Abstract
In pregnancy fetal growth and development occur in a sexually dimorphic manner. Male and female fetuses respond differently to the intrauterine environment with males disproportionately suffering from perinatal morbidity and mortality. We have demonstrated placental dysfunction and sexually dimorphic responses in pregnancies complicated by severe preeclampsia. Production of cytokines and apoptosis in the male placenta is heightened relative to that of the female placenta. We also find increased expression and stabilization and a sexual dimorphism in expression of the transcription factor HIF-1α, but a defect in binding to the hypoxia response element with corresponding reduced expression of HIF-1α target genes including VEGF and Glut-1. HIF-1α is involved in crosstalk with the redox sensitive transcription factor NFκB in regulation by cytokines, reactive oxygen species and expression of inflammatory genes. We find increased placental expression and DNA binding of NFκB and a sexually dimorphic response suggesting a role for NFκB in placental dysfunction with preeclampsia. Placental mitochondrial complex III activity and complex I and IV expression are reduced and alterations in mitochondrial morphology are found in preeclampsia and are linked to the hypoxamir miR-210. We propose that with severe PE placental HIF-1α is stabilized by excessive ROS, inflammation and relative hypoxia. This increases the expression of miR-210 in the placenta causing repression of mitochondria-associated target genes, potentially leading to mitochondrial and placental dysfunction. This placental dysfunction may lead to a fetal programming effect that results in disease in later life.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The syndrome of preeclampsia (PE) is defined by hypertension and significant proteinuria developed at or after 20 weeks of gestation in previously normotensive women and which resolves postpartum [1]. It is a multisystem disorder, which complicates 5–8 % of pregnancies worldwide [2] and is associated with significant fetal and maternal morbidity and mortality. Severe PE is associated with fetal growth restriction, indicating placental dysfunction, and with preterm birth and perinatal death. Several mechanisms have been suggested to play a role in the pathogenesis of PE including an abnormal immune response, defective placentation, relative placental hypoxia or ischemia and oxidative/nitrative stress [3]. This leads to an exaggerated maternal inflammatory response [4] and generalized maternal endothelial cell activation, the causes of which are still uncertain but thought to be triggered by angiogenic or other factors released from the placenta [5] that damage the maternal endothelium [6, 7]. In particular, our studies have focused on the effect of preeclampsia on placental function as a mediator of fetal programming. Recently, developmental programming of cardiovascular disease, potentially mediated by placental dysfunction, has been suggested to occur in offspring of preeclamptic women [8–10]. We summarize our recent studies on placental function in PE, revealing a sexually dimorphic effect on inflammation and apoptosis and the novel role of micro RNA’s in regulation of placental mitochondrial function.
2 Sexual Dimorphism in Pregnancy
In “normal” pregnancy and development fetal growth occurs in is a sexually dimorphic manner with the male and female fetus responding differently to the intrauterine environment. Male fetuses grow faster and are usually larger than females [11]. However, a male fetus is more at a risk of poor outcome than the female fetus in association with placental insufficiency, PE, infection, IUGR, preterm delivery [11] and more late stillbirths associated with pre-gestational diabetes [12]. A Norwegian population-based study of 1.7 million singleton births clearly identified that preterm delivery and perinatal mortality and morbidity are dominated by the male sex [13]. While some reports suggest that PE is more prevalent with male fetuses [14], the Norwegian study shows an increased incidence of PE at <37 weeks gestation with a female fetus, but which may reflect the fact that male fetuses are delivered earlier due to other problems [15] and may not therefore stay in utero to allow the mother to develop PE. Sex specific adaptation of the placenta may be central to the differences seen in fetal growth and survival. Male fetuses reputedly try to maximize growth in utero, a strategy that places them at risk in an adverse environment [12] and may lead to increased incidence of adverse perinatal outcomes, including preterm birth, placenta previa, premature lung development; in contrast, females were shown to be more sensitive to maternal asthma [16–19]. Females, however, may adapt to the adverse intrauterine environment in an attempt to survive further maternal insults and ensure survival. The female neonate can more readily adapt to ex utero life even when delivered in a highly immature state at mid gestation, an effect possibly mediated by in utero adaptations to an adverse environment prior to delivery [20]. This may then relate to their risk of developing disease in adult life where differences in incidence to various diseases are clearly documented. The sex of the fetus also seems to be able to affect maternal physiology, an effect potentially mediated via the placenta. The male fetus is associated with a more vasoconstricted state in the maternal microcirculation and greater endothelial dysfunction of preeclamptic women compared to those with female fetus [18].
3 Role of the Placenta in Sexually Dimorphic Events in the Fetus
What underlies the sexual dimorphism in fetal growth and development and response to an adverse intrauterine environment? The placenta functions as a key regulator of fetal growth and development by facilitating nutrient supply to and waste removal from the fetus and secretion of peptide and steroid hormones that regulate fetal growth and development. Alterations in placental function have the ability to mediate fetal programming [21, 22]. There is burgeoning evidence that these roles of the placenta can be regulated in a sexually dimorphic manner. Microarray analysis has shown distinct sexually dimorphic differences in gene expression in the human placenta. In particular immune genes were expressed at higher level in female placenta compared to male [23]. Expression of 59 genes were changed in the placenta of women with asthma vs. no asthma with a female fetus compared to only 6 genes changed in those with asthma but a male fetus [24]. Hence gene expression in the placenta also responds to maternal inflammatory status in sex-dependent manner [24–27] with differences seen in placental cytokine expression, insulin-like growth factor pathways and the placental response to cortisol in relation to an adverse maternal condition (asthma). Changes in diet also provide distinctive signature of sexually dimorphic genes in placenta with expression generally higher in genes in female than male placentas [28]. Yeganegi et al. have shown that male placenta has higher TLR4 expression and a greater production of TNFα in response to LPS than the female placenta, which may underlie the propensity to preterm birth in males [29]. The mechanisms underlying such changes remain unknown; but evidence from other complicated pregnancies links sex differences to gonadal steroids. Immune function in adults is known to be regulated in a sex-specific manner as determined by differential effects of estrogen and testosterone [30]. There have been reports that women with PE have increased plasma testosterone levels compared to those of healthy pregnant women, with significantly higher levels in male- than in female-bearing preeclamptic pregnancies [31–34]. At the same time, the placental levels of aromatase, a rate-limiting enzyme converting androgens to estrogens, varied depending on fetal sex: it was much higher in the preeclamptic placentas with female than male fetuses [35]. Aromatase can be downregulated by TNFα, hypoxia, insulin and leptin, which mirror the actual conditions of the placenta in the context of maternal obesity [33, 36–38].
