Abstract
The use of ultrasound in the imaging of abdominal vascular structures has become commonplace in the evaluation and management of patients with vascular disease. Because it is noninvasive, portable, and repeatable, it holds advantages over other imaging modalities that require ionizing radiation, intravenous contrast, or transportation away from a typical patient care environment. While the quality of ultrasound imaging is user dependent, increasing familiarity with its uses and limitations has allowed it to become the study of choice to both initially and definitively identify disease and guide treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Abdominal Aortic Aneurysm
- Abdominal Aortic Aneurysm
- Intravascular Ultrasound
- Pulse Repetition Frequency
- Celiac Trunk
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Significant advances in technology have resulted in both better visualization and the development of smaller and more portable ultrasound units. The combination of brightness mode (B-mode) imaging with Doppler analysis, or so-called duplex ultrasound (DUS), has been a long-standing tool of the vascular surgeon. An understanding of the capabilities of the vascular laboratory is a central piece of the educational curriculum of vascular trainees; no other imaging modality plays as central a role in the overall care of the vascular patient. While the physical principles of ultrasound are discussed elsewhere, an understanding of ultrasound physics, in particular, the Doppler equation, is a key concept in the use of DUS.
Ultrasound Physics
Sound is the propagation of an energy wave through vibration of particles that make up the medium through which the sound travels. The wave proceeds as a succession of an area of high pressure, known as compression, followed by an area of low pressure, known as rarefaction. Every sound wave has a wavelength that is determined by the distance between the peaks (or troughs) of the energy wave. The number of these pulses that pass in a given period of time refers to the wave frequency (cycles per second, or Hertz). The human ear can detect a frequency between approximately 20 and 20,000 Hertz (Hz). Ultrasound represents higher-frequency sound and those frequencies used in medical applications typically fall between 2 and 20,000 megahertz (MHz).
The Doppler effect refers to the predictable change in frequency of a sound wave that is produced by the relative motion between a sound source and a listener. In the case of DUS, Doppler shifts occur between the frequency of the transmitted and reflected sound wave when it encounters a moving object. In the bloodstream, the red blood cells act as the spectral reflectors. This frequency shift is directly proportional to the velocity of the moving reflector. The angle between the incident ultrasound beam and the direction of blood flow also affects the frequency shift. In clinical practice, this angle is defined as the angle between the axis of the ultrasound beam and the adjacent vessel wall. This is based on the assumption that blood cell motion is parallel to the vessel wall. By convention, an angle of 60° is used to obtain Doppler velocity measurements.
The simplest clinical use of Doppler does not require either simultaneous B-mode ultrasound or determination of the Doppler angle. Pocket-sized Doppler machines, known as continuous-wave or CW Doppler, are often used to determine the presence of arterial flow such as when measuring ankle-brachial indices. These instruments house both a transmitting and receiving element into a single transducer, sometimes shaped like a pencil (so-called pencil Doppler). Because they are unable to identify flow at a specific depth or site within the body, multiple vessels in the path of the sound beam result in a combination of superimposed signals.
The use of pulsed Doppler, along with B-mode imaging, overcomes this limitation, by allowing measurement of the velocity of blood in a specific location or sample volume. In this case, a single ultrasound transducer alternates between sending a short burst or pulse of ultrasound and then receiving the returning signal. The B-mode image provides the distance from the probe to the sample volume, which allows the machine to calculate the time required for the pulse to be sent and then subsequently received (see Fig. 9.1).
Spectral Broadening: Normal arterial flow is laminar, and spectral waveforms taken in a discrete sample volume will display a relatively narrow band of frequencies. In areas of stenosis or other abnormalities that disrupt laminar flow, these disturbances will display a broader range of frequencies at any given point in time. This increase in width of the displayed frequency shifts is referred to as spectral broadening and along with increases in the peak-systolic and end-diastolic velocities is used as a criterion to define stenosis within arterial beds (see Fig. 9.2).
