Abstract
In patients with severe acute pancreatitis complicated by pancreatic parenchymal necrosis, one of the feared complications is infected pancreatic necrosis and/or infected peripancreatic tissue. Because of this concern many patients with severe pancreatitis have been treated with prophylactic antibiotics in an attempt to prevent this complication, and one early open label trial in 1993 appeared to show benefit for this approach. Since that time multiple additional studies have been carried out, and review of these trials fails to demonstrate any reduction in infectious complications or the need for operative intervention when prophylactic antibiotics are used. An analysis of trials comparing prophylactic antibiotics with placebo shows that the highest quality studies (rigorous blinding, placebo protocols, inclusion only of severe disease, detailed patient flow descriptions) uniformly fail to show benefit for prophylaxis.
Patients with severe acute pancreatitis or necrotizing pancreatitis should not receive prophylactic antibiotics, but they should be carefully observed in order to facilitate early diagnosis and specific treatment if infection occurs. This is facilitated by fine needle, CT-guided aspiration of suspicious areas. This is an accurate and safe mechanism for determining the presence of infection and identifying the responsible organisms.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Severe acute pancreatitis
- Necrotizing pancreatitis
- Infected pancreatic necrosis
- Prophylactic antibiotics
- Septic complications
- Operative intervention
- Fine needle aspiration
- Clinical trials
Introduction
Acute pancreatitis has a wide range of clinical severity, potential complications and outcomes . Approximately 80 % of patients have mild disease with a relatively quick recovery. Mild pancreatitis patients do not require antibiotic treatment and generally discharge from the hospital within 1 week. However, 15–20 % of patients develop severe acute pancreatitis (SAP) and necrosis of peri-pancreatic tissue or of the parenchyma itself [1–3]. Those patients with necrosis of >30 % of the gland demonstrated by contrast enhanced CT scan are at high risk of developing infected necrosis; overall, 15–35 % of patients with SAP develop infected pancreatic necrosis , typically in the second to fourth week of hospitalization [1, 2, 4, 5]. If the necrosis becomes infected, this increases systemic complications, raises rates of multiple organ failure, and increases the overall SAP mortality rate from 10 % to 30–40 % [2, 6, 7]. Organisms from the gastrointestinal tract are the most common causative agents and include Escherichia coli, Pseudomonas aeruginosa, Clostridium species, Bacteroides species, enterococci, Klebsiella species, Proteus species and Enterobacter species [2, 5, 7, 8]. Gram positive, drug-resistant and fungal organisms are also becoming more common [1, 9–11].
Making the diagnosis of infected pancreatic necrosis can be difficult. Patients with SAP and pancreatic necrosis almost always present with an impressive systemic inflammatory response syndrome (SIRS) with tachypnea, tachycardia, fever and leukocytosis. This initial clinical presentation is similar to one resulting from an underlying infection (sepsis), regardless of whether sterile necrosis or infected necrosis is present. Although this goes against the intuition of the treating physician, clinical parameters in SAP patients do not reliably distinguish between infected versus sterile necrosis [12–14].
In the face of clinical uncertainty and the potential for high mortality with infected necrosis, treating clinicians have often initiated early broad-spectrum antimicrobial prophylaxis for patients with SAP. The rationale is clear: one can surmise that prophylactic antibiotics in these critically-ill patients would reduce the incidence of infected necrosis and improve patient morbidity and mortality. Myriad trials and meta-analyses spanning the past four decades have attempted to show this anticipated benefit, but the published data have led to mixed and sometimes directly contradictory conclusions.
Our aim in this chapter is to determine if antibiotic prophylaxis benefits patients with severe acute pancreatitis (SAP). We will address the apparent impact of antibiotic prophylaxis on the incidence of infected necrosis, septic complications, length of stay, need for operative intervention, mortality and emerging antibiotic resistance.
Search Strategy
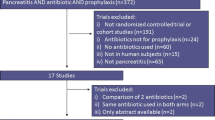
Using the PICO format (Table 39.1), a literature search using the PubMed database was performed to survey available published data on acute pancreatitis and antibiotic prophylaxis. Results were limited to English-language publications, human studies only, with publication range from 1993 to August 2014. Exceptions were made for publications prior to 1993 if they were widely referenced studies. Search terms were as follows: “antibiotic prophylaxis,” “antibiotics,” “antibacterial agent,” “antifungal agent,” “antibiotic resistance,” AND (“acute necrotizing pancreatitis” OR “acute pancreatitis” OR “necrotizing pancreatitis” OR “severe acute pancreatitis”).
We performed a validation of our search strategy using the bibliographies from several recent review articles and meta-analyses [1, 3, 15, 16]. A search of published literature from 1993 to 2009 was performed using the terms: “antibiotics,” “antibiotic prophylaxis” AND (“acute pancreatitis ” OR “necrotizing pancreatitis”). This strategy returned all but 3 of 43 relevant studies in the reference list by Wittau et al., all but 3 of 40 in Howard et al., all but 2 of 28 in Jiang et al., and all but 1 of 45 relevant references cited by De Waele et al. These unique references were included in our review.
Studies were excluded if they were case reports only or if they were studies devoted primarily to surgical decision making/surgical technique. Studies were also excluded if they primarily addressed regional arterial infusion of antibiotics or selective gastrointestinal decontamination.