4 Sexual Dimorphism in the Placenta with Preeclampsia
We have reported elevated levels of TNF-a, IL-6 and IL-8 in preeclamptic placentae compared to normotensive controls, and a sexual dimorphism in expression of cytokines with male preeclamptic placenta showing much higher levels of cytokines than female preeclamptic placentas [39] (Fig. 12.1). Reinforcing our previous work showing increased placental oxidative and nitrative stress during PE and significant alterations in antioxidant defenses [40] we found significant increases in ROS levels defined by DCF staining in placenta from preeclamptic compared to normotensive pregnancies [41]. Oxygen tension has a major role in placental development [42] and human cytotrophoblast proliferation [43]. The transcription factor hypoxia-inducible factor-1α (HIF), which is expressed in the villous cytotrophoblast and decreases with gestational age in normal pregnancies [44], plays a role in the regulation of trophoblast function [45]. Hypoxia is reported to stimulate expression of a number of angiogenic proteins including endothelin, VEGF and Flt-1 [46] possibly via the action of HIF-1α [47]. Increased placental HIF-1α has been previously observed in pregnancies complicated by PE [48, 49], however, a defect in the oxygen sensing mechanism was also seen in early onset PE such that HIF-1α was not responsive to hypoxia [49].
Production of cytokines and chemokines by male and female placentas of normotensive and preeclamptic pregnancies. (a) TNFa, (b) IL-8 and. (c) IL-6 levels in CTRL and PE placentas. N = 5 in each group. *p < 0.05 vs. FCTRL and MCTRL. #p < 0.05 compared to FPE. Reproduced from Muralimanoharan et al. [39] with permission from Elsevier
We recently found increased placental HIF-1α protein levels with severe PE at term, but no change in HIF-1α mRNA [41] indicating that HIF-1α protein is stabilized. In addition to hypoxia, inflammatory cytokines, estrogen and reactive oxygen species (ROS) stabilize HIF-1α during normoxia in a number of tissue types including placenta [50]. Hence the increased ROS may be responsible for the stabilization of otherwise short lived HIF-1α in placenta seen during PE [50]. HIF-1α is thought to bind to the consensus HRE and activates transcription of downstream targets such as VEGF and GLUT-1. However, in the placenta with severe PE we found low binding of HIF-1α to the HRE and thus significantly lower levels of VEGF and GLUT-1 mRNA levels with PE compared to normotensive controls [41]. This aberrant response of placental cells to a hypoxic or inflammatory insult may lead to tissue damage underlying the pathology observed in PE. We also revealed a sexually dimorphic effect as we have recently shown that levels of HIF-1α were significantly higher in male preeclamptic placentas compared to both female preeclamptics and to normotensive male and female controls (Fig. 12.2). VEGF protein levels were significantly lower in preeclamptic placenta and still lower in male preeclamptic compared to female [39].
Expression of HIF-1a and VEGF in the placental villous tissue of normotensive and preeclamptic pregnancies. (a) Representative Western blots showing expression of HIF-1a and VEGF. Actin expression was used as loading control. (b) Scatter plot showing the quantification of HIF-1a and VEGF. N = 5 in each group. *p < 0.05 compared to FCTRL and MCTRL. #p < 0.05 compared to FPE. Reproduced from Muralimanoharan et al. [39] with permission from Elsevier
Increased trophoblast apoptosis has been observed in placentas from pregnancies complicated by PE and thought to contribute to the pathogenesis of this condition [51]. Early studies found no difference in Bcl-2, Bcl-xL, Bax and Bak expression in placental villi of preeclamptic vs. normotensive placentas [52], but others reported the expression of Bcl-2 to be less abundant in syncytiotrophoblast from severe preeclamptic placentas [53]. The increased trophoblast apoptosis with PE is thought to be the result of placental oxidative stress, in part triggered by hypoxia [54] which decreases expression of Bcl-2 (anti-apoptotic) while increasing the expression of p53 and Bax (pro-apoptotic) [55]. We observed an increase in apoptosis in preeclamptic placenta, which was significantly greater in the placentas of males compared to females, again indicating sexual dimorphism [39]. The increased expression of the apoptotic proteins p53 and p53 upregulated modulator of apoptosis (PUMA), as well as Bax, activated caspase-3 and caspase-9 together with significantly lower expression of Bcl-2 in preeclamptic placentas are consistent with the increased apoptosis. In addition, we have found that PUMA, Bax and Bcl-2 were changed in a fetal sex-dependent manner with significantly greater expression in the male preeclamptic placenta [39].
There is a growing body of evidence that HIF-1α can also be activated through inflammation-related factors that include cytokines (IL-1b and TNFα) with NFκB as the key link that drives cytokine cellular signaling [56]. There is a crosstalk between hypoxia and inflammation in placenta: HIF-1α activates NFκB [57], NFκB controls HIF-1α transcription [57], and HIF-1α activation may be concurrent with inhibition of NFκB [58]. NFκB is a redox-sensitive transcription factor regulating a battery of inflammatory genes, and has a variety of different effects in numerous pathological states [59]. In most cells, NFκB is found in the cytoplasm in its inactive form, bound to inhibitory proteins. Many extracellular stimuli, including bacterial lipopolysaccharide, viruses, oxidants, inflammatory cytokines, and immune stimuli, can activate NFκB. Once activated, it binds to regulatory DNA elements in the promoter regions of inflammatory and immune response genes, such as those encoding pro-inflammatory cytokines, chemokines, enzymes relevant for inflammation, and adhesion molecules [60]. Vaughan and Walsh reported a marked increase in NFκB activity in preeclamptic placentas as well as in cultured trophoblasts exposed to either hypoxia or inflammation or both [61].
