Abstract
Quantitative coronary angiography (QCA) developed 30 years ago after invasive coronary angiography became an established procedure with concrete indications and therapeutic applications. Digital acquisition of cine angiograms made QCA much more available and practical. New developments in software and hardware led to exciting opportunities to visualize coronary stenoses in two and three dimensions and tailor therapy. Moreover, QCA provided excellent reliability and consistency in interpretation of coronary angiograms, allowing angiographic endpoints to become important surrogate endpoints in clinical trials.
Once coronary atherosclerosis could be quantified using QCA and intravascular ultrasound (IVUS), it became imperative to attempt to document regression of this relentless process and quantify it. Medical therapies directed at atherosclerosis regression centered predominantly on lipid-lowering therapy with statins. Numerous studies evaluated the extent of coronary artery disease (CAD) before and after 12–24 months of therapy and reached important conclusions. Atherosclerosis regression is quantitatively very modest—1–5 % changes in minimal lumen diameter or diameter stenosis and comparable reductions in plaque area and volume measured by IVUS. Yet, these apparently unimpressive changes track robust reductions in low-density lipoprotein and result in substantial lowering of clinically relevant ischemic events. This dissociation between changes in plaque dimensions and reduction in clinical events reinforces our current understanding of CAD pathophysiology and of the mechanisms responsible for plaque destabilization.
The development of intracoronary devices has been closely linked to QCA and its ability to reliably differentiate between various responses to vessel wall injury induced by angioplasty. There is a continuous, robust relationship between late lumen loss after coronary angioplasty and binary angiographic restenosis or need for repeat revascularization. QCA-derived parameters of reperfusion are powerful predictors of survival and freedom from adverse events after STEMI.
Yet, QCA does not assist in identification of plaque type, its vulnerability or its functional significance. Newer technologies incorporating CT-derived coronary flow as well as intracoronary magnetic resonance may resolve these deficiencies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Primary Percutaneous Coronary Intervention
- Invasive Coronary Angiography
- Diameter Stenosis
- Minimal Lumen Diameter
- Late Lumen Loss
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Coronary artery disease (CAD) remains the entity responsible for most non-accidental deaths in the world [1]. Despite significant progress in understanding the pathophysiology of this condition and in treating its acute presentations, there is currently no cure for CAD and there is no consistent therapy for slowing its progression. Hence, considerable interest exists in developing reliable technologies to assess the effect of new medical and interventional therapies on the rate of progression of CAD and on the factors responsible for its destabilization. The matter is further complicated by the fact that CAD is a process that predominantly affects the vessel wall, such that the early phases of the disease are not at all manifested by impingement on the lumen of the epicardial coronary arteries and their branches, which are visualized during invasive coronary angiography [2–4]. As early as the second decade of life, changes in endothelial function caused by exposure to adverse metabolic or hemodynamic conditions lead to penetration of lipid moieties in the coronary vessel wall. An inflammatory reaction ensues, marked by accumulation of macrophages and oxidation of low-density lipoprotein. A fatty plaque is formed, and it is this precursor of CAD which progresses slowly over decades until it becomes clinically active. The early and intermediate stages of this process are almost entirely invisible to imaging of the lumen of the coronary artery, particularly when visual estimates are used, because of the compensatory expansion of the vessel outward [5].
For over 50 years, invasive coronary angiography with contrast media has been the mainstay for evaluation of CAD and accompanied all the major therapeutic breakthroughs in this field. The first two decades of the technology were dedicated to perfecting the techniques for imaging the coronary arteries and for storing this information on transferable media. Even before the advent of digital storage of images, considerable interest developed in the quantitative aspects of coronary angiography (QCA), particularly in order to measure and compare the effects of medical and interventional therapies on the progression of CAD.
In this chapter we will review the main principles of QCA and assess its utility for quantification of CAD progression or response to intravascular devices.
