Abstract
Advancing age is known to severely affect female fertility with correlations to increased spontaneous abortions, chromosomal defects in offspring, preterm delivery, and intrauterine growth restriction. In contrast, the effect of advanced paternal age has received far less attention. This is likely a result of the absence of such striking effects compared with those associated with maternal aging. Nevertheless, recent data suggesting an association between advanced paternal age and neuropsychiatric disorders in offspring have increased the attention given to the effects of paternal age on sperm quality and to offspring health and disease susceptibility. We have learned from many recent studies that paternal aging does significantly affect fecundity in males through declines in semen parameters and increases in genetic and epigenetic abnormalities. The identification of these risks and their coverage in popular media require that physicians are well versed in the data and are able to communicate the relative risks of paternal aging on offspring health in addition to interpreting the absolute risk of these abnormalities to concerned patients. This chapter will review the current literature regarding male age-associated changes to semen parameters and the effects of advanced paternal age on offspring disease risk. We will also attempt to put these risks into clinical context.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Advanced paternal age has become a heavily investigated topic recently as a result of multiple studies demonstrating ties between advanced paternal age and various offspring abnormalities. Further contributing to the increasing interest in the role of advanced paternal age in reproduction is the trend of delayed parentage believed to be a result of socioeconomic pressures in developed countries [1]. Though this trend is justified by increasing life expectancies in both sexes, advanced paternal age significantly affects general semen parameters and sperm quality that ultimately alters fecundity and may additionally affect offspring health. While many couples consider the risks associated with advanced maternal age in family planning decisions, very little thought is given to the age of male partners. As a result, it is important that physicians consulting couples with an aged male partner have the available data to help patients make well-informed family planning decisions based on the risks associated with advanced paternal age. This chapter will outline what is currently known regarding the effects of paternal age on fecundity and will also discuss the associations between advanced paternal age and the offspring’s disease risk. These effects, based on current data are summarized in Table 3.1.
Delayed Parenthood
In recent history, the age of parenthood for both males and females has steadily increased in many developed countries. This trend is believed to be associated with increased life expectancy, socioeconomic pressures, and divorce rates with subsequent remarriage at older ages [2]. During a 10-year span (1993–2003) in Great Britain, the percent of fathers who were in the age range of 35–54 increased from 25 % of total births to 40 %. Associated with this trend was a decrease in the number of births to fathers less than 35 years of age from 74 % of total births to only 60 % [3]. In Australia, over two decades (1988–2008), the average age of fathers has increased by approximately 3 years [4]. Similarly, the average age of fathers in Germany increased by 2 years over a 10-year period [2]. Similar trends can be found in the United States and many other developed countries. As average paternal age continues to increase in many countries it is becoming increasingly important to characterize the potential consequences of advanced paternal age on fertility and offspring health.
Age-Related Changes in Sperm Quality
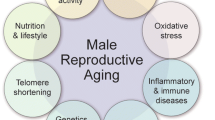
With advancing male age, a number of changes occur to sperm and semen that can impact fertility status or increase the risk of disease transmission to offspring. These changes include declines in some semen parameters, increased sperm DNA damage, genetic changes in sperm resulting from mitotic or meiotic errors or errors that arise during DNA replication, and epigenetic changes to sperm DNA. These changes are discussed below.
Changes in Semen Parameters
Unlike females, who are born with a finite number of gametes that are generally exhausted between the age of 45 and 55 years, coincident with menopause, men continue to produce sperm throughout their lives. While spermatogenesis continues well into old age, some semen parameters do decline as men age. Numerous studies have evaluated the effects of male age on semen parameters, but shortcomings of some of the individual studies include small sample size and failure to control for potentially confounding factors. For this reason there exists a significant degree of discordance between studies, making the reliable estimate of age effects difficult to quantify. However, a thorough review of the literature from 1980 to 1999 by Kidd et al. evaluated the effect of age on semen parameters and concluded that there is general agreement among studies that semen volume, sperm motility, and proportion of morphologically normal sperm all decline with advancing age [5]. These conclusions were corroborated by more recent literature reviews and carefully controlled primary research [6–8].
From the available literature, it can be inferred that semen volume significantly decreases with age, with a decline of 3–22 % from age 30 to age 50 [5, 8]. Similarly, a 3–37 % decrease in sperm motility is estimated to occur over the same period, as indicated in several studies [5, 8]. Finally, the best estimates for declines in normal sperm morphology indicate a decrease of 4–22 % between the ages of 30 and 50 [5, 8]. The data regarding changes in sperm concentration with age are less conclusive, and total sperm count has rarely been evaluated. Of more than 20 studies that evaluated the effect of male age on sperm concentration, there is essentially an even split between studies that report a decline, those that report no age effect, and those that report increased sperm concentrations with advancing age [5, 8]. As semen volume significantly declines with age, if spermatogenic output remained constant, then sperm concentration would necessarily increase in older men. A recent study of 1,174 men age 45 and older reported a non-significant increase in sperm concentration with age, and a significant decline in total sperm count with advancing age in men between the ages of 45 and 80 [9].
While the consensus based on large datasets is that semen volume, sperm motility, and normal sperm morphology decrease with advancing age, the decreases are generally modest. Moreover, the number of confounding variables such as lifestyle factors, environmental influences, health status, abstinence periods, and others make it nearly impossible to identify the age-associated causes that are directly responsible for these declines.
Genetic Changes
The molecular hallmarks of aging throughout the body include increased oxidative damage, increased aneuploidy rates and chromosomal rearrangements, the accumulation of mutations within the genome, and telomere shortening [10, 11]. Sperm are particularly prone to many of these changes due to the high rate of cell division relative to most other cells types in the body. However, unlike telomere attrition that occurs in the majority of other cell types, the telomeres length in sperm actually increases with age. Genetic changes to sperm are discussed in the following section.