Aliasing: One of the physical limitations of ultrasound is the frequency at which ultrasound pulses can be sent in order to ensure that the reflected signal from each pulse is received before the transmission of the next pulse. The limitation of this pulse repetition frequency (PRF) is defined as
where C is the speed of sound in tissue and d is the distance from the transducer to the sample volume. Higher PRF values result in more ultrasound pulses to provide a better representation of the Doppler signal. When the pulsed Doppler provides less than two samples for each cycle of the Doppler signal, a phenomenon called aliasing occurs where the spectral waveform appears to be “cut off” and then “wraps around” and appears as flow below the baseline. This is an artifact of the sampling process and can occur in an area with high flow velocity, such as a jet of blood associated with a severe stenosis, or in deep structures where low PRF values are needed to detect flow due to the attenuation of the additional tissue. The same effect can be seen in color flow imaging, where aliasing results in flow appearing to be present in opposite directions (colors) at a single sample volume. This is often referred to as a “color bruit” (see Fig. 9.3a, b).
Aliasing. (a) Sagittal view of the aorta where the relationship between the pulse repetition frequency and velocity causes the spectral waveform to be cut off (small arrow) and wrap around below the baseline (large arrow). (b) Color flow used in sagittal view of the same aorta as in (a). While multiple colors (color bruit) suggest turbulence, this is in fact an artifact of aliasing
Anatomy
Vascular structures in the abdomen and retroperitoneum that are typically imaged with ultrasound include the aorta and its branches, as well as the vena cava and associated branches, and the portal circulation. Variations in anatomy can provide challenges, but many of these variations are well described, and an experienced technician can typically identify them. Obesity provides perhaps the greatest challenge to accurate identification of disease within the abdominal vascular structures. Bowel gas also limits visualization and these tests are best performed in the morning or at a time when the patient has had limited oral intake to limit associated bowel gas.
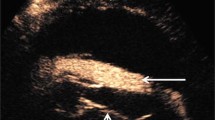
Aorta: The abdominal aorta lies in the retroperitoneum and is typically imaged from the midline. Lower-frequency transducers will sacrifice resolution but are required to adequately image structures at this depth. An ultrasound unit with color flow Doppler capabilities is necessary, and proper imaging requires range-gated spectral Doppler that has the ability to adjust the depth and position of the range gate within the area of interest. Both longitudinal and transverse views are required to assess the aorta for flow and size. The aorta should be visualized in its proximal, mid-, and distal portions, and aneurysm size should be determined at its widest diameter measured outer wall to outer wall (see Fig. 9.4a, b).
(a) Gray-scale sagittal image of the aorta visualizing the proximal aorta (large arrow), celiac trunk (hollow arrow), and superior mesenteric artery (small arrows). Note the use of the liver as an acoustic window to visualize the proximal aorta. (b) Gray-scale transverse view of the aorta and adjacent inferior vena cava (IVC). The liver is used as an acoustic window
Visceral/Renal Arteries: Imaging of these vessels in any significant detail is best performed in a qualified and accredited facility by experienced operators. These challenging studies require a thorough understanding of both typical and variant anatomy among these adjacent structures. The celiac trunk and the superior mesenteric artery, the two most cephalad aortic branches, can be imaged in both a transverse and longitudinal axis. From a transverse image, the celiac trunk can be followed to its bifurcation into the splenic and hepatic arteries. The superior mesenteric artery can be visualized at its origin from the aorta in a longitudinal plane, with the left renal vein seen between it and the aorta. The renal arteries can also be imaged from an anterior position; however, in order to accurately identify and quantify flow in the distal arteries, a flank approach may be necessary with the kidney serving as an acoustic window (see Figs. 9.5a, b, 9.6a, b and 9.7a, b).
