Abstract
Novice clinicians vary greatly in physical examination (PE) skill levels. In this chapter, the authors define common PE deficits, explore institutional and educator constraints to educating about physical exam skills, describe methods of identifying learners needing remediation, describe potential tools that can be used in remediation, and, finally, revisit each of the major PE skills deficit domains with illustrative cases and specific remediation strategies for those cases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Clinical Reasoning
- Necrotizing Fasciitis
- Remediation Strategy
- Deliberate Practice
- Physical Examination Skill
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
“Observe, record, tabulate, communicate. Use your five senses. Learn to see, learn to hear, learn to feel, learn to smell, and know that by practice alone you can become expert.”
—Sir William Osler [1]
1 Introduction
Novice clinicians demonstrate a diversity of physical examination (PE) skill levels. Learners’ approaches to and facility with the PE are influenced by many factors, ranging from knowledge and application of physiology and pathophysiology, to personal biases and perceptions, to workplace-based experiences (the “hidden curriculum”) during the preclinical years and clerkships. In this chapter, we will briefly name and define common areas of deficits for PE skills, describe methods of identifying learners needing remediation, describe potential tools that can be used in remediation, and, finally, revisit each of the major PE skills deficit domains with illustrative cases and specific remediation strategies. Notably, there is usually some overlap between domains, and students often exhibit more than one deficit.
2 Deficit Domains for Physical Examination Skills
Deficit domains for physical examination skills
-
1.
Basic motor and technical skills
-
2.
Experience and medical knowledge
-
3.
Interaction
-
4.
Clinical reasoning
2.1 Motor/Technical Skills Deficits
Typically, these deficits are readily observable in the mechanical delivery of the skill—for example, palpating the thyroid incorrectly, insufficient force when percussing the lungs or abdomen to produce adequate percussion tones, or auscultating using the bell of the stethoscope instead of the diaphragm.
These types of deficits, however, may indicate more complex educational system issues. Students often learn the mechanics of PE skills (for example, auscultating the lungs from one side to the other in at least four places) in classroom settings, on peers, or on standardized patients. This method, though efficient and least disruptive to busy clinical practice, separates the relevance of PE skills from actual clinical contexts. A seasoned clinician, for example, would auscultate the lungs differently in a patient suspected of having a pneumothorax vs. one suspected of being in heart failure. In addition, students quickly pick up poor habits, such as listening to the heart and lungs through the patient’s gown, from residents (or even attendings) on clinical rotations, and remediating faculty should remain aware that this strong hidden curricular force around the PE can thwart their efforts.
2.2 Experiential/Medical Knowledge Deficit
Learners with this type of deficit usually exhibit some ability to perform an appropriately focused exam but have difficulty with one of two types of exam: what to look for in a well-person visit or a follow-up examination for a chronic illness (for example, the PE for an annual check-up or a 3-month diabetes follow-up), or inability to discern subtleties between disease entities (for example, mistakenly identifying the dry “Velcro” crackles of interstitial lung disease as “rales” of congestive heart failure). Unless accompanied by other deficits, this scenario typically represents a teaching opportunity to expand a student’s experience and knowledge base.
2.3 Interactional Deficit
This deficit constitutes a communication skills problem—how learners interact with the patient during the physical exam, and how they communicate physical exam maneuvers, results, and findings. These deficits can range from forgetting to wash their hands, to awkwardly performing aspects of the physical examination, to poor or omitted explanations to the patient about maneuvers the physician is doing, to not recognizing a patient’s confusion during a jargon-filled explanation. (Please refer to Chap. 4 for a more complete discussion of remediating communication deficits.)
2.4 Clinical Reasoning
This may represent the most challenging to diagnose, as there are multiple steps in the clinical reasoning process (see Chap. 6). Many students know how to perform the specific maneuvers or a complete examination but lack the ability to select the relevant (focused) physical exam maneuvers to perform based on a presenting situation: they know “how” to do the exam but not “when” to do the exam [2].
Overall, the problems encountered can be found on a spectrum. At one end, learners demonstrate a complete disconnect or lack of organization. These students may not have generated a list of differential diagnoses prior to initiating the exam. They may not understand that the physical exam is supposed to support and refute the differential diagnoses created. These students perform almost the same exam on every patient and/or do not have an organized approach to the encounter that causes them to miss the diagnostic boat completely. In a clinic setting, this is the student who is the “data collector.” He/she asks the history questions according to a formula, then performs a formulaic exam, presents the findings, and expects the resident or attending to synthesize the information provided. In an exam setting, he/she may run out of time to perform any exam because of a disorganized approach. In the middle of the spectrum is a learner who creates a limited differential diagnosis, and, therefore, a limited and inappropriate exam ensues. This may be due to omitting dangerous entities or often due to premature closure. Alternatively, the learner may create an appropriate differential diagnosis, but not know what they are looking for on exam, or what positive findings represent. Finally, at the other end of the spectrum, and often difficult to differentiate from medical knowledge deficit, the student may not know what specific maneuvers represent or how they help differentiate between disease processes.
