Abstract
Youth with autism spectrum disorders (ASD) commonly experience clinically significant anxiety disorders. Diagnosis and assessment of anxiety disorders in youth with ASD has proven difficult. Potential contributing factors to the development of anxiety disorders in this population are discussed. Furthermore, the chapter reviews research on the effectiveness of modified cognitive-behavioral therapy (CBT) that addresses both the anxiety and clinical needs of youth with ASD. The chapter concludes with a case study exemplifying a modified CBT program for a child with high-functioning autism.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Nature of Problem
Prevalence
Considerable research indicates that youth diagnosed with autism spectrum disorders (ASD) experience psychiatric symptoms meeting clinical diagnostic criteria for a range of disorders, including anxiety disorders (Gadow, Devincent, Pomeroy, & Azizian, 2005; Kim, Szatmari, Bryson, Streiner, & Wilson, 2000; Sukhodolsky et al., 2008; White, Oswald, Ollendick, & Scahill, 2009). The presence of anxiety disorders in ASD has been widely documented, but the prevalence rate varies across the literature (e.g., de Bruin, Ferdinand, Meester, de Nijs, & Verheij, 2007; Leyfer et al., 2006). For example, White et al. (2009) demonstrated in a comprehensive review that significantly impairing anxiety symptoms were present in 11–85% of youth diagnosed with ASD. More specifically, studies using robust diagnostic criteria indicate that anxiety disorders occur in at least 45% of youngsters with ASD (Leyfer et al., 2006; Simonoff et al., 2008; Sukhodolsky et al., 2008). Simonoff et al. (2008) found that up to 71% of the youth met criteria for at least one psychiatric disorder and, of these, 42% met criteria for an anxiety disorder according to the Diagnostic and Statistical Manual of Mental Disorders—4th Edition criteria (DSM-IV-TR; American Psychiatric Association, 2000) based on a population-derived sample of children and adolescents diagnosed with an ASD.
Symptomology and Diagnostic Issues
Youth with ASD have been reported to present frequently with simple phobias, generalized anxiety disorder, separation anxiety disorder, obsessive-compulsive disorder, and social anxiety. There does not seem to be one anxiety disorder that is specifically associated with ASD. Rather, heterogeneity exists in the rates in which the different types of anxiety disorders have been reported. In one clinical sample of school-aged children diagnosed with ASD, of those who met diagnostic criteria for anxiety disorders, simple phobia was the most widely endorsed (31%), then social phobia (20%), separation anxiety disorder (11%), and generalized anxiety disorder (10%; Sukhodolsky et al., 2008). In another study, social phobia was the most commonly diagnosed (30%) followed by generalized anxiety (13%; Simonoff et al., 2008).
Among youth with ASD, anxiety disorders occur at commensurate or higher frequency and severity levels than that observed in the general community (e.g., Kim et al., 2000; Lecavalier, 2006; Russell & Sofronoff, 2005; White et al., 2009). Gadow et al. (2005) found that 25% of youth with ASD in their sample met diagnostic criteria for generalized anxiety disorder relative to 20% of a typically developing outpatient comparison group. Social anxiety appears to occur at higher rates in youth with ASD than in the typically developing population, with results from a number of studies indicating 20–57% of children and adolescents with high-functioning ASD exhibit clinically relevant symptoms of social anxiety, as compared to 1–5% in typically developing youth (Kuusikko et al., 2008; Muris, Steerneman, Merckelbach, Holdrinet, & Meesters, 1998). Also, findings are emerging that youth with ASD who demonstrate higher cognitive and functioning levels may be more susceptible to developing anxiety disorders and experience greater symptom severity (Sukhodolsky et al., 2008; Weisbrot, Gadow, DeVincent, & Pomeroy, 2005); however, others have not observed such a trend (Kim et al., 2000; Pearson et al., 2006).
The high occurrence of comorbid anxiety disorders in ASD has raised some concerns about the validity of diagnosis and assessment methods with this population. Wood and Gadow (2010) underscore that diagnostic methods need to be refined to tease apart anxiety and core ASD symptoms in order to improve differential diagnosis and obtain more accurate prevalence rates. For example, they suggest taking into account the emotional valence of symptoms when differentiating between obsessive-compulsive symptoms and ASD-related restricted interests and ritualistic behaviors. Positive affect is more likely to be associated with restricted interests than with disturbing OCD-related obsessions. They also point out that anxiety in ASD can be phenotypically identical to the anxiety disorders in non-ASD groups, but it can also uniquely manifest stemming from the interplay between ASD core symptoms and anxiety (e.g., anxiety stemming from a child prevented from engaging in autistic routines). Accurate diagnosis will inform treatment development and ensure appropriate access to mental health services for children on the autism spectrum.
The extant research presents strong evidence that comorbid anxiety disorders have direct implications for the overall functioning and quality of life of youth with ASD and their families (Matson & Nebel-Schwalm, 2007). Youth with comorbid mood or anxiety were found to engage in increased aggression and oppositional behaviors and experience poorer social relationships compared to youngsters with ASD who did not have such comorbidities (Kim et al., 2000). Other functional impairments such as poor social responsiveness and social skill deficits have been associated (Bellini, 2004; Sukhodolsky et al., 2008). The relationship between the presence of anxiety and overall impairment in affected youth underscores the importance of treatments to relieve such symptoms.
Potential Contributing Factors
The most common hypotheses to explain the high occurrence of psychiatric comorbidity in ASD have been: (a) that there may be a common genetic linkage between ASD and other psychiatric disorders, increasing the risk of each (e.g., Gadow, Roohi, DeVincent, Kirsch, & Hatchwell, 2009), (b) that the stresses caused by having ASD (e.g., social rejection, sensory over-responsiveness, confusion in light of communication challenges) overwhelm coping skills and induce emotional and behavioral disorders (e.g., Meyer, Mundy, Van Hecke, & Durocher, 2006), or (c) that core autism symptoms are sometimes “counted as” aspects of a comorbid disorder that has phenotypically similar features (Gillott, Furniss, & Walter, 2001; Wood & Gadow, 2010).