In addition to sexual dimorphism in pro-inflammatory cytokine production and apoptosis in the placenta with PE [39], we also found an increase in the expression and binding activity of NFκB p65 in the preeclamptic placentas compared to CTRL with much higher levels in male preeclamptic compared to female (Fig. 12.3). This may suggest that increased inflammatory and trophoblast cell death observed in the placenta of preeclamptic pregnancies are, at least partially, induced by NFκB p65, further emphasizing the role of inflammation in the etiology of PE. Further studies are required to understand the mechanism(s) underlying the sexual dimorphism in inflammatory responses and the involvement of NFκB.
NFkB p65 expression and binding to DNA in placentas from normotensive and preeclamptic pregnancies. (a) Representative Western blots and (b) quantification bars showing expression of NFkB p65 expression in nuclear fraction of CTRL and PE villous tissue. Expression of histone H3 was used as loading control. (c) EMSA showing binding of nuclear protein extract to the consensus DNA binding site of p65. N = 5 in each group. *p < 0.05 compared to FCTRL and MCTRL. #p < 0.05 compared to FPE. Reproduced from Muralimanoharan et al. [39] with permission from Elsevier
5 Inflammation, Oxidative Stress and Mitochondrial Function
The inflammation and oxidative stress of normal pregnancy are heightened in PE [62] with placental mitochondria, an important source of reactive oxygen species (ROS), contributing to generation of oxidative stress [63]. Mitochondria are the major oxygen consuming organelles, play a crucial role in sensing the cellular oxygen concentration [64] and are the main source of endogenous ROS in most mammalian cell types [65]. Of the oxygen consumed by mitochondria, up to 5 % is converted to ROS as byproducts of oxidation-reduction reactions in the respiratory chain. When dysfunctional, mitochondria generate excessive amounts of ROS which may be involved in the triggering of PE and IUGR [66, 67]. Obesity, a major health issue in both the developed world and in developing countries [68], is associated with increased morbidity in pregnancy per se, but is also associated with programming of offspring for disease in adult life [69]. Obesity increases the risk of development of PE, thought to be due to the pre-existing low grade inflammation and oxidative stress of obesity [70]. An increase in reactive oxygen species (ROS) and reduction in the oxidative capacity of brown adipocytes results in impaired thermogenesis, and has been linked to diet-induced obesity [71]. Wilson-Fritch et al. demonstrated down-regulation of approximately 50 % of gene transcripts encoding mitochondrial proteins in adipose tissue in a rodent model with the onset of obesity [72]. In adults, obesity is associated with compromised mitochondrial function [73] suggesting this may be a mechanism linking obesity to PE.
Mitochondrial oxidative phosphorylation is a key energy source for placental function [74]. Several studies have shown that the increasing metabolic activity of placental mitochondria results in excessive production of ROS leading to oxidative stress, which may be exaggerated in pregnancies complicated by PE, IUGR and maternal obesity [75–80]. Thus, mitochondrial abnormalities and ROS formation could be part of a vicious cycle and represent a central mechanism of placental dysfunction in these disease states. Mitochondrial function in other metabolic tissues (e.g., liver, heart and brain) appears to be regulated by sex hormones [81–85]. The involvement of placental mitochondrial dysfunction in the pathogenesis of PE has been described in patients with mitochondrial disorder patients [67] and since reinforced [86], the exact mechanism remains unclear.
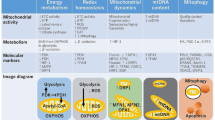
Mitochondria exist as dynamic networks and alterations in mitochondrial morphology during apoptotic cell death, fragmentation of the network and the remodeling of the cristae have been reported [87, 88]. We have reported significant morphological abnormalities at the ultrastructural level, together with reduction in complex III activity and reduction in the protein expression of complexes I and IV in the preeclamptic placentas [41] (Fig. 12.4). Reduction in complex activity suggests altered electron flow through complex III and perhaps damage to other complexes, which may contribute to an increase in ROS production. The scope and nature of the decreased activity in complex III in PE remains to be defined.
Mitochondrial dysfunction in preeclampsia. (a) Electron micrograph illustrating the morphological changes in the mitochondria of control and preeclamptic placenta (magnification = 50,000). Hash indicates mitochondrial swelling and broken cristae in placentas from PE and asterisk showing intact mitochondria form CTRL placenta. (b) Mitochondrial complex activity measured calorimetrically in the isolated mitochondria from flash frozen villous tissue of control and preeclampsia. (c) Immunoblots showing expression of mitochondrial complex proteins. VDAC was used as loading control. (d) Band intensity of the mitochondrial complexes is normalized to the intensity of VDAC Values shown are mean ± SEM, *p < 0.05 vs. control, (n = 6 each group). Reproduced from Muralimanoharan et al. [41] with permission from Elsevier
6 MicroRNA and Placental Function
Regulation of cell proliferation, mitochondrial metabolism, oxygen sensing and apoptosis in placenta has been recently found to be regulated by small (22 nucleotide) non-coding RNAs-microRNAs (miRNAs) [89]. MiRNAs are highly conserved, regulatory molecules that play an important role in the post-transcriptional regulation of gene expression by promoting RNA instability or translational inhibition [90]. Enquobahrie et al. [91] have shown eight differentially expressed placental miRNAs in pregnancies complicated by PE with miR-34C, 139 and 328 being downregulated and miR-210 upregulated [91]. Upregulation of placental miR-210 has been also described in preterm and severe PE [92–96]. Zhang et al. found that elevated miR-210 during PE suppresses trophoblast cell migration and invasion by targeting Homeobox-A9 (HOXA9) and Ephrin-A3 (EFNA3) [97]. MiR-210 is known to be involved in the hypoxic response and has been shown to be over-expressed in a HIF-1α-dependent manner in many types of tumors. It is purported to be involved in the shift of tumor metabolism from oxidative phosphorylation to glycolysis (Warburg effect) [98]. In addition, a mechanistic link between miR-210, HIF-1α, mitochondria-associated target proteins, and mitochondrial function has been identified in cancer cells [99, 100]. MiRNAs are now recognized as essential mediators of numerous cellular processes [101] with a number of hypoxia-related miRNAs (hypoxamirs) such as miR-23, miR-24, miR-26, miR-107 and miR-210 being identified that display significant upregulation in hypoxia [102]. MiR-210 expression is under direct control of HIF-1α and is downregulated in HIF-1α knockout cell lines [103] and is robustly induced in the hypoxic state in several tissues [104]. Interestingly miR-210 is involved in mitochondrial dysfunction in various types of cancer [105] with miR-210 delivery under normal oxygen conditions being able to inhibit mitochondrial energy production, impair oxygen consumption [106], induce lactate accumulation [99, 100], alter mitochondrial membrane potential and disrupt mitochondrial structure in cancer cells [107].