Principles of Quantitative Coronary Angiography
Thirty years ago, Brown and colleagues introduced the first quantitative assessment of coronary arteries by magnifying 35 mm cine angiograms and tracing the contour of the arteries on a large screen [6, 7]. Early computer software corrected for pincushion distortion (created by the magnification process and leading to “pinching” of the artery in the middle of the segment) and tracings were then digitized and reconstructed into a three dimensional rendering of the coronary arteries, assuming elliptical geometry. This early prototype served as the basis for the automated contour detection software used routinely in QCA today. As digital acquisition of images became the standard in invasive cardiology, the need for digitization of the cine angiograms disappeared. The images, acquired in a DICOM (Digital Imaging and Communications in Medicine) format with 2:1 JPEG lossless compression, are then calibrated using the dye-filled injection catheter’s known dimensions as the reference. A calibration factor (mm per pixel) allows the measurement of various aspects of the vessel. Each such study occupies ~500 MB of storage. The most basic measurements include reference vessel diameter (RVD), minimal lumen diameter (MLD), and percent diameter stenosis (DS). RVD determination is particularly important as it is the basis for derivation of many of the other parameters. Typically the interpolation method is used by the software algorithm to approximate the normal decrease in vessel diameter as it progresses distally. The lesion length (LL), defined from shoulder-to-shoulder (where DS is at least 50 % of RVD), can also be measured. In every angiography core laboratory (ACL), inter- and intra-observer variability is measured frequently to ensure consistency of film review. In general, the inter-observer variability is <0.25 mm for most automated software. Considering coronary vessels of 3–4 mm in diameter, this translates in ~5 % variability. Beyond the variability caused by observer, biological factors play an important role in our ability to perform adequate QCA. Acquisition of images is affected significantly by the quality of the camera, by the consistency of the acquisition (respiratory variation, quantum mottling or nonuniform film density, foreshortening, and out-of-plane magnification), and by the skill of the angiographer. Inadequate filling of the artery (streaming), lack of separation of branches, different angles (important for follow-up studies), and vasomotor tone can all influence the precision of QCA. The two most commonly used systems for QCA are discussed briefly below.
The Cardiovascular Angiography Analysis System (CAAS, Pie Medical Data, The Netherlands) is an online and off-line analysis system. It has pincushion distortion correction and a weighted (50 %) sum of the first two derivatives of the mean pixel density. It provides an interpolated RVD and has subsegmental and specialty modules for bifurcation lesions, three-dimensional reconstruction, and stent analysis.
The Coronary Measurement System (CMS, MEDIS, The Netherlands) uses similar technology but also has a two-point user-defined centerline identification for catheter calibration and vessel contour.
Beyond RVD, DS, and MLD, typical QCA parameters used in clinical trials include late lumen loss (LLL, defined as the difference between MLD at baseline minus MLD at follow-up), late loss index (defined as LLL divided by initial MLD gain), and binary angiographic restenosis (BAS, defined as DS > 50 % at follow-up). In addition to these classical parameters of percutaneous coronary intervention (PCI) and atherosclerosis studies, semiquantitative and quantitative indices have been devised to describe coronary perfusion at the epicardial and myocardial (tissue) level. These include TIMI (thrombolysis in myocardial infarction) flow grade (0—no flow, to 3—normal flow), TIMI frame counts (number of frames needed for contrast to traverse a defined segment of the coronary tree), and myocardial blush grade (MBG, defined as the penetration of contrast in the microcirculation supplied by the vessel undergoing PCI). These three indices are particularly relevant to patients undergoing reperfusion therapy with fibrinolytic therapy or primary PCI for ST-elevation myocardial infarction.