A cognitive-behavioral model of psychopathology in high-functioning youth with ASD provides a framework for understanding the development and treatment of co-occurring anxiety. The interaction between behavioral, environmental, and cognitive factors may explain the clinical presentation of youth in this population. The combination of their increased intellectual capabilities (capacity for insight) and ASD features likely contribute to the development of maladaptive schemas (e.g., low self-efficacy; Bandura, Adams, & Beyer, 1977), limited coping strategies, and shape anxiety symptomology.
Similar to typically developing children, categorical psychosocial stressors such as parental discord or peer victimization (Shytayermman, 2007) have been associated with increased emotional stress in youth with ASD. Higher anxiety levels have been linked to the presence of such stressors, impaired behavioral flexibility to minor life changes, and a decreased ability to manage resulting emotions (Evans, Canavera, Kleinpeter, Maccubbin, & Taga, 2005; Green et al., 2006; Tantam, 2000). Biological factors such as an inhibited temperament style in ASD (Bellini, 2006) and a familial predisposition for psychiatric conditions (Ghaziuddin, Ghaziuddin, & Greden, 2002) also seem to contribute to these risk factors. Impairments associated with core ASD features likely limit the repertoire of coping skills to effectively manage emotional disturbance associated with adverse life experiences.
High-functioning youth with ASD have a capacity for awareness of their social-communicative limitations (Meyer et al., 2006). Children with Asperger Syndrome endorsed greater social worries relative to typically developing peers (Russell & Sofronoff, 2005). Severity of generalized anxiety symptoms is more pronounced in Asperger disorder relative to high-functioning autism (Thede & Coolidge, 2007). Contrary to the belief that youth with ASD are satisfied being alone, affected children endorse greater social difficulty, social distress, dissatisfactory interpersonal relationships, and decreased social competency relative to a matched control group of children diagnosed with learning disabilities (Burnette et al., 2005) and typically developing peers (Bauminger & Kasari, 2000). Youth with ASD likely experience great distress and concern with interpersonal relationships.
Adaptive functioning impairments can also contribute to poor social-emotional functioning. Youth with high-functioning ASD demonstrated adaptive functioning levels markedly below their cognitive potential (Klin, Saulnier, et al., 2007) and only 50% of a clinical sample of individuals with ASD independently completed basic self-care needs such as grooming (Green, Gilchrist, Burton, & Cox, 2000). Anxiety symptoms likely compound these deficits given that even among typically developing children diagnosed with separation anxiety disorder, decreased adaptive living skills was positively correlated with anxiety severity (Wood, 2006). Youngsters with ASD seem to lack the social self-sufficiency or “real-life skills” to lead independent lives, highlighting the importance of incorporating these skills into intervention.
The meditational role of cognition may influence the development of maladaptive beliefs in ASD. Difficulties with perspective taking, drawing inferences from contextual information, and executive functioning can contribute to social-emotional issues in ASD; however, further research exploring this area is necessary (Meyer et al., 2006; Thede & Coolidge, 2007). Similar to typically developing children with social-emotional disturbances (Dodge, 1993), youth with ASD displaying greater atypical social attribution processes and a hostile attribution bias (tendency to attribute hostile intent in others) were more likely to endorse anxiety and depression symptoms (Meyer et al., 2006).
Treatment Approaches
Cognitive-behavioral therapy (CBT) is an effective form of treatment for typically developing youth with childhood anxiety disorders (Barrett, Duffy, Dadds, & Rapee, 2001; Gosch, Flannery-Schroeder, Mauro, & Compton, 2006; Kendall, 1994; Walkup et al., 2008; Wood, 2006), particularly those incorporating family-based approaches (e.g., Wood, Piacentini, Southam-Gerow, Chu, & Sigman, 2006). According to this treatment approach, the theory of change primarily focuses on cognitive and behavioral mechanisms for symptom improvement. The main components of CBT for children include psychoeducation; developing coping skills (e.g., awareness of anxiety feelings, cognitive restructuring); and applying skills in graduated in vivo exposures (e.g., Kendall, 1994). An integral aspect to CBT is that children collaborate with clinical guidance to actively engage in empirical and logical question-asking and evaluation of anxiety-related situations through sequential and graduated experiences. Exposures are a core element as it provides mechanisms for hierarchical counterconditioning, extinction and habituation, thereby altering children’s expectations of themselves and others (Gosch et al., 2006). Kendall et al. (1997) showed that in typically developing youth cognitive intervention aspects of the treatment (e.g., challenging irrational beliefs) alone—when not paired with in vivo exposure elements—was not effective in reducing children’s anxiety levels.
Contemporary CBT methods promote the development of schemas that guide adaptive responses while suppressing maladaptive ones. Generally, schemas are underlying mental frameworks or memory representations that broadly encompass an individual’s network of attitudes, emotional associations, and episodic memories linked with a concept or situation. This notion of a schema differs from those that may be more specific to the patterns of thinking styles and cognitive models associated with particular psychological disorders such as depression (e.g., Beck, 1987). One model of memory retrieval competition in CBT (Brewin, 2006) suggests that adaptive schemas may need to be encoded with positive information and rehearsed in relevant situations in order to successfully be retrieved over coexisting maladaptive ones. The development of salient adaptive schema can be enhanced by elaborated rehearsal of such adaptive responses through deep semantic processing using active discussion, practice of skills within settings to encode schema relevant to actual situations, and incorporating emotionally positive elements such as humor.
