Abstract
Antibiotics are organic small molecules, many of which are from natural sources, which are used to treat human infections caused by pathogenic microorganisms. While most validated antibiotics are initially very useful clinically, the pathogenic microorganisms that these compounds target are able to evade the action of the antibiotic by development of resistance mechanisms, which eventually render these antibiotics ineffective. Moreover, these resistance mechanisms can be passed on among different types of bacteria in a very simplistic manner that further compromises the usefulness of antibiotics. As a consequence, many diseases that were thought to have been eradicated by antibiotics (such as tuberculosis) have reemerged within these antibiotic-resistant strains. Hence, there is a constant need for the development of new and better antibiotic molecules that can be used to target these drug-resistant microbial populations.
This chapter, which has been modified slightly for the purposes of this volume, was originally published as part of the Encyclopedia of Sustainability Science and Technology edited by Robert A. Meyers. DOI:10.1007/978-1-4419-0851-3
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Fatty Acid Biosynthesis
- Trojan Horse
- Cell Wall Biosynthesis
- Antibiotic Molecule
- Fatty Acid Biosynthesis Pathway
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Definition of the Subject
Antibiotics are organic small molecules, many of which are from natural sources, which are used to treat human infections caused by pathogenic microorganisms. While most validated antibiotics are initially very useful clinically, the pathogenic microorganisms that these compounds target are able to evade the action of the antibiotic by development of resistance mechanisms, which eventually render these antibiotics ineffective. Moreover, these resistance mechanisms can be passed on among different types of bacteria in a very simplistic manner that further compromises the usefulness of antibiotics. As a consequence, many diseases that were thought to have been eradicated by antibiotics (such as tuberculosis) have reemerged within these antibiotic-resistant strains. Hence, there is a constant need for the development of new and better antibiotic molecules that can be used to target these drug-resistant microbial populations.
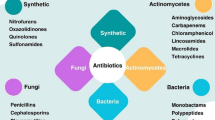
Traditionally, the discovery and development of new antibiotics and other drug molecules has relied on two parallel and complimentary approaches: the discovery of new molecules of clinical relevance from natural sources, and the use of synthetic chemistry methods to derive compounds, based on the scaffold of naturally occurring molecules, with enhanced favorable antimicrobial properties. More recent development includes the identification of molecules without any natural precedents, based on the use of high-throughput screening methods of potential antibiotic targets against a large number of synthetic compound libraries to identify new classes of antibiotic molecules. Continued developments in all of these approaches, by an amalgam of both academic and industrial efforts, are essential for the development of compounds aimed at treating the evolution of drug-resistant pathogenic microorganisms.
Introduction
The interaction of prokaryotic microorganisms with human beings is widespread and significant, and the number of bacterial cells within the human body far exceeds the number of the human eukaryotic cells. This interaction between humans and bacteria is designed to be mutually beneficial to both [1, 2]. However, a small number of these bacterial microorganisms are known to cause disease in human beings and are hence called pathogens. The mechanisms by which these pathogenic organisms cause disease are extremely diverse and affect nearly all types of tissues and organs. The advancement of medical science has resulted in the development of two frontline defense mechanisms to fight infections and diseases caused by microbes. The first line of defense is the vaccines that specifically elicit the human host’s adaptive immune response to recognize and eliminate pathogenic and harmful microbes, while selectively preserving the beneficial microbe population. Vaccines are generally biological macromolecules, derived from the pathogenic microbes themselves, which provide the adaptive immune response with the information necessary to elicit an antibody or cellular immune response against future invasions by the pathogenic microbes. Vaccines have been developed against several pathogens and have led to very significant reductions of deadly diseases such as tuberculosis and tetanus. However, vaccinations are not currently available against all pathogens, and the natural evolution of the pathogens themselves may render these vaccinations ineffective against future infections, as exemplified by the inherent difficulties in vaccine development against viral infections such as influenza and HIV/AIDS.
The second frontline defense against pathogenic infections is the discovery and development of small molecule antibiotics that are designed to target and kill the harmful microorganisms with minimal side effects against the human host. Antibiotics are naturally occurring molecules produced by a number of different bacterial species to give them a selective competitive advantage for nutrients or other growth necessities over other microorganisms with which they share their surroundings. Serendipitous discovery and exploitation of these molecules dates back to ancient history [3–5] with numerous early reports, such as the use of the bark from cinchona tree, which contains the antibiotic quinine, used to treat malaria. Antibiotics generally have well-defined mechanisms of action against microbes and target specific biological processes to either retard growth (bacteriostatic antibiotics) or kill the microbe (bacteriocidal antibiotics).
The first report of an isolated antibiotic molecule used to effectively treat infections was the development and use of penicillin from the fungus Penicillium notatum by Alexander Fleming in 1928. Penicillin was used to treat diseases such as syphilis and other infections caused by staphylococci and streptococci. The term “antibiotic” was coined by the microbiologist Selman Waksman in 1942 [6] and is derived from the Greek antibiosis (“against life”). Hailed as a wonder drug, the discovery of penicillin marked the beginning of the antibiotic age, during which time antibiotics were developed to treat almost all major human infectious diseases. During this era, thousands of antibiotic molecules were discovered and these compounds were applied to fight bacterial, fungal, protozoan, and yeast infections. Concurrently, synthetic organic chemistry was also applied for the production of derivatives of naturally occurring antibiotics, and these synthetic compounds exhibited more desirable properties, such as decreased incidences of allergic reactions in humans. The discovery and development of these molecules marked a decreased incidence of outbreaks of the most common infectious diseases and contributed to an increase in life expectancy around the world.
However, repeated challenge of the pathogenic microorganisms with these antibiotics, in combination with the natural evolution of their genetic information, has resulted in the development of antibiotic resistance in these pathogens [7–9]. This process has led to the development of microbial resistance against nearly all available antibiotic molecules and has precipitated to an immense medical and financial challenge. The arsenal available to fight infections is becoming increasingly limited, and the rate of development of new molecules has not kept pace with the emergence of antibiotic resistance.
