Abstract
This chapter is devoted to drug-resistant epilepsy and its genetic mechanisms. There are currently six hypotheses proposed for pharmacoresistant epilepsy. The genetic aspects of five of the six hypotheses are addressed in this chapter except from the intrinsic hypothesis as it does not comprise genetic mechanisms.
In the end, we propose two assertions in the definition of genetic “drug-resistant” epilepsies: (1) when the antiseizure medication (ASM) has a proven effect on the molecular lesion, but seizures persist in spite of ASM treatment; this latter, we believe is true genetic pharmacorresistant epilepsy and (2) epilepsies are drug resistant because the antiseizure drug ASM does not have an effect on the specific molecular lesion of the epilepsy syndrome. The epilepsy is supposedly “drug resistant,” but seizures do not stop because “the key does not fit the lock in the door”.
In diagnosis poor response to treatment, it is also important to consider that incorrect diagnosis in some epilepsies can also lead to “pseudo-drug resistance,” where mistreatment can lead to poor response or aggravation of seizures, this happens more frequently in genetic epilepsies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
17.1 Genetics of Target Hypothesis
Target hypothesis consists in the lack of response or decreased sensitivity to the medication, as seizure control is not achieved, further changes occur in the structure and/or function of the ASM target, this leads to greater drug resistance in epilepsy (Juvale and Che Has 2021).
It is suggested that altered gene expression due to epigenetic regulation and/or the formation of receptor mosaics because of exogenous environmental factors such as the high frequency of seizures, may cause transcriptional or posttranscriptional changes with the consequent structural alterations that cause decrease effectiveness in various targets (Łukawski and Czuczwar 2021).
Despite target ineffectiveness, it is still crucial to use different therapeutic targets in patients with DRE, although it is still not possible to understand why people with drug resistance do not respond to the use of several drugs with different mechanisms of action that would try to compensate for these differences.
This theory involves voltage-gated ion channels and receptors of neurotransmitters and/or enzymes.
17.1.1 Genetic Variants of Voltage-Gated Ion Channels
Channels are essential in the generation and propagation of action potentials, therefore loss or gain-of-function mutations related to channel inactivation are relevant (Shlobin and Sander 2022). Although the main theme of the genetic variants of ion channels in epilepsy are channelopathies, there are other particularities to consider.
17.1.1.1 Voltage-Dependent Alterations of Sodium (Na+) Channels
These channels are the primary target of most ASMs, they act by blocking the resting phase (tonic block), selectively preventing the opening of the channel and the conductance of Na+. These channels are formed by an α subunit (pore-forming) and two β subunits (associated auxiliary), when modified they have a role in drug resistance, mainly in relation to the use of carbamazepine (CBZ) or phenytoin (PHT) (Łukawski and Czuczwar 2021).
The β subunit is responsible for modulating the membrane expression of the Na+ channel, its alterations cause incorrect protein folding, and/or abnormal expression of the channel, which are slowly inactivated, causing an increase in Na+ currents, thus way they promote a lower sensitivity to ASMs. The mutation in the gene that encodes the subunit has been related to genetic epilepsy with febrile seizures plus (GEFS+) (Juvale and Che Has 2021).
A relationship has been identified between the rs3812718 and rs2298771 variants of the SCN1A gene and the risk of resistance to CBZ, but the findings are controversial. Given this, a meta-analysis was conducted and all controlled clinical trials on the association of SCN1A, rs3812718 and rs2298771 variants with CBZ resistance in epilepsy were included. A significant association was found between rs2298771 (GG vs. GA + AA) and CBZ resistance in patients of Asian origin with epilepsy, indicating that patients of Asian descent with epilepsy and SCN1A variant rs2298771, especially with the GG genotype, may be at risk of CBZ resistance. In addition, an interaction between the constitutive androstane receptor (CAR) variant rs2502815 and the CBZ response was observed, being identified for the first time a potentially significant interaction between the rs2502815 CAR variant and CBZ response in patients with epilepsy (Kong et al. 2021).
17.1.1.2 Voltage-Dependent Alterations of Calcium (Ca+) Channels
They are transmembrane channels formed by an α1 subunit that functions as the main pore and sensor during the change in potential. They are encoded by 10 genes and have several accessory subunits identified as β, γ, and α2δ (Juvale and Che Has 2021; Sheilabi et al. 2020).
Ca + channel has an excitatory function because it contributes to the initiation of the action potential by acting as a second messenger. There are 6 types (T, L, N, P / Q, R), which are subdivided according to the voltage required for their activation (high or low threshold). When these channels are altered, the activity and expression can be increased superficially in the membrane, causing a precipitous hyperpolarization, which leads to drug resistance due to the high frequency of seizures (Shin et al. 2008).
The T-type Ca+ channel is the only one that is activated with a low threshold. This channel is involved in the pathophysiology of absence-type seizures due to the generation of thalamocortical discharges. An imbalance between the α1 and α1G subunits in Ca+ channel is likely to reduce the response to ethosuximide (ESM), lamotrigine (LTG), valproate (VPA), and zonisamide (ZNS), since the α1G subunit has been linked to generation of spikes and waves of epileptiform discharge (Chioza et al. 2001).
17.1.2 Genetic Variants of Neurotransmitters Receptors
The functional brain requires optimal balance both excitatory and inhibitory inputs for efficient information processing at both the cellular and network level. At network level, this balance is provided by the organization of your main elements: the stimulation of glutamatergic basal cells and inhibition of GABAergic interneurons (Sears and Hewett 2021). A disturbance in balance has been implicated in the etiology and expression of epilepsy, as in the case of Dravet syndrome. However, not only pathogenic genetic variants are important in epilepsy but also nonpathogenic variants that influence response to treatment.
17.1.2.1 Alterations of Gamma Aminobutyric Acid (GABA) Channels
GABA is the main inhibitory neurotransmitter in the adult brain, but in the newborn, it behaves as an excitatory neurotransmitter. GABAA receptors are assembled by 7 different subfamilies (α, β, γ, δ, π, θ, and ρ). The rearrangement of these subfamilies results in the absence of the specific ligand-binding site for benzodiazepines and barbiturates. Traumatic injury may also cause increased GABAA inhibition causing neuronal synchrony or aberrant disinhibition of the epileptogenic network; both alterations lead to an increase in recurrent epileptic seizures and drug resistance (Juvale and Che Has 2021; Łukawski and Czuczwar 2021).