3 Identification of Learners
Although seasoned clinicians would ideally observe learners in multiple patient encounters in their entirety to identify PE skills-related deficits in clinical reasoning, knowledge, and/or skill, logistical constraints usually limit this type of comprehensive direct observation and feedback [3]. Often, and more viably, faculty observe learners performing small “essential” parts of an exam, allowing for identification of some technical and interactional deficits. Unfortunately, the format by which most learners’ skill levels are assessed typically relies on conference room-based “rounding”—hearing patient case presentations that include the exam findings [4]. Although rounding efficiently addresses routine patient care issues, it poses inherent challenges to clinicians trying to accurately identify learners’ weaknesses in PE skills.
Without direct observation, the accuracy of findings obtained by student’s examination comes into question. For example, when told that the “neuro exam was unremarkable,” which components of the exam were done? If the learner reports diminished reflexes, is this due to a physiological problem, or were they just poorly elicited? Perhaps the learner didn’t appreciate (or even listen for) a carotid murmur but was “coached” about its presence by a resident. Finally, the interactional component of bedside manner and approach to performing sensitive exam maneuvers cannot be assessed during these rounds. The ultimate danger is that inaccuracies can significantly compromise the validity of patient management plans. As a relevant aside, many have written about a “hidden curriculum” among clinicians denigrating the value of the physical examination because of the presence of laboratory or imaging modalities. Directed teaching and/or assessment of the physical examination can potentially interrupt perpetuation of these myths.
Despite the logistical constraints posed by busy clinical practice, several structured opportunities, all of which require direct observation by seasoned faculty clinicians, allow for the identification of learner weaknesses in PE skills:
-
Bedside teaching—Often used to demonstrate a patient’s exam findings to a group of students or residents (and not intended to put any learner on the spot), bedside rounding can allow a learner to demonstrate PE skills and can effectively highlight motor, experiential, and interactional deficits.
-
Semiformal patient interaction—(e.g., clinical evaluation exercise—CEX, Mini-CEX [5], or BSCOs—Brief Structured Clinical Observations)—These are structured opportunities to observe a learner perform specific parts of a clinical encounter and are more flexible in terms of the setting and time. However, faculty must know that multiple observations are necessary when using these tools to achieve an acceptable level of accuracy in assessing a student’s performance [5].
-
Formally structured skills courses or workshops—These structured learning experiences are specifically designed to teach specific skills (for example, cardiopulmonary or musculoskeletal examination techniques) that use standardized or real patients in small group settings and present opportunities for direct observation of student performance.
-
Formal testing—(e.g., OSCEs—Objective Structured Clinical Examinations using Standardized Patients) [6]—Multiple stations with clinical encounters using standardized patients present opportunities for faculty clinicians to review focused encounters and to identify deficits in clinical reasoning, knowledge, and skills. In addition, standardized patients complete checklists of historical, PE-related, and interactional components of the exam that assess learners’ clinical performance in a standardized setting. These exercises are expensive to carry out and thus would not be ideal for many clinical learning settings [7, 8]. However, especially if they are videotaped, OSCEs can provide objective information about learner performance. For learners with deficits, faculty can review performance with learners, encourage learner self-reflection, and prescribe individualized remediation plans [9–11].
4 Approaches to PE Skills Remediation
Once we identify the learners needing assistance and the scope of the problem, we use a three-step approach:
-
1.
Identification of the students’ deficit(s)
-
2.
Creation of an individualized remediation strategy
-
3.
Reassessment to ensure improvement
Exercises can be categorized into four major types: clinical activities, independent study, precepted video review, and organized group activities [12]. The remediation strategies recommended for the domains below incorporate some combination of these exercises to optimize learning outcomes.
4.1 Deficit Identification
Faculty-Observed Clinical Performance Assessment: This assessment can be achieved by precepted video review or by any of the direct observation opportunities listed above. Certain deficits are clear from direct observations (e.g., technical skills and interactional elements) while others (especially clinical reasoning) must be ascertained by provocative questioning. Leading the learners through the thought process behind why they chose to examine the patient a certain way, what focused exam they would do, or how they would examine correctly if done again is paramount. A self-reflection exercise can help prepare the student for a video review encounter and can also help guide the discussion with the clinical faculty member [11] (Example 5.1).
It is helpful to review either multiple videos or key segments of multiple encounters to see if detected deficits are global or specific to an encounter. This understanding can point to lack of experience or medical knowledge as the source of the deficit.
We name other means of identifying PE skills deficits with the individual cases in the next section.
Example 5.1
Learners’ instructions for a self-reflection exercise while reviewing video recording of their clinical performance examination. A similar exercise can be adapted to assess learners’ thinking in actual clinical settings, rather than in the context of video review; however, video reviews present a distinct advantage in building in time for reflection and metacognition (Chap. 13).
Self-reflection Exercise
There are four QUESTIONS you need to answer for each case. To answer them, you will need to think back to when you were seeing the patient for the first time and reflect on what you were thinking during each of the four segments listed below.
-
1.
Before starting your video, read the Presenting Situation provided in the folder and answer:
“What were you thinking after reading the instructions on the door?”
-
2.
Start the video and stop when you have finished the history taking portion of the encounter and answer:
“What did you think was going on at this point in the encounter? Do you still feel that way?”
-
3.
Start the video again and stop after you have finished the physical exam portion of the encounter and answer:
“What did you think was going on at this point in the encounter? Reflecting back, is there anything that you would have done differently?”
-
4.
Start the video again and stop after you have ended the encounter and answer:
“What do you think about the encounter? Reflecting back, is there anything that you would have done differently?”
Examples of questions to ask during performance review:
-
1.