7 miR-210 and Placental Mitochondrial Function
We recently tested the hypothesis that mitochondrial dysfunction seen in the placenta of pregnancies complicated by PE is mediated by over-expression of miR-210. We observed a twofold increase in the expression of miR-210 during PE and strong correlation between miR-210 expression and hypoxic markers in our patient cohort [41], confirming that miR-210 expression was likely driven by hypoxia in vivo, as previously shown in other solid tumors.
We subsequently searched for targets of miR-210 involved in mitochondrial function. MiR-210 targets ISCU in trophoblast cell lines [93] possibly by targeting the transcript coding for ISCU, which facilitate the assembly of iron–sulfur clusters that are incorporated into enzymes involved in energy production, including mitochondrial respiratory complexes [106]. ISCU are a prosthetic group that promotes electron transport and oxidation-reduction in mitochondria cluster assembly protein [108]. Reduced expression of ISCU mediated by miR-210 contribute to a decrease in the activity of the TCA cycle (through aconitase targeting) and the electron transport chain (through complex I destabilization) [106]. Mir-210 regulates the expression of ISCU, a key factor in the assembly of Fe-S cluster subunits of complexes I, II and III in the mitochondria of cancer cells [100]. Indeed we found a reduction in placental ISCU mRNA expression during severe preeclampsia (Fig. 12.5). Repression of ISCU by miR-210 could alter the stoichiometry and function of complexes in electron transport and oxygen consumption leading to an increase in ROS production and decreased protein expression of complex I and activity of complex III as corroborated by our data.
Expression of miRs and target gene in villous tissue. (a) Expression of miR-34C (b) miR139, (c) miR-328 (d) miR-210, normalized to U18. (e) mRNA expression of ISCU normalized to18SRNA measured in the villous tissue of control pregnancies and those complicated by preeclampsia. Values shown are mean ± SEM, *p < 0.05 vs. control, (n = 6 each group). Reproduced from Muralimanoharan et al. [41] with permission from Elsevier
To explore the role of miR-210 in placental mitochondrial respiration we conducted gain- and loss-of-function experiments using cultured primary trophoblast. Mitochondrial function of isolated trophoblast was determined by extracellular flux measurements, sequentially adding pharmacological inhibitors of the respiratory chain similar to previous approaches [109]. Over-expression of miR-210 caused a 50 % reduction in maximum respiration and 60 % reduction in reserve (spare) capacity of trophoblast cells [41]. Furthermore, miR-210 inhibition rescued the mitochondrial respiration in the presence of Deferoxamine (DFO) which chemically simulates hypoxia. When cells are subjected to stress, mitochondria are capable of drawing upon their reserve capacity to serve the increasing energy demands for maintenance of organ function, cellular repair or ROS detoxification [110]. This suggests that mir-210 acts to regulate mitochondrial function during hypoxia to prevent the cells depleting their spare capacity in order to preserve ATP production. We propose that short-term hypoxia treatment does not alter cellular ATP production, since we did not find a significant effect on the ATP coupled respiration. However, long-term hypoxia or continuous cycles of ischemia/reoxygenation may result in further depletion of mitochondrial spare capacity and an inability of the cells to maintain ATP production resulting in excessive ROS production and increase in mitochondrial damage. Based on our in vivo and in vitro functional studies, we suggest that miR-210 exerts a major influence on placental mitochondrial function during PE.
8 Summary
We have demonstrated placental dysfunction in pregnancies complicated by severe preeclampsia and clearly show sexually dimorphic responses, with the response of the male placenta being heightened relative to that of the female placenta, both in production of cytokines and in apoptotic responses. We also show increased expression and stabilization of the transcription factor HIF-1α, together with a sexual dimorphism in HIF-1α expression but a defect in binding to the hypoxia response element and corresponding reduced expression of HIF-1α target genes including VEGF and Glut-1. HIF-1α is involved in crosstalk with the redox sensitive transcription factor NFκB in regards to their regulation by cytokines, reactive oxygen species and their effect on expression of inflammatory genes. We find increased expression and DNA binding of NFκB with preeclampsia and again a sexually dimorphic response. This perhaps underlies a role for NFκB in placental dysfunction with preeclampsia. We also find mitochondrial dysfunction in preeclampsia, evidenced by reductions in complex III activity and complex I and IV expression and alterations in mitochondrial morphology. We have also demonstrated a link between the increases in the hypoxamir miR-210 and placental mitochondrial dysfunction in preeclampsia and have identified the mitochondrial targets of miR-210 as ISCU.
