Abstract
The field of drug delivery technology research has continued to grow in recent decades, expanding from technologies traditionally focused on controlled release to now include nanotechnologies and functionalized molecular architectures for target-specific delivery. While these emerging novel technologies are beginning to mature, many of the clinical applications of controlled-release drug delivery technologies continue to focus on well-characterized biodegradable polymer particles, in situ forming gel depots, and lipid-based particulate formulations. This review principally focuses on the physicochemical and functional characteristics of in situ forming semisolid depot formulations and lipid-based drug delivery technologies and also discusses the broader considerations in bringing drug delivery-enabled products to market.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Advances in molecular biology and genomics have revolutionized the treatment of human diseases, with an increasingly diverse array of molecular modalities appearing in the clinic to treat conditions that were once considered unmanageable. As the number of new molecular entities continues to increase, however, success in the clinic can often be limited by suboptimal stability, solubility, or pharmacokinetics, among other factors. Furthermore, as the biopharmaceutical market becomes increasingly competitive (Aggarwal 2011), pharmaceutical manufacturers are paying increasingly close attention on enabling strategies for product differentiation and life cycle management to maximize commercial value. Taken together, these challenges pose unique opportunities for novel drug delivery technologies to help bring new drug products to market.
Polymer- and lipid-based controlled-release drug delivery systems have long been considered as part of strategies to enable clinical and commercial success of a drug product. From a clinical perspective, these technologies are used to achieve constant plasma concentration levels of drug within the desired therapeutic window over an extended period of time, thereby reducing the possibility of side effects and reducing the frequency of administration. Increasingly, these technologies are considered in the early stages of clinical development to modulate the pharmacokinetic profile of a molecular candidate whose viability might otherwise be limited by short intrinsic half-life.
Drug delivery technology research has evolved over the years to encompass not only the well-known polylactide-co-glycolide (PLGA) family of polymers but also emerging novel functional biomaterials and an ever-dizzying repertoire of colloidal nanoscale systems for targeted drug delivery. Most current clinical applications of controlled-release drug delivery technologies focus on biodegradable polymer particles, in situ forming gel depots, and lipid-based particulate formulations. The encapsulation of biotherapeutic agents in PLGA-based materials has a storied history (Okada and Toguchi 1995) and will not be covered here. This review of the literature broadly discusses the functional characteristics of in situ forming semisolid depot formulations and lipid-based drug delivery technologies and also discusses the broader considerations to be taken into account in bringing such products to market.
2 Polymer-Based In Situ Forming Semisolid (Gel) Depots
In situ forming semisolid depots are injected as liquids and then undergo a phase transition to a semisolid gel at the site of injection to form the drug-releasing depot (He et al. 2008; Packhaeuser et al. 2004; Van Tomme et al. 2008). These in situ forming systems may offer advantages over microencapsulation by way of their relatively less complex manufacturing and more mild processing conditions. On the other hand, however, several of these systems tend to rely on precipitation from organic solvents, which may present challenges in maintaining the stability of the active ingredient, particularly macromolecules. Given that these systems are complex mixtures that must undergo phase transitions from liquid to semisolid or solid states, the phase behaviors of these systems are nonlinear and not fully understood thermodynamically; therefore, the formulation parameters that determine the release profile are highly empirical, making it critical to determine the appropriate fit between technology and the nature of the active molecule.
As the name implies, the hallmark of these formulations is the ability to be injected as a liquid and then undergo a phase transition at the site of injection. The phase transition most occurs as a result upon solvent precipitation or in response to an environmental stimulus, usually temperature, pH, or solubility. Biomaterials exhibiting these behaviors are most frequently biodegradable or biocompatible copolymers, but in addition there is growing interest in amphiphilic lipids whose phase behavior may also lend themselves to depot formation with hydrophilic or hydrophobic molecules. The appeal of polymer systems is that the chemical space is sufficiently large, and the synthesis techniques are sufficiently advanced to allow precise control of molecular weight, polydispersity, and molar ratios such that specific polymers can be optimized to fit the desired release characteristics of a particular drug.
