (2000) Low-dose 5-aza-2′-deoxycytidine, a DNA hypomethylating agent, for the treatment of high-risk myelodysplastic syndrome: a multicenter phase II study in elderly patients. J Clin Oncol 18:956–962
Willemze R, Suciu S, Archimbaud E, Muus P, Stryckmans P, Louwagie EA, Berneman Z, Tjean M, Wijermans P, Dohner H, Jehn U, Labar B, Jaksic B, Dardenne M, Zittoun R (1997) A randomized phase II study on the effects of 5-Aza-2′-deoxycytidine combined with either amsacrine or idarubicin in patients with relapsed acute leukemia: an EORTC Leukemia Cooperative Group phase II study (06893). Leukemia 11(Suppl 1):S24–S27
Yoshikawa H, Matsubara K, Qian GS, Jackson P, Groopman JD, Manning JE, Harris CC, Herman JG (2001) SOCS-1, a negative regulator of the JAK/STAT pathway, is silenced by methylation in human hepatocellular carcinoma and shows growth-suppression activity. Nat Genet 28:29–35
Acknowledgements
We would like to thank Sandra Mellen and Ingeborg Wiegand for expert technical assistance and Albert Esser for help with the statistical analysis. We also thank Dr. Michael Lübbert for critical reading of the manuscript and helpful discussion. This work was supported by a grant from the Rheinisch-Westfälische Technische Hochschule Aachen (START program). JGH is a paid consultant to and receives research support from OncoMethylome Sciences. The terms of this arrangement are being managed by the Johns Hopkins University in accordance with its conflict of interest policies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Galm, O., Wilop, S., Lüders, C. et al. Clinical implications of aberrant DNA methylation patterns in acute myelogenous leukemia. Ann Hematol 84 (Suppl 1), 39–46 (2005). https://doi.org/10.1007/s00277-005-0005-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-005-0005-0