Abstract
Disrupted information transfer and processing at gamma-aminobutyric acid (GABA) and glutamate synapses, especially in corticolimbic circuits, has been proposed as a critical component of the pathophysiology of mood disorders. Here we review evidence of the primary pathology from human postmortem brains, supported by imaging studies in living subjects, for alterations in pyramidal excitatory neurons, GABA inhibitory neurons, and supporting glia, including oligodendrocytes and astrocytes. The data suggest combinatorial changes in most investigated components, converge on putative functional changes at glutamate and GABA synapses, and indicate that a subset of GABA neurons, which express specific cellular markers (calbindin, somatostatin, neuropeptide Y) and target distal dendrites of pyramidal neurons, may be more selectively and robustly affected in major depression. Pathologies in this subset of GABA neurons display a continuum of changes across brain disorders, may significantly contribute to deregulated GABA-containing tripartite synapses providing dendritic inhibition, and have implications for corticolimbic information processing in major depression and other brain disorders sharing similar pathologies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
13.1 Introduction
Major depressive disorder , or major depression, is a common, devastating mood disorder characterized by low mood and a reduced ability to experience pleasure from previously enjoyable activities (anhedonia), which occurs in the presence of additional cognitive and physiological symptoms, such as loss of attention and concentration, recurrent thoughts of suicide, changes in weight, sleep patterns, and psychomotor retardation (American Psychiatric Association 2000). The costs at the individual and societal levels of this disorder are profound: the lifetime prevalence of major depression in the USA is approximately 17 % (Kessler et al. 2005) , and depression is currently considered the leading cause of years of healthy life lost due to disability, or “time spent in less than full health” among both men and women worldwide, as defined by the World Health Organization (WHO 2008). Women are disproportionately at risk, with twice as many women affected as men (Kessler et al. 2005). Despite this dire public health concern, current treatments have low efficacy, and only one out of two patients who meet criteria for major depression is expected to achieve remission (Huynh and McIntyre 2008; Kennedy and Giacobbe 2007) .
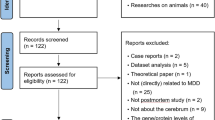
Recent neural models of emotion perception have implicated the amygdala, anterior cingulate cortex (ACC), and dorsal lateral prefrontal cortex (dlPFC) as core regions of a neural network of identification and regulation of emotion (Phillips et al. 2008) . Functional and morphological alterations have been reported in all three of these regions in mood disorders , and increased activation in the subgenual ACC (sgACC), an anatomical subdivision of the ACC, and amygdala are frequently reported in major depression (Mayberg et al. 1999; Siegle et al. 2007; Suslow et al. 2010) . Within this neural network, several lines of evidence, from human postmortem brains to molecular imaging studies in live subjects, suggest that the pathophysiology of major depression may involve altered gamma-aminobutyric acid (GABA) and glutamate signaling. Specifically, disrupted information transfer and processing at GABAergic and glutamatergic synapses in major depression may occur at several points throughout the signaling process, from the movement of information (i.e., an excitatory signal) down a glutamatergic axon, to neurotransmitter release and recycling at the synapse, and to postsynaptic modulation of transferred signal by GABAergic inhibition. Here we review postmortem studies for specific cell types (pyramidal and GABA neurons, astrocytes, and oligodendrocytes) and genes, which together provide evidence for putative changes in glutamate and/or GABA structural tripartite synapses, involving presynaptic neurons, postsynaptic targets, and astrocytic support. The nature of affected genes and cellular markers further suggests that GABAergic signaling targeting distal dendrites of pyramidal neurons may be more selectively and robustly affected in major depression. Implications of altered dendritic GABAergic inhibition for corticolimbic information processing in major depression and other brain disorders sharing similar pathologies are discussed. Aspects of this chapter were presented in Sibille and French (2013b) .
13.2 Altered components of the GABA tripartite synapse in major depression
13.2.1 The GABA Structural Tripartite Synapse
Before discussing cellular findings from postmortem investigations in major depression, we briefly review the major cell components and biochemical pathways engaged in GABA homeostasis (Fig. 13.1). GABA is the principal neurotransmitter responsible for neural inhibition and is present in approximately 20 % of all neurons in the adult neocortex (Hendry et al. 1987; Sahara et al. 2012) . In inhibitory neurons at a GABA synapse, the enzyme glutamic acid decarboxylase (GAD), found in two forms, GAD65 and GAD67 (Erlander et al. 1991) , synthesizes GABA through decarboxylation of glutamate , which is then packaged into synaptic vesicles by the vesicular GABA transporter (VGAT) (Fon and Edwards 2001) . Upon release of GABA from the synapse, the neurotransmitter acts at two main classes of receptors: (i) the ionotropic GABAARs, heteropentameric ligand-gated chloride channels which mediate fast inhibitory actions of GABA, and (ii) the metabotropic GABABRs, G-protein coupled receptors that, on a slower time scale, modulate synaptic transmission through second messenger systems. Termination of GABA transmission occurs when GABA transporters (GAT) on both GABAergic presynaptic terminals and neighboring glia remove GABA from the synaptic cleft. While neurons can recycle GABA by direct reuptake from the synaptic cleft, GABA is also metabolized in glial cells by GABA transaminase (GABA-T) to succinate, which enters the TCA cycle and is converted to glutamate. This glutamate is further converted by glutamine synthetase (GS) into glutamine, which is shuttled back to GABA neurons. In GABA neurons, glutamine released by astrocytic system N transporters (SNAT3) is taken by system A transporters (SNAT1/SNAT2) (Broer and Brookes 2001; Chaudhry et al. 2002) , converted to glutamate by glutaminase (GLS), and to GABA by GAD, as reviewed in Bak et al. (2006) and Owens and Kriegstein (2002) .
Gamma-aminobutyric acid (GABA) and glutamate tripartite synapses. The top panel represents synapses between an excitatory axonal terminal (top) and a GABAergic inhibitory terminal (middle; red) onto a pyramidal dendritic spine (bottom; black). Astrocytes (right and left middle; blue) are present at both excitatory and inhibitory synapses, and myelination of the excitatory axon by oligodendrocytes is shown (green spiral). In major depression, the integrity of information transfer and processing could be compromised at several compartments (numbers correspond to figure components): (1) Decreased oligodendrocyte support of axonal function leading to suboptimal conduction of action potentials along the axon; (2) Disruption of synaptic transfer of information, due to changes in the structure of pyramidal neurons and the availability of glutamate; (3) Suboptimal modulation or “fine-tuning” of excitatory postsynaptic signals onto dendritic spines due to reduced somatostatin (SST)-positive GABAergic dendritic targeted inhibition; and (4) Impaired astrocyte function resulting in altered extracellular neurotransmitter clearance, affecting the GABA/glutamate balance and cycling.