After completing your history, what are the top (3–5) disease processes in your differential diagnosis in order of likelihood?
-
2.
What are the disease processes you are most concerned about that need to be ruled out?
-
3.
What do you think is going on at this point in the encounter?
-
4.
What pertinent positives or negatives were you looking for or would you look for now?
-
5.
If you were to perform the physical exam again based on this differential, describe what you would do.
-
6.
What examination findings would support or refute that hypothesis?
-
7.
I see that you listened to the [heart]: what were you listening for? How would you change the exam to find what you are looking for?
-
8.
What do you think is the best position for the patient to be in in order to elicit that finding? Why?
4.2 Individualized Remediation Strategies
4.2.1 Real-Time Remediation
We find it highly efficient and meaningful to take learners to the bedside to demonstrate correct PE techniques, discuss underlying physiological rationale for those techniques, and to teach PE pearls (e.g., how to examine a ticklish patient). Obviously, when a more in-depth teaching conversation is needed, teaching at a patient’s bedside may be inappropriate.
4.2.2 Independent Study/Self-directed Learning Exercises
We often pair these activities with other experiential activities (for example, practice interactions with standardized or real patients) in order to establish the fundamental knowledge base needed to learn more skills. Many of these activities can be done alone or in small study groups. Useful exercises include:
-
Listing differential diagnoses for certain chief complaints based on age, gender, and possible comorbidities in order of most common and most dangerous.
-
Creating charts that discriminate which exam findings are consistent with or help discern between different but similar entities (Example 5.2).
-
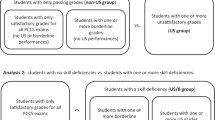
Considering what examination elements would be required in a patient with various chief complaints—can be done as an exercise on a simulated patient (either role play with another student or on paper) (Fig. 5.1).
-
Considering what examination should be performed in a well-person visit when the patient has various underlying medical problems. This is usually a two-step process: first, identification of the possible complications of a disease process, followed by demonstration of an exam to look for those items (Example 5.3).
-
Reading parts of a PE skills textbook or watching videos that elucidate appropriately and correctly performed PE maneuvers. Texts that are organized by cases or chief complaints rather than by organ system may have the added benefit of modeling more accurate and complete examinations.
Example 5.2:
Example of a Focused Physical Exam exercise using a case adapted from the Hypothesis-Driven Physical Examination Student Handbook. [13]
FOCUSED PHYSICAL EXAMINATION EXERCISE
Complaint: Abdominal Pain
Daniel, 40 years old, came to the doctor because he has been experiencing abdominal discomfort on his right side and appetite loss. He has also noticed a low-grade fever over the past few days. He’s been a steady drinker. You are thinking of possible alcoholic hepatitis or cholangitis-cholecystitis. In anticipation of your physical exam of the abdomen, list the positive sign(s) associated with each diagnostic hypothesis.

Example 5.3
Sample exercise—Considering what examination should be performed in a well-person visit when the patient has various underlying medical problems.
What examination would you perform in a 48-year-old man with diabetes at his 3-month visit?
-
1.
Consider the possible complications of diabetes pertaining to each organ system.
-
HEENT
-
Cardiovascular
-
Respiratory
-
Gastrointestinal
-
Genito-urinary
-
Muscular
-
Skin
-
Neurological
-
-
2.
What examination would you perform to evaluate/rule out each of the complications above that you identified? Describe what exam you would do (including special tools used) and specifically what you are looking for (e.g., for a patient with a headache—ophthalmoscopic exam of discs to rule out papilledema).
4.2.3 Clinical Activities Focused on PE Skills
These are activities specific to the learners’ deficits and can be incorporated as part of the regular clinical rotation. Examples include: (1) practice with systematizing approaches to the history and physical exams, (2) practice creating an appropriate differential diagnosis that includes dangerous entities, asking specific questions to rule these in or out and then performing an exam that supports/refutes these entities in the differential, (3) increase the speed and flow of the encounters to improve patient comfort, and (4) practice performing certain examinations (e.g., ophthalmological or cardiovascular exam) on each patient during a clerkship.
4.2.4 Organized Group Activities/Courses
Courses have been designed for third- or fourth-year students specifically to address the deficits identified either via a structured curriculum or faculty teaching at the bedside. They can be faculty-intensive but are often very well attended and appreciated.
-
Advanced diagnostic skills course uses real patients with chronic but stable medical problems to appreciate the subtleties of the physical exam.
-
Teaching pre-clerkship students helps review fundamental PE skills.
-
Hypothesis-driven PE workshops use standardized patients to act out different medical problems to guide learners through the reasoning process in conducting a focused physical examination based on a chief complaint [14, 15].
-
Evidence-based PE workshops that use the Rational Clinical Examination series from the Journal of the American Medical Association to recap basic PE skills and to learn the highest-yield disease-specific PE maneuvers.
4.3 Reassessment
Reassessment can take the form of any of the strategies used for primary assessment. It is most helpful to have an evaluator who is aware of what specific deficit(s) had been the focus of the remediation to ensure it remains a focus in the reassessment.
5 Tailored Remediation for Specific Physical Examination Deficits
Learners require individualized remediation strategies depending on their learning needs and the domain(s) involved. Strategies that incorporate hands-on, practical, and interactive activities are more effective than reading and shadowing alone [16]. For fundamental knowledge gaps, reading ideally precedes interactive case-based exercises that promote the transfer of knowledge [17].
