Abstract
There are numerous pitfalls and artifacts in computed tomography colonography (CTC) interpretation. One must be cognizant of these in order not to overcall pathology and refer patients for unnecessary optical colonoscopies (OC). This chapter will demonstrate the most common pitfalls and artifacts associated with CTC interpretation and provide ways to best analyze and accurately assess these findings. At a minimum, a combined 3-D and 2-D analysis is required to adequately analyze and accurately interpret a CTC. In order to minimize artifacts, one must start with the best 3-D model possible. Many interpretation pitfalls and image artifacts can be avoided when attention is paid to proper patient preparation and image acquisition. A diagnostic quality CTC requires an adequate bowel cleansing prep, stool and fluid tagging with barium and water-soluble contrast agents, adequate patient hydration, mechanical CO2 insufflation of the colon, and optimal distension of all colon segments (Fig. 8.1a–d).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Source Image
- Compute Tomography Colonography
- Ileocecal Valve
- Optical Colonoscopy
- Pneumatosis Cystoides Intestinalis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
There are numerous pitfalls and artifacts in computed tomography colonography (CTC) interpretation. One must be cognizant of these in order not to overcall pathology and refer patients for unnecessary optical colonoscopies (OC). This chapter will demonstrate the most common pitfalls and artifacts associated with CTC interpretation and provide ways to best analyze and accurately assess these findings. At a minimum, a combined 3-D and 2-D analysis is required to adequately analyze and accurately interpret a CTC. In order to minimize artifacts, one must start with the best 3-D model possible. Many interpretation pitfalls and image artifacts can be avoided when attention is paid to proper patient preparation and image acquisition. A diagnostic quality CTC requires an adequate bowel cleansing prep, stool and fluid tagging with barium and water-soluble contrast agents, adequate patient hydration, mechanical CO2 insufflation of the colon, and optimal distension of all colon segments (Fig. 8.1a–d).
The artifacts associated with CTC interpretation can be considered in three major categories: (a) bowel preparation-related artifacts, (b) imaging-related pitfalls and artifacts, and (c) anatomical variants. Preparation-related pitfalls and artifacts include retained stool and fluid, retained dense and dilute contrast, and problems related to detection and measuring of submerged polyps. Imaging-related artifacts include segmental spasm, air–fluid interface artifact, electronic cleansing artifact, respiratory motion artifact, image noise or quantum mottle artifact, spray artifact, and data dropout. Anatomical variants include extrinsic compression effects from adjacent structures, stool-filled diverticula, flat and pedunculated polyps, lipomas, rectal veins, hemorrhoids, and variations of the ileocecal valve and appendix. Each of these will be addressed below.
Preparation-Related Pitfalls and Artifacts
All bowel preparations leave behind residual stool and fluid in the colon. Depending on the length and redundancy of the colon, this stool and fluid contamination may be significant. It is imperative that patients understand the significance of following the bowel preparation and stool tagging instructions so that optimal cleansing and tagging can be accomplished. The majority of retained stool and fluid can be adequately tagged and electronically subtracted in most patients. When there is significant stool and fluid contamination present, there may not be complete tagging and electronic cleansing. Large collections of stool contain small pockets of air and fecal fat that can be easily visualized on 2-D source images and attenuation color mapping (Fig. 8.2a–c). Even moderate-sized stool balls demonstrate this heterogeneous attenuation on 2-D source images and color mapping (Fig. 8.3a–c). Smaller stool balls, however, may not contain significant collections of air or fecal fat and therefore can mimic polyps. To distinguish these small stool balls from true polyps, one must look to the contour and mobility of the lesions in question. Stool balls have an angulated, squared, or facetted contour (Fig. 8.4a–c), and, unless adherent to the colon wall, fall to the dependent portion of the colon on prone and supine views (Fig. 8.5a–d). Figure 8.6a–h demonstrates varying degrees of stool contamination found on CTC.