Results
Early Studies: Prophylaxis and Decreased Infected Necrosis
Two randomized trials in 1975 by Howes et al. [17] and Finch et al. [18] (Tables 39.2 and 39.3) first assessed the efficacy of prophylactic ampicillin in acute pancreatitis . Both papers conclude that there was no difference in clinical outcomes between groups who received prophylaxis versus no prophylaxis. However, these initial studies have several limitations. Both included very mild cases of pancreatitis in their study populations, which introduced considerable heterogeneity in the study groups. Moreover, the rate of pancreatic necrosis and subsequent pancreatic infections was so low in the study groups that both papers were underpowered to detect a difference in treatments (high probability of a type II error).
In 1993, Pederzoli et al. [19] completed a randomized multicenter trial which compared imipenem prophylaxis versus no antibiotic treatment in acute pancreatitis (n = 74). The authors reported an impressive 18 % decrease in the incidence of pancreatic sepsis with the use of prophylactic antibiotics. However, they were unable to show a difference in ultimate clinical endpoints like organ failure rates, operative rates, or mortality . Moreover, this study had several methodological flaws, most significant of which is the lack of any blinding. Lack of blinding is particularly problematic for pancreatitis studies because of historically ambiguous criteria for diagnosing patients with infection vs sepsis vs SIRS (as previously discussed). In addition, un-blinded studies may create a tendency to initiate more off-protocol antibiotics in control patients, leading to crossover between study arms [20]. Other methodological limitations in this study include the lack of a placebo, a heterogeneous study sample (varying severity pancreatitis patients were included), unbalanced study arms, and lack of any comments on patient recruitment/study flow.
Subsequent trials published in the 1990s concluded that pancreatic infections were reduced with prophylactic antimicrobials, but these studies were similarly limited methodologically. Limitations included heterogeneous severity of pancreatitis in study groups, lack of blinding, lack of placebo, low samples sizes (underpowered analyses), and frequent changes in antibiotic regimens in both intervention and control arms. Moreover, although many of these studies showed decreased pancreatic infections and systemic infections with prophylaxis, they failed to show any difference in observed mortality or the need for operations [21–28] (Tables 39.2 and 39.3). Notable exceptions include studies by Sainio et al. [22] and Nordback, et al. [23], who respectively noted a significant mortality benefit and a reduced operative rate in prophylaxis groups. However, both of these studies chose unique methods for defining pancreatic infection, and one study used only clinical parameters to define pancreatic infection (which we have previously described as inherently inaccurate). Finally, it is noteworthy that none of the aforementioned studies documented detailed methods of nutrition for sample populations. The use of enteral nutrition in pancreatitis studies is a highly significant potential confounding factor, given its demonstrated significant benefits for patients with SAP in terms of decreased systemic infections, need for operations, multiple organ failure and death [2, 6, 29, 30].
Recent Randomized Trials: Prophylaxis Reconsidered
Three more recent double-blinded placebo-controlled, randomized controlled trials (DBPCRCT) avoided several of the aforementioned methodological limitations and represent the highest quality evidence yet published. In the first double-blinded study in 2004, Isenmann et al. [31] (Tables 39.2 and 39.3) enrolled 114 pts with SAP and randomized them into two groups (metronidazole and ciprofloxacin versus placebo). No significant differences were noted in mortality , need for operations, length of stay or infected necrosis. Subgroup analysis of those with confirmed pancreatic necrosis >30 % (those deemed at higher risk of pancreatic infection) also showed no differences between groups. Notably, 46 % in placebo group required conversion to open antibiotic treatment due to systemic and septic complications, compared with just 28 % of patients in the intervention group. The next DBPCRCT was performed in 2007 by Dellinger et al. [5] and included 100 patients who had necrotizing SAP. Patients received either meropenem or placebo, and after 42 days follow-up, groups showed similar rates of mortality, infection and need for operative intervention. The authors concluded that the data do not support early prophylactic antibiotics in SAP. Finally, in 2009, Garcia-Barrasa et al. [32] performed a DBPCRCT in 41 patients diagnosed with SAP who had a CT scan showing evidence of pancreatic necrosis. No significant differences between groups were found for infected pancreatic necrosis, mortality, systemic complications, need for operations or length of stay. Of note, due to limitations inherent to this study’s design (described below), the authors stated that no conclusions could be drawn regarding efficacy of prophylactic antibiotics in SAP.
These three DBPCRCTs have methodological strengths that are worth reviewing, but they also contain several limitations. Notable strengths of these studies include rigorous blinding and placebo protocols, homogeneity of patients (designed to include only severe disease), and detailed patient flow descriptions. Moreover, the 2007 DBPCRCT is one of the first studies that ensured standardized nutrition protocols between study groups, thus controlling for this significant source of bias. One limitation inherent to all three studies is small sample size, which diminishes the power to detect a small magnitude effect. Moreover, the conclusions from these studies must be interpreted with caution because all study protocols allowed substantial heterogeneity in both the time of initiation (range: 3–10 days) and duration of therapy among patients (range 6–21 days). Finally, large proportions (up to half) of patients in control and intervention arms received non-protocol antibiotics for other clinical indications.Footnote 1 Taken together, the limitations of these three DBPCRCTs have the potential to bias results toward acceptance of a null hypothesis (type II error). That is, all these described limitations would more likely diminish the effect seen from prophylactic antibiotics and make it more likely to conclude that no significant difference exists between groups.
