Abstract
Despite advances in supportive care for patients with acute necrotizing pancreatitis, the majority of patients who die succumb to infectious complications often late (2–4 weeks) in the disease process. Research completed over the past two decades has improved our understanding of infectious complications in patients with acute pancreatitis. Patients with acute necrotizing pancreatitis are at the greatest risk of developing an infection with bacteria translocated from the bowel lumen into the necrotic pancreatic tissue. The most effective antimicrobial agents are the fluoroquinolones and carbapenems, which achieve optimal pancreatic tissue penetration and inhibit the growth of enteric bacteria present in pancreatic infection juice and necrotic tissue. The role of antibiotics in reducing infectious morbidity and mortality has been debated for decades, but current evidence does not support the use of prophylactic antibiotics for the prevention of infection of sterile necrosis. In cases of suspected infected pancreatic necrosis (IPN), antibiotic therapy should be initiated while the source of the infection is being investigated. If no source of infection is identified, antibiotics should be discontinued. Recent evidence suggests a select group of patients with IPN can be managed by antibiotics alone without requiring percutaneous drainage or necrosectomy. However, if these patients deteriorate clinically, more aggressive therapy is warranted.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute Pancreatitis
- Clostridium Difficile Infection
- Pancreatic Tissue
- Severe Acute Pancreatitis
- Bacterial Translocation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Acute pancreatitis is a condition involving acute inflammation of the pancreas that results in considerable morbidity and 10–40 % mortality [1]. There are two major forms of acute pancreatitis: interstitial (about 80 % of cases) and necrotizing (about 20 %). Acute necrotizing pancreatitis usually runs a severe course and can be sterile or infected. Although patients with sterile pancreatic necrosis may have a severe course and die, infection of the nonviable necrotic pancreatic tissue usually portends a worse prognosis. Previous studies have shown that the extent and infection of pancreatic necrosis correlate with the development of organ failure and mortality in acute pancreatitis [2, 3]. The incidence of infected pancreatic necrosis (IPN) in patients with necrotizing pancreatitis has remained stable (around 30 %) during the last two decades [4, 5]. The peak incidence of infected necrosis is between 2 and 4 weeks after onset of disease [6] and is the cause of most of the late mortality during the course of acute pancreatitis [7].
In addition to IPN, patients with acute pancreatitis may have extra pancreatic infectious complications such as pneumonia, cholangitis, bacteremia, and urinary tract infections that are often hospital-acquired. The early course of severe acute pancreatitis (SAP) may present with signs of systemic inflammatory response syndrome (SIRS): fever, leukocytosis, tachycardia, tachypnea and may be indistinguishable from infectious complications of pancreatitis or sepsis syndrome.
Given the poor prognosis of IPN, it would be helpful to be able to prevent it. Whether antibiotics can prevent IPN and can thus improve patient survival is controversial. In this chapter, we review the studies that have investigated which antibiotics penetrate sufficiently well into pancreatic necrosis and whether antibiotic treatment in patients with sterile and IPN is of clinical benefit.
Diagnosis of Infected Necrosis
The gold standard for the differentiation between interstitial pancreatitis and necrotizing pancreatitis remains contrast-enhanced computed tomography (CECT). See also Chap. 3. However, CECT is not always a helpful tool for diagnosing infection. Infected necrosis is typically suspected when there is persistent sepsis, new-onset sepsis, or progressive clinical deterioration (i.e., signs of sepsis) despite maximal support in the second phase of the disease, without another source of infection. A pathognomonic sign of infected necrosis is the presence of peripancreatic or intrapancreatic gas bubbles in a collection on CECT (Fig. 9.1), although this is present in only a minority of patients. Otherwise, there is no specific feature on CECT that is able to distinguish between infected or sterile necrosis. The gold standard for the detection of IPN is ultrasound-guided or CT-guided percutaneous aspiration of suspected pancreatic fluid collections with bacteriologic sampling (gram stain and cultures with sensitivity). The utility of this technique will be discussed later in this chapter.
