Abstract
Prion diseases are characterized by the deposition of PrPSc, an abnormal form of the normal cellular protein, PrPc in the brain. The unique nature of human prion diseases includes their pathogenesis, mode of transmission and neuropathology. In humans, a long incubation time, rapid and dramatic evolution of the disease course and always a lethal outcome are key features of the clinical syndrome. The clinical diagnosis in sCJD is supported by detection of periodic sharp and slow wave complexes (PSWCs) in the electroencephalogram, 14-3-3 proteins in the cerebrospinal fluid (CSF) and hyperintense signal changes in the basal ganglia, thalamus and cortical areas on magnetic resonance imaging (MRI). These three tests became part of the clinical diagnostic criteria for probable CJD. The sensitivity of diagnostic tests varies across molecular CJD subtypes. Alzheimer’s disease and Lewy body dementia are the most frequent differential diagnoses in elderly patients, while chronic inflammatory CNS disorders have to be considered in younger patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
13.1 Introduction
Human prion diseases share many common features—transmissibility in animal experiments, fatal progressive disease course, neuronal loss, astrogliosis, and PrPSc deposition in the brain. Despite this, several forms are distinguished depending on assumed pathophysiology: genetic, acquired, and sporadic disease forms. In addition, sporadic disease forms display clinicopathological diversity, which origins in codon 129 PRNP genotype and PrPSc type (see molecular disease subtypes). In clinical terms, signs and symptoms of the disease are heterogeneous and comprise a wide spectrum of neurological and psychiatric abnormalities. Because of this and because of the fact that a definite early clinical test or biomarker is still lacking, several diagnostic investigations have to be taken into account and considered in the context of comprehensive clinical examination, thoughtful evaluation of the clinical history and consideration of other differential, potentially curable diagnosis.
A definite and final diagnosis requires invasive procedures such as brain biopsy or analysis of brain material at autopsy. Early detection will become increasingly important once forthcoming effective therapies are available (Krammer et al. 2009). Clinical diagnostic criteria for sCJD were first suggested 30 years ago, using a combination of distinctive clinical features and best available investigations, which at that time was EEG (Masters et al. 1979). In recent years, there is a substantial progress in developing other specialized investigations, including useful surrogate biomarkers in the cerebrospinal fluid and brain imaging, and clinical diagnostic criteria have been amended (Collins et al. 2006; Zerr et al. 2000, 2009).
13.2 Cerebrospinal Fluid
Cerebrospinal fluid (CSF) is the main component of the brain extracellular space and participates in the exchange of many biochemical products in the central nervous system (CNS). Consequently, CSF contains a dynamic and complex mixture of proteins, which reflects physiological or pathological state of the CNS. CSF analysis is an important part in clinical neurology and is used to diagnose various inflammatory and malignant disorders and recently also neurodegenerative disorders. The alterations in CSF composition are also discussed to reflect pathological changes in the brain and thus contribute to a better understanding of the pathophysiology of the underlying disorders affecting CNS.
For many years, CSF analysis in CJD has been used to exclude brain inflammation in patients with rapid progressive dementia. Since modern proteomic technologies allow us to identify proteins and protein patters in human fluids, the CSF analysis in dementia disorders became even more important. Historically, first CSF abnormalities in human prion diseases were reported by Harrington et al. (1986), who identified two proteins spots, named p130/131 in the CSF of CJD patients. Decades later, these proteins became known as 14-3-3 proteins and were the first CSF biomarker ever used in clinical criteria in patients with a neurodegenerative dementia.
13.2.1 Routine
The routine examination of CSF from patients with CJD or GSS usually reveals normal results. An unspecific increase in total protein, the presence of oligoclonal IgG bands or raised cell count is an extremely rare finding (see Table 13.1). In the most comprehensive study on this subject, data from 450 patients with sporadic CJD and 47 patients with other TSEs were analyzed as part of an EC-supported multinational study. Raised white cell counts of >5 cells/μl were found in three out of 298 patients with sporadic CJD, in two with cell counts of 7 cells/μl and in one of 20 cells/μl. Total protein concentrations of >0.9 g/l were found in five of 438 patients with sporadic CJD, but none had a concentration of >1 g/l. CSF oligoclonal IgG was detected in eight out of 182 sporadic CJD patients. Among patients with other TSEs, six had elevated cell counts ranging from 6 to 14 cells/μl, but none had total protein concentrations of >0.9 g/l and one patient had detectable oligoclonal IgG. None of the patients with sporadic CJD or other TSEs had abnormalities in all three tests.