Molecular correlates of the GABA tripartite synapse. The bottom panel is a close-up on the GABA tripartite synapse. Genes whose products are associated with the presynaptic GABAergic neuron (top; red) are listed. SST, neuropeptide Y (NPY), and cortistatin (CORT) encode for neuropeptide markers for a specific subset of dendritic-targeting inhibitory interneurons (see Fig. 13.2). Glutamate decarboxylase 1 (GAD1) and GAD2 encode the 67- and 65-kDa forms of GAD, which are responsible for synthesizing GABA from L-glutamic acid. SLC32A1 (vesicular GABA transporter, VGAT) encodes for an integral membrane protein that packages GABA into synaptic vesicles for release into the synaptic cleft. SLC6A1 (GABA transporter 1; GAT1) encodes a GABA transporter that removes GABA from the synaptic cleft. Glutaminase (GLS) encodes glutaminase, which generates glutamate from glutamine. GABA B receptors are also found on the presynaptic neuron. At the postsynaptic neuron (bottom), both GABAA and GABAB receptors are present, exhibiting various subunit combinations. For astrocytes (blue), both aldehyde hydrogenase 1 family, member L1 (ALDH1L1) and glial fibrillary acidic protein (GFAP) can be used as markers. Glutamate ammonia ligase (GLUL) encodes for the GS protein that is important for glutamate-glutamine-GABA cycling; GS catalyzes synthesis of glutamine from glutamate. ABAT encodes for the enzyme 4-aminobutyrate aminotransferase, which catabolizes GABA. SLC6A1 (GAT1), SLC6A13 (GAT2), and SLC6A11 (GAT3) all encode for various GABA transporters present in astrocytes. Although GAT1 is primarily considered a neuronal GABA transporter, it is present on some astrocytic processes. (Figure adapted from Sibille and French 2013b)
13.2.2 Glial Pathology in Major Depression
Glial cells are nonneuronal cells of the adult brain, which provide support and protection for neurons and are traditionally classified into three main groups: astrocytes , oligodendrocytes, and microglia . Observations of a 24 % decrease in mean number of subgenual PFC glial cells in patients with familial major depression provided early evidence for glial cell changes in depression (Ongur et al. 1998) . Reduced glial cell density was also observed in the dlPFC and ACC in depression (Rajkowska et al. 1999; Cotter et al. 2001) , alongside reports of low glial numbers in the amygdala (Bowley et al. 2002) . Although there are negative reports citing no changes in glial cells in orbital frontal cortex (OFC) and dlPFC in late-life depression (Khundakar et al. 2009, 2011) , the majority of studies point towards reductions in glial density and number in subjects with major depression. Technological challenges associated with isolating and identifying homogenous cell types partially account for the absence of cell-specific findings in the earliest reports, but more recent studies do distinguish between the glial classes. Evidence suggesting astrocyte- and oligodendrocyte-specific pathologies in major depression is discussed here .
13.2.3 Reduced Oligodendrocyte Structure and Numbers in Major Depression
Oligodendrocytes ensheathe neurons with myelin and provide critical axonal insulation to facilitate the conduction of electrical impulses and enable saltatory conduction, together ensuring integrity of information transfer along axons. Using morphological cell-type determination, it has been suggested that decreased glial cell numbers in the amygdala and PFC may be attributed to a specific reduction in oligodendrocytes (Hamidi et al. 2004; Uranova et al. 2004) . Decreased oligodendrocytes have also been reported by flow cytometry, using fluorescently labeled suspended nuclei from the frontopolar cortex in major depression (Hayashi et al. 2011) . Although negative findings were reported in the ACC (Sibille et al. 2009) and amygdala (Guilloux et al. 2012) in female subjects, a gene array study in the amygdala of male subjects with major depression showed reduced expression of numerous genes related to oligodendrocyte structure and function (Sibille et al. 2009), consistent with reduced transcripts in the parietal and prefrontal cortices in other studies (Klempan et al. 2009; Kim and Webster 2010) . Pathological oligodendrocyte function may result in impaired communication and altered integrity of neuronal information transfer in major depression (Edgar and Sibille 2012) . This hypothesis is grounded in the basis of the role of oligodendrocytes in facilitating axonal conduction (Brodal 2010) , and of specific dysregulation of genes coding for proteins located at the nodes of Ranvier (Sibille et al. 2009), the site of functional interaction between oligodendrocytes and neurons. Hence, altered conduction and/or maintenance of axonal signaling integrity through altered oligodendrocyte structure and function may represent in some cases an early deregulated component (i.e., incoming information) contributing to altered information flow in major depression (green spindles in Fig. 13.1).
13.2.4 Astrocyte-Related Findings in Major Depression
Divided into two primary categories, protoplasmic (found in gray matter) and fibrous (found in white matter), astrocytes are principally responsible for regulating the neuronal chemical environment, and play an important role in extracellular clearance and recycling of neurotransmitters, including glutamate and GABA , as discussed above (Brodal 2010) . Controversial evidence also suggests a more active role for astrocytes in neurotransmission than previously considered, as they may release gliotransmitters, including glutamate, when depolarized (Araque et al. 1999) . However, recent findings that Gq-coupled metabotropic receptors mediating calcium influx (i.e., mGluR5) may not be expressed by adult human cortical astrocytes (Sun et al. 2013) , indicate that the role of depolarization and calcium-triggered neurotransmission of astrocytes may need to be revisited. Astrocyte-specific investigations of glial pathology in major depression suggest cellular hypertrophy in ACC white matter (Torres-Platas et al. 2011) . In addition, decreases in GFAP, a commonly used astrocytic marker, and in glutamate clearance transporters (EAAT1, EAAT2) expressed in astrocytes have been observed in the PFC of subjects with major depression (Miguel-Hidalgo et al. 2000; Si et al. 2004; Choudary et al. 2005; Miguel-Hidalgo et al. 2010) . In one study, GFAP levels between subjects with major depression and controls under 60 years of age showed a tenfold reduction; in contrast, no difference was seen between depressed subjects and controls over 60 years of age (Si et al. 2004). Astrocyte connexins 43 and 30, which mediate gap junction-based direct communication between astrocytes, and also participate in astrocyte-oligodendrocyte junctions (Orthmann-Murphy et al. 2008) , were observed to have decreased expression in suicide victims with a range of psychiatric diagnoses, including bipolar disorder, schizophrenia, and major depression (Ernst et al. 2011) . Together, the current model for altered glutamate and GABA neurotransmission in major depression includes the contribution of dysregulated astrocytic neurotransmitter recycling and homeostasis (Valentine and Sanacora 2009; Oh et al. 2012) (blue cells in Fig. 13.1).
13.2.5 Altered Cortical Neuronal Structure and Function in Major Depression
Several reviews have been published on the topic of morphological and cellular changes in the context of depression (Hercher et al. 2009; Rajkowska 2003; Rajkowska and Miguel-Hidalgo 2007) . Using morphological techniques to investigate changes in cell size and/or number, Rajkowska et al. have reported reduced density of neuronal cell bodies with large cell body size in cortical layers 2 through 5 of the OFC and in layers 2, 3, and 6 of the dlPFC in subjects with major depression (Rajkowska et al. 1999; Rajkowska 2000) . These findings were concurrent with increased density of neurons with small body size in layer 3 (OFC) and layers 3 and 6 (dlPFC). Decreased mean neuronal cell body size was also reported in layers 3 and 6 (dlPFC), layers 2 and 3 (OFC), and layer 6 (ACC) (Rajkowska et al. 1999; Cotter et al. 2001) . Reduced neuronal size in layer 6 of the dlPFC (Cotter et al. 2002b) and lower combined neuron density in both dorsal and frontal PFC (Underwood et al. 2012) were confirmed in later studies. Although post hoc comparisons between controls and depressed subjects were not significant, one study found the lowest density of pyramidal neurons in subjects with major depression compared to two other psychiatric disorders (bipolar disorder, schizophrenia) (Law and Harrison 2003) . Interestingly, in elderly depressed subjects, reduced pyramidal density in cortical layers 3 and 5 of the OFC (Rajkowska et al. 2005) , but not the dlPFC (Van Otterloo et al. 2009) was reported, potentially reflecting a separate etiology for late-life depression in elderly patients. More recently, a reduction in pyramidal neuron density was identified in layer 5b of the ACC in a cohort of primarily older mood disorder subjects, of which five subjects were diagnosed with major depression and two of whom suffered from bipolar disorder (Gittins and Harrison 2011) .
Despite earlier speculation that the reductions in neuronal density observed in dlPFC involved glutamatergic pyramidal neurons (due to location of the reductions in pyramidal layers), no difference in packing density of pyramidal neurons labeled using NF200, a neurofilament protein marker, was observed between depressed and control subjects (Miguel-Hidalgo et al. 2005) . While the authors concluded that this presented lack of evidence for neurofilament-related cytoskeleton deficiencies in NF200 immunoreactive neurons in PFC circuitry in depression , it should be noted that an earlier study using a variation of the same antibody (N200), found that even with the three antibodies used to label subpopulations of pyramidal cells (FNPY, SMI32, N200), at least half of all pyramidal neurons remained unlabeled (Law and Harrison 2003) .