DNA Damage
Numerous studies have reported an age-related increase in sperm DNA damage [12–16]. The increase in DNA fragmentation index (DFI) is marked, with a nearly fourfold increase in men age 60–80 compared with men age 20–29 reported in one study [14]. In a large study of 1,125 men from infertile couples, DFI more than doubled in men over the age of 45 compared with men aged 30 and younger [16]. The mechanisms responsible for increased sperm DNA damage in older men are not completely characterized, but increased reactive oxygen species (ROS) [17], coupled with the insufficiency of DNA repair and apoptotic machinery, have been proposed [18].
Aneuploidy Rates
The increase in gamete aneuploidy rates in women with advancing age is well documented and dramatic. It is estimated that about 20 % of human oocytes are aneuploid, and the incidence has been reported to be as high as 60 %, with a sharp increase in the decade preceding menopause [19–21]. In contrast, sperm aneuploidy rates are much lower with an estimated average incidence of 1–2 % [20], and the effect of male age on sperm aneuploidy rate remains unclear. Some studies have failed to find an effect of male age on sperm aneuploidy frequency [14, 22], while others have reported a modest increase in aneuploidy rates related to age, particularly increased disomies of the sex chromosomes [23–25].
While there is no consensus on the effect of male age on sperm aneuploidy rates, the majority of evidence suggests a slight increase in sex chromosome disomy rates in older men and a general lack of an effect or a weak effect in the autosomes [8].
Increased Mutations
The introduction of de novo mutations into the genome is the basis for heritable genetic variation, and the number of mutations per genome is related to the number of replication cycles that a cell undergoes, as there is an error rate inherent in replication machinery. Based on family-based sequencing and single sperm sequencing as well as evolutionary measures, the de novo mutation rate of sperm is estimated to be between 1 and 4 changes per 100 million bases per generation [26, 27], while the mutation rate per cell division is almost three orders of magnitude lower than the per generation mutation rate [28]. The more cycles of DNA replication and cell division a cell undergoes, the greater the chance for mutations to occur in that cell. In women, from the primordial germ cell stage to ovulation, an oocyte will have undergone approximately 24 cell divisions [29]. In men that number is estimated to be approximately 30 cell divisions at puberty, with one spermatocyte cell division every 16 days, or 23 divisions per year after puberty (see Fig. 3.1) [29].
Clearly there is a greater opportunity for mutations to arise in sperm than in oocytes, and male age is predicted to be a strong contributing factor. Lionel Penrose was the first to propose a relationship between male age and mutations in offspring [30]. While the mutation load of individual sperm as a function of male age has not been directly measured, molecular genetics predicts that sperm from older men will, on average, harbor more mutations than sperm from younger men. This prediction is substantiated by a recent study of genomic sequence in parent–offspring trios that estimated an increase of approximately two mutations per year of paternal age [31]. In addition, the increased rates of specific autosomal dominant diseases and disease-specific mutation analysis also support an age effect on sperm mutation frequency [14], as will be discussed in detail below.
Changes in Telomeres
While the consequences of advanced paternal age on the genetics of sperm are generally negative, the age-related changes to sperm telomeres might confer some advantage to offspring. Telomeres are composed of long tracts of TTAGGG repeats located at the ends of each chromosome and serve as a buffer to the loss of important genetic material due to the inability of DNA replication machinery to replicate DNA at the very end of each chromosome. In addition, the telomere cap at the end of each chromosome distinguishes chromosome ends from double strand breaks and thus serves to protect against spurious chromosomal fusion [32]. While in most tissues, telomeres progressively shorten with age, ultimately resulting in cell cycle arrest or apoptosis, the telomeres in sperm are longer in older men [33], and children of older fathers have longer leukocyte telomeres than do children of younger fathers [34, 35]. Telomere inheritance may represent an example of a genetic advantage of delayed reproduction in men as longer leukocyte telomere length is associated with decreased risk of atherosclerosis and increased lifespan [36].
Epigenetic Changes
The effect of advanced paternal age on offspring has begun to receive much attention. Recent studies have linked paternal aging and the prevalence of well-known neuropsychiatric disorders in offspring [37–39]. Large retrospective studies demonstrate the effect of paternal age on various birth outcomes, including weight, premature deliveries, and various offspring abnormalities [40, 41]. Additionally, recent research has begun to elucidate associations between aged fathers and increased incidence of obesity in offspring. These findings were independent of maternal age and other outside factors [42]. However, the etiology of the increased frequency of various disorders in the offspring of aged males remains poorly defined, though there are likely candidates.
In both sexes, aging alters DNA methylation marks in most somatic tissues throughout the body [43, 44]. Because of its prevalence in other cell types, aging-associated DNA methylation alteration is likely to occur in sperm as well. In fact, Oakes et al. have described age-associated hypermethylation at specific genomic loci in both sperm and liver tissue in male rats [44]. Similarly, our laboratory has identified increased global DNA methylation associated with age in human sperm from fertile donors (unpublished data). In further support of this idea is work demonstrating that frequently dividing cells have more striking methylation changes associated with age than do cells which divide less often [45]. Additionally, a recent study also indicates that, at specific gene promoters, there is increased DNA methylation in the offspring of older fathers [46]. These data further suggest the possibility of heritable DNA methylation alterations associated with advanced paternal age.
In addition to DNA methylation alterations there are data to suggest alterations in chromatin packing that occur with age as well. It has been suggested that chromatin remodeling plays a key role in cellular senescence, organismal aging, and age-associated disease and thus could play a role in age-associated sperm alterations that may ultimately affect the offspring [47]. In fact, Nijs et al. described altered chromatin packing associated with age as assessed by the sperm chromatin structure assay [48]. The subtle nature of the effect and, in some cases, the absence of well-characterized genetic factors, in addition to the aging-associated somatic cell methylation alterations, suggest that a major contributing factor to the increased prevalence of various diseases among the offspring of aged fathers is the sperm epigenome.