For each PE skills deficit domain, we provide some learner profile examples and the remediation plans prescribed for the specific deficits we uncovered.
5.1 Motor/Technical Skills Deficit
Case 1
Frank is a third year medical student who saw an older male with atherosclerotic disease who had gnawing back pain. Frank palpated below the umbilicus to a depth of about 1 cm, checking for an enlarged pulsating aorta. Frank did not feel the enlarged pulsating mass that was quite obvious with palpation to the correct depth in the correct location and with the correct technique.
Case 2
Ming was auscultating the lungs of a standardized patient with possible asthma or COPD during a diagnostic skills course. She listened only to the beginning of expiration before moving her stethoscope to another area. After a discussion about the pathophysiology of the diseases, she recognized that it would be difficult to hear end-expiratory wheezes with her technique.
5 Remediation
Step 1: Deficit identification:
Engage in a conversation with the student to ascertain if there are additional deficits involved.
Besides not understanding the physiology of the aorta and where it branches, Frank commented that he did not palpate very deeply for fear of hurting the patient. On further discussion, the fear of causing patient discomfort was a recurrent problem that transcended many examination elements. This interactional deficit highlighted that Frank still needed to acquire the emotional maturity needed to ultimately balance the patient’s comfort with the need for an effective clinical exam.
Ming demonstrated an additional deficit in medical knowledge about what exam characteristics suggest severity of disease, as well as how the character and timing of a wheeze can confer information about the type of obstruction that may be present in the respiratory tract.
Step 2: Real-time remediation:
Demonstrate correct technique and rationale (e.g., physiology or pathophysiology) so students can observe the difference between correct and incorrectly performed techniques, and follow by close observation of student re-performance of the PE elements. Note that if the student requires more in-depth teaching due to a concurrent knowledge deficit or complete lack of knowledge about approaching a patient, these conversations could more appropriately occur away from a patient’s bedside.
Step 3: Planned remediation for motor/technical skills deficit:
Recommend resources to improve the technical skills aspect of the physical exam. Possible resources include:
-
Physical examination textbooks
-
Online videos or real-life/real-time demonstration of correct exam techniques (Bates’ Physical Examination Videos provided as part of the textbook package; UCSD Practical Guide to Clinical Medicine) [20]
-
Course in diagnostic or physical examination skills
We directed both students to books and online resources and suggested studying a certain technique one day followed by deliberate practice of that technique on every patient seen in their clerkship the next day, considering what findings they would expect (even if normal). We encouraged them to choose a new technique once they feel they had perfected the prior set of skills.
Step 4: Remediation for other deficits:
Frank and I returned to the patient to solicit his experience with the “correct” exam that we had conducted. The patient’s reassurance that the exam was more “uncomfortable” than painful and that he understood that we needed to do “whatever was necessary to figure out what was going on,” referring specifically to inflicting pain as part of the exam, reassured the student. Frank also found it advantageous to have the exam performed on him to experience the depth and degree of discomfort.
Ming read more about lung diseases and made extra efforts to practice auscultation on patients with lung diseases. She was also directed to online audio recordings that demonstrated different breath sounds and their diagnoses (recommendation: search on MedEd Portal www.mededportal.org) [21].
Step 5: Reassessment:
This step must involve direct observation of learner’s performance with specific feedback after steps 1–4 above.
-
Formal (standardized patient experience) or informal (at the clinic/bedside) direct observation of learner performance
-
Testing to verify improvement/mastery of skills
Frank was reassessed at the end of his rotation on another patient presenting with back pain.
Ming was reassessed during a clinical performance examination of a patient with shortness of breath.
5.2 Experiential/Medical Knowledge Deficit
We divide this section into experience/knowledge deficits for initial diagnosis and for management of chronic illness.
5.2.1 Initial Diagnosis
Case 3
Paulina recognized that her patient had cellulitis. She even knew that she should consider necrotizing fasciitis in her differential, but did not have the medical knowledge or experience to identify the findings that would help differentiate the two.
Case 4
During an observed history and exam, Carlos determined that his middle aged female patient had some sort of arthritis. He couldn’t recall whether distal interphalangeal (DIP) joint involvement was more common in rheumatoid arthritis or psoriatic arthritis.
Step 1: Deficit identification:
This deficit is usually detected during a patient presentation, with direct inquiry about how the student could differentiate between similar disease processes. It is helpful to go to the bedside and ask for a demonstration of the PE (if not already witnessed) to ensure correct technique and to ascertain if there are additional deficits involved.
Paulina had a basic understanding about soft tissue infections but thought that necrotizing fasciitis was just a very bad cellulitis that needed intravenous medications.
Carlos recalled something about polyarticular, oligoarticular, and monoarticular arthritis and that they affected different joints. He even recalled that PIP vs. DIP involvement was a differentiating characteristic, but could not recall which joints were involved with which disease process between rheumatoid, psoriatic, gout, and osteoarthritis.
Step 2: Real-time remediation:
Discuss using a query format about physiology or pathophysiology and how to differentiate between disease processes.
Paulina and her faculty advisor returned to the patient to discuss exam findings—toxic appearance, satellite lesions, pain out of proportion to exam, rate of spread, etc.—as well as laboratory evaluations that would be most consistent with necrotizing fasciitis.