As a rule, inflammatory CSF findings exclude the diagnosis of a human prion disease.
13.2.2 14-3-3
14-3-3 proteins were initially described as abundant, acidic brain proteins and their name is derived from the combination of its fraction number on DEAE-cellulose chromatography and migration position in the subsequent starch gel electrophoresis. Despite the fact that the pathology behind the elevated level of 14-3-3 in CJD is still a question of debate, the detection of 14-3-3 protein in CSF is part of clinical diagnostic criteria for probable sCJD, because of its high sensitivity and, even more important, high predictive values in clinical setting. The large number of studies proved that in the appropriate clinical circumstances a positive 14-3-3 is highly sensitive and specific for sCJD diagnosis. 14-3-3 detection correlated with clinical diagnosis in 85–94% in sporadic CJD (Table 13.2). The sensitivity of 14-3-3 varies among TSE subtypes (Table 13.3). Patients with iatrogenic and gCJD have elevated 14-3-3 levels in 75% and 78% of the cases, respectively. In variant CJD (vCJD), only 40% patients were positive, while GSS and FFI patients were almost always negative in this test.
Biological parameters significantly influence the sensitivity of 14-3-3 test in patients with sCJD, i.e., disease duration, codon 129 genotype, age at onset and time of the lumbar puncture. In general, the 14-3-3 test displays best sensitivity in patients older than 40 years with short disease duration, homozygous at codon 129 genotype and when lumbar puncture is performed at later disease stages (Sanchez-Juan et al. 2006). Differences in the sensitivity of 14-3-3 test are also observed between classical vs. nonclassical CJD types (see molecular disease subtypes). In classical CJD (which basically fulfill the criteria of having the tendency to be older, homozygous for methionine at codon 129, short disease duration and rapid progression), 14-3-3 test sensitivity is superior to nonclassical (or atypical) cases.
Although this test was often found to be positive at onset of the first neurological symptoms, higher sensitivity was reported in the middle or late stage of the disease. Moreover, in the terminal stage of disease 14-3-3 level might decrease in CSF, but this observation is based on case reports and might reflect extremely long disease duration.
13.2.3 Tau/p-tau
Tau concentration in CSF of CJD patients is highly increased and its quantitative analysis is a good diagnostic tool for CJD. Several studies revealed that the optimum cut-off point for CJD is at 1.300 pg/ml. This cut-off is three times higher than levels reported for Alzheimer’s dementia, and in the latter, only rare cases display such extreme tau levels as CJD patients. Determination of tau has shown to yield specificity and sensitivity comparable to those for 14-3-3 testing. Concerning the phosphorylated tau isoforms in CSF of CJD, tau phosphorylated at threonine 181 (p-tau) was significantly raised in sCJD as well in vCJD. Interestingly, tau concentration was lower in vCJD when compared to sCJD, whereas p-tau concentration was much higher in vCJD than in sCJD.
13.2.4 Other CSF Markers
Besides common TSE markers, several other proteins have been proposed as possibly useful in the diagnosis of the human TSE. So far, they were tested in small numbers of patients and need further rigorous testing and thoughtful validation of their potentials to be classified as biomarkers in human prion disorders (Table 13.4).
13.3 Magnetic Resonance Imaging
13.3.1 General Introduction
MRI has played an important role in the diagnosis of CJD (Tschampa et al. 2005; Urbach et al. 1998). In 1988, a hyperintense signal of the basal ganglia on T2-weighted images was first described as a characteristic finding in sCJD patients, followed by further case reports. Subsequently, systematic studies on the sensitivity and specificity of hyperintense signal changes in the striatum in sCJD were performed. Along with the availability of methods, the early MR studies mainly focused on T2-weighted, proton density weighted (Finkenstaedt et al. 1996; Schröter et al. 2000), and to a lesser extent on FLAIR (Choi et al. 2009) imaging, while current studies mainly rely on DWI and FLAIR MRI (Matoba et al. 2001; Young et al. 2005).
