Abstract
CT colonography (CTC) is a minimally invasive, fast, safe and accurate screening examination for colorectal cancer. It also allows evaluation of structures outside the colon. There have been several changes in the performance of a study since it was first used in 1994. A successful CTC examination requires the use of an automated pressure-controlled carbon dioxide insufflator, a well-prepared colon, the use of tagging, an adequately distended colon and correct positioning for two-view series and additional view scans. CTC produces two-dimensional (2D) images and three-dimensional (3D) endoluminal views, and software is required to interpret them. How to perform a CTC study is described step by step. Performing a CTC after an incomplete optical colonoscopy (OC) is discussed, with a caveat of assessing whether free air is present before commencing the study. A colonic classification table is used for reporting CTC findings. CTC images are presented to illustrate differentiation of a polypoidal lesion and stool, as well as interpretation of images, and measurement of polyps. The role of translucent display is illustrated with examples.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
10.1 Introduction
CTC has been clearly identified as a valid screening test for CRC [1, 2]. It has demonstrated both cost-effectiveness [3] and a high degree of acceptance among patients [4]. It has been shown that screening of asymptomatic individuals can reduce CRC mortality [1]. Removal of an advanced adenoma may reduce the incidence of CRC [1].
There have been significant changes in the performance of a CTC study since it was first used by Vining in 1994 [5], the main changes being in computer hardware and CTC technique. Initially it took hours to process images, but technological advances in computers now allow us to generate vast numbers of images in real time [6]. CT scanners have advanced from single-slice to super-fast multiple detector CT (MDCT) scanners that can scan up to 320 slices per second. It is not necessary to use super-fast MDCT scanners for CTC studies; good studies can be performed on 16-slice up to 64-slice MDCT scanners. The advances in CT hardware have resulted in shorter scanning times. Breath holds of 5 s for the scout film and 10 s for abdominal scans are the norm now. A 2003 study by Pickhardt et al. [2] brought about changes to CTC technique. Their study included two tagging agents: 2 % w/v barium sulphate to tag stool and diatrizoate meglumine (Gastrografin) to tag remaining fluid (see Table 9.1). In their study tagging agents were administered to all participants (patients) prior to the CTC procedure. Apart from tagging stool, barium has been shown to also lightly cover a polyp, thereby making it more conspicuous on 2D viewing. A useful tip is to scroll carefully through the polyp to assess if soft tissue is present underlying the barium. A fairly recent paper underscores that contrast coating of a flat polyp can act as a marker for detection (Fig. 10.1) [7].
Use of the relatively high-density barium has several disadvantages and is therefore not recommended for routine use in CTC examinations. If 40 % w/v barium sulphate is used for a CTC study, this does not include a cathartic bowel cleansing or fluid tagging [8]. Electronic cleansing is not currently routinely performed because it may cause a large number of artefacts that could make interpretation difficult [8]. Part of the surface mucosa may be electronically removed and could result in missed lesions. Furthermore, use of 40 % w/v barium sulphate will prevent a same-day optical colonoscopy (OC) examination being performed.
CTC examinations are straightforward when a clean bowel and an adequately distended colon are imaged with a MDCT scanner. The role of CT software is important in CTC: clinically significant polyps can be readily detected with dedicated software [9]. All CTC components must be in place to perform a successful examination. This entails (i) patient compliance in terms of bowel preparation, (ii) an adequately distended colon, (iii) the use of at least a 16-slice MDCT scanner and (iv) interpretation of images using a dedicated 3D platform. These components are interdependent. A deficiency in any of them can cause a poor CTC result [10]. Chapter 9 focuses on bowel preparation, the role of tagging and the use of automated-carbon dioxide (CO2) insufflation. CTC technique and methods of interpreting images are the main focus in this chapter.
10.2 Indications and Contraindications
Table 10.1 presents indications and contraindications for CTC. These must be covered when informed consent is obtained from patients.
10.3 Colonic Classifications
A C1–C4 classification is used when reporting CTC findings. For example, normal colon or benign lesion would be classified as C1. If a polyp or possibly advanced adenoma were noted on the study, the classification would be C3. A non-diagnostic study would be C0. Table 10.2 presents the colonic C1–C4 classifications.
10.4 Positioning and Introduction of CO2
Before commencing a CTC examination, the patient is sent to the restroom/lavatory as the rectum must be emptied of any residual fluid [10]. The patient is requested to remove all clothing and wear a disposable gown with the opening at the back. Ensure there are no metal objects on the patient. Record any prosthetics as these could cause artefacts on the final image.
As discussed in Chap. 9, the colon is distended with CO2. The author uses an automated pressure-controlled CO2 insufflator. It is essential to check that there is sufficient CO2 in the cylinder before commencing the study.
A CTC study usually only requires a 180° two-view series: supine and prone. A 90° two-view CTC study that comprises supine and right lateral decubitus (RLD) may not clear the ileocaecal valve (ICV) of fluid. The RLD series is therefore used for obese patients and poor colon distension as well as single or multiple breaks in the colon outline obtained from the supine and prone series. The transverse colon is often compressed, with resultant non-filling of the segment, in obese patients in the prone position. Figure 10.2a (i and ii) illustrates the value of a RLD when there are multiple breaks in the two-view scans. Figure 10.2b is a synopsis of the CTC technique described below.