Alterations of the GABAA receptor in animal models have been associated with neuronal loss of the hippocampus in the face of recurrent seizures and/or sustained status epilepticus. Theories hold that a transcriptional change occurs in the α subunit (reduction of the α1 subunit and increase of the α4 subunit) or change in the composition of subunits (loss of the γ2 subunit and incorporation of the δ subunit), with activation of GABAA receptors nonfunctional “leftovers” and an alteration in the phosphorylation state of this receptor (Juvale and Che Has 2021).
The influence of genetic variants on response to ASMs has proved to be controversial as the findings that described the G1465A variant of the GABAB1 receptor to be associated with susceptibility to develop temporal lobe epilepsy and to determine the severity of the epilepsy (Gambardella et al. 2003); while these results have not been supported by other authors (Ma et al. 2005).
Interestingly, the C588T variant of GABRG2 has been identified as a risk variant for the development of idiopathic generalized epilepsy in the Pakistani population, but this gene variant has not been identified to be associated with drug-resistant epilepsy (Saleem et al. 2022). Equally contrasting results were obtained in a study of three cohorts: mesial temporal lobe epilepsy with hippocampal sclerosis (MTLE-HS) (prototype of ASM-resistant epilepsy syndrome), juvenile myoclonic epilepsy (prototype of ASM-responsive epilepsy syndrome), and non-epilepsy controls. The study population were ethnically matched South Indian ancestry and the results identified that rs211037 GABRG2 variant predisposes to epilepsy, irrespective of its phenotype, but not to ASM resistance (Balan et al. 2013).
17.1.2.2 Glutamate Channel Alterations
Glutamate is the main excitatory neurotransmitter in the central nervous system (CNS). Its function is mediated through ionotropic glutamate receptors (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) [AMPA], N-methyl-d-aspartate [NMDA], and kainite, as well as metabotropic receptors (Juvale and Che Has 2021).
NMDA receptors have magnesium ions blocking their pores, AMPA receptors are easily activated, generating rapid excitatory neurotransmission. The expression, composition, and location of both receptors depend on the amount of presynaptic glutamate released and the strength of the resulting synapses, thus generating long-term potentiation and/or depression (Juvale and Che Has 2021).
During seizures, there is abnormal excitation in the brain, resulting in an alteration in AMPA receptor expression, which results in recurrent seizures and neural circuit remodeling. The same can happen with NMDA receptors but with slower activation, but once activated there is a constant influx of Ca+ into the neuron and with them a greater long-term potentiation arises that turns out to be even more damaging (Juvale and Che Has 2021).
Both receptors in a patient with poorly controlled epilepsy contribute to an imbalance and overload the inhibitory system. Moreover, various studies have observed a more specific role after NMDA activation because the internalization of GABA receptors is mediated through clathrin, not only reducing inhibition but also avoiding reaching the target.
The genes encoding the glutamate receptor Gría2 and GluR2 have been found altered in epileptic tissue by epigenetic regulation regarding both histone acetylation and DNA methylation. Glutamine synthetase (GS) responsible for glutamate synthesis is downregulated in hippocampal astrocytes, generating astrogliosis and with them deregulation of glutamate homeostasis, which has also been related to susceptibility to febrile seizures in animal models (Hauser et al. 2018).
17.2 Genetics of Transporter Hypothesis in Drug-Resistant Epilepsy (See Fig. 17.1)
The transporter hypothesis is one of the two most inquired hypotheses regarding DRE. Resistance may be evident from the onset of ASM therapy or after an adequate initial response. There may even be cross-resistance to several ASM as a result of overexpression of transport proteins of membrane (Leandro et al. 2019). Various ASMs, their mechanisms of action, and their corresponding transporters are shown in Table 17.1.
ABC transporters in drug-resistant epilepsy. (a) Neurovascular unit made up of endothelial cells (red), pericyte (yellow), astrocytes (purple), and neurons (green). (b) ABC transporters in blood–brain barrier (BBB): ABCB1 transporter is upregulated in neurons and astrocytes (sky blue) of epileptogenic tissue and some antiseizures drugs affected by the overexpression of this transporter are phenytoin (PHT), phenobarbital (PB), lamotrigine (LTG), and carbamazepine (CBZ); ABCC transporters are overexpressed in astrocytes and/or dysplastic neurons (blue) of epileptogenic tissues and suggested substrates are phenytoin (PHT), phenobarbital (PB), levetiracetam (LEV), carbamazepine (CBZ), and valproate (VPA); finally, ABCG2 transporter is expressed in the endothelial cells of the BBB (gray) and suggested substrates are phenobarbital (PB), levetiracetam (LEV), tiagabine (TGB), and gabapentin (GBP)
According to this theory, excessive activation of P-glycoprotein (P-gp) leads to resistance of ASMs due to excessive clearance of these compounds through the blood–brain barrier back into the blood, resulting in scarce penetration of these drugs in the brain (Miller et al. 2008; Rizzi et al. 2002; van Vliet et al. 2007) (Fig. 17.1). There is evidence of P-gp overexpression in the brain induced by prolonged seizures, which may explain why delaying the start of treatment leads to a decrease in the effectiveness of ASMs (Sisodiya and Thom 2003).
Probable mechanisms associated with the rise in output transporters are inflammation and oxidative stress, drug-mediated induction, the release of glutamate during seizures, and the presence of genetic polymorphisms (Leandro et al. 2019). In this section, we will address the influence of genetic variants on the expression of these transporters.