Reproductive Consequences of Age-Related Changes in Sperm
Fecundity
Among the consequences of delayed paternity, and likely the most dramatic alteration that occurs with increased paternal age, is that of decreased fecundity. Though very different from the universal and abrupt age-associated cessation of fertility seen in females, there is a significant decline in a male’s capacity to produce viable offspring that is correlated with age. However, the age at which an individual male’s reproductive capacity declines and even the frequency of this decline among a population of men remains controversial. Despite this, there are many studies that demonstrate an age effect on male fecundity with study groups, including natural conception, artificial insemination, and in vitro fertilization.
In an observational study performed in the United Kingdom in 2003, Hassan et al. found that men >45 years of age had a fivefold increase in their time to pregnancy in comparison to individuals <25 years of age [49]. Interestingly, when compared to males <25, men 45 and older were also 12.5 times more likely to have a time to pregnancy of greater than 2 years [49]. As expected, this effect is amplified when the female member of a couple is of advanced reproductive age as well (35–39). In these couples, men >40 were more than two times more likely to fail to conceive during a 12 month period in comparison to men <40 [50]. Additionally, when taken into account unsuccessful pregnancies in the same groups men over 40 were three times less likely to produce viable offspring than do the younger cohort [50]. Other studies support these data by suggesting an increased frequency of fetal loss to those fathered by older men, increased time to pregnancy, and decreased probability of conception [51–53]. However, there are conflicting data which suggest little to no effect of paternal age on fertility in natural conception [54].
Research has also described effects of paternal age on the outcomes of assisted reproductive techniques. A total of 17,000 intrauterine insemination (IUI) cycles analyzed in a French study revealed that the pregnancy rate for couples whose male partner was less than 30 years of age had a pregnancy rate of 12.3 % where couples whose male partner was over 30 years of age had a significantly lower pregnancy rate of 9.3 % after adjusting for female age [55]. Similarly, in 1995, Mathieu et al. showed that increasing male age (≥35 years of age) was associated with decreased rates of conception [56]. However, these data are controversial. Additional studies have failed to find a paternal age effect on IUI pregnancy rates [57]. Other studies have analyzed the paternal age effect on in vitro fertilization (IVF) success with a similar controversy. Many studies suggested that there is a paternal age effect in achieving viable pregnancy outcomes in IVF cycles [58] and also have suggested that this effect is amplified with partners of advanced maternal age [59]. In large studies involving the use of donor eggs in an IVF cycle showed a significant effect of paternal age on pregnancy outcome [60]. However, an even more recent study that corrected for age of the egg donor found no effect of paternal age on pregnancy outcome [61].
Disease Risk in Offspring
As would be expected, the numerous genetic and epigenetic changes that occur to sperm through the aging process are associated with elevated risk of some diseases in the offspring of older fathers. These include several rare, autosomal disorders, disorders involving expanded trinucleotide repeats, offspring aneuploidy, certain cancers, and several neuropsychiatric disorders. These diseases and associated risks will be discussed below. While risks of these disorders are demonstrably elevated in offspring of older fathers, it is important to emphasize that the paternal age contribution to the increased risk is generally quite low (with the exception of the autosomal dominant and triplet repeat disorders) and absolute risk for any of these disorders remains quite low.
Autosomal Dominant Disorders
Rare autosomal disorders, including Apert syndrome and achondroplasia, are among the most striking and earliest characterized examples of increased disease risk as a consequence of advanced paternal age. As early as 1912, it was observed that sporadic cases of achondroplasia, a dominantly inherited form of dwarfism, was most often found in the last-born children of a family [29]. More recently, a number of other diseases have been shown to display similar paternal age effects.
A dozen diseases showing a significant paternal age effect were described in a paper more than three decades ago, and several others have been described since that time [62]. In addition to achondroplasia and Apert syndrome, the list of autosomal dominant disorders that display a paternal age effect includes acrodysostosis, fibrodysplasia ossificans progressive, neurofibromatosis, multiple endocrine neoplasia 2A (MEN 2A) and MEN 2B, and syndromes including Marfan, Treacher-Collins, Crouzon, Noonan, and Pfeiffer, among others [62].
Remarkably, many of these conditions, including Apert syndrome, achondroplasia, Crouzon syndrome, Pfeiffer syndrome, MEN 2A, and MEN 2B, involve mutations in three genes, FGF3R, FGFR2, and RET [29, 63]. Moreover, in almost every case where parental origin of the de novo, disease-causing mutation in these genes was assessed, the mutation was paternally derived [29, 63–68]. In addition, the mutated loci linked to many of these disorders are among the most frequently mutated nucleotides in the entire genome [29]. These observations led to the hypothesis of selfish spermatogonial selection, the idea that some spermatogonial mutations confer some advantage, leading to clonal expansion of mutant sperm over time [63, 69]. This mechanism may explain, at least in part, the molecular basis for the increased incidence of these disorders with advanced paternal age.
While it is well established that increasing paternal age does increase the risk for numerous autosomal dominant disorders, it is important to note that the absolute risk for these diseases remains quite low. Additional research is required to fully characterize the mechanisms involved in increased transmission of these diseases by older fathers.