(a) (i) Colon view showing breaks in colon filling. A (ii) Complete filling of colon in the RLD scan (b) Schematic presentation of CTC technique (c) Green arrow indicates trifurcation of tube. Attached syringe for balloon distension. Yellow arrow indicates rectal drainage bag. White arrow indicates connection to CO2 insufflator. White circle shows black indicator line. The catheter must not be inserted into the rectum beyond the black line. Inflated balloon (open white arrows). Open blue arrows indicate two green filters to trap any faecal fluid from entering and contaminating the CO2 insufflator. (d) Close-up of CO2 insufflator. Black arrow litres of CO2 insufflated (1.6 L). Green arrow pressure in mmHg (15 mmHg) recording rectal pressure, and the white arrow on back dial shows the insufflation pressure at start of procedure. These two readings may be discordant when rectal pressure increases above 15 mmHg and no flow of CO2 can occur. Orange arrow indicates volume of CO2 in the cylinder. (e) 2D coronal view shows sigmoid colon in left inguinal region (white arrows). Note the pacemaker wires (white circle). (f) Colon-map showing air in small bowel (open white arrows). S stomach (g) (i) Air in stomach (closed white arrow). Note excessive air in small bowel (open white arrow). (g) (ii) 2D axial view of stomach distension (arrow)
The patient is positioned feet first in a left lateral position in the scanner. A disposable soft small gauge rubber rectal catheter (25 F or smaller) is then gently inserted into the rectum, and the balloon is insufflated with 30 cc of air employing a three-way connection as shown in Fig. 10.2c. For all female patients, always check that the catheter is in the rectum and not the vagina before commencing insufflation.
The automated pressure-controlled CO2 insufflator is switched on and the pressure set to 15 mmHg to enable the CO2 to gently flow at low pressure into the descending colon until one litre (1 L) of CO2 has been introduced [10]. The amount of CO2 is indicated on the gauge. Figure 10.2d is a close-up view of the dials of an insufflator (PROTOCO2L – Bracco). At this point, turn the patient prone and then immediately onto the right side to fill the proximal transverse and ascending colon. The pressure at this stage may be increased to 20 mmHg to distend the colon. When the volume reaches 2 L, return the patient to the supine position and commence scanning. For all scans, instruct the patient to inhale, then exhale and suspend breathing during scanning. Scanning is performed in exhalation as this elevates the diaphragm and allows the colon and flexures to expand [10]. The first breath hold (5 s) allows acquisition of the scout film. Once this film is reviewed, inform the patient that a full supine scan of the abdomen will commence. Duration of breath hold depends on the type of CT scanner used. The higher the scanning rating, the shorter the breath hold. For example, a patient needs to maintain a 10 s breath hold with a 16-slice scanner, whereas a longer breath hold would be necessary with a 4-slice scanner.
Next, the CO2 insufflator is switched off whilst the patient is turned prone. This is done because elderly and obese patients may have trouble turning prone and the intracolonic pressure rises rapidly, often above 60 mmHg, thereby triggering the machine alarm [10]. Some radiologists use the deflation manoeuvre after completion of the supine scan by emptying the rectum of air and then reinflating for the prone scan; this reduces the incidence of pain [12]. From time to time, it may not be possible for some patients to turn into the prone position, and a lateral decubitus view will be required instead. Ensure that, when scanning in the prone position, a pillow which is placed under the patient’s chest does not impinge on the abdomen [10].
Before introducing CO2, the balloon is deflated when the patient is in the prone position. This is done for two reasons: to obtain a full scan series without an inflated balloon, as it may obscure good visualisation of the distal rectum, and to better visualise internal haemorrhoids, if present (see Chap. 13). When the balloon is deflated, the CO2 insufflator is switched on. The patient is positioned for scanning. A scout film is taken on exhalation and breath hold of about 5 s. The abdominal scan usually takes 10 s. When the prone scan is completed, the insufflator is switched off and the clip of the rectal bag is opened to empty the rectum of CO2. This manoeuvre gives immense relief to the patient, [10] who is then turned into the right lateral decubitus (RLD) position whilst the images are examined by either a radiologist or appropriately trained radiographer. The reason for placing the patient in this position is because an RLD series may be required. On average, the acquisition and assessment of a two-view CTC study takes no more than 5 min. A CTC study requires on average between 15 and 20 min room time. Note that during scanning, extracolonic structures are also imaged. If the patient is poorly prepared and there is a lot of faecal material in the large bowel which is felt to make the study non-diagnostic (CO), the radiologist/radiographer has not completed the examination unless a full report is given on any extracolonic findings that may be present.