Although it is unlikely that neuronal loss underlies these changes, it remains to be resolved whether the decreased neuronal density reflects changes in neuropil or dendritic complexity. Supporting the hypothesis of reduced dendritic complexity in depression, a decrease in total dendritic length and somal areas was observed in deep and superficial layer 3 in a cohort enriched in patients with major depression (Yung et al. 2000) . Reduced numbers of third-order basilar dendritic branches were also reported in ACC layer 6 of depressed suicide victims using Golgi staining of neuronal processes (Hercher et al. 2010) . All together, despite evidence for reduced density and dendritic length of pyramidal neurons, findings of potential pathological changes in pyramidal cells in major depression are often subtle, depend on the age of the subjects, are regionally specific, mixed, and are overall in need of further confirmation in large cohorts.
13.2.6 Glutamate Levels in Major Depression
In support of functional changes related to glutamatergic signaling in major depression, investigators have reported altered in vivo levels of glutamate and glutamate-related metabolites in subjects with major depression using proton magnetic resonance spectroscopy (1H MRS) . These studies frequently report their findings using the term Glx, a measurement which primarily reflects glutamate and glutamine, but does contain small contributions from other metabolites, including GABA (Valentine and Sanacora 2009; Maddock and Buonocore 2012) . Moreover, it is important to keep in perspective that MRS findings do not reflect what is occurring at the level of neurotransmission, as only a small part of these measurements reflect synaptic levels and the majority of metabolites measured with 1H MRS are intracellular (Sanacora et al. 2012). Nevertheless, diagnostic differences reported in these studies suggest changes in neurotransmitter cycling and clearance, which may affect GABA/glutamate homeostasis. As reviewed in Yuksel and Ongur (2010) , MRS studies have shown reduced Glx and/or glutamate concentrations across multiple cortical and subcortical brain regions including ACC (Auer et al. 2000; Pfleiderer et al. 2003; Zhang et al. 2012) , PFC (Michael et al. 2003a; Hasler et al. 2007) , amygdala (Michael et al. 2003b), and hippocampus (Block et al. 2009) . However, no differences in hippocampus (Milne et al. 2009) and occipital cortex (Price et al. 2009) and even increased glutamate levels have also been reported in the occipital cortex (Sanacora et al. 2004) , suggesting region-specific pathological effects, and opposing findings in frontal cortex and cingulate regions (reduced glutamate) versus occipital and parietal/occipital regions (increased glutamate) (Sanacora et al. 2012) . Notably, both glutamate (Zhang et al. 2012) and Glx (Pfleiderer et al. 2003; Michael et al. 2003a, b) have been shown to increase with electroconvulsive treatment .
13.2.7 Low GABA Levels and Reduced Markers of Dendritic-Targeting GABA Neurons in Major Depression
GABA neurons can be divided into subpopulations not only based on diverse morphology, but also on the calcium-binding proteins or neuropeptides that they express (Fig. 13.2). GABA neurons expressing SST , NPY, and CORT are known to target and inhibit the distal dendrites of pyramidal neurons; whereas interneurons expressing parvalbumin (PV) and cholecystokinin (CCK) target the cell body and axon initial segment, and calretinin (CR)-expressing neurons target other GABA neurons. Reduced density of GABA neurons immunoreactive for specific calcium-binding proteins has been reported in the dlPFC in major depression (Rajkowska et al. 2007) , but see also Beasley et al. (2002) and Cotter et al. (2002a) for negative findings in the dlPFC and ACC. In Rajkowska et al. (2007) , the density of calbindin (CB)-positive neurons was reduced by 50 % in dlPFC, and no differences in PV-positive neurons were observed. Reductions in the density of CB-positive neurons were also reported in the occipital cortex (Maciag et al. 2010) .
GABA microcircuitry. GABA neurons expressing somatostatin (SST), neuropeptide Y (NPY), and cortistatin (CORT) target and inhibit the distal dendrites of pyramidal neurons (PYR); whereas interneurons expressing parvalbumin (PV) and cholecystokinin (CCK) target the cell body and axon initial segment, and calretinin (CR)-expressing neurons target other GABA neurons. Evidence from human postmortem studies suggest that the subsets of GABA neurons that selectively target the dendrites of pyramidal neurons (i.e., SST-, NPY-, and CORT-positive) are affected in major depression, while evidence for changes in other GABA neuron subtypes are fewer (i.e., PV) or mostly (i.e., CCK, CR) negative. (Figure adapted from Sibille 2013a)
Recently, our group has reported reduced SST, a modulatory neuropeptide, in the dlPFC (Sibille et al. 2011) , subgenual ACC (Tripp et al. 2011; Tripp et al. 2012), and amygdala (Guilloux et al. 2012) of subjects with major depression. These findings are consistent with previous studies, as SST is mostly expressed in CB-positive cells in the cortex (Martel et al. 2012) . Intriguingly, based on their common target of distal dendrites of excitatory pyramidal neurons, NPY and CORT expression was also lower in the sgACC and amygdala in subjects with major depression (Guilloux et al. 2012; Tripp et al. 2012) . In contrast, CCK and CR were unaffected in the ACC and amygdala, and PV expression was lower in the ACC, but not the dlPFC (Sibille et al. 2011; Tripp et al. 2012) . Consistent with an elevated female vulnerability for major depression, analysis of these GABA interneuron markers stratified by sex revealed more robust downregulation of SST in female subjects with major depression in the subgenual ACC compared to males patients (Tripp et al. 2011, 2012). Additionally, SST was reduced in the amygdala of females (Guilloux et al. 2012) , but not males with major depression (Sibille et al. 2009). Interestingly, control female subjects (i.e., not depressed) already displayed lower expression of SST, CORT, and NPY, compared to male control subjects, suggesting that baseline expression of these genes is already close to the low levels observed in depressed subjects in female subjects. Reduced levels of GAD67, an enzyme responsible for synthesis of GABA from glutamate, have not been consistently reported, but were observed in some studies, including at the protein level in the dlPFC (Karolewicz et al. 2010) , and at the mRNA levels coding for both GAD65 and GAD67 in the sgACC (Tripp et al. 2012). Adding another layer of complexity, expression profiles of SST, NPY, and CORT also decrease with age in multiple brain regions (Erraji-Benchekroun et al. 2005) . For instance, SST levels are approximately 40–50 % lower at age 70 compared to age 20 (Erraji-Benchekroun et al. 2005; Tripp et al. 2011); the age-related reduction in SST is present in both controls and subjects with major depression, with depressed subjects consistently exhibiting lower levels across all ages (Sibille et al. 2011; Tripp et al. 2011) .
Notably, these cellular findings are consistent with reports of decreased GABA concentration in major depression, as observed by 1H MRS or by transcranial magnetic stimulation occipital and frontal cortices (Hasler et al. 2007; Levinson et al. 2010; Gabbay et al. 2012; Hasler and Northoff 2011) . Selective serotonin reuptake inhibitors or electroconvulsive therapy reverse these changes (Sanacora et al. 2002, 2003) . It has been suggested that the concentration of GABA in the ACC mediates default-mode network negative responses during emotion processing by studies that combine functional imaging and resting-state MRS (Northoff et al. 2007), and interestingly, reduced GABA levels in the ACC correlate with measures of anhedonia across depressed and control adolescents (Gabbay et al. 2012). These data provide brain-based evidence in human subjects with major depression for the GABA hypothesis of emotion dysregulation in depression (Brambilla et al. 2003; Luscher et al. 2011) , originally proposed in 1980 as a broader GABAergic dysfunction hypothesis of affective disorders, based on the efficacy of sodium valproate, a GABAergic anticonvulsant, in treatment of mania (Emrich et al. 1980) . This hypothesis was supported by reports of low GABA levels in the plasma and cerebrospinal fluid of depressed subjects (Gold et al. 1980; Petty and Schlesser 1981; Petty and Sherman 1984; Gerner and Hare 1981) , and later by the association between GABAergic transmission and control of stress, reviewed in Luscher et al. (2011), the effect of monoaminergic antidepressants on GABAergic transmission (Sanacora et al. 2002) , and genetic manipulation studies in rodents (Earnheart et al. 2007) .
The combined results from these studies provide supporting evidence for reduced GABA levels and for selective cellular changes potentially affecting neuropeptide- and/or GABA-related functions of the CB/SST-positive interneuron subtype (red cells in Fig. 13.1), which in some studies paralleled the heightened female vulnerability to suffer from depressive episodes. Together, these converging results suggest that GABA neurons regulating dendritic inhibition may represent a “weak link” within the biological module formed by the GABA tripartite synapse, which is frequently affected in major depression and potentially moderated by age and sex.