17.2.1 The ABC Transporters (ATP Binding Cassette)
The ABCB1 gene, encoding P-gp is located on chromosome 7 (7q21.1), contains 28 exons and is highly polymorphic. Variant genetic of this gene may be related to the effectiveness of antiseizure therapy and a rise in its expression leads to an increase in the amount of P-gp in the blood–brain barrier and astrocytes (Smolarz et al. 2021). Some genetic variants identified in ABCB1 are in the coding part of the gene, and those located in exon 26 seem to have functional significance. There are three single nucleotide variants whose allele frequency appear to be of biological significance and are being intensively studied in the context of drug-resistant epilepsy: in exon 12 (rs1128503, 1236C>T), in exon 21 (rs2032582, 2677G >T/A) and in exon 26 (rs1045642, 3435C>T) (Skalski et al. 2011).
It has been found that the genotype C3435T/CC is associated with an increase in P-gp expression, which affects the concentration of ASMs in plasma of patients with DRE epilepsy (Lazarowski and Czornyj 2011; van Vliet et al. 2010). Pharmacogenomic studies regarding membrane drug transporters have found the association of DRE with the genotype 3435CC of the ABCB1 gene (Siddiqui et al. 2003; Soranzo et al. 2005). However, studies of the relationship between ABCB1 genetic variants and response to antiseizure treatment have yielded contradictory results (Cascorbi et al. 2001; Mosyagin et al. 2008; Sills et al. 2005; Tan et al. 2004; Vahab et al. 2009; von Stülpnagel et al. 2009).
Because there are differences in the efficacy of ASMs, studies have been conducted to assess the impact of genetic variants of membrane drug transporters on specific drugs. The effect of variants in the gene encoding P-gp on levetiracetam (LEV) disposition in children with epilepsy have been described (Zhao et al. 2020). It is reported an association to specific variants that may affect LEV therapeutic efficacy in children with epilepsy. Also, ABCB1 gene loci genotypes have been compared in children with epilepsy and healthy children, identifying genotypes that are associated with DRE (Gao et al. 2019).
On the other hand, a strong association between genetic variants rs2235048, rs1045642, rs2032582, and rs1128503 of the ABCB1 gen with ASM resistance has been demonstrated among women, but not men. This data suggests that there is a gender-dependent relationship between ABCB1 genetic variants and the response to ASMs (Tamimi et al. 2021). However, more research is needed to confirm this association.
Furthermore, there is a dilemma about the influence of the genetic variants of the ABCC2 and ABCG2 transporters in altering the response to ASMs, with controversial and inconclusive results (Al-Eitan et al. 2019; Chen et al. 2019; Shen et al. 2016; Yang et al. 2019). A meta-analysis identified a significant association of the variant ABCC2 rs717620 with ASM resistance in the general population, as well as an association of ABCC2 rs3740066 with resistance to ASM. ABCG2 rs2273697, ABCG2 rs2231137, and rs2231142 were not associated with response to ASMs in the meta-analysis (Zan et al. 2021).
Therefore, therapies focused on combating drug resistance through direct inhibition of P-gp efflux transporters have been created. There are four generations of inhibitor drugs to be mentioned: (1) first generation, nonspecific for P-gp: cyclosporine A and verapamil; (2) second generation, more specific for P-gp but interfere with the cytochrome CYP3A4 metabolizing enzyme: valspodar (cyclosporin A analog); (3) third generation, specific for P-gp and do not interfere with enzymes that metabolize drugs: Tariquidar; (4) fourth generation, still under study for its use in humans: cyclic peptide QZ59SE and the natural compounds lamellarin and gomisin (Tang et al. 2017). However, the use of specific P-gp inhibitors is not without concern, as systemic P-gp inhibition could increase plasma concentrations of drugs and toxins, potentially leading to systemic toxicity (Czornyj et al. 2022; Tang et al. 2017).
Among the P-gp inhibitors, the most used in epilepsy research is verapamil as adjuvant therapy in DRE. Its use is limited by its side effects on heart rate, blood pressure, skin rashes, and foot edema. Despite the fact that in an open non-placebo controlled study of 19 patients, in which verapamil was used without reports of effects on hemodynamics and a decrease of seizures by 50%, it is necessary to have more solid evidence with double-blind studies with larger populations. Nifedipine and diltiazem have also been coadministered with ASMs to inhibit P-gp, increasing brain plasma levels of ASMs, achieving better control of seizures. Moreover, as medications that inhibit Ca+ channels, they could have an intrinsic activity and their inhibitory effect on CYP3A4 is difficult to differentiate from the effect of P-gp inhibition (Leandro et al. 2019; Tang et al. 2017).
17.3 Genetics of Neural Networks Hypothesis
The basis of this hypothesis is that recurrent seizures cause cell death, and the remodeling of these circuits can result in aberrant excitatory networks, either they have hyper excitatory properties or they do not respond to endogenous inhibitory mechanisms or to the action of the ASMs by not allowing them to reach their targets. It is suggested that, under the command of an erroneous message generated by recurrent seizures, the damaged brain tissue will spread to nonphysiological regions, forming abnormal connections with neurons far from their original synapses, all this through neuronal degeneration, necrosis, gliosis, sprouting, synaptic reorganization, and finally network remodeling (Fang et al. 2011).
Before the emergence of the neural network theory, it was already suggested that hippocampal sclerosis might play a causal role in the mechanisms of drug resistance in MTLE, and how its resection allowed seizure freedom in almost 60% of patients, although later it was corroborated that not all postoperative patients became drug sensitive. The experimental models carried out by Volk et al. and Bethmann et al. compared hippocampal damage in drug-sensitive epileptic rats with those that were drug-resistant. More than 90% of drug-resistant animals showed significant neuronal loss in CA1, Ca3c/CA4 and in the dentate gyrus (Löscher et al. 2020). These structural changes could be the basis of the affection in multiple functional systems that patients with DRE suffer over time and evolution of the disease; for example, in executive functions, language and memory (Lazarowski et al. 1999).
The molecular basis of the network hypothesis can involve changes in multiple genes related to the cytoskeleton (Rho-family GTPase: Cdc42, RhoA, N-WASP, and actin related protein 2/3), neuronal plasticity, and structural reorganization identified in patients with DRE and mostly associated with the axonal growth cone. These findings expose how epileptogenesis shares characteristics with normal neurodevelopment (Fang et al. 2011). The greatest weaknesses of this hypothesis are basically the impossibility to find, to date, an adequate animal model for its reproducibility and the fact that these brain morphological changes do not always lead to DRE.