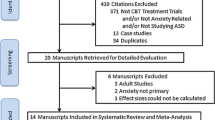
Research on the efficacy of CBT in reducing comorbid anxiety in youth with high-functioning ASD and Asperger’s disorder has been promising and spans from case studies (Lehmkuhl, Storch, Bodfish, & Geffken, 2008; Reaven & Hepburn, 2003; Sze & Wood, 2008) to group-design clinical studies (e.g., Reaven et al., 2009; Sofronoff, Attwood, & Hinton, 2005; Wood et al., 2009). The established efficacy of CBT for the treatment of childhood anxiety disorders in typically developing youth has served as a foundation for the development of this intervention for children and adolescents with ASD. Due to the complex clinical presentation of ASD and unique cognitive and emotional profile of this group of youth, modifications to the implementation of treatment have been evident across studies. The general consensus in modifying traditional CBT highlights the importance of tailoring CBT to meet the clinical needs of children with ASD to maximize the uptake and active use of coping skills. Some modifications to standard CBT methods for comorbid anxiety include the incorporation of visual aids (e.g., cartoons and thought bubbles) to supplement discussion of clinical material with the child, increased instruction on emotion recognition (self-awareness of anxiety symptoms), and clear and concrete presentation of ideas and materials (breaking down abstract ideas, direct and explicit directions). Reaven et al. (2009) modified CBT to treat anxiety in children with ASD in an unrandomized, open enrollment of a 12-week group intervention that included individual child, individual parent, and conjoint parent–child components. The authors drew upon several existing CBT manuals to develop an original program to accommodate ASD. They incorporated visual and concrete approaches to teach coping skills, emphasized drawing, photography, and video modeling to enhance generalization of skills and concepts. The results from their study demonstrated an improvement in anxiety symptoms in the active treatment group in comparison to the waitlist group. Trials of CBT conducted with typically developing children and youth with anxiety disorders (e.g., Barrett, Dadds, & Rapee, 1996) indicate that including parent training in the intervention can lead to superior intervention effects as compared to exclusively child-focused treatments. Sofronoff et al. (2005) found evidence that a CBT program for children with ASD and anxiety that included a combined child and parent treatment was more effective than working with children alone. Also, CBT programs for individuals with ASD and high anxiety in the current literature vary widely with regard to the emphasis placed on in vivo exposure relative to less active treatment elements (e.g., role-playing). Only a few intervention studies included in vivo exposures on a daily basis (e.g., Wood et al., 2009).
Some researchers have remarked that modifications to CBT, alone, may not fully address the expression of anxiety in ASD (Reaven et al., 2009; White et al., 2009; Wood et al., 2009). CBT interventions for anxiety in ASD are based on treatment that was initially developed for typically developing children, potentially limiting the efficacy of treatment. Some have questioned whether CBT for anxiety in children with ASD should be tailored specifically for this group (e.g., White et al., 2009). Current evidence suggests that despite this concern, CBT interventions have produced positive treatment gains in remediating anxiety in ASD. The effectiveness of CBT for children with ASD seems comparable to that observed in typically developing children with anxiety (e.g., Chalfant, Rapee, & Carroll, 2007) suggesting that some manifestations of anxiety in ASD may be similar to that in typically developing youth given the positive response to treatment. For example, up to 84% of children with ASD and co-occurring anxiety who received CBT with adjunctive family intervention (Chalfant et al., 2007; Wood et al., 2009) no longer met criteria for a primary anxiety disorder which was consistent with that observed in randomized clinical trials (RCT) of CBT for typically developing children with anxiety (e.g., Silverman et al., 1999; Storch et al., 2010). The basic elements of CBT are likely foundational components in treating anxiety disorders, applicable across populations.
The traditional model of CBT has been widened to develop interventions that are uniquely tailored to youth with ASD. Enhancement of CBT by expanding both treatment conceptualization and methods to go beyond the immediate implementational concerns (i.e., making the treatment materials and skills accessible) has given way to develop CBT that specifically targets ASD characteristics that could contribute to the manifestation of anxiety in order to enhance efficacy of treatment. The degree to which CBT has been expanded to meet the clinical needs of youth with ASD ranges on a continuum. Three RCTs for the treatment of anxiety in ASD currently exist in the literature (Chalfant, Rapee, & Carroll, 2007; Sofronoff et al., 2005; Wood et al., 2009). Additional RCTs are currently underway (e.g., White et al., 2010), including a multi-site investigation by the authors of this chapter in early adolescents with ASD and comorbid anxiety. All three of these studies had some methodological limitations, but overall, the results demonstrate a reduction in anxiety symptoms (with two of the more scientifically methodologically sound studies demonstrating that up to 71% of the children in treatment no longer met diagnostic criteria at the completion of CBT treatment) (Chalfant et al., 2007; Wood et al., 2009). More importantly, these studies employed methodological components (e.g., random assignment to conditions) that were consistent with the criteria necessary to establish empirically supported interventions (Chambless & Hollon, 1998). The RCTs will be described in more detail below in order of the increasing degree to which CBT was expanded. These exemplars will be used to demonstrate efficacy for the respective interventions and the specific adaptations that were made to the traditional model of CBT.
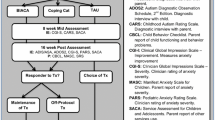
In the first example, Chalfant et al. (2007) developed an adapted CBT model that was tailored to accommodate the visual and concrete learning style of ASD. Forty-seven children aged 8–13 years-old diagnosed with high-functioning ASD were provided with group CBT and were randomly assigned to either immediate or wait-list conditions. The CBT was adapted from a program intended to treat core anxiety symptoms in typically developing children. The sessions were 2 h in duration and intervention was extended to 6 months (12 weekly sessions and three monthly booster sessions) to accommodate additional skill-building opportunities. Treatment effects were assessed with a structured diagnostic measure; child self-report measures; parent-report measures; and a teacher-report. Results at posttreatment revealed that about 71% of the children in the immediate treatment group no longer met criteria for a primary anxiety disorder in comparison to 0% of the youth in the wait-list group. Children in the CBT group demonstrated a greater reduction in the number of anxiety diagnoses from pre- to post-treatment and the self-, parent-, and teacher-reports generally showed that the CBT group reported significantly less internalizing thoughts about anxiety and self-esteem, reduced anxiety symptoms, and less emotional difficulties relative to the waitlist group. Some methodological concerns for this study were that independent evaluators blind to treatment assignment was not employed to administer the post-treatment diagnostic interviews and treatment fidelity was not examined.
