Abstract
This chapter is devoted to resistance to antiepileptic drugs (AEDs) and its genetic mechanisms. There are three general hypothesis proposed for pharmacoresistant epilepsy: (1) Target hypothesis, (2) Drug transporter hypothesis, and the (3) Intrinsic Severity Hypothesis (Gorter and Potschka, Jasper’s basic mechanisms of the epilepsies, 4th ed. National Center for Biotechnology Information (USA), Bethesda, MD, 2012).
In diagnosing poor response to treatment, it is also important to separate drug resistance from incorrect diagnosis of epilepsy syndrome for example: (a) Epilepsy caused by mutations in Glucose transporter gene 1 (GLUT1) being treated with valproate (VPA) worsens the seizures in this disease whereas replacement of glucose with ketogenic diet alleviates seizures and the glucose deficit in the central nervous system. (Klepper, Epilepsia 49(Suppl 8):46–49, 2008; Klepper et al., Neuropediatrics 40(5):207–210, 2009) (b) Genetic or idiopathic epilepsies such as Childhood Absence Epilepsy (CAE), Juvenile Myoclonic Epilepsy (JME) and Dravet’s Syndrome can be aggravated when treated with Na+ channel blockers (Genton, Brain Dev 22(2):75–80, 2000; Guerrini et al., Epilepsia 39(5):508–512, 1998; Thomas et al., Brain 129(Pt 5):1281–1292, 2006; Martínez-Juárez et al., Brain 129(Pt 5):1269–1280, 2006) and (c) Mitochondrial disorders can also be aggravated by VPA (Finsterer and Zarrouk Mahjoub, Expert Opin Drug Metab Toxicol 8(1):71–79, 2012).
Herein, we describe the three general hypothesis; we also summarize the “difficult to treat” genetic epilepsies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Target Hypothesis
A drug must have one or more actions on target sites of the brain to exert its therapeutic action. The resistance to drugs is caused by a structural or functional change at the site of action of drugs causing change in the pharmacodynamics of the drug (Sanchez-Alvarez et al. 2007).
The molecular targets refer to the sites that act as ligands of AEDs by which they exert their mechanism of action. These groups of molecules can be divided into two: voltage-gated channels and neurotransmitter receptors associated with neuronal excitation. These alterations at the site of action may be genetically determined or developed as a result of epigenetic and exogenous environmental factors.
2.1.1 Alterations of Sodium (Na+) Channels
Sodium channels are the main target of most AEDs, which act by blocking their resting phase (tonic block), preventing channel opening and Na+ conductance selectively. It has been suggested that mutations in Na+ channels may affect the clinical response to AEDs (Ragsdale and Avoli 1998).
The Na+ channels are formed by a pore-forming α subunit and two auxiliary associated subunits β. The modification of any of its subunits may play an important role in drug resistance (Sanchez-Alvarez et al. 2007).
The target theory was based on studies in voltage-regulated Na+ channel in hippocampal neurons with the use of carbamazepine (CBZ). Most antiepileptic drugs act blocking Na+ channels in their resting phase (tonic block), which prevents channel opening and ion conductance. It is considered that this alteration may be genetic or acquired. An alteration in the Na+ channel can modify the sensitivity to one particular drug, but does not necessarily modify all responses to all drugs that share the same mechanism of action in the Na+ channel.
In genetic drug resistance, it is known that some mutations in genes encoding VGSC subunits may cause refractory or drug-resistant epilepsy (Claes et al. 2001). The SCN1A gene is located on chromosome 2q24.3; it has been linked to several diseases, including severe myoclonic epilepsy of infancy or Dravet Syndrome and Generalized Epilepsy with Febrile Seizure Plus (GEFS+). SCNA1 gene encodes for the α subunit of the VGSC; however, an exact physiological basis of drug resistance related to structural alterations of the subunit of VGSC in Dravet Syndrome has not been demonstrated.