Adequate distension does not imply complete distension of all segments in all cases. Should areas of poor distension be identified in the same areas in both the supine and prone positions, in particular the sigmoid colon in cases of diverticular disease, the patient is ready to be scanned in the RLD position. The main reason for an additional view is because moderate or severe diverticular disease usually results in inadequate distension of the sigmoid colon. When the patient is in the RLD position, the insufflator is switched on again to allow for introduction of a further L of CO2, because the rectum was previously emptied when the bag was unclamped [10]. After the CO2 has been introduced, scanning on breath hold can recommence. Whilst waiting for the images to be processed, the CO2 is switched off. In the rare case where the RLD is unable to distend the appropriate area, the patient is turned into the left lateral decubitus (LLD) position. The CO2 is switched on and the patient re-scanned. Now and again it may happen that a four-view series fails to distend the colon adequately. The author then takes another supine scan because the bowel may have relaxed to allow for adequate distension.
Pain is not a feature of CTC. If a patient does complain of pain early on in the procedure, it is important to immediately check the inguinal regions for possible bowel herniation (Fig. 10.2e) [10]. If no herniation is evident, then the most likely cause of pain is underlying diverticular disease. As stated previously, it is essential in female patients to check that the catheter is in the rectum and not the vagina.
If a spasmolytic is used, it may relax the ICV and result in the small bowel filling with air (Fig. 10.2f). Occasionally the valve may be incompetent without the use of a spasmolytic. Carbon dioxide refluxes into the small bowel and it may rapidly reach the stomach (Fig. 10.2g (i and ii)). When this occurs, the patient usually complains of nausea and often breaks into a sweat. It is essential to instruct the patient to burp as this causes immediate relief [10].
10.5 Evaluation of Polypoidal Lesions
There are clues that allow differentiation between a polypoidal lesion and stool: 2D and 3D views are complementary. The former is the most useful method for making the distinction. When a polypoidal lesion is observed on 3D endoluminal fly-through, it is important to ascertain whether it is a polyp or stool. The latter can mimic a polyp, particularly in patients with suboptimal bowel preparation. The following steps should be performed.
-
Evaluate the lesion using 2D viewing and check for the presence of air within the lesion. If air is present, it is stool and not a polyp.
-
Note the position of the lesion during postural change. Does it move or not?
-
Use translucent display (TD) software, if available. TD enables one to evaluate below the surface of the mucosa.
It is important to evaluate a polypoidal lesion by performing 2D viewing with multiplanar views. The position of a polypoidal lesion, in both the supine and prone views, must be checked. If there is movement due to postural change, then this favours stool rather than polyp. Most typically stool will move to the opposite wall when a patient is turned from the supine to the prone position. Beware of the pedunculated polyp on a long stalk which may move with postural change [10]. A sessile polyp does not move with postural change; sessile polyps are fixed to the colon wall or haustral folds thus they do not shift in position. However, a paper by Laks, Macari and Bini [13] showed that 27 % of polyps moved from an anterior location to a posterior one relative to the colonic surface when a patient turned from the supine to prone position. In other words the polyps appeared to be mobile, but the polyp mobility was related to positional changes of the colon due to lax mesentery. Therefore, the shift in polyp location is not true mobility of the polyp. A further caveat to this is that occasionally a polyp is noted to move in position. However, it is not the polyp that moves, but the segment of colon in which it lies. Bowel segments that may move are the sigmoid colon, which may be redundant, the transverse colon and the ascending colon (see Chap. 11). If movement is detected, the structure would favour stool and not a polyp. In most cases, stool moves, but occasionally it may be adherent to the colon wall.
To distinguish between stool and polyp on 2D viewing, the following observations can be made:
-
Areas of internal gas, or areas of high attenuation, indicate the lesion is residual faecal matter and not a polyp.
-
Polyps are homogenous in attenuation.
-
Morphology of a lesion. Small polyps and cancers may have lobulated rounded borders.
-
Residual faecal material may look similar. However, if it shows irregular angulated borders or geometric pattern, it is residual faecal material.
-
Mobility of a lesion. Stool tends to move to the dependent surface of the mucosa in 180° postural change. Pedunculated polyps, and occasionally soft-tissue polyps, may move depending on what section of the colon they are present in.
The colon is not a fixed structure; positional abnormalities are common [14]. The sigmoid colon, transverse colon and caecum are located in the peritoneal cavity. These bowel segments may be on a long mesentery, which allows them to rotate on the mesentery. The rectum, descending colon, and ascending colon are located in the extra-peritoneal space. Portions of the ascending colon, however, are frequently mobile.
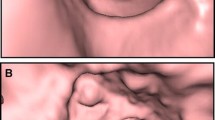
It is important during 2D viewing to check for the presence of air within the lesion (Fig. 10.3a). If air is evident, this would confirm that stool is the cause of the lesion. Stool is favoured if there is mixed heterogeneity within the polypoidal lesion. Stool is a potential CTC pitfall in image interpretation, hence it is covered in greater detail in Chap. 12.