Modifications to the CBT program were primarily in the presentation of materials and enhanced skill-building support through concurrent parent training. Specifically, Chalfant et al. (2007) sought to accommodate the visual and concrete learning style of youth with ASD. Visual aids and structured worksheets were used extensively for psychoeducation, anxiety symptom recognition, and skill-building of coping skills. For example, the youngsters were provided with worksheets to encircle their bodily feelings associated with anxiety from a list in order to alleviate demands on verbal skills. Cognitive restructuring activities (e.g., developing coping thoughts) were also simplified to accommodate language impairments. Concrete and behaviorally based activities were of focus through relaxation and exposure activities. However, the exposure activities were completed at home as sessions focused on planning exposure activities with the child and their family. No live coaching was provided to parents through in vivo exposures. Although parents completed a daily diary entry to record the outcomes of the home-based exposures, no checks were in place to validate the completion or fidelity of home-based exposures.
Parents were provided with a training program in parallel to their children’s group therapy. To supplement the development and practice of the children’s coping skills (e.g., parents providing exposure activities) the parent component was comprised of anxiety education and teaching relaxation strategies, cognitive restructuring exercises, graded exposure, parent management training for behavioral problems associated with anxiety, and relapse prevention. Conjoint parent–child sessions were not a part of this CBT model, providing little opportunity for direct practice or in vivo feedback from trained clinicians.
In the second example, Sofronoff et al. (2005) conducted an RCT with 71 children, ages 10–12 years, diagnosed with Asperger’s Disorder who were randomly assigned to: (a) child-based intervention, (b) combined child and parent intervention, or (c) waitlist condition. CBT was provided in 2-h sessions for 6 weeks in group therapy format. The child condition consisted of therapy provided in group format to children, with no parent training (parents were only informed of weekly assigned home-based exposures). In the child–parent condition, children received therapy in group format while parents also were trained to be “co-therapists” in parallel to the child sessions. These separate, concurrent parent sessions involved teaching parents intervention strategies and distal coaching on implementing exposures. Treatment effects were examined using an exploratory measure to assess for children’s self-generation of coping strategies and traditional parent-report measures.
Across measures, a significant improvement was observed in the CBT groups in comparison to the waitlist condition, with greater improvement observed in the parent–child intervention condition. Children in the CBT groups demonstrated an increased ability to generate coping strategies to a hypothetical scenario, and a significant reduction in the total number of anxiety symptoms and social worries relative to the waitlist group youth. However, this study lacked more rigorous diagnostic assessment, psychometrically sound measures, and methodology (e.g., did not employ independent evaluators). Interestingly, most of the significant changes in the measures were observed in follow-up (6 weeks after treatment was completed), rather than posttreatment. The authors cited that the children may have needed additional time to benefit from the coping strategies.
This treatment program went beyond modifying materials to make them more understandable to the youth (simplifying materials or using visual aids). Sofronoff et al. attempted to make the concepts more relatable and targeted a few core ASD areas implicated in compounding anxiety symptoms. First, the presentation of coping concepts and skills incorporated children’s special interests. For example, capitalizing on a common special interest in science among children with ASD, the youth in this intervention were given the role of a “scientist” or “astronaut” to practice and learn coping skills. Also, the metaphor of a tool box (tools to fix feelings, social tools, and thinking tools) was used in presenting coping strategies and emotion awareness. Second, social awareness about the behaviors of the children and other people around them within anxiety provoking situations was targeted. Last, the authors used cartoons and thought bubbles in relation to children’s anxiety-related scenarios that were borrowed from an intervention strategy used by youth with ASD to promote awareness and development of core social skills.
In the third example, Wood et al. (2009) significantly expanded upon traditional CBT by developing a comprehensive CBT model that emphasized treatment elements to target both core ASD features associated with anxiety symptomology. In this RCT, 40 children aged 7–11 years were randomized to either 16 weeks of 90 min sessions of a family-based CBT program plus 2 school consultation sessions or a waitlist. Treatment effects were assessed with a structured diagnostic interview; independent rating of improvement in anxiety (Clinical Global Improvement Scale (CGI-I)); and parent and child report of anxiety symptoms. The results showed large effect sizes for most outcome measures; remission of all anxiety disorders for more than 50% of the children in the immediate treatment group by posttreatment or follow-up; and a high rate of positive treatment response on the CGI-I (78.5% from intent-to-treat analyses). The children in the study had an average of 4.18 psychiatric disorders at intake, yet despite a high level of comorbidity, they demonstrated primary outcomes comparable to those of other studies treating childhood anxiety in typically developing patients (e.g., Barrett et al., 1996; Wood et al., 2006). For treatment completers, 64% of the children in the treatment group did not meet criteria for any anxiety disorder at posttreatment. Parent-reported anxiety symptoms also decreased significantly in the CBT group as compared to the waitlist group. However, child-reported anxiety did not differ significantly from pretreatment to follow-up. The authors described that a floor effect was expected, as baseline levels were low and decreased with treatment. This study had several methodologically rigorous elements including randomization and use of independent evaluators.
Wood et al. (2009) significantly enhanced the traditional CBT model by specifically targeting core ASD areas associated with the expression of anxiety in addition to making the CBT relatable to this group of children. In conjunction with the traditional coping skills training (developing coping thoughts) and in vivo exposure elements concerted efforts were made to treat both anxiety and associated ASD features. The core deficits of social-communication, perspective-taking skills, and the presence of idiosyncratic restricted interests and repetitive behaviors were actively targeted concurrently with anxiety symptoms. Social skills closely tied to anxiety and likely to interfere with the practice of more adaptive coping skills were addressed. For example, social skills deficits have been associated social anxiety in ASD (Bellini, 2006); therefore, Wood et al. used social coaching techniques to teach functional social skills to children and their parents. Specific strategies included the identification and practice of age-appropriate social overtures (e.g., joining in games with peers), friendship (e.g., listening to friends) and playdate hosting skills (e.g., playing flexibly, giving complements), reciprocal conversational skills, and perspective-taking skills (e.g., understanding the thoughts of peers). Peer intervention techniques (training peers to promote increased interactions with the target child) to develop positive peer relationships within naturalistic such as park and school were also implemented.