2.1 Solvent-Precipitating Depot Formulations
2.1.1 Atrigel Drug Delivery Technology
Initial reports of in situ forming gel depots as a result of solvent precipitation date back to the work of Dunn (1990). A nonaqueous-soluble polymer is dissolved in a biocompatible organic, but miscible, solvent and added to a drug to form a solution or suspension. The formulation is injected into the subcutaneous space and precipitates in situ as the organic solvent dissipates from the site of injection. Perhaps the most prominent example of an in situ precipitating gel depot is Eligard® (Sanofi-Aventis), a sustained-release leuprolide formulation based on the Atrigel delivery technology platform. The development history of this technology platform has been previously described and will not be repeated here (Sartor 2003; Dunn 2002). The Eligard® formulation is principally comprised of a PLGA copolymer dissolved in N-methyl-2-pyrrolidone (NMP) in a fixed ratio. By varying the PLGA copolymer molar ratios, the NMP to PLGA to drug ratio, several dosage strengths, each corresponding to a different dosing interval, are available. The various dosage strengths range from 7.5 to 45 mg, with recommended dosing from once monthly to once every 6 months, respectively.
As previously described, the thermodynamic phase behavior of PLGA solutions can be complex; as such, the formulation parameter space for these precipitating gels is highly nonlinear and therefore very sensitive to the formulation components, including polymer (lactide to glycolide ratio and molecular weight), choice of organic solvent, the solvent to polymer ratio, and drug load. A number of fundamental studies exploring the solution thermodynamics of PLGA-solvent mixtures have demonstrated that the release kinetics from these systems is significantly driven by solvent strength and water miscibility (Brodbeck et al. 1999; Graham et al. 1999).
The conspicuous drawbacks of these precipitating gel formulations is the rather cumbersome formulation preparation and mixing steps that require these injections to be administered in an outpatient or inpatient setting. Eligard® is presented in a single-use kit comprising two prefilled, interconnecting syringes: one containing the Atrigel delivery system and the other containing the leuprolide powder. The contents of the two syringes are thoroughly mixed by pushing the mixture between the two syringes. Presumably due to viscosity, the formulation is injected using 18- or 20-gauge needle. The use of organic solvents in these formulations often leads to significant discomfort upon injection and local site reactions. For the prostate cancer patient population and the time interval between injections, these discomforts of administration are ostensibly acceptable; in looking at expanding the use of these systems to patients with chronic conditions, however, the viability of the dosage preparation and administration procedure may be limited.
2.1.2 Sucrose Acetate Isobutyrate-Based Formulations
Similar in principle to the Atrigel system, sucrose acetate isobutyrate (SABER, Durect Corp.) is a material that forms a semisolid depot as solvent diffuses from the site of injection (Reynolds 1998; Reynolds and Chappel 1998). With SABER being a non-polymeric material, however, there is less flexibility in tuning the specific molecular properties of the material itself; rather the drug release kinetics are driven primarily by the choice of solvent system and other added components of the general formulation. The formulation development of a SABER human growth hormone (hGH) depot highlights the interdependency between the protein formulation and drug delivery matrix formulation in achieving the desired release profile (Okumu et al. 2002). The general manufacturing process for the hGH SABER depot was also developed as a dual-container configuration, with the liquid delivery matrix and the spray-dried solid active drug being mixed together at the point of use. For the delivery matrix, the solvent system was a mixture of ethanol and benzyl alcohol, and the addition of the hydrophobic polymer polylactic acid (PLA) in the formulation allowed for improved control of the initial burst release, while the inclusion of sucrose in the protein formulation led to improved release of hGH primarily due to its well-known stabilizing effects. While sucrose acetate isobutyrate is commonly used as a food additive (Reynolds and Chappel 1998), the biocompatibility of this material as a drug delivery matrix for parenteral administration is still undergoing investigation.