A 67-year-old man admitted to the hospital with biliary pancreatitis. (a) Abdominal CT scan 2 weeks after presentation, based on pancreatic fluid collection a nasojejunal feeding tube was placed for enteral feeding. (b) Four weeks after initiation of jejunal feeding, patient called complaining of fever and diaphoresis for the past 2 days. Repeat CT scan revealed decreased size of the collection with extensive air bubbles (arrows). The patient was started on antibiotics and laparoscopically debrided
Epidemiology
The microbial pathogens that cause IPN in necrotizing pancreatitis are predominantly gut-derived, including Escherichia coli, Pseudomonas, Klebsiella, and Enterococcus. Approximately 75 % of infections are monomicrobial. Fungal infection and infection with gram-positive organisms are uncommon but occur more frequently in the setting of prophylactic antibiotic use for SAP, especially when used for more than 10–14 days. The incidence of fungal infections in necrotizing pancreatitis is approximately 9 %, and it is not clear if this is associated with higher mortality [8].
Pathogenesis
Various theories have been proposed as to how pancreatic necrosis becomes infected. First, previous studies in SAP have shown gut mucosal defenses against bacterial translocation become impaired [9, 10]. Second, disturbed gastrointestinal motility may lead to bacterial overgrowth and failure of the structural mucosal barrier, which may lead to increased gut permeability. These events may result in the process of bacterial translocation—bacteria cross the gastrointestinal mucosal barrier and invade the systemic compartment [11, 12]. Bacterial translocation is thought to be the mechanism causing most infections in acute pancreatitis. Therefore, antibiotics aimed at preventing bacterial translocation and subsequent infections have been widely studied over the last two decades.
Pancreatic Penetration of Antibiotics
Because of the consistency of pancreatic necrosis, few antibiotics are able to penetrate the dead pancreatic tissue when given intravenously. However, antibiotics that effectively penetrate viable but not necrotic pancreatic tissue may at least achieve high microbicidal levels in adjacent tissues [13–15]. In addition, high circulating levels may also prevent infection via hematogenous and lymphatic routes [16]. Whether there is a benefit to a specific class of antibiotics has been extensively studied. Multiple studies have evaluated the penetration of antibiotics in the human pancreas with variable results [17–29]. Most studies utilized a parenteral route of antibiotic administration, which seems appropriate for a patient with acute pancreatitis. Eight studies measured the presence and concentration of the antibiotic in pancreatic secretions, obtained either on endoscopic retrograde cholangiopancreatography (ERCP) or after stimulation via a pancreatic fistula [17–23]. In the remaining studies, antibiotic concentrations were measured in pseudocysts [29] and pancreatic tissue [28]. Tissue samples were obtained from patients with different pancreatic diseases and different degrees of inflammation (acute pancreatitis, chronic pancreatitis, pancreatic carcinoma). Human studies have shown that the antibiotic concentration depends on the degree of inflammation, with higher levels in acute pancreatitis compared with controls [26].
Based on these studies, it is possible to classify antibiotics into three groups with regard to their efficacy in the pancreas: Group A, substances with low tissue concentrations that were below the minimal inhibitory concentrations of most bacteria found in pancreatic infection (aminoglycosidase, netilmicin, tobramycin); Group B, antibiotics with pancreatic tissue concentrations that were sufficient to inhibit some, but not all, bacteria in pancreatic infection (mezclocillin, piperacillin, ceftizoxime, cefotaxime); and Group C, substances with high pancreatic tissue levels, as well as high bactericidal activity against most of the organisms present in pancreatic infection (ciprofloxacin, ofloxacin, imipenem-cilastatin).
Preventing Infection in Sterile Necrosis
Experimental Studies
Various experimental studies using different animal models have investigated the effect of prophylactic antibiotics for the prevention of pancreatic infection in acute pancreatitis. Using a perfusion model in cats, Widdison et al. [30] studied the effect of cefotaxime, administered 12 h after the induction of acute experimental pancreatitis. Their group found cefotaxime reached bactericidal levels in pancreatic tissue and juice and significantly prevented pancreatic infection. The effect of piperacillin given immediately after experimentally induced acute pancreatitis in rats was studied by Araida et al. [31] and found a positive effect both on the infection and survival rate. The effect of intravenously administered cefotaxime and imipenem plus the effect of complete gut decontamination in a duct hyperstimulation model in the rat was studied by Foitzik et al. [32]. Neither treatment had a positive effect on survival. Pancreatic bacterial counts, on the other hand, were significantly reduced by imipenem, but not by cefotaxime. A study from the same group [37] and identical model investigated the effect of imipenem and ciprofloxacin but increased the antibiotic treatment from 4 to 7 days. An increased survival rate was observed in this study possibly related to increased duration of therapy. Both antibiotics reduced early and late septic pancreatic complications.