With the emergence of more sensitive MRI techniques, such as FLAIR (fluid-attenuated inversion recovery) and DWI (diffusion-weighted image), cortical signal increase was additionally observed in sCJD patients and hyperintense basal ganglia were detected more frequently (Fig. 13.1). Using FLAIR- and diffusion-weighted imaging, signal increase of the cortex has been reported even more frequently than basal ganglia signal increase. Apart from the cortex and basal ganglia hyperintensity, signal increase has also been reported for the hippocampus, thalamus, and cerebellum and for the mesencephalon. In general, the most sensitive technique to date seems to be DWI, followed by FLAIR and T2 imaging.
13.3.2 Test Sensitivity
In the diagnosis of sCJD, the hyperintense signal abnormalities in the striatum have a sensitivity of 58–78% (Choi et al. 2009; Cohen et al. 2011; Fulbright et al. 2006) and among non-CJD dementia patients, the specificity is higher (82–93%) (Choi et al. 2009; Fulbright et al. 2006). With the introduction of diffusion-weighted imaging, MR changes are detected earlier at the disease (Collins et al. 2006; Demaerel et al. 1999; Heinemann et al. 2007b; Holsinger et al. 2006; Hsich et al. 1996; Jesse et al. 2009; Josephs et al. 2009; Kelley et al. 2008) and serial imaging studies allowed to follow the disease progression by MR imaging (Kelley et al. 2008; Kettlun et al. 2003; Korczyn 1991). DW imaging improves interobserver reliability (Demaerel et al. 1999).
13.3.3 Changes During the Disease
Data on serial MR examinations in CJD are limited in the literature. In early disease stages, characteristic basal ganglia lesions are not found in up to one-third of the patients (Meissner et al. 2008). In single case reports, basal ganglia lesions were only developed during the disease course (Demaerel et al. 1999; Parazzini et al. 2003; Tomita et al. 2004; Tribl et al. 2002; Matoba et al. 2001). According to Ukisu and colleagues, on DW MRI cortical changes (9/9 cases) preceded the hyperintensities in the basal ganglia (5/9 cases at early stage). During the course of the disease, there is generally an expansion of the signal changes and progressive cerebral atrophy (Tribl et al. 2002). In the late stage of the disease, the diffusion changes may disappear (Arruda et al. 2004; Matoba et al. 2001; Shyu et al. 1996; Tribl et al. 2002).
13.4 EEG
For decades, periodic sharp wave complexes (PSWCs) in the EEG were reported to represent the most typical finding in the course of sCJD. The apparent advantages of the EEG are: this investigation is widely available, noninvasive and can easily be repeated several times. At onset, the EEG might show only nonspecific changes such as background slowing of alpha-activity and dysrhythmia. As disease progresses, slow periodic complexes might appear occasionally, later the typical periodic pattern is seen. In end stage of CJD, the EEG might show an isoelectric line. PSWCs might be provoked by acoustic or tactile stimulation. Typical periodic patterns (Fig. 13.2) are observed in 60–70% of all cases after about 12 weeks (median) from disease onset but might occur as early as 3 weeks after onset. They may disappear at late disease stages. Since the term PSWCs has not been operationalized before, sensitivity of the detection of this abnormality varied among studies. EEG criteria have been suggested (Fig. 13.3). According to these criteria, PSWCs are detectable in two-thirds of CJD patients at mid and late disease stages (sensitivity 64%). The sensitivity increases when several EEG recordings are performed. Specificity is comparable high (89%), and a good interrater agreement was achieved (kappa 0.95).
13.5 Molecular Disease Subtype Specific Diagnosis
Recently, a molecular basis has been defined, which might explain the clinical and pathological disease heterogeneity. The polymorphism for methionine (M) or valine (V) at codon 129 of PRNP gene has been shown to influence the clinical features of sCJD. In 1996, two PrPSc subtypes in brain homogenates of sCJD patients were identified. The polymorphism at codon 129 and the prion protein types 1 and 2 were the basis for a new molecular classification of sCJD, which replaced the previous attempts. Currently, patients with the MM1/MV1 subtype, who display a short disease duration, dementia, myoclonus, and typical EEG pattern, are frequently referred to as having “classical” or “common” CJD subtype. Other (“nonclassical” and “atypical”) subtypes are rare (Fig. 13.4).