17.4 Gene Variant Hypothesis
This theory postulates that there are variations in genes that encode enzymes involved in the metabolism of ASMs, ion channels or neurotransmitter receptors that are the target of these drugs. These changes cause alterations in the pharmacokinetics and pharmacodynamics of ASMs and compromise their efficacy (Łukawski and Czuczwar 2021; Pérez-Pérez et al. 2021). For example, a strong association was found between low activity of CYP2C9 alleles (CYP2C9*2 and CYP2C9*3) and a decrease in the required dose of phenytoin. An intronic single nucleotide polymorphism found in the SCN1A gene (IVS5-91G→A or rs3812718) was associated with higher required doses of CBZ and PHT. There is a high frequency of the SCN1A IVS5-91 AA genotype in patients with CBZ resistance. Many other single nucleotide polymorphisms associated with Na+ channel genes are currently under study (including SCN1A c.3184 A→G and SCN2A c.56 G→A).
The genetic associations require subsequent confirmation in larger populations, which is difficult because they are infrequent alleles, so the impact of this theory alone remains very limited.
It is worth mentioning the epigenetic changes that are not included in this or other DRE theories. Whether through DNA methylation, posttranslational modifications in histones, or noncoding RNAs, recurrent seizures can produce epigenetic changes, which could modify the response to drugs. On the other hand, it is believed that the ASMs by themselves could induce epigenetic changes that favor drug resistance. There is still no experimental evidence for these (Tang et al. 2017).
17.5 Genetics of Pharmacokinetic Hypothesis
Several patients with DRE had serum concentrations below the range considered therapeutic despite adequate adherence (Lancelin et al. 2007; Lazarowski et al. 1999; Mohammed Ebid et al. 2007). This hypothesis should be understood more specifically as the abnormalities in the metabolism and elimination of ASMs (Pérez-Pérez et al. 2021). It indicated that DRE can be explained by the low availability in the amount of ASM that enters the brain to reach the epileptogenic focus, since there is overexpression of ASM efflux transporters in other organs: intestine, liver, and kidneys (Tang et al. 2017).
Up to 90% of all prescribed medications are metabolized by CYP450 (CYP) enzymes. CYP34A4 represents more than 30% of hepatic CYPs, but there are others that are also of great importance for drug metabolism: CYP1A2, CYP2B6, CYP2C9, CYP2C19, and CYP2D6. Indeed, they are also expressed in endothelial cells and in the blood–brain barrier (Ghosh et al. 2010, 2011). They are encoded in genes that are highly polymorphic, such as CYP2D6, with more than 100 known allelic variants. Genetic variants can modify the function of the P450 enzymes (Feng et al. 2018). In fact, large ethnic and intersubject variations of these enzymes can explain partial or complete loss of enzyme function.
Regarding PHT, 13 alleles of the CYP2C9 gene have been identified, of which CYP2C9*2 and CYP2C9*3 resulted from mutations in the CYP29C*1 coding sequence leading to the substitution of one amino acid—R144C and I359L, respectively. This is associated with reduced activity of the enzyme to metabolize PHT (Brandolese et al. 2001). Other study shows that patients carrying at least one mutant CYP2C9 allele required 37% lower doses of PHT than the wild-type subjects (van der Weide et al. 2001). Another study in children demonstrated an important role of the allelic variant CYP 3A4*1B as a risk factor for the development of drug resistance (López-García et al. 2017). Moreover, it has been identified that the genetic variants rs1799853 and rs1057910 CYP2C9 and the polymorphism rs4244285 CYP2C19 may be associated with the occurrence of DRE in children (Makowska et al. 2020).
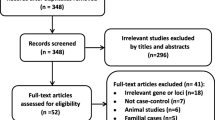
17.6 Pharmacogenetics of DRE in Children
DRE occurs frequently in epileptic syndromes such as Dravet syndrome during infancy (Gonzalez-Giraldo and Sullivan 2020), thus pharmacogenetic research in this age group has been increasing. A systematic review identified the genetic variants associated to the efficacy of ASMs in children with DRE. In this review included case–control and cross-sectional studies with analysis of ion channel genes, genes coding for drug transporters, and enzymes genes. Summarizing the results, variants of the ABCB1 gene have been associated with high-risk of resistance to ASMs, as S893A polymorphism (T allele, Ser893Ala) that was associated with risk of resistance to LTG in absence epilepsy, and C and T alleles of C3435T polymorphism that were shown to predispose to more resistant disease (Gogou and Pavlou 2019). In addition, while the variants of SCN1A gene and cytochrome P450 gene had a significant impact (either positive or negative) on responsiveness to ASMs, variants of uridine diphosphate glucuronosyltransferase UGT2B7 gene were associated with increased remission rate in children with generalized seizures (Gogou and Pavlou 2019). This demonstrates the impact of genetics on the development and management of DRE in children.
17.7 Genetic Epilepsies “Difficult to Treat”
Pathogenic alterations or mutation in genes and structural abnormalities in chromosomes (deletions, insertions) are responsible of a variety of epilepsies. In some, the possibility of DRE is high. Several mechanisms may be interrelated between genetic disorders and the presence of epilepsy. It is important to distinguish between the susceptibility to generate epilepsy caused by a functional abnormality of a gene and epilepsy that results from structural or functional abnormalities in a chromosome. Some genetic disorders relate more to certain types of epilepsy, but overall, any seizure type may be present. Table 17.2 summarizes some genetic pharmacoresistant epilepsies.
17.8 Conclusions
17.8.1 Limitations of the Gene Hypothesis
To prove a given drug resistance theory, it is important to show that the subgroup of patients with DRE has differences in their receptors in comparison to those of responders. However, this is difficult to achieve because patients who respond to ASMs are not subjected to epilepsy surgery or further study, although, sometimes as controls.
Any proposed mechanism for drug resistance must meet the following requirements to be considered valid: be detectable in epileptic brain tissue, have a pathophysiological mechanism demonstrable in human epilepsy, and, when modified, must affect the phenomenon of drug resistance (Sisodiya and Thom 2003).