13.2.8 GABA Receptors in Major Depression and Other Mood Disorders
Deficits in GABAAR-binding sites have been implicated by studies of benzodiazepine receptor binding sites in various anxiety disorders, such as generalized anxiety disorder (Tiihonen et al. 1997) and posttraumatic stress disorder (Bremner et al. 2000) . An absence of alterations in benzodiazepine receptor binding was found in depressed subjects (Kugaya et al. 2003) ; although microarray expression profiling and analysis of gene expression by quantitative polymerase chain reaction (qPCR) have reported altered expression and subunit composition of specific GABAAR subunits in depressed suicides and in major depression in various brain regions, including among others, multiple areas of the frontal and motor cortices and inferior temporal gyrus (Merali et al. 2004; Sequeira et al. 2009, 2007; Aston et al. 2005; Choudary et al. 2005; Klempan et al. 2009) . In major depression, decreased expression of the β2 and δ subunits of the GABAA receptor has been reported by microarray analysis in the middle temporal area (Brodmann area (BA) 21) (Aston et al. 2005) and dlPFC (BA9/46) (Choudary et al. 2005), respectively, along with increased expression of the β3 and γ2 subunits in the dlPFC (BA9/46) (Choudary et al. 2005). Reports of dysregulation in a number of GABAA receptors by microarray analysis of the ACC and dlPFC in subjects with major depression were made in conjunction with changes in glutamate receptor subunits, and lowered expression of GS and glial glutamate transporters (EAAT1, EAAT2) (Choudary et al. 2005). In depressed suicides, decreased expression of the α1, α3, and α4 subunits were found by either qPCR or microarray in BA8, BA9, BA10, and BA24 (Merali et al. 2004; Klempan et al. 2009; Sequeira et al. 2007) ; β1 was reported up in BA24 (Sequeira et al. 2007, 2009), but down in BA46; β3 was reported increased in BA 6, 10, and 38 (Sequeira et al. 2009); δ was up in BA6, BA44, and BA46 (Sequeira et al. 2009; Klempan et al. 2009); decreased expression of γ1 was found for BA 10, 21, and 46 (Merali et al. 2004; Sequeira et al. 2009; Klempan et al. 2009); γ2 was found increased in BA 20 (Sequeira et al. 2009; Klempan et al. 2009); and finally, decreases in ρ1 expression were found for BA21 and BA44 (Sequeira et al. 2009; Klempan et al. 2009); as reviewed in (Luscher et al. 2011) . Upregulation in expression of the α5 subunit of the GABAA receptor, which is selective to dendritic branches, was reported in bipolar disorder. Although one study reported an upregulation of the α5 subunit in BA46 in major depression (Sequeira et al. 2009), these changes were not evident in other studies, or elevated levels were restricted to depressed suicides compared to suicide victims with no lifetime history of major depression (Klempan et al. 2009; Choudary et al. 2005) . Alterations in GABAB receptor subunits have also been implicated in psychiatric disorders. For instance, upregulation in expression of GABBR1 (GABABR1) has been reported for bipolar disorder (Choudary et al. 2005), and up-regulation in expression of GABBR2 (GABABR2) has been reported for depressed suicides (Klempan et al. 2009) .
Altogether, reports of changes in the levels of GABA receptors in mood disorders are complex, differ depending on the brain region investigated, and are not consistently replicated across studies. This may reflect variable attempts to adapt and/or compensate to deregulations in GABA signaling and local circuits, and the limitations of postmortem studies to capture events that occur on time frame of hours, as noted for adaptive changes in GABA receptors (Jacob et al. 2008) . Further studies are needed to characterize the role of changes in GABA receptors, including of dynamic changes over time and more systematic investigation in cohorts with equal representation of male and female subjects with major depression .
13.3 Implications of Altered GABA Function in Major Depression
13.3.1 Summary of Postmortem Findings
Molecular and cellular evidence from postmortem studies , combined with imaging data, suggest alterations in several components of the local cell circuitry in major depression, which may affect GABA and glutamate homeostasis, including changes to the structure and function of glutamatergic neurons, dendritic-targeting GABAergic neurons, astrocytes, and oligodendrocytes. Based on the findings summarized here, a speculative set of events contributing to dysregulated information processing and transfer in depression may occur in corticolimbic circuits as follows (Fig. 13.1): first, suboptimal conduction of action potentials along the axon could be caused by decreased oligodendrocyte support, leading to decreased integrity of information input or output. Second, changes in pyramidal neuron structure and in the availability of glutamate could disrupt the synaptic transfer of information. Third, reduced inhibition by dendritic targeting SST-positive GABA interneurons may lead to suboptimal modulation of excitatory postsynaptic signals onto dendritic spines. Finally, impaired astrocyte function may cause altered extracellular neurotransmitter clearance and recycling, which in turn may lead to an imbalance in GABA and glutamate homeostasis within their respective tripartite synapses. Although the situation in the diseased condition is more complex than proposed here, disrupted information transfer may result from pathologies occurring in any of these components. The glutamate component of this model is discussed elsewhere in this book, and this chapter has focused primarily on evidence suggesting a robust deregulated GABA component, specifically affecting dendritic inhibition .
13.3.2 GABA-Related Dendritic Inhibition, as a Vulnerable Biological Component of the Local Cell Circuitry in Major Depression; Continuum with Other Brain Disorders and Implications for Information Processing
The fact that the above-mentioned GABA-related findings were identified in corticolimbic brain regions suggests that these local circuit changes may affect the function of several nodes within a critical neural network of mood regulation, potentially resulting in altered sensing and processing of emotionally salient information. Current models of emotion regulation identify the amygdala as critical for sensing and assessing emotionally-salient stimuli, the dlPFC as one of the regions responsible for top-down cognitive assessment of emotional salience, and the ACC as the site of integration of information between bottom-up amygdala information and top-down dlPFC control, together providing cognitive control over emotional and motivational states (Phillips et al. 2008) . Reduced GABA-mediated inhibition may contribute to increased activity in respective brain areas, including increased amygdala and/or sgACC activities, as frequently reported in major depression (Surguladze et al. 2005; Fu et al. 2004) . So, restoring GABA-mediated dendritic inhibitory function may reduce pyramidal cell activation and excitatory tone, contributing to reduced ACC activation with positive response to therapeutic intervention such as deep brain stimulation, for instance (Mayberg et al. 2005) .
At the local circuit level, the converging evidence points towards selective deficits in the subtype of GABA neurons that targets the dendrites of excitatory glutamatergic neurons, whereas evidence for reduced markers of other GABA neuron subtypes are sparse or negative. On the other hand, cortical inhibitory deficits are frequent in other neuropsychiatric disorders , and alterations in SST levels have also been identified in schizophrenia (Morris et al. 2008) , bipolar disorder (Konradi et al. 2004, 2010), and in Huntington’s (Timmers et al. 1996) , Alzheimer’s (Davies et al. 1980; Epelbaum et al. 2009), and Parkinson’s diseases (Epelbaum et al. 1989). This could suggest the presence of intrinsic vulnerability factors within SST and related GABA neurons , and that common biological insults may similarly affect this cell population across several brain disorders. This dimensional perspective on disease pathology is more consistent with biological principles than with the categorical definition of psychiatric syndromes, although the functional output of similar pathologies may vary based on the biological context. For instance, the downstream effects of reduced dendritic inhibition may depend on the presence of additional pathological entities, such as robust downregulation of markers of soma-targeting GABA neurons, i.e., PV-positive, in schizophrenia (Lewis and Sweet 2009) , or the presence of neurodegenerative processes in other neurological disorders. These more complex inhibitory deficits, compared to evidence of more focused reductions in markers of GABA neurons mediating dendritic inhibition in major depression , may complicate the interpretation across disorders. Consequently, while the GABA tripartite synapse may represent a vulnerable biological module in the brain and accordingly across brain disorders, it may not lead to a unique behavioral endophenotype across these disorders. In major depression, the observation that reduced SST levels were more robust in female patients provides an interesting parallel with the increased female vulnerability to depression, although this putative causal link will need to be tested directly, potentially through the use of rodent models.