Factors Contributing to Increased Antibiotic Resistance
-
1.
Widespread and indiscriminate overuse of antibiotics in the clinical environment, which exposes pathogenic microorganisms to an ever increasing concentration of different antibiotic molecules, which in turn increases the selection pressure to develop resistance against these antibiotic molecules [10, 11].
-
2.
Use of antibiotics in agriculture and livestock rearing also leads to increased exposure of pathogenic bacteria to antibiotic molecules. Many of the antibiotics in use in agriculture and livestock feeds are also used for treating humans, and hence, development of resistant bacterial strains can be transferred from one setting to the other very easily [12–14].
-
3.
Genetic recombination and transfer of genes from an antibiotic-resistant microbe to a non-resistant microbe, which leads to spread of resistance among microbial species. Antibiotic resistance genes are usually borne on highly mobile genetic vehicles called plasmids, which can easily be transmitted among microbes [15]. Microorganisms are able to sequester multiple plasmids, resulting in the evolution of plasmids that contain more than one resistance determinant. For example, the Shigella epidemic that caused nearly a quarter million deaths in Guatemala in 1968 was caused by a pathogen that contained a plasmid with resistance against four of the most commonly used antibiotics [16–18].
Mechanisms by Which Microorganisms Develop Resistance to Antibiotics
-
1.
Efflux pumps in the microbial cell walls and membranes which actively transport the antibiotic molecule out of the cell and hence decrease its concentration within the cell. Consequently, increasing doses of antibiotics are required to target such microbes [19–21]. This mechanism is typified by the resistance to the broad-spectrum antibiotic tetracycline, which is mediated by the genetically mobile tet genes that encode for active efflux pumps for tetracycline and its derivatives [22–24].
-
2.
Chemical modification of the antibiotic molecule by specific enzymes within the target pathogenic microbe, which render the antibiotic ineffective [25]. This mechanism is of particular concern against β-lactam antibiotics, such as penicillin and its derivatives [26, 27].
-
3.
Modulation of the antibiotic target within the target cell so that the antibiotic is no longer able to bind and engage the target. Random mutations within the antibiotic target genes may lead to the emergence and subsequent selection of microbe species with a desensitized antimicrobial target. This mechanism of resistance is operative for development of resistance against the macrolide antibiotic erythromycin, and resistance results from the modification of its target, the bacterial ribosome, such that the antibiotic is no longer able to find the target [28, 29]. Another example is resistance to the “drug of last resort” vancomycin, which results as a change in its target of the D-Ala- D-Ala dipeptide moiety of the bacterial cell wall to D-Ala- D-Lac or to D-Ala- D-Ser [30–32].
-
4.
Alteration of the metabolic pathways that are targeted by the antibiotic molecule so that inhibition of these metabolic pathways is not inhibitory or lethal to the microbe. A primary example of this class of resistance is the alterations in the sterol biosynthesis pathway in fungi which confer resistance to azole antibiotics [33, 34].
In light of the above factors, there is an ever-growing need for academic laboratories as well as for the pharmaceutical industries to search for antibiotics that have new and as yet unexplored mode of actions. New chemical classes of drug molecules are needed to mitigate the effects of resistance against the current drug chemical entities.
Emerging Targets of Antibiotic Molecules
Several new classes of antimicrobial targets have been identified, and drug development based on these findings, though still in its infancy, have taken major leaps forward.
Microbial Fatty Acid Biosynthesis Inhibition
The microbial fatty acid biosynthesis pathway presents numerous targets for drug development, particularly against the causative agent of tuberculosis – Mycobacterium tuberculosis. The metabolic pathways and chemical mechanisms for the synthesis of fatty acids are shared between a majority of prokaryotes and eukaryotes, including humans. However, as a result of differences in protein sequence and different arrangement of the active sites, compounds that target the bacterial fatty acid synthesis pathway are not cross-reactive or toxic against humans. The most well-characterized class of fatty acid biosynthesis inhibitor molecules is the antituberculosis molecule isoniazid, which inhibits the biosynthesis of mycolic acid, an essential component of the mycobacterial cell wall. Triclosan, an extensively used molecule in consumer products, such as toothpastes and mouthwashes, is also a fatty acid biosynthesis inhibitor.
An example of an emerging molecule in this class of antimicrobials is platensimycin (Fig. 2.1), produced by the organism Streptomyces platensis [35], which inhibits the growth of several pathogenic Gram-positive bacteria such as Staphylococcus aureus, Enterococcus faecalis, and Staphylococcus pneumonia [36]. Platensimycin inhibits the 3-ketoacyl-ACP synthase (KAS) enzyme FabF. Continued high-throughput screening and host genetic engineering efforts led to the identification of a platensimycin analog, platencin [37–39], which, in addition to FabF, inhibits another KAS enzyme called FabH and displays enhanced pharmacodynamic properties as compared to platensimycin. Chemical structures of microbial fatty acid biosynthesis inhibitor molecules discussed in this section are illustrated in Fig. 2.1.
Other KAS inhibitor molecules include cerulenin and thiolactomycin [40, 41]. Cerulenin is a broad-spectrum antifungal antibiotic produced by fungus Caephalosporium caerulens and preferentially inhibits the KAS enzymes FabB and FabF. Cerulenin forms a stable covalent adduct with the active site cysteine residue of these enzymes, and thus inhibits malonyl-group incorporation in the growing fatty acid chains [40, 42]. Thiolactomycin and related compounds have been isolated from various Streptomycetes and show potent inhibitory activity against fatty acid biosynthesis and mycolic acid biosynthesis in mycobacteria as well as against protozoan parasites such as malaria-causing Plasmodium falciparum. Thiolactomycin mimics the binding of malonyl coenzyme A molecule in the active site of KAS enzymes FabB, FabF, and FabH [41, 43]. Attempts for the preparation of semisynthetic derivatives of thiolactomycin are currently underway, and some of these derivatives are expected to improve upon its antimicrobial properties of thiolactomycin [44].