A Review of Disparate Results
The meta-analyses, reviews, editorials and observational studies published on this topic are too numerous to review individually [6, 15, 20, 33–48], but some trends are worth noting. Results from the meta-analyses on this topic must be interpreted with caution because of the myriad differences between available trials. Any comparison among the previously described trials is limited because of variety in: (a) sampled severities of pancreatitis, (b) definitions for pancreatic infections, (c) outcomes evaluated, (d) thresholds for operative intervention, and (e) antibiotics administered. The majority of these meta-analyses found a significant difference in pancreatic infections for those patients who received antibiotic prophylaxis, but found no differences in mortality , LOS or the need for operations. In contrast, some meta-analyses did show significant differences in mortality, LOS and operative interventions, but these authors failed to include data from relevant DBPCRCTs published after 2004 [36, 41, 43, 45, 47, 48]. Those meta-analyses that included data from DBPCRCTs published after 2004 showed that prior perceived differences in outcomes failed to achieve significance [15, 16, 46].
Some meta-analyses have used unique approaches and explanations to highlight trends in the available data on antibiotic prophylaxis for SAP. One meta-analysis by De Vries et al. [20] reviewed six randomized controlled trials addressing antibiotic prophylaxis in SAP and noted a significant inverse relationship between their methodological quality and the reported effect of antibiotic prophylaxis on mortality . In other words, studies that were assessed as methodologically rigorous tended to report negligible differences in mortality with the use of prophylaxis. Moreover, after grading for quality, and including studies only with a standardized score >5, the meta-analysis revealed that there was no difference found in infection of pancreatic necrosis or mortality. A subsequent meta-analysis by Wittau et al. in 2010 [15] independently confirmed this correlation between study quality and reported outcomes . The authors concluded that prophylaxis had no associated reduction in mortality, infected necrosis, systemic complications or the need for operations. Moreover, the authors found a “borderline significant” pooled relative risk for infected necrosis (RR = 0.78, [95 % CI 0.60–1.02]) but note that this is a surrogate outcome, and that the “real effects” seen by the patient (mortality or need for an operation) are not close to achieving significant differences. Finally, a meta-analysis from 2012 [16] pooled results from studies prior to the year 2000 and demonstrated a relative risk reduction for mortality (RR 0.31, [95 % CI, 0.12–0.79], p = 0.01). This difference was not present when results were pooled for studies after the year 2000 (RR 1.01, 95 % CI 0.65–1.56 p 0.98). Interestingly, the authors note a high potential for publication bias prior to the year 2000 based on the asymmetric results of a funnel plot analysis. The combination of this publication bias and un-blinded study designs prior to 2000 created an environment which would be more likely to produce studies showing a significant effect with prophylactic antibiotics in SAP.
Antimicrobial Resistance and Atypical Organisms
Published studies of moderate quality are available regarding antimicrobial resistance patterns in relation to antibiotics and SAP; overall trends indicate that exposure to broad-spectrum prophylaxis is associated with atypical and resistant organisms. A study in 2002 by Howard et al. [9] compared operative cultures taken from SAP patients before (1977–1992) and after (1993–2001) institution of routine prophylactic antibiotics at a single institution. There was a significant change in bacteriology between groups from gram negative organisms to predominantly gram positive organisms (52 % gram positive organisms in recent samples versus 23 % in older samples). The organisms most frequently cultured in antibiotic-treated patients were S. aureus, S. epidermidis and Corynebacterium. Of note, there were no differences in B-lactam resistance noted between groups. A subsequent case series of 46 patients with SAP and infected necrosis found that approximately 52 % of the patients developed infection with resistant organisms [10]. Those who developed resistant organisms were treated with antibiotics, on average, for 9 days longer than those without resistant organisms (p < 0.05). The authors note that patients with resistant organisms required longer ICU stays, and tended to have higher mortality (37 % vs 23 %, p = 0.28). Other studies have confirmed that the prevalence of antibiotic resistant microorganisms is increasing in patients with SAP and exposure to antibiotic prophylaxis [5, 11, 27, 28, 31, 32, 49, 50]. Classic pathophysiologic teaching on infected pancreatic necrosis cultures has attributed the predominant growth of gram negative species to a prior translocation event from the gastrointestinal tract [2, 4, 6]. However, in the new antibiotic era, increased growth of gram positive flora and fungal organisms may indicate that sources of infection are changing. Some authors speculate that these atypical and resistant organisms may emanate from central lines, catheters, and endotracheal tubes [9, 11]. This was corroborated by a retrospective study which found that patients who had any bacteremia episode while under treatment for SAP with pancreatic necrosis had an increased risk of infected necrosis (65 % vs 37 %) [4].
