Abstract
Hospitalization of end-stage renal disease (ESRD) is a major morbidity to the patient and cost to the payer. Forty-eight percent decline has been noted in admissions related to vascular access in 2009 compared to 1994, and the number one reason for hospitalization in ESRD patients now is infection-related admissions. Interventionists are routinely performing these procedures at outpatient vascular access centers providing limiting disruptions in dialysis care. Invasive procedures have associated complications and require that the operator has in-depth knowledge of rescue when required and use inpatient admission if indicated. Procedure sedation analgesia (PSA) plays an integral role in managing invasive procedures and has risks that should be weighed prior to each encounter. Comprehensive intraoperative care and on occasion’s inpatient observation is warranted after a complication is witnessed. This chapter reviews the conditions that warrant the patient to be operated inpatient or placed in observation after the procedure.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Access Center
- Metastatic Infection
- Phlegmasia Cerulea Dolens
- Native Kidney Biopsy
- Tunnel Dialysis Catheter
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Dialysis access care is integral to wholesome management of an ESRD patient. Access care contributes to major mortality and morbidity in ESRD and is also associated with tremendous cost to the system [1]. Over the last 15 years, there has been approximately 50 % drop in the rate of hospitalizations for access-related complications in ESRD [1]. Untimely, improper and low priority care of access resulted in nephrologists stepping up to take care of problems affecting their patients. Nephrologists traditionally had performed kidney biopsies and inserted temporary dialysis catheters. Interventional nephrologists have shown excellent outcomes when performing endovascular procedures with minimal complications [2, 3]. Over the years, growth in interventional nephrology (IN) has occurred primarily as freestanding access centers bringing financial value to the practice. Timely care, convenience, comfort, and improved outcomes are all benefits delivered to patients by IN, but safety during the intervention should remain the prime goal and responsibility of the operator. Decision of admission to hospital is taken after careful assessment of risk to a patient before, during, and after a procedure.
3.1 Are There Patients That Will Require Hospitalization Prior to a Procedure?
The ability to deliver safe and effective moderate sedation is crucial to the ability to perform invasive procedures [4]. Intraoperative procedure experience should be as smooth for the patient as can be and should start with preemptive assessment of patient’s comorbid conditions, physical examination, history of allergies, or prior experiences with medications used in procedure sedation analgesia (PSA). Sedative drugs used for PSA should have a quick onset of action, maintain moderate sedation during surgical treatment, provide rapid and clear-headed recovery, and be easy to administer and monitor. Sedation and analgesia comprise a continuum of states ranging from minimal sedation (anxiolysis) through general anesthesia. Decision to apply level of sedation/analgesia has to be individualized to a given patient taking into account factors including but not limited to nature of the procedure, comorbid medical conditions, patient’s level of anxiety, history of complications in prior procedures with use of anesthetic drugs, and operator experience with sedating procedure.
Preoperative work-up should incorporate a focused physical examination, including vital signs, auscultation of the heart and lungs, and evaluation of the airway. Laboratory testing should be guided by the patient’s underlying medical condition and the likelihood that the results will affect the management of sedation/analgesia. Most commonly used agents for PSA include a combination of benzodiazepines, opioids providing amnesia, and analgesia, respectively.
Ability to maintain airway and ventilation is directly affected by sedation/analgesia. The effect of sedative medications on patient’s ability to maintain and protect airway is exacerbated in CKD patients, and PSA may be relatively contraindicated in patients who may have a difficult airway. Key to minimizing risk is to identify and monitor patients at higher risk. Uncooperative patients, morbid obesity, potentially difficult airway, and sleep apnea are all associated with an increased risk of ventilation/oxygenation complication and may benefit from preprocedure consultation to anesthesia. There is no specific age above which PSA may not be performed, though the risk is higher for elderly patients [5, 6]. Comorbid conditions including heart failure, dehydration, chronic obstructive pulmonary disease (COPD), and neuromuscular disease should be assessed prior to the procedure and corrective measures be taken to optimize hemodynamics [7]. Several recent studies have supported the use of PSA across a broad patient population with careful clinical supervision. When careful attention is paid to examine subject and modus operandi individualized, most procedures can be completed with minimal complications and no hospitalization [8–10].