QCA in Studies of Medical Treatment of Atherosclerosis
In reviewing this topic, the most important element to understand is the underlying mechanisms of CAD. As briefly mentioned above, coronary atherosclerosis develops predominantly in the vessel wall before it extends into the lumen. The coronary artery remodels and expands outwardly to accommodate this increased volume of tissue in its media. As such, coronary angiography has limited ability to evaluate changes related to progression or regression of atherosclerosis, except when the process is sufficiently advanced to affect lumen size. Furthermore, changes in plaque size, or lumen size can be very modest and yet coexist with dramatic reduction in clinical events. This important observation reflects the ability of plaque-modifying agents, such as statins, to reduce the propensity for plaque rupture or disruption leading to acute coronary syndromes. Thus, much more relevant information has been obtained in this area by studies utilizing intravascular ultrasound (IVUS) to detect small changes in plaque area and volume, including that residing in the vessel wall. Yet, the beginnings of the science of atherosclerosis regression date back to a time when IVUS was not yet available and QCA was the best tool available to assess these changes.
One of the first trials to illustrate the paradox of minimal changes in MLD and large reductions in clinical events was HATS (HDL Atherosclerosis Treatment Study) [8]. Among 146 randomized men who had apolipoprotein B levels ≥125 mg/dL, documented CAD, 120 completed the study, including baseline and follow-up angiography. Patients were given dietary counseling and were randomly assigned to one of the three treatments: lovastatin (20 mg twice a day) and colestipol (10 g three times a day); niacin (1 g four times a day) and colestipol (10 g three times a day); or conventional therapy with placebo (or colestipol if the LDL level was elevated). Coronary events were reduced by 66 % by the combination therapy (6.5 % vs. 19.2 % for placebo) after 2.5 years of therapy. This dramatic effect was achieved despite very modest changes in angiographic parameters: among 1,316 baseline lesions, DS increased by 2.1 % in the conventional therapy group and decreased by 0.7 % in the combination therapy arm (P = 0.003), with more effect in lesions with DS ≥ 50 % at baseline. MLD decreased by 0.05 mm in the conventional therapy group and increased by 0.012 mm in the combination therapy group among the proximal segment lesions (P = 0.01). In a similar study—REGRESS (Regression Growth Evaluation Statin Study), treatment with pravastatin, compared with placebo, resulted in less progression of atherosclerosis (change in mean lumen diameter 0.06 mm vs. 0.10 mm, P = 0.02, change in MLD 0.03 mm vs. 0.09 mm, P = 0.001) and fewer cardiovascular events (11 % vs. 19 %, P = 0.002) [9]. Reduction in coronary events with statin therapy has been most pronounced in patients with established coronary disease (secondary prevention) but also occurs in those without it (primary prevention). The benefit of aggressive lipid-lowering therapy with statins in the former category was indexed directly to the on-treatment LDL level. When LDL falls below 100 mg/dL, the rate of CAD events is below 10 % and reaches as low as 5 % with the recommended target for LDL in high-risk patients (70 mg/dL) [10, 11]. For the latter, Brugts et al. compiled data from ten randomized clinical trials encompassing nearly 70,000 patients. All-cause mortality was reduced by 12 % with statins, major coronary events—by 30 % and cerebrovascular events—by 19 % [12]. There was no heterogeneity in response based on gender, age, or the presence of diabetes mellitus.
When angiography was performed at baseline and after treatment in studies of primary and secondary prevention, the changes in angiographic parameters were consistent with data from HATS and REGRESS. Gotto performed a systematic analysis of such trials and showed that while there was a statistically significant correlation between change in MLD and on-treatment LDL (R 2 = 0.61, P = 0.001), absolute changes in MLD varied between −0.01 mm (progression of atherosclerosis) and 0.05 mm (regression) [13]. Brown et al. examined the ability of experienced operators to distinguish in serial studies between lesions that definitely changed in severity, those that possibly changed and those that did not. In FATS (Familial Atherosclerosis Treatment Study) 120 patients were randomized to three lipid-lowering strategies. In 81 % of lesions scored as “definitely” changed by operators, there was more than 10 % change in DS, as measured by QCA. It appeared that the threshold for visual classification of definite changes was 9.3 % [14].