Retained fluid within the colon can also significantly impair visualization of the colon wall and degrade polyp detection. When there is significant retained fluid present, oral contrast agents will be diluted down to a point below the cutoff for electronic cleansing. As a result, this dilute and tagged fluid will not be subtracted out. This can mask the dependent colon wall on the 3-D endoluminal views. Imaging of the colon in the prone and supine positions is performed in order to shift the dilute fluid to opposing dependent walls or to different segments of colon. This allows for visualization of the colon surface on at least one view (Fig. 8.7a–d). When diluted fluid fills the entire lumen of the colon, 3-D endoluminal visualization of the involved segment cannot be performed. With prone and supine imaging, however, the dilute fluid will typically shift and allow adequate visualization of the colon lumen on at least one view (Fig. 8.8a–f). If there is adequate luminal distension by the residual tagged fluid, the 2-D source CT images can be used to evaluate for polyps or masses. The 2-D source images should be viewed with the electronic cleansing algorithm turned off. Then, just like with solid column barium enema, polyps or masses will be visible as filling defects in the fluid pool on the 2-D CT images (Fig. 8.9a, b).
Images (a)–(d) demonstrate the problem with significant dilute fluid filling the entire lumen of the colon. In the prone position, fluid fills the mid-transverse colon preventing 3-D endoluminal visualization of that segment. In the supine position, the fluid moves to the ascending or descending colon, allowing for 3-D endoluminal visualization of the mid-transverse colon
Dense contrast collections may also decrease sensitivity for polyp detection. Droplets of desiccated barium can adhere to the colon wall and mimic sessile polyps on the endoluminal views. These droplets are usually seen in patients who did not maintain adequate hydration during the bowel preparation or who did not take the water-soluble contrast agent with the barium tagging agent. The water-soluble contrast agent is hyperosmolar and serves as a wetting agent in the colon, thereby preventing desiccation of the barium droplets on the colon surface. Desiccated barium droplets can be differentiated from true polyps by their high density on both the 2-D source images and colon window images. They make interpretation difficult only due to their increased number (Fig. 8.10a–c). Contrast tagged fluid surrounding submerged polyps can complicate detection and analysis of polyps. The electronic cleansing algorithms are not complete. They can distort the surface of the colon wall or polyp that abuts the tagged fluid. Due to this subtraction artifact, the surface of a submerged polyp may be irregular on the 3-D endoluminal views, mimicking the surface of stool. Polyps will maintain their normal smooth contour on the non-submerged endoluminal view. Evaluation of submerged polyps can be facilitated by again turning the subtraction algorithm off on the 2-D source images. The polyp will be seen as a filling defect in the tagged fluid on the 2-D source images (Fig. 8.11a–d).
Images (a)–(d) demonstrate the effect of the electronic cleansing algorithm on the surface contour of submerged polyps. Images (a) and (b) show the smooth surface contour of a non-submerged sessile polyp. Images (c) and (d) show the same polyp submerged in contrast. Note the irregular surface contour of the polyp on the 3-D endoluminal images
Polyp measurement is best obtained on the 3-D endoluminal images with the polyp free from surrounding tagged fluid (i.e., on the nondependent wall of the colon). Polyp measurements should be taken perpendicular to the base of the polyp and colon wall. Measurements taken of submerged polyps on the 3-D endoluminal views will underestimate the true size of the polyp (Fig. 8.12a, b).