The risk to patient for complications may persist after their procedure is completed. Decreased procedural stimulation and slow drug elimination in chronic kidney disease (CKD) patients may contribute to residual sedation and cardiorespiratory depression during the recovery period.
Continued monitoring will be required if patient is not fully alert and oriented; infants and patients whose mental status was initially abnormal should have returned to their baseline status [5, 7]. Abnormal vital signs should be watched till they return to acceptable limits. If the patient required a reversal agent during the procedure, practicing physician needs to be aware of the short half-life of these agents (naloxone, flumazenil) and up to 2 h should have elapsed after the last administration of reversal agent [7]. This would ensure that patients do not become resedated after reversal effects have worn off.
In summary, comprehensive assessment prior to a procedure will identify patients at high risk for complication. PSA can be safely administered in all patients with adequate planning and preparation [7].
3.2 Does the Nature of Procedure Require Inpatient Care?
The last decade has seen tremendous growth in vascular access centers and the role of nephrologists has been redefined, from being passive facilitator of patient care to an interventionist rendering solutions to complex dialysis access demands. List of procedures performed by nephrologists continues to grow, with more complex procedure being added to the roll [2, 11–14]. So as more complex cases are performed at freestanding access centers without any backup, are there any interventions that will warrant inpatient care? Reviewed below are common procedures and recommendations for the place of service.
3.2.1 Percutaneous Needle Biopsy of Kidney
Native kidney biopsy is frequently performed for diagnostic purposes. Minor complications are defined as gross hematuria and perinephric hematoma that resolve without the need for transfusion or intervention. Major complications are defined as those requiring a blood transfusion, invasive radiological procedure (angiogram/coil), nephrectomy, and bowel perforation [15–17]. Automated spring-loaded biopsy gun is widely accepted to be standard approach and biopsies are done under real-time ultrasonography [18]. The standard of care has been to observe patient post-biopsy for 24 h as suggested by most studies [15–17]. There was correlation with the 6-h post-hematocrit drop with rate of complication in one study [15], yet another study suggested that >20 % of complications may be missed if patient is discharged within 8-h post-renal biopsy [17]. The only randomized control study comparing manual to automated kidney biopsy noted 11 % incidence of perirenal hematoma post-kidney biopsy. All patients were required to have 12 h of strict bed rest after the biopsy [18]. Based on above data it is safe practice that patient be observed for 24-h post-biopsy.
3.2.2 Interventions Directed at Vascular Access
Wide spectrum of services are now offered at access centers with an objective to create, maintain, and salvage hemodialysis access. Data over the last decade, from several operators, supports safe application of these techniques in freestanding access centers with minimal complications [2, 19–21]. Ability of nephrologist to provide wholesome care has helped improve overall access health [1], and we strive to attain goals set by CMS and fistula first for hemodialysis patients [22].
3.2.2.1 Angiogram, Angioplasty, and Stent Placements
Success of angiography/angioplasty procedures has been upwards of 98 % [21] and the complications associated with the procedures are low [21]. Complications graded as high-grade complications are noted to be less than 0.05 % [2], and though the data is not available as to what percentage of these may require admission for management of the complication, the overall numbers may be lower than 1 out of 2,000 patients at risk [2]. 99.9 % of procedures performed in access center have no complication (>98 %) or minor complications noted during the procedure managed with nominal interventions [2].
3.2.2.2 Central Vein Catheter Placement/Tunneled/Port
About a quarter of all dialysis patients require a central venous catheter for long-term dialysis causing considerable morbidity and mortality. Infections continue to be a major cause of admissions into hospitals and contribute to a high mortality [1]. Since 1993 infection-related hospitalizations have increased a whopping 43 % [1], and a majority of these are associated with tunneled dialysis catheter (TDC).
TDC patients on hemodialysis have 0.9–2.0 episodes of bacteremia per year of catheter use. If we account for the total dialysis population inUSA, this would account for 100,000 incidents of bacteremia and with roughly 10 % of these developing infection-related complications, over 10,000 admissions for catheter infection [23–25]. Complications from catheter infection include sepsis, metastatic infection to the cardiac valves or the spine most commonly, septic arthritis, skin abscess, and thrombosis of the insertion vein.
Port-a-catheters are similar to TDC with subcutaneous port reservoir and are primarily used for central vein access for chemotherapy. Successful placement and management of port-a-catheters will involve the nephrologists to be aware of indications for catheter removal and management of infections at times requiring hospitalization and intravenous antibiotics [13].