The fact that most patients are resistant to multiple treatments, including several ASMs with different mechanisms of action, suggests that other less specific or unknown mechanisms with some commonality about ASM cellular or network actions contribute to drug resistance, or that more than one mechanism may be involved (Löscher et al. 2006). Some changes were induced only transiently in animal models of epilepsy which do not necessarily explain chronic pharmacorresistance (Deeken and Löscher 2007; van Vliet et al. 2005). According to Schmidt and Löscher (2009), the intrinsic hypothesis lacks studies and “a subgroup of patients with a higher seizure frequency at the onset of treatment will become seizure-free but require higher serum concentrations of ASMs to do so than those with a lower seizure frequency, and this hypothesis does not have a genetic component.”
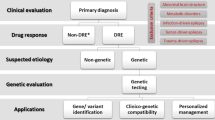
17.8.2 How to Define Genetic Drug-Resistant Epilepsies?
This chapter leads us to the question—what is the definition of genetic “drug- resistant” epilepsies? In the end, we propose two assertions: (1) epilepsies are drug-resistant because the ASM does not have effect on the specific molecular lesion of the epilepsy syndrome. The epilepsy is supposedly “drug resistant” and seizures do not stop because “the key does not fit the lock in the door” and (2) when the ASM has a proven effect on the molecular lesion, but seizures persist despite a proper treatment; this later, we believe is true genetic pharmacorresistant epilepsy. Therefore, we favor the “intrinsic disease” mechanisms as an explanation for the resistance in genetic epilepsies (Fig. 17.2).
(a) EFHC1 /Myoclonin mutations in juvenile myoclonic epilepsy (JME) frequently respond to treatment with valproate (VPA); however, other JME mutations (illustrated as Myoclonin 2 and Myoclonin 3) might not achieve seizure control due to a different molecular lesion unresponsive to VPA therapy. (b) EFHC1 /Myoclonin mutations in a susceptibility or early stage respond adequately to VPA treatment, whereas in established epileptogenesis drug resistance is seen even though the same molecular lesion is present; therefore, a true genetic pharmacorresistance is encountered
17.8.3 Future Directions
The question is how to tackle the problem in patients. A recommended step now is to genotype epilepsies and use the information obtained to guide ASM administration. It would be ideal to perform a whole or large scale pharmacogenomic study of how ASMs effects are genetically determined to look for responders and nonresponders and identify patients that could develop side effects as consequence of specific ASMs.
A large-scale pharmacogenomic study could also be done in patients who were submitted to surgery for DRE. Surgical specimens could be reviewed for their neuropathologic and biochemical abnormalities and correlate the findings with whole genome sequencing.
References
Al-Eitan LN, Al-Dalalah IM, Mustafa MM, Alghamdi MA, Elshammari AK, Khreisat WH, Aljamal HA. Effects of MTHFR and ABCC2 gene polymorphisms on antiepileptic drug responsiveness in Jordanian epileptic patients. Pharmacogenom Personal Med. 2019;12:87–95. https://doi.org/10.2147/PGPM.S211490.
Angelman H. Puppet children: a report on three cases. Dev Med Child Neurol 1965;7:681–8.
Balan S, Sathyan S, Radha SK, Joseph V, Radhakrishnan K, Banerjee M. GABRG2, rs211037 is associated with epilepsy susceptibility, but not with antiepileptic drug resistance and febrile seizures. Pharmacogenet Genomics. 2013;23(11):605–10. https://doi.org/10.1097/FPC.0000000000000000.
Brandolese R, Scordo MG, Spina E, Gusella M, Padrini R. Severe phenytoin intoxication in a subject homozygous for CYP2C9*3. Clin Pharmacol Therapeutics. 2001;70(4):391–4. https://doi.org/10.1016/S0009-9236(01)95478-5.
Cassidy SB, Thuline HC, Holm VA. Deletion of chromosome 15 (q11-13) in a Prader-Labhart-Willi syndrome clinic population. Am J Med Genet. 1984;17(2):485–95.
Chan EM, Young EJ, Ianzano L, Munteanu I, Zhao X, Christopoulos CC, et al. Mutations in NHLRC1 cause progressive myoclonus epilepsy. Nat Genet. 2003;35(2):125–7.
Canevini MP, Sgro V, Zuffardi O, Canger R, Carrozzo R, Rossi E, et al. Chromosome 20 ring: a chromosomal disorder associated with a particular electroclinical pattern. Epilepsia. 1998;39(9):942–51.
Cascorbi I, Gerloff T, Johne A, Meisel C, Hoffmeyer S, Schwab M, et al. Frequency of single nucleotide polymorphisms in the P-glycoprotein drug transporter MDR1 gene in white subjects. Clin Pharmacol Therapeutics. 2001;69(3):169–74. https://doi.org/10.1067/MCP.2001.114164.
Chen J, Su Q, Qin J, Zhou Y, Ruan H, Chen Z, et al. Correlation of MCT1 and ABCC2 gene polymorphisms with valproic acid resistance in patients with epilepsy on valproic acid monotherapy. Drug Metab Pharmacokinet. 2019;34(3):165–71. https://doi.org/10.1016/J.DMPK.2018.01.006.
Chioza B, Wilkie H, Nashef L, Blower J, McCormick D, Sham P, Asherson P, Makoff AJ. Association between the alpha(1a) calcium channel gene CACNA1A and idiopathic generalized epilepsy. Neurology. 2001;56(9):1245–6.
Czornyj L, Auzmendi J, Lazarowski A. Transporter hypothesis in pharmacoresistant epilepsies. Is it at the central or peripheral level? Epilepsia Open. 2022;7 Suppl 1(Suppl 1):S34–S46. https://doi.org/10.1002/EPI4.12537.
Deeken JF, Löscher W. The blood-brain barrier and cancer: transporters, treatment, and Trojan horses. Clin Cancer Res. 2007;13(6):1663–74.
Dobyns WB, Reiner O, Carrozzo R, Ledbetter DH. Lissencephaly. A human brain malformation associated with deletion of the LIS1 gene located at chromosome 17p13. JAMA. 1993;270(23):2838–42.