2.2 Stimuli-Responsive Injectable Depots
Several other materials exhibit distinct phase transitions at around body temperature (Jeong et al. 2002), although these systems are in earlier stages of development than solvent-precipitating gels. The most common of these systems are two triblock copolymer systems: polypropylene oxide/polyethylene oxide systems and PLGA/polyethylene glycol systems. Both of these materials attract considerable interest because they are available in many different variations and are often used in preclinical proof of concept studies, though demonstrations of late stage development and commercialization are limited.
The triblock copolymers based on polypropylene oxide and polyethylene oxide, PEO-PPO-PEO, referred to as poloxamers (Poloxamers® or Pluronics®) are commonly investigated for drug delivery applications (Kabanov et al. 2002) because they are available in a variety of different compositions and the gelation behavior has been extensively studied. These materials exhibit physiologically relevant gelling behavior only at high concentrations, and therefore these systems may be at a disadvantage due to the osmolality of the formulations, viscosity, and frequently observed cytotoxicity (Sriadibhatla et al. 2006).
As an alternative to the poloxamers, the triblock copolymer made of PLGA-PEG-PLGA (ReGel®), polymers also undergo phase transition at physiologically relevant temperatures. Studies have shown that the block ratio of PEG:PLGA, molecular weight, block lengths, and polydispersity can all affect the properties of the gelation behavior (Fig. 3.1) (Chen et al. 2005; Yu et al. 2008). Although organic solvents are not required for these systems, a common problem is high drug burst. Peptide and protein drugs are often very hydrophilic due to exclusion of the aqueous phase during the course of the sol–gel transition. At this point in time, the application of the ReGel polymers is likely to be limited to hydrophobic drugs, such as paclitaxel (Elstad and Fowers 2009), and hydrophilic drugs with wide therapeutic windows.
Phase diagram of representative PLGA-PEG-PLGA solutions. The three triblock copolymers are distinguished by the number-averaged molecular weight, Mn, of each polymer block: copolymer-1, 1730-1500-1730; copolymer-2, 1740-1500-1740; and copolymer-3, 1400-1000-1400. Reprinted from reference (Yu et al. 2008), with permission from Elsevier
3 Formulation Development of Lipid–Drug Delivery Systems
A close examination of an electron micrograph of an erythrocyte membrane, thinly sectioned and stained with osmium tetroxide, reveals a bilayer structure composed of phospholipids, in which polar head groups face outwardly to sequester the hydrophobic fatty acyl tails from the surrounding aqueous environment. It was a similar microscopic observation of biomembranes that led to the seminal paper published by Bangham et al. (Deamer and Bangham 1976) in the 1970s on structures that went on to become modern day liposomes.
Liposomes in the broadest sense are self-assembled colloidal particles with phospholipids as their major molecular constituents. Phospholipids belong to a class of amphiphilic lipids (Fahy et al. 2005, 2007) (i.e., soaps, detergents), and their often polar and hydrophilic head group and adjoining nonpolar hydrophobic tail together have the ability to form a sheetlike structure that encloses on itself when presented to an aqueous environment under agitation, forming multilamellar vesicles. Liposomes’ potential as drug delivery vehicles was once overshadowed by their inherent thermodynamic instability, though today, these challenges have been addressed and many of the “nonconventional” drug delivery systems approved or in development for parenteral administration for both human and veterinary applications fall into the liposomal formulation category (Tables 3.1 and 3.2) (Janoff 1999; ElBayoumi and Torchilin 2009). Most of the formulations approved for use in humans contain phosphatidylcholine (neutral charge), with fatty acyl chains of varying lengths and degrees of saturation (Langer 1990; Lian and Ho 2001). However, some of the important challenges associated with liposomal formulation remain, including their limited physical stability, burst release, low activity due to nonspecific tumor targeting, and nonspecific clearance by the reticuloendothelial system (RES) (Davis 2004; Wissing et al. 2004a).
3.1 Preparation and Characterization of Liposomes
The preparation of liposomes is broadly divided into two categories; one approach entails the physical modification of existing bilayers, while another approach involves synthesis of new bilayers via removal of a lipid-solubilizing agent. For preparation of small unilamellar vesicles (SUVs) at a large scale, a thin film is either formed via lyophilization of lipid mixtures from tert-butanol or spray-drying followed by primary hydration of lipids. For final preparation of the liposomes, ultrasonication irradiation, and high-pressure homogenization or extrusion are often utilized (Lasic 1998).