(a) 2D view shows air in stool (white arrow). (b) (i) Translucent display (TD) of a pedunculated polyp showing high intensity red centre (open white arrow) as well as high intensity stalk (closed white arrow). Green fatty tissue. (b) (ii) TD shows barium covered stool which simulates a polyp on 3D (open black arrow). (b) (iii) TD showing stool covered with barium (open black arrow)
A 3D translucent display (TD) is a Viatronix software tool. It provides a semi-transparent view in different colours beneath the surface [15]. The software’s different colour attenuation values are red indicates soft tissue; white indicates high attenuation values, such as barium; green indicates negative values in the fat attenuation range; and blue indicates negative values, such as air [16]. The use of TD allows for visualisation of the composition of a polypoidal lesion. A polyp on TD will have a high intensity (red) centre, surrounded by a thin layer of green (fatty tissue) and a blue layer which is air as shown in Fig. 10.3b (i). If the lesion is stool, the high intensity is usually of mixed density. As discussed in Chap. 9, barium tags stool in the colon. In most cases if barium makes up the entire polypoidal lesion, then this indicates stool as shown in Fig. 10.3b (ii and iii). A TD image that shows a white interior is barium/stool. Barium tends to coat a polyp superficially, making it more conspicuous. Barium cannot get into a centre of a lesion.
The above process may seem to be complicated, but in fact it is an easy process. It can be performed in less than a minute. Measurement of polyps is described in detail in Chap. 14.
10.6 Diagnostic CTC Following Incomplete OC
Failure to reach the caecum during OC represents an incomplete or failed examination. The percentage of OC studies which may be incomplete shows a wide variation from 0.4 to 15 % [17, 18]. Reasons for a failed OC might include older patients, female gender, colon length, number of acute angle bends and flexures, advanced diverticular disease, prior abdominal surgery, occlusive cancers, benign strictures, colon containing hernias, intestinal malrotation and poor bowel preparation. From a CTC perspective, this group of patients is the most challenging [10]. They would have predominantly been prepared for an OC using a ‘wet’ preparation, such as PEG, which results in a large amount of residual colonic fluid, as discussed in Chap. 9. In addition, these patients would not have been given pre-procedural contrast or fluid tagging, making it more challenging to exclude false positives, such as stool adherent to the wall.
CTC has been the procedure of choice following an incomplete study as it could be performed as a same-day study on patients who had a failed or incomplete OC. This meant that there was no need for two separate bowel preparations. Patients were referred for a same-day CTC when they were fully conscious. In the absence of tagging agents (barium and Gastrografin), it was necessary to consider a compromise [10]. This entailed giving such a patient 60 cc of Gastrografin on arrival, and a CTC study usually could commence about 2 h later to allow time for the tagging agent to reach the rectum. However, over a period of time, it became obvious that significant lesions were being missed. Most centres that offer CTC have thus changed their protocols by performing the study the day after a failed or incomplete OC. The patient is kept on a liquid diet for a further 24 h, and steps 2–4 in Table 9.1 are followed for bowel preparation.
Before commencing with patient preparation, it is important to establish whether a recent polypectomy or biopsy (superficial or deep) has been performed. Occasionally, with superficial biopsies, the CO2 may track submucosally and result in pneumatosis coli [10]. If a deep biopsy or polypectomy has recently been performed, it is advisable to wait at least 4–6 weeks for proper healing of the mucosa before proceeding with the CTC to allow the mucosa to heal (see Table 10.1).
Before beginning a CTC study, a pre-procedure low-dose CT scan is taken to assess whether free air is or is not present. It is important to first exclude the possibility of an OC-caused colonic perforation. There have been rare reports of colonic perforation at CTC, especially in patients with obstructive lesions [19]. Approximately 50 % of patients with colonic perforations do not have symptoms. The author performs a low-dose CT scan, comprising 10 mm slice thickness at 10 mm intervals, before inserting a rectal catheter [20]. The images are viewed and, if any extra-luminal air is present, a CTC is not performed (see Fig. 10.4). The referring clinician must be immediately informed of this CT finding. If no free is identified to suggest perforation, the scanning protocol in Fig. 10.2b is implemented.
Hough et al. [20] reported a total effective dose of 0.9 mSv for men and 1.2 mSv for women in low-dose abdomino-pelvic CT to exclude perforation. Alternative techniques may be used, such as a slice through the upper, middle and lower abdomen. These increased gaps may be a trade-off for sensitivity. Professor P Pickhardt (personal email correspondence, May 2014) stated that low-dose CT is preferred to erect plain-film radiographs. According to him, the latter only excludes free air, whereas most perforations have contained extra-luminal gas, retroperitoneally or intramurally [10]. The scanning protocol in Fig. 10.2b is implemented if no free is identified on the pre-procedure low-dose CT scans to suggest perforation.
10.7 Diagnostic CTC Versus Colon Capsule Endoscopy Following Incomplete OC
In 2011 colon capsule endoscopy (CCE) was introduced, and a second-generation capsule has been available since 2014. The angle of view of images was increased from 156° to 172°. Two cameras are present and a full mucosal view is therefore obtained. The PillCam Colon 2 (Given Imaging Inc, Yoqneam, Israel) can photograph 4 FPS (frames per second) when stationary and 35 FPS when moving. A recent study reported that CCE’s sensitivity and specificity were 88 % and 82 %, respectively, in terms of identifying conventional adenomas 6 mm or larger [17]. The conclusion of another study, which compared CCE and CTC in patients with incomplete colonoscopy, was that both tools were of comparable efficacy in terms of colon evaluation [21]. CTC also detects lesions outside the colon, but this is not possible with CCE.