The electronic cleansing algorithm will also distort the size of submerged polyps. Image (a) shows the measurements taken of a 5-mm sessile polyp on a nondependent wall of the colon. Image (b) shows the measurements taken on the same polyp submerged in retained fluid. The measurements taken on a submerged polyp greatly underestimate the actual size of that polyp
Preparation-related pitfalls and imaging artifacts can best be minimized with the utilization of a proper cathartic bowel preparation, stool and fluid tagging with electronic cleansing, and imaging the patient in the prone and supine positions. However, when faced with significant residual stool or fluid and contrast contamination, one can utilize the characteristic morphology and density of stool and dense contrast coupled with the physics of prone and supine positioning to help differentiate true polyps from contamination. Using the 2-D source images with the cleansing algorithm turned off can help in detecting polyps when there is complete filling of the colon lumen by tagged fluid. Finally, by understanding the effects of residual fluid on submerged polyps, one can accurately identify and measure these lesions.
Imaging-Related Pitfalls and Artifacts
There are multiple pitfalls and artifacts related to the actual imaging of the CTC patient. Some of these artifacts and pitfalls can be minimized with proper imaging techniques. Others are the inevitable by-product of the standard low-dose technique used for this screening study and the imaging properties of CT. Luminal narrowing, segmental collapse, air–fluid interface artifact, electronic cleansing or subtraction artifact, image noise artifact, spray artifact, and data dropout are the major imaging-related pitfalls and artifacts. Each of these will be addressed below.
Adequate colon distension is critical for proper 3-D model building. Inadequate distension leads to luminal narrowing or frank segmental collapse. Luminal narrowing produces thickening of the colonic folds, which, if focal enough, can mimic a polyp. This is especially true when evaluating for polyps on the 2-D source images. True fold thickening, in contrast to adherent stool/barium or a sessile polyp, should be uniform in caliber and smooth. It is usually found on the inside curve of a flexure or a turn of the sigmoid or transverse colon (Fig. 8.13a–f). Segmental narrowing can result from spasm, colon cancer, diverticulosis, scarring from prior surgery, radiation, or inflammation (Fig. 8.14a–f). Figure 8.15a, b demonstrates a stent placed across a known colon cancer in the descending colon. Suboptimal distension of the colon requires an intense 3-D and 2-D analysis of the involved segments to exclude underlying polyps or masses.
Two examples of segmental narrowing. Images (a)–(c) demonstrate an annular constricting mass with overhanging edges in the distal sigmoid colon that turned out to be an adenocarcinoma. Images (d)–(f) demonstrate segmental narrowing in the sigmoid colon secondary to diverticulosis with secondary muscular hypertrophy and spasm
Frank collapse secondary to focal spasm results in total loss of visualization of the colon lumen on both the 3-D and 2-D images. Significant polyps or masses cannot be excluded from these segments. If the segmental collapse involves the same segment on both the supine and prone series, then this constitutes an incomplete CTC (Fig. 8.16a, b). Tailoring the exam to the patient’s anatomy can minimize luminal narrowing and segmental collapse. Obtaining a scout image or representative preliminary slices through the abdomen and pelvis prior to scanning the patient allows the CT technologist to verify maximal distention of the colon. Review of the scout images may also result in the detection of pathology outside of the colon (Fig. 8.17a–d). If narrowed or collapsed segments are identified on the scout view or preliminary slices, placing the patient in a decubitus or oblique position and re-insufflating the colon may adequately distend the narrowed or collapsed segments identified (Fig. 8.18a–f).