3.1.1 Ultrasonication Irradiation
In this method, a probe sonicator is utilized to form SUVs rapidly and conveniently. The procedure is often carried out in presence of inert atmosphere and lowered temperatures to decrease the oxidation risk of unsaturated lipids. A cooling bath is used to dissipate the heat generated as the result of sonication. The final step includes centrifugation to remove the small titanium particles that may be shed during the course of sonication.
3.1.2 High-Pressure Homogenization or Extrusion
High-pressure homogenization or extrusion involves forcing multilamellar liposomes through defined size “straight-through” pores at high pressures. Repeated passage of the liposomes through these small-sized pores at temperatures lower than the crystallization temperature (Tc) leads to deformation and reformation of lamellar layers in defined size and subsequently results in a more a monodisperse population.
3.1.3 Drug Loading
Neutral, hydrophilic drugs are introduced into the liposomal formulation in the hydration step, whereas hydrophobic drugs may be solubilized in the preliminary steps of lipid mixture solubilization and lyophilization. In the case of charged molecules, a pH gradient may be utilized to remotely load the liposomes. For example, an ammonium sulfate buffer gradient can be used to create an acidic interior, or sodium bicarbonate can be used to generate a basic interior.
3.1.4 Effect of Lipid Composition on Size and Surface Characteristics
The fate of liposomes in vivo is largely dependent upon liposome–liposome interactions as well as interactions between liposomes and their local environment; these interactions vary in nature from electrostatic to Van der Waals depending on the size and surface of liposomes. The optimal size for preparation of liposomes lies in the range of 10–100 nm. The lower bound is based on a threshold for first-pass elimination via kidneys and the upper bound is roughly based on the size of the leaky vasculature of mouse tumor models (Davis et al. 2008). As for the surface charge, studies have shown that particles with slight negative or positive charge have longer circulation times than those that are highly charged (positive or negative).
3.2 Representative FDA-Approved Liposomal Formulations
Two examples of FDA-approved and FDA-marketed liposomal formulations are Doxil® and DaunoXome® both of which are used to treat AIDS-related Kaposi’s sarcoma (Table 3.1) (Janoff 1999; ElBayoumi and Torchilin 2009). The Doxil® (Johnson & Johnson) formulation is a liquid suspension containing 80–100 nm liposomal formulation composed of 2000 MW PEG-distearoylphosphatidylethanolamine-hydrogenated soybean phosphatidylcholine-cholesterol (20 mM) with doxorubicin hydrochloride. The active pharmaceutical ingredient (API) is loaded into the liposomes using an ammonium sulfate pH gradient method (Barenholz 2012). Doxil’s long circulating formulation was granted accelerated FDA approval in 1995, with DaunoXome® following soon after.
DaunoXome® (Galen) is a solution of citrate salt of daunorubicin (DAU) encapsulated within the aqueous core of a SUV composed of distearoylphosphatidylcholine (DSPC) and cholesterol in a 2:1 molar ratio. The overall lipid to drug composition is 10:5:1 for DSPC:Chol:DAU, and similarly a pH gradient method is used to load DAU into the liposome (Forssen 1997). While the exact manufacturing details of the aforementioned formulations are not available, they likely were prepared using high-shear homogenization or extrusion of the phospholipid derivatives followed by API loading using pH gradient method; the free drug is then further removed using dialysis under aseptic conditions, followed by aseptic filtration to ensure sterility of the final product.