10.8 Extracolonic Findings
CTC screening is usually performed in healthy asymptomatic individuals using supine and prone scans without intravenous (i.v.) contrast [1]. As a result of the scan views, extracolonic structures are visualised. An advantage of CTC, compared with other CRC screening tools, such as OC and CCE, is that it is able to detect incidental lesions external to the colon [1]. An automatic retrospective reconstruction of the supine series of all patients is performed for evaluation of extracolonic findings. This consists of 5 mm sections at 3 mm intervals. It is important to remember that, when performing the prone series, there is often more coverage and certain lesions, such as those from lung cancer, may only be detected on prone imaging. Extracolonic findings are covered in Chap. 18.
10.9 Interpretation
A successful CTC is not difficult to perform if the bowel is clean and the colon is well distended. There are two methods available to read the scans: 2D and 3D. Some proponents prefer using 2D as a primary approach with 3D reserved for problem-solving, whereas others prefer 3D as the primary method, with 2D for problem-solving [1, 22]. There is consensus that readers need to be skilled in both interpretation methods. For 2D polyp detection, the window setting should be at a window width of 2000 and centred at 0 to −200 [15]. Soft tissue windows are set at 400 with a centre of 50. Sessile polyps have a round or ovoid morphology and are of soft-tissue density. These should be visualised in both prone and supine scans as their position is not affected by postural change, except possibly the previously mentioned portions of the bowel which may be mobile. Stool, on the other hand, does move as previously discussed. Air is often visible in the stool, giving it a heterogeneous appearance. One must beware the pedunculated polyp on a long stalk in terms of postural change as evident in Fig. 10.5a (i and ii) [10].
(a) (i) 2D supine view shows pedunculated polyp on medial wall of colon (arrow). (a) (ii) 2D prone view shows movement of pedunculated polyp to the lateral wall of colon (arrow). (b) (i) 3D showing circular fold in descending colon (arrows). (b) (ii) 3D view showing triangular fold of ascending colon (arrows) (c) (i) Viatronix V3D workstation showing all the icons. Spray can icon (black arrow). Green arrow location of total number of missed areas and their distance from anal verge (image courtesy of Viatronix, Stony Brook, New York). (c) (ii) Colon view showing three missed areas (arrows): caecum, ascending colon and distal transverse colon. (c) (iii) 3D endoluminal view. Pink (arrows) indicates region not visualised (missed regions) (d) Black arrow points to a sessile polyp on posterior haustral fold. White arrow points to a smaller sessile polyp on anterior haustral fold. Open green arrow indicates flight from rectum to caecum. (e) Colon-map with a ‘bookmark’ red dot indicating site of lesion (open black arrow). Note green centre line. (f) (i) Pedunculated polyp (head a, b). Long stalk (open black arrow). (f) (ii) 3D view of a small sessile polyp (diameter = 7.5 mm). Base of polyp (open black arrows)
Pickhardt et al. [22] maintain that primary 3D evaluation is preferable; they advocate the use of 2D for evaluation of polyp/stool differentiation. They maintain that this approach is easy, quick and extremely accurate. They conducted research on the accuracy of readers when using 2D compared with 3D [22]. According to these authors, primary 2D CTC is less sensitive than primary 3D CTC for polyp detection in low-prevalence screening cohorts.
All current systems allow improved 3D fly-through. The author’s preference is a primary 3D system, such as the Viatronix V3D system (Stonybrook, New York), but there are other options. The author’s standard protocol is to perform supine and prone scans; additional views in the RLD and LLD may be required. Changing a patient’s position by 180° allows shifting of pooled liquid, as well as movement of stool, from one wall to the opposite wall [10]. A unidirectional fly-through from the rectum to the caecum covers only a maximum of 90 % of colonic mucosa. This is the maximum percentage of mucosa visualised at OC on withdrawal of the scope. CTC visualises the total bowel mucosa four times: from the rectum to the caecum and back in the supine position and again in the prone series. This means that 100 % of colonic mucosa is visualised.
For CTC interpretation, the 3D colon-map view and automated centre line are essential for effective 3D evaluation. The centre line allows for an automated fly-through. The 3D map provides precise location in real time and allows for bookmarks to be placed indicating site of lesion. The colon-map also indicates relevant anatomy, such as an excessively tortuous portion of bowel. A centre line is automatically generated and continues in a retrograde fashion to the caecum and ICV. An icon is then clicked which reverses the fly-through from the caecum to the rectum [10]. The same is done in the prone study. It takes less than 2 min to perform this bidirectional flight.
The field-of-view (FOV) setting for Viatronix is 120° as this provides a good field of evaluation with no geometric distortion. Using a FOV of 120° allows for approximately 90 % coverage for a single one-way fly-through. A second complete fly-through in the opposite direction allows for coverage of approximately 96 %. The folds in the left colon (anal verge to splenic flexure) are usually circular; in the right colon (caecum to splenic flexure), they become triangular (Fig. 10.5b (i and ii)).