Available data suggest that SAP patients who have a longer exposure to broad spectrum antibiotics are also at a higher risk of infections with Candida species. In one retrospective study of 92 patients, the authors found that patients with fungal infections were on antibiotics for a mean of 19 days versus 6.4 days in patients without fungal infections (p = 0.0001) [51]. This trend was independently confirmed by a case series of 46 patients in 2004 [10], a prospective study of 50 SAP patients in 2009 [52], and a randomized trial in 2009 [28]. A more recent nonrandomized prospective cohort study of 210 SAP patients [50] found that candida species from pancreatic cultures were significantly more frequent in the patients who received prophylactic antibiotics versus those who did not (10.7 % vs 3.8 %, p 0.04). The mortality rate for SAP patients with Candida has been reported at 65 % versus about 20 % in non-Candida patients [4, 51]. Some studies have found less impressive differences in mortality but still note that SAP patients who develop fungal infections suffer more in-hospital morbidity and have longer hospital and ICU stays [10, 50, 53, 54].
Nevertheless, the reviewed studies on atypical and resistant organisms constitute moderate to low-quality evidence. Much of the published data is un-blinded, non-randomized, and considers two different time periods. Moreover, some considered studies [50] had control groups where large proportions of patients actually received prophylaxis while intervention groups had large proportions of patients who actually did not receive prophylaxis, making the labels ‘control’ and ‘intervention’ less meaningful. Finally, much of the available data on resistance patterns comes from larger studies which assessed this only as a secondary outcome. There is a need for larger epidemiological studies focused specifically on atypical and resistant organisms in patients with SAP who receive antibiotic prophylaxis.
A detailed review of the evidence for antifungal prophylaxis in SAP is beyond the scope of this chapter. In brief, there is insufficient evidence to recommend routine antifungal prophylaxis for all patients with SAP, but there is evidence of a survival benefit in high risk subsets of critically-ill surgical patients [1, 7, 39, 52, 55]. More research is needed to determine if patients with SAP fall within these subsets of patients that could benefit from anti-fungal prophylaxis.
Evidence-Based Protocol for “On-Demand” Antibiotics
The use of prophylactic antibiotics remains suspect, but “on-demand” antibiotics [31] should be initiated in clear cases of infection. If patients with SAP continue to deteriorate or fail to improve after the first or second week of hospitalization, obtaining a CT with or without fine needle aspiration (FNA) of pancreatic tissue is warranted. If the CT shows retroperitoneal air inside pancreatic fluid collections, this is pathognomonic for infection. If the diagnosis remains ambiguous, FNA should be obtained [56, 57]. FNA results can help tailor antibiotic therapy and identify drug-resistant organisms as well. If a positive CT or FNA is obtained, antibiotics should be initiated and source control should be obtained via a “step-up approach” (percutaneous drainage , followed by surgical or endoscopic debridement if necessary) [1–3, 31, 58]. While awaiting full speciation on culture, empiric antibiotics should be initiated and should cover enteric organisms. Standard empiric regimens include carbapenems or quinolones plus metronidazole [1, 39]. Since infected necrosis rarely presents before 10 days, clinical worsening during this time period is typically the result of SIRS evolution rather than infected necrosis. Therefore, it is generally safe to wait up to 10 days to perform a diagnostic FNA [4, 8]. FNA of pancreatic necrosis is relatively sensitive and specific and is reported overall at 88 % and 90 % respectively. After the first week, the FNA sensitivity increases to 97 % and specificity increases to 100 % [1, 8, 56, 59, 60]. Some patients fail to improve after several weeks despite a negative culture results on FNA. In this case, repeat FNA or even empiric drainage/debridement may be warranted [7, 8, 61].
Summary and Recommendations
In summary, we performed a literature review to survey published data on antibiotic prophylaxis in patients with SAP (inclusive of those with pancreatic and peri-pancreatic necrosis ). The relevant outcomes reviewed included the incidence of infected necrosis, septic complications, mortality , need for operative interventions, length of stay, and antibiotic resistance. Search results revealed a myriad of studies with diverse results and conclusions.
Early studies reported decreased pancreatic and systemic infections with prophylaxis, but largely failed to show corresponding differences in ultimate outcomes like operative rates, length of stay or mortality . Early studies constitute low-quality evidence (Table 39.2) because they were limited by publication bias, lack of blinding, lack of placebo, limited recruitment/study flow descriptions, high cross-over from control to intervention arms, and small sample sizes (underpowered). Moreover, early studies were limited by heterogeneity of disease severity and heterogeneity in nutrition methods. As a result of these limitations, no recommendations can be made based on these data.
Later DBPCRCTs constitute high-quality evidence (Table 39.2). These studies failed to show any significant differences between prophylaxis and placebo groups; rates of pancreatic infections, operations, mortality and length of stay were similar. While these studies did show trends toward decreased systemic infections in patients who received prophylaxis, they showed no significant differences in ultimate clinical outcomes for those treated “on-demand” [31] with antibiotics as soon as nosocomial infections arose. On the basis of these studies, we strongly recommend against using antibiotics to prevent infection in patients with SAP or in patients who develop sterile pancreatic necrosis . Antibiotics should only be used for patients with already proven pancreatic or systemic infections. However, even these high quality studies are limited by small sample sizes (under-powered analyses), variation in initiation/duration of antibiotics, and frequent use of additional ‘off-protocol’ antibiotics in both placebo and control groups. The net effect of these limitations may diminish small magnitude effects from prophylaxis and may result in failure to appreciate subtle but real differences (a type II error).