Etiological pathways leading to reduced markers of dendritic inhibition may also vary across disorders. Brain-derived neurotrophic factor (BDNF) , a necessary trophic factor for SST and NPY expression (Glorioso et al. 2006) , shows reduced expression in neuropsychiatric disorders , such as depression , schizophrenia, and bipolar disorder (Lu and Martinowich 2008; Rakofsky et al. 2012) . Altered BDNF signaling in major depression, as evidenced by reduced expression in amygdala (Guilloux et al. 2012) and reduced receptor (TRKB) expression in the sgACC (Tripp et al. 2012) , is expected to impact SST expression. SST cells may also be particularly vulnerable to oxidative stress due to their expression of neuronal nitric oxide synthase (Jaglin et al. 2012) . In schizophrenia, reduced SST levels occur more systematically in the context of reduced PV, suggestive of a role for etiological pathways involving early developmental disturbances, such as deficits in transcription factors known to regulate the ontogeny of both neuron subtypes (Volk et al. 2012) . It is also interesting to note that a recent report in the rodent cortex revealed that a small subset of SST-positive GABA neurons differs from the traditional dendritic targeting model, and in fact disinhibits layer 4 neurons, through the targeted inhibition of PV-positive GABA neurons in that layer (Xu et al. 2013) . If confirmed in other cortical areas and across species, the implication of this finding could be of opposing effects of low SST-positive GABA neuron function on excitatory neurons (i.e., less inhibition in layers 2 and 5, less disinhibition in layer 4). This would also indicate that an even downregulation across cortical layers in major depression (Tripp and Sibille, unpublished report) may reflect the presence of common upstream causal factors, rather than compensatory mechanisms to maintain local circuit homeostasis across cortical layers which could take complex patterns, together consistent with a model of SST-positive GABA neuron subtype intrinsic vulnerabilities.
13.4 Conclusion, Future Directions
How does the framework of the tripartite synapse, informed by a robust identification of reduced GABA-mediated inhibition in major depression , enable us to move forward in uncovering the pathophysiology of major depression? The evidence reviewed above suggests that a dimensional approach considering the biological modules of the glutamate and GABA tripartite synapses (Fig. 13.1) and their subcellular targeted components (Fig. 13.2; e.g., dendritic versus perisomatic) may contribute to the identification of biological vulnerabilities (i.e., weak links) in major depression that will also have implications across several brain-related disorders. Further molecular characterization of the primary cellular pathology in the human postmortem brain of patients and control subjects is needed; for example, by using a combination of laser capture microscopy with gene expression panels and targeted proteomic approaches for groups of genes and gene products related to the glutamate, GABA, and astrocyte components of local circuit modules (Fig. 13.1). Imaging genetics for panels of genetic variants corresponding to these local circuit components may serve to bridge those basic cellular and gene studies with functional outcomes to systematically assess specificities and/or continuum between putative cellular pathologies and symptom dimensions in major depression and across other categorically defined neuropsychiatric disorders.
Abbreviations
- ABAT:
-
4-Aminobutyrate aminotransferase
- ACC:
-
Anterior cingulate cortex
- ALDH1L1:
-
Aldehyde hydrogenase 1 family, member L1
- BA:
-
Brodmann area
- BDNF:
-
Brain-derived neurotrophic factor
- CB:
-
Calbindin
- CCK:
-
Cholecystokinin
- CORT:
-
Cortistatin
- CR:
-
Calretinin
- dlPFC:
-
Dorsal lateral prefrontal cortex
- EAAT1:
-
Excitatory amino acid transporter1 glutamate clearance transporter 1
- EAAT2:
-
Excitatory amino acid transporter1glutamate clearance transporter 2
- GABA:
-
Gamma-aminobutyric acid
- GABAAR:
-
GABA A receptor
- GABABR:
-
GABA B receptor
- GABA-T:
-
GABA transaminase
- GABBR1:
-
GABA B receptor 1
- GABBR2:
-
GABA B receptor 2
- GAD:
-
Glutamic acid decarboxylase
- GAT:
-
GABA transporter
- GFAP:
-
Glial fibrillary acidic protein
- GLS:
-
Glutaminase
- GLUL:
-
Glutamate ammonia ligase
- GS:
-
Glutamine synthetase
- 1H MRS:
-
Proton magnetic resonance spectroscopy
- NPY:
-
Neuropeptide Y
- OFC:
-
Orbital frontal cortex
- PFC:
-
Prefrontal cortex
- PV:
-
Parvalbumin
- qPCR:
-
Quantitative polymerase chain reaction
- sgACC:
-
Subgenual anterior cingulate cortex
- SNAT3:
-
Astrocytic system N transporter
- SNAT1/SNAT2:
-
System A transporters
- SST:
-
Somatostatin
- TRKB:
-
Tropomyosin related kinase B
- VGAT:
-
Vesicular GABA transporter
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC:American Psychiatric Association; 2000.
Araque A, Parpura V, Sanzgiri RP, Haydon PG. Tripartite synapses: glia, the unacknowledged partner. Trends Neurosci. 1999;22(5):208–15.
Aston C, Jiang L, Sokolov BP. Transcriptional profiling reveals evidence for signaling and oligodendroglial abnormalities in the temporal cortex from patients with major depressive disorder. Mol Psychiatry. 2005;10(3):309–22.
Auer DP, Putz B, Kraft E, Lipinski B, Schill J, Holsboer F. Reduced glutamate in the anterior cingulate cortex in depression: an in vivo proton magnetic resonance spectroscopy study. Biol Psychiatry. 2000;47(4):305–13.
Bak LK, Schousboe A, Waagepetersen HS. The glutamate/GABA-glutamine cycle: aspects of transport, neurotransmitter homeostasis and ammonia transfer. J Neurochem. 2006;98(3):641–53.
Beasley CL, Zhang ZJ, Patten I, Reynolds GP. Selective deficits in prefrontal cortical GABAergic neurons in schizophrenia defined by the presence of calcium-binding proteins. Biol Psychiatry. 2002;52(7):708–15.
Block W, Traber F, von Widdern O, Metten M, Schild H, Maier W, Zobel A, Jessen F. Proton MR spectroscopy of the hippocampus at 3 T in patients with unipolar major depressive disorder: correlates and predictors of treatment response. Int J Neuropsychopharmacol. 2009;12(3):415–22.
Bowley MP, Drevets WC, Ongur D, Price JL. Low glial numbers in the amygdala in major depressive disorder. Biol Psychiatry. 2002;52(5):404–12.
Brambilla P, Perez J, Barale F, Schettini G, Soares JC. GABAergic dysfunction in mood disorders. Mol Psychiatry. 2003;8(8):721–37, 715.
Bremner JD, Innis RB, Southwick SM, Staib L, Zoghbi S, Charney DS. Decreased benzodiazepine receptor binding in prefrontal cortex in combat-related posttraumatic stress disorder. Am J Psychiatry. 2000;157(7):1120–6.
Brodal P. The central nervous system: structure and function. 4th ed. New York: Oxford University Press; 2010.
Broer S, Brookes N. Transfer of glutamine between astrocytes and neurons. J Neurochem. 2001;77(3):705–19.
Chaudhry FA, Reimer RJ, Edwards RH. The glutamine commute: take the N line and transfer to the A. J Cell Biol. 2002;157(3):349–55.
Choudary PV, Molnar M, Evans SJ, Tomita H, Li JZ, Vawter MP, Myers RM, Bunney WE Jr, Akil H, Watson SJ, Jones EG. Altered cortical glutamatergic and GABAergic signal transmission with glial involvement in depression. Proc Natl Acad Sci U S A. 2005;102(43):15653–8.
Cotter D, Mackay D, Landau S, Kerwin R, Everall I. Reduced glial cell density and neuronal size in the anterior cingulate cortex in major depressive disorder. Arch Gen Psychiatry. 2001;58(6):545–53.
Cotter D, Landau S, Beasley C, Stevenson R, Chana G, MacMillan L, Everall I. The density and spatial distribution of GABAergic neurons, labelled using calcium binding proteins, in the anterior cingulate cortex in major depressive disorder, bipolar disorder, and schizophrenia. Biol Psychiatry. 2002a;51(5):377–86.