Carlos demonstrated his PE findings of asymmetric joint swelling with DIP involvement. On closer observation, we were able to discern pitting in the nails and mild scaling of several extensor surfaces.
Step 3: Planned remediation:
-
Reading about similar diseases and examination findings that help discriminate between them
-
Making a chart of similar diseases with expected historical and physical differences (see Chap. 6)
-
Pairing with a clinician who can provide one-on-one guidance: practice creating discriminating questions/exam characteristics that differentiate between similar disease processes
Paulina read about soft tissue infections.
Carlos created a spreadsheet of the different arthritides and how they differ both clinically and historically.
Step 4: Reassessment:
This step must involve direct observation of learner’s performance with specific feedback after steps 1–3 above.
-
Formal (standardized patient experience) or informal (at the clinic/bedside) direct observation of learner performance
-
Testing to verify improvement/mastery of skills
After reading about soft tissue infections, Paulina sought out additional patients and presented her findings to another attending.
Carlos referred to his spreadsheet when evaluating other patients with arthritis complaints.
5.2.2 Management of Chronic Illness
Case 5
During a clinical performance exam, Beth does poorly on a case involving a patient with diabetes who presented for a 6-month follow-up. She does a great job assessing the patient’s history since the last visit in regard to diet and medication and even asks questions about potential consequences of his disease, but she has difficulty focusing the physical exam. She examines the feet for peripheral neuropathy using light touch only and fails to perform a fundoscopic exam, a cardiovascular exam, or check for neuropathy with a microfilament or tuning fork.
Step 1: Self-reflection exercise:
In preparation for a face-to-face meeting, Beth was asked to review her video and complete a self-guided reflection exercise.
Step 2: Deficit identification:
We engaged in a conversation to ascertain if there were additional deficits involved or any other issues that may have prevented her from performing better. Beth stated that she had no idea what, if any, examination was expected from her with this kind of patient. She thought she was being tested on how well she counseled the patient on diet and exercise. During our discussion, Beth demonstrated appropriate knowledge about the expected disease progression and possible consequences of poorly controlled diabetes, including problems involving the ocular, cardiovascular, renal, and neurological systems. The additional deficit elicited in the discussion pertained to knowledge about which neuroanatomical tract is most affected in diabetes and about the use of a microfilament to test for peripheral neuropathy.
Step 3: Real-time remediation:
Review general expectations of chronic care/follow-up/well-person visits—focusing a query-based discussion on rationale and correct technique (e.g., pathophysiologic consequences of progression of disease process or expected “screening exam”).
After our discussion, Beth appropriately demonstrated which head-to-toe exam maneuvers she would have performed if allowed to repeat the case.
Step 4: Planned remediation for awareness deficit:
-
Videos of an encounter/observe a clinician conducting such type of encounter
-
Reference to national standards/guidelines (e.g., Standards of Medical Care in Diabetes-2012 by the American Diabetes Association)
-
Shadowing an expert clinician (must make sure this is someone who can demonstrate the “correct” approach or one agreed upon by a consensus panel)
-
Deliberate practice during clerkships
Step 5: Planned remediation of other deficit:
It was suggested that Beth review the pathophysiology of diabetic neuropathy and the examination maneuvers that elicit findings in each of the spinal tracts.
Step 6: Reassessment:
This step must involve direct observation of learner’s performance with specific feedback after steps 2–5 above.
-
Formal (SP experience) or informal (at the clinic/bedside) direct observation of learner performance
-
Testing to verify improvement/mastery of skills
Beth was required to take a mini-clinical performance exam where a clinical educator observed her and provided feedback.
Step 7: Curricular questions:
A students’ expression of knowledge and skill not only reflects his/her own abilities but is also an expression of the education and training he or she is receiving. If multiple students are noted to have similar deficits of this type, the question arises whether there is a deficiency in the curriculum and whether there needs to be additional education and/or skill building in this arena.
Once a consensus is reached (perhaps by the medical education committee or other assigned committee) about what should constitute a “screening examination” or “well patient visit,” a decision about where to implement this learning needs to be reached, and, ideally, the educators need to be trained to teach consistently with this vision. Should this be part of a Fundamentals course? Should it be a required lecture during a clerkship? Should a patient encounter be required during a primary care clerkship?
5.3 Interactional Deficit
Case 6
Ivan was uncomfortable with having to perform a rectal exam on a male patient to assess for a perirectal abscess. His extremely tenuous and awkward approach was met with so much hesitation and concern from the patient, the patient ultimately requested that a faculty clinician perform the exam instead.
Case 7
During Ken’s clinical performance exam, he acted very distracted and disinterested—repeating questions, looking at his watch, leaning back in his chair with his leg crossed over his knee and his arms crossed. The exam was curt and dissociative. The standardized patient’s response was quite negative and cited feeling uncared for, not listened to, and unimportant. Ken failed the physician interaction component of the exam.
Step 1: Deficit identification:
Discuss with the learner about how the encounter went and how well he/she interacted with patient. It is important to determine whether the learner was aware of what the patient’s reaction to the encounter was. Ascertain whether there are additional deficits. This can be done after the patient encounter or after reviewing a video-recorded encounter. Self-reflection exercises that target communication/interactive type of skills are often useful.