In the SCN1A gene, exon 5 encodes for one of the four voltage sensitive channel, the I-S4 domain. This has two versions, one neonatal (N) and another adult (A), which differ in three amino acids. Normally both exons are coexpressed in the adult brain. In studies by Tate et al. (Tate et al. 2005), a G to A polymorphism was identified in the SCN1A gene that affects the alternative splicing of exon 5. This polymorphism has been observed in the intron adjacent to exon 5. Apparently this region determines which sequence, either neonatal or adult, is incorporated into each channel. Ancestral allele G allows both exons to be expressed, whereas the mutant allele alters the expression of neonatal exon by interrupting the consensus sequence, reducing the expression of this exon relative to exon 5A. By studying the minimum dose required of two AEDs, namely, CBZ and phenytoin (PHT) prescribed in 706 patients, Tate et al. (2006) found that AA homozygotes had an average dose of CBZ and PHT higher than that of heterozygotes, and the latter also had higher dose than GG homozygotes. A second study by the same authors failed to report this association; therefore, more studies are needed to confirm this (Tate et al. 2006).
An association between polymorphisms of the SCN2A gene channel, which codes for the α2 subunit of neuronal Na+ channel, and resistance to drugs acting on Na+ channels has also been found (Kwan et al. 2008).
The β subunits function is to modulate the membrane expression of the Na+ channel. A mutation in the gene encoding for the β1 subunit has been linked with GEFS+. In epilepsy animal models a decreased expression of β1 and β2 subunit has been found. However, this lack of effect of CBZ on Na+ channels in kindled rats is transient, and the inhibitory effect of CBZ on Na+ channels is recovered. This effect has not been described in vivo (Gastaldi et al. 1998; Ellerkmann et al. 2003).
In acquired drug resistance, exogenous factors such as the presence of repeated seizures can promote transcriptional or post-transcriptional changes capable of inducing structural changes in VGSC, changes that are enough to induce refractory or drug-resistant epilepsy (Beck 2007). Remy et al. (2003) observed in brain tissue, from patients undergoing surgery for temporal lobe epilepsy with hippocampal sclerosis, a tonic loss of VGSC blockade, in contrast to the CBZ sensitive patient tissue samples.
2.1.2 Alterations of Voltage-Dependent Calcium (Ca+) Channels
The Ca+ channels are voltage transmembrane ion channels with an excitatory function. There are at least six types of Ca+ channels (T, L, N, P/Q, R) classified in two categories on the basis of the voltage necessary for activation: low threshold and high threshold. The T-type channel is the only low-threshold Ca2+ channel current described (Shin et al. 2008).
Each VGCC is formed by an α1 subunit which serves as main pore and sensor in potential change, which is encoded by ten distinct genes, and several accessory subunits identified as β, γ, and α2δ subunits. The VGCC has a highly functional heterogeneity as a result of its wide distribution.
The T-type calcium channels are involved in generating thalamocortical discharges, involved in the pathophysiology of absence seizures. The α1G subunit of T-type calcium channels is related to the generation of spike and wave discharges, while the α1 subunit does not have this physiological property. Therefore, it is possible that an imbalance in the proportion of α1 and α1G subunits in the T Ca+ channel reduces the response to anti-absence AEDs such as ethosuximide (ESM), lamotrigine (LTG), VPA, and zonisamide (ZNS). However, there is not experimental evidence yet to confirm this hypothesis (Chioza et al. 2001).
2.1.3 Alterations of Gamma Aminobutyric Acid Channels
Gamma Aminobutyric Acid (GABA) is the major inhibitory neurotransmitter in the adult brain. There are two GABA receptors: GABAA and GABAB. The GABAA receptor has specific binding sites for benzodiazepines and barbiturates. GABAA channels mediate most inhibitory neurotransmission in the brain. Most GABAA channels are assembled by seven different subfamilies, which are defined by similar sequences: α, β, γ, δ, π, θ, and ρ. Most of the GABAA channels are formed by α, β and γ subunits. The 60 % of GABAA subunits are assembled by α1β2γ2 subunits. The GABAA receptor subtypes are distinguished by their affinity for GABA, channel kinetics and the rate of desensitization, distribution and pharmacology. Changes in the composition of the channel may have implications on its role and sensitivity to AEDs, especially of benzodiazepines (Schmidt and Lösher 2005).