Cotter D, Mackay D, Chana G, Beasley C, Landau S, Everall IP. Reduced neuronal size and glial cell density in area 9 of the dorsolateral prefrontal cortex in subjects with major depressive disorder. Cereb Cortex. 2002b;12(4):386–94.
Davies P, Katzman R, Terry RD. Reduced somatostatin-like immunoreactivity in cerebral cortex from cases of Alzheimer disease and Alzheimer senile dementa. Nature. 1980;288(5788):279–80.
Earnheart JC, Schweizer C, Crestani F, Iwasato T, Itohara S, Mohler H, Luscher B. GABAergic control of adult hippocampal neurogenesis in relation to behavior indicative of trait anxiety and depression states. J Neurosci. 2007;27(14):3845–54.
Edgar N, Sibille E. A putative functional role for oligodendrocytes in mood regulation. Transl Psychiatry. 2012;2:e109.
Emrich HM, von Zerssen D, Kissling W, Moller HJ, Windorfer A. Effect of sodium valproate on mania. The GABA-hypothesis of affective disorders. Arch Psychiatr Nervenkr. 1980;229(1):1–16.
Epelbaum J, Agid F, Agid Y, Beaudet A, Bertrand P, Enjalbert A, Heidet V, Kordon C, Krantic S, Leonard JF, et al. Somatostatin receptors in brain and pituitary. Horm Res. 1989;31(1-2):45–50.
Epelbaum J, Guillou JL, Gastambide F, Hoyer D, Duron E, Viollet C. Somatostatin, Alzheimer’s disease and cognition: an old story coming of age? Prog Neurobiol. 2009;89(2):153–61.
Erlander MG, Tillakaratne NJ, Feldblum S, Patel N, Tobin AJ. Two genes encode distinct glutamate decarboxylases. Neuron. 1991;7(1):91–100.
Ernst C, Nagy C, Kim S, Yang JP, Deng X, Hellstrom IC, Choi KH, Gershenfeld H, Meaney MJ, Turecki G. Dysfunction of astrocyte connexins 30 and 43 in dorsal lateral prefrontal cortex of suicide completers. Biol Psychiatry. 2011;70(4):312–9.
Erraji-Benchekroun L, Underwood MD, Arango V, Galfalvy H, Pavlidis P, Smyrniotopoulos P, Mann JJ, Sibille E. Molecular aging in human prefrontal cortex is selective and continuous throughout adult life. Biol Psychiatry. 2005;57(5):549–58.
Fon EA, Edwards RH. Molecular mechanisms of neurotransmitter release. Muscle Nerve. 2001;24(5):581–601.
Fu CH, Williams SC, Cleare AJ, Brammer MJ, Walsh ND, Kim J, Andrew CM, Pich EM, Williams PM, Reed LJ, Mitterschiffthaler MT, Suckling J, Bullmore ET. Attenuation of the neural response to sad faces in major depression by antidepressant treatment: a prospective, event-related functional magnetic resonance imaging study. Arch Gen Psychiatry. 2004;61(9):877–89.
Gabbay V, Mao X, Klein RG, Ely BA, Babb JS, Panzer AM, Alonso CM, Shungu DC. Anterior cingulate cortex gamma-aminobutyric acid in depressed adolescents: relationship to anhedonia. Arch Gen Psychiatry. 2012;69(2):139–49.
Gerner RH, Hare TA. CSF GABA in normal subjects and patients with depression, schizophrenia, mania, and anorexia nervosa. Am J Psychiatry. 1981;138(8):1098–101.
Gittins RA, Harrison PJ. A morphometric study of glia and neurons in the anterior cingulate cortex in mood disorder. J Affect Disord. 2011;133(1-2):328–32.
Glorioso C, Sabatini M, Unger T, Hashimoto T, Monteggia LM, Lewis DA, Mirnics K. Specificity and timing of neocortical transcriptome changes in response to BDNF gene ablation during embryogenesis or adulthood. Mol Psychiatry. 2006;11(7):633–48.
Gold BI, Bowers MB, Roth RH, Sweeney DW. Gaba levels in CSF of patients with psychiatric-disorders. Am J Psychiat. 1980;137(3):362–4.
Guilloux JP, Douillard-Guilloux G, Kota R, Wang X, Gardier AM, Martinowich K, Tseng GC, Lewis DA, Sibille E. Molecular evidence for BDNF- and GABA-related dysfunctions in the amygdala of female subjects with major depression. Mol Psychiatry. 2012;17(11):1130–42.
Hamidi M, Drevets WC, Price JL. Glial reduction in amygdala in major depressive disorder is due to oligodendrocytes. Biol Psychiatry. 2004;55(6):563–9.
Hasler G, Northoff G. Discovering imaging endophenotypes for major depression. Mol Psychiatry. 2011;16(6):604–19.
Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, Drevets WC. Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2007;64(2):193–200.
Hayashi Y, Nihonmatsu-Kikuchi N, Yu X, Ishimoto K, Hisanaga SI, Tatebayashi Y. A novel, rapid, quantitative cell-counting method reveals oligodendroglial reduction in the frontopolar cortex in major depressive disorder. Mol Psychiatry. 2011;16(12):1155–8.
Hendry SH, Schwark HD, Jones EG, Yan J. Numbers and proportions of GABA-immunoreactive neurons in different areas of monkey cerebral cortex. J Neurosci. 1987;7(5):1503–19.
Hercher C, Turecki G, Mechawar N. Through the looking glass: examining neuroanatomical evidence for cellular alterations in major depression. J Psychiatr Res. 2009;43(11):947–61.
Hercher C, Canetti L, Turecki G, Mechawar N. Anterior cingulate pyramidal neurons display altered dendritic branching in depressed suicides. J Psychiatr Res. 2010;44(5):286–93.
Huynh NN, McIntyre RS. What Are the Implications of the STAR*D Trial for Primary Care? A Review and Synthesis. Prim Care Companion J Clin Psychiatry. 2008;10(2):91–6.
Jacob TC, Moss SJ, Jurd R. GABA(A) receptor trafficking and its role in the dynamic modulation of neuronal inhibition. Nat Rev Neurosci. 2008;9(5):331–43.
Jaglin XH, Hjerling-Leffler J, Fishell G, Batista-Brito R. The origin of neocortical nitric oxide synthase-expressing inhibitory neurons. Front Neural Circuits. 2012;6:44.
Karolewicz B, Maciag D, O’Dwyer G, Stockmeier CA, Feyissa AM, Rajkowska G. Reduced level of glutamic acid decarboxylase-67 kDa in the prefrontal cortex in major depression. Int J Neuropsychopharmacol. 2010;13(4):411–20.
Kennedy SH, Giacobbe P. Treatment resistant depression-advances in somatic therapies. Ann Clin Psychiatry. 2007;19(4):279–87.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602.
Khundakar A, Morris C, Oakley A, McMeekin W, Thomas AJ. Morphometric analysis of neuronal and glial cell pathology in the dorsolateral prefrontal cortex in late-life depression. Br J Psychiatry. 2009;195(2):163–9.
Khundakar A, Morris C, Oakley A, Thomas AJ. A morphometric examination of neuronal and glial cell pathology in the orbitofrontal cortex in late-life depression. Int Psychogeriatr. 2011;23(1):132–40.
Kim S, Webster MJ. Correlation analysis between genome-wide expression profiles and cytoarchitectural abnormalities in the prefrontal cortex of psychiatric disorders. Mol Psychiatry. 2010;15(3):326–36.
Klempan TA, Sequeira A, Canetti L, Lalovic A, Ernst C, Ffrench-Mullen J, Turecki G. Altered expression of genes involved in ATP biosynthesis and GABAergic neurotransmission in the ventral prefrontal cortex of suicides with and without major depression. Mol Psychiatry. 2009;14(2):175–89.
Konradi C, Eaton M, MacDonald ML, Walsh J, Benes FM, Heckers S. Molecular evidence for mitochondrial dysfunction in bipolar disorder. Arch Gen Psychiatry. 2004;61(3):300–8.