A ‘missed region’ tool is available on Viatronix whereby the operator can quickly flip through the unseen areas by clicking on an icon (Fig. 10.5c (i)). By doing this adds about an extra 30 s per study. To detect any lesions, which may have been missed, a click on the spray can icon colours the visualised areas of the bowel green (Fig. 10.5c (ii). The regions that have not been visualised are pink (Fig. 10.5c (iii)). Clicking on the detectable missed region icon takes the viewer automatically to the different missed regions until 100 % of the bowel is visualised. Note that flying unidirectional only results in about 90 % coverage of the colon.
A colour-density map is used to assess the density of any protrusions suggestive of polyps or stool that are encountered on the way. Polyps appear as red, barium appears white and lipomas display as green coloration. The anterior surface of a colon fold faces the rectum and anus; the posterior surface of the fold faces the caecum and ICV (Fig. 10.5d). The anterior folds are seen on a retrograde fly-through from the rectum; the posterior ones are seen on the reverse fly-through from the caecum. A ‘bookmark’ or red dot can be placed on the colon outline to indicate the site of a polyp or carcinoma. The bookmark is useful if a subsequent OC needs to be done [10]. The red dot indicates the site of the lesion as well as the distance from the anal verge (Fig. 10.5e). The green line indicates the automated centre line.
How to manage polyps is important. Radiologists, and appropriately trained radiographers, need to have a working knowledge of polyp morphology and how to measure polyps [20], as well as what recommendations to make when polyps are present. It is advisable to include the following disclaimer in all CTC reports: ‘CTC is not intended for detection of diminutive polyps (≤5 mm), the presence or absence of which will not change the clinical management of the patient’ [10]. A reporting template is included in Chap. 19.
Some software allows one to decide which view is best to measure polyps and is covered in Chap. 14. The head of a pedunculated polyp is measured; the length of its stalk is not measured (Fig. 10.5f (i)). The largest diameter of a sessile polyp is measured (Fig. 10.5f (ii)). Polyps of 6–9 mm are termed small. A study is considered positive when a lesion ≥6 mm is detected. If there are more than three polyps in the 6–9 mm range, OC is recommended on the same day. If the polyp burden is lower (<3 polyps), an option is a 3-year surveillance. If after 3 years there is an increase in polyp size, the patient can be referred for an OC. Most polyps, however, tend to regress in size. Polyps ≥10 mm are routinely removed. The chance of malignancy is <1 % in an asymptomatic low-risk individual [23, 24].
A 2015 study that involved 9336 adults reported interesting results in terms of OC’ s status as the gold standard colon test [25]. The findings underscore that lesions are missed at OC. The study included discordant lesions (findings that were not confirmed with initial OC) and nonblinded lesions (endoscopist provided with advanced knowledge of specific polyp size, location and morphological appearance at CTC). The findings revealed that 144 patients (21.5 %) of all discordant lesions were confirmed as false negative at OC, and that these were on average of 8.5 ± 3 mm in diameter and were more likely to be in the right colon. In summary 21.5 % of discordant polyps 6 mm or greater were detected at CTC, but not confirmed at subsequent OC [25]. These polyps were later proved to be true positives on CTC, even though the endoscopists had full advanced knowledge prior to the OC of the respective size, location and CTC morphological appearance of the polyp. Furthermore, of the discordant lesion subsequent follow-up by OC, 40 % proved to be CTC true-positive findings. The remaining balance was considered to be CTC false-positive findings as they were not detected at OC. A small percentage had follow-up CTC studies, and the lesions were again identified, which suggested that OC diagnosis of false positives was wrong. In terms of the false-negative findings at OC, 81 % were subsequently found to be neoplastic (adenomas or serrated lesions); 43 % were advanced lesions, and 89 % of advanced lesions were located in the right colon [25]. In a nutshell the findings show that OC is not infallible nor the final arbiter. If a lesion ≥6 mm is detected at CTC, but not at OC, this does not always mean that CTC is wrong. Patient management should be a 3-year surveillance programme, or redo CTC in 3 years to check whether the lesion is still evident; if not present it was probably a false-positive CTC lesion. However, if the lesion is again identified, or if it has grown, then repeat OC as indicated. The characteristics of advanced adenomas should be known (see Table 10.3) [15, 24, 26].
10.10 Methods and Software to View CTC Images
CTC interpretation is underpinned by knowledge of both normal and abnormal anatomical variations. CTC produces two-dimensional (2D) images comprising axial, multiplanar reformations (MPR) coronal, sagittal and oblique views and three-dimensional (3D) endoluminal views. What is the best method to analyse data? There is consensus that readers need to be skilled in both 2D and 3D interpretation methods. Given the ongoing technological advances in imaging, there are new CTC display techniques also available, such as the ‘filet dissection’ views where the colon is opened up to view for polyps, or the band view [27]. Virtual dissection (filet) view is an alternative 3D Viatronix software tool (Fig. 10.6). The colon is dissected open and flattened. A filet view’s appearance is that of a pinned pathology specimen. These specimen-type images suffer from geometric distortions thus polyps, especially in the flexure regions, become more difficult to identify. These new techniques speed up interpretation time but there is distortion of the mucosal folds sometimes making polyp visualisation difficult.