Lipid lowering may be only one paradigm for atherosclerosis regression. Correction of other risk factors for CAD, such as hypertension, may have a similar effect on atherosclerosis progression. Amlodipine, a long-acting calcium channel blocker used to treat hypertension, was found to have antioxidant effects and to prevent the abnormal accumulation of calcium induced by cholesterol in smooth muscle cells in animals [15]. In one trial, amlodipine reduced progression of atherosclerosis in carotid arteries, but not in coronary arteries [16]. The NORMALISE (Norvasc for Regression of Manifest Atherosclerotic Lesions by Intravascular Sonographic Evaluation) trial compared the effects of amlodipine, enalapril, and placebo among 431 normotensive patients followed for 2 years with coronary angiography and IVUS at baseline and at the end of study, as part of the larger CAMELOT (Comparison of Amlodipine versus Enalapril to Limit Occurrences of Thrombosis) study [17]. Only 69 % of patients completed the follow-up angiographic study. The mean change in MLD was −0.02 ± 0.13 for amlodipine, −0.03 ± 0.12 for enalapril, and −0.03 ± 0.17 mm for placebo (P = 0.40). There were no significant correlations between changes in MLD and blood pressure reduction, age, gender, or the presence of diabetes mellitus [18]. An ischemic event, as defined in the primary endpoint, occurred in 20.2, 24.0, and 25.2 % of the amlodipine, enalapril, and placebo groups, respectively (P = 0.68). The change in MLD in patients with and without cardiovascular events (cardiovascular death, nonfatal MI, resuscitated cardiac arrest, coronary revascularization, angina or heart failure requiring hospitalization, ischemic stroke or transient ischemic attack, or a new diagnosis of peripheral arterial disease), regardless of treatment assignment, was −0.05 ± 0.20 mm and −0.02 ± 0.13 mm, respectively (P = 0.48). Thus, there was neither a significant change in atherosclerosis burden nor a reduction in cardiovascular events, regardless of antihypertensive agent used in this trial.
In summarizing the utility of QCA in assessing the effects of medical treatment of CAD, we can state that there is considerable dissociation between the angiographic changes induced by statin therapy and their clinical effects, suggesting that pleiotropic effects of statins are very important [19]. These include the prevention of white blood cells attachment to the endothelial cells, attenuation of platelet reactivity, and reduction in secretion of CD40 ligand from platelets and anti-inflammatory effects. In general, changes in lumen dimensions are very modest and reflect the fact that most of the atherosclerotic plaque in patients with less than critical CAD resides in the vessel wall, and cannot be reliably imaged with coronary angiography. While this statement reflects our current understanding of CAD pathophysiology, it is notable that even IVUS cannot detect major changes in plaque volume after treatment with statins. For example, in ASTEROID (A Study to Evaluate the Effect of Rosuvastatin on Intravascular Ultrasound-Derived Coronary Atheroma Burden), rosuvastatin lowered LDL from 130 to 60 mg/dL (53 %, P < 0.001). Yet mean percent atheroma volume (PAV), the primary endpoint, decreased by only 0.98 % (P < 0.001) [20]. The totality of these data suggests that the effect of statins in the medical therapy of CAD is exerted via stabilization of plaque and not via significant change in atherosclerosis burden.
QCA in Studies of Intravascular Devices
Ever since PCI became available more than 30 years ago, procedural success was defined by two important criteria—adequacy of flow in the treated artery (TIMI flow grade) and residual diameter stenosis. Furthermore, the long-term success of the procedure has been defined by the maintenance of vessel patency at the treated site, expressed as DS at a follow-up angiogram. Interventional cardiologists are quite adept at assessing DS, particularly when classifying it in major categories based on clinical significance. Gottsauner-Wolf et al. compared visual estimate of DS with QCA in 30 patients and found excellent correlation, supported by functional assessment with dipyridamole stress test, for stenoses >50 and >75 % [21].