In some animal models of chronic epilepsy there has been a progressive decrease in GABA receptor response to benzodiazepines. In these models hippocampal neuronal loss has been observed and has been associated with recurrent seizures with the subsequent development of acquired resistance, secondary to altered GABAA receptor. Combined molecular and functional studies indicate that the transcriptional change occurs in the α subunit of the GABAA receptor, consistent with a decrease in the α1 subunit expression and an increase in the α4 (Brooks-Kayal et al. 1998).
2.2 Multidrug Transporter Hypothesis (See Fig. 2.1)
The multidrug transporter hypothesis is based on the modification of the drug pharmacokinetics causing an inadequate concentration of antiepileptic drugs in brain tissue. This phenomenon occurs by an increase in cell membrane proteins which expel the endogenous toxins and xenobiotics, thus preventing penetration the blood–brain barrier and a decreased concentration of the medications at the epileptogenic focus or zones.
Drug resistance that occurs as a result of an increase in membrane proteins has become evident in several diseases such as cancer and epilepsy. Now it is considered a major cause of treatment failure. Resistance may be evident from the start of therapy or after an adequate initial response. There may even be cross-resistance to several drugs as a result of overexpression of membrane transport proteins. This phenomenon is called multidrug resistance (MDR).
These proteins are expressed at the luminal surface of cells that form the blood–brain barrier, glial and endothelial cells, and neurons, thus acting as a “second barrier”. This would explain why, despite the use of AEDs at maximum doses, these are not effective in patients with refractory or drug-resistant epilepsy (Dombrowski et al. 2001).
2.2.1 ABC Superfamily (ATP-Binding Cassette Transporters)
The ABC proteins are associated with multiple drug resistance. These are members of an energy-dependent protein superfamily. Several members of the superfamily have been identified and classified into seven subfamilies (ABCA, ABCB, ABCC, ABCD, ABCE, ABCF, and ABCG). Among these, the subfamilies ABCB, ABCC, and ABCG are involved in MDR.
The ABCB1 (MDR1) and its protein, P-glycoprotein (P-gp) were the first ones to be described and are the most studied among those associated with resistance to multiple drugs. The MDR1 gene is located on chromosome 7q21.1. The P-gp is a membrane protein with 1,280 amino acids and sized/weighing 170 kDa. It is found in different tissues with excretory or secretory function, such as liver, pancreas, kidney, intestine, and others. Substances that interact with P-gp are very diverse and have great ability to cross plasma barriers for their characteristics: high molecular weight, positive charge, and high lipophilicity (Kwan and Brodie 2005).
Tishler et al. (1995) suggested that the poor response to AED treatment in patients with refractory epilepsy was secondary to a reduction in the penetration of the drugs to the central nervous system. They observed an increased expression of MDR1 mRNA in 11 of 19 brain tissue of patients undergoing surgery with an increase in P-gp immunostaining. The concentration of PHT in cells was reduced to ¼ in patients expressing MDR1 in contrast to those that did not express it.
The variable expression of P-gp suggests a genetic influence, environmental factors or both. MDR1 gene is highly polymorphic. More than 50 single nucleotide polymorphism (SNP) along with insertion/deletion polymorphisms have been reported in the MDR1 (ABCB1) gene that encodes P-gp. Environmental factors could cause the expression of MDR1 in tissues where it was not previously found; this could explain the fact that symptomatic epilepsies are more resistant to AEDs than idiopathic or genetic epilepsies (Kwan and Brodie 2000, 2005).