After Ivan’s encounter, when asked about his tenuousness, he reported feeling uncomfortable “probing a man there.” He felt it was disgusting. He also lacked knowledge about the differential diagnosis of perirectal abscess.
Ken was assigned to complete a self-reflection exercise prior to his video review. Upon review, he lacked insight into why he failed—he felt he said all the right things.
Step 2: Real-time remediation:
-
Discussion and acknowledgement of discomfort with exam maneuvers
-
Simulated student experience—student becomes the patient who would have a simulated physical exam while having legs dangle off end of gurney, uncovered while in lithotomy position (though clothed), or awkwardly vs. confidently requesting to perform exam maneuvers for which the patient may feel uncomfortable
-
Simulated feedback—Experience of the remediation itself with negative followed by positive nonverbal communication while providing feedback (body language, distractibility vs. focus, etc.)
It was critical to acknowledge Ivan’s discomfort and distaste for the exam. At the end of our discussion, he recognized the need to differentiate perirectal from perianal abscess because of the differences in work-up and management. Ivan also came to realize that the patient was probably more uncomfortable than he was, and that displaying confidence and normalizing the exam to patients can help alleviate their discomfort.
During the first part of Ken’s video review, the remediator provided feedback on the case while displaying distracted nonverbal behaviors such as repeatedly checking the cell phone and watch, sitting back, crossing arms, and looking away disinterestedly. Then the remediator asked Ken to consider how he felt about the feedback encounter. The remediator then continued the session while leaning forward, focused and engaged in the discussion of the case, followed by discussing how different these experiences could be for the patient and while reviewing portions of the history and exam with special note to his nonverbal communication.
Step 3: Planned remediation:
-
Readings about patient experience. We often add reading on the potential legal ramifications of positive vs. negative patient experiences and bad outcomes [18]
-
Possible counseling about personal aversions to performing exam maneuvers
-
Deliberate practice being empathetic to the patient experience during exam maneuvers assuming that the patient is scared, wary, and in pain with each encounter
-
Shadowing clinical faculty with excellent bedside manner
Both Ivan and Ken were provided some readings and were asked to deliberately practice performing examinations paying attention to patient experience.
Step 4: Reassessment:
This step must involve direct observation of learner’s performance with specific feedback after steps 1–3 above
-
Formal (standardized patient experience) or informal (at the clinic/bedside) direct observation of learner performance
-
Testing to verify improvement/mastery of skills
Ivan was observed performing a pelvic exam on a young woman (another procedure he felt uncomfortable with). Again, the clinician needed to guide him through maneuvers that ensured patient comfort such as properly covering the patient and explaining what he was doing. He continued to feel awkward with subsequent observed examinations, but did eventually perform the appropriate mechanics of the maneuvers.
Ken retook a clinical performance exam and demonstrated some improvement in nonverbal communication skills. However, he needed further coaching in communication skills overall.
5.4 Cognitive/Clinical Reasoning
Case 8
On three different presenting situations on the clinical performance exam, Leon performed the following exam: Swung light back and forth between patient’s eyes, listened to the heart in four places, listened to the lungs in four places, and palpated the abdomen in four places. When asked what the student was looking for during each of these maneuvers, he had no clear idea.
Case 9
A patient presented to the Emergency department with RLQ pain. Her history was concerning for appendicitis. Upon presenting the patient, Martin reported his exam findings that included rebound and guarding of the abdomen and tenderness at McBurney’s point. His plan was to perform a CT scan. He missed considering gynecological causes and did not perform a pelvic exam. The patient had an ectopic pregnancy.
Case 10
On review of a clinical performance exam in a patient with chest pain, Paris recognized that the patient needed a “cardiac” exam. She palpated and auscultated the heart in the appropriate places with the patient upright, at 30°, and lying on his left side with both the bell and the diaphragm. She felt for PMI and heaves in various positions, then she looked for pedal edema. She did not listen to the lungs.
Case 11
Jody recognized that her patient presenting with mechanical falls needed a neurologic exam to determine whether the cause was muscular, sensory, or balance. She discovered that the patient had difficulty with gait and her Romberg test was positive. She tested for strength and sensation and noted rapid alternating hand and finger nose tests were all normal. Lacking an understanding about what the Romberg maneuver tests are for, she did not proceed to test position or vibration sense in order to assess for pathology in the dorsal columns.
Case 12
Xavier was evaluating a young male with syncope. He recognized that he should listen for a cardiac murmur consistent with hypertrophic cardiomyopathy but did not recall the exam maneuvers that would express the murmur so he did as many as he could think of.
Step 1: Deficit identification:
In order to identify deficits in clinical reasoning, one must first ascertain what differential diagnosis forms the basis for a student’s physical exam. This is especially true for chief complaint-based examinations that require more focused maneuvers to rule in and out the various disease processes in the differential. In addition, it is important to determine if the student has developed any kind of systematic approach to the examination, as it will aid in providing remediation strategies. Finally, one must ascertain if there are additional deficits involved.
We found Leon to be disorganized in all aspects of data collection. He suffered from examination anxiety and was attempting to pass via a shotgun approach to collecting as much data as possible to accrue points. He also lacked the ability to limit a differential diagnosis to the most common and most dangerous entities because of his disorganization that proved to transcend testing situations.
Martin felt that he has seen patients with symptoms of appendicitis like this one so many times on his surgery clerkship, that the diagnosis seemed obvious.