The most important contribution of QCA to the field of interventional cardiology is the ability to consistently and systematically evaluate early and late results of PCI. LLL has become a surrogate endpoint for the efficacy of new interventional devices and was accepted by regulatory agencies as an important endpoint in clinical trials. The introduction of bare-metal stents (BMS) in the late 1980s and drug-eluting stents (DES) in the early 2000s was made possible by this process. Compared with balloon angioplasty (PTCA) alone, stenting with BMS has reduced significantly LLL and the incidence of restenosis (BAR). In the landmark BENESTENT study, 520 patients were assigned to PTCA or BMS. Repeat angiography was performed in 93 % of the eligible patients and the primary angiographic endpoint was MLD at follow-up. MLD at follow-up was 1.73 mm vs. 1.82 mm, respectively, P = 0.09 but restenosis decreased from 32 % for PTCA to 22 % with BMS, P = 0.02. The study elegantly demonstrated the principle that BMS achieves a larger initial lumen after procedure than PTCA (2.48 mm vs. 2.05 mm, P < 0.001) but there is greater late loss in follow-up (0.65 mm vs. 0.32 mm, P < 0.001), resulting ultimately in a larger MLD at follow-up. The concept was compared by Kuntz et al. to a “higher tax paid on a higher income,” resulting eventually in a larger net income [22]. In a similarly designed study, the STRESS (STent REstenosis Study) Investigators randomized 410 patients to PTCA or BMS, with 6 month follow-up angiography, which was performed in 88 % of eligible patients. The primary endpoint was BAR. Patients assigned to BMS had larger acute gain (1.72 vs. 1.23 mm, P < 0.001), larger late loss (0.74 mm vs. 0.38 mm, P < 0.001) and larger net gain (0.98 mm vs. 0.80 mm, P = 0.01), compared with PTCA patients. Restenosis occurred in 31.6 % and 42.1 % of the groups, respectively, P = 0.046.
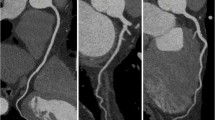
Many subsequent analyses have confirmed that BMS results in LLL of 0.7–1.0 mm. DES revolutionized interventional cardiology because of their ability to reduce neointimal proliferation and restenosis. In a meta-analysis of 29 trials comparing various DES with nearly 9,000 patients undergoing follow-up, protocol-mandated angiography, LLL proved to be an excellent indicator of BAR (R 2 = 0.5301; P < 0.0001) and target vessel revascularization (TVR−R 2 = 0.4604; P < 0.0001) [23]. These data extended across five major platforms of DES (Figs. 3.1 and 3.2) and showed LLL of 0.13–0.56 mm. DES containing sirolimus or its analogues had TVR as low as 2.8 % (Table 3.1). Importantly, there was no threshold in this relationship, meaning that the lower LLL was, the lower the probability for revascularization was as well. Nearly 75 % of patients with angiographic restenosis needed TVR.
Relationship between in-stent loss (ISL) and binary angiographic restenosis (Adapted from Brener SJ, Prasad AJ, Khan Z, Sacchi TJ. The relationship between late lumen loss and restenosis among various drug-eluting stents: a systematic review and meta-regression analysis of randomized clinical trials. Atherosclerosis. 2011; 214(1):158–62. With permission from Elsevier)
Relationship between in-stent loss (ISL) and target vessel revascularization (TVR) (Adapted from Brener SJ, Prasad AJ, Khan Z, Sacchi TJ. The relationship between late lumen loss and restenosis among various drug-eluting stents: a systematic review and meta-regression analysis of randomized clinical trials. Atherosclerosis. 2011;214(1):158–62. With permission from Elsevier)
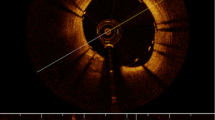
Beyond measurements of lumen size and evaluation of restenosis, QCA provides important insight into the process of reperfusion in patients with ST-elevation myocardial infarction (STEMI). Grading of flow in the infarct-related artery (IRA) after treatment with fibrinolytic therapy or with primary PCI provides critical prognostic information regarding survival. Using the TIMI classification [24], it was shown convincingly that patients with TIMI 3 flow in the IRA have better survival than those with lesser grades. In an analysis of two large STEMI trials with over 5,000 patients, final TIMI 3 flow increased survival at 1 year threefold, compared with TIMI 0–2 (HR = 3.67 [2.45, 5.48], P < 0.001) [25]. Because TIMI flow classification is semiquantitative, a fully quantitative evaluation of flow—corrected TIMI frame count (cTFC)—was developed by Gibson et al. [26]. They showed that flow was disturbed not only in IRA, but also in non-culprit arteries, compared with normal arteries in patients without STEMI (39.2 ± 20.0 vs. 25.5 ± 9.8 vs. 21.0 ± 3.1, P < 0.001), reflecting the heightened platelet reactivity and vascular tone in the former group. The same group extended these observations in patients treated with fibrinolytic therapy for STEMI and showed that cTFC was an independent predictor of survival at 2 years (P = 0.01), after adjusting for important baseline characteristics and revascularization [27].