Trinucleotide Repeat Disorders
In addition to the association between point mutations in the male germline and male age, there is also evidence to suggest that other genomic changes, namely changes in trinucleotide repeat length, are also more frequent in the germline of older men. The cause of Huntington’s disease has been traced to an expanded block of CAG tandem repeats within the Huntingtin (HTT) gene [70]. Longer triplet repeats in HTT result in altered protein function and Huntington’s symptoms. It was demonstrated that repeat expansion is almost entirely driven through the male germline [71], and the extent of repeat expansion is significantly associated with paternal age [72].
Myotonic dystrophy (DM) is another disease associated with trinucleotide repeat expansion. Like Huntington’s disease, expanded CTG repeats are more frequently transmitted from the father [73], and paternal age appears to be a risk factor for transmission of the disease [74]. One large study of 3,419 cases of Down syndrome did find a significant paternal age effect after adjusting for maternal age when mothers were older than 35, and the paternal age effect was most significant when maternal age was over 40 [75].
Offspring Aneuploidy
The majority of aneuploidies are embryonic lethal, however trisomies 13, 18, and 21 along with sex chromosome aneuploidies (XXY, XYY, XXX, XO, etc.) are compatible with life. The great majority of somatic aneuploidies are maternally derived. For example in a cohort of 352 cases of Down syndrome, approximately 91 % were of maternal origin, and a maternal contribution to other cases of trisomy involving chromosomes 13, 14, 15, and 22 were similar, ranging from 83 to 89 % [76]. Interestingly, the story is different for sex chromosome aneuploidies, with a little more than half of cases being paternally derived [20].
Given the relatively minor effect of paternal age on sperm aneuploidy rates, it is not surprising that epidemiologic data for the paternal contribution to trisomic offspring generally do not support a paternal age effect [8, 77, 78]. A recent study based on 22 EUROCAT congenital anomaly registers identified a marginally significant association between paternal age and Klinefelter syndrome [79]. Several studies have evaluated the relationship between paternal age and incidence of Down syndrome, and in general have reported a weak paternal age effect [80] or no effect at all [81]. Based on available data, clearly the paternal age effect on offspring aneuploidy is relatively small and is eclipsed by the significant maternal age effect.
Cancer
Based on the current literature, it appears that paternal age may have an effect on incidence of various types of cancers in offspring. These data are intriguing but remain quite controversial. One of the most heavily studied classes of disease in these studies is hematological cancers. A recent epidemiological study has described a decreased risk of acute myeloid leukemia in firstborn children, indirectly suggesting that maternal and paternal age may play a role in the frequency of cancer incidence in the offspring. The same study was able to directly detect an increased risk of being diagnosed with any form of childhood leukemia in children sired by fathers of between 35 and 45 years of age when compared to fathers <25 years of age [82]. In agreement with these data is research by Murray et al. which suggests that children born to fathers >35 years of age are 50 % more likely (relative risk = 1.5) to receive a diagnosis of a childhood leukemia [83]. However, a Swedish epidemiological study published in 1999 detected no significant impact of paternal age on hematologic cancers [84].
The impact of paternal age on offspring cancer incidence is not limited to hematologic metastases. There also appears to be an increased risk of developing childhood central nervous system tumors in the offspring of older fathers. One retrospective study showed that children born to a father >30 years of age were at a 25 % increased risk of developing a childhood brain tumor compared to children of fathers <25 years [84]. Similarly, Yip et al. demonstrated that the offspring of fathers >40 had an increased relative risk (approximately 1.7) of developing a central nervous system cancer [85].
Advanced paternal age also appears to affect the incidence of adult onset cancers in offspring. The incidence of breast cancer has been shown to increase in the daughters of fathers who are >40 compared to fathers <30 [86]. Similarly, prostate cancer risk increases by approximately 70 % in the offspring of fathers >38 years of age compared to the children of fathers <27 years of age [87].
The mechanism behind this effect is likely multifactorial and may additionally vary by race. However, there are some candidates that likely play at least some role in the etiology of increased incidence of multiple cancers seen in the offspring of aged fathers. Environmental exposures that accumulate throughout the life of a male are one of the most likely effectors, as this may affect subtle DNA mutations and epigenetic alterations that are capable of being inherited. In fact, as mentioned earlier, there are some data that suggest that the offspring of older fathers have increased levels of DNA methylation at specific loci [46]. If any of these alterations (gene mutations or epigenetic modifications) occur at tumor suppressor genes or other important genes in the etiology of various cancers, the result would be increased cancer incidence as is seen in the current literature. Though this correlation is intriguing, it should be noted that much work is still required to further define the effects of paternal aging on the incidence of cancer in offspring.
Neuropsychiatric Disorders
In recent years, with the application of genomic tools, the genetic complexity of neuropsychiatric disorders is becoming increasingly apparent. However, it has long been suggested that advanced paternal age is a risk factor for schizophrenia [88], and more recently, advanced paternal age has been implicated in risk for autism, bipolar disorder, behavioral disorders, and reduced cognitive ability.
The paternal age effects on schizophrenia risk have been widely studied [89–91]. A recent meta-analysis representing 24 qualifying studies confirmed advanced paternal age to be a significant risk factor for schizophrenia [89]. In this study, the authors reported a slight but significant increase in the risk of developing schizophrenia in offspring from fathers >30 years of age, with relative risk (RR) increasing in older fathers. At the extreme, a combined RR for schizophrenia in the offspring of fathers >50 years of age compared with fathers age 25–29 was 1.66 [89]. Interestingly, there also appears to be a slight but significant risk of schizophrenia in offspring of fathers < 25 years (RR = 1.08) only in male offspring [89].
Associations between paternal age and risk of autism spectrum disorders (ASD) have also been thoroughly investigated, with two meta-analyses confirming a significant association [92, 93]. In the most recent population-based study and meta-analysis, it was estimated that fathers >50 years of age had a 2.2-fold increased risk of autism in offspring compared with men aged 29 years or less [93].