It is important to evaluate polyps in terms of postural change (see Chap. 14). There is a range of available software. All systems today allow for an improved 3D fly-through. Available 3D software systems do not always produce comparative images. The software of independent manufacturers is often superior to that of CT manufacturers. A 2003 comparative study, which was undertaken to directly compare 3D endoluminal capabilities of three commercial systems, found that Viatronix V3D-Colon was the best in terms of an effective time-efficiency primary 3D evaluation [9]. However, technological advances in software over the years have improved and have resulted in several good options. Which is the best method for evaluation of polyps? The acid test is the one that furnishes the best specificity and sensitivity for detection of polyps <6 mm. Pickhardt et al. [2] analysed 1233 asymptomatic patients with 3D and 2D readings. Tagging was employed. Their results of detection of polyps were:
-
≥6 mm 86 % sensitivity
-
≥8 mm 93 % sensitivity
-
≥10 mm 92 % sensitivity
Computer-aided detection (CAD) systems have become available [28, 29]. These systems are designed primarily to identify lesions that have been missed by the reader [30]. Reading time using CAD, especially by inexperienced readers, is usually longer [31]. CAD does have a role as either a primary or secondary reader depending on a reader’s experience.
10.11 Key Messages
-
Check volume of CO2 in the cylinder before commencing the study.
-
Patient must be sent to restroom/lavatory to empty rectum of fluid before the CTC study commences.
-
Patient preparation includes cathartic and tagging agents.
-
If patient complains of pain, check inguinal regions for possible bowel herniation.
-
If a patient complains of nausea and breaks into a sweat, this usually is due to air in the stomach: instruct the patient to burp as this causes immediate relief.
-
Balloon is deflated when patient is in prone position to obtain a full scan series without an inflated balloon, as it may obscure good visualisation of the distal rectum, and to better visualise internal haemorrhoids, if present.
-
Most centres do not undertake a same-day CTC study following incomplete OC. Protocol is to schedule for the next day. Patient remains on liquid diet for 24 h and tagging agents are administered.
-
Before beginning a CTC study following a failed OC, a pre-procedure low-dose CT scan must be taken to assess whether free air is, or is not present. It is important to first exclude the possibility of an OC-caused colonic perforation.
-
Image interpretation requires both 2D and 3D viewing.
-
Areas of internal gas, or areas of high attenuation, indicate the lesion is residual faecal matter and not a polyp.
-
Polyps are homogenous in attenuation.
-
Residual faecal material may look similar. However, if it shows irregular angulated borders or geometric pattern, it is residual faecal material.
-
Mobility of a lesion. Stool tends to move to the dependent surface of the mucosa in 180° postural change. Pedunculated polyps, and occasionally soft-tissue polyps, may move depending on what section of the colon they are present in.
10.12 Summary
Most CTC studies comprise a two-view series: supine and prone. A non-diagnostic study requires reporting of any extracolonic findings. Both 2D and 3D viewing is required to evaluate the colon. Software may include translucent display, checking missed colon regions and virtual dissection options. Computer-aided detection (CAD) systems do have a role as either a primary or secondary reader.
References
Yee J, Weinstein S, Morgan T, Alore P, Aslam R. Advances in CT colonography for colorectal cancer screening and diagnosis. J Cancer. 2013;4(3):200–9. [http://dx.doi.org/10.7150/jca.5858].
Pickhardt PJ, Choi R, Hwang I, Butler JA, Puckett ML, Hildebrandt A, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349(23):2191–200. [http://dx.doi.org/10.1056/NEJMoa031618].
Pickhardt PJ, Hassan G, Laghi A, et al. Cost-effectiveness of colorectal cancer screening with computed tomography colonography. The impact of not reporting diminutive lesions. Cancer. 2007;109(11):2213–21.
Gluecker TM, Johnson CD, Harmsen WS, Offord KP, et al. Colorectal cancer screening with CT colonography, colonoscopy and double-contrast barium enema examination: prospective assessment of patient perceptions and preferences. Radiology. 2003;227(2):378–84. [http://dx.doi.org/10.1148/radiol.2272020293].
Vining DJ, Gelfand DW, Bechtold RE, et al. Technical feasibility of colon imaging with helical CT and virtual reality. AJR. 1994;162:104.
Vining DJ. Virtual colonoscopy: a storm is brewing. Appl Radiol. 2008;37(11):12–6.
Kim DH, Hinshaw L, Lubner MG, Munoz de Rio A, Pooler BD, Pickhardt PJ. Contrast coating for the surface of flat polyps at CT colonography: a marker for detection. Eur Radiol. 2014. [http://dx.doi.org/10.1007/s00330-014-3095-z].
Pickhardt PJ. Screening CT colonography: how I do it. AJR. 2007;189(2):290–8. [http://dx.doi.org/10.2214/ajr.07.2136].
Pickhardt PJ. Three-dimensional endoluminal CT colonography (virtual colonoscopy): comparison of three commercially available systems. AJR. 2003;181(6):1599–606.
Bortz JH. An approach for performing a successful computed tomography colonography examination. S Afr J Rad. 2014;18(1); Art. #607, 11 pages. http://dx.doi/org/10.4102/sajr. v18i1.607.