Even more important than epicardial flow is the tissue myocardial perfusion after STEMI. Ito et al. were among the first to demonstrate that nearly 40 % of patients with successful reperfusion of the IRA have no-reflow at the myocyte level, using myocardial contrast echocardiography. Patients with no-reflow had adverse ventricular remodeling, more heart failure, and other adverse outcomes [28]. Thus, accurate evaluation of myocardial reperfusion after primary PCI may help the operator tailor therapy, in the angiography suite and after the procedure, to the risk for adverse events. Myocardial reperfusion, or “blush score,” can be assessed using two paradigms. The dynamic method (TIMI myocardial perfusion grade—TMPG) assesses the entry and exit of contrast from the myocardium distal to initial IRA lesion [29]. The densitometric method (myocardial blush grade—MBG) compares the density of contrast opacification of the IRA territory to a reference territory [30]. Assessment of MBG can be computerized [31]. Both scales use grades from 0 to 3 and grades 2 or 3 indicate an open microcirculation [32]. In the HORIZONS AMI (Harmonizing Outcomes with Revascularization and Stents in AMI), myocardial reperfusion was assessed independently by both methods. Both TMPG 2 or 3 (HR = 0.53 [0.38, 0.73], P < 0.0001) and MBG 2 or 3 (HR = 0.54 [0.40, 0.75], P < 0.0001) were significant independent predictor survival at 3 years, even after adjusting for TIMI flow grade in IRA [33].
The principal limitation of QCA is its insensitivity to the functional significance of coronary stenoses. Recent advances in CT imaging promise to resolve this deficiency [34].
In summary, QCA plays a critical role in assessing the efficacy of intravascular devices and procedures. There is a robust correlation between measures of lumen loss and angiographic and clinical restenosis, which lead to TVR. QCA can reliably differentiate between the antiproliferative effects of various DES platforms and serves as an excellent surrogate endpoint for stent-vs.-stent comparisons. QCA-derived parameters of reperfusion are powerful predictors of survival and freedom from adverse events after STEMI.
Conclusions
Systematic and consistent evaluation of angiographic parameters has contributed significantly to improvements in CAD therapy, both for pharmacological interventions and for intravascular devices and procedures. Accurate measurement of changes in lumen and plaque size has highlighted the important dissociation between atherosclerosis regression and prevention of ischemic cardiac events. Changes in lumen size and even in plaque volume are small, yet they are associated with an important reduction in clinical events, suggesting that plaque modification and stabilization is more important than the change in size, particularly in earlier stages of the disease. Technologies geared at assessing plaque composition and vulnerability are much more critical to this field than QCA.
In contrast, the development and approval of intravascular devices is critically linked to QCA. Surrogate endpoints of most clinical trials incorporate angiographic parameters. QCA has proven able to differentiate between devices with reliability and accuracy. There is robust correlation between angiographic endpoints of lumen size and reperfusion and clinical endpoints.