The data regarding the association between paternal age and other neuropsychiatric and behavioral disorders are less clear, but there does seem to be an increase in bipolar disorder [94, 95] and behavioral issues [96, 97] in children of older fathers. In addition, some studies indicate that children of older fathers display slightly reduced IQ compared with children of younger fathers [98, 99], although the differences are small, and conflicting reports exist [100].
While evidence clearly suggests that paternal age does have some impact on neurological development and the incidence of neuropsychiatric disorders, the mechanisms for neurodevelopmental changes have not been elucidated. It has been suggested that increased risk may be related to increased mutations [101], changes in gene dosage as a result of copy number changes in the genome [102], or epigenetic changes associated with age [103]. It is also likely that behavioral factors in the fathers that result in delayed marriage also contribute [88], as these factors are very difficult to quantify and correct for in epidemiological studies.
Consequences in Context
From the available data, it is clear that advanced paternal age affects sperm quality, fecundity, and offspring health. However, this topic is only beginning to be thoroughly explored partially due to the recently growing trend of delayed parenthood that appears to have driven increased media attention toward to the study of advanced paternal age and offspring health. This has placed many physicians in the difficult position of consulting concerned patients regarding their capacity to produce healthy offspring with only scant amounts of data from a field of study in its relative infancy. This discussion is fascinating and extremely complex as a result of the socioeconomic, emotional, and general health issues involved. Physicians should be prepared to address many questions from their patients, but should specifically be able to address two main concerns in this discussion. The first are patients who request to preemptively store sperm at relatively young ages as an alternative to natural conception at an advanced age. The second are male patients who seek advice on the “risks” of having children at advanced age. In either case, the patients must be well informed and comfortable in making their decisions.
Are cryopreserved sperm from a young healthy individual more capable of producing healthy offspring than fresh sperm from the same individual collected at an advanced age? This central question in the paternal aging debate is not easily addressed. In fact, the most accurate answer would be that we simply do not know. It is clear that advanced paternal age has been associated with increased incidence of many disease states in the offspring as has been previously outlined. It is also known that there is a slightly increased risk of birth defects in children conceived through in vitro fertilization (the advanced reproductive technology that would most likely be used in these cases). Additionally, though still controversial, it has been demonstrated that the cryopreservation of sperm, even in the presence of cryomedium, can result in DNA damage thus compounding the problem of using stored samples as an alternative to natural conception at an advanced age [104]. Despite this, because of the low risk in cryopreservation of male gametes, if a patient desires to store sperm at a young age with the intent of future use, it would not be unreasonable to support this decision if the patient has been well educated on the available data.
Patients of advanced age who are considering having children but have not previously stored sperm may also seek medical advice on whether or not they should attempt parenthood based on the recent data that demonstrates increased relative risk to the offspring. Would they be placing their offspring at a significant risk/disadvantage? In response to this question it is important to understand that while the data do suggest a relative increase in the risk of offspring of aged fathers developing many disorders and diseases including, but not limited to schizophrenia, autism and even cancer, the absolute risk of these are still very low. For example, the risk of developing childhood leukemia is approximately 1 in 25,000 in the general public, and in the offspring of older fathers that risk climbs to 1 in 17,000, approximately a 50 % increase [83]. Though the relative risk in this case is statistically significant, the absolute risk to the offspring of an aged father actually developing leukemia remains very low. It will be important for physicians to additionally encourage patients to consider their familial relationships and the emotional benefits of having children and weigh these with the subtle increases in risk of having children at an older age. In consulting male patients of an advanced age, the data do not support the recommendation of halting attempts at conception because of the risks to the offspring as it does in advanced maternal age. Despite this it is important to consider these risks and understand that the cumulative data on the disorders that have relatively increased prevalence in the offspring of older fathers may dissuade some from having children at an older age.
Conclusions
In recent years, we have learned a great deal regarding the effect of aging on male fertility. Advanced paternal age is negatively associated with many semen parameters, and these negative effects likely drive the general decrease in fertility and fecundity seen in males of advanced age. Though not an abrupt and complete loss of fertility as seen in advanced maternal aging, there is a gradual decrease in gamete quality associated with aging in males. This decrease in quality includes DNA damage, various genetic mutations, and epigenetic alterations that appear to be capable of causing abnormalities in the offspring. Though we currently have evidence to support the paternal age associated increase in offspring disease susceptibility, the absolute risk remains quite low. Despite this, couples with an aged male partner should consider these risks and discuss them with their health care provider to determine their best course of action in their desire to conceive a child.
References
Mills M, Rindfuss RR, McDonald P, et al. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update. 2011;17(6):848–60.
Kuhnert B, Nieschlag E. Reproductive functions of the ageing male. Hum Reprod Update. 2004;10(4):327–39.
Bray I, Gunnell D, Davey SG. Advanced paternal age: how old is too old? J Epidemiol Community Health. 2006;60(10):851–3.
Australian Bureau of Statistics: Births, Australia, 2011. 2012 [updated October 25, 2012; cited 2013 March 28]; Available from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/3301.0.
Kidd SA, Eskenazi B, Wyrobek AJ. Effects of male age on semen quality and fertility: a review of the literature. Fertil Steril. 2001;75(2):237–48.
Eskenazi B, Wyrobek AJ, Sloter E, et al. The association of age and semen quality in healthy men. Hum Reprod. 2003;18(2):447–54.
Sartorius GA, Nieschlag E. Paternal age and reproduction. Hum Reprod Update. 2010;16(1):65–79.
Kuhnert B, Nieschlag E. Reproductive functions of the ageing male. Hum Reprod Update. 2004;10(4):327–39.
Hellstrom WJ, Overstreet JW, Sikka SC, et al. Semen and sperm reference ranges for men 45 years of age and older. J Androl. 2006;27(3):421–8.