Thus, we propose a model that with severe PE placental HIF-1α is stabilized by different factors including excessive production of ROS, inflammation and relative hypoxia. This, in turn, increases the expression of miR-210 in the placenta causing repression of mitochondria—associated target genes, potentially leading to mitochondrial and placental dysfunction. This placental dysfunction may lead to a fetal programming effect that results in disease in later life.
References
Vitoratos N, Vrachnis N, Iavazzo C, Kyrgiou M. Preeclampsia: molecular mechanisms, predisposition, and treatment. J Pregnancy. 2012;2012:145487.
Hogberg U. The World Health Report 2005: “make every mother and child count”—including Africans. Scand J Public Health. 2005;33:409–11.
Myatt L, Miodovnik M. Prediction of preeclampsia. Semin Perinatol. 1999;23:45–57.
Redman CW, Sargent IL. Preeclampsia and the systemic inflammatory response. Semin Nephrol. 2004;24:565–70.
Staff AC, Benton SJ, von Dadelszen P, Roberts JM, Taylor RN, Powers RW, et al. Redefining preeclampsia using placenta-derived biomarkers. Hypertension. 2013;61:932–42.
Myatt L. Role of placenta in preeclampsia. Endocrine. 2002;19:103–11.
Rampersad R, Nelson DM. Trophoblast biology, responses to hypoxia and placental dysfunction in preeclampsia. Front Biosci. 2007;12:2447–56.
Fugelseth D, Ramstad HB, Kvehaugen AS, Nestaas E, Stoylen A, Staff AC. Myocardial function in offspring 5–8 years after pregnancy complicated by preeclampsia. Early Hum Dev. 2011;87:531–5.
Jayet PY, Rimoldi SF, Stuber T, Salmon CS, Hutter D, Rexhaj E, et al. Pulmonary and systemic vascular dysfunction in young offspring of mothers with preeclampsia. Circulation. 2010;122:488–94.
Lazdam M, de la Horra A, Diesch J, Kenworthy Y, Davis E, Lewandowski AJ, et al. Unique blood pressure characteristics in mother and offspring after early onset preeclampsia. Hypertension. 2012;60:1338–45.
Clifton VL. Review: sex and the human placenta: mediating differential strategies of fetal growth and survival. Placenta. 2010;31(Suppl):S33–9.
Eriksson JG, Kajantie E, Osmond C, Thornburg K, Barker DJ. Boys live dangerously in the womb. Am J Hum Biol. 2010;22:330–5.
Vatten LJ, Skjaerven R. Offspring sex and pregnancy outcome by length of gestation. Early Hum Dev. 2004;76:47–54.
Makhseed M, Musini VM, Ahmed MA. Association of fetal gender with pregnancy-induced hypertension and pre-eclampsia. Int J Gynaecol Obstet. 1998;63:55–6.
Challis J, Newnham J, Petraglia F, Yeganegi M, Bocking A. Fetal sex and preterm birth. Placenta. 2013;34:95–9.
Murphy VE, Gibson PG, Giles WB, Zakar T, Smith R, Bisits AM, et al. Maternal asthma is associated with reduced female fetal growth. Am J Respir Crit Care Med. 2003;168:1317–23.
Murphy VE, Gibson P, Talbot PI, Clifton VL. Severe asthma exacerbations during pregnancy. Obstet Gynecol. 2005;106:1046–54.
Stark MJ, Dierkx L, Clifton VL, Wright IMR. Alterations in the maternal peripheral microvascular response in pregnancies complicated by preeclampsia and the impact of fetal sex. J Soc Gynecol Investig. 2006;13:573–8.
Stark MJ, Clifton VL, Wright IMR. Sex-specific differences in peripheral microvascular blood flow in preterm infants. Pediatr Res. 2008;63:415–9.
Stark MJ, Wright IM, Clifton VL. Sex-specific alterations in placental 11beta-hydroxysteroid dehydrogenase 2 activity and early postnatal clinical course following antenatal betamethasone. Am J Physiol Regul Integr Comp Physiol. 2009;297:R510–4.
Wu G, Imhoff-Kunsch B, Girard AW. Biological mechanisms for nutritional regulation of maternal health and fetal development. Paediatr Perinat Epidemiol. 2012;26 Suppl 1:4–26.
Myatt L. Placental adaptive responses and fetal programming. J Physiol. 2006;572:25–30.
Sood R, Zehnder JL, Druzin ML, Brown PO. Gene expression patterns in human placenta. Proc Natl Acad Sci U S A. 2006;103:5478–83.
Osei-Kumah A, Smith R, Jurisica I, Caniggia I, Clifton VL. Sex-specific differences in placental global gene expression in pregnancies complicated by asthma. Placenta. 2011;32:570–8.
Scott NM, Hodyl NA, Murphy VE, Osei-Kumah A, Wyper H, Hodgson DM, et al. Placental cytokine expression covaries with maternal asthma severity and fetal sex. J Immunol. 2009;182:1411–20.
Prescott SL, Clifton V. Asthma and pregnancy: emerging evidence of epigenetic interactions in utero. Curr Opin Allergy Clin Immunol. 2009;9:417–26.
Clifton VL. Sexually dimorphic effects of maternal asthma during pregnancy on placental glucocorticoid metabolism and fetal growth. Cell Tissue Res. 2005;322:63–71.
Mao J, Zhang X, Sieli PT, Falduto MT, Torres KE, Rosenfeld CS. Contrasting effects of different maternal diets on sexually dimorphic gene expression in the murine placenta. Proc Natl Acad Sci U S A. 2010;107:5557–62.
Yeganegi M, Leung CG, Martins A, Kim SO, Reid G, Challis JR, et al. Lactobacillus rhamnosus GR-1 stimulates colony-stimulating factor 3 (granulocyte) (CSF3) output in placental trophoblast cells in a fetal sex-dependent manner. Biol Reprod. 2011;84:18–25.
Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8:737–44.
Steier JA, Ulstein M, Myking OL. Human chorionic gonadotropin and testosterone in normal and preeclamptic pregnancies in relation to fetal sex. Obstet Gynecol. 2002;100:552–6.