Molecules such as triclosan, isoniazid, diazaborines, and ethionamide target the enoyl-ACP reductase enzyme FabI of the fatty acid biosynthesis pathway. Each of these molecules binds in the active site of the enzyme and forms a tight complex with the nicotinamide adenine dinucleotide (NAD+) cofactor required for catalysis by FabI. However, pseudomonads and S. pneumoniae contain an additional enoyl-ACP reductase enzyme, FabK, which is not susceptible to inhibition by these compounds, which allows these pathogens to overcome the antibacterial activities of these compounds.
The fatty acid biosynthesis pathways also present several other enzymes that can be targeted for drug development. The isomerase activity of the enzyme FabA can be inhibited by the drug candidate compound 3-decynoyl-N-acetylcysteamine. Metabolic interaction of the acetyl coenzyme A carboxylase enzyme with the fatty acid biosynthetic pathway also poses a potential target for inhibitor screening. Finally, compounds such as phenethyl alcohol, which inhibit the enzyme PlsB, responsible for the link between fatty acid biosynthesis and phospholipid biosynthesis, are also antimicrobial agents.
Isoprenoid Biosynthesis Inhibition
Isoprenoids are naturally occurring diverse organic compounds derived from the condensation of two or more isoprene monomeric units. They represent the largest class of small molecules on Earth. The isoprenoid pathways between prokaryotes and eukaryotes are very divergent: Humans synthesize isoprenoids by the mevalonate pathway, while microbes synthesize isoprenoids via the nonmevalonate pathways. Both pathways present numerous potential drug targets. One of the most widely used cholesterol-lowering drug, Lipitor, targets the mevalonate pathway in humans which is responsible for cholesterol biosynthesis. Antimicrobials such as terbinafine target the nonmevalonate pathways in fungi and yeast.
Several promising lead compounds that target the nonmevalonate pathway in the malaria parasite Plasmodium falciparum have been characterized. Principal among these are the phosphonate molecules fosmidomycin, first isolated from Streptomyces lavendulae, and its derivative FR900098, isolated from Streptomyces rubellomurinus [45, 46]. Fosmidomycin inhibits the enzyme 1-deoxy-D-xylulose 5-phosphate reductoisomerase (DXR) of the malaria parasite and has progressed to the stage of human phase II clinical trials for use in combination therapy with lincosamide antibiotic clindamycin [47–49]. However, the bioavailability of this molecule is low in bacterial models, with tuberculosis-causing bacterial pathogen essentially resistant to this molecule due to lack of uptake [50]. FR900098 is a structural analog of fosmidomycin and has been shown to demonstrate better efficacy in vivo than the parent compound. Synthetic and biosynthetic routes for the production and manipulation of this compound are currently being pursued [51, 52], as is the synthesis of several other structural analogs of fosmidomycin [53]. Fosmidomycin and FR900098 belong to the phosphonate class of antimicrobials, which are characterized by the presence of a stable carbon–phosphorous covalent linkage [54].
In addition to the DXR enzyme, a second potential drug target is the isoprenoid biosynthesis enzyme IspH, which is present in the vast majority of pathogenic bacteria and the malaria parasite but not in humans [55]. IspH is an attractive target for the development of inhibitors which could be potential drug and herbicide candidates. A series of diphosphate and bisphosphonate compounds have been synthesized, some of which inhibited the IspH enzyme at nanomolar concentrations [56, 57].
Other isoprenoid biosynthetic drug targets include the enzyme dehydrosqualene synthase CrtM, from the human pathogen Staphylococcus aureus, which can be inhibited by phosphonosulfonates and phosphonoacetamide compounds [58]. These compounds lead to inhibition of production of the S. aureus virulence factor staphyloxanthin, which makes these otherwise recalcitrant pathogenic cells susceptible to reactive oxygen species and subsequent clearance by the human immune system [59, 60]. Finally, the antiarrythmia drug amiodarone, which blocks various metal ion channels in the cell membrane [61], in conjunction with itraconazole, a fungal cytochrome P450 inhibitor [62], is also being reevaluated for the treatment of Chagas disease and cutaneous leismaniasis [63].
Cell Wall Biosynthesis Inhibition
Inhibition of cell wall biosynthesis has been one of the earliest validated targets for antibiotic development and still remains one of the most fruitful areas for the development of new drugs. However, drug development against cell wall biosynthesis is particularly challenging due to the presence of an additional lipopolysaccharide layer in Gram-negative bacteria and the fungal chitin cell wall in fungi, both of which are extremely rigid and impermeable to most small molecule drugs. The following section focuses on some new nucleosidic antibiotic molecules that inhibit microbial cell wall biosynthesis and hold promise for future development. Chemical structures of microbial cell wall biosynthesis inhibitor molecules discussed in this section are illustrated in Fig. 2.2.
Nucleoside antifungal polyoxin molecules, such as nikkomycins, were isolated from several strains of Streptomyces [64] and have been shown to inhibit the biosynthesis of the fungal chitin cell wall. Nikkomycins display a wide spectrum of bioactivity while being nontoxic to animals and plants and have traditionally been used for controlling plant fungal diseases in agriculture. The parent nikkomycin compounds show relatively weak activity against opportunistic human pathogenic fungi, and semisynthetic derivatives are now being prepared which may display better pharmacological properties [65].
Capuramycin was first isolated from Streptomyces griseus in the 1980s and shows potent antibacterial properties against the human pathogens Streptococcus pneumoniae and Mycobacterium smegmatis [66]. Structure activity relationships have been explored by the synthesis of capuramycin derivatives [67, 68]. In in vivo studies against Mycobacterium tuberculosis , capuramycin demonstrated unique phenotypic changes in the pathogen which are not shown by any other currently available antibiotic and which may signify a mode of action distinct from those of known antibiotics [69].