Johnson FB, Sinclair DA, Guarente L. Molecular biology of aging. Cell. 1999;96(2):291–302.
Guarente L, Kenyon C. Genetic pathways that regulate ageing in model organisms. Nature. 2000;408(6809):255–62.
Humm KC, Sakkas D. Role of increased male age in IVF and egg donation: is sperm DNA fragmentation responsible? Fertil Steril. 2013;99(1):30–6.
Schmid TE, Eskenazi B, Baumgartner A, et al. The effects of male age on sperm DNA damage in healthy non-smokers. Hum Reprod. 2007;22(1):180–7.
Wyrobek AJ, Eskenazi B, Young S, et al. Advancing age has differential effects on DNA damage, chromatin integrity, gene mutations, and aneuploidies in sperm. Proc Natl Acad Sci USA. 2006;103(25):9601–6.
Varshini J, Srinag BS, Kalthur G, et al. Poor sperm quality and advancing age are associated with increased sperm DNA damage in infertile men. Andrologia. 2012;44 Suppl 1:642–9.
Moskovtsev SI, Willis J, Mullen JB. Age-related decline in sperm deoxyribonucleic acid integrity in patients evaluated for male infertility. Fertil Steril. 2006;85(2):496–9.
Cocuzza M, Athayde KS, Agarwal A, et al. Age-related increase of reactive oxygen species in neat semen in healthy fertile men. Urology. 2008;71(3):490–4.
Colin A, Barroso G, Gomez-Lopez N, et al. The effect of age on the expression of apoptosis biomarkers in human spermatozoa. Fertil Steril. 2010;94(7):2609–14.
Jones KT. Meiosis in oocytes: predisposition to aneuploidy and its increased incidence with age. Hum Reprod Update. 2008;14(2):143–58.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2(4):280–91.
Handyside AH. Molecular origin of female meiotic aneuploidies. Biochim Biophys Acta. 2012;1822(12):1913–20.
Luetjens CM, Rolf C, Gassner P, et al. Sperm aneuploidy rates in younger and older men. Hum Reprod. 2002;17(7):1826–32.
Bosch M, Rajmil O, Martinez-Pasarell O, et al. Linear increase of diploidy in human sperm with age: a four-colour FISH study. Eur J Hum Genet. 2001;9(7):533–8.
Griffin DK, Abruzzo MA, Millie EA, et al. Non-disjunction in human sperm: evidence for an effect of increasing paternal age. Hum Mol Genet. 1995;4(12):2227–32.
Lowe X, Eskenazi B, Nelson DO, et al. Frequency of XY sperm increases with age in fathers of boys with Klinefelter syndrome. Am J Hum Genet. 2001;69(5):1046–54.
Conrad DF, Keebler JE, DePristo MA, et al. Variation in genome-wide mutation rates within and between human families. Nat Genet. 2011;43(7):712–4.
Wang J, Fan HC, Behr B, et al. Genome-wide single-cell analysis of recombination activity and de novo mutation rates in human sperm. Cell. 2012;150(2):402–12.
Lynch M. Rate, molecular spectrum, and consequences of human mutation. Proc Natl Acad Sci USA. 2010;107(3):961–8.
Crow JF. The origins, patterns and implications of human spontaneous mutation. Nat Rev Genet. 2000;1(1):40–7.
Penrose LS. Parental age and mutation. Lancet. 1955;269(6885):312–3.
Kong A, Frigge ML, Masson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature. 2012;488(7412):471–5.
Ferreira MG, Miller KM, Cooper JP. Indecent exposure: when telomeres become uncapped. Mol Cell. 2004;13(1):7–18.
Allsopp RC, Vaziri H, Patterson C, et al. Telomere length predicts replicative capacity of human fibroblasts. Proc Natl Acad Sci USA. 1992;89(21):10114–8.
Unryn BM, Cook LS, Riabowol KT. Paternal age is positively linked to telomere length of children. Aging Cell. 2005;4(2):97–101.
Njajou OT, Cawthon RM, Damcott CM, et al. Telomere length is paternally inherited and is associated with parental lifespan. Proc Natl Acad Sci USA. 2007;104(29):12135–9.
Aviv A. Genetics of leukocyte telomere length and its role in atherosclerosis. Mutat Res. 2012;730(1–2):68–74.
Smith RG, Kember RL, Mill J, et al. Advancing paternal age is associated with deficits in social and exploratory behaviors in the offspring: a mouse model. PLoS One. 2009;4(12):e8456.
Naserbakht M, Ahmadkhaniha HR, Mokri B, et al. Advanced paternal age is a risk factor for schizophrenia in Iranians. Ann Gen Psychiatry. 2011;10:15.
Dalman C. Advanced paternal age increases risk of bipolar disorder in offspring. Evid Based Ment Health. 2009;12(2):59.
Wiener-Megnazi Z, Auslender R, Dirnfeld M. Advanced paternal age and reproductive outcome. Asian J Androl. 2012;14(1):69–76.
Alio AP, Salihu HM, McIntosh C, et al. The effect of paternal age on fetal birth outcomes. Am J Mens Health. 2012;6(5):427–35.
Eriksen W, Sundet JM, Tambs K. Paternal age at birth and the risk of obesity in young adulthood: a register-based birth cohort study of norwegian males. Am J Hum Biol. 2013;25(1):29–34.
Wilson VL, Jones PA. DNA methylation decreases in aging but not in immortal cells. Science. 1983;220(4601):1055–7.
Oakes CC, Smiraglia DJ, Plass C, et al. Aging results in hypermethylation of ribosomal DNA in sperm and liver of male rats. Proc Natl Acad Sci USA. 2003;100(4):1775–80.