(a) Longitudinal view of the aorta with Doppler interrogation of origin of the celiac trunk. Peak systolic velocity is 205 cm/s suggesting no evidence of significant stenosis. (b) Transverse view of the celiac trunk and hepatic and splenic arteries. Color flow is useful to identify vascular structures
(a) Longitudinal view of the aorta with Doppler interrogation of origin of the superior mesenteric artery. Peak systolic velocity is 271.6 cm/s suggesting no evidence of significant stenosis. (b) Transverse view of the aorta (AO) and superior mesenteric artery (SMA), with the left renal vein (LRV) interposed between as it empties into the inferior vena cava (IVC). Note the similarity between this and a familiar view from cross-sectional imaging such as CT or MRI
(a) Transverse view of the right renal artery (RA) as it exits the aorta (AO) and lies posterior to the inferior vena cava (IVC). RV renal vein, RT KID right kidney. (b) The distal renal artery (RA DIST) may sometimes need to be imaged by placing the transducer on the flank and using the kidney (arrows) as an acoustic window
Vena Cava: The vena cava is imaged in a similar fashion to the abdominal aorta. Transverse and longitudinal views can be used, and color flow is often helpful to identify these large vascular structures that lie in the retroperitoneum. The vena cava can be imaged both centrally (at the hepatic vein confluence) and more distally (between the renal veins and the caval bifurcation). Overlying bowel gas is the most consistent challenge to overcome adequate imaging of these structures (see Fig. 9.8a, b).
Portal Venous Structures: Diagnostic imaging of the hepatoportal system is best left to the highly trained technicians in the vascular laboratory and radiology suite and to those who perform routine intraoperative assessment (see Chap. 15). An understanding of these structures can be helpful for diagnostic and therapeutic interventions on the liver, which is discussed elsewhere (see Chap. 16) (see Fig. 9.9).
Application
Aneurysmal Disease: Perhaps the most common application of abdominal vascular ultrasound is to identify and determine the size of abdominal aortic aneurysms (AAA). Because it is noninvasive and portable, ultrasound is the study of choice when assessing AAA. B-mode ultrasound can identify the maximum diameter of the AAA, as well as extension of aneurysmal disease into the paravisceral aorta and the iliac arteries. For the general surgeon, the use of ultrasound for the diagnosis of AAA falls into two basic categories: acute and chronic.
Acute Diagnosis: In the acute setting, the old axiom “gray hair + back pain = ruptured aortic aneurysm until proven otherwise” still holds true. While rapid diagnosis and treatment are important to obtain good outcomes, it is just as important to be able to exclude the presence of AAA to allow other diagnoses to be considered. The performance of surgeon-performed ultrasound by appropriately trained providers clearly has a role in this abbreviated and directed study [1–3]. Perhaps the greatest impediment is the presence of overlying bowel gas that can make imaging more challenging. While rapid diagnosis can allow patients to be taken straight to surgery, adequate preoperative planning with the use of cross-sectional imaging (CT scanning) is becoming more common, particularly in the endovascular era (see Fig. 9.10a–c).
Chronic Diagnosis and Follow-up: The majority of AAA are not detectable on physical examination [4]. Imaging is most commonly performed in a dedicated radiology or vascular laboratory and typically includes assessment for screening purposes, suspected physical findings, or follow-up [5]. Screening is currently recommended in certain populations by the U.S. Preventive Services Task Force with follow-up studies performed at routine intervals depending on aneurysm size [6]. DUS evaluation of endovascular repair of abdominal aortic aneurysms continues to be studied and compared to CT scan for the detection of endoleaks [7]. Because of the hazards of ionizing radiation and contrast nephropathy, ultrasound clearly has a role in the postoperative surveillance of these patients [4] (see Fig. 9.11a, b).
(a) Gray-scale transverse image of residual abdominal aortic aneurysm sac after endovascular repair of aortic aneurysm (EVAR). Note the presence of the graft limbs within the aneurysm sac (arrows). The residual sac measures 5 cm. (b) Color flow image showing no evidence of endoleak, i.e., no flow outside of the graft limbs that is within the aneurysm sac
Vascular Stenoses and Occlusions: DUS can provide a significant amount of information in real-time regarding blood flow. Using the Doppler equation, velocity measurements within a particular vessel can be made which can then provide reproducible estimates of degrees of stenosis based on these velocities or on the ratio of the velocity relative to the velocity in an adjacent vessel. Well-established criteria exist for determining degrees of stenosis within the iliac, mesenteric, and renal vessels (see Fig. 9.12).