Images (a) and (b) are scout images from a CTC which demonstrate adequate CO2 distension of the entire colon on both the prone and supine series. Obtaining scout images or representative preliminary slices through the abdomen and pelvis prior to imaging the patient helps to guarantee maximal distension of the colon during imaging. Review of the scout images may also detect pathology outside of the colon. The supine scout on this patient demonstrates a clinically occult right upper lobe pulmonary mass. Images (c) and (d) demonstrate a diagnostic quality 3-D model of the colon on both the prone and supine series. The colon is adequately inflated on both views, and a continuous virtual flight path (demarcated by the green line) has been established from the rectum to the cecum on both the prone and supine series
Large air–fluid levels in the colon can lead to an air–fluid interface artifact within the lumen of the colon that can obscure portions of the colon wall. Manual fly-through both above and below this artifact on the 3-D views, as well as careful analysis of the 2-D source images, is required to adequately evaluate the involved segment (Fig. 8.19a–d). Stool and fluid cleansing algorithms, in addition to distorting the contour of submerged polyps, can produce irregularities in the colon wall itself. Electronically cleansed pools of fluid leave a “bathtub ring” type of irregularity on the dependent wall of the colon (Fig. 8.20a–d). Thin folds submerged in tagged fluid can have significant erosions of the apex of the fold (Fig. 8.21a–d). If tagged fluid is present in adjacent segments of bowel, the contiguous walls may be subtracted out together producing a communicating hole between the two segments of the bowel. When present, a manual fly-through of the excluded segment of the bowel is required (Fig. 8.22a–c). These electronic cleansing artifacts are positional in nature, involving the dependent portions of bowel, and therefore should not be persistent on both the supine and prone views.
Images (a)–(d) demonstrate the characteristic “bathtub ring”-type artifact produced by the electronic cleansing algorithm. This artifact is seen on the posterior wall of the rectum with the patient in the supine position. Rolling the patient into the prone position shifts the tagged fluid into the proximal sigmoid colon. The posterior wall of the rectum in the prone position demonstrates the normal smooth colonic mucosa with clearing of the ring artifact
With today’s multi-slice CT scanners, imaging of the abdomen and pelvis can usually be obtained during a single breath hold. However, in some patients with underlying respiratory or cardiovascular conditions, imaging in the supine or prone positions may be problematic. Significant tachypnea can result in a stair-stepping artifact involving those bowel segments and solid organs adjacent to the diaphragm. This can be pronounced on the 3-D images as well as the 2-D sagittal- and coronal-formatted images. The axial 2-D images source images will show the least motion artifact (Fig. 8.23a–c).
CTC utilizes a low-dose technique to obtain the source CT data that is used to build the 3-D model. This low-dose technique, coupled with the large body habitus of the average patient, results in a decrease in the signal to noise ratio of the source images. This produces a mottled irregularity to the 2-D source images as well as the colon surface on the 3-D endoluminal images. On the 2-D source images, this image noise, or quantum mottle, is manifested to a greater extent on the narrow soft tissue windows. It is recommended that the 2-D images be evaluated on the wider bone windows (Fig. 8.24a–d).
Images (a) and (b) show a mottled irregularity to the surface of the colon on the 3-D endoluminal views which is the result of increased image noise associated with the low-dose imaging of CTC. Image (c) demonstrates the same image noise or quantum mottle on the 2-D source images. Image noise can be decreased on the 2-D images through the use of wider windows as seen in image (d)
Spray artifact from retained metal hardware can degrade both the 3-D endoluminal and 2-D source images. Hip prostheses, Harrington rods, and spinal fusion hardware can produce significant spray artifact, limiting visualization of the bowel and adjacent structures in the abdomen and pelvis. As with image noise, spray artifact is less pronounced on the 2-D images when viewed with the wider bone windows (Fig. 8.25a–c).
Spray artifact from hip replacements can severely degrade the 3-D endoluminal views of the rectum as well as the adjacent pelvic structures on the 2-D source images, as seen in images (a)–(c). Spray artifact, like image noise, is less pronounced on the 2-D source images when viewed with wider windows
Data dropout occurs when portions of the colon are not included in the 2-D CT data set. This usually involves the flexures or the rectum. Data dropout appears as a black region devoid of any mucosal detail in the 3-D colon model. This artifact can be avoided with proper imaging of the entire abdomen and pelvis from the dome of the diaphragm to the pubic symphysis. It is also unusual for it to be present on both the prone and supine views (Fig. 8.26a–f).