Wood et al. integrated the use of special interests into treatment. They specifically used special interests as motivators for treatment and as a medium for learning and practicing adaptive coping skills. For example, a child’s interest in cartoon characters was used as a reward for practicing coping skills and to develop thought bubbles about anxious and coping thoughts through related cartoons, which was drawn from the perspective that idiosyncratic interests and repetitive behaviors can be used to motivate children with ASD (Baker, Koegel, & Koegel, 1998). Engagement in these interests was gradually suppressed for increasing lengths of time through a contingency management plan to increase the likelihood that children would benefit from using functional and coping skills given that these behaviors can detrimentally interfere with functioning over time (Klin, Danovitch, Merz, & Volkmar, 2007).
Self-help skills necessary for daily, adaptive functioning was also an intervention enhancement. Poor adaptive skills associated with ASD (Howlin, Goode, Hutton, & Rutter, 2004) and impaired self-help skills in typically developing children with anxiety disorders (Wood, 2006) served as guiding posts to promote youth with ASD and their parents to practice age-appropriate self-help skills (e.g., showering independently). Wood et al. targeted comorbid externalizing symptoms associated with anxiety in children with ASD (Kim et al., 2000) by promoting children’s perspective of these behaviors (through role-play and Socratic Questioning) and developing a contingent reward plan for the gradual increased display of appropriate behaviors and use of emotional regulation strategies.
Child motivation and active treatment participation was also an element of the expanded CBT. The authors concentrated their efforts in parent participation, practice within natural settings to enhance generalization of skills, and continuously used rewards (e.g., access to playing videogames) and other positive experiences (humor, restricted interests) for the youth to actively participate in treatment. Parent- and teacher-training components were included to ensure that coping skills were employed in daily settings. The program incorporated these elements to maintain engagement and to promote the recall of adaptive responses that were informed through the long-established efficacy demonstrated by the literature on treatments targeting core ASD skill development (Hwang & Hughes, 2000; Koegel & Egel, 1979; Koegel, Koegel, & Brookman, 2003).
Integrating the treatment and efficacy considerations from the available research highlights a number of important aspects in treating anxiety in youth with ASD using CBT. First, at the most basic level, CBT must be presented in a way that is understandable to youth with ASD to ensure the uptake of concepts and skills. Presenting materials, concepts, and opportunities to practice both more adaptive coping thoughts and behaviors need to be modified to accommodate the learning profiles of children and adolescents with ASD. This largely has been accomplished through the use of visual aids (cartoons, lists, diagrams), increased structure in the sessions (developing predictable routines in the layout of the sessions), presenting concepts using clear, explicit, and simple language, and increased practice identifying and recognizing emotional and body feelings related to anxiety. Second, CBT concepts and skills should be made relatable to children with ASD to increase the likelihood of their active participation in treatment and generalization of skills in real world settings. This requires going beyond the simple modification of materials by individualizing treatment and incorporating elements of these children’s interests to serve as a medium for developing skills and capitalize on the motivational and reinforcing properties of special interests in ASD. Additionally, it requires skill building through in vivo exposures in naturalistic settings rather than through more distal role-play or limited to a clinic setting. Practice and mastery in real world settings will make the skills relatable to children with ASD and develop adaptive schemas that are relevant to their lives and likely to be employed by the children in actual situations. Parent training components also ensure that the skills will be practiced by the children and make the concepts and skills relevant to both the family and the child. Third, enhancement of CBT for youth with ASD also requires going a step further to address the complex integration between anxiety expression and core ASD features. It is clear from the research that anxiety can be manifested in a unique way in ASD. Although anxiety can be expressed in prototypical form similar to non-ASD cases of anxiety, anxiety seems to have a reciprocal, dynamic relationship with core ASD features. Anxiety can exacerbate core ASD features and ASD characteristics can contribute to anxiety expression. Therefore, in the case of CBT for youth with ASD, additional components of treating this unique intersection of anxiety and ASD characteristics seems to be an integral aspect of treatment for this group. In tandem with core CBT skills of cognitive restructuring and mastering coping skills, social-communicative skill enhancement (e.g., conversation skills or playdate skills), mastery of age-appropriate adaptive skills, development of flexibility in interests and the ability to suppress restricted interests when necessary are some behaviors that can be promoted and acquired alongside traditional CBT skills. Increased research in both the theoretical understanding of ASD and anxiety and components associated with efficacious treatment will further guide the field in ensuring that children with ASD receive effective interventions.
Case Study
Case description. Oliver was an 8-year-old boy who attended the second grade at a local public elementary school. He was fully included in the general education classroom with support from a one-to-one aide. Oliver was diagnosed with high-functioning autism at age 3. He was referred for psychosocial treatment by his psychiatrist due to impairing symptoms of anxiety. A modified and enhanced family-based CBT program (Wood & McLeod, 2008) was provided consisting of 16, 90-min sessions, one follow-up booster session, and two school visits. Each session consisted of individual child, individual parent, and conjoint child–parent portions.