Human Studies
Over the years, there has been controversy surrounding the use of antibiotics in pancreatic necrosis. Three randomized studies were published in the 1970s, in which ampicillin or a placebo was given to less than 200 patients who had acute pancreatitis (only 1 patient died and 26 had infectious complications) [33–35]. All studies showed ampicillin had no beneficial effect on the clinical course of the disease [33–35]. For many years, this conclusion led to the impression that antibiotic prophylaxis was of no benefit in pancreatitis. However, these studies had various limitations. First, ampicillin has a modest activity against Gram-negative microorganisms, which are common in pancreatic infection. Second, ampicillin achieves poor penetration in pancreatic tissue [36] and in pancreatic fluid [18]. Third, the severity of acute pancreatitis in these studies was low [33–35], resulting in insufficient statistical power [16].
Since the 1990s, there have been numerous prospective, randomized trials that have evaluated the use of prophylactic antibiotics in SAP. Unfortunately, the design, methodological quality, and most importantly, outcome of the included studies vary widely [37]. An attempt to summarize these studies in a systematic review (from 2006) concluded prophylactic antibiotics decreased mortality in severe pancreatitis, but not the rate of IPN [38].
However, more updated meta-analyses (from 2010) did not demonstrate a significant beneficial effect of antibiotic prophylaxis (except when imipenem was used) on infection of pancreatic necrosis and mortality [39, 40] with the number needed to treat of 1,429 for one patient to benefit [41]. It remains uncertain if a subgroup of patients with SAP (such as extensive necrosis with organ failure) may benefit from antibiotics, but large studies with sufficient statistical power required to determine whether any benefit exists will be difficult to perform.
Based on the current literature, use of prophylactic antibiotics to prevent infection in patients with sterile necrosis (even predicted as having severe disease) is not recommended. In addition, current guidelines do not recommend routine antibiotic prophylaxis [42, 43]. Overall, there has been a decrease in incidence of infected necrosis among patients even in the placebo arms of trials (15–20 % of cases with necrosis), consistent with findings from contemporary cohort studies [44]. Further casting doubt on the benefit of prophylactic antibiotics is recognition that it can be associated with the selection of resistant organisms and the development of fungal infection [45–47].
Prevention of Fungal Infections
Prevention of fungal infections in patients with sterile pancreatic necrosis is also not recommended. Although it was suggested that fungal infection may be a more common cause of mortality in acute pancreatitis, further study has not confirmed this finding [48]. It is unclear if the mere presence of candida within pancreatic necrosis indicates only colonization. Furthermore, candida infection may go unrecognized and untreated due to false negative microbiological sampling.
Gut Decontamination and Probiotics
There is one successful randomized controlled, clinical trial that used selective decontamination of the bowel, targeting both bacteria and fungi, in order to prevent infected necrosis [49]. Because of the decreased morbidity and mortality in this trial in patients with SAP who had undergone selective decontamination, further study in this area is needed. With regard to probiotics, they should not be given in SAP. Although earlier trials suggested a benefit, a very well-conducted, randomized controlled clinical trial demonstrated increased mortality [50]. This lack of benefit has also been shown in a recent meta-analysis [51].