The discovery of several distinct molecular CJD subtypes explains many features observed in sporadic CJD patients. The clinical presentation at early disease stage is peculiar in most disease subtypes and the detailed investigation of the clinical syndrome often allows the assignment to the distinct CJD subtype. This observation is supported by EEG, CSF, and MRI results, which appear in subtype distinctive pattern as described below.
Table 13.5 gives an overview of the diagnostic investigations in distinct molecular CJD subtypes.
EEG is abnormal in all disease subtypes, but the typical periodic sharp and slow wave pattern (PSWC) is observed in MM1/MV1 subtype only and is rare in MM2/MV2/VV1-2 patients. Because of a long time CJD diagnosis was based on the triad: dementia, myoclonus, and PSWC in EEG, we might speculate that the frequency of so-called classical myoclonic CJD type was overestimated in earlier studies because of the selection bias.
As mentioned above, results of various CSF tests vary considerably by disease subtype. 14-3-3 test sensitivity is best in MM1 and VV patients and has the lowest sensitivity in MV2 and MM2 patients. This can easily be explained by quantitative analysis of this protein in CSF. Figure 13.5 displays results of the 14-3-3 test ELISA in various CJD subtypes, demonstrating low levels in MM2 and MV2 patients. Similar results were obtained for CSF tau protein (Sanchez-Juan et al. 2006; Heinemann et al. 2007a).
A recent analysis of a multicentre international study aimed to describe the brain MRI findings associated with each of the sCJD molecular subtypes. MRI scans were evaluated in 211 CJD patients with various disease subtypes. Although basal ganglia hyperintensities on the MRI represented a consistent finding in all subtypes (except VV1), the frequency and location of cortex hyperintensities as well as the presence or absence of thalamus involvement varied between the subtypes.
Across all molecular subtypes, VV2 patients showed the most frequent involvement of basal ganglia and thalamus. Cerebral cortical signal increase was usually restricted to less than three regions and most frequently found in the cingulate gyrus (Table 13.6 and Fig. 13.6).
The most characteristic MRI lesion patterns were found in MV2 and VV2 showing predominant involvement of thalamus and basal ganglia. Limited cortical signal increase was significantly related to PrPSc type 2. A further possible characteristic lesion pattern was found in VV1 showing widespread cortical hyperintensities and absence of basal ganglia signal alterations. In the other subtypes, there was a higher overlap between cortical and subcortical involvement. MV2 subtype was characterized by basal ganglia and thalamic involvement (Krasnianski et al. 2006). The pulvinar sign according to current criteria was identified in the MV2 subtype only (Collie et al. 2003). Due to the generally high frequency of thalamic hyperintensities in MV2, this subtype is the most likely to be mistaken for variant CJD (vCJD) on MRI.
13.6 Genetic TSE
Patients with inherited forms of human prion diseases are diagnosed by genetic analysis of the PRNP gene. However, the family history of a prion disease might be absent in a considerable number of patients, thus it is important to know the outcomes of conventional tests such as EEG, CSF, and MRI.
Only limited data are available for genetic TSE. Data from the literature are restricted to single case reports on patients with rare mutations. The most comprehensive studies have been carried out in genetic CJD with E200K and V210I mutations and in fatal familial insomnia (FFI).
PSWCs are not recorded in Gerstmann–Sträussler–Scheinker (GSS) syndrome, fatal familial insomnia, and in transmitted forms of the disease such as Kuru, iCJD, and vCJD. In patients with genetic prion diseases, PSWCs are only occasionally seen with exception of patients with the mutation at the codon 200 and 210 (Korczyn 1991; Ladogana et al. 2005). In these patients, the sensitivity of the EEG is almost the same as in sCJD (Zerr et al. 1998a).
So far there has been only limited information available about biochemical markers in genetic transmissible spongiform encephalopathies (gTSE), although they represent 10–15% of human TSEs. However, there is a special interest in studying biochemical markers in CSF to improve diagnosis and to monitor disease progression in genetic forms, especially when disease phenotype differs from that of typical sporadic CJD (Ladogana et al. 2009).
Concerning CSF 14-3-3 testing, sensitivity varies across the spectrum of genetic mutations. Apparently, the types of mutation significantly influence the biomarker concentration in the CSF and, thus, test sensitivity. According to current information, changes in the CSF of patients with familial genetic forms of CJD (gCJD) are comparable to those found in sCJD samples. Table 13.7 gives an overview. 14-3-3 proteins are detectable in patients with an E200K and V210I mutation (Rosenmann et al. 1997; Zerr et al. 1998a) but only in rare cases in FFI and GSS (Zerr et al. 1998a, b).