3.3 Targeted In Vivo Delivery Using Liposomal Formulations: Stealth Liposomes and Immunoliposomes
3.3.1 Effect of Lipid Composition on In Vivo Fate: Stealth Liposomes
Early liposomal formulations were mainly composed of neutral and negatively charged phospholipids such as phosphatidylcholine or sphingomyelin, leading to their recognition and eventual endocytosis by cells of the mononuclear phagocytic system (MPS), mostly fixed Kupffer cells in the liver and spleen. This fate suits drug delivery to these organs, though it also prevents delivery applications elsewhere. Frank Davis and colleagues developed the first generation of polyethylene glycol (PEG)-conjugated proteins and peptides in the late 1970s (Davis 2002). Their findings showed that the PEGylated complex was 5–10 times larger than the free drug form due to the binding of water molecules to the ethylene glycol subunits, which decreases renal clearance rates and improves the pharmacodynamic and pharmacokinetic properties of PEGylated polypeptide drugs (Harris and Chess 2003). Additionally a closer look at the recognition and uptake mechanism by RES showed that adsorption of degraded blood proteins and opsonins onto the negatively charged liposomal surface expedited their clearance; employing a similar strategy to evade uptake by the RES and to prolong circulation time in the plasma culminated in development of PEG-coated, sterically stabilized liposomes (Harris and Chess 2003; Kozlowski et al. 2001; Skubitz and Haddad 2005; Spira et al. 2008). The density of the attached PEG groups showed a direct correlation to increased circulation time in vivo. The hydrophilic shield provided by the PEG groups increases the circulation time of liposomes in the system by reducing the rate of plasma protein adsorption on the hydrophilic surface. Further understanding of the extent of therapeutic potential of liposomal formulations were brought into light when a detailed understanding of lipid polymorphisms, physiological mechanisms of in vivo liposome deposition, and lipid–drug and lipid–protein interaction emerged and resulted in enhanced design of such systems with increased in vivo stability and improved biodistribution (Lian and Ho 2001).
3.3.2 Active Targeting: Immunoliposomes
Various candidate ligands have been examined to target liposomes to tumors with overexpressed receptors. Targeting ligands can range from macromolecules, such as antibodies and transferrin, to small-molecule ligands such as folate, lectins, and others (Skubitz and Haddad 2005; Benesch and Urban 2008; Gabizon et al. 2003). The design criteria for a viable ligand with the potential to successfully target tumors include ease of ligand production in large scale, purification and stability, and the know-how of ligand-liposomes conjugation strategies without compromising the properties of either factor.
The use of monoclonal antibodies (mAb) is not straightforward; although the presence of two binding sites promotes mAb stability and high affinity, the Fc receptor-mediated response may lead to high spleen and liver uptake and subsequent increase in immunogenicity of the molecule. To counter this effect, modification and fragmentation of the whole antibody molecule has been undertaken and tremendous efforts are being made to improve the fate of antibody-coated liposomes. One such example is the so-called post-insertion method, in which ligands are conjugated to end-functionalized groups in PEGylated lipid micelles. The ligand–PEG–lipid conjugate is then transferred in an incubation step from micellar form to the outer monolayer of the already-formed liposomes (often Doxil®). This method has been used in studies of HER2-scFv conjugated liposomes for cancer therapy and anti-TfR scFv-lipoplexes for gene delivery. Another method relies on use of grafted maleimide-containing PEG lipids in liposomal preparation, followed by conjugation of cysteine-bearing antibodies at the c-terminus. While both of these methods can be rather cumbersome and difficult to control, the later may be more straightforward while the former combines the challenging insertion process with the task of separating the micellar ligand-PEG-lipids from the coated lipsomes (Puri et al. 2009).
The challenges that remain in the development of immunoliposomes vary from a continuous effort to improve their current design to determination of optimal ligand density on the liposomal surface and the choice of ligands for different tumor cell models. Evidence seems to indicate a balance between ligand density and ligand affinity, as well as the use of low affinity ligands may offer further penetration into the tumor environment (Puri et al. 2009).
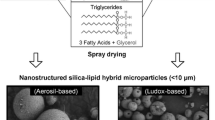
3.4 Alternative/Composite Systems in Preclinical Development: Solid Lipid Particles
The need for development of an alternative lipid-based drug delivery system besides liposomes, which allows for higher control over drug release and better loading efficiency, has brought solid lipid carriers into light (Jaspart et al. 2007; Kohane 2007; Mehnert and Mader 2001; Muller et al. 2002, 2007; Reithmeier et al. 2001; Saraf et al. 2006). Solid lipid particles are made from solid lipids (i.e., lipids that remain solid at room and body temperature) and are stabilized by surfactants. By definition, the lipids can be purified triglyceride, complex glyceride mixtures (mono-, di-), and waxes (Muller et al. 2002; Wissing et al. 2004b). The main advantages of solid lipid particles are the excellent physical stability, protection of encapsulated labile drugs from degradation, controlled release depending on the incorporation model, good tolerability, and the potential for targeted delivery (Wissing and Muller 2002).