An increased expression of multidrug transporters has also been associated with constitutive, genetic or hereditary mechanism. Increased expression of MDR1 was demonstrated in endothelial cells of the blood–brain barrier up to 130 % in patients with epilepsy, MRP5 was increased up to 180 % and MDR2 up to 225 % in comparison to patients without epilepsy (Dombrowski et al. 2001). Siddiqui et al. (2003) reported an association between drug resistance in epilepsy and a polymorphism in the ABCB1 gene. They reported that patients with the CC genotype expressed more P-gp, which was associated with increased drug resistance versus patients with the TT genotype. However, this association has been poorly reproduced and other studies have even documented an inverse association (Tan et al. 2004; Sills et al. 2005).
The association of drug-resistant or refractory epilepsy and some specific etiologies, including mesial temporal sclerosis, cortical dysplasias, and glial tumors has been known now for some time (Semah and Ryvlin 2005). Overexpression of multidrug resistance protein is regionally selective areas, affecting mainly epileptic brain areas. Overexpression of MRP1 and MDR1 was demonstrated in perivascular astrocytes of patients with temporal lobe epilepsy due to hippocampal sclerosis. An aberrant expression in neurons and glial cells was observed as well in patients with dysembryoplastic neuroepithelial tumors and malformation of cortical development (Sisodiya et al. 2002; Sanchez-Alvarez et al. 2007).
It has been proposed that sustained augmentation of glutamate secondary to seizures is the mechanism of acquired increased P-gp expression in cells of the blood–brain barrier. Glutamate acts through NMDA-R, which produces the signal for arachidonic acid, which is then oxidized by the cyclooxygenase 2 (COX-2) producing prostanoids, including prostaglandin E2 (PGE2). PGE2 acts on the Prostaglandin E receptor 1 (EP1-R), which by means of a second messenger system increases transcription of P-gp (Potschka 2012).
Among the drugs transported by P-gp are CBZ, felbamate (FBM), gabapentin (GBP), LTG, phenobarbital (PB), PHT, and topiramate (TPM). Levetiracetam (LVT) and benzodiazepines are not substrates of P-gp in the blood–brain barrier. Kwan et al. (2010) reported a negative relationship between seizure control after epilepsy surgery and P-gp expression on the resected tissue of patients. Various antiepileptic drugs, their mechanisms of action and their corresponding transporters are shown on Table 2.1.
2.3 Intrinsic Severity Hypothesis
A prognostic factor associated with drug-resistant epilepsy is the frequency of seizures at the beginning of the disease, in some cases associated with the number of seizures before the start of treatment (Kwan and Brodie 2000). Even some cases of drug-resistant epilepsies had prolonged episodes of remission in its initial phases. The intrinsic severity hypothesis implies that the frequency of seizures is associated with refractoriness: if seizures are easy to trigger, then seizures will be more difficult to suppress, and the usual dose of the drug will not be enough. There is as yet no evidence that genetic factors directly contribute to the severity of epilepsy in idiopathic (genetic generalized epilepsies, Rogawski and Johnson 2008).
2.4 Genetic Epilepsies “Difficult to Treat”
Pathogenic alterations or mutation in genes and structural abnormalities in chromosomes (deletions, insertions) are responsible of a variety of epilepsies. In some, the possibility of drug-resistant epilepsy is high.
Several mechanisms may be interrelated between genetic disorders and the presence of epilepsy. It is important to distinguish between the susceptibility to generate epilepsy caused by a functional abnormality of a gene, and epilepsy that results from structural or functional abnormalities in a chromosome. Some genetic disorders relate more to certain types of epilepsy but overall any seizure type may be present.
Table 2.2 summarizes some genetic pharmacoresistant epilepsies.