As previously discussed, it is largely impossible to differentiate sterile from infected pancreatic necrosis on the basis of clinical signs alone. Additional tools like CT and FNA are needed to help obtain a definitive diagnosis . Available moderate-quality evidence suggests that FNA is a sensitive and specific tool. Observational studies and randomized trials have noted that infected necrosis is extremely rare prior to day 7–10 of hospitalization. Therefore, we strongly recommend investigation with a CT with or without an FNA in any patient with pancreatic or peri-pancreatic necrosis if clinical deterioration or failure to improve occurs beyond 7–10 days of hospitalization. Treatment with empiric antibiotics should occur only if positive FNA cultures are obtained. Nevertheless, a negative FNA should be interpreted with caution in a patient who fails to improve and should not be used to definitively rule-out infected necrosis.
Available published data on prophylaxis and antimicrobial resistance/atypical organisms is of moderate to low quality. Many of these studies were observational in nature, but some evidence was from larger randomized trials. These studies have shown that drug-resistant organisms are frequent in patients with SAP and that the prevalence of resistant bacteria and fungi is associated with both exposure and duration of exposure to broad-spectrum antibiotics. It is unclear whether infections with resistant and/or atypical organisms lead to increased mortality , but fungal infections have been associated with increased morbidity and longer length of hospital stay. On the basis of these data, we recommend caution in all decisions to initiate antibiotics and limitation of the treatment duration whenever possible (weak recommendation).
A Personal View of the Data
Despite mounting evidence against the use of prophylactic antibiotics in SAP, a recent survey of intensivists and surgeons indicates that routine prophylaxis is an ongoing and common practice [62]. If the data are becoming more convincing, what can we infer from this generalized reluctance to adopt evidence-based practices? Certainly the cacophony of contradictory results and conclusions in the literature contributes to this slow uptake. Perhaps more importantly, as an individual clinician taking care of a critically-ill deteriorating patient, making the diagnosis of infected pancreatic necrosis is difficult and decisions must often be made quickly. In this context, antibiotic prophylaxis may be employed to allay the fears and anxieties of the clinician rather than to treat the patient. Prescribing prophylactic antibiotics ‘buys time’ while the patient stabilizes and while diagnostic workup occurs.
We caution against this practice and encourage a more rigorous application of evidence-based practice. Despite aforementioned limitations in the current evidence, we must balance the proven risks of antimicrobial resistance against the (at best) nominal potential and unproven benefits of prophylactic antibiotics. Moreover, we are a priori suspect regarding the use of antibiotics to prevent an infection of any necrotic tissue. Dead tissue lacks adequate perfusion and therefore lacks an adequate conduit for any antibiotic; studies of antibiotic penetration and tissue concentrations in living pancreatic tissue may not be applicable to this topic. Finally, the risk of infection in pancreatitis starts at the onset of inflammation and persists over several weeks. Generally accepted teaching dictates that infectious risks which persist over long periods of time do not benefit from antibiotic prophylaxis (for example, prophylaxis has been found ineffective for foley catheters, endotracheal tubes, central lines, burns, etc…).
Further studies to clarify this subject are needed, but improvements beyond currently published literature will prove challenging. Obtaining early access to patients for enrollment continues to be difficult due to frequent transfers from outside hospitals. Moreover, defining strict inclusion criteria often mandates obtaining a CT scan, but necrosis of pancreatic parenchyma often is not adequately depicted on CT until an interval of 2–3 days past initial presentation [27]. This further limits timeliness of enrollment. Finally, given the high prevalence of systemic (nonpancreatic) infections in these patients, studies on patients with SAP will likely always require frequent initiation of non-protocol, open -label antibiotics.
Future DBPCRCTs could be structured to evaluate specifically early versus late administration of prophylactic antibiotics and would offer methodological improvements beyond currently published studies on this topic [23, 27]. In any future studies, efforts must be focused on creating larger samples so that adequately powered analyses can occur. As it currently stands, the proven risks of antibiotic prophylaxis in SAP outweigh the potential nominal benefits, and available evidence indicates that the use of prophylaxis is not warranted.
Recommendations
-
1.
We recommend against using antibiotics to prevent infection in patients with severe acute pancreatitis and in patients who develop sterile pancreatic necrosis . Antibiotics should only be used for patients with already proven pancreatic or systemic infections. (High-quality evidence, strong recommendation).
-
2.
We recommend investigation with a CT +/− FNA in any patient with pancreatic or peri-pancreatic necrosis if clinical deterioration or failed improvement occurs beyond 7–10 days of hospitalization. Treatment with empiric antibiotics should occur only if positive FNA cultures are obtained (moderate-quality evidence, strong recommendation).
-
3.
If patients with severe acute pancreatitis have a confirmed infection, we recommend judicious initiation and limited duration of antibiotic treatment when possible to decrease the development of drug-resistant organisms (moderate-low quality evidence, weak recommendation).
Notes
- 1.