Dravet C. - Vie Med. Les epilepsies graves de l’enfant. 1978;8:543–48.
Fang M, Xi ZQ, Wu Y, Wang XF. A new hypothesis of drug refractory epilepsy: neural network hypothesis. Med Hypotheses. 2011;76(6):871–6.
Feng W, Mei S, Zhu L, Yu Y, Yang W, Gao B, et al. Effects of UGT2B7, SCN1A and CYP3A4 on the therapeutic response of sodium valproate treatment in children with generalized seizures. Seizure. 2018;58:96–100. https://doi.org/10.1016/J.SEIZURE.2018.04.006.
Fu YH, Kuhl DP, Pizzuti A, Pieretti M, Sutcliffe JS, Richards S, et al. Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell. 1991;67(6):1047–58.
Gambardella A, Manna I, Labate A, Chifari R, la Russa A, Serra P, et al. GABA(B) receptor 1 polymorphism (G1465A) is associated with temporal lobe epilepsy. Neurology. 2003;60(4):560–3. https://doi.org/10.1212/01.WNL.0000046520.79877.D8.
Ganesh S, Delgado-Escueta AV, Sakamoto T, Avila MR, Machado-Salas J, Hoshii Y, et al. Targeted disruption of the Epm2a gene causes formation of Lafora inclusion bodies, neurodegeneration, ataxia, myoclonus epilepsy and impaired behavioral response in mice. Hum Mol Genet. 2002a;11(11):1251–62.
Ganesh S, Delgado-Escueta AV, Suzuki T, Francheschetti S, Riggio C, Avanzini G, et al. Genotype-phenotype correlations for EPM2A mutations in Lafora’s progressive myoclonus epilepsy: exon 1 mutations associate with an early-onset cognitive deficit subphenotype. Hum Mol Genet. 2002b;11(11):1263–71.
Gao L, Yin X, Li Y, Xiao H, Yang L, Fan H, et al. Association of MDR1 gene polymorphisms with refractory epilepsy in children. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2019;36(11):1073–6. https://doi.org/10.3760/CMA.J.ISSN.1003-9406.2019.11.004.
Ghosh C, Gonzalez-Martinez J, Hossain M, Cucullo L, Fazio V, Janigro D, Marchi N. Pattern of P450 expression at the human blood-brain barrier: roles of epileptic condition and laminar flow. Epilepsia. 2010;51(8):1408–17. https://doi.org/10.1111/J.1528-1167.2009.02428.X.
Ghosh C, Marchi N, Desai NK, Puvenna V, Hossain M, Gonzalez-Martinez J, et al. Cellular localization and functional significance of CYP3A4 in the human epileptic brain. Epilepsia. 2011;52(3):562–71. https://doi.org/10.1111/J.1528-1167.2010.02956.X.
Gogou M, Pavlou E. Efficacy of antiepileptic drugs in the era of pharmacogenomics: a focus on childhood. Eur J Paediatr Neurol. 2019;23:674–84. W.B. Saunders Ltd. https://doi.org/10.1016/j.ejpn.2019.06.004.
Gonzalez-Giraldo E, Sullivan JE. Advances in the treatment of drug-resistant pediatric Epilepsy. Semin Neurol. 2020;40(2):257–62. https://doi.org/10.1055/s-0040-1702941.
Harkin LA, McMahon JM, Iona X, Dibbens L, Pelekanos JT, Zuberi SM, et al. Infantile Epileptic Encephalopathy Referral Consortium, Sutherland G, Berkovic SF, Mulley JC, Scheffer IE. The spectrum of SCN1A-related infantile epileptic encephalopathies. Brain. 2007;130(Pt 3):843–52.
Hauser RM, Henshall DC, Lubin FD. The epigenetics of epilepsy and its progression. Neuroscientist. 2018;24(2):186–200.
Juvale IIA, Che Has AT. Possible interplay between the theories of pharmacoresistant epilepsy. Eur J Neurosci. 2021;53(6):1998–2026. https://doi.org/10.1111/EJN.15079.
Klepper J, Voit T. Facilitated glucose transporter protein type 1 (GLUT1) deficiency syndrome: impaired glucose transport into brain– a review. Eur J Pediatr. 2002;161(6):295–304.
Kong FC, Ma CL, Lang LQ, Zhong MK. Association of xenobiotic receptor polymorphisms with carbamazepine response in epilepsy patients. Gene. 2021;771 https://doi.org/10.1016/J.GENE.2020.145359.
Kubota H, Ishihara H, Langmann T, Schmitz G, Stieger B, Wieser HG, et al. Distribution and functional activity of P-glycoprotein and multidrug resistance associated proteins in human brain microvascular endothelial cells in hippocampal sclerosis. Epilepsy Res. 2006;68(3):213–28.
Lancelin F, Franchon E, Kraoul L, Garciau I, Brovedani S, Tabaouti K, et al. Therapeutic drug monitoring of levetiracetam by high-performance liquid chromatography with photodiode array ultraviolet detection: preliminary observations on correlation between plasma concentration and clinical response in patients with refractory epilepsy. Ther Drug Monit. 2007;29(5):576–83. https://doi.org/10.1097/FTD.0B013E318157032D.
Lazarowski A, Czornyj L. Potential role of multidrug resistant proteins in refractory epilepsy and antiepileptic drugs interactions. Drug Metabol Drug Interact. 2011;26(1):21–6. https://doi.org/10.1515/DMDI.2011.006/MACHINEREADABLECITATION/RIS.
Lazarowski A, Sevlever G, Taratuto A, Massaro M, Rabinowicz A. Tuberous sclerosis associated with MDR1 gene expression and drug- resistant epilepsy. Pediatr Neurol. 1999;21(4):731–4. https://doi.org/10.1016/S0887-8994(99)00074-0.
Leandro K, Bicker J, Alves G, Falcão A, Fortuna A. ABC transporters in drug-resistant epilepsy: mechanisms of upregulation and therapeutic approaches. Pharmacol Res. 2019;144:357–76. https://doi.org/10.1016/J.PHRS.2019.04.031.