Structurally related uridylpeptide molecules such as mureidomycins, pacidamycins, napsamycins, and sansanmycins have demonstrated activity against infections of the opportunistic human pathogen Pseudomonas aeruginosa in rodent models. Such infections are difficult to treat in immune-compromised patients as this pathogen can form a protective biofilm layer resulting in chronic infections [70–72]. These molecules do not show any cross-reactivity with mammalian cells.
Emerging Chemical Classes of Antibiotic Molecules
Peptidic Antibiotics
Peptidic antimicrobials are typically synthesized by the ribosome and consist of short polymers of the 20 naturally occurring amino acids linked together by amide bonds. A second class of peptide antimicrobials are generated by a molecular assembly line, called nonribosomal peptide synthases (NRPS), which can incorporate nonnatural amino acids. The use of peptides to target pathogenic microbes is exemplified by the production of short cationic peptides by the human and plant immune systems, which either recruit the immune system for pathogen clearance or disrupt the outer cell and organelle cell membranes of microbes. A common conserved feature among all peptidic antimicrobials is posttranslational modifications conferred upon the peptide backbone, which are essential for their biological activities [73–75].
A well-known example of one class of ribosomally produced antimicrobial peptides is lantibiotics. Although these molecules are synthesized on the ribosome, they undergo posttranslational processing, resulting in the formation of several ring-like structures that add rigidity [76]. These compounds can be further modified on the amino and carboxy termini of these peptides as well, as shown in the structures of the lantibiotics epilancin [77] and microbisporicin [78]. Lantibiotics demonstrated multiple modes of action and exert their biological activities by binding to the lipid II cell wall moiety in bacteria [79], which leads to both inhibition of peptidoglycan biosynthesis as well as cell membrane permeabilization.
The most extensively used and well-characterized lantibiotic to date is Nisin (Fig. 2.3), initially identified as a by-product of milk fermentation, which contains seven lantibiotic rings, and has been used in the livestock industry for the treatment of bovine mastitis [80, 81]. Nisin, produced by the bacterium Lactococcus lactis, shows no adverse effects in humans and is being evaluated in human trials for the treatment of staphylococcal mastitis in lactating women [82].
Among the NRPS peptides, the most promising drug candidates are the lipopeptide antibiotic daptomycin and glycopeptides vancomycin and teicoplanin. Lipopeptide antibiotic such as daptomycin (Fig. 2.4) contains a long lipid chain attached to the peptide, which helps in targeting the bacterial cell wall. Daptomycin is produced by Streptomyces roseosporus, and genetic manipulations of the producer organism have led to the production of a combinatorial library of daptomycin derivatives [83–86]. Daptomycin shows potent antimicrobial activity against methicillin-resistant Staphylococcus aureus (MRSA) [87], infections by which are a rising global concern, and is already registered for the treatment of skin and soft tissue infections [88], bacteremia, and bacterial endocarditis [89].
The glycopeptide antibiotics are produced as cyclic aglycones (without sugars) and are then decorated by a number of different sugar molecules that are covalently attached by dedicated glycosyltransferase enzymes [90–92]. Among these, vancomycin (Fig. 2.5) [93], which prevents cell wall biosynthesis in Gram-positive bacteria, is clinically approved as the “drug of last resort” against MRSA infections [94]. Oritavancin (Fig. 2.5), a semisynthetic derivative of vancomycin, is potent against vancomycin-resistant enterococci (VRE) and is currently under human trials for the treatment of soft tissue infections by Gram-positive bacteria [95]. Also of note are the cyclic lactone linkage–containing depsipeptides katanosins/plusbacins [96] and glycolipodepsipeptide ramoplanin [97], which are also active against MRSA.
Polyketide Antibiotics
Polyketide antibiotics are similar to nonribosomal peptide antibiotics as they are synthesized by multimodular polyketide synthases. These enzymes are analogous to the nonribosomal peptide synthases but typically catalyze the condensation of malonyl coenzyme A–derived monomeric units into cyclic lactone rings, onto which further modifications such as hydroxylations, glycosylations, and methylations are added. The most well-known polyketide antibiotic is erythromycin (Fig. 2.6), produced by Streptomyces erythreus, which has been in clinical use for more than 50 years. Several derivatives of erythromycin, such as clarithromycin and azithromycin (Fig. 2.6), have been developed for clinical use [98]. The mode of action of these compounds is inhibition of protein synthesis through binding to the various subunits of the bacterial ribosome [99].
Advancements in genetic technologies have opened up avenues for the manipulation and reprogramming of polyketide synthases for the production of new and novel molecules, which may yield drug candidates with enhanced pharmacological properties [100–102]. Of particular note are the ansamycin group of macrolide molecules, which differ from the molecules previously discussed in that the monomeric unit is 3-amino-5-hydroxybenzoic acid rather than a malonyl coenzyme A derivative. Various ansamycin molecules, such as rifamycin, geldanamycin, herbimycin, and ansamitocins, have been isolated, and their biosynthetic routes have been characterized. Of these, rifamycin, which inhibits bacterial RNA polymerase [103], is widely used in the treatment of tuberculosis. Geldanamycin, biosynthesized by Streptomyces hygroscopicus, and its analogs [104] inhibit heat shock protein 90 (Hsp90) [105] and are being evaluated in human clinical trials as antitumor agents [106].
Trojan Horse Antibiotics
A limiting factor for many antimicrobials and antibiotics is the lack of permeability across the microbial cell membranes. The outer membrane of the Gram-negative bacteria presents a formidable obstacle for drug entry [107]. Such Gram-negative bacteria employ a variety of active importer channels and pores to internalize requisite nutrient material. Nature has ingeniously designed several antimicrobial compounds that utilize a “Trojan horse” strategy to overcome permeability barriers; specifically, these drug molecules are covalently attached to a carrier that facilitates recognition and import through the active transporters. Once inside the target cell, the carrier is removed to release the active drug, which then exerts its antimicrobial activities. This strategy for drug delivery has several advantages. First, active transport of the molecule inside susceptible cells alleviates the need for very high doses for the drug. Second, targeting of the molecule is highly specific only for those microbial cells that have the required transporter to internalize the molecules. Consequently, these “Trojan horse” are not taken up in humans and can be effective microbials even at very low doses.