Solid lipid nanoparticles (SLN) are usually made by means of high-pressure homogenization and are mainly characterized by their less than 200 nm size. Use of physiologically derived lipids and the absence of organic solvents in SLN’s preparation minimize the risk for potentially acute and chronic toxic response and pose these delivery systems as strong contenders for parenteral delivery. Full characterization of SLN has shown that methods of preparation, lipid composition, and choice of emulsifier have a direct impact on the final size, charge, and stability of these particles. In addition, the degree of lipid crystallinity and degree of modification of lipids are strongly correlated with drug incorporation within SLN and their release rates (Gershkovich et al. 2008). The shortcomings of SLN delivery are similar to other nanotechnology-based platforms, in particular their rapid physiological clearance via the spleen and liver. Similar to liposomal formulations, this response is advantageous for those particular cases where spleen and liver are targeted delivery sites; however, it remains an undesirable outcome in case of delivery intended for other major organs.
4 Conclusion
Drug delivery technology research has blossomed in recent decades, expanding from technologies traditionally focused on extended release to now include nanotechnologies and other functionalized molecular architectures for target-specific delivery. Despite the extensive literature and high levels of research activity in developing novel delivery systems, however, the number of products on the market is few and far between due to the significant manufacturing, regulatory, and safety challenges that must be addressed.
From a formulation and manufacturing scale-up point of view, the addition of a controlled-release technology arguably adds an additional element of complexity to the formulation and process development of parenteral formulations, so the key consideration is to balance the cost and benefits in matching the appropriate molecule to the technology. Experience has shown that the large-scale reproducible production of drug delivery technologies is rarely straightforward from bench to industrial scale, and significant investments in the production process are very common. The challenges in scaling up production of these systems are large, and the publications on this topic are relatively rare. In the face of such challenges, and even more so as costs of development continue to soar, the overarching need within drug delivery is to develop technologies that can be applied widely across molecule classes, instead of the ostensibly bespoke formulations that are on the market thus far.
In spite of these challenges, academic and industry continue to invest in drug delivery technologies, a salient indicator of the needs for these enabling technologies in driving medical and marketplace differentiation for pharmaceutical products. As these technologies mature and gain acceptance in the marketplace, drug delivery technologies will play an increasingly prominent role in meeting the current and future needs of medical providers and patients.
References
Aggarwal S (2011) What’s fueling the biotech engine—2010 to 2011. Nat Biotechnol 29(12):1083–1089
Barenholz Y (2012) Doxil—the first FDA-approved nano-drug : lessons learned. J Control Release 160(2):117–134
Benesch M, Urban C (2008) Liposomal cytarabine for leukemic and lymphomatous meningitis: recent developments. Expert Opin Pharmacother 9(2):301–309
Brodbeck KJ, DesNoyer JR, McHugh AJ (1999) Phase inversion dynamics of PLGA solutions related to drug delivery. Part II. The role of solution thermodynamics and bath-side mass transfer. J Control Release 62(3):333–344