Antimicrobial Therapy in Infected Necrosis
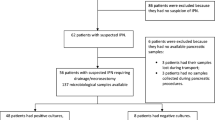
Rather than preventing infection, the role of antibiotics in patients with necrotizing pancreatitis is now to treat established infected necrosis, or to treat other hospital-acquired infections in these often critically ill patients. The dogma that IPN requires prompt surgical debridement has also been challenged by multiple reports and case series showing that antibiotics alone can lead to resolution of infection and, in select patients, avoid surgery altogether [52–55]. A study by Garg et al. reported 47/80 patients with infected necrosis over a 10-year period who were successfully treated conservatively with antibiotics alone [55]. The mortality in the conservative group was 23 % as compared with 54 % in the surgical group. The same group published a meta-analysis of eight studies involving 409 patients with infected necrosis of whom 324 were successfully treated with antibiotics alone [56]. Overall, 64 % of the patients with infected necrosis in this meta-analysis could be managed by conservative antibiotic treatment with 12 % mortality, and only 26 % underwent surgery. Thus, a select group of relatively stable patients with IPN can be managed by antibiotics alone, without requiring percutaneous drainage. However, it should be cautioned that these patients require close supervision and percutaneous or endoscopic necrosectomy should be considered if the patient fails to improve or deteriorates clinically. We suggest using imipenem or meropenem for patients with suspected infected necrosis based on their high pancreatic tissue levels and bactericidal activity against most of the organisms present in pancreatic infection. Whenever clinically feasible, radiological, endoscopic, and surgical interventions for infected necrosis are postponed until there is sufficient encapsulation and demarcation of the infected peripancreatic or pancreatic collections, generally 4 weeks after onset of symptoms [57]. A discussion of these interventions is given in other chapters.
Role of CT-Guided FNA
The technique of computed tomography-guided fine needle aspiration (CT FNA) has proven to be safe, effective, and accurate in distinguishing infected and sterile necrosis [43, 58]. As patients with either infected necrosis or sterile necrosis may present similarly with leukocytosis, fever, and organ failure [59], it is impossible to separate these entities without needle aspiration. Historically, the use of antibiotics is best established in clinically proven pancreatic or extrapancreatic infection, and therefore CT FNA should be considered when an infection is suspected. An immediate review of the Gram stain will often establish a diagnosis. However, it may be prudent to begin antibiotics while awaiting microbiologic confirmation. If culture reports are negative, the antibiotics can be discontinued.
There is some controversy as to whether a CT FNA is necessary in all patients. Although use of CT FNA is recommended in some guidelines [42] and complications such as bleeding and exacerbation of acute pancreatitis are rare [60, 61], CT FNA is performed only in a minority of centers. To assess compliance with guidelines in Germany, for example, only one third of senior gastroenterologists said that they used the procedure [62]. In addition, FNA is associated with a risk of false-negative results, since a negative fine-needle aspiration does not confidently exclude infection [63]. Finally, in many patients, the CT FNA does not influence the management in patients with suspected infected necrosis [64]. Increased use of conservative management and minimally invasive drainage has decreased the use of FNA for the diagnosis of IPN [65]. Many patients with sterile or infected necrosis either improve quickly or become unstable, and decisions on intervention via a minimally invasive route will not be influenced by the results of the aspiration. A consensus conference concluded that FNA should only be used in select situations where there is no clinical response to antibiotics, such as when a fungal infection is suspected [65].
Therapy for Extrapancreatic Infections
Extrapancreatic infections such as bloodstream infections, pneumonia, and urinary tract infections occur in up to 20 % of patients with acute pancreatitis and increase mortality twofold [57, 66]. If sepsis is suspected during the course of pancreatitis, it is reasonable to start antibiotic therapy while waiting for culture results. If culture results are negative, then antibiotics should be discontinued to reduce the risk of fungemia, or Clostridium difficile infection.
Conclusion
Management of infectious complications of SAP remains complex and challenging despite major advances in the field over the last two decades. In summary, quinolones and carbapenems are the antibiotics with optimal pancreatic tissue penetration and bactericidal activity against most of the organisms present in pancreatic infection. With regard to prevention of infection of necrosis, routine antibiotic or probiotic prophylaxis is not recommended. In cases of suspected IPN or sepsis, antibiotic therapy should be initiated while the source of the infection is being investigated [51]. However, once blood and other cultures are found to be negative and no source of infection is identified, antibiotics should be discontinued. A select group of relatively stable patients with IPN can be managed by antibiotics alone without requiring percutaneous drainage or necrosectomy. However, these patients should be closely monitored for failure to improve or clinical deterioration, in which case more aggressive therapy will be warranted.