In a multicenter EC-funded study on biomarkers in CJD, the crude analyses of disease modifying factors on 14-3-3 test in gCJD revealed that age at onset and PRNP codon 129 genotype influenced sensitivity. Age at onset correlated significantly with 14-3-3 test sensitivity in gCJD, being lower in those patients with disease onset before 40 years. These data parallel the results of the same analysis performed on sporadic CJD (Ladogana et al. 2009; Sanchez-Juan et al. 2006). Interestingly, the PRNP codon 129 genotype seemed to influence 14-3-3 sensitivity in gCJD in a different way as in sporadic CJD. Valine homozygous gCJD patients had a statistically significant lower sensitivity in 14-3-3 test than heterozygous patients, but sensitivity was not significantly lower when adjusted for the mutation. This might be due to the fact that the PRNP mutations coupled with valine alleles (P105T, R208H, D178N, and E196K) yielded lower sensitivity to 14-3-3. However, numbers were too low to draw any definite conclusions (Ladogana et al. 2009).
An important point of interest for biomarkers in gTSEs is to analyze their potential use as surrogate parameter for disease progression in clinical trials. These data might be used for selection of homogenous patients group when testing new drugs to obtain a more reliable assessment of their effects on the disease progression and to reduce the sample size needed in clinical trials. In addition, such biomarkers might be used to monitor the disease progression (Ladogana et al. 2009).
Some data are available concerning MRI changes in gCJD cases, based on few larger studies and case reports. Of special importance, thalamostriatal diffusion reductions have been shown to precede disease onset in E200K prion mutation carriers and might therefore serve as an early diagnostic marker (Lee et al. 2009).
A series of case reports and a small number of larger imaging studies have described MRI changes in different gCJD point mutations (20–22). They illustrated a variety of distinctive features found mainly in the basal ganglia, thalamus, and cortical areas. In patients with E200K mutation, 50% were reported to display high signal intensities. Using FLAIR or DWI, the sensitivity is apparently even higher (Fulbright et al. 2008). Most common changes are reported in gyrus cinguli and are less notable in other cortical areas. An overview of reports from the literature is given in Table 13.8.
13.7 Differential Diagnosis
The differential diagnosis of sCJD includes a large number of neurological and psychiatric diseases. In most cases, the diagnosis of CJD as the primary diagnosis is not taken into account when patients are admitted to hospital. Alzheimer’s disease is the most important differential diagnosis in older patients. Rapid disease courses, in particular, can rarely be discriminated from CJD, especially when myoclonus is present. Dementia with Lewy bodies is another neurodegenerative dementia that must be considered. Because of the typical clinical presentation in CJD might be a rapid evolving neurological disorder, the spectrum of differential diagnosis also comprises some potentially treatable conditions. Figure 13.7 and Table 13.9 give an overview on differential diagnoses in CJD.
With respect to the clinical syndrome, we could demonstrate that ataxia (77%) and dysmetria (48%) was significantly more frequent in CJD than in AD or DLB patients (Edler et al. 2009). Comparable results for the occurrence of ataxia in CJD were seen by Parchi et al. (1996), Tschampa et al. (2001), and Van Everbroeck et al. (2004) as shown in Table 13.10.
On contrary, hypokinesia was found four to five times more often in AD and DLB than in CJD patients. Investigating constellations of movement disturbances using the principal component analysis, prominent statistical effects are seen, when comparing CJD with AD patients (Table 13.10). In patients presenting ataxia without hypokinesia, the diagnosis of CJD was the most likely diagnosis. In AD, hypokinesia without ataxia is more typical.
13.8 Criteria
The symptoms and signs of disease in patients with prion diseases are heterogeneous. This heterogeneity is the result of the involvement of various brain structures and still undefined biological determinants influencing disease course. The classification criteria are based on the etiology of the disease, which can be divided into four categories: sporadic, iatrogenic, familial/genetic, and variant CJD (WHO 2003; Will et al. 2000; Zerr et al. 2009). Criteria for sporadic CJD have been amended by 14-3-3 CSF test and more recently, MRI. They are displayed in Fig. 13.8.