Laivuori H, Kaaja R, Rutanen EM, Viinikka L, Ylikorkala O. Evidence of high circulating testosterone in women with prior preeclampsia. J Clin Endocrinol Metab. 1998;83:344–7.
Acromite MT, Mantzoros CS, Leach RE, Hurwitz J, Dorey LG. Androgens in preeclampsia. Am J Obstet Gynecol. 1999;180:60–3.
Salamalekis E, Bakas P, Vitoratos N, Eleptheriadis M, Creatsas G. Androgen levels in the third trimester of pregnancy in patients with preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2006;126:16–9.
Sathishkumar K, Balakrishnan M, Chinnathambi V, Chauhan M, Hankins GD, Yallampalli C. Fetal sex-related dysregulation in testosterone production and their receptor expression in the human placenta with preeclampsia. J Perinatol. 2012;32:328–35.
Diaz L, Noyola-Martinez N, Barrera D, Hernandez G, Avila E, Halhali A, et al. Calcitriol inhibits TNF-alpha-induced inflammatory cytokines in human trophoblasts. J Reprod Immunol. 2009;81:17–24.
Jiang B, Kamat A, Mendelson CR. Hypoxia prevents induction of aromatase expression in human trophoblast cells in culture: potential inhibitory role of the hypoxia-inducible transcription factor Mash-2 (mammalian achaete-scute homologous protein-2). Mol Endocrinol. 2000;14:1661–73.
Christensen A, Froyshov D, Fylling P. Hormone and enzyme assays in pregnancy. IV. The human chorionic somatomammotrophin, placental cystine-aminopeptidase, progesterone and the urinary oestrogens in pregnancies complicated with essential hypertension, mild or severe pre-eclampsia. Acta Endocrinol (Copenh). 1974;77:344–55.
Muralimanoharan S, Maloyan A, Myatt L. Evidence of sexual dimorphism in the placental function with severe preeclampsia. Placenta. 2013;34:1183–9.
Myatt L, Eis AL, Brockman DE, Kossenjans W, Greer IA, Lyall F. Differential localization of superoxide dismutase isoforms in placental villous tissue of normotensive, pre-eclamptic, and intrauterine growth-restricted pregnancies. J Histochem Cytochem. 1997;45:1433–8.
Muralimanoharan S, Maloyan A, Mele J, Guo C, Myatt LG, Myatt L. MIR-210 modulates mitochondrial respiration in placenta with preeclampsia. Placenta. 2012;33:816–23.
Adelman DM, Gertsenstein M, Nagy A, Simon MC, Maltepe E. Placental cell fates are regulated in vivo by HIF-mediated hypoxia responses. Genes Dev. 2000;14:3191–203.
Genbacev O, Zhou Y, Ludlow JW, Fisher SJ. Regulation of human placental development by oxygen tension. Science. 1997;277:1669–72.
Caniggia I, Winter JL. Adriana and Luisa Castellucci Award lecture 2001. Hypoxia inducible factor-1: oxygen regulation of trophoblast differentiation in normal and pre-eclamptic pregnancies—a review. Placenta. 2002;23:S47–57.
Rajakumar A, Conrad KP. Expression, ontogeny, and regulation of hypoxia-inducible transcription factors in the human placenta. Biol Reprod. 2000;63:559–69.
Nevo O, Soleymanlou N, Wu Y, Xu J, Kingdom J, Many A, et al. Increased expression of sFlt-1 in in vivo and in vitro models of human placental hypoxia is mediated by HIF-1. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1085–93.
Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature. 1992;359:843–5.
Rajakumar A, Brandon HM, Daftary A, Ness R, Conrad KP. Evidence for the functional activity of hypoxia-inducible transcription factors overexpressed in preeclamptic placentae. Placenta. 2004;25:763–9.
Rolfo A, Many A, Racano A, Tal R, Tagliaferro A, Ietta F, et al. Abnormalities in oxygen sensing define early and late onset preeclampsia as distinct pathologies. PLoS One. 2010;5:e13288.
Patel J, Landers K, Mortimer RH, Richard K. Regulation of hypoxia inducible factors (HIF) in hypoxia and normoxia during placental development. Placenta. 2010;31:951–7.
DiFederico E, Genbacev O, Fisher SJ. Preeclampsia is associated with widespread apoptosis of placental cytotrophoblasts within the uterine wall. Am J Pathol. 1999;155:293–301.
Allaire AD, Ballenger KA, Wells SR, McMahon MJ, Lessey BA. Placental apoptosis in preeclampsia. Obstet Gynecol. 2000;96:271–6.
Ishihara N, Matsuo H, Murakoshi H, Laoag-Fernandez JB, Samoto T, Maruo T. Increased apoptosis in the syncytiotrophoblast in human term placentas complicated by either preeclampsia or intrauterine growth retardation. Am J Obstet Gynecol. 2002;186:158–66.
Kilani RT, Mackova M, Davidge ST, Guilbert LJ. Effect of oxygen levels in villous trophoblast apoptosis. Placenta. 2003;24:826–34.
Levy R, Smith SD, Chandler K, Sadovsky Y, Nelson DM. Apoptosis in human cultured trophoblasts is enhanced by hypoxia and diminished by epidermal growth factor. Am J Physiol Cell Physiol. 2000;278:C982–8.
Taylor CT, Cummins EP. The role of NF-kappaB in hypoxia-induced gene expression. Ann N Y Acad Sci. 2009;1177:178–84.
Gorlach A, Bonello S. The cross-talk between NF-kappaB and HIF-1: further evidence for a significant liaison. Biochem J. 2008;412:e17–9.
Carbia-Nagashima A, Gerez J, Perez-Castro C, Paez-Pereda M, Silberstein S, Stalla GK, et al. RSUME, a small RWD-containing protein, enhances SUMO conjugation and stabilizes HIF-1alpha during hypoxia. Cell. 2007;131:309–23.