López-García MA, Feria-Romero IA, Serrano H, Rayo-Mares D, Fagiolino P, Vázquez M, et al. Influence of genetic variants of CYP2D6, CYP2C9, CYP2C19 and CYP3A4 on antiepileptic drug metabolism in pediatric patients with refractory epilepsy. Pharmacol Rep. 2017;69(3):504–11. https://doi.org/10.1016/J.PHAREP.2017.01.007.
Löscher W, Poulter MO, Padjen AL. Major targets and mechanisms of antiepileptic drugs and major reasons for failure. Adv Neurol. 2006;97:417–27.
Löscher W, Potschka H, Sisodiya SM, Vezzani A. Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol Rev. 2020;72(3):606–38.
Łukawski K, Czuczwar SJ. Understanding mechanisms of drug resistance in epilepsy and strategies for overcoming it. Expert Opin Drug Metab Toxicol. 2021;17(9):1075–90. https://doi.org/10.1080/17425255.2021.1959912.
Ma S, Abou-Khalil B, Sutcliffe JS, Haines JL, Hedera P. The GABBR1 locus and the G1465A variant is not associated with temporal lobe epilepsy preceded by febrile seizures. BMC Med Genet. 2005;6(1):1–5. https://doi.org/10.1186/1471-2350-6-13/PEER-REVIEW.
Makowska M, Smolarz B, Bryś M, Forma E, Romanowicz H. An association between the rs1799853 and rs1057910 polymorphisms of CYP2C9, the rs4244285 polymorphism of CYP2C19 and the prevalence rates of drug-resistant epilepsy in children. 2020;131(12):1147–54. https://doi.org/10.1080/00207454.2020.1781110.
Miller JQ- Lissencephaly in 2 siblings. Neurology. 1963;13:841–50.
Miller DS, Bauer B, Hartz AMS. Modulation of P-glycoprotein at the blood-brain barrier: opportunities to improve central nervous system pharmacotherapy. Pharmacol Rev. 2008;60(2):196–209. https://doi.org/10.1124/PR.107.07109.
Minassian BA, DeLorey TM, Olsen RW, Philippart M, Bronstein Y, Zhang Q, et al. Angelman syndrome: correlations between epilepsy phenotypes and genotypes. Ann Neurol. 1998;43(4):485–93.
Mohammed Ebid AHI, Ahmed MMM, Mohammed SA. Therapeutic drug monitoring and clinical outcomes in epileptic Egyptian patients: a gene polymorphism perspective study. Ther Drug Monit. 2007;29(3):305–12. https://doi.org/10.1097/FTD.0B013E318067CE90.
Mosyagin I, Runge U, Schroeder HW, Dazert E, Vogelgesang S, Siegmund W, et al. Association of ABCB1 genetic variants 3435C>T and 2677G>T to ABCB1 mRNA and protein expression in brain tissue from refractory epilepsy patients. Epilepsia. 2008;49(9):1555–61. https://doi.org/10.1111/J.1528-1167.2008.01661.X.
Ohmori I, Ouchida M, Ohtsuka Y, Oka E, Shimizu K. Significant correlation of the SCN1A mutations and severe myoclonic epilepsy in infancy. Biochem Biophys Res Commun. 2002;295(1):17–23.
Pérez-Pérez D, Frías-Soria CL, Rocha L. Drug-resistant epilepsy: from multiple hypotheses to an integral explanation using preclinical resources. Epilepsy Behav. 2021;121(Pt B) https://doi.org/10.1016/J.YEBEH.2019.07.031.
Povey S, Burley MW, Attwood J, Benham F, Hunt D, Jeremiah SJ, et al. Two loci for tuberous sclerosis: one on 9q34 and one on 16p13. Ann Hum Genet. 1994;58(Pt 2):107–27.
Rizzi M, Caccia S, Guiso G, Richichi C, Gorter JA, Aronica E, et al. Limbic seizures induce P-glycoprotein in rodent brain: functional implications for pharmacoresistance. J Neurosci. 2002;22(14):5833–9. https://doi.org/10.1523/JNEUROSCI.22-14-05833.2002.
Saleem T, Maqbool H, Sheikh N, Tayyeb A, Mukhtar M, Ashfaq A. GABRG2 C588T polymorphism is associated with idiopathic generalized Epilepsy but not with antiepileptic drug resistance in Pakistani Cohort. Biomed Res Int. 2022;2022:3460792. https://doi.org/10.1155/2022/3460792.
Schmidt D, Löscher W. New developments in antiepileptic drug resistance: an integrative view. Epilepsy Curr. 2009;9(2):47–52.
Sears SMS, Hewett SJ. Influence of glutamate and GABA transport on brain excitatory/inhibitory balance. Exper Biol Med. 2021;246:1069–83. SAGE Publications Inc. https://doi.org/10.1177/1535370221989263.
Shahwan A, Farrell M, Delanty N. Progressive myoclonic epilepsies: a review of genetic and therapeutic aspects. Lancet Neurol. 2005;4(4):239–48.
Sheilabi MA, Takeshita LY, Sims EJ, Falciani F, Princivalle AP. The sodium channel B4-subunits are dysregulated in temporal lobe epilepsy drug-resistant patients. Int J Mol Sci. 2020;21(8):2955.
Shen CH, Zhang YX, Lu RY, Jin B, Wang S, Liu ZR, et al. Specific OCT1 and ABCG2 polymorphisms are associated with Lamotrigine concentrations in Chinese patients with epilepsy. Epilepsy Res. 2016;127:186–90. https://doi.org/10.1016/J.EPLEPSYRES.2016.09.004.
Shin HS, Cheong EJ, Choi S, Lee J, Na HS. T-type Ca2+ channels as therapeutic targets in the nervous system. Curr Opin Pharmacol. 2008;8(1):33–41.
Shlobin NA, Sander JW. Current principles in the management of drug-resistant Epilepsy. CNS Drugs. 2022;36(6):555–68. https://doi.org/10.1007/S40263-022-00922-4.
Singh R, Andermann E, Whitehouse WP, Harvey AS, Keene DL, Seni MH, Crossland KM, Andermann F, Berkovic SF, Scheffer IE. Severe myoclonic epilepsy of infancy: extended spectrum of GEFS+? Epilepsia. 2001;42:837–44.