(a)EFHC1/Myoclonin mutations in Juvenile Myoclonic Epilepsy (JME) frequently respond to treatment with valproate (VPA), however other JME mutations (illustrated as: Myoclonin 2 and Myoclonin 3) might not achieve seizure control due to a different molecular lesion unresponsive to VPA therapy. (b) EFHC1/Myoclonin mutations in a susceptibility or early stage respond adequately to VPA treatment whereas in established epileptogenesis drug resistance is seen even though the same molecular lesion is present; therefore a true genetic pharmacorresistance is encountered
2.5 Conclusions
2.5.1 Limitations of the Three Hypothesis
To prove a given drug resistance theory, it is important to show that the subgroup of patients with drug resistance has differences in their receptors in comparison to those of responders. However, this is difficult to achieve because patients who respond to drugs are not subjected to epilepsy surgery. Any proposed mechanism for drug resistance must meet the following requirements to be considered valid: be detectable in epileptic brain tissue, have a pathophysiological mechanism, demonstrable in human epilepsy and, when modified, must affect the phenomenon of drug resistance (Sisodiya 2003).
The fact that most patients are resistant to multiple treatments, including several AEDs with different mechanisms of action, suggests that other less specific or unknown mechanisms with some commonality about AED cellular or network actions contribute to drug resistance or that more than one mechanism may be involved (Löscher et al. 2006). Some changes were induced only transiently in animal models of epilepsy which do not necessarily explain chronic pharmacorresistance (Van Vliet et al. 2005; Löscher 2007).
According to Schmidt and Löscher, (2009) the intrinsic hypothesis lacks studies and “a subgroup of patients with a higher seizure frequency at the onset of treatment will become seizure-free but require higher serum concentrations of AEDs to do so than those with a lower seizure frequency”.
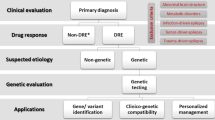
2.5.2 How to Define Genetic Drug-Resistant Epilepsies?
We have collected over a thousand patients with CAE, JME and CAE evolving to JME, Lafora disease, GEFS+, and Angelman Syndrome. These epilepsies respond variably to AED therapy, depending on their molecular lesion.
This chapter leads us to the question—what is the definition of genetic “drug-resistant” epilepsies. In the end we propose two assertions: (1) epilepsies are drug-resistant because the AED does not have an effect on the specific molecular lesion of the epilepsy syndrome. The epilepsy is supposedly “drug resistant” but seizures do not stop because “the key does not fit the lock in the door” and (2) when the AED has a proven effect on the molecular lesion but seizures persist in spite of AED treatment; this latter, we believe is true genetic pharmacorresistant epilepsy. Therefore, we favor the “intrinsic disease” mechanisms as an explanation for the resistance in genetic epilepsies (Fig. 2.2).
2.5.3 Future Directions
The question is how to attack the problem in patients. A recommended step now, in assessing AED use, is to genotype epilepsies and use the genotype to guide AED use.
It would be ideal to perform a whole or large scale pharmacogenomic study of how AEDs effects are genetically determined in order to look for responders and non-responders and also for patients that will develop side effects from a specific AED. A large-scale pharmacogenomic studies could also be done in patients who were submitted to surgery for drug-resistant epilepsy. We could study the surgical specimens for their neuropathologic and biochemical abnormalities and correlate the findings with whole genome sequencing.
References
Angelman H. Puppet children: a report on three cases. Dev Med Child Neurol 1965;7:681–8.
Beck H. Plasticity of antiepileptic drug targets. Epilepsia. 2007;48 Suppl 1:14–8.
Brooks-Kayal AR, Shumate MD, Jin H, Rikhter TY, Coulter DA. Selective changes in single cell GABA(A) receptor subunit expression and function in temporal lobe epilepsy. Nat Med. 1998;4(10):1166–72.
Canevini MP, Sgro V, Zuffardi O, Canger R, Carrozzo R, Rossi E, et al. Chromosome 20 ring: a chromosomal disorder associated with a particular electroclinical pattern. Epilepsia. 1998;39(9):942–51.
Cassidy SB, Thuline HC, Holm VA. Deletion of chromosome 15 (q11-13) in a Prader-Labhart-Willi syndrome clinic population. Am J Med Genet. 1984;17(2):485–95.
Chan EM, Young EJ, Ianzano L, Munteanu I, Zhao X, Christopoulos CC, et al. Mutations in NHLRC1 cause progressive myoclonus epilepsy. Nat Genet. 2003;35(2):125–7.