As with patient preparation, the actual imaging of the CTC patient can be problematic, resulting in imaging pitfalls and artifacts. Adequate colonic distension is critical to the production of a diagnostic quality CTC study. The mechanical CO2 insufflator has revolutionized CTC imaging. Slow and gentle CO2 insufflation, coupled with maintaining a steady state luminal pressure of 25 psi during the exam, has significantly reduced the incidence of luminal narrowing or frank segmental collapse. Targeting narrowed or collapsed segments on the scout or preliminary views and aggressively distending those segments through the use of decubitus patient positioning can also decrease the incidence of segmental narrowing or collapse. Air–fluid interface artifact, electronic cleansing artifact, image noise artifact, spray artifact, and data dropout artifact are the by-products of the 3-D model building software algorithms and low-dose CT imaging technique used in CTC. They must be understood and recognized as imaging artifacts in order to adequately interpret a CTC study.
Anatomical Variant Pitfalls and Artifacts
No two patients are the same. There are numerous anatomical variants that can mimic pathology on 3-D endoluminal images. It is important to recognize these anatomical variants when evaluating the colon for pathology. Essentially, any structure in the abdomen or pelvis that abuts the colon can cause mass effect on the bowel wall and can be mistaken for pathology on the endoluminal views. Diverticular disease can simulate sessile polyps. Flat polyps are a variant of sessile polyps, which are especially difficult to detect on both CTC and OC. Pedunculated polyps can be mistaken for mobile stool if their stalk is long and inconspicuous. Benign lipomas of the colon can look identical to sessile polyps on 3-D endoluminal views. Rectal veins, anal papillae, and internal hemorrhoids can produce mucosal defects in the rectum that can be mistaken for intracolonic neoplasia. Finally, variations in contour and configuration of the appendix and ileocecal valve can represent normal variants or true pathology. Examples of each of these cases will be discussed below.
Extrinsic compression of the colon by any of the adjacent structures in the abdomen and pelvis can produce a mass effect on the bowel wall resulting in a pseudopolyp or mass on the 3-D endoluminal views. Rib ends (Fig. 8.27a, b), the sacrum (Fig. 8.28a, b), the iliac arteries (Fig. 8.29a–c), uterine fibroids (Fig. 8.30a–c), small bowel (Fig. 8.31a–c), and even a calcified gallstone (Fig. 8.32a–c) have been shown to produce such extrinsic compression artifacts on the colon wall. Extrinsic compression by foreign bodies such as surgical clips (Fig. 8.33a, b), a granulation tissue in a suture line (Fig. 8.34a–c), a vaginal tampon (Fig. 8.35a, b), and a rectal tube (Fig. 8.36a, b) can produce similar pseudopolyp or mass-like artifacts on the 3-D endoluminal views. Endoluminal views of a pedunculated polyp (Fig. 8.37a, b), a sessile polyp (Fig. 8.37c, d), and a flat polyp (Fig. 8.37e, f) are shown for comparison. Correlation with the 2-D CT images is required to exclude extrinsic compression by an adjacent structure as the etiology of these polyps or masses on the 3-D endoluminal images.
The aorta and iliac arteries can produce extrinsic compression on adjacent segments of colon in the abdomen and pelvis, which in turn can mimic pathology on the 3-D endoluminal views. Images (a)–(c) show extrinsic compression on the lateral wall of the cecum by the right external iliac artery, which produces a pseudo flat polyp on the 3-D endoluminal view
There are many conditions associated with a prepared colon that can mimic polyps. These include dense adherent stool (Fig. 8.38a–c), air bubbles trapped under contrast (Fig. 8.39a–c), tagged stool in a barium pool (Fig. 8.40a–c), and residual ingested material (Fig. 8.41a–d). Even submucosal air-filled cysts as seen in pneumatosis cystoides intestinalis (Fig. 8.42a–c) can simulate polyps in the prepared colon. These entities can usually be differentiated from true polyps by density analysis and correlation with the 2-D source images.