References
Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med. 2006;354:2142–50.
Garg PK, Madan K, Pande GK, Khanna S, Sathyanarayan G, Bohidar NP, et al. Association of extent and infection of pancreatic necrosis with organ failure and death in acute necrotizing pancreatitis. Clin Gastroenterol Hepatol. 2005;3:159–66.
Isenmann R, Rau B, Beger HG. Bacterial infection and extent of necrosis are determinants of organ failure in patients with acute necrotizing pancreatitis. Br J Surg. 1999;86:1020–4.
van Santvoort HC, Bakker OJ, Bollen TL, Besselink MG, Ahmed Ali U, Schrijver AM, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254–63.
Beger HG, Büchler M, Bittner R, Oettinger W, Block S, Nevalainen T. Necrosectomy and postoperative local lavage in patients with necrotizing pancreatitis: results of a prospective clinical trial. World J Surg. 1988;12:255–62.
Besselink MG, van Santvoort HC, Boermeester MA, Nieuwenhuijs VB, van Goor H, Dejong CH, et al. Timing and impact of infections in acute pancreatitis. Br J Surg. 2009;96:267–73.
Baril NB, Ralls PW, Wren SM, Selby RR, Radin R, Parekh D, et al. Does an infected peripancreatic fluid collection or abscess mandate operation? Ann Surg. 2000;231:361–7.
Banks PA, Freeman ML. Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379.
Ammori BJ, Leeder PC, King RF, Barclay GR, Martin IG, Larvin M, McMahon MJ. Early increase in intestinal permeability in patients with severe acute pancreatitis: correlation with endotoxemia, organ failure, and mortality. J Gastrointest Surg. 1999;3(3):252–62.
Rahman SH, Ammori BJ, Holmfield J, Larvin M, McMahon MJ. Intestinal hypoperfusion contributes to gut barrier failure in severe acute pancreatitis. J Gastrointest Surg. 2003;7(1):26–35.
Dervenis C, Smailis D, Hatzitheoklitos E. Bacterial translocation and its prevention in acute pancreatitis. J Hepatobiliary Pancreat Surg. 2003;10:415–8.
van Santvoort HC, Besselink MG, Timmerman HM, van Minnen LP, Akkermans LM, Gooszen HG. Probiotics in surgery. Surgery. 2008;143:1–7.
Burns GP, Stein TA, Kabnick LS. Blood-pancreatic juice barrier to antibiotic excretion. Am J Surg. 1986;151:205–8.
Büchler M, Malfertheiner P, Friess H, Isenmann R, Vanek E, Grimm H, et al. Human pancreatic tissue concentration of bactericidal antibiotics. Gastroenterology. 1992;103(6):1902–8.
Kramer KM, Levy H. Prophylactic antibiotics for severe acute pancreatitis: the beginning of an era. Pharmacotherapy. 1999;19(5):592–602.
Barie PS. A critical review of antibiotic prophylaxis in severe acute pancreatitis. Am J Surg. 1996;172(6A):38S–43S.
Pederzoli P, Orcalli F, Falconi M, Bozzini L, Martini N. Penetration of mezlocillin into pancreatic juice. J Antimicrob Chemother. 1986;17:397.
Roberts EA, Williams RJ. Ampicillin concentrations in pancreatic fluid bile obtained at endoscopic retrograde cholangiopancreatography (ERCP). Scand J Gastroenterol. 1979;14:669–72.
Koch K, Drewelow B, Liebe S, Reding R, Riethling AK. Die Pankreasgängigkeit von Antibiotica. Chirurg. 1991;62:317–22.
Brattstrom C, Malmborg A-S, Tyden G. Penetration of clindamycin, cefoxitin, and piperacillin into pancreatic juice in man. Surgery. 1988;103:563–7.
Gregg JA, Maher L, DeGirolami PC, Gregg Jr JA. Secretion of b-lactam antibiotics in pure human pancreatic juice. Am J Surg. 1985;150:333–5.
Pederzoli P, Falconi M, Bassi C, Girelli R, Vesentini S, Martini N, et al. Ofloxacin penetration into bile and pancreatic juice. J Antimicrob Chemother. 1989;23:805–7.