Thompson RF, Atzmon G, Gheorghe C, et al. Tissue-specific dysregulation of DNA methylation in aging. Aging Cell. 2010;9(4):506–18.
Adkins RM, Thomas F, Tylavsky FA, et al. Parental ages and levels of DNA methylation in the newborn are correlated. BMC Med Genet. 2011;12:47.
Tominaga K, Pereira-Smith OM. The role of chromatin reorganization in the process of cellular senescence. Curr Drug Targets. 2012;13(13):1593–602.
Nijs M, De Jonge C, Cox A, et al. Correlation between male age, WHO sperm parameters, DNA fragmentation, chromatin packaging and outcome in assisted reproduction technology. Andrologia. 2011;43(3):174–9.
Hassan MA, Killick SR. Effect of male age on fertility: evidence for the decline in male fertility with increasing age. Fertil Steril. 2003;79 Suppl 3:1520–7.
de la Rochebrochard E, Thonneau P. Paternal age and maternal age are risk factors for miscarriage; results of a multicentre European study. Hum Reprod. 2002;17(6):1649–56.
Selvin S, Garfinkel J. Paternal age, maternal age and birth order and the risk of a fetal loss. Hum Biol. 1976;48(1):223–30.
Ford WC, North K, Taylor H, et al. Increasing paternal age is associated with delayed conception in a large population of fertile couples: evidence for declining fecundity in older men. The ALSPAC Study Team (Avon Longitudinal Study of Pregnancy and Childhood). Hum Reprod. 2000;15(8):1703–8.
Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod. 2002;17(5):1399–403.
Olsen J. Subfecundity according to the age of the mother and the father. Dan Med Bull. 1990;37(3):281–2.
Belloc S, Cohen-Bacrie P, Benkhalifa M, et al. Effect of maternal and paternal age on pregnancy and miscarriage rates after intrauterine insemination. Reprod Biomed Online. 2008;17(3):392–7.
Mathieu C, Ecochard R, Bied V, et al. Cumulative conception rate following intrauterine artificial insemination with husband’s spermatozoa: influence of husband’s age. Hum Reprod. 1995;10(5):1090–7.
Bellver J, Garrido N, Remohi J, et al. Influence of paternal age on assisted reproduction outcome. Reprod Biomed Online. 2008;17(5):595–604.
Klonoff-Cohen HS, Natarajan L. The effect of advancing paternal age on pregnancy and live birth rates in couples undergoing in vitro fertilization or gamete intrafallopian transfer. Am J Obstet Gynecol. 2004;191(2):507–14.
de La Rochebrochard E, de Mouzon J, Thepot F, et al. Fathers over 40 and increased failure to conceive: the lessons of in vitro fertilization in France. Fertil Steril. 2006;85(5):1420–4.
Frattarelli JL, Miller KA, Miller BT, et al. Male age negatively impacts embryo development and reproductive outcome in donor oocyte assisted reproductive technology cycles. Fertil Steril. 2008;90(1):97–103.
Whitcomb BW, Turzanski-Fortner R, Richter KS, et al. Contribution of male age to outcomes in assisted reproductive technologies. Fertil Steril. 2011;95(1):147–51.
Risch N, Reich EW, Wishnick MM, et al. Spontaneous mutation and parental age in humans. Am J Hum Genet. 1987;41(2):218–48.
Lim J, Maher GJ, Turner GD, et al. Selfish spermatogonial selection: evidence from an immunohistochemical screen in testes of elderly men. PLoS One. 2012;7(8):e42382.
Moloney DM, Slaney SF, Oldridge M, et al. Exclusive paternal origin of new mutations in Apert syndrome. Nat Genet. 1996;13(1):48–53.
Wilkin DJ, Szabo JK, Cameron R, et al. Mutations in fibroblast growth-factor receptor 3 in sporadic cases of achondroplasia occur exclusively on the paternally derived chromosome. Am J Hum Genet. 1998;63(3):711–6.
Sol-Church K, Stabley DL, Nicholson L, et al. Paternal bias in parental origin of HRAS mutations in Costello syndrome. Hum Mutat. 2006;27(8):736–41.
Tartaglia M, Cordeddu V, Chang H, et al. Paternal germline origin and sex-ratio distortion in transmission of PTPN11 mutations in Noonan syndrome. Am J Hum Genet. 2004;75(3):492–7.
Carlson KM, Bracamontes J, Jackson CE, et al. Parent-of-origin effects in multiple endocrine neoplasia type 2B. Am J Hum Genet. 1994;55(6):1076–82.
Goriely A, Wilkie AO. Paternal age effect mutations and selfish spermatogonial selection: causes and consequences for human disease. Am J Hum Genet. 2012;90(2):175–200.
MacDonald ME, Ambrose CM, Duyao MP, et al. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell. 1993;72(6):971–83.
Duyao M, Ambrose C, Myers R, et al. Trinucleotide repeat length instability and age of onset in Huntington’s disease. Nat Genet. 1993;4(4):387–92.
Goldberg YP, Kremer B, Andrew SE, et al. Molecular analysis of new mutations for Huntington’s disease: intermediate alleles and sex of origin effects. Nat Genet. 1993;5(2):174–9.
Brunner HG, Bruggenwirth HT, Nillesen W, et al. Influence of sex of the transmitting parent as well as of parental allele size on the CTG expansion in myotonic dystrophy (DM). Am J Hum Genet. 1993;53(5):1016–23.
Zheng CJ, Byers B, Moolgavkar SH. Allelic instability in mitosis: a unified model for dominant disorders. Proc Natl Acad Sci USA. 1993;90(21):10178–82.
Fisch H, Hyun G, Golden R, et al. The influence of paternal age on down syndrome. J Urol. 2003;169(6):2275–8.