Roebuck KA. Oxidant stress regulation of IL-8 and ICAM-1 gene expression: differential activation and binding of the transcription factors AP-1 and NF-kappaB (review). Int J Mol Med. 1999;4:223–30.
Matsushita H, Morishita R, Nata T, Aoki M, Nakagami H, Taniyama Y, et al. Hypoxia-induced endothelial apoptosis through nuclear factor-kappaB (NF-kappaB)-mediated bcl-2 suppression: in vivo evidence of the importance of NF-kappaB in endothelial cell regulation. Circ Res. 2000;86:974–81.
Vaughan JE, Walsh SW. Activation of NF-kappaB in placentas of women with preeclampsia. Hypertens Pregnancy. 2012;31:243–51.
Myatt L. Review: reactive oxygen and nitrogen species and functional adaptation of the placenta. Placenta. 2010;31(Suppl):S66–9.
Wang Y, Walsh SW. Increased superoxide generation is associated with decreased superoxide dismutase activity and mRNA expression in placental trophoblast cells in pre-eclampsia. Placenta. 2001;22:206–12.
Van Houten B, Woshner V, Santos JH. Role of mitochondrial DNA in toxic responses to oxidative stress. DNA Repair (Amst). 2006;5:145–52.
Lee H-C, Wei Y-H. Oxidative stress, mitochondrial DNA mutation, and apoptosis in aging. Exp Biol Med (Maywood). 2007;232:592–606.
Myatt L, Cui X. Oxidative stress in the placenta. Histochem Cell Biol. 2004;122:369–82.
Torbergsen T, Oian P, Mathiesen E, Borud O. Pre-eclampsia—a mitochondrial disease? Acta Obstet Gynecol Scand. 1989;68:145–8.
Yogev Y, Visser GH. Obesity, gestational diabetes and pregnancy outcome. Semin Fetal Neonatal Med. 2009;14:77–84.
Rogers LK, Velten M. Maternal inflammation, growth retardation, and preterm birth: insights into adult cardiovascular disease. Life Sci. 2011;89:417–21.
Zhu MJ, Du M, Nathanielsz PW, Ford SP. Maternal obesity up-regulates inflammatory signaling pathways and enhances cytokine expression in the mid-gestation sheep placenta. Placenta. 2010;31:387–91.
Feldmann HM, Golozoubova V, Cannon B, Nedergaard J. UCP1 ablation induces obesity and abolishes diet-induced thermogenesis in mice exempt from thermal stress by living at thermoneutrality. Cell Metab. 2009;9:203–9.
Wilson-Fritch L, Nicoloro S, Chouinard M, Lazar MA, Chui PC, Leszyk J, et al. Mitochondrial remodeling in adipose tissue associated with obesity and treatment with rosiglitazone. J Clin Invest. 2004;114:1281–9.
Boudina S, Sena S, O'Neill BT, Tathireddy P, Young ME, Abel ED. Reduced mitochondrial oxidative capacity and increased mitochondrial uncoupling impair myocardial energetics in obesity. Circulation. 2005;112:2686–95.
Bax BE, Bloxam DL. Energy metabolism and glycolysis in human placental trophoblast cells during differentiation. Biochim Biophys Acta. 1997;1319:283–92.
Llurba E, Gratacós E, Martín-Gallán P, Cabero L, Dominguez C. A comprehensive study of oxidative stress and antioxidant status in preeclampsia and normal pregnancy. Free Radic Biol Med. 2004;37:557–70.
Watson AL, Skepper JN, Jauniaux E, Burton GJ. Susceptibility of human placental syncytiotrophoblastic mitochondria to oxygen-mediated damage in relation to gestational age. J Clin Endocrinol Metab. 1998;83:1697–705.
Wang Y, Walsh SW. Placental mitochondria as a source of oxidative stress in pre-eclampsia. Placenta. 1998;19:581–6.
Lattuada D, Colleoni F, Martinelli A, Garretto A, Magni R, Radaelli T, et al. Higher mitochondrial DNA content in human IUGR placenta. Placenta. 2008;29:1029–33.
Valsamakis G, Kanaka-Gantenbein C, Malamitsi-Puchner A, Mastorakos G. Causes of intrauterine growth restriction and the postnatal development of the metabolic syndrome. Ann N Y Acad Sci. 2006;1092:138–47.
Poston L, Igosheva N, Mistry HD, Seed PT, Shennan AH, Rana S, et al. Role of oxidative stress and antioxidant supplementation in pregnancy disorders. Am J Clin Nutr. 2011;94(6 Suppl):1980S–5S.
Yan L, Ge H, Li H, Lieber SC, Natividad F, Resuello RRG, et al. Gender-specific proteomic alterations in glycolytic and mitochondrial pathways in aging monkey hearts. J Mol Cell Cardiol. 2004;37:921–9.
Justo R, Boada J, Frontera M, Oliver J, Bermúdez J, Gianotti M. Gender dimorphism in rat liver mitochondrial oxidative metabolism and biogenesis. Am J Physiol Cell Physiol. 2005;289:C372–8.
Arnold S, de Araújo GW, Beyer C. Gender-specific regulation of mitochondrial fusion and fission gene transcription and viability of cortical astrocytes by steroid hormones. J Mol Endocrinol. 2008;41:289–300.
Sanz A, Hiona A, Kujoth GC, Seo AY, Hofer T, Kouwenhoven E, et al. Evaluation of sex differences on mitochondrial bioenergetics and apoptosis in mice. Exp Gerontol. 2007;42:173–82.
Lagranha CJ, Deschamps A, Aponte A, Steenbergen C, Murphy E. Sex differences in the phosphorylation of mitochondrial proteins result in reduced production of reactive oxygen species and cardioprotection in females. Circ Res. 2010;106:1681–91.
Widschwendter M, Schrocksnadel H, Mortl MG. Pre-eclampsia: a disorder of placental mitochondria? Mol Med Today. 1998;4:286–91.