Pederzoli P, Falconi M, Bassi C, Vesentini S, Orcalli F, Scaglione F, et al. Ciprofloxacin penetration in pancreatic juice. Chemotherapy. 1987;33:397–401.
Bassi C, Pederzoli P, Vesentini S, Falconi M, Bonora A, Abbas H, et al. Behavior of antibiotics during human necrotizing pancreatitis. Antimicrob Agents Chemother. 1994;38:830–6.
Drewelow B, Koch K, Otto C, Franke A, Riethling AK. Penetration of ceftazidime into human pancreas. Infection. 1993;21:229–34.
Buchler M, Malfertheiner P, Frieß H, Isenmann R, Vanek E, Grimm H, et al. Human pancreatic tissue concentration of bactericidal antibiotics. Gastroenterology. 1992;103:1902–8.
Koch K, Drewelow B, Brinckmann W. Die Pankreaspenetration von Ofloxacin: Eine Pilotstudie. Z Gastroenterol. 1993;31:587–91.
Lankisch PG, Klesel N, Seeger K, Seidel G, Winckler K. Penetration of cefotaxime into the pancreas. Z Gastroenterol. 1983;21:601–3.
Benveniste GL, Morris RG. Penetration of cefotaxime into pancreatic juice. Lancet. 1985;1:588–9.
Widdison AL, Karanjia ND, Reber HA. Antimicrobial treatment of pancreatic infection in cats. Br J Surg. 1994;81:886–9.
Araida T, Frey CF, Ruebner B, Carlson J, King J. Therapeutic regimens in acute experimental pancreatitis in rats: effects of a protease inhibitor, a b-agonist, and antibiotics. Pancreas. 1995;11:132–40.
Foitzik T, Fernández-del Castillo C, Ferraro MJ, Mithöfer K, Rattner DW, Warshaw AL. Pathogenesis and prevention of early pancreatic infection in experimental acute necrotizing pancreatitis. Ann Surg. 1995;222:179–85.
Craig RM, Dordal E, Myles L. The use of ampicillin in acute pancreatitis. Ann Intern Med. 1975;83:831–2.
Finch WT, Sawyers JL, Schenker S. A prospective study to determine the efficacy of antibiotics in acute pancreatitis. Ann Surg. 1976;183:667–71.
Howes R, Zuidema GD, Cameron JL. Evaluation of prophylactic antibiotics in acute pancreatitis. J Surg Res. 1975;18:197–200.
Trudel JL, Wittnich C, Brown RA. Antibiotics bioavailability in acute experimental pancreatitis. J Am Coll Surg. 1994;178:475–9.
de Vries AC, Besselink MG, Buskens E, Ridwan BU, Schipper M, van Erpecum KJ, et al. Randomized controlled trials of antibiotic prophylaxis in severe acute pancreatitis: relationship between methodological quality and outcome. Pancreatology. 2007;7:531–8.
Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev 2006; CD002941.
Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011;46:261–70.
Villatoro E, Mulla M, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev 2010:CD002941.
Jiang K, Huang W, Yang XN, Xia Q. Present and future of prophylactic antibiotics for severe acute pancreatitis. World J Gastroenterol. 2012;18:279–84.
Forsmark CE, Baillie J. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–244.
Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–15; 1416.
Bakker OJ, van Santvoort HC, Besselink MG, van der Harst E, Hofker HS, Gooszen HG, Dutch Pancreatitis Study Group. Prevention, detection, and management of infected necrosis in severe acute pancreatitis. Curr Gastroenterol Rep. 2009;11:104–10.
Grewe M, Tsiotos GG, Luque de-Leon E, Sarr MG. Fungal infection in acute necrotizing pancreatitis. J Am Coll Surg. 1999;188:408.
Isenmann R, Schwarz M, Rau B, Trautmann M, Schober W, Beger HG. Characteristics of infection with Candida species in patients with necrotizing pancreatitis. World J Surg. 2002;26:372.
Gloor B, Müller CA, Worni M, Stahel PF, Redaelli C, Uhl W, et al. Pancreatic infection in severe pancreatitis: the role of fungus and multiresistant organisms. Arch Surg. 2001;136:592.