Dense adherent stool can mimic polyps on the 3-D endoluminal images. Adherent stool will not change positions on the prone and supine images. It can be differentiated from a true polyp by the presence of internal fat and air. Images (a)–(c) demonstrate small pockets of fecal fat and air within the adherent stool on density analysis and on the corresponding 2-D source images
Small air bubbles that become trapped under collections of contrast can mimic smooth sessile polyps. Images (a)–(c) demonstrate a small bubble in the descending colon. These air bubbles can be differentiated from true polyps with the help of density analysis and correlation with the 2-D source images
Diverticular disease is endemic in the CRC screening population. It usually involves the descending and sigmoid colon and can be rather extensive in these segments. Stool-filled diverticula can mimic sessile polyps (Fig. 8.43a–c). Correlation with the 2-D CT images as well as density interrogation, however, can usually differentiate these lesions from true polyps. The retained stool in the diverticulum will contain dense contrast as well as low-density fecal fat and air bubbles. Its location in a diverticulum can be confirmed on the appropriate 2-D CT images.
Retained stool in a diverticulum usually contains a mixture of dense contrast, fecal fat, and microbubbles of air. Images (a)–(c) demonstrate a stool-filled sigmoid colon diverticulum. The heterogeneous makeup of the stool ball is readily apparent on density analysis and the corresponding 2-D source image (image c)
Flat polyps, given their diminutive height above the colon wall, are difficult to identify on both CTC and OC. Flat polyps appear as subtle mucosal irregularities on the 3-D endoluminal views. Varying the artificial light source and correlation with the 2-D CT views can help in detecting the subtle lesions (Fig. 8.44a–d).
Images (a)–(d) demonstrate a subtle flat polyp on the medial wall of the cecum. The polyp is not easily seen on the standard 3-D endoluminal view (images a and b). By varying the position of the artificial light source, the flat lesion becomes more apparent (image c). This flat polyp has a subtle appearance on the 2-D source image as well (image d)
Mobility in positioning on the prone and supine views is one of the characteristics of stool. Pedunculated polyps on long stalks can also demonstrate such mobility and therefore be mistaken for stool if the stalk is not recognized (Fig. 8.45a–c). Whenever dealing with mobile lesions in the colon, always consider the pedunculated polyp and look for the diminutive stalk on both the 3-D and 2-D images.
Lipomas of the colon are benign entities that do not require removal. They can mimic polyps on the 3-D endoluminal images. Lipomas are usually sessile in nature. Given their soft consistency, they may show different degrees of prominence on the supine and prone images. They will demonstrate uniform fat attenuation with Hounsfield units of −75 to −125 on the 3-D and 2-D images (Fig. 8.46a–c). Density interrogation can usually differentiate a lipoma from a sessile polyp.
Prominent veins, anal papillae, and internal hemorrhoids are anatomical variants found in the rectum. The isolated rectal vein can usually be differentiated from a polyp or rectal fold by its torturous and bifurcating nature (Fig. 8.47). Anal papillae are small skin tags that are typically found abutting the rectal catheter as it traverses the anus (Fig. 8.48). Internal hemorrhoids are dilated veins found around the anus. They can be displayed as linear or polypoid mucosal defects radiating from the anus (Fig. 8.49a, b). Any of these entities, if prominent enough, can mimic a rectal polyp.
The appendix is readily apparent on most CTC studies. In fact, with the present day use of mechanical CO2 insufflation and stool/fluid tagging, the appendix is usually well distended with gas or contrast. A “mass” involving the appendiceal orifice can represent a multitude of conditions. If the patient has had a prior appendectomy, it may represent an inverted appendiceal stump. Correlation with the patient’s surgical history is required when considering this entity (Fig. 8.50a–c). A prolapsing base of the appendix can also produce a mass or pseudopolypoid defect of the appendiceal orifice. This defect is usually self-reducible on the contralateral images (Fig. 8.51a–d). If there is a persistent mass or defect involving the appendiceal orifice, then such entities such as carcinoid, mucocele, adenocarcinoma, and lymphoma must also be considered (Fig. 8.52a, b). Endoluminal visualization of the cecum and appendiceal orifice incompletely evaluates the entire appendix, and analysis of the 2-D source images is required for complete assessment of the appendix.