Clinical profile. Oliver met diagnostic criteria for three anxiety disorders: social anxiety, separation anxiety, and obsessive-compulsive disorder. He exhibited significant apprehension about social interactions and negative social evaluation. As a result, he avoided partaking in age-appropriate activities (e.g., class participation). Distress in social situations further compounded his ASD-related social deficits, preventing him from developing friendships at school. Also, he presented with significant anxiety towards separation from his mother, endorsing fears that either he or his mother would be harmed or “stolen.” For example, Oliver exhibited excessive clinginess around his mother and engaged in co-sleeping with his parents. With regard to OCD, his obsessions included repeated and unwanted thoughts about the number six, the color red, contracting germs, and distressing images of a pony character from a cartoon he enjoyed watching. He experienced times when mental images of the pony became intrusive and distressing. Compulsions included repeated handwashing, hoarding trash, and a set of ritualistic behaviors he felt compelled to perform “just right” involving his stuffed animal. Consistent with ASD symptoms, Oliver demonstrated impairments with reciprocal social interactions (i.e., lack of shared enjoyment), communication (i.e., difficulty sustaining conversations), and stereotyped interests and behaviors (i.e., occasional hand flapping). His special interests were related to vehicles, science, and cartoons intended for a younger audience. Oliver’s adaptive skills were below age expectations.
Sessions 1–3: building coping and independence skills. The general focus was on establishing rapport, providing psychoeducation on the nature of ASD and anxiety, collecting information on anxiety symptoms, and providing an overview of the CBT program. Oliver and his mother were taught core cognitive restructuring skills (recognizing anxiety feelings, identifying anxious thoughts, developing coping thoughts, and the concept of gradually facing fears). Rapport building focused on identifying Oliver’s interests. A functional assessment of Oliver’s ASD features and anxiety was conducted. His mother identified his current level of adaptive skills and selected age-appropriate target skills, focusing on private self-care tasks (self-grooming). She was taught key parenting communication strategies (providing choices, gradually fading assistance). Oliver’s mother identified powerful rewards ranging from daily to longer term incentives to use throughout the program to increase his motivation for completing CBT assignments.
Oliver was encouraged to indicate his preference for labeling anxiety (he preferred the term “scared” and endorsed feeling “hot” when worried). Systematic Socratic questioning was employed to recognize bodily cues, challenge anxious cognitions (“The pony might get me”), develop adaptive coping thoughts (“The pony is a silly cartoon, so it can’t harm me!”), and incrementally face feared situations with the aid of cartoon-based stories involving his special interests relevant to anxiety-provoking scenarios.
Sessions 4–5: development of the hierarchy and treatment plan. The focus was on providing an overview of exposure therapy, developing the exposure hierarchy, and implementing an incentive system. Oliver and his mother were presented with a list of fearful situations based on his diagnostic interview and information from the initial sessions. They provided ratings for each item on the hierarchy that included both anxiety and ASD-related symptoms (e.g., talking about his special interests). Coaching was provided to his mother to plan, negotiate, and complete exposures.
Sessions 6–15: comprehensive skill application in real world settings. The focus was on conducting in vivo and home-based exposures and monitoring the reward system. Concurrently, skills compromised by core ASD symptomology such as appropriate social entry behaviors (e.g., joining games) were targeted towards the middle of the treatment phase. Items rated as easier on his hierarchy were first attempted; steadily including several items from across anxiety domains. Cognitive restructuring was practiced both in session and at home to develop coping and parent communication skills. Home-based exposures served as extensions of in-session exposures. Given his interest in science, he was encouraged to think about exposures as a way to go about “busting myths.” Homework gradually targeted multiple anxiety symptoms, self-care areas, and ASD-related deficits.
Social coaching intervention was provided to the parent and child. First, role-playing of typical social exchanges between Oliver and his peers was practiced in the session and at home (e.g., asking to join in a game). Then, his mother was encouraged to consider social coaching as a long-term strategy; look for naturalistic opportunities to practice positive social exchanges in the community (during school drop off and pick up); and provide him with positive feedback for practicing social and coping skills in real world situations.
Oliver was taught friendship skills of hosting playdates with peers. His mother was taught skills to foster Oliver’s friendships and identify potential friends for playdates. Oliver was introduced to and practiced the rules of a good host (provide compliments, stay with the friend, and play flexibly by allowing the friend to choose the games). He was asked to select peers, make phone calls to invite them, and host playdates as part of his ongoing CBT homework.
Oliver’s mother was taught strategies for increasing Oliver’s age-appropriate activities. She was encouraged to raise Oliver’s interest in age-appropriate TV shows enjoyed by most children his age. His interest in idiosyncratic topics and immature activities gradually diminished over time by rewarding him for increasing lengths of time in which he did not engage in these behaviors or engaged in more appropriate activities. He was gradually asked to refrain from watching preschool cartoons or talking about them for 1 day. He was rewarded for watching or discussing more age-appropriate topics.
The last phase of treatment involved a school observation, developing school-based exposures and home-school notes, and training relevant adults in the school setting. Social coaching was introduced to and implemented by his one-to-one aide during recess and lunch in the context of naturally occurring peer exchanges.
Session 16: termination. Treatment progress was reviewed with both parent and child during which they planned future home-based exposures to practice coping skills, self-care, and ASD-related skill development.
Session 17: follow-up. The purpose was to maintain Oliver’s treatment gains and prevent symptom relapse through progress review and problem-solving to address new areas of anxiety in a collaborative manner.
Treatment outcome. Oliver no longer met diagnostic criteria for any of the three anxiety diagnoses. For example, obsessions related to cartoon characters remitted and he did not engage in compulsive hoarding. He made gains in friendships, as evidenced by an increased number of playdates in which he had the opportunity to play the role of host and guest. Overall, his anxiety and related ASD symptoms improved to the extent to which they became manageable, increasing his quality of life and functioning.
Conclusion and Future Directions
Anxiety at clinical levels is a phenomenon that occurs at high rates in youth with ASD and requires treatment. It is becoming increasingly evident that in order to accommodate the complexity of anxiety expression in ASD, CBT must be tailored to complement and meet the needs of youth in this population. Traditional CBT has provided solid foundations for the effective treatment of anxiety in typically developing children and those with ASD. Similar to the growing consideration in the field for more refined diagnostic methods to identify comorbid anxiety diagnoses, the development of CBT programs for anxiety in ASD is continuing to evolve with the growing fund of knowledge in the field. Children and adolescents with ASDs are susceptible to anxiety disorders and require and deserve appropriate treatment to promote their psychological well-being. The advancement of enhanced CBT interventions should be guided by research on the development of anxiety in both typically developing children and youth with ASD, paired with findings from both psychosocial and behavioral treatments for youth on the autism spectrum. In this way, CBT can have a lasting and meaningful impact on youth with ASD and concurrent anxiety.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Task Force.