Indications for hospitalization and management of infection from a TDC or a port-a-catheter will be severe sepsis with hemodynamic instability, diagnosis and management of a suspected metastatic infection after bacteremia, treatment of deep vein thrombosis associated with catheter insertion/infection, amongst other clinical indications.
If catheter-related bacteremia is suspected clinically, empiric antibiotic therapy should be started quickly, without waiting for the culture report. Bacteriological data from several studies show a mixture of gram-negative/gram-positive rods, thus mandating broad-spectrum antibiotic coverage for both gram-positive and gram-negative organisms pending culture results. Many staphylococcal infections in hemodialysis patients are caused by methicillin-resistant species, requiring empiric therapy with vancomycin pending sensitivity reports.
Treatment of catheter-related bacteremia with systemic antibiotics without catheter removal has a high failure rate. Hospitalized patients should get a catheter-free period with a temporary dialysis catheter used in the interval for dialysis. TDC can be replaced on clinical improvement [23].
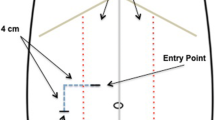
3.2.2.3 Peritoneal Dialysis [PD] Catheter Placement Using Fluoroscopy/Peritoneoscopy
Growing interest amongst nephrologists and dialysis chains for peritoneal dialysis has sparked tremendous interest for placement and management of PD catheters by nephrologists themselves. Several studies have shown risk of complication to be very low when catheters are placed under PSA using either fluoroscopy [26, 27] or peritoneoscopy [28]. Complications associated with PD catheter placement can be classified into intraoperative and postoperative. Intraoperative complication that may require hospital admission will include bowel perforation, bladder perforation, intraperitoneal bleeding, and laceration of the inferior epigastric artery [14, 26]. The risk of above complications is extremely low, and most patients can be safely discharged after the PD catheter placement within the same day [26].
PD catheter infections are associated with major morbidity and require dedicated personnel geared towards rapid identification/classification of infection. As more interventionists are performing PD catheter placement procedures, it is required a wholesome care approach be used when a catheter does get infected. Exit site infections are treated with oral/topical antibiotics alone, but a tunnel infection or peritonitis may require PD catheter removal/replacement [29].
Removal of PD catheter poses challenge to continue renal replacement therapy (RRT), occasionally requiring admission for acute hemodialysis.
3.2.2.4 Peripheral Arterial Interventions
Arterial stenosis accounts for significant number of immature fistulae and plays a major role in late access complications including distal ischemia hypoperfusion syndrome [DHIS], commonly identified as “steal” [30]. Arterial interventions involve at times arterial approach where femoral or radial artery puncture is used to place a sheath for access. Removal of sheath may be done once the anticoagulation given during the course of the procedure has dissipated. Observation will be required until homeostasis can be secured using a closure device for femoral access or band for radial access [31].
Rare and mostly unforeseen, significant complications will require admission and inpatient care of the asymptomatic patient prior to the intervention. An arterial embolus to the brain with ischemic cerebral vascular accident (CVA) after percutaneous fistula thrombectomy [32], suppurative thrombophlebitis (Lemierre’s syndrome) of the internal jugular vein after a central venous catheter placement [33], phlegmasia cerulea dolens (PCD) characterized by massive venous thrombosis leading to arterial compromise and tissue ischemia [34], severe acute pancreatitis after percutaneous mechanical thrombectomy of arterial thrombus occlusion [35], rapidly progressing superior vena cava syndrome with a thrombus around a central venous catheter in superior vena cava [36, 37], breakage and migration of hemodialysis catheter on removal [38], and catheter tip embedded into the wall of the superior vena cava on attempted removal of catheter [38] are all examples of what makes interventional field unpredictable. These and other unpredicted complications underline importance of being ready for every case and to take into account that even a trivial case of TDC removal can turn into a major cardiac bypass surgical event for a patient [38].
3.3 Recording Procedure-Related Complications [PRC]
A procedural-related complication is defined as an unanticipated adverse event that requires therapy. In general, unanticipated events that do not require therapy are not considered procedure complications [19, 39, 40]. Complications which occur during or immediate postoperative period should, in most instances, be attributed to the procedure. Uniform classification and reporting of these events has been supported by all interventional societies including Society of Interventional Radiology (SIR) [40], Society of Vascular Surgery (SVS) [39], and American Society of Diagnostic and Interventional Nephrology [19]. Hospitalization of a patient for a procedure-related event should be noted as a major complication and is graded as a grade 3 or grade 4 complication based on the severity and number of days spent in the hospital.