Trikudanathan G, Navaneethan U, Vege SS. Intra-abdominal fungal infections complicating acute pancreatitis: a review. Am J Gastroenterol. 2011;106:1188–92.
Luiten EJ, Hop WC, Lange JF, Bruining HA. Controlled clinical trial of selective decontamination for the treatment of severe acute pancreatitis. Ann Surg. 1995;222:57–65.
Besselink MG, van Santvoort HC, Buskens E, Boermeester MA, van Goor H, Timmerman HM, et al. Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet. 2008;371:651–9.
Sun S, Yang K, He X, Tian J, Ma B, Jiang L. Langenbecks probiotics in patients with severe acute pancreatitis: a meta-analysis. Arch Surg. 2009;394:171–7.
Hartwig W, Maksan SM, Foitzik T, Schmidt J, Herfarth C, Klar E. Reduction in mortality with delayed surgical therapy of severe pancreatitis. J Gastrointest Surg. 2002;6:481–7.
Dubner H, Steinberg W, Hill M, Bassi C, Chardavoyne R, Bank S. Infected pancreatic necrosis and peripancreatic fluid collections: serendipitous response to antibiotics and medical therapy in three patients. Pancreas. 1996;12:298.
Runzi M, Niebel W, Goebell H, Gerken G, Layer P. Severe acute pancreatitis: non surgical treatment of infected necrosis. Pancreas. 2005;30:195–9.
Garg PK, Sharma M, Madan K, Sahni P, Banerjee D, Goyal R. Primary conservative treatment results in mortality comparable to surgery in patients with infected pancreatic necrosis. Clin Gastroenterol Hepatol. 2010;8:1089–94.
Mouli VP, Vishnubhatla S, Garg PK. Efficacy of conservative treatment, without necrosectomy, for infected pancreatic necrosis: a systematic review and meta-analysis. Gastroenterology. 2013;144:333–40.
van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010;362:1491–502.
Buchler MW, Gloor B, Musller CA, Friess H, Seiler CA, Uhl W. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232:619–26.
Tenner SM, Feng S, Noerdook S, Noordhoek E, Feng S, Zinner M, et al. The relationship of organ failure to pancreatic necrosis. Gastroenterology. 1997;113:899–903.
Evans WK, Ho C-S, McLoughlin MJ, Tao LC. Fatal necrotizing pancreatitis following fine-needle aspiration biopsy of the pancreas. Radiology. 1981;141(1):61–2.
Levin DP, Bret PM. Percutaneous fine-needle aspiration biopsy of the pancreas resulting in death. Gastrointest Radiol. 1991;16:67–9.
Lankisch PG, Weber-Dany B, Lerch MM. Clinical perspectives in pancreatology: compliance with acute pancreatitis guidelines in Germany. Pancreatology. 2005;5:591–3.
Morimoto A, Imamura T, Ishii R, Nakabayashi Y, Nakatani T, Sakagami J, et al. Successful management of severe L-asparaginase-associated pancreatitis by continuous regional arterial infusion of protease inhibitor and antibiotic. Cancer. 2008;113:1362.
Pappas T. Is CT, guided fine needle aspiration helpful in patients with infected necrosis. Am J Gastroenterol. 2005;100:2371–4.
Freeman MF, Werner J, van Santvoort HC, Baron TH, Besselink MG, Windsor JA, et al. Interventions for necrotizing pancreatitis. Summary of a multi-disciplinary consensus conference. Pancreas. 2012;8:1176–94.
Seifert H, Biermer M, Schmitt W, Jürgensen C, Will U, Gerlach R, et al. Transluminal endoscopic necrosectomy after acute pancreatitis: a multicentre study with long-term follow-up (the GEPARD Study). Gut. 2009;58:1260–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Leung, W., Gelrud, A. (2015). Antibiotic Therapy. In: Forsmark, C., Gardner, T. (eds) Prediction and Management of Severe Acute Pancreatitis. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0971-1_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0971-1_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0970-4
Online ISBN: 978-1-4939-0971-1
eBook Packages: MedicineMedicine (R0)