Chen S, Pieper R, Webster DC, Singh J (2005) Triblock copolymers: synthesis, characterization, and delivery of a model protein. Int J Pharm 288(2):207–218
Davis FF (2002) The origin of pegnology. Adv Drug Deliv Rev 54(4):457–458
Davis SS (2004) Coming of age of lipid-based drug delivery systems. Adv Drug Deliv Rev 56(9):1241–1242
Davis ME, Chen ZG, Shin DM (2008) Nanoparticle therapeutics: an emerging treatment modality for cancer. Nat Rev Drug Discov 7(9):771–782
Deamer D, Bangham AD (1976) Large volume liposomes by an ether vaporization method. Biochim Biophys Acta 443(3):629–634
Dunn RL (2002) The atrigel drug delivery system. In: Rathbone MJ, Hadgraft J, Roberts MS (eds) Modified Release Drug Delivery Technology. Marcel Dekker, New York, pp 647–656
Dunn DL, English JP, Cowsar DR, Vanderbelt DP (1990) Biodegradable in situ forming implants and methods of producing the same. US Patent 4,938,763
ElBayoumi TA, Torchilin VP (2009) Current trends in liposome research. In: Weissig V (ed) Liposomes, methods and protocols. Springer, New York, pp 1–27
Elstad NL, Fowers KD (2009) OncoGel (ReGel/paclitaxel)—clinical applications for a novel paclitaxel delivery system. Adv Drug Deliv Rev 61(10):785–794
Fahy E, Subramaniam S, Brown HA, Glass CK, Merrill AH Jr, Murphy RC, Raetz CR, Russell DW, Seyama Y, Shaw W, Shimizu T, Spener F, van Meer G, VanNieuwenhze MS, White SH, Witztum JL, Dennis EA (2005) A comprehensive classification system for lipids. J Lipid Res 46(5):839–861
Fahy E, Sud M, Cotter D, Subramaniam S (2007) LIPID MAPS online tools for lipid research. Nucleic Acids Res 35(Web Server issue):W606–W612
Forssen EA (1997) The design and development of DaunoXome® for solid tumor targeting in vivo. Adv Drug Deliv Rev 24:133–150
Gabizon A, Shmeeda H, Barenholz Y (2003) Pharmacokinetics of pegylated liposomal Doxorubicin: review of animal and human studies. Clin Pharmacokinet 42(5):419–436
Gershkovich P, Wasan KM, Barta CA (2008) A review of the application of lipid-based systems in systemic, dermal/transdermal, and ocular drug delivery. Crit Rev Ther Drug Carrier Syst 25(6):545–584
Graham PD, Brodbeck KJ, McHugh AJ (1999) Phase inversion dynamics of PLGA solutions related to drug delivery. J Control Release 58(2):233–245
Harris JM, Chess RB (2003) Effect of pegylation on pharmaceuticals. Nat Rev Drug Discov 2(3):214–221
He C, Kim SW, Lee DS (2008) In situ gelling stimuli-sensitive block copolymer hydrogels for drug delivery. J Control Release 127(3):189–207
Janoff AS (1999) Liposomes as pharmaceuticals. In: Jannoff AS (ed) Liposomes: rational design. Marcel Dekker, New York, pp xix–xxxi
Jaspart S, Bertholet P, Piel G, Dogne JM, Delattre L, Evrard B (2007) Solid lipid microparticles as a sustained release system for pulmonary drug delivery. Eur J Pharm Biopharm 65(1):47–56
Jeong B, Kim SW, Bae YH (2002) Thermosensitive sol–gel reversible hydrogels. Adv Drug Deliv Rev 54(1):37–51
Kabanov AV, Batrakova EV, Alakhov VY (2002) Pluronic block copolymers for overcoming drug resistance in cancer. Adv Drug Deliv Rev 54(5):759–779
Kohane DS (2007) Microparticles and nanoparticles for drug delivery. Biotechnol Bioeng 96(2):203–209
Kozlowski A, Charles SA, Harris JM (2001) Development of pegylated interferons for the treatment of chronic hepatitis C. BioDrugs 15(7):419–429
Langer R (1990) New methods of drug delivery. Science 249(4976):1527–1533
Lasic DD (1998) Novel applications of liposomes. Trends Biotechnol 16(7):307–321
Lian T, Ho RJ (2001) Trends and developments in liposome drug delivery systems. J Pharm Sci 90(6):667–680
Mehnert W, Mader K (2001) Solid lipid nanoparticles: production, characterization and applications. Adv Drug Deliv Rev 47(2–3):165–196