Patients may experience an adverse reaction to intravascular radiographic contrast media or medications administered for PSA. Adverse reactions to medications typically occur soon after administration of the drug, although significant reactions may occur several hours after completion of the procedure [5]. Hospital admission may be required and major complication will be recorded when prolonged (>30 s) decrease in O2 saturation (<90 %) is recognized and it fails to improve with minor therapy [19, 39, 40]. Hemodynamic instability with profound and persistent hypotension, cardiac arrhythmias refractory to reversal of sedation and requiring antiarrhythmic medications, or a persistent mental status change that fails to return to baseline during recovery ought to be charted as major complication and infrequently may require hospitalization [5, 19, 39, 40].
3.4 Conclusion
There is no absolute indication for admission to hospital for a given procedure. All procedures can be done safely as outpatient visits, saving disruptions in patient’s schedule and providing batter value to the insurers. Decision of admission to hospital should be taken after careful assessment of risk associated with procedure itself and the PSA.
References
USRDS: U S Renal Data System, USRDS 2011 Annual Data Report: atlas of chronic kidney disease and end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda; 2011.
Beathard GA, Litchfield T, Physician Operators Forum of RMS Lifeline, Inc. Effectiveness and safety of dialysis vascular access procedures performed by interventional nephrologists. Kidney Int. 2004;66(4):1622–32.
Vachharajani TJ, Moossavi S, Salman L, et al. Dialysis vascular access management by Interventional Nephrology Programs at University Medical Centers in the United States. Semin Dial. 2011;24(5):564–9.
Gan TJ. Pharmacokinetic and pharmacodynamic characteristics of medications used for moderate sedation. Clin Pharmacokinet. 2006;45(9):855–69.
Beathard GA, Urbanes A, Litchfield T, Weinstein A. The risk of sedation/analgesia in hemodialysis patients undergoing interventional procedures. Semin Dial. 2011;24(1):97–103.
Mace SE. 190: Adverse events of emergency department procedural sedation. Ann Emerg Med. 2006;48(4):59.
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96(4):1004–17.
Holdgate A, Taylor DM, Bell A, et al. Factors associated with failure to successfully complete a procedure during emergency department sedation. Emerg Med Australas. 2011;23(4):474–8.
Sacchetti A, Senula G, Strickland J, Dubin R. Procedural sedation in the community emergency department: initial results of the ProSCED registry. Acad Emerg Med. 2007;14(1):41–6.
Weaver CS, Terrell KM, Bassett R, et al. ED procedural sedation of elderly patients: is it safe? Am J Emerg Med. 2011;29(5):541–4.
Asif A, Yevzlin AS. Arterial stent placement in arteriovenous dialysis access by interventional nephrologists. Semin Dial. 2009;22(5):557–60.
Carrillo RG, Garisto JD, Salman L, Merrill D, Asif A. A novel technique for tethered dialysis catheter removal using the laser sheath. Semin Dial. 2009;22(6):688–91.
Pervez A, Zaman F, Aslam A, et al. Port catheter placement by nephrologists in an interventional nephrology training program. Semin Dial. 2004;17(1):61–4.
Zaman F, Pervez A, Atray NK, Murphy S, Work J, Abreo KD. Fluoroscopy-assisted placement of peritoneal dialysis catheters by nephrologists. Semin Dial. 2005;18(3):247–51.
Khajehdehi P, Junaid SMA, Salinas-Madrigal L, Schmitz PG, Bastani B. Percutaneous renal biopsy in the 1990s: safety, value, and implications for early hospital discharge. Am J Kidney Dis. 1999;34(1):92–7.
Manno C, Strippoli GF, Arnesano L, et al. Predictors of bleeding complications in percutaneous ultrasound-guided renal biopsy. Kidney Int. 2004;66(4):1570–7.
Marwah DS, Korbet SM. Timing of complications in percutaneous renal biopsy: what is the optimal period of observation? Am J Kidney Dis. 1996;28(1):47–52.