Notable among this class of compounds are the sideromycins [108, 109], which are characterized by the attachment of the antibiotic molecule to ferric ion–binding chemical components called siderophores. The siderophore–iron complexes are specifically recognized and internalized by dedicated transport machinery in bacteria. Sideromycins consists of structurally diverse molecules including danomycins, salmycins, albomycins, ferrimycins, and microcins. Bioactivities for all these molecules have been established against several human pathogens [110]. Interestingly, as rapidly dividing cancerous cells also display siderophore uptake receptors on their cell surfaces, these molecules are also being evaluated as potential anticancer compounds [109]. Several synthetic conjugates of antibiotic molecules with siderophores have also been generated for evaluation of antimicrobial properties [111].
A different class of “Trojan horse” molecules consists of drugs that are attached to peptide carrier molecules. An example of one such drug is the compound (Z)-l-2-amino-5-phosphono-3-pentenoic acid (APPA), which is a potent inhibitor of the metabolic enzyme threonine synthase, and the “Trojan horse” version consists of APPA attached to a dipeptide. Depending on the amino acids in the dipeptide, the resultant conjugate can either be an antifungal (rhizocticins) or antibacterial (plumbemycin) [112]. Thus, a variety of activities can be encoded in the identical molecule by simply altering the nature of the conjugated peptide. A similar strategy for peptide attachment is utilized in the protein synthesis inhibitor microcin C7 [113].
Future Directions
Maintenance of global health in light of the reemergence of life-threatening infectious diseases requires a continuous influx of new and potent antibiotic molecules that are efficacious and safe for human and animal clinical use. Pathogenic organisms have displayed a remarkable resilience in both developing and propagating mechanisms for overcoming the activities of these antibiotic molecules. The development of new antibiotic molecules relies on two principal paradigms: the characterization of new microbial targets against which new drug molecules can be developed, and the identification of new chemical entities which can be used as antibiotics. Both routes have resulted in the production of very successful drug molecules, and future prospects for antibiotic development are reliant on further progress in these directions. Recent biotechnological advances in the area of microbial genome sequencing have led to a rapid increase in exploration of the microbial metabolome for both novel pathways to target in pathogens and new candidates for use as antibiotics. Semisynthetic chemical derivatization of naturally occurring antibiotics has further expanded upon the repertoire of candidate drugs, and combinatorial synthetic approaches have generated vast chemical libraries which may be screened for compounds with desired biological properties.
Future antibiotic development will require an amalgamation of various academic and industrial approaches such as (1) systems biology to explore metabolic connections and effects of antibiotic molecules on the human host and targeted pathogenic microbes, (2) synthetic biochemistry to generate and diversify arrays of compounds, (3) genomics and bioinformatics to identify and analyze antibiotic biosynthetic gene clusters, and (4) microbial ecological evaluations to better understand the role of naturally occurring antibiotic scaffolds in their native microbial niches. Another promising developing area is combinatorial therapy, in which multiple antibiotic molecules are administered together in order to overcome microbial resistance mechanisms and achieve better efficacy and pathogen clearance. This approach has proven to be very successful in antiviral and oncological applications, and combination regimens have been used for the treatment of tuberculosis for several decades now. Another area of rapid progress in the future promises to be the development of narrow-spectrum antibiotics and better diagnostic tools which would aid in curtailing the indiscriminate use of broad-spectrum antibiotics, and thus reduce the incidence of microbial resistance against antibiotics.
Abbreviations
- Microorganism:
-
A microscopic or submicroscopic organism, too small to be seen by unaided human eye, comprising of bacteria, virus, yeast, protozoa and fungi.
- Pathogen:
-
A disease-causing microorganism which may or may not be infectious.
- Antibiotic:
-
A chemical substance, usually organic in nature, capable of destroying or inhibiting the growth of pathogenic microorganisms.
- Antibiotic resistance:
-
The developed or acquired ability of antibiotic susceptible pathogenic microorganisms to grow and survive despite the inhibitory action of the antibiotic molecules.
- Plasmid:
-
Small, linear or circular genetic elements which can replicate independently of the chromosomal DNA inside a cell.
- Tuberculosis:
-
A highly contagious bacterial disease of humans and animals caused by various strains of Mycobacterium, which normally affects the lungs but can also spread to other organs of the body.
- Malaria:
-
A highly contagious protozoal disease caused by various strains of mosquito-borne Plasmodium.
- Peptide:
-
Short chains of amino acids connected by peptide bonds.
- Polyketide:
-
Compounds characterized by more than two carbonyl groups connected by single intervening carbon atoms.