Baker, M. J., Koegel, R. L., & Koegel, L. K. (1998). Increasing the social behavior of young children with autism using their obsessive behaviors. Journal of the Association for Persons with Severe Handicaps, 23, 300–308.
Bandura, A., Adams, N. E., & Beyer, J. (1977). Cognitive processes mediating behavioral change. Journal of Personality and Social Psychology, 35(3), 125–139.
Barrett, P. M., Dadds, M. R., & Rapee, R. M. (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342.
Barrett, P. M., Duffy, A. L., Dadds, M. R., & Rapee, R. M. (2001). Cognitive-behavioral treatment of anxiety disorders in children: Long-term (6-year) follow-up. Journal of Consulting and Clinical Psychology, 69(1), 135–141.
Bauminger, N., & Kasari, C. (2000). Loneliness and friendship in high-functioning children with autism. Child Development, 71(2), 447–456.
Beck, A. T. (1987). Cognitive models of depression. Journal of Cognitive Psychotherapy, 1(1), 5–37.
Bellini, S. (2004). Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disorders, 19, 78–86.
Bellini, S. (2006). The development of social anxiety in adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 21, 138–145.
Brewin, C. R. (2006). Understanding cognitive behaviour therapy: A retrieval competition account. Behaviour Research and Therapy, 44, 765–784.
Burnette, C. P., Mundy, P. C., Meyer, J. A., Sutton, S. K., Vaughan, A. E., & Charak, D. (2005). Weak central coherence and its relations to theory of mind and anxiety in autism. Journal of Autism and Developmental Disorders, 35(1), 63–73.
Chalfant, A. M., Rapee, R., & Carroll, L. (2007). Treating anxiety disorders in children with high functioning autism spectrum disorders: A controlled trial. Journal of Autism and Developmental Disorders, 37, 1842–1857.
Chambless, D. L., & Hollon, S. D. (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 66, 7–18.
de Bruin, E. I., Ferdinand, R. F., Meester, S., de Nijs, P. F., & Verheij, F. (2007). High rates of psychiatric co-morbidity in PDD-NOS. Journal of Autism and Developmental Disorders, 37, 877–886.
Dodge, K. A. (1993). Social-cognitive mechanisms in the development of conduct disorder and depression. Annual Review of Psychology, 44, 559–584.
Evans, D. W., Canavera, K., Kleinpeter, F. L., Maccubbin, E., & Taga, K. (2005). The fears, phobias and anxieties of children with autism spectrum disorders and down syndrome: Comparisons with developmentally and chronologically age matched children. Child Psychiatry and Human Development, 36(1), 3–26.
Gadow, K. D., Devincent, C. J., Pomeroy, J., & Azizian, A. (2005). Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism, 9(4), 392–415.
Gadow, K. D., Roohi, J., DeVincent, C. J., Kirsch, S., & Hatchwell, E. (2009). Association of COMT (Val158Met) and BDNF (Val66Met) gene polymorphisms with anxiety, ADHD, and tics in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 39(11), 1542–1551.
Ghaziuddin, M., Ghaziuddin, N., & Greden, J. (2002). Depression in persons with autism: Implications for research and clinical care. Journal of Autism and Developmental Disorders, 32(4), 299–306.
Gillott, A., Furniss, F., & Walter, A. (2001). Anxiety in high-functioning children with autism. Autism, 5(3), 277–286.
Gosch, E. A., Flannery-Schroeder, E., Mauro, C. F., & Compton, S. N. (2006). Principles of cognitive-behavioral therapy for anxiety disorders in children. Journal of Cognitive Psychotherapy, 20(3), 247–262.
Green, J., Gilchrist, A., Burton, D., & Cox, A. (2000). Social and psychiatric functioning in adolescents with Asperger syndrome compared with conduct disorder. Journal of Autism and Developmental Disorders, 30(4), 279–293.
Green, V. A., Sigafoos, J., Pituch, K. A., Itchon, J., O’Reilly, M., & Lancioni, G. E. (2006). Assessing behavioral flexibility in individuals with developmental disabilities. Focus on Autism and Other Developmental Disabilities, 21(4), 230–236.
Howlin, P., Goode, S., Hutton, J., & Rutter, M. (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 45(2), 212–229.
Hwang, B., & Hughes, C. (2000). The effects of social interactive training on early social communicative skills of children with autism. Journal of Autism and Developmental Disorders, 30(4), 331–343.
Kendall, P. C. (1994). Treating anxiety disorders in children: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 62, 100–110.
Kendall, P. C., Flannery-Schroeder, E., Panichelli-Mindel, S. M., Southam-Gerow, M., Henin, A., & Warman, M. (1997). Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology, 65, 366–380.
Kim, J. A., Szatmari, P., Bryson, S. E., Streiner, D. L., & Wilson, F. J. (2000). The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism, 4(2), 117–132.
Klin, A., Danovitch, J., Merz, A., & Volkmar, F. (2007). Circumscribed interests in higher functioning individuals with autism spectrum disorders: An exploratory study. Research and Practice for Persons with Severe Disabilities, 32, 89–100.
Klin, A., Saulnier, C. A., Sparrow, S. S., Cicchetti, D. V., Volkmar, F. R., & Lord, C. (2007). Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: The Vineland and the ADOS. Journal of Autism and Developmental Disorders, 37(4), 748–759.
Koegel, R. L., & Egel, A. L. (1979). Motivating autistic children. Journal of Abnormal Psychology, 88, 418–426.
Koegel, R. L., Koegel, L. K., & Brookman, L. I. (2003). Empirically supported pivotal response interventions for children with autism. In A. E. Kazdin & J. R. Weisz (Eds.), Evidence-based psychotherapies for children and adolescents. New York: Guilford.