However, Dellinger et al. [5] note that the vast majority of ‘off-protocol’ antibiotics given in this trial occurred three or more weeks after randomization. This permits evaluation of the efficacy of early antibiotic prophylaxis and does not diminish the validity of their conclusions. This is strengthened by evidence that bacterial seeding of pancreatic and peri-pancreatic necrosis often occurs as early as the first 1–2 weeks of hospitalization [13].
References
Howard TJ. The role of antimicrobial therapy in severe acute pancreatitis. Surg Clin N Am. 2013;93(3):585–93. PubMed Epub 2013/05/02. eng.
da Costa DW, Boerma D, van Santvoort HC, Horvath KD, Werner J, Carter CR, et al. Staged multidisciplinary step-up management for necrotizing pancreatitis. Br J Surg. 2014;101(1):e65–79. PubMed.
De Waele JJ. Acute pancreatitis. Curr Opin Crit Care. 2014;20(2):189–95. PubMed.
Besselink MG, van Santvoort HC, Boermeester MA, Nieuwenhuijs VB, van Goor H, Dejong CH, et al. Timing and impact of infections in acute pancreatitis. Br J Surg. 2009;96(3):267–73. PubMed.
Dellinger EP, Tellado JM, Soto NE, Ashley SW, Barie PS, Dugernier T, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Ann Surg. 2007;245(5):674–83. PubMed Pubmed Central PMCID: PMC1877078, Epub 2007/04/26. eng.
Bakker OJ, Issa Y, van Santvoort HC, Besselink MG, Schepers NJ, Bruno MJ, et al. Treatment options for acute pancreatitis. Nat Rev Gastroenterol Hepatol. 2014;11(8):462–9. PubMed.
Tenner S, Baillie J, DeWitt J, Vege SS, American College of G. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–15; 16. PubMed.
Hasibeder WR, Torgersen C, Rieger M, Dunser M. Critical care of the patient with acute pancreatitis. Anaesth Intensive Care. 2009;37(2):190–206. PubMed Epub 2009/04/30. eng.
Howard TJ, Temple MB. Prophylactic antibiotics alter the bacteriology of infected necrosis in severe acute pancreatitis. J Am Coll Surg. 2002;195(6):759–67. PubMed Epub 2002/12/24. eng.
De Waele JJ, Vogelaers D, Hoste E, Blot S, Colardyn F. Emergence of antibiotic resistance in infected pancreatic necrosis. Arch Surg (Chicago, Ill : 1960). 2004;139(12):1371–5. PubMed Epub 2004/12/22. eng.
Behrman SW, Bahr MH, Dickson PV, Zarzaur BL. The microbiology of secondary and postoperative pancreatic infections: implications for antimicrobial management. Arch Surg. 2011;146(5):613–9. PubMed Epub 2011/05/18. eng.
Block S, Buchler M, Bittner R, Beger HG. Sepsis indicators in acute pancreatitis. Pancreas. 1987;2(5):499–505. PubMed Epub 1987/01/01. eng.
Beger HG, Bittner R, Block S, Buchler M. Bacterial contamination of pancreatic necrosis. A prospective clinical study. Gastroenterology. 1986;91(2):433–8. PubMed Epub 1986/08/01. eng.
Gerzof SG, Banks PA, Robbins AH, Johnson WC, Spechler SJ, Wetzner SM, et al. Early diagnosis of pancreatic infection by computed tomography-guided aspiration. Gastroenterology. 1987;93(6):1315–20. PubMed Epub 1987/12/01. eng.
Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011;46(3):261–70. PubMed Epub 2010/11/12. eng.
Jiang K, Huang W, Yang XN, Xia Q. Present and future of prophylactic antibiotics for severe acute pancreatitis. World J Gastroenterol. 2012;18(3):279–84. PubMed Pubmed Central PMCID: PMC3261546, Epub 2012/02/02. eng.
Howes R, Zuidema GD, Cameron JL. Evaluation of prophylactic antibiotics in acute pancreatitis. J Surg Res. 1975;18(2):197–200. PubMed Epub 1975/02/01. eng.
Finch WT, Sawyers JL, Schenker S. A prospective study to determine the efficacy of antibiotics in acute pancreatitis. Ann Surg. 1976;183(6):667–71.
Pederzoli P, Bassi C, Vesentini S, Campedelli A. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surg Gynecol Obstet. 1993;176(5):480–3. PubMed Epub 1993/05/01. eng.
de Vries AC, Besselink MG, Buskens E, Ridwan BU, Schipper M, van Erpecum KJ, et al. Randomized controlled trials of antibiotic prophylaxis in severe acute pancreatitis: relationship between methodological quality and outcome. Pancreatology. 2007;7(5–6):531–8. PubMed.
Rokke O, Harbitz TB, Liljedal J, Pettersen T, Fetvedt T, Heen LO, et al. Early treatment of severe pancreatitis with imipenem: a prospective randomized clinical trial. Scand J Gastroenterol. 2007;42(6):771–6. PubMed.
Sainio V, Kemppainen E, Puolakkainen P, Taavitsainen M, Kivisaari L, Valtonen V, et al. Early antibiotic treatment in acute necrotising pancreatitis. Lancet. 1995;346(8976):663–7. PubMed Epub 1995/09/09. eng.