Siddiqui A, Kerb R, Weale ME, Brinkmann U, Smith A, Goldstein DB, et al. Association of multidrug resistance in Epilepsy with a polymorphism in the drug-transporter gene ABCB1. 2003;348(15):1442–8. https://doi.org/10.1056/NEJMOA021986.
Sills GJ, Mohanraj R, Butler E, McCrindle S, Collier L, Wilson EA, Brodie MJ. Lack of association between the C3435T polymorphism in the human multidrug resistance (MDR1) gene and Response to antiepileptic drug treatment. Epilepsia. 2005;46(5):643–7. https://doi.org/10.1111/J.1528-1167.2005.46304.X.
Sisodiya SM, Thom M. Widespread upregulation of drug-resistance proteins in fatal human status epilepticus. Epilepsia. 2003;44(2):261–4. https://doi.org/10.1046/J.1528-1157.2003.42802.X.
Skalski D, Smolarz B, Wendorff J. Zwia˛zek pomie˛dzy polimorfizmami pojedynczych nukleotydów genu opornos’ci wielolekowej typu 1. a padaczka˛ lekooporna. Neuropsychiatry Neuropsychol. 2011;2:79–84.
Smolarz B, Makowska M, Romanowicz H. Pharmacogenetics of drug-resistant epilepsy (Review of literature). Int J Mol Sci. 2021, November 1;22. MDPI. https://doi.org/10.3390/ijms222111696.
Soranzo N, Goldstein DB, Sisodiya SM. The role of common variation in drug transporter genes in refractory epilepsy. 2005;6(8):1305–12. https://doi.org/10.1517/14656566.6.8.1305.
Tamimi DE, Abduljabbar R, Yousef AM, Saeed RM, Zawiah M. Association between ABCB1 polymorphisms and response to antiepileptic drugs among Jordanian epileptic patients. Neurol Res. 2021;43(9):724–35. https://doi.org/10.1080/01616412.2021.1922182.
Tan NCK, Heron SE, Scheffer IE, Pelekanos JT, McMahon JM, Vears DF, et al. Failure to confirm association of a polymorphism in ABCB1 with multidrug-resistant epilepsy. Neurology. 2004;63(6):1090–2. https://doi.org/10.1212/01.WNL.0000137051.33486.C7.
Tang F, Hartz AMS, Bauer B. Drug-resistant Epilepsy: multiple hypotheses, few answers. Front Neurol. 2017;8(JUL) https://doi.org/10.3389/FNEUR.2017.00301.
Vahab SA, Sen S, Ravindran N, Mony S, Mathew A, Vuayan N, et al. Analysis of genotype and haplotype effects of ABCB1 (MDR1) polymorphisms in the risk of medically refractory Epilepsy in an Indian population. Drug Metab Pharmacokinet. 2009;24(3):255–60. https://doi.org/10.2133/DMPK.24.255.
van der Weide J, Steijns LSW, van Weelden MJM, de Haan K. The effect of genetic polymorphism of cytochrome P450 CYP2C9 on phenytoin dose requirement. Pharmacogenetics. 2001;11(4):287–91. https://doi.org/10.1097/00008571-200106000-00002.
van Vliet EA, Redeker S, Aronica E, Edelbroek PM, Gorter JA. Expression of multidrug transporters MRP1, MRP2, and BCRP shortly after status epilepticus, during the latent period, and in chronic epileptic rats. Epilepsia. 2005;46(10):1569–80. https://doi.org/10.1111/j.1528-1167.2005.00250.x
van Vliet EA, van Schaik R, Edelbroek PM, Voskuyl RA, Redeker S, Aronica E, et al. Region-specific overexpression of P-glycoprotein at the blood-brain barrier affects brain uptake of phenytoin in epileptic rats. J Pharmacol Exp Ther. 2007;322(1):141–7. https://doi.org/10.1124/JPET.107.121178.
van Vliet EA, Zibell G, Pekcec A, Schlichtiger J, Edelbroek PM, Holtman L, et al. COX-2 inhibition controls P-glycoprotein expression and promotes brain delivery of phenytoin in chronic epileptic rats. Neuropharmacology. 2010;58(2):404–12. https://doi.org/10.1016/J.NEUROPHARM.2009.09.012.
von Stülpnagel C, Plischke H, Zill P, Bäumel C, Spiegel R, Gruber R, Kluger G. Letter: lack of association between MDR1 polymorphisms and pharmacoresistance to anticonvulsive drugs in patients with childhood-onset epilepsy. Epilepsia. 2009;50(7):1835–7. https://doi.org/10.1111/J.1528-1167.2009.02077.X.
Yang X, Yan Y, Fang S, Zeng S, Ma H, Qian L, et al. Comparison of oxcarbazepine efficacy and MHD concentrations relative to age and BMI associations among ABCB1, ABCC2, UGT2B7, and SCN2A polymorphisms. Medicine (United States). 2019;98(12) https://doi.org/10.1097/MD.0000000000014908.
Zan X, Yue G, Hao Y, Sima X. A systematic review and meta-analysis of the association of ABCC2/ABCG2 polymorphisms with antiepileptic drug responses in epileptic patients. Epilepsy Res. 2021;175:106678. https://doi.org/10.1016/J.EPLEPSYRES.2021.106678.
Zhao T, Yu J, Wang TT, Feng J, Zhao WB, Sun L, et al. Impact of ABCB1 polymorphism on levetiracetam serum concentrations in epileptic Uygur children in China. Ther Drug Monit. 2020;42(6):886–92. https://doi.org/10.1097/FTD.0000000000000805.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Martínez-Juárez, I.E. et al. (2023). Genes Involved in Pharmacoresistant Epilepsy. In: Rocha, L.L., Lazarowski, A., Cavalheiro, E.A. (eds) Pharmacoresistance in Epilepsy. Springer, Cham. https://doi.org/10.1007/978-3-031-36526-3_17
Download citation
DOI: https://doi.org/10.1007/978-3-031-36526-3_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36525-6
Online ISBN: 978-3-031-36526-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)