Konradi C, Zimmerman EI, Yang CK, Lohmann KM, Gresch P, Pantazopoulos H, Berretta S, Heckers S. Hippocampal interneurons in bipolar disorder. Arch Gen Psychiatry. 2011;68(4):340–50.
Kugaya A, Sanacora G, Verhoeff NP, Fujita M, Mason GF, Seneca NM, Bozkurt A, Khan SA, Anand A, Degen K, Charney DS, Zoghbi SS, Baldwin RM, Seibyl JP, Innis RB. Cerebral benzodiazepine receptors in depressed patients measured with [123I]iomazenil SPECT. Biol Psychiatry. 2003;54(8):792–9.
Law AJ, Harrison PJ. The distribution and morphology of prefrontal cortex pyramidal neurons identified using anti-neurofilament antibodies SMI32, N200 and FNP7. Normative data and a comparison in subjects with schizophrenia, bipolar disorder or major depression. J Psychiatr Res. 2003;37(6):487–99.
Levinson AJ, Fitzgerald PB, Favalli G, Blumberger DM, Daigle M, Daskalakis ZJ. Evidence of cortical inhibitory deficits in major depressive disorder. Biol Psychiatry. 2010;67(5):458–64.
Lewis DA, Sweet RA. Schizophrenia from a neural circuitry perspective: advancing toward rational pharmacological therapies. J Clin Invest. 2009;119(4):706–16.
Lu B, Martinowich K. Cell biology of BDNF and its relevance to schizophrenia. Novartis Found Symp. 2008;289:119–29; discussion 29–35, 93–5.
Luscher B, Shen Q, Sahir N. The GABAergic deficit hypothesis of major depressive disorder. Mol Psychiatry. 2011;16(4):383–406.
Maciag D, Hughes J, O’Dwyer G, Pride Y, Stockmeier CA, Sanacora G, Rajkowska G. Reduced density of calbindin immunoreactive GABAergic neurons in the occipital cortex in major depression: relevance to neuroimaging studies. Biol Psychiatry. 2010;67(5):465–70.
Maddock RJ, Buonocore MH. MR spectroscopic studies of the brain in psychiatric disorders. Curr Top Behav Neurosci. 2012; 11:199–251.
Martel G, Dutar P, Epelbaum J, Viollet C. Somatostatinergic systems: an update on brain functions in normal and pathological aging. Front Endocrinol (Lausanne). 2012;3:154.
Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, Silva JA, Tekell JL, Martin CC, Lancaster JL, Fox PT. Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am J Psychiatry. 1999;156(5):675–82.
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, Schwalb JM, Kennedy SH. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45(5):651–60.
Merali Z, Du L, Hrdina P, Palkovits M, Faludi G, Poulter MO, Anisman H. Dysregulation in the suicide brain: mRNA expression of corticotropin-releasing hormone receptors and GABA(A) receptor subunits in frontal cortical brain region. J Neurosci. 2004;24(6):1478–85.
Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B Metabolic changes within the left dorsolateral prefrontal cortex occurring with electroconvulsive therapy in patients with treatment resistant unipolar depression. Psychol Med. 2003a;33(7):1277–84.
Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B Neurotrophic effects of electroconvulsive therapy: A proton magnetic resonance study of the left amygdalar region in patients with treatment-resistant depression. Neuropsychopharmacology. 2003b;28(4):720–5.
Miguel-Hidalgo JJ, Baucom C, Dilley G, Overholser JC, Meltzer HY, Stockmeier CA, Rajkowska G. Glial fibrillary acidic protein immunoreactivity in the prefrontal cortex distinguishes younger from older adults in major depressive disorder. Biol Psychiatry. 2000;48(8):861–73.
Miguel-Hidalgo JJ, Dubey P, Shao Q, Stockmeier C, Rajkowska G. Unchanged packing density but altered size of neurofilament immunoreactive neurons in the prefrontal cortex in schizophrenia and major depression. Schizophr Res. 2005;76(2–3):159–71.
Miguel-Hidalgo JJ, Waltzer R, Whittom AA, Austin MC, Rajkowska G, Stockmeier CA. Glial and glutamatergic markers in depression, alcoholism, and their comorbidity. J Affect Disord. 2010;127(1-3):230–40.
Milne A, MacQueen GM, Yucel K, Soreni N, Hall GB. Hippocampal metabolic abnormalities at first onset and with recurrent episodes of a major depressive disorder: a proton magnetic resonance spectroscopy study. Neuroimage. 2009;47(1):36–41.
Morris HM, Hashimoto T, Lewis DA. Alterations in somatostatin mRNA expression in the dorsolateral prefrontal cortex of subjects with schizophrenia or schizoaffective disorder. Cereb Cortex. 2008;18(7):1575–87.
Northoff G, Walter M, Schulte RF, Beck J, Dydak U, Henning A, Boeker H, Grimm S, Boesiger P. GABA concentrations in the human anterior cingulate cortex predict negative BOLD responses in fMRI. Nat Neurosci. 2007;10(12):1515–7.
Oh DH, Son H, Hwang S, Kim SH. Neuropathological abnormalities of astrocytes, GABAergic neurons, and pyramidal neurons in the dorsolateral prefrontal cortices of patients with major depressive disorder. Eur Neuropsychopharmacol. 2012;22(5):330–8.
Ongur D, Drevets WC, Price JL. Glial reduction in the subgenual prefrontal cortex in mood disorders. Proc Natl Acad Sci U S A. 1998;95(22):13290–5.
Orthmann-Murphy JL, Abrams CK, Scherer SS. Gap junctions couple astrocytes and oligodendrocytes. J Mol Neurosci. 2008;35(1):101–16.
Owens DF, Kriegstein AR. Is there more to GABA than synaptic inhibition? Nat Rev Neurosci. 2002;3(9):715–27.
Petty F, Schlesser MA. Plasma GABA in affective illness. A preliminary investigation. J Affect Disord. 1981;3(4):339–43.
Petty F, Sherman AD. Plasma GABA levels in psychiatric illness. J Affect Disord. 1984;6(2):131–8.
Pfleiderer B, Michael N, Erfurth A, Ohrmann P, Hohmann U, Wolgast M, Fiebich M, Arolt V, Heindel W. Effective electroconvulsive therapy reverses glutamate/glutamine deficit in the left anterior cingulum of unipolar depressed patients. Psychiat Res-Neuroim. 2003;122(3):185–92.
Phillips ML, Ladouceur CD, Drevets WC. A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Mol Psychiatry. 2008;13(9):829, 833–57.
Price RB, Shungu DC, Mao X, Nestadt P, Kelly C, Collins KA, Murrough JW, Charney DS, Mathew SJ. Amino acid neurotransmitters assessed by proton magnetic resonance spectroscopy: relationship to treatment resistance in major depressive disorder. Biol Psychiatry. 2009;65(9):792–800.
Rajkowska G. Postmortem studies in mood disorders indicate altered numbers of neurons and glial cells. Biol Psychiatry. 2000;48(8):766–77.
Rajkowska G. Depression: what we can learn from postmortem studies. Neuroscientist. 2003;9(4):273–84.
Rajkowska G, Miguel-Hidalgo JJ. Gliogenesis and glial pathology in depression. CNS Neurol Disord Drug Targets. 2007;6(3):219–33.
Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY, Overholser JC, Roth BL, Stockmeier CA. Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biol Psychiatry. 1999;45(9):1085–98.
Rajkowska G, Miguel-Hidalgo JJ, Dubey P, Stockmeier CA, Krishnan KR. Prominent reduction in pyramidal neurons density in the orbitofrontal cortex of elderly depressed patients. Biol Psychiatry. 2005;58(4):297–306.
Rajkowska G, O’Dwyer G, Teleki Z, Stockmeier CA, Miguel-Hidalgo JJ. GABAergic neurons immunoreactive for calcium binding proteins are reduced in the prefrontal cortex in major depression. Neuropsychopharmacology. 2007;32(2):471–82.
Rakofsky JJ, Ressler KJ, Dunlop BW. BDNF function as a potential mediator of bipolar disorder and post-traumatic stress disorder comorbidity. Mol Psychiatry. 2012;17(1):22–35.