We questioned Paris about the incompleteness of her examination. She stated that auscultating the lung was part of the “pulmonary” exam and was therefore not part of a focused exam for cardiac concerns. We diagnosed that she lacked understanding of how a pulmonary examination helps with cardiac diagnoses such as congestive heart failure, and likely had insufficient understanding of cardiac pathophysiology.
Jody performed the neurological maneuvers she learned without having a clear understanding what a positive result represented or what further testing would be required.
Xavier had created a good differential and even performed the cardiac examination with technical skill. His deficit was a lack of understanding of the pathophysiology of hypertrophic cardiomyopathy and a lack of recall about how to elicit the murmur.
Step 2: Real-time remediation:
Faculty demonstration of correct technique and rationale (e.g., physiology or pathophysiology) provides the most useful and immediate feedback. Almost every student who requires remediation can benefit from suggestions about how to improve organization or how to employ strategies to generate memory triggers to help prevent missing historical or examination data that would help hone the differential. Over the years, we have included in almost every remediation session a brief discussion about how to utilize the review of systems to ensure that no important historical data is missed. This exercise can be done as part of a systematic approach to a “relevant and focused” head-to-toe exam.
An example script: “My clinical examination begins with an assessment of the eyes of every patient. It establishes rapport and gives relevant information—for patients with abdominal pain, I look for icterus and conjunctiva pallor, for diabetic patients, I perform a funduscopic exam, and for rheumatological complaints I look for evidence of uveitis. While I begin the exam with the same body part systematically, I consider the differential in the findings for which I am searching.”
Step 3: Planned remediation:
-
Creating a “scut sheet” exercise (Fig. 5.2) that helps organize historical and exam data, in addition to lab data and patient to-do lists
-
Constructing an individual or group exercise to go through appropriate differential diagnoses for chief complaints given different demographics, followed by an exercise in creating lists of discriminating questions and focused exam maneuvers to differentiate between similar disease processes
-
Referring to books or videos that demonstrate system-based or chief complaint-based physical examinations (e.g., hypothesis-driven physical examination) [15]
-
Referring to online or computer-based software (several commercial offerings available) that provide exercises in systematic approaches to doing PE, for example, asking “what exam would I do to support/refute items in a given differential?”
-
Offering a course in diagnostic or physical examination skills that provides practice in creating appropriate differential diagnoses with case exercises
-
Practicing a systematic approach to both history and PE
-
Shadowing exemplary clinical faculty
-
Practicing an organized review of systems approach (for example, head-to-toe) to gather relevant data and prevent premature closure
All of the above was recommended to Leon. He was required to take the skills course and online practice prior to re-testing for the clinical performance exam. He was also given a referral to a specialist to discuss his testing anxieties.
We pushed Martin to consider all dangerous entities when generating differential diagnoses. We asked him to purposefully broaden his differential if he noted that a diagnostic conclusion came to him quickly during patient encounters, and recommended that he deliberately practice using the review of systems and “head-to-toe” exam to ensure that he didn’t miss any important organ systems.
We recommended that Paris and Jody review the anatomy, physiology, and pathophysiology of the cardiovascular and neurologic examination, respectively. We offered them a preceptor shadowing experience. We also enrolled them in our diagnostic skills course and asked them to deliberately practice what they learned during their subsequent clerkships.
Xavier took an online cardiac course created for students and residents to learn with visual and auditory cues about physiology and pathophysiology of the cardiac exam [22]. He was also asked to deliberately practice such an exam.
Step 4: Reassessment:
Must involve direct observation of student’s performance with deliberate feedback after steps 1–3 above.
-
Formal (standardized patient experience) or informal (at the clinic/bedside) direct observation of student performance
-
Testing to verify improvement/mastery of skills. (See Chap. 6 for additional information on Clinical Reasoning deficits.)
Step 5: Curricular questions:
As previously mentioned, a students’ expression of knowledge and skill reflects the education and training they receive. If multiple students are noted to have similar deficits, this may indicate a systematic deficiency in the curriculum and whether students need additional education and/or skill building in this arena. For example, several students independently claimed that their teaching of the cardiovascular exam omitted the pulmonary component. Perhaps confusion arises when these examinations are taught in separate contexts. Should this be further and more explicitly or even repeatedly taught? Should there be some methodological change in an area of the curriculum that focuses on system or chief complaint-driven examinations?
6 Conclusion
Remediation of PE skills is a complex enterprise. We have discussed four deficit domains, but most learners requiring remediation will demonstrate a combination of deficits, suggesting that remediation strategies must be individualized for best results. Though remediation can occur simply at the bedside using role modeling and impelling students toward deliberate practice, strategies increasingly include technological aids, for example, using simulation, multi-headed teaching or digitally enhanced stethoscopes, simultaneous cardiac echo, online games that reward accuracy, among others. Even You-Tube videos of examination skills can be useful teaching aids, though, ideally, there would be a catalog of “approved” ones that are most accurate and effective. Early identification, use of diverse remediation strategies targeted to learner needs, and confirmation of improving skill represent the core three steps to maximize learner proficiency in the physical examination.
Yet, significant logistical constraints in the remediation process remain to be addressed. Accumulating common themes of student PE errors can indicate a need to reassess or alter medical school curricula to ensure effective teaching of PE skills. Faculty clinicians with exemplary PE skills must have time and resources available in order to perform assessments, remediate, and then reassess learners. Ultimately, with these approaches and close coaching, we believe that learners will attain the skills to be both excellent clinicians and capable teachers for future generations.