Chioza B, Wilkie H, Nashef L, Blower J, McCormick D, Sham P, et al. Association between the alpha(1a) calcium channel gene CACNA1A and idiopathic generalized epilepsy. Neurology. 2001;56(9):1245–6.
Claes L, Del-Favero J, Ceulemans B, Lagae L, Van Broeckhoven C, De Jonghe P. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. Am J Hum Genet. 2001;68(6):1327–32.
Dobyns WB, Reiner O, Carrozzo R, Ledbetter DH. Lissencephaly. A human brain malformation associated with deletion of the LIS1 gene located at chromosome 17p13. JAMA. 1993;270(23):2838–42.
Dombrowski SM, Desai SY, Marroni M, Cucullo L, Goodrich K, Bingaman W, et al. Overexpression of multiple drug resistance genes in endothelial cells from patients with refractory epilepsy. Epilepsia. 2001;42(12):1501–6.
Dravet C. - Vie Med. Les epilepsies graves de l'enfant. 1978. - 543–548: Vol.8.
Ellerkmann RK, Remy S, Chen J, Sochivko D, Elger CE, Urban BW, et al. Molecular and functional changes in voltage-dependent Na(+) channels following pilocarpine-induced status epilepticus in rat dentate granule cells. Neuroscience. 2003;119(2):323–33.
Finsterer J, Zarrouk MS. Mitochondrial toxicity of antiepileptic drugs and their tolerability in mitochondrial disorders. Expert Opin Drug Metab Toxicol. 2012;8(1):71–9.
Fu YH, Kuhl DP, Pizzuti A, Pieretti M, Sutcliffe JS, Richards S, et al. Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell. 1991;67(6):1047–58.
Ganesh S, Delgado-Escueta AV, Sakamoto T, Avila MR, Machado-Salas J, Hoshii Y, et al. Targeted disruption of the Epm2a gene causes formation of Lafora inclusion bodies, neurodegeneration, ataxia, myoclonus epilepsy and impaired behavioral response in mice. Hum Mol Genet. 2002a;11(11):1251–62.
Ganesh S, Delgado-Escueta AV, Suzuki T, Francheschetti S, Riggio C, Avanzini G, et al. Genotype-phenotype correlations for EPM2A mutations in Lafora’s progressive myoclonus epilepsy: exon 1 mutations associate with an early-onset cognitive deficit subphenotype. Hum Mol Genet. 2002b;11(11):1263–71.
Gastaldi M, Robaglia-Schlupp A, Massacrier A, Planells R, Cau P. mRNA coding for voltage-gated sodium channel beta2 subunit in rat central nervous system: cellular distribution and changes following kainate-induced seizures. Neurosci Lett. 1998;249(1):53–6.
Genton P. When antiepileptic drugs aggravate epilepsy. Brain Dev. 2000;22(2):75–80.
Gorter JA, Potschka H. Drug Resistance in Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV editors. Jasper's Basic Mechanisms of the Epilepsies. 4th edition. Bethesda (MD): National Center for Biotechnology Information (US); 2012.
Guerrini R, Dravet C, Genton P, Belmonte A, Kaminska A, Dulac O. Lamotrigine and seizure aggravation in severe myoclonic epilepsy. Epilepsia. 1998;39(5):508–12.
Harkin LA, McMahon JM, Iona X, Dibbens L, Pelekanos JT, Zuberi SM, et al. Infantile Epileptic Encephalopathy Referral Consortium, Sutherland G, Berkovic SF, Mulley JC, Scheffer IE. The spectrum of SCN1A-related infantile epileptic encephalopathies. Brain. 2007;130(Pt 3):843–52.
Jq M. Lissencephaly in 2 siblings. Neurology. 1963;13:841–50.
Klepper J. Glucose transporter deficiency syndrome (GLUT1DS) and the ketogenic diet. Epilepsia. 2008;49 Suppl 8:46–9.