Muller RH, Radtke M, Wissing SA (2002) Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv Drug Deliv Rev 54(Suppl 1):S131–S155
Muller RH, Petersen RD, Hommoss A, Pardeike J (2007) Nanostructured lipid carriers (NLC) in cosmetic dermal products. Adv Drug Deliv Rev 59(6):522–530
Okada H, Toguchi H (1995) Biodegradable microspheres in drug delivery. Crit Rev Ther Drug Carrier Syst 12(1):1–99
Okumu FW, Dao le N, Fielder PJ, Dybdal N, Brooks D, Sane S, Cleland JL (2002) Sustained delivery of human growth hormone from a novel gel system: SABER. Biomaterials 23(22):4353–4358
Packhaeuser CB, Schnieders J, Oster CG, Kissel T (2004) In situ forming parenteral drug delivery systems: an overview. Eur J Pharm Biopharm 58(2):445–455
Puri A, Loomis K, Smith B, Lee J, Yavlovich A, Heldman E, Blumental R (2009) Lipid-based nanoparticles as pharmaceutical drug carriers: from concept to clinic. Crit Rev Ther Drug Carrier Syst 26(6):523–580
Reithmeier H, Herrmann J, Gopferich A (2001) Lipid microparticles as a parenteral controlled release device for peptides. J Control Release 73(2–3):339–350
Reynolds RC (1998) Metabolism and pharmacokinetics of sucrose acetate isobutyrate (SAIB) and sucrose octaisobutyrate (SOIB) in rats, dogs, monkeys or humans: a review. Food Chem Toxicol 36(2):95–99
Reynolds RC, Chappel CI (1998) Sucrose acetate isobutyrate (SAIB): historical aspects of its use in beverages and a review of toxicity studies prior to 1988. Food Chem Toxicol 36(2):81–93
Saraf S, Mishra D, Asthana A, Jain R, Singh S, Jain NK (2006) Lipid microparticles for mucosal immunization against hepatitis B. Vaccine 24(1):45–56
Sartor O (2003) Eligard: leuprolide acetate in a novel sustained-release delivery system. Urology 61(2 Suppl 1):25–31
Skubitz KM, Haddad PA (2005) Paclitaxel and pegylated-liposomal doxorubicin are both active in angiosarcoma. Cancer 104(2):361–366
Spira J, Plyushch OP, Andreeva TA, Khametova RN (2008) Evaluation of liposomal dose in recombinant factor VIII reconstituted with pegylated liposomes for the treatment of patients with severe haemophilia A. Thromb Haemost 100(3):429–434
Sriadibhatla S, Yang Z, Gebhart C, Alakhov VY, Kabanov A (2006) Transcriptional activation of gene expression by pluronic block copolymers in stably and transiently transfected cells. Mol Ther 13(4):804–813
Van Tomme SR, Storm G, Hennink WE (2008) In situ gelling hydrogels for pharmaceutical and biomedical applications. Int J Pharm 355(1–2):1–18
Wissing SA, Muller RH (2002) Solid lipid nanoparticles as carrier for sunscreens: in vitro release and in vivo skin penetration. J Control Release 81(3):225–233
Wissing SA, Kayser O, Muller RH (2004a) Solid lipid nanoparticles for parenteral drug delivery. Adv Drug Deliv Rev 56(9):1257–1272
Wissing SA, Muller RH, Manthei L, Mayer C (2004b) Structural characterization of Q10-loaded solid lipid nanoparticles by NMR spectroscopy. Pharm Res 21(3):400–405
Yu L, Chang GT, Zhang H, Ding JD (2008) Injectable block copolymer hydrogels for sustained release of a PEGylated drug. Int J Pharm 348(1–2):95–106
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 American Association of Pharmaceutical Scientists
About this chapter
Cite this chapter
Chen, D., Yazdi, S. (2013). Polymer- and Lipid-Based Systems for Parenteral Drug Delivery. In: Kolhe, P., Shah, M., Rathore, N. (eds) Sterile Product Development. AAPS Advances in the Pharmaceutical Sciences Series, vol 6. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7978-9_3
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7978-9_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7977-2
Online ISBN: 978-1-4614-7978-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)