Kuusikko, S., Pollock-Wurman, R., Jussila, K., Carter, A. S., Mattila, M., Ebeling, H., et al. (2008). Social anxiety in high-functioning children and adolescents with autism and Asperger syndrome. Journal of Autism and Developmental Disorders, 39(9), 1697–1709.
Lecavalier, L. (2006). Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders, 36(8), 1101–1114.
Lehmkuhl, H. D., Storch, E. A., Bodfish, J. W., & Geffken, G. R. (2008). Brief report: Exposure and response prevention for obsessive compulsive disorder in a 12 year-old with autism. Journal of Autism and Developmental Disorders, 38, 977–981.
Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36(7), 849–861.
Matson, J. L., & Nebel-Schwalm, M. S. (2007). Comorbid psychopathology with autism spectrum disorder in children: An overview. Research in Developmental Disabilities, 28(4), 341–352.
Meyer, J. A., Mundy, P. C., Van Hecke, A. V., & Durocher, J. S. (2006). Social attribution processes and comorbid psychiatric symptoms in children with Asperger syndrome. Autism, 10(4), 383–402.
Muris, P., Steerneman, P., Merckelbach, H., Holdrinet, I., & Meesters, C. (1998). Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders, 12, 387–393.
Pearson, D. A., Loveland, K. A., Lachar, D., Lane, D. M., Reddoch, S. L., Mansour, R., et al. (2006). A comparison of behavioral and emotional functioning in children and adolescents with autistic disorder and PDD-NOS. Child Neuropsychology, 12(4–5), 321–333.
Reaven, J. A., Blakeley-Smith, A., Nichols, S., Dasari, M., Flanigan, E., & Hepburn, S. (2009). Cognitive-behavioral group treatment for anxiety symptoms in children with high-functioning autism spectrum disorders: A pilot study. Focus on Autism and Other Developmental Disabilities, 24, 27–37.
Reaven, J., & Hepburn, S. (2003). Cognitive-behavioral treatment of obsessive-compulsive disorder in a child with Asperger syndrome: A case report. Autism, 7(2), 145–164.
Russell, E., & Sofronoff, K. (2005). Anxiety and social worries in children with Asperger syndrome. The Australian and New Zealand Journal of Psychiatry, 39(7), 633–638.
Shytayermman, O. (2007). Peer victimization in adolescents and young adults with Asperger’s syndrome: A link to depressive symptomatology, anxiety symptomatology, and suicidal ideation. Issues in Comprehensive Pediatric Nursing, 30(3), 87–107.
Silverman, W. K., Kurtines, W. M., Ginsburg, G. S., Weems, C. F., Lumpkin, P. W., & Carmichael, D. H. (1999). Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67(6), 995–1003.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929.
Sofronoff, K., Attwood, T., Hinton, S. (2005). A randomised controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry, 46, 1152–1160.
Storch, E. A., Lehmkuhl, H. D., Ricketts, E., Geffken, G. R., Marien, W., & Murphy, T. K. (2010). An open trial of intensive family based cognitive-behavioral therapy in youth with obsessive-compulsive disorder who are medication partial responders or nonresponders. Journal of Clinical Child and Adolescent Psychology, 39(2), 260–268.
Sukhodolsky, D. G., Scahill, L., Gadow, K. D., Arnold, L. E., Aman, M. G., McDougle, C. J., et al. (2008). Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology, 36(1), 117–128.
Sze, K. M., & Wood, J. J. (2008). Enhancing CBT for the treatment of autism spectrum disorders and concurrent anxiety: A case study. Behavioural and Cognitive Psychotherapy, 36, 403–409.
Tantam, D. (2000). Psychological disorder in adolescents and adults with Asperger syndrome. Autism, 4(1), 47–62.
Thede, L. L., & Coolidge, F. L. (2007). Psychological and neurobehavioral comparisons of children with Asperger’s disorder versus high-functioning autism. Journal of Autism and Developmental Disorders, 37(5), 847–854.
Walkup, J. T., Albano, A. M., Piacentini, J., Birmaher, B., Compton, S. N., Sherill, J. T., et al. (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine, 359, 2753–2766.
Weisbrot, D. M., Gadow, K. D., DeVincent, C. J., & Pomeroy, J. (2005). The presentation of anxiety in children with pervasive developmental disorders. Journal of Child and Adolescent Psychopharmacology, 15(3), 477–496.
White, S. W., Albano, A. M., Johnson, C. R., Kasari, C., Ollendick, T., Klin, A., et al. (2010). Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clinical Child and Family Psychology Review, 13(1), 77–90.
White, S. W., Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229.
Wood, J. J. (2006). Parental intrusiveness and children’s separation anxiety in a clinical sample. Child Psychiatry and Human Development, 37(1), 73–87.
Wood, J. J., Drahota, A., Sze, K., Van Dyke, M., Decker, K., Fujii, C., et al. (2009). Brief report: Effects of cognitive behavioral therapy on parent-reported autism symptoms in school-age children with high-functioning autism. Journal of Autism and Developmental Disorders, 39, 1609–1612.
Wood, J. J., & Gadow, K. D. (2010). Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology: Science and Practice, 17(4), 281–292.
Wood, J. J., Piacentini, J. C., Southam-Gerow, M., Chu, B. C., & Sigman, M. (2006). Family cognitive behavioral therapy for child anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 45(3), 314–321.
Wood, J. J., & McLeod, B. M. (2008). Child anxiety disorders: A treatment manual for practitioners. New York: Norton.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Lin, C.E., Wood, J.J., Storch, E.A., Sze, K.M. (2013). Treatment of Childhood Anxiety in Autism Spectrum Disorders. In: Storch, E., McKay, D. (eds) Handbook of Treating Variants and Complications in Anxiety Disorders. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6458-7_5
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6458-7_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6457-0
Online ISBN: 978-1-4614-6458-7
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)