13.9 Conclusions
Creutzfeldt–Jakob disease is a frequent cause of rapid progressive dementia. Achieving a correct early diagnosis has important implications for (1) distinguishing prion disease from other, potentially treatable diseases, (2) preventing infectious material from being distributed via blood transfusions, surgery, or organ donations, and (3) selecting homogeneous population for upcoming drug trials. The clinical diagnosis of sCJD is supported by detection of biomarkers in blood or CSF, including the biomarkers such as 14-3-3 and tau/phosphorylated tau. In the differential diagnosis of neurodegenerative disorders, elevated levels of these proteins support the diagnosis of sCJD with a sensitivity of 85–95% and specificity of 80%. Recently, it has been demonstrated that advanced brain imaging techniques significantly contribute to the clinical diagnosis on one hand, but might also help in the early differentiation in molecular disease subtypes in sporadic CJD on the other hand. Clinical diagnostic criteria are amended and are based on detailed algorithm.
References
Aksamit AJ Jr, Preissner CM, Homburger HA (2001) Quantitation of 14-3-3 and neuron-specific enolase proteins in CSF in Creutzfeldt-Jakob disease. Neurology 57:728–30
Alberti C, Gonzalez J, Maldonado H, Medina F, Barriga A, Garcia L, Kettlun A, Collados L, Puente J, Cartier L, Valenzuela M (2009) Comparative study of CSF neurofilaments in HTLV-1-associated myelopathy/tropical spastic paraparesis and other neurological disorders. AIDS Res Hum Retroviruses 25:803–9
Albrecht D, Garcia L, Cartier L, Kettlun AM, Vergara C, Collados L, Valenzuela MA (2006) Trophic factors in cerebrospinal fluid and spinal cord of patients with tropical spastic paraparesis, HIV, and Creutzfeldt-Jakob disease. AIDS Res Hum Retroviruses 22:248–54
Arruda WO, Bordignon KC, Milano JB, Ramina R (2004) Creutzfeldt-Jakob disease, Heidenhain variant: case report with MRI (DWI) findings. Arq Neuropsiquiatr 62:347–52
Beaudry P, Cohen P, Brandel JP, Delasnerie-Laupretre N, Richard S, Launay JM, Laplanche JL (1999) 14-3-3 protein, neuron-specific enolase, and S-100 protein in cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. Dement Geriatr Cogn Disord 10:40–6
Cartier L, Garcia L, Kettlun AM, Castaneda P, Collados L, Vasquez F, Giraudon P, Belin MF, Valenzuela MA (2004) Extracellular matrix protein expression in cerebrospinal fluid from patients with tropical spastic paraparesis associated with HTLV-I and Creutzfeldt-Jakob disease. Scand J Clin Lab Invest 64:101–7
Castellani RJ, Colucci M, Xie Z, Zou W, Li C, Parchi P, Capellari S, Pastore M, Rahbar MH, Chen SG, Gambetti P (2004) Sensitivity of 14-3-3 protein test varies in subtypes of sporadic Creutzfeldt-Jakob disease. Neurology 63:436–42
Chitravas N, Jung RS, Kofskey DM, Blevins JE, Gambetti P, Leigh RJ, Cohen ML (2011) Treatable neurological disorders misdiagnosed as Creutzfeldt-Jakob disease. Ann Neurol 70:437–44
Choe LH, Green A, Knight RS, Thompson EJ, Lee KH (2002) Apolipoprotein E and other cerebrospinal fluid proteins differentiate ante mortem variant Creutzfeldt-Jakob disease from ante mortem sporadic Creutzfeldt-Jakob disease. Electrophoresis 23:2242–6
Choi BY, Kim SY, Seo SY, An SS, Kim S, Park SE, Lee SH, Choi YJ, Kim SJ, Kim CK, Park JS, Ju YR (2009) Mutations at codons 178, 200–129, and 232 contributed to the inherited prion diseases in Korean patients. BMC Infect Dis 9:132