Venous: Ultrasound evaluation of the vena cava and iliac veins is helpful to determine the extent of deep venous thrombosis that originates in the lower extremities. As in the lower extremities, DUS can not only diagnose thrombotic occlusions but can also identify reflux, such as postthrombotic reflux from dysfunctional valves that have been recanalized after previous deep venous thrombosis. Valve closure times greater than 0.5 sec are generally defined as significant reflux [8]. In those patients undergoing intervention such as endoluminal angioplasty and/or stenting, intravascular ultrasound plays a significant adjunctive role to contrast venography to determine the size and length of the devices to be used (see Fig. 9.13).
Longitudinal view of the iliac vein demonstrating reflux. At time 0 (−5 on the horizontal scale), venous flow is toward the heart. Valsalva maneuver (large arrow) produces sustained reversal of flow in the iliac vein which persists approximately 2.5 s (small arrow). A total of 5 s of data is collected in this spectral analysis
Portal: Assessment of portal venous blood flow is an excellent application of DUS. While operator dependent, it is a noninvasive and repeatable method to assess the portal circulation. Thrombosis of the splenoportal circulation is readily identified with ultrasound and can be used as a surveillance imaging modality for splenoportal thrombosis after surgical intervention such as splenectomy [9]. With the use of color flow and spectral analysis, hepatopetal (toward the liver) and hepatofugal (from the liver) flow directions can be determined. Using flow characteristics as well as B-mode diameter measurements, estimates of portal venous flow and pressures can then be made [10, 11] (see Fig. 9.14a, b).
Intervention
Unlike the peripheral vessels, direct percutaneous access to the visceral vessels is uncommon, and thus ultrasound-guided percutaneous abdominal vascular interventions are relatively rare. The use of intraoperative ultrasound, however, is quite helpful to assess the adequacy of mesenteric vascular reconstructions such as bypass or endarterectomy. In these circumstances, velocity elevations relative to the adjacent vessel can identify areas that may require technical correction, such as retained vein valves in a bypass conduit, anastomotic stenoses, or residual plaque at an endarterectomy site.
While the use of intravascular ultrasound (IVUS) is beyond the scope of this text, its use has become significant in abdominal vascular interventions, including endoluminal interventions such as balloon angioplasty or stenting, as well as during placement of abdominal aortic endografts. Catheters with lower frequencies (relative to those used in coronary applications) allow identification of visceral branches within the aorta and can lessen the amount of intravenous contrast required during complex endovascular reconstructions. In the treatment of arterial occlusive disease, IVUS interrogation after stent placement can be used to determine the adequacy of stent apposition against the arterial wall. Finally, IVUS can more accurately determine intraluminal diameters, optimizing size selection of devices, particularly when dealing with central venous reconstructions.
The use of ultrasound to direct placement of vena cava filters has been well described with both transabdominal and intravascular ultrasound [12–14]. The limitations of poor visualization using transabdominal ultrasound, particularly in the obese patient, have been overcome by the use of intravascular ultrasound. As smaller-diameter probes have become available, this can be performed through acceptably small-diameter sheaths. Both double-puncture and single-puncture techniques are well described, with excellent results [14].
Conclusion
Because of its noninvasiveness, repeatability, and portability, ultrasound plays a key role in the imaging of the vascular structures of the abdomen and retroperitoneum. Experience, an awareness of anatomic variations, and a healthy amount of patience will lead to the best results. In any given individual, optimal DUS imaging of the vascular structures may be accomplished through various angles, planes, and acoustic windows. The number of nondiagnostic or incomplete studies can be limited by performing these studies as early in the day as possible to minimize the effects of overlying bowel gas. Additionally, at times success will be achieved when the study is performed at another time or by another sonographer. Because the quality of the study is highly operator dependent, familiarity with the physical principles of ultrasound and the Doppler equation allows an understanding of the strengths and limitations of the use of ultrasound in this setting.