References
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart Disease and Stroke Statistics–2011 Update: A report from the American Heart Association. Circulation. 2011;123(4):e18–209. Epub 2010/12/17.
Libby P. Changing concepts of atherogenesis. J Intern Med. 2000;247(3):349–58.
Libby P, Ridker PM, Maseri A. Inflammation and Atherosclerosis. Circulation. 2002;105(9):1135–43.
Libby P, Theroux P. Pathophysiology of Coronary Artery Disease. Circulation. 2005;111(25):3481–8.
Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ. Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med. 1987;316(22):1371–5.
Brown B, Bolson E, Frimer M, Dodge H. Quantitative coronary arteriography. Estimation of dimensions, hemodynamic resistance, and atheroma mass of coronary artery lesions using the arteriogram and digital computation. Circulation. 1977;55:329–37.
Brown B, Bolson E, Dodge H. Quantitative computer techniques for analyzing coronary arteriograms. Prog Cardiovasc Dis. 1986;28:403–18.
Brown G, Albers JJ, Fisher LD, Schaefer SM, Lin JT, Kaplan C, et al. Regression of coronary artery disease as a result of intensive lipid-lowering therapy in men with high levels of apolipoprotein B. N Engl J Med. 1990;323(19):1289–98.
Jukema JW, Bruschke AV, van Boven AJ, Reiber JH, Bal ET, Zwinderman AH, et al. Effects of lipid lowering by pravastatin on progression and regression of coronary artery disease in symptomatic men with normal to moderately elevated serum cholesterol levels. The Regression Growth Evaluation Statin Study (REGRESS). Circulation. 1995;91(10):2528–40.
O’Keefe Jr JH, Cordain L, Harris WH, Moe RM, Vogel R. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol. 2004;43(11):2142–6. Epub 2004/06/03.
Robinson JG, Smith B, Maheshwari N, Schrott H. Pleiotropic effects of statins: benefit beyond cholesterol reduction?: A meta-regression analysis. J Am Coll Cardiol. 2005;46(10):1855–62.
Brugts JJ, Yetgin T, Hoeks SE, Gotto AM, Shepherd J, Westendorp RG, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ. 2009;338:b2376.
Gotto Jr AM. Review of primary and secondary prevention trials with lovastatin, pravastatin, and simvastatin. Am J Cardiol. 2005;96(5A):34F–8. Epub 2005/08/30.
Brown BG, Hillger LA, Lewis C, Zhao XQ, Sacco D, Bisson B, et al. A maximum confidence approach for measuring progression and regression of coronary artery disease in clinical trials. Circulation. 1993;87(3 Suppl):II66–73.
Tulenko TN, Brown J, Laury-Kleintop L, Khan M, Walter MF, Mason RP. Atheroprotection with amlodipine: cells to lesions and the PREVENT trial. Prospective Randomized Evaluation of the Vascular Effects of Norvasc Trial. J Cardiovasc Pharmacol. 1999;33 Suppl 2:S17–22.
Pitt B, Byington RP, Furberg CD, Hunninghake DB, Mancini GB, Miller ME, et al. Effect of amlodipine on the progression of atherosclerosis and the occurrence of clinical events. PREVENT Investigators. Circulation. 2000;102(13):1503–10. Epub 2000/09/27.
Nissen SE, Tuzcu EM, Libby P, Thompson PD, Ghali M, Garza D, et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA. 2004;292(18):2217–25.
Brener SJ, Ivanc TB, Poliszczuk R, Chen M, Tuzcu EM, Hu T, et al. Antihypertensive therapy and regression of coronary artery disease: insights from the Comparison of Amlodipine versus Enalapril to Limit Occurrences of Thrombosis (CAMELOT) and Norvasc for Regression of Manifest Atherosclerotic Lesions by Intravascular Sonographic Evaluation (NORMALISE) trials. Am Heart J. 2006;152(6):1059–63. Epub 2006/12/13.