Cohen OS, Chapman J, Lee H, Nitsan Z, Appel S, Hoffman C, Rosenmann H, Korczyn AD, Prohovnik I (2011) Pruritus in familial Creutzfeldt-Jakob disease: a common symptom associated with central nervous system pathology. J Neurol 258:89–95
Collie DA, Summers DM, Sellar RJ, Ironside JW, Cooper S, Zeidler M, Knight R, Will R (2003) Diagnosing variant Creutzfeldt-Jakob disease with the pulvinar sign: MR imaging findings in 86 neuropathologically confirmed cases. Am J Neuroradiol 24:1560–9
Collins SJ, Sanchez-Juan P, Masters CL, Klug GM, van Duijn C, Poleggi A, Pocchiari M, Almonti S, Cuadrado-Corrales N, de Pedro-Cuesta J, Budka H, Gelpi E, Glatzel M, Tolnay M, Hewer E, Zerr I, Heinemann U, Kretzschmar HA, Jansen GH, Olsen E, Mitrova E, Alpérovitsch A, Brandel JP, Mackenzie J, Murray K, Will RG (2006) Determinants of diagnostic investigation sensitivities across the clinical spectrum of sporadic Creutzfeldt-Jakob disease. Brain 129:2278–87
Demaerel P, Heiner L, Robberecht W, Sciot R, Wilms G (1999) Diffusion-weighted MRI in sporadic Creutzfeldt-Jakob disease. Neurology 52:205–8
Edler J, Mollenhauer B, Heinemann U, Varges D, Werner C, Zerr I, Schulz-Schaeffer WJ (2009) Movement disturbances in the differential diagnosis of Creutzfeldt-Jakob disease. Mov Disord 24:350–6
Farbu E, Tysnes OB, Mork S, Krossnes BK, Bindoff LA (2007) Two Norwegian sisters with late onset Creutzfeldt-Jakob disease caused by the E200K mutation. J Neurol 254:262–3
Finkenstaedt M, Szudra A, Zerr I, Poser S, Hise JH, Stoebner JM, Weber T (1996) MR imaging of Creutzfeldt-Jakob disease. Radiology 199:793–8
Fulbright RK, Kingsley PB, Guo X, Hoffmann C, Kahana E, Chapman JC, Prohovnik I (2006) The imaging appearance of Creutzfeldt-Jakob disease caused by the E200K mutation. Magn Reson Imaging 24:1121–9
Fulbright RK, Hoffmann C, Lee H, Pozamantir A, Chapman J, Prohovnik I (2008) MR imaging of familial Creutzfeldt-Jakob disease: a blinded and controlled study. AJNR Am J Neuroradiol 29:1638–43
Furukawa H, Kitamoto T, Hashiguchi H, Tateishi J (1996) A Japanese case of Creutzfeldt-Jakob disease with a point mutation in the prion protein gene at codon 210. J Neurol Sci 141:120–2
Gaig C, Valldeoriola F, Gelpi E, Ezquerra M, Llufriu S, Buongiorno M, Rey MJ, Marti MJ, Graus F, Tolosa E (2011) Rapidly progressive diffuse Lewy body disease. Mov Disord 26:1316–23
Gawinecka J, Ciesielczyk B, Sanchez-Juan P, Schmitz M, Heinemann U, Zerr I (2012) Desmoplakin as a potential candidate for cerebrospinal fluid marker to rule out 14-3-3 false positive rates in sporadic Creutzfeldt–Jakob disease differential diagnosis. Neurodegener Dis 9:139–44
Ghoshal N, Cali I, Perrin RJ, Josephson SA, Sun N, Gambetti P, Morris JC (2009) Codistribution of amyloid beta plaques and spongiform degeneration in familial Creutzfeldt-Jakob disease with the E200K-129 M haplotype. Arch Neurol 66:1240–6
Gmitterová K, Heinemann U, Bodemer M, Krasnianski A, Meissner B, Kretzschmar HA, Zerr I (2009) 14-3-3 CSF levels in sporadic Creutzfeldt-Jakob disease differ across molecular subtypes. Neurobiol Aging 30(11):1842–50
Green AJ, Ramljak S, Muller WE, Knight RS, Schroder HC (2002) 14-3-3 in the cerebrospinal fluid of patients with variant and sporadic Creutzfeldt-Jakob disease measured using capture assay able to detect low levels of 14-3-3 protein. Neurosci Lett 324:57–60