References
Hendrickson RG, Dean AJ, Costantino TG. A novel use of ultrasound in pulseless electrical activity: the diagnosis of an acute abdominal aortic aneurysm rupture. J Emerg Med. 2001;21:141–4.
Kuhn M, Bonnin RL, Davey MJ, Rowland JL, Langlois SL. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000;36:219–23.
Shuman WP, Hastrup Jr W, Kohler TR, Nyberg DA, Wang KY, Vincent LM, Mack LA. Suspected leaking abdominal aortic aneurysm: use of sonography in the emergency room. Radiology. 1988;168:117–9.
Chaikof EL, Brewster DC, Dalman RL, Makaroun MS, Illig KA, Sicard GA, Timaran CH, Upchurch GR, Veith FJ. The care of patients with an abdominal aortic aneurysm: the Society for Vascular Surgery practice guidelines. J Vasc Surg. 2009;50:2–49S.
Thompson SG, Ashton HA, Gao L, Buxton MJ, Scott RA. Final follow-up of the Multicentre Aneurysm Screening Study (MASS) randomized trial of abdominal aortic aneurysm screening. Br J Surg. 2012;99:1649–56.
Screening for abdominal aortic aneurysm. Clinician Fact Sheet. June 2009. Rockville: Agency for Healthcare Research and Quality; 2009. http://www.ahrq.gov/clinic/cvd/aaaprovider.htm
Manning BJ, O’Neill SM, Haider SN, Colgan MP, Madhavan P, Moore DJ. Duplex ultrasound in aneurysm surveillance following endovascular aneurysm repair: a comparison with computed tomography aortography. J Vasc Surg. 2009;49:60–5.
Raju S, Hollis K, Neglen P. Obstructive lesions of the inferior vena cava: clinical features and endovenous treatment. J Vasc Surg. 2006;44:820–7.
Tran T, Demyttenaere SV, Polyhronopoulos G, Séguin C, Artho GP, Kaneva P, Fried GM, Feldman LS. Recommended timing for surveillance ultrasonography to diagnose portal splenic vein thrombosis after laparoscopic splenectomy. Surg Endosc. 2010;24:1670–8.
Chow PK, Yu WK, Ng TH, Ong HS, Ooi PJ, Chan ST, Aw SE, Soo KC. Influence of respiration and portal pressure on transabdominal duplex Doppler ultrasound measurement of portal blood flow: a porcine model for experimental studies. J Surg Res. 2000;89: 66–73.
Singal AK, Ahmad M, Soloway RD. Duplex Doppler examination of the portal venous system: an emerging novel technique for the estimation of portal vein pressure. Dig Dis Sci. 2010;55:1230–40.
Corriere MA, Passman MA, Guzman RJ, Dattilo JB, Naslund TC. Comparison of bedside transabdominal duplex ultrasound versus contrast venography for inferior vena cava filter placement: what is the best imaging modality? Ann Vasc Surg. 2005;19:229–34.
Kassavin DS, Constantinopoulos G. The transition to IVUS-guided IVC filter deployment in the nontrauma patient. Vasc Endovascular Surg. 2011;45:142–5.
Jacobs DL, Motaganahalli RL, Peterson BG. Bedside vena cava filter placement with intravascular ultrasound: a simple, accurate, single venous access method. J Vasc Surg. 2007;46:1284–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Calderon, D.R., Han, D.C. (2014). Abdominal/Retroperitoneal Vascular Ultrasound. In: Hagopian, E., Machi, J. (eds) Abdominal Ultrasound for Surgeons. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9599-4_9
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9599-4_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9598-7
Online ISBN: 978-1-4614-9599-4
eBook Packages: MedicineMedicine (R0)