References
Life in the fastlane [Internet]. Australia: Frontier Group and GMEP; 2013. Sir William Osler memorable quotes [cited 5 July 2013] [about p. 8]. Available from http://lifeinthefastlane.com/resources/oslerisms/
Wilkerson L, Lee M. Assessing physical examination skills of senior medical students: knowing how versus knowing when. Acad Med. 2003;78(10 Suppl):S30–2. PubMed PMID: 14557088.
Herbers Jr JE, Noel GL, Cooper GS, Harvey J, Pangaro LN, Weaver MJ. How accurate are faculty evaluations of clinical competence? J Gen Intern Med. 1989;4(3):202–8. PubMed PMID: 2723833.
Kassebaum DG, Eaglen RH. Shortcomings in the evaluation of students’ clinical skills and behaviors in medical school. Acad Med. 1999;74(7):842–9. PubMed PMID: 10429595.
Norcini JJ, Blank LL, Duffy FD, Fortna GS. The mini-CEX: a method for assessing clinical skills. Ann Intern Med. 2003;138(6):476–81. PubMed PMID: 12639081.
Harden RM. What is an OSCE? Med Teach. 1988;10(1):19–22. PubMed PMID: 3221760.
Barman A. Critiques on the Objective Structured Clinical Examination. Ann Acad Med Singapore. 2005;34(8):478–82. PubMed PMID: 16205824.
Frye AW, Richards BF, Philp EB, Philp JR. Is it worth it? A look at the costs and benefits of an OSCE for second-year medical students. Med Teach. 1989;11(3–4):291–3. PubMed PMID: 2518040.
Chang A, Chou CL, Teherani A, Hauer KE. Clinical skills-related learning goals of senior medical students after performance feedback. Med Educ. 2011;45(9):878–85. doi:10.1111/j.1365-2923.2011.04015.x.
Dornan T, Scherpbier A, Boshuizen H. Towards valid measures of self-directed clinical learning. Med Educ. 2003;37(11):983–91. PubMed PMID: 14629411.
Sargeant J, Eva KW, Armson H, Chesluk B, Dornan T, Holmboe E, Lockyer JM, Loney E, Mann KV, van der Vleuten CP. Features of assessment learners use to make informed self-assessments of clinical performance. Med Educ. 2011;45(6):636–47. doi:10.1111/j.1365-2923.2010.03888.x.
Saxena V, O’Sullivan PS, Teherani A, Irby DM, Hauer KE. Remediation techniques for student performance problems after a comprehensive clinical skills assessment. Acad Med. 2009;84(5):669–76. doi:10.1097/ACM.0b013e31819fa832.
Yudkowsky R, Otaki J, Bordage G, Lowenstein T, Riddle J, Nishigori H. Hypothesis-driven physical exam student handbook. Chicago, IL: Board of Trustees of the University of Illinois; 2008.
Nishigori H, Masuda K, Kikukawa M, Kawashima A, Yudkowsky R, Bordage G, Otaki J. A model teaching session for the hypothesis-driven physical examination. Med Teach. 2011;33(5):410–7. doi:10.3109/0142159X.2010.540269.
Yudkowsky R, Otaki J, Lowenstein T, Riddle J, Nishigori H, Bordage G. A hypothesis-driven physical examination learning and assessment procedure for medical students: initial validity evidence. Med Educ. 2009;43(8):729–40. doi:10.1111/j.1365-2923.2009.03379.x.
Clark RE, Vogel A. Transfer of training principles for instructional design. Educ Technol Res Dev. 1985;33(2):113–23. doi:10.1007/BF02769112.
Perkins DS, Salomon G. Transfer of learning. In: Husen T, Postlewaithe TN, editors. International Encyclopedia of Education. 2nd ed. Oxford, England: Pergamon Press; 1992 [cited 5 July 2013]. Available from http://learnweb.harvard.edu/alps/thinking/docs/traencyn.htm
Bickley LS, Szilagyi PG. Bates’ guide to physical examination and history taking. 11th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013. p. 994.
DeGowin RL, Brown DD, LeBlond RF. DeGowin’s diagnostic examination. 9th ed. New York: McGraw-Hill; 2009. p. 914.
Goldberg C. A practical guide to clinical medicine [Internet]. San Diego, CA: The Regents of the University of California. 1997–2009 [updated 16 Aug 2008; cited 5 July 2013]. Available from http://meded.ucsd.edu/clinicalmed/
Association of American Medical Colleges (AAMC). MedEdPORTAL [Internet]. Washington, DC: Association of American Medical Colleges; 1995–2013 [cited 5 July 2013]. Available from https://www.mededportal.org/
Criley JM, Keiner J, Boker JR, Criley SR, Warde CM. Innovative web-based multimedia curriculum improves cardiac examination competency of residents. J Hosp Med. 2008;3(2):124–33. doi:10.1002/jhm.287.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Spector, T., Fung, CC. (2014). Remediation of Physical Exam Skills. In: Kalet, A., Chou, C. (eds) Remediation in Medical Education. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9025-8_5
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9025-8_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9024-1
Online ISBN: 978-1-4614-9025-8
eBook Packages: MedicineMedicine (R0)