Klepper J, Voit T. Facilitated glucose transporter protein type 1 (GLUT1) deficiency syndrome: impaired glucose transport into brain– a review. Eur J Pediatr. 2002;161(6):295–304.
Klepper J, Scheffer H, Elsaid MF, Kamsteeg EJ, Leferink M, Ben-Omran T. Autosomal recessive inheritance of GLUT1 deficiency syndrome. Neuropediatrics. 2009;40(5):207–10.
Kubota H, Ishihara H, Langmann T, Schmitz G, Stieger B, Wieser HG, et al. Distribution and functional activity of P-glycoprotein and multidrug resistance associated proteins in human brain microvascular endothelial cells in hippocampal sclerosis. Epilepsy Res. 2006;68(3):213–28.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342(5):314–9.
Kwan P, Brodie MJ. Potential role of drug transporters in the pathogenesis of medically intractable epilepsy. Epilepsia. 2005;46(2):224–35.
Kwan P, Poon WS, Ng HK, Kang DE, Wong V, Ng PW, et al. Multidrug resistance in epilepsy and polymorphisms in the voltage-gated sodium channel genes SCN1A, SCN2A, and SCN3A: correlation among phenotype, genotype, and mRNA expression. Pharmacogenet Genomics. 2008;18(11):989–98.
Kwan P, Li HM, Al-Jufairi E, Abdulla R, Gonzales M, Kaye AH, et al. Association between temporal lobe P-glycoprotein expression and seizure recurrence after surgery for pharmacoresistant temporal lobe epilepsy. Neurobiol Dis. 2010;39(2):192–7.
Löscher W. Drug transporters in the epileptic brain. Epilepsia. 2007;48 Suppl 1:8–13.
Löscher W, Poulter MO, Padjen AL. Major targets and mechanisms of antiepileptic drugs and major reasons for failure. Adv Neurol. 2006;97:417–27.
Martínez-Juárez IE, Alonso ME, Medina MT, Durón RM, Bailey JN, López-Ruiz M, et al. Juvenile myoclonic epilepsy subsyndromes: family studies and long-term follow-up. Brain. 2006;129(Pt 5):1269–80.
Minassian BA, DeLorey TM, Olsen RW, Philippart M, Bronstein Y, Zhang Q, et al. Angelmansyndrome: correlations between epilepsy phenotypes and genotypes. Ann Neurol. 1998;43(4):485–93.
Ohmori I, Ouchida M, Ohtsuka Y, Oka E, Shimizu K. Significant correlation of the SCN1A mutations and severe myoclonic epilepsy in infancy. Biochem Biophys Res Commun. 2002;295(1):17–23.
Potschka H. Role of CNS efflux drug transporters in antiepileptic drug delivery: overcoming CNS efflux drug transport. Adv Drug Deliv Rev. 2012;64(10):943–52.
Povey S, Burley MW, Attwood J, Benham F, Hunt D, Jeremiah SJ, et al. Two loci for tuberous sclerosis: one on 9q34 and one on 16p13. Ann Hum Genet. 1994;58(Pt 2):107–27.
Ragsdale DS, Avoli M. Sodium channels as molecular targets for antiepileptic drugs. Brain Res Brain Res Rev. 1998;26(1):16–28.
Remy S, Beck H. Molecular and cellular mechanisms of pharmacoresistance in epilepsy. Brain. 2006;129(Pt 1):18–35.
Remy S, Gabriel S, Urban BW, Dietrich D, Lehmann TN, Elger CE, et al. A novel mechanism underlying drug resistance in chronic epilepsy. Ann Neurol. 2003;53(4):469–79.
Rogawski MA, Johnson MR. Intrinsic severity as a determinant of antiepileptic drug refractoriness. Epilepsy Curr. 2008;8(5):127–30.
Sánchez Alvarez JC, Serrano Castro PJ, Serratosa Fernández JM. Clinical implications of mechanisms of resistance to antiepileptic drugs. Neurologist. 2007;13(6 Suppl 1):S38–46.