Kim D, Kim H, Shin G, et al. A randomized, prospective, comparative study of manual and automated renal biopsies. Am J Kidney Dis. 1998;32(3):426–31.
Vesely TM, Beathard G, Ash S, Hoggard J, Schon D, ACPC: Classification of complications associated with hemodialysis vascular access procedures. A position statement from the American Society of Diagnostic and Interventional Nephrology. Semin Dial. 2007;20(4):359–64.
Asif A, Salman L, Carrillo RG, et al. Patency rates for angioplasty in the treatment of pacemaker-induced central venous stenosis in hemodialysis patients: results of a multi-center study. Semin Dial. 2009;22(6):671–6.
Lifeline Access 2011 Outcomes Report, LifelineAcess.com, Three Hawthorn Parkway, Suite 410; Vernon Hills 60061.
Schinstock CA, Albright RC, Williams AW, et al. Outcomes of arteriovenous fistula creation after the fistula first initiative. Clin J Am Soc Nephrol. 2011;6(8):1996–2002.
Allon M. Dialysis catheter-related bacteremia: treatment and prophylaxis. Am J Kidney Dis. 2004;44(5):779–91.
Lee T, Barker J, Allon M. Tunneled catheters in hemodialysis patients: reasons and subsequent outcomes. Am J Kidney Dis. 2005;46(3):501–8.
Beathard GA, Urbanes A. Infection associated with tunneled hemodialysis catheters. Semin Dial. 2008;21(6):528–38.
Sharma M, Sachdeva B. Percutaneous peritoneal dialysis catheter insertion: making a case for an outpatient procedure. J Invest Med. 2012;60(1):1.
Maya ID. Ambulatory setting for peritoneal dialysis catheter placement. Semin Dial. 2008;21(5):457–8.
Alvarez AC, Salman L. Peritoneal dialysis catheter insertion by interventional nephrologists. Adv Chronic Kidney Dis. 2009;16(5):378–85.
Li PK, Szeto CC, Piraino B, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int. 2010;30(4):393–423.
Leon C, Asif A. Arteriovenous access and hand pain: the distal hypoperfusion ischemic syndrome. Clin J Am Soc Nephrol. 2007;2(1):175–83.
Yevzlin AS, Schoenkerman AB, Gimelli G, Asif A. Arterial interventions in arteriovenous access and chronic kidney disease: a role for interventional nephrologists. Semin Dial. 2009;22(5):545–56.
Pinard EA, Fazal S, Schussler JM. Catastrophic paradoxical embolus after hemodialysis access thrombectomy in a patient with a patent foramen ovale. Int Urol Nephrol. 2012;45(4):1215–7.
Kar S, Webel R. Septic thrombophlebitis: percutaneous mechanical thrombectomy and thrombolytic therapies. Am J Ther. 2011.
Mufarrij AJ, Hitti E. A case of phlegmesia cerulea dolens after dialysis catheter insertion. Emerg Med Australas. 2011;23(5):644–6.
Hershberger R, Bornak A, Aulivola B, Mannava K. Acute pancreatitis after percutaneous mechanical thrombectomy: case report and review of the literature. Cardiovasc Intervent Radiol. 2011;34 Suppl 2:S25–30.
Rabinstein A, Wijdicks E. Fatal brain swelling due to superior vena cava syndrome. Neurocrit Care. 2009;10(1):91–2.
Küçükarslan N, Yilmaz M, Us M, Arslan Y, Güler A, Yilmaz A. Superior vena cava syndrome caused by dialysis catheter. Ulus Travma Acil Cerrahi Derg. 2007;13(1):63–6.
Sequeira A, Sachdeva B, Abreo K. Uncommon complications of long-term hemodialysis catheters: adhesion, migration, and perforation by the catheter tip. Semin Dial. 2010;23(1):100–4.
Sidawy AN, Gray R, Besarab A, et al. Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg. 2002;35(3):603–10.
Sacks D, McClenny T, Cardella J, Lewis C. Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14(9 Pt 2):S199–202.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Sachdeva, B. (2014). Admission After Intervention: When and Why. In: Yevzlin, A., Asif, A., Salman, L. (eds) Interventional Nephrology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8803-3_3
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8803-3_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8802-6
Online ISBN: 978-1-4614-8803-3
eBook Packages: MedicineMedicine (R0)