Bibliography
Sears CL (2005) A dynamic partnership: celebrating our gut flora. Anaerobe 11(5):247–251
Backhed F et al (2005) Host-bacterial mutualism in the human intestine. Science 307(5717):1915–1920
Lindblad WJ (2008) Considerations for determining if a natural product is an effective wound-healing agent. Int J Low Extrem Wounds 7(2):75–81
Forrest RD (1982) Early history of wound treatment. J R Soc Med 75(3):198–205
Forrest RD (1982) Development of wound therapy from the dark ages to the present. J R Soc Med 75(4):268–273
Waksman SA (1947) What is an antibiotic or an antibiotic substance? Mycologia 39(5):565–569
Davies J, Davies D (2010) Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74(3):417–433
Allen HK et al (2010) Call of the wild: antibiotic resistance genes in natural environments. Nat Rev Microbiol 8(4):251–259
Moellering RC Jr (1998) Antibiotic resistance: lessons for the future. Clin Infect Dis 27(Suppl 1):S135–S140 discussion S141–2
Goossens H et al (2005) Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365(9459):579–587
Tacconelli E et al (2008) Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis. J Antimicrob Chemother 61(1):26–38
Mathew AG, Cissell R, Liamthong S (2007) Antibiotic resistance in bacteria associated with food animals: a United States perspective of livestock production. Foodborne Pathog Dis 4(2):115–133
Angulo FJ, Nargund VN, Chiller TC (2004) Evidence of an association between use of anti-microbial agents in food animals and anti-microbial resistance among bacteria isolated from humans and the human health consequences of such resistance. J Vet Med B Infect Dis Vet Public Health 51(8–9):374–379
Singer RS et al (2003) Antibiotic resistance–the interplay between antibiotic use in animals and human beings. Lancet Infect Dis 3(1):47–51
Koch AL (1981) Evolution of antibiotic resistance gene function. Microbiol Rev 45(2):355–378
Mendoza MC et al (1988) Plasmid typing of Shigella sonnei epidemic strains and molecular relationship of their R-plasmids. Eur J Epidemiol 4(2):158–163
Yagupsky P et al (1991) Use of multiple markers for investigation of an epidemic of Shigella sonnei infections in Monroe County, New York. J Clin Microbiol 29(12):2850–2855
Kariuki S et al (1996) Molecular typing of multi-drug resistant Shigella dysenteriae type 1 by plasmid analysis and pulsed-field gel electrophoresis. Trans R Soc Trop Med Hyg 90(6):712–714
Li XZ, Nikaido H (2009) Efflux-mediated drug resistance in bacteria: an update. Drugs 69(12):1555–1623
Lin L, Ling BD, Li XZ (2009) Distribution of the multidrug efflux pump genes, adeABC, adeDE and adeIJK, and class 1 integron genes in multiple-antimicrobial-resistant clinical isolates of Acinetobacter baumannii-Acinetobacter calcoaceticus complex. Int J Antimicrob Agents 33(1):27–32
Van Bambeke F, Balzi E, Tulkens PM (2000) Antibiotic efflux pumps. Biochem Pharmacol 60(4):457–470
Chopra I, Roberts M (2001) Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol Mol Biol Rev 65(2):232–260, second page, table of contents
Rodrigues L et al (2009) The role of efflux pumps in macrolide resistance in Mycobacterium avium complex. Int J Antimicrob Agents 34(6):529–533
Pages JM, Amaral L (2009) Mechanisms of drug efflux and strategies to combat them: challenging the efflux pump of gram-negative bacteria. Biochim Biophys Acta 1794(5):826–833
Wright GD (2005) Bacterial resistance to antibiotics: enzymatic degradation and modification. Adv Drug Deliv Rev 57(10):1451–1470
Bradford PA (2001) Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 14(4):933–951
Jacoby GA, Sutton L (1985) Beta-Lactamases and beta-lactam resistance in Escherichia coli. Antimicrob Agents Chemother 28(5):703–705
Lovmar M et al (2009) Erythromycin resistance by L4/L22 mutations and resistance masking by drug efflux pump deficiency. EMBO J 28(6):736–744
Walsh C (2000) Molecular mechanisms that confer antibacterial drug resistance. Nature 406(6797):775–781
Bugg TD et al (1991) Molecular basis for vancomycin resistance in Enterococcus faecium BM4147: biosynthesis of a depsipeptide peptidoglycan precursor by vancomycin resistance proteins VanH and VanA. Biochemistry 30(43):10408–10415
Bugg TD et al (1991) Identification of vancomycin resistance protein VanA as a D-alanine:D-alanine ligase of altered substrate specificity. Biochemistry 30(8):2017–2021
Walsh CT et al (1996) Bacterial resistance to vancomycin: five genes and one missing hydrogen bond tell the story. Chem Biol 3(1):21–28
Joseph-Horne T, Hollomon DW (1997) Molecular mechanisms of azole resistance in fungi. FEMS Microbiol Lett 149(2):141–149
Lupetti A et al (2002) Molecular basis of resistance to azole antifungals. Trends Mol Med 8(2):76–81
Herath KB, Attygalle AB, Singh SB (2007) Biosynthetic studies of platensimycin. J Am Chem Soc 129(50):15422–15423
Wang J et al (2006) Platensimycin is a selective FabF inhibitor with potent antibiotic properties. Nature 441(7091):358–361
Smanski MJ et al (2009) Engineered Streptomyces platensis strains that overproduce antibiotics platensimycin and platencin. Antimicrob Agents Chemother 53(4):1299–1304
Jayasuriya H et al (2007) Isolation and structure of platencin: a FabH and FabF dual inhibitor with potent broad-spectrum antibiotic activity. Angew Chem Int Ed Engl 46(25):4684–4688
Wang J et al (2007) Discovery of platencin, a dual FabF and FabH inhibitor with in vivo antibiotic properties. Proc Natl Acad Sci USA 104(18):7612–7616
Siggaard-Andersen M et al (1994) The fabJ-encoded beta-ketoacyl-[acyl carrier protein] synthase IV from Escherichia coli is sensitive to cerulenin and specific for short-chain substrates. Proc Natl Acad Sci USA 91(23):11027–11031