Sahara S, Yanagawa Y, O’Leary DD, Stevens CF. The fraction of cortical GABAergic neurons is constant from near the start of cortical neurogenesis to adulthood. J Neurosci. 2012;32(14):4755–61.
Sanacora G, Mason GF, Rothman DL, Krystal JH. Increased occipital cortex GABA concentrations in depressed patients after therapy with selective serotonin reuptake inhibitors. Am J Psychiatry. 2002;159(4):663–5.
Sanacora G, Mason GF, Rothman DL, Hyder F, Ciarcia JJ, Ostroff RB, Berman RM, Krystal JH. Increased cortical GABA concentrations in depressed patients receiving ECT. Am J Psychiatry. 2003;160(3):577–9.
Sanacora G, Gueorguieva R, Epperson CN, Wu YT, Appel M, Rothman DL, Krystal JH, Mason GF. Subtype-specific alterations of gamma-aminobutyric acid and glutamate in patients with major depression. Arch Gen Psychiatry. 2004;61(7):705–13.
Sanacora G, Treccani G, Popoli M. Towards a glutamate hypothesis of depression: an emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62(1):63–77.
Sequeira A, Klempan T, Canetti L, ffrench-Mullen J, Benkelfat C, Rouleau GA, Turecki G. Patterns of gene expression in the limbic system of suicides with and without major depression. Mol Psychiatry. 2007;12(7):640–55.
Sequeira A, Mamdani F, Ernst C, Vawter MP, Bunney WE, Lebel V, Rehal S, Klempan T, Gratton A, Benkelfat C, Rouleau GA, Mechawar N, Turecki G. Global brain gene expression analysis links glutamatergic and GABAergic alterations to suicide and major depression. PLoS ONE. 2009;4(8):e6585.
Si X, Miguel-Hidalgo JJ, O’Dwyer G, Stockmeier CA, Rajkowska G. Age-dependent reductions in the level of glial fibrillary acidic protein in the prefrontal cortex in major depression. Neuropsychopharmacology. 2004;29(11):2088–96.
Sibille E. Molecular aging of the brain, neuroplasticity, and vulnerability to depression and other brain-related disorders. Dialogues Clin Neurosci. 2013a; 15:53–65.
Sibille E, French B. Biological substrates underpinning diagnosis of major depression. Int J Neuropsychopharmacol. 2013b; 16:1893–1909.
Sibille E, Wang Y, Joeyen-Waldorf J, Gaiteri C, Surget A, Oh S, Belzung C, Tseng GC, Lewis DA. A molecular signature of depression in the amygdala. Am J Psychiatry. 2009;166(9):1011–24.
Sibille E, Morris HM, Kota RS, Lewis DA. GABA-related transcripts in the dorsolateral prefrontal cortex in mood disorders. Int J Neuropsychopharmacol. 2011:1–14.
Siegle GJ, Thompson W, Carter CS, Steinhauer SR, Thase ME. Increased amygdala and decreased dorsolateral prefrontal BOLD responses in unipolar depression: related and independent features. Biol Psychiatry. 2007;61(2):198–209.
Sun W, McConnell E, Pare JF, Xu Q, Chen M, Peng W, Lovatt D, Han X, Smith Y, Nedergaard M. Glutamate-dependent neuroglial calcium signaling differs between young and adult brain. Science. 2013;339(6116):197–200.
Surguladze S, Brammer MJ, Keedwell P, Giampietro V, Young AW, Travis MJ, Williams SC, Phillips ML. A differential pattern of neural response toward sad versus happy facial expressions in major depressive disorder. Biol Psychiatry. 2005;57(3):201–9.
Suslow T, Konrad C, Kugel H, Rumstadt D, Zwitserlood P, Schoning S, Ohrmann P, Bauer J, Pyka M, Kersting A, Arolt V, Heindel W, Dannlowski U. Automatic mood-congruent amygdala responses to masked facial expressions in major depression. Biol Psychiatry. 2010;67(2):155–60.
Tiihonen J, Kuikka J, Rasanen P, Lepola U, Koponen H, Liuska A, Lehmusvaara A, Vainio P, Kononen M, Bergstrom K, Yu M, Kinnunen I, Akerman K, Karhu J. Cerebral benzodiazepine receptor binding and distribution in generalized anxiety disorder: a fractal analysis. Mol Psychiatry. 1997;2(6):463–71.
Timmers HJ, Swaab DF, van de Nes JA, Kremer HP. Somatostatin 1-12 immunoreactivity is decreased in the hypothalamic lateral tuberal nucleus of Huntington’s disease patients. Brain Res. 1996;728(2):141–8.
Torres-Platas SG, Hercher C, Davoli MA, Maussion G, Labonte B, Turecki G, Mechawar N. Astrocytic hypertrophy in anterior cingulate white matter of depressed suicides. Neuropsychopharmacology. 2011;36(13):2650–8.
Tripp A, Kota RS, Lewis DA, Sibille E. Reduced somatostatin in subgenual anterior cingulate cortex in major depression. Neurobiol Dis. 2011;42(1):116–24.
Tripp A, Oh H, Guilloux JP, Martinowich K, Lewis DA, Sibille E. Brain-derived neurotrophic factor signaling and subgenual anterior cingulate cortex dysfunction in major depressive disorder. Am J Psychiatry. 2012;169(11):1194–202.
Underwood MD, Kassir SA, Bakalian MJ, Galfalvy H, Mann JJ, Arango V. Neuron density and serotonin receptor binding in prefrontal cortex in suicide. Int J Neuropsychopharmacol. 2012;15(4):435–47.
Uranova NA, Vostrikov VM, Orlovskaya DD, Rachmanova VI. Oligodendroglial density in the prefrontal cortex in schizophrenia and mood disorders: a study from the Stanley Neuropathology Consortium. Schizophr Res. 2004;67(2-3):269–75.
Valentine GW, Sanacora G. Targeting glial physiology and glutamate cycling in the treatment of depression. Biochem Pharmacol. 2009;78(5):431–9.
Van Otterloo E, O’Dwyer G, Stockmeier CA, Steffens DC, Krishnan RR, Rajkowska G. Reductions in neuronal density in elderly depressed are region specific. Int J Geriatr Psychiatry. 2009;24(8):856–64.
Volk DW, Matsubara T, Li S, Sengupta EJ, Georgiev D, Minabe Y, Sampson A, Hashimoto T, Lewis DA. Deficits in transcriptional regulators of cortical parvalbumin neurons in schizophrenia. Am J Psychiatry. 2012;169(10):1082–91.
WHO. World Health Organization—The Global Burden of Disease—2004 update. Geneva: WHO Library; 2008.
Xu H, Jeong HY, Tremblay R, Rudy B. Neocortical somatostatin-expressing GABAergic interneurons disinhibit the thalamorecipient layer 4. Neuron. 2013;77(1):155–67.
Yuksel C, Ongur D. Magnetic resonance spectroscopy studies of glutamate-related abnormalities in mood disorders. Biol Psychiatry. 2010;68(9):785–94.
Yung WK, Albright RE, Olson J, Fredericks R, Fink K, Prados MD, Brada M, Spence A, Hohl RJ, Shapiro W, Glantz M, Greenberg H, Selker RG, Vick NA, Rampling R, Friedman H, Phillips P, Bruner J, Yue N, Osoba D, Zaknoen S, Levin VA. A phase II study of temozolomide vs. procarbazine in patients with glioblastoma multiforme at first relapse. Br J Cancer. 2000;83(5):588–93.
Zhang J, Narr KL, Woods RP, Phillips OR, Alger JR, Espinoza RT. Glutamate normalization with ECT treatment response in major depression. Mol Psychiatry. 2013;18(3):268–70.
Acknowledgements
The authors have no disclosure. This work was supported by National Institute of Mental Health (NIMH) MH084060 (ES) and MH077159 (ES) grants. The funding agency had no role in the study design, data collection and analysis, decision to publish, and preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
French, B., Seney, M., Sibille, E. (2014). Altered GABA function in Major Depression. In: Popoli, M., Diamond, D., Sanacora, G. (eds) Synaptic Stress and Pathogenesis of Neuropsychiatric Disorders. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1056-4_13
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1056-4_13
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1055-7
Online ISBN: 978-1-4939-1056-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)