Zaragoza MV, Jacobs PA, James RS, et al. Nondisjunction of human acrocentric chromosomes: studies of 432 trisomic fetuses and liveborns. Hum Genet. 1994;94(4):411–7.
Sloter E, Nath J, Eskenazi B, et al. Effects of male age on the frequencies of germinal and heritable chromosomal abnormalities in humans and rodents. Fertil Steril. 2004;81(4):925–43.
Fonseka KG, Griffin DK. Is there a paternal age effect for aneuploidy? Cytogenet Genome Res. 2011;133(2–4):280–91.
De Souza E, Morris JK. Case–control analysis of paternal age and trisomic anomalies. Arch Dis Child. 2010;95(11):893–7.
Zhu JL, Madsen KM, Vestergaard M, et al. Paternal age and congenital malformations. Hum Reprod. 2005;20(11):3173–7.
De Souza E, Alberman E, Morris JK. Down syndrome and paternal age, a new analysis of case–control data collected in the 1960s. Am J Med Genet A. 2009;149A(6):1205–8.
Oksuzyan S, Crespi CM, Cockburn M, et al. Birth weight and other perinatal characteristics and childhood leukemia in California. Cancer Epidemiol. 2012;36(6):e359–65.
Murray L, McCarron P, Bailie K, et al. Association of early life factors and acute lymphoblastic leukaemia in childhood: historical cohort study. Br J Cancer. 2002;86(3):356–61.
Hemminki K, Kyyronen P, Vaittinen P. Parental age as a risk factor of childhood leukemia and brain cancer in offspring. Epidemiology. 1999;10(3):271–5.
Yip BH, Pawitan Y, Czene K. Parental age and risk of childhood cancers: a population-based cohort study from Sweden. Int J Epidemiol. 2006;35(6):1495–503.
Choi JY, Lee KM, Park SK, et al. Association of paternal age at birth and the risk of breast cancer in offspring: a case control study. BMC Cancer. 2005;5:143.
Zhang Y, Kreger BE, Dorgan JF, et al. Parental age at child’s birth and son’s risk of prostate cancer. The Framingham Study. Am J Epidemiol. 1999;150(11):1208–12.
Hare EH, Moran PA. Raised parental age in psychiatric patients: evidence for the constitutional hypothesis. Br J Psychiatry. 1979;134:169–77.
Miller B, Messias E, Miettunen J, et al. Meta-analysis of paternal age and schizophrenia risk in male versus female offspring. Schizophr Bull. 2011;37(5):1039–47.
Matheson SL, Shepherd AM, Laurens KR, et al. A systematic meta-review grading the evidence for non-genetic risk factors and putative antecedents of schizophrenia. Schizophr Res. 2011;133(1–3):133–42.
Wohl M, Gorwood P. Paternal ages below or above 35 years old are associated with a different risk of schizophrenia in the offspring. Eur Psychiatry. 2007;22(1):22–6.
Gardener H, Spiegelman D, Buka SL. Prenatal risk factors for autism: comprehensive meta-analysis. Br J Psychiatry. 2009;195(1):7–14.
Hultman CM, Sandin S, Levine SZ, et al. Advancing paternal age and risk of autism: new evidence from a population-based study and a meta-analysis of epidemiological studies. Mol Psychiatry. 2011;16(12):1203–12.
Frans EM, Sandin S, Reichenberg A, et al. Advancing paternal age and bipolar disorder. Arch Gen Psychiatry. 2008;65(9):1034–40.
Menezes PR, Lewis G, Rasmussen F, et al. Paternal and maternal ages at conception and risk of bipolar affective disorder in their offspring. Psychol Med. 2010;40(3):477–85.
Kuja-Halkola R, Pawitan Y, D’Onofrio BM, et al. Advancing paternal age and offspring violent offending: a sibling-comparison study. Dev Psychopathol. 2012;24(3):739–53.
Saha S, Barnett AG, Buka SL, et al. Maternal age and paternal age are associated with distinct childhood behavioural outcomes in a general population birth cohort. Schizophr Res. 2009;115(2–3):130–5.
Malaspina D, Reichenberg A, Weiser M, et al. Paternal age and intelligence: implications for age-related genomic changes in male germ cells. Psychiatr Genet. 2005;15(2):117–25.
Saha S, Barnett AG, Foldi C, et al. Advanced paternal age is associated with impaired neurocognitive outcomes during infancy and childhood. PLoS Med. 2009;6(3):e40.
Svensson AC, Abel K, Dalman C, et al. Implications of advancing paternal age: does it affect offspring school performance? PLoS One. 2011;6(9):e24771.
Reichenberg A, Gross R, Weiser M, et al. Advancing paternal age and autism. Arch Gen Psychiatry. 2006;63(9):1026–32.
Hehir-Kwa JY, Rodriguez-Santiago B, Vissers LE, et al. De novo copy number variants associated with intellectual disability have a paternal origin and age bias. J Med Genet. 2011;48(11):776–8.
Perrin MC, Brown AS, Malaspina D. Aberrant epigenetic regulation could explain the relationship of paternal age to schizophrenia. Schizophr Bull. 2007;33(6):1270–3.
Zribi N, Feki Chakroun N, El Euch H, et al. Effects of cryopreservation on human sperm deoxyribonucleic acid integrity. Fertil Steril. 2010;93(1):159–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Jenkins, T.G., Aston, K.I., Carrell, D.T. (2013). The Aging Male and Impact on Offspring. In: Schlegel, P., Fauser, B., Carrell, D., Racowsky, C. (eds) Biennial Review of Infertility. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7187-5_3
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7187-5_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7186-8
Online ISBN: 978-1-4614-7187-5
eBook Packages: MedicineMedicine (R0)