Machutta CA et al (2010) Slow onset inhibition of bacterial beta-ketoacyl-acyl carrier protein synthases by thiolactomycin. J Biol Chem 285(9):6161–6169
Johansson P et al (2008) Inhibition of the fungal fatty acid synthase type I multienzyme complex. Proc Natl Acad Sci USA 105(35):12803–12808
Nishida I, Kawaguchi A, Yamada M (1986) Effect of thiolactomycin on the individual enzymes of the fatty acid synthase system in Escherichia coli. J Biochem 99(5):1447–1454
McFadden JM et al (2005) Application of a flexible synthesis of (5R)-thiolactomycin to develop new inhibitors of type I fatty acid synthase. J Med Chem 48(4):946–961
Okuhara M et al (1980) Studies on new phosphonic acid antibiotics. III. Isolation and characterization of FR-31564, FR-32863 and FR-33289. J Antibiot (Tokyo) 33(1):24–28
Okuhara M et al (1980) Studies on new phosphonic acid antibiotics. I. FR-900098, isolation and characterization. J Antibiot (Tokyo) 33(1):13–17
Lell B et al (2003) Fosmidomycin, a novel chemotherapeutic agent for malaria. Antimicrob Agents Chemother 47(2):735–738
Missinou MA et al (2002) Fosmidomycin for malaria. Lancet 360(9349):1941–1942
Wiesner J, Jomaa H (2007) Isoprenoid biosynthesis of the apicoplast as drug target. Curr Drug Targets 8(1):3–13
Brown AC, Parish T (2008) Dxr is essential in Mycobacterium tuberculosis and fosmidomycin resistance is due to a lack of uptake. BMC Microbiol 8:78
Fokin AA et al (2007) Synthesis of the antimalarial drug FR900098 utilizing the nitroso-ene reaction. Org Lett 9(21):4379–4382
Johannes TW et al (2010) Deciphering the late biosynthetic steps of antimalarial compound FR-900098. Chem Biol 17(1):57–64
Kurz T et al (2007) Conformationally restrained aromatic analogues of fosmidomycin and FR900098. Arch Pharm (Weinheim) 340(7):339–344
Metcalf WW, van der Donk WA (2009) Biosynthesis of phosphonic and phosphinic acid natural products. Annu Rev Biochem 78:65–94
Rohrich RC et al (2005) Reconstitution of an apicoplast-localised electron transfer pathway involved in the isoprenoid biosynthesis of Plasmodium falciparum. FEBS Lett 579(28):6433–6438
Wang K et al (2010) Inhibition of the Fe(4)S(4)-cluster-containing protein IspH (LytB): electron paramagnetic resonance, metallacycles, and mechanisms. J Am Chem Soc 132(19):6719–6727
Wang W et al (2010) Bioorganometallic mechanism of action, and inhibition, of IspH. Proc Natl Acad Sci USA 107(10):4522–4527
Liu CI et al (2008) A cholesterol biosynthesis inhibitor blocks Staphylococcus aureus virulence. Science 319(5868):1391–1394
Song Y et al (2009) Inhibition of staphyloxanthin virulence factor biosynthesis in Staphylococcus aureus: in vitro, in vivo, and crystallographic results. J Med Chem 52(13):3869–3880
Song Y et al (2009) Phosphonosulfonates are potent, selective inhibitors of dehydrosqualene synthase and staphyloxanthin biosynthesis in Staphylococcus aureus. J Med Chem 52(4):976–988
Kodama I, Kamiya K, Toyama J (1999) Amiodarone: ionic and cellular mechanisms of action of the most promising class III agent. Am J Cardiol 84(9A):20R–28R
Isoherranen N et al (2004) Role of itraconazole metabolites in CYP3A4 inhibition. Drug Metab Dispos 32(10):1121–1131
Paniz-Mondolfi AE et al (2009) Amiodarone and itraconazole: a rational therapeutic approach for the treatment of chronic Chagas’ disease. Chemotherapy 55(4):228–233
Chen W, Zeng H, Tan H (2000) Cloning, sequencing, and function of sanF: A gene involved in nikkomycin biosynthesis of Streptomyces ansochromogenes. Curr Microbiol 41(5):312–316
Stauffer CS et al (2007) Total synthesis and antifungal activity of a carbohydrate ring-expanded pyranosyl nucleoside analogue of nikkomycin B. J Org Chem 72(26):9991–9997
Yamaguchi H et al (1986) Capuramycin, a new nucleoside antibiotic. Taxonomy, fermentation, isolation and characterization. J Antibiot (Tokyo) 39(8):1047–1053
Hotoda H et al (2003) Synthesis and antimycobacterial activity of capuramycin analogues. Part 2: acylated derivatives of capuramycin-related compounds. Bioorg Med Chem Lett 13(17):2833–2836
Hotoda H et al (2003) Synthesis and antimycobacterial activity of capuramycin analogues. Part 1: substitution of the azepan-2-one moiety of capuramycin. Bioorg Med Chem Lett 13(17):2829–2832
Reddy VM, Einck L, Nacy CA (2008) In vitro antimycobacterial activities of capuramycin analogues. Antimicrob Agents Chemother 52(2):719–721
Isono F et al (1989) Mureidomycins A-D, novel peptidylnucleoside antibiotics with spheroplast forming activity. III. Biological properties. J Antibiot (Tokyo) 42(5):674–679
Isono F et al (1989) Mureidomycins A-D, novel peptidylnucleoside antibiotics with spheroplast forming activity. II. Structural elucidation. J Antibiot (Tokyo) 42(5):667–673
Inukai M et al (1989) Mureidomycins A-D, novel peptidylnucleoside antibiotics with spheroplast forming activity I Taxonomy, fermentation, isolation and physico-chemical properties. J Antibiot (Tokyo) 42(5):662–666
Hancock RE, Sahl HG (2006) Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat Biotechnol 24(12):1551–1557
Sahl HG (2006) Optimizing antimicrobial host defense peptides. Chem Biol 13(10):1015–1017
Peschel A, Sahl HG (2006) The co-evolution of host cationic antimicrobial peptides and microbial resistance. Nat Rev Microbiol 4(7):529–536
Willey JM, van der Donk WA (2007) Lantibiotics: peptides of diverse structure and function. Annu Rev Microbiol 61:477–501
Ekkelenkamp MB et al (2005) Isolation and structural characterization of epilancin 15X, a novel lantibiotic from a clinical strain of Staphylococcus epidermidis. FEBS Lett 579(9):1917–1922
Castiglione F et al (2008) Determining the structure and mode of action of microbisporicin, a potent lantibiotic active against multiresistant pathogens. Chem Biol 15(1):22–31