Nordback I, Sand J, Saaristo R, Paajanen H. Early treatment with antibiotics reduces the need for surgery in acute necrotizing pancreatitis – a single-center randomized study. J Gastrointest Surg. 2001;5(2):113–8; discussion 8–20. PubMed Epub 2001/05/02. eng.
Delcenserie R, Yzet T, Ducroix JP. Prophylactic antibiotics in treatment of severe acute alcoholic pancreatitis. Pancreas. 1996;13(2):198–201. PubMed Epub 1996/08/01. eng.
Bassi C, Falconi M, Talamini G, Uomo G, Papaccio G, Dervenis C, et al. Controlled clinical trial of pefloxacin versus imipenem in severe acute pancreatitis. Gastroenterology. 1998;115(6):1513–7. PubMed Epub 1998/12/03. eng.
Manes G, Rabitti PG, Menchise A, Riccio E, Balzano A, Uomo G. Prophylaxis with meropenem of septic complications in acute pancreatitis: a randomized, controlled trial versus imipenem. Pancreas. 2003;27(4):e79–83. PubMed Epub 2003/10/25. eng.
Manes G, Uomo I, Menchise A, Rabitti PG, Ferrara EC, Uomo G. Timing of antibiotic prophylaxis in acute pancreatitis: a controlled randomized study with meropenem. Am J Gastroenterol. 2006;101(6):1348–53. PubMed.
Xue P, Deng LH, Zhang ZD, Yang XN, Wan MH, Song B, et al. Effect of antibiotic prophylaxis on acute necrotizing pancreatitis: results of a randomized controlled trial. J Gastroenterol Hepatol. 2009;24(5):736–42. PubMed Epub 2009/02/18. eng.
Cao Y, Xu Y, Lu T, Gao F, Mo Z. Meta-analysis of enteral nutrition versus total parenteral nutrition in patients with severe acute pancreatitis. Ann Nutr Metab. 2008;53(3–4):268–75. PubMed Epub 2009/01/13. eng.
Al-Omran M, Albalawi ZH, Tashkandi MF, Al-Ansary LA. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010;(1):CD002837. PubMed Epub 2010/01/22. eng.
Isenmann R, Rünzi M, Kron M, Kahl S, Kraus D, Jung N, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial1 ☆. Gastroenterology. 2004;126(4):997–1004.
Garcia-Barrasa A, Borobia FG, Pallares R, Jorba R, Poves I, Busquets J, et al. A double-blind, placebo-controlled trial of ciprofloxacin prophylaxis in patients with acute necrotizing pancreatitis. J Gastrointest Surg. 2009;13(4):768–74. PubMed.
Bai Y, Gao J, Zou DW, Li ZS. Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in acute necrotizing pancreatitis: evidence from a meta-analysis of randomized controlled trials. Am J Gastroenterol. 2008;103(1):104–10. PubMed Epub 2007/10/11. eng.
Jafri NS, Mahid SS, Idstein SR, Hornung CA, Galandiuk S. Antibiotic prophylaxis is not protective in severe acute pancreatitis: a systematic review and meta-analysis. Am J Surg. 2009;197(6):806–13. PubMed Epub 2009/02/17. eng.
Mazaki T, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. Br J Surg. 2006;93(6):674–84. PubMed Epub 2006/05/17. eng.
Sharma VK, Howden CW. Prophylactic antibiotic administration reduces sepsis and mortality in acute necrotizing pancreatitis: a meta-analysis. Pancreas. 2001;22(1):28–31. PubMed Epub 2001/01/04. eng.
Heinrich S, Schafer M, Rousson V, Clavien PA. Evidence-based treatment of acute pancreatitis: a look at established paradigms. Ann Surg. 2006;243(2):154–68. PubMed Pubmed Central PMCID: PMC1448904, Epub 2006/01/25. eng.
De Waele JJ. A role for prophylactic antibiotics in necrotizing pancreatitis? Why we may never know the answer. Crit Care. 2008;12(6):195. PubMed Pubmed Central PMCID: PMC2646304. Epub 2008/12/19. eng.
De Waele JJ. Rational use of antimicrobials in patients with severe acute pancreatitis. Semin Respir Crit Care Med. 2011;32(2):174–80. PubMed Epub 2011/04/21. eng.
Beger HG, Rau B, Isenmann R, Schwarz M, Gansauge F, Poch B. Antibiotic prophylaxis in severe acute pancreatitis. Pancreatology. 2005;5(1):10–9. PubMed Epub 2005/03/19. eng.
Dambrauskas Z, Gulbinas A, Pundzius J, Barauskas G. Meta-analysis of prophylactic parenteral antibiotic use in acute necrotizing pancreatitis. Medicina (Kaunas). 2007;43(4):291–300. PubMed Epub 2007/05/09. eng.
Tellado JM. Prevention of infection following severe acute pancreatitis. Curr Opin Crit Care. 2007;13(4):416–20. PubMed Epub 2007/06/30. eng.
Xu T, Cai Q. Prophylactic antibiotic treatment in acute necrotizing pancreatitis: results from a meta-analysis. Scand J Gastroenterol. 2008;43(10):1249–58. PubMed Epub 2008/07/09. eng.