Schmidt D, Löscher W. Drug resistance in epilepsy: putative neurobiologic and clinical mechanisms. Epilepsia. 2005;46(6):858–77.
Schmidt D, Löscher W. New developments in antiepileptic drug resistance: an integrative view. Epilepsy Curr. 2009;9(2):47–52.
Semah F, Ryvlin P. Can we predict refractory epilepsy at the time of diagnosis? Epileptic Disord. 2005;7 Suppl 1:S10–3.
Shahwan A, Farrell M, Delanty N. Progressive myoclonic epilepsies: a review of genetic and therapeutic aspects. Lancet Neurol. 2005;4(4):239–48.
Shin HS, Cheong EJ, Choi S, Lee J, Na HS. T-type Ca2+ channels as therapeutic targets in the nervous system. Curr Opin Pharmacol. 2008;8(1):33–41.
Siddiqui A, Kerb R, Weale ME, Brinkmann U, Smith A, Goldstein DB, et al. Association of multidrug resistance in epilepsy with a polymorphism on the drug-transporter GEBE ABCB1. N Engl J Med. 2003;348(15):1442–8.
Sills GJ, Mohanraj R, Butler E, McCrindle S, Collier L, Wilson EA, et al. Lack of association between the C3435T polymorphism in the human multidrug resistance (MDR1) gene and response to antiepileptic drug treatment. Epilepsia. 2005;46(5):643–7.
Singh R, Andermann E, Whitehouse WP, Harvey AS, Keene DL, Seni MH, Crossland KM, Andermann F, Berkovic SF, Scheffer IE. Severe myoclonic epilepsy of infancy: extended spectrum of GEFS+? Epilepsia. 2001;42:837–44.
Sisodiya SM. Mechanisms of antiepileptic drug resistance. Curr Opin Neurol. 2003;16(2):197–201.
Sisodiya SM, Lin WR, Harding BN, Squier MV, Thom M. Drug resistance in epilepsy: expression of drug resistance proteins in common causes of refractory epilepsy. Brain. 2002;125(Pt 1):22–31.
Tan NC, Heron SE, Scheffer IE, Pelekanos JT, McMahon JM, Vears DF, et al. Failure to confirm association of a polymorphism in ABCB1 with multidrug-resistant epilepsy. Neurology. 2004;63(6):1090–2.
Tate SK, Depondt C, Sisodiya SM, Cavalleri GL, Schorge S, Soranzo N, et al. Genetic predictors of the maximum doses patients receive during clinical use of the anti-epileptic drugs carbamazepine and phenytoin. Proc Natl Acad Sci U S A. 2005;102(15):5507–12.
Tate SK, Singh R, Hung CC, Tai JJ, Depondt C, Cavalleri GL, et al. A common polymorphism in the SCN1A gene associates with phenytoin serum levels at maintenance dose. Pharmacogenet Genomics. 2006;16(10):721–6.
Thomas P, Valton L, Genton P. Absence and myoclonic status epilepticus precipitated by antiepileptic drugs in idiopathic generalized epilepsy. Brain. 2006;129(Pt 5):1281–92.
Tishler DM, Weinberg KI, Hinton DR, Barbaro N, Annett GM, Raffel C. MDR1 gene expression in brain of patients with medically intractable epilepsy. Epilepsia. 1995;36(1):1–6.
van Vliet EA, Redeker S, Aronica E, Edelbroek PM, Gorter JA. Expression of multidrug transporters MRP1, MRP2, and BCRP shortly after status epilepticus, during the latent period, and in chronic epileptic rats. Epilepsia. 2005;46(10):1569–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Martínez-Juárez, I.E., Hernández-Vanegas, L.E., Rodríguez y Rodríguez, N., León-Aldana, J.A., Delgado-Escueta, A.V. (2013). Genes Involved in Pharmacoresistant Epilepsy. In: Rocha, L., Cavalheiro, E. (eds) Pharmacoresistance in Epilepsy. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6464-8_2
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6464-8_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6463-1
Online ISBN: 978-1-4614-6464-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)