Bauer R, Dicks LM (2005) Mode of action of lipid II-targeting lantibiotics. Int J Food Microbiol 101(2):201–216
Cao LT et al (2007) Efficacy of nisin in treatment of clinical mastitis in lactating dairy cows. J Dairy Sci 90(8):3980–3985
Wu J, Hu S, Cao L (2007) Therapeutic effect of nisin Z on subclinical mastitis in lactating cows. Antimicrob Agents Chemother 51(9):3131–3135
Fernandez L et al (2008) The bacteriocin nisin, an effective agent for the treatment of staphylococcal mastitis during lactation. J Hum Lact 24(3):311–316
Nguyen KT et al (2006) Combinatorial biosynthesis of novel antibiotics related to daptomycin. Proc Natl Acad Sci USA 103(46):17462–17467
Penn J et al (2006) Heterologous production of daptomycin in Streptomyces lividans. J Ind Microbiol Biotechnol 33(2):121–128
Baltz RH, Miao V, Wrigley SK (2005) Natural products to drugs: daptomycin and related lipopeptide antibiotics. Nat Prod Rep 22(6):717–741
Miao V et al (2005) Daptomycin biosynthesis in Streptomyces roseosporus: cloning and analysis of the gene cluster and revision of peptide stereochemistry. Microbiology 151(Pt 5):1507–1523
Tally FP, DeBruin MF (2000) Development of daptomycin for Gram-positive infections. J Antimicrob Chemother 46(4):523–526
Henken S et al (2010) Efficacy profiles of daptomycin for treatment of invasive and noninvasive pulmonary infections with Streptococcus pneumoniae. Antimicrob Agents Chemother 54(2):707–717
Fowler VG Jr et al (2006) Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med 355(7):653–665
Walsh C, Freel Meyers CL, Losey HC (2003) Antibiotic glycosyltransferases: antibiotic maturation and prospects for reproGramming. J Med Chem 46(16):3425–3436
Sussmuth RD, Wohlleben W (2004) The biosynthesis of glycopeptide antibiotics–a model for complex, non-ribosomally synthesized, peptidic secondary metabolites. Appl Microbiol Biotechnol 63(4):344–350
Donadio S et al (2005) Comparative analysis and insights into the evolution of gene clusters for glycopeptide antibiotic biosynthesis. Mol Genet Genomics 274(1):40–50
Levine DP (2006) Vancomycin: a history. Clin Infect Dis 42(Suppl 1):S5–S12
Gonzalez C et al (1999) Bacteremic pneumonia due to Staphylococcus aureus: A comparison of disease caused by methicillin-resistant and methicillin-susceptible organisms. Clin Infect Dis 29(5):1171–1177
Scheinfeld N (2007) A comparison of available and investigational antibiotics for complicated skin infections and treatment-resistant Staphylococcus aureus and enterococcus. J Drugs Dermatol 6(1):97–103
Maki H, Miura K, Yamano Y (2001) Katanosin B and plusbacin A(3), inhibitors of peptidoglycan synthesis in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 45(6):1823–1827
Fulco P, Wenzel RP (2006) Ramoplanin: a topical lipoglycodepsipeptide antibacterial agent. Expert Rev Anti Infect Ther 4(6):939–945
Weissman KJ, Leadlay PF (2005) Combinatorial biosynthesis of reduced polyketides. Nat Rev Microbiol 3(12):925–936
Menninger JR (1995) Mechanism of inhibition of protein synthesis by macrolide and lincosamide antibiotics. J Basic Clin Physiol Pharmacol 6(3–4):229–250
McDaniel R et al (1995) Rational design of aromatic polyketide natural products by recombinant assembly of enzymatic subunits. Nature 375(6532):549–554
Katz L (1997) Manipulation of modular polyketide synthases. Chem Rev 97(7):2557–2576
Ruan X et al (1997) Acyltransferase domain substitutions in erythromycin polyketide synthase yield novel erythromycin derivatives. J Bacteriol 179(20):6416–6425
Floss HG, Yu TW (2005) Rifamycin-mode of action, resistance, and biosynthesis. Chem Rev 105(2):621–632
Kim W et al (2009) Rational biosynthetic engineering for optimization of geldanamycin analogues. Chembiochem 10(7):1243–1251
Bedin M et al (2004) Geldanamycin, an inhibitor of the chaperone activity of HSP90, induces MAPK-independent cell cycle arrest. Int J Cancer 109(5):643–652
Neckers L, Schulte TW, Mimnaugh E (1999) Geldanamycin as a potential anti-cancer agent: its molecular target and biochemical activity. Invest New Drugs 17(4):361–373
Delcour AH (2009) Outer membrane permeability and antibiotic resistance. Biochim Biophys Acta 1794(5):808–816
Mollmann U et al (2009) Siderophores as drug delivery agents: application of the “Trojan Horse” strategy. Biometals 22(4):615–624
Braun V et al (2009) Sideromycins: tools and antibiotics. Biometals 22(1):3–13
Ballouche M, Cornelis P, Baysse C (2009) Iron metabolism: a promising target for antibacterial strategies. Recent Pat Antiinfect Drug Discov 4(3):190–205
Wencewicz TA et al (2009) Is drug release necessary for antimicrobial activity of siderophore-drug conjugates? Syntheses and biological studies of the naturally occurring salmycin “Trojan Horse” antibiotics and synthetic desferridanoxamine-antibiotic conjugates. Biometals 22(4):633–648
Borisova SA et al (2010) Biosynthesis of rhizocticins, antifungal phosphonate oligopeptides produced by Bacillus subtilis ATCC6633. Chem Biol 17(1):28–37
Vondenhoff GH et al (2011) Characterization of peptide chain length and constituency requirements for YejABEF-mediated uptake of Microcin C analogues. J Bacteriol 193(14):3618–3623
Acknowledgments
Research in the Nair lab is supported by the NIGMS. We thank Neha Garg, Yue Hao, and Zhi Li for stimulating discussions.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Agarwal, V., Nair, S.K. (2013). Antibiotics for Emerging Pathogens. In: Kanki, P., Grimes, D. (eds) Infectious Diseases. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5719-0_2
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5719-0_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5718-3
Online ISBN: 978-1-4614-5719-0
eBook Packages: MedicineMedicine (R0)