Yao L, Huang X, Li Y, Shi R, Zhang G. Prophylactic antibiotics reduce pancreatic necrosis in acute necrotizing pancreatitis: a meta-analysis of randomized trials. Dig Surg. 2010;27(6):442–9. PubMed Epub 2010/11/13. eng.
Villatoro E, Bassi C, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. 2006;(4):CD002941. PubMed Epub 2006/10/21. eng.
Villatoro E, Mulla M, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. 2010;(5):CD002941. PubMed Epub 2010/05/14. eng.
Golub R, Siddiqi F, Pohl D. Role of antibiotics in acute pancreatitis: a meta-analysis. J Gastrointest Surg. 1998;2(6):496–503. PubMed Epub 1999/08/24. eng.
Zhou YM, Xue ZL, Li YM, Zhu YQ, Cao N. Antibiotic prophylaxia in patients with severe acute pancreatitis. Hepatobiliary Pancreat Dis Int. 2005;4(1):23–7. PubMed Epub 2005/02/26. eng.
Israil AM, Palade R, Chifiriuc MC, Vasile D, Grigoriu M, Voiculescu D, et al. Spectrum, antibiotic susceptibility and virulence factors of bacterial infections complicating severe acute pancreatitis. Chirurgia (Bucur). 2011;106(6):743–52. PubMed Epub 2012/02/09. eng.
Ignatavicius P, Vitkauskiene A, Pundzius J, Dambrauskas Z, Barauskas G. Effects of prophylactic antibiotics in acute pancreatitis. HPB (Oxf). 2012;14(6):396–402. PubMed Pubmed Central PMCID: PMC3384864, Epub 2012/05/10. eng.
Isenmann R, Schwarz M, Rau B, Trautmann M, Schober W, Beger HG. Characteristics of infection with Candida species in patients with necrotizing pancreatitis. World J Surg. 2002;26(3):372–6. PubMed Epub 2002/02/28. eng.
Kochhar R, Ahammed SK, Chakrabarti A, Ray P, Sinha SK, Dutta U, et al. Prevalence and outcome of fungal infection in patients with severe acute pancreatitis. J Gastroenterol Hepatol. 2009;24(5):743–7. PubMed Epub 2009/02/18. eng.
Vege SS, Gardner TB, Chari ST, Baron TH, Clain JE, Pearson RK, et al. Outcomes of intra-abdominal fungal vs. bacterial infections in severe acute pancreatitis. Am J Gastroenterol. 2009;104(8):2065–70. PubMed Epub 2009/06/06. eng.
Trikudanathan G, Navaneethan U, Vege SS. Intra-abdominal fungal infections complicating acute pancreatitis: a review. Am J Gastroenterol. 2011;106(7):1188–92. PubMed.
He YM, Lv XS, Ai ZL, Liu ZS, Qian Q, Sun Q, et al. Prevention and therapy of fungal infection in severe acute pancreatitis: a prospective clinical study. World J Gastroenterol. 2003;9(11):2619–21. PubMed Epub 2003/11/08. eng.
Buchler MW, Gloor B, Muller CA, Friess H, Seiler CA, Uhl W. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232(5):619–26. PubMed Pubmed Central PMCID: PMC1421214, Epub 2000/11/07. eng.
van Baal MC, Bollen TL, Bakker OJ, van Goor H, Boermeester MA, Dejong CH, et al. The role of routine fine-needle aspiration in the diagnosis of infected necrotizing pancreatitis. Surgery. 2014;155(3):442–8. PubMed Epub 2013/11/30. eng.
van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010;362(16):1491–502. PubMed Epub 2010/04/23. eng.
Schoenberg MH, Rau B, Beger HG. New approaches in surgical management of severe acute pancreatitis. Digestion. 1999;60 Suppl 1:22–6. PubMed Epub 1999/02/23. eng.
Ashley SW, Perez A, Pierce EA, Brooks DC, Moore Jr FD, Whang EE, et al. Necrotizing pancreatitis: contemporary analysis of 99 consecutive cases. Ann Surg. 2001;234(4):572–9. PubMed Pubmed Central PMCID: PMC1422080, discussion 9–80. Epub 2001/09/27. eng.
Rodriguez JR, Razo AO, Targarona J, Thayer SP, Rattner DW, Warshaw AL, et al. Debridement and closed packing for sterile or infected necrotizing pancreatitis: insights into indications and outcomes in 167 patients. Ann Surg. 2008;247(2):294–9. PubMed Pubmed Central PMCID: 3806106.
De Waele JJ, Rello J, Anzueto A, Moreno R, Lipman J, Sakr Y, et al. Infections and use of antibiotics in patients admitted for severe acute pancreatitis: data from the EPIC II study. Surg Infect. 2014;15(4):394–8. PubMed Epub 2014/05/14. eng.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Parent, B., Dellinger, E.P. (2016). Antibiotic Prophylaxis for Acute Necrotizing Pancreatitis. In: Millis, J., Matthews, J. (eds) Difficult Decisions in Hepatobiliary and Pancreatic Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-319-27365-5_39
Download citation
DOI: https://doi.org/10.1007/978-3-319-27365-5_39
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-27363-1
Online ISBN: 978-3-319-27365-5
eBook Packages: MedicineMedicine (R0)