Ray KK, Cannon CP. The potential relevance of the multiple lipid-independent (Pleiotropic) effects of statins in the management of acute coronary syndromes. J Am Coll Cardiol. 2005;46(8):1425–33.
Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006;295(13):1556–65.
Gottsauner-Wolf M, Sochor H, Moertl D, Gwechenberger M, Stockenhuber F, Probst P. Assessing coronary stenosis. Quantitative coronary angiography versus visual estimation from cine-film or pharmacological stress perfusion images. Eur Heart J. 1996;17(8):1167–74. Epub 1996/08/01.
Kuntz RE, Gibson CM, Nobuyoshi M, Baim DS. Generalized model of restenosis after conventional balloon angioplasty, stenting and directional atherectomy. J Am Coll Cardiol. 1993;21(1):15–25. Epub 1993/01/01.
Brener SJ, Prasad AJ, Khan Z, Sacchi TJ. The relationship between late lumen loss and restenosis among various drug-eluting stents: a systematic review and meta-regression analysis of randomized clinical trials. Atherosclerosis. 2011;214(1):158–62. Epub 2010/12/03.
The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group. N Engl J Med. 1985;312(14):932–6.
Brener SJ, Mehran R, Brodie BR, Guagliumi G, Witzenbichler B, Cristea E, et al. Predictors and implications of coronary infarct artery patency at initial angiography in patients with acute myocardial infarction (from the CADILLAC and HORIZONS-AMI Trials). Am J Cardiol. 2011;108(7):918–23. Epub 2011/07/19.
Gibson CM, Cannon CP, Daley WL, Dodge Jr JT, Alexander Jr B, Marble SJ, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996;93(5):879–88.
Gibson CM, Cannon CP, Murphy SA, Marble SJ, Barron HV, Braunwald E. Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction. Circulation. 2002;105(16):1909–13.
Ito H, Maruyama A, Iwakura K, Takiuchi S, Masuyama T, Hori M, et al. Clinical implications of the ‘no reflow’ phenomenon. A predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction. Circulation. 1996;93(2):223–8.
Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation. 2000;101(2):125–30.
van’t Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation. 1998;97(23):2302–6.
Vogelzang M, Vlaar PJ, Svilaas T, Amo D, Nijsten MW, Zijlstra F. Computer-assisted myocardial blush quantification after percutaneous coronary angioplasty for acute myocardial infarction: a substudy from the TAPAS trial. Eur Heart J. 2009;30(5):594–9.
Poli A, Fetiveau R, Vandoni P, del Rosso G, D’Urbano M, Seveso G, et al. Integrated analysis of myocardial blush and ST-segment elevation recovery after successful primary angioplasty: Real-time grading of microvascular reperfusion and prediction of early and late recovery of left ventricular function. Circulation. 2002;106(3):313–8. Epub 2002/07/18.
Brener SJ, Cristea E, Mehran R, Dressler O, Lansky AJ, Stone GW. Relationship between angiographic dynamic and densitometric assessment of myocardial reperfusion and survival in patients with acute myocardial infarction treated with primary percutaneous coronary intervention: The Harmonizing Outcomes with Revascularization and Stents in AMI (HORIZONS-AMI) trial. Am Heart J. 2011;162(6):1044–51. Epub 2011/12/06.
Ko BS, Cameron JD, Meredith IT, Leung M, Antonis PR, Nasis A, et al. Computed tomography stress myocardial perfusion imaging in patients considered for revascularization: a comparison with fractional flow reserve. Eur Heart J. 2012;33(1):67–77. Epub 2011/08/04.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Brener, S.J. (2014). Evaluation of Medical Therapies and Intravascular Devices with Quantitative Coronary Angiography. In: Nicholls, S., Crowe, T. (eds) Imaging Coronary Atherosclerosis. Contemporary Cardiology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-0572-0_3
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0572-0_3
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-0571-3
Online ISBN: 978-1-4939-0572-0
eBook Packages: MedicineMedicine (R0)