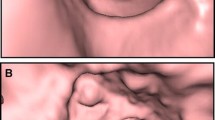
The ileocecal valve is also readily apparent on most CTC studies. It has a variable appearance between individual patients and also between positioning in the same patient. Ileocecal valve morphology can range from a sessile, fish-mouth appearance to a more bulbous, polypoid appearance. The valve usually takes on a more bulbous contour when the patient is imaged in the prone position. This is felt to be secondary to increased intraluminal small bowel pressure associated with prone positioning (Fig. 8.53a–c). The ileocecal valve usually demonstrates fat attenuation on the 3-D and 2-D images as well as on color windows and region of interest (ROI) interrogation (Fig. 8.54a–c). Polypoid projections off of the ileocecal valve are a common finding on CTC. These can represent benign entities such as a drop of barium (Fig. 8.55a–c) or a lipoma (Fig. 8.56a–c). Any polypoid projection off the ileocecal valve that demonstrates soft tissue density, however, must be considered a polyp until proven otherwise (Fig. 8.57a–d). One must also be careful not to assume any polypoid structure in the cecum is simply the ileocecal valve. A cecal mass can be mistaken for the ileocecal valve (Fig. 8.58a–c). Complete assessment of the ileocecal valve must include evaluation of the valve’s morphology, attenuation, and position in the cecum on the 3-D and 2-D images.
Conclusion
There are multiple potential pitfalls and artifacts associated with CTC imaging. The reader must be cognizant of these to adequately analyze the study and provide an accurate interpretation. This chapter has provided examples of the most common CTC pitfalls and artifacts, along with techniques for correctly identifying and characterizing these findings. With proper attention to technique in patient preparation, bowel distension, and image acquisition diagnostic quality, high-quality CTC studies can be obtained. Through careful analysis of the 3-D images with 2-D correlation, color windows, and ROI interrogation, the majority of these pitfalls and artifacts can be recognized and adequately managed.
Suggested Readings
Mang T, et al. Pitfalls in multi-detector row CT colonography: a systematic approach. Radiographics. 2007;27:431–54.
Dachman AH, et al. CT colonography: visualization methods, interpretation, and pitfalls. Radiol Clin North Am. 2007;45:347–59.
Halligan S, Taylor SA. CT colonography: results and limitations. Eur J Radiol. 2007;61:400–8.
Christensen KN, Fidler JL, Fletcher JG, Maccarty R, Johnson CD, et al. Pictorial review of colonic polyp and mass distortion and recognition with the CT virtual dissection technique. Radiographics. 2010. doi:10.1148/rg.e42.
Barish MA, et al. Multislice CT colonography: current status and limitations. Radiol Clin North Am. 2005;43:1049–62.
Hoon JI, et al. Multislice CT colonography: current status and limitations. Eur J Radiol. 2003;47:123–34.
Fletcher JG, Gluecker TM. CT colonography (virtual colonoscopy) for the detection of colorectal polyps and neoplasms: current status and future developments. Eur J Cancer. 2002;38:2070–8.
Dachman AH. Atlas of virtual colonoscopy. New York: Springer; 2003.
Pickhardt PJ, Kim DH. CT colonography: principles and practice of virtual colonoscopy. Philadelphia, PA: Saunders; 2010.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Jensen, D.W., Barlow, D. (2013). CTC Pitfalls/Limitations. In: Cash, B. (eds) Colorectal Cancer Screening and Computerized Tomographic Colonography. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5943-9_8
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5943-9_8
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5942-2
Online ISBN: 978-1-4614-5943-9
eBook Packages: MedicineMedicine (R0)