Bereiter-Hahn J, Voth M. Dynamics of mitochondria in living cells: shape changes, dislocations, fusion, and fission of mitochondria. Microsc Res Tech. 1994;27:198–219.
Karbowski M, Youle RJ. Dynamics of mitochondrial morphology in healthy cells and during apoptosis. Cell Death Differ. 2003;10:870–80.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136:215–33.
Inui M, Martello G, Piccolo S. MicroRNA control of signal transduction. Nat Rev Mol Cell Biol. 2010;11:252–63.
Enquobahrie DA, Abetew DF, Sorensen TK, Willoughby D, Chidambaram K, Williams MA. Placental microRNA expression in pregnancies complicated by preeclampsia. Am J Obstet Gynecol. 2011;204:178. e12–21.
Ishibashi O, Ohkuchi A, Ali MM, Kurashina R, Luo SS, Ishikawa T, et al. Hydroxysteroid (17-beta) dehydrogenase 1 is dysregulated by mir-210 and mir-518c that are aberrantly expressed in preeclamptic placentas: a novel marker for predicting preeclampsia. Hypertension. 2012;59:265–73.
Lee DC, Romero R, Kim JS, Tarca AL, Montenegro D, Pineles BL, et al. miR-210 targets iron-sulfur cluster scaffold homologue in human trophoblast cell lines: siderosis of interstitial trophoblasts as a novel pathology of preterm preeclampsia and small-for-gestational-age pregnancies. Am J Pathol. 2011;179:590–602.
Liu C, Zhou Y, Zhang Z. MiR-210: an important player in the pathogenesis of preeclampsia? J Cell Mol Med. 2012;16:943–4.
Pineles BL, Romero R, Montenegro D, Tarca AL, Han YM, Kim YM, et al. Distinct subsets of microRNAs are expressed differentially in the human placentas of patients with preeclampsia. Am J Obstet Gynecol. 2007;196:261. e1–6.
Zhu XM, Han T, Sargent IL, Yin GW, Yao YQ. Differential expression profile of microRNAs in human placentas from preeclamptic pregnancies vs normal pregnancies. Am J Obstet Gynecol. 2009;200:661. e1–7.
Zhang Y, Fei M, Xue G, Zhou Q, Jia Y, Li L, et al. Elevated levels of hypoxia-inducible microRNA-210 in pre-eclampsia: new insights into molecular mechanisms for the disease. J Cell Mol Med. 2012;16:249–59.
Huang X, Ding L, Bennewith KL, Tong RT, Welford SM, Ang KK, et al. Hypoxia-inducible mir-210 regulates normoxic gene expression involved in tumor initiation. Mol Cell. 2009;35:856–67.
Chen Z, Li Y, Zhang H, Huang P, Luthra R. Hypoxia-regulated microRNA-210 modulates mitochondrial function and decreases ISCU and COX10 expression. Oncogene. 2010;29:4362–8.
Favaro E, Ramachandran A, McCormick R, Gee H, Blancher C, Crosby M, et al. MicroRNA-210 regulates mitochondrial free radical response to hypoxia and krebs cycle in cancer cells by targeting iron sulfur cluster protein ISCU. PLoS One. 2010;5:e10345.
Ivan M, Harris AL, Martelli F, Kulshreshtha R. Hypoxia response and microRNAs: no longer two separate worlds. J Cell Mol Med. 2008;12:1426–31.
Kulshreshtha R, Ferracin M, Wojcik SE, Garzon R, Alder H, Agosto-Perez FJ, et al. A microRNA signature of hypoxia. Mol Cell Biol. 2007;27:1859–67.
Nakada C, Tsukamoto Y, Matsuura K, Nguyen TL, Hijiya N, Uchida T, et al. Overexpression of miR-210, a downstream target of HIF1alpha, causes centrosome amplification in renal carcinoma cells. J Pathol. 2011;224:280–8.
Chan YC, Banerjee J, Choi SY, Sen CK. miR-210: the master hypoxamir. Microcirculation. 2012;19:215–23.
Devlin C, Greco S, Martelli F, Ivan M. miR-210: more than a silent player in hypoxia. IUBMB Life. 2011;63:94–100.
Chan SY, Zhang YY, Hemann C, Mahoney CE, Zweier JL, Loscalzo J. MicroRNA-210 controls mitochondrial metabolism during hypoxia by repressing the iron-sulfur cluster assembly proteins ISCU1/2. Cell Metab. 2009;10:273–84.
Puissegur MP, Mazure NM, Bertero T, Pradelli L, Grosso S, Robbe-Sermesant K, et al. miR-210 is overexpressed in late stages of lung cancer and mediates mitochondrial alterations associated with modulation of HIF-1 activity. Cell Death Differ. 2011;18:465–78.
Harner M, Korner C, Walther D, Mokranjac D, Kaesmacher J, Welsch U, et al. The mitochondrial contact site complex, a determinant of mitochondrial architecture. EMBO J. 2011;30:4356–70.
Moran M, Rivera H, Sanchez-Arago M, Blazquez A, Merinero B, Ugalde C, et al. Mitochondrial bioenergetics and dynamics interplay in complex I-deficient fibroblasts. Biochim Biophys Acta. 1802;2010:443–53.
Dranka BP, Hill BG, Darley-Usmar VM. Mitochondrial reserve capacity in endothelial cells: the impact of nitric oxide and reactive oxygen species. Free Radic Biol Med. 2010;48:905–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this paper
Cite this paper
Myatt, L., Muralimanoharan, S., Maloyan, A. (2014). Effect of Preeclampsia on Placental Function: Influence of Sexual Dimorphism, microRNA’s and Mitochondria. In: Zhang, L., Ducsay, C. (eds) Advances in Fetal and Neonatal Physiology. Advances in Experimental Medicine and Biology, vol 814. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1031-1_12
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1031-1_12
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1030-4
Online ISBN: 978-1-4939-1031-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)