Zalis ME, Barish MA, Choi JR, Dachman AH, et al. CT colonography reporting and data system: a consensus proposal. Radiology. 2005;236(1):3–9. [http://dx.doi.org/10.1148/radiol.2361041926].
Dachman AH. Advice for optimising colonic distention and minimising risk of perforation during CT colonography. Radiology. 2006;239(2):317–21.
Laks S, Macari M, Bini E. Positional change in colon polyps at CT colonography. Radiology. 2004;231(3):761–6.
Saunders BP, Phillips RK, Williams CB. Intraoperative measurement of colonic anatomy and attachments with relevance to colonoscopy. Br J Surg. 1995;82(11):1491–3.
Pickhardt PJ, Kim DH. CT colonography: principles and practice of virtual colonoscopy. Philadelphia: Saunders; 2009.
Bortz J. Inverted appendix: computed tomographic colonography diagnosis in a patient and lesson learned. S Afr J Rad. 2015;19(1); Art. #748, 4 pages. http://dx.doi.org/10.4102/sajr.v19i1.748.
Rex DK, Adler SN, Aisenberg J, et al. Accuracy of capsule colonoscopy in detecting colorectal polyps in a screening population. Gastroenterology. 2015;148(5):948–57.
Spada C, Hassan C, Munoz-Navos M, et al. Second generation colon capsule endoscopy compared with colonoscopy. Gastrointest Endosc. 2011;74(3):581–9.
Burling D, Halligan S, Slater A, Noakes MJ, Taylor SA. Potentially serious adverse events at CT colonography in symptomatic patients: national survey of the United Kingdom. Radiology. 2006;239(2):464–71. [http://dx.doi.org/10.1148/radiol.2392051101].
Hough DM, Kuntz MA, Fidler JL, Johnson CD, et al. Detection of occult colonic perforation before CT colonography after incomplete colonoscopy: perforation rate and use of a low-dose diagnostic scan before CO2 insufflation. AJR. 2008:191(4):1077–81. [http://dx.doi.org/10.2214/ajr.07.2746].
Spada C, Hassan C, Barbaro B, et al. Colon capsule versus CT colonography in patients with incomplete colonoscopy. A prospective, comparative trial. Gut. 2015;64(2):272–81.
Pickhardt PJ, Lee AD, Taylor AJ, Michel SJ, et al. Primary 2D versus primary 3D polyp detection at screening CT colonography. AJR. 2007;189:1451–6. [http://dx.doi.org/10.2214/ajr.07.2291].
Pickhardt PJ, Kim DH. Colorectal cancer screening with CT colonography: key concepts regarding polyp prevalence, size, histology, morphology, and natural history. AJR. 2009;193(1):40–6. [http://dx.doi.org/10.2214/ajr.08.1709].
Johnson CD, Chen M, Toledano AY, Heiken JP, et al. Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 2008;359(12):1207–17. [http://dx.doi.org/NEJMoa0800996].
Pooler DB, Kim DH, Weiss JM, et al. Colorectal polyps missed with optical colonoscopy despite previous detection and location with CT colonography. Radiology. 2016;278(2):422–9.
Kim DH, Pickhardt PJ, Taylor AJ. Characteristics of advanced adenomas detected at CT colonographic screening: implications for appropriate size thresholds for polypectomy versus surveillance. AJR. 2007;188(4):940–4.
Lee SS, Park SH, Kim JK, Kim N, et al. Panoramic endoluminal display with minimal image distortion using circumferential radial ray-casting for primary three-dimensional interpretation of CT colonography. Eur Radiol. 2009;19:1951–9. [http://dx.doi.org/10.1007/s00330-009-1362-1].
Lawrence EM, Pickhardt PJ, Kim DH, Robbins JB. Colorectal polyps: stand-alone performance of computer-aided detection in a large asymptomatic screening population. Radiology. 2010;256(3):791–8. [http://dx.doi.org/10.1148/radiol.10092292].
Halligan S, Mallett S, Altman DG, et al. Incremental benefit of computer-aided detection when used as a second and concurrent reader of CT colonographic data: multiobserver study. Radiology. 2011;258(2): 469–76. [http://dx.doi.org/10.1148/radiol.10100354].
De Haan MC, Pickhardt PJ, Stoker J. CT colonography: accuracy, acceptance, safety and position in organized population screening. GUT. 2015; 64(2):342–50. doi:10.1136/gutjnl-2014-308696.
Helbren EL, Plumb AA, Taylor SA. The future developments in gastrointestinal radiology. Frontline Gastroenterol. 2012;3(Supp 1):i36–41. doi:10.1136/flgastro-2012-100121.
Acknowledgements
Viatronix V3D workstation image courtesy of Viatronix, Stony Brook, New York.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bortz, J.H. (2016). CTC Technique and Methods of Interpreting Images. In: Bortz, J., Ramlaul, A., Munro, L. (eds) CT Colonography for Radiographers. Springer, Cham. https://doi.org/10.1007/978-3-319-29379-0_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-29379-0_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29377-6
Online ISBN: 978-3-319-29379-0
eBook Packages: MedicineMedicine (R0)