Green A, Sanchez-Juan P, Ladogana A, Cuadrado-Corrales N, Sanchez-Valle R, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki J, Heinemann U, Hess K, Slivarichova D, Saiz A, Calero M, Mellina V, Knight R, van Dujin CM, Zerr I (2007) CSF analysis in patients with sporadic CJD and other transmissible spongiform encephalopathies. Eur J Neurol 14:121–4
Guillaume E, Zimmermann C, Burkhard PR, Hochstrasser DF, Sanchez JC (2003) A potential cerebrospinal fluid and plasmatic marker for the diagnosis of Creutzfeldt-Jakob disease. Proteomics 3:1495–9
Harrington MG, Merril CR, Asher DM, Gajdusek DC (1986) Abnormal proteins in the cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. N Engl J Med 315:279–83
Heinemann U, Krasnianski A, Meissner B, Gloeckner SF, Kretzschmar HA, Zerr I (2007a) Molecular subtype-specific clinical diagnosis of prion diseases. Vet Microbiol 123:328–35
Heinemann U, Krasnianski A, Meissner B, Varges D, Kallenberg K, Schulz-Schaeffer WJ, Steinhoff BJ, Grasbon-Frodl EM, Kretzschmar HA, Zerr I (2007b) Creutzfeldt-Jakob disease in Germany: a prospective 12-year surveillance. Brain 130:1350–9
Holsinger RM, Lee JS, Boyd A, Masters CL, Collins SJ (2006) CSF BACE1 activity is increased in CJD and Alzheimer disease versus [corrected] other dementias. Neurology 67:710–2
Hsich G, Kenney K, Gibbs CJ Jr, Lee KH, Harrington MG (1996) The 14-3-3 brain protein in cerebrospinal fluid as a marker for transmissible spongifrom encephalopathies. N Engl J Med 335:924–30
Jesse S, Steinacker P, Cepek L, von Arnim CA, Tumani H, Lehnert S, Kretzschmar HA, Baier M, Otto M (2009) Glial fibrillary acidic protein and protein S-100B: different concentration pattern of glial proteins in cerebrospinal fluid of patients with Alzheimer’s disease and Creutzfeldt-Jakob disease. J Alzheimers Dis 17:541–51
Josephs KA, Ahlskog JE, Parisi JE, Boeve BF, Crum BA, Giannini C, Petersen RC (2009) Rapidly progressive neurodegenerative dementias. Arch Neurol 66:201–7
Kelley BJ, Boeve BF, Josephs KA (2008) Young-onset dementia: demographic and etiologic characteristics of 235 patients. Arch Neurol 65:1502–8
Kettlun A, Collados L, Garcia L, Cartier LA, Wolf ME, Mosnaim AD, Valenzuela MA (2003) Matrix metalloproteinase profile in patients with Creuztfeldt-Jakob disease. Int J Clin Pract 57:475–8
Korczyn AD (1991) Creutzfeldt-Jakob disease among Libyan Jews. Eur J Epidemiol 7:490–3
Kovacs GG, Puopolo M, Ladogana A, Pocchiari M, Budka H, Van Duijn C, Collins S, Boyd A, Guilivi A, Coulthart M, Delasnerie-Laupretre N, Brandel JP, Zerr I, Kretzschmar H, de Pedro-Cuesta J, Calero-Lara M, Glatzel M, Aguzzi A, Bishop M, Knight R, Belay G, Will R, Mitrova E (2005) Genetic prion disease: the EUROCJD experience. Hum Genet 118:166–74
Krammer C, Vorberg I, Schätzl HM, Gilch S (2009) Therapy in prion diseases: from molecular and cellular biology to therapeutic targets. Infect Disord Drug Targets 9:3–14
Krasnianski A, Schulz-Schaeffer WJ, Kallenberg K, Meissner B, Collie DA, Roeber S, Bartl M, Heinemann U, Varges D, Kretzschmar HA, Zerr I (2006) Clinical findings and diagnostic tests in the MV-2 subtype of sporadic CJD. Brain 129:2288–96
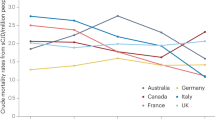
Ladogana A, Puopolo M, Croes EA, Budka H, Jarius C, Collins S, Klug GM, Sutcliffe T, Giulivi A, Alperovitch A, Delasnerie-Laupretre N, Brandel J-P, Poser S, Kretzschmar H, Rietveld I, Mitrova E, de Pedro-Cuesta J, Martinez-Martin P, Glatzel M, Aguzzi A, Knight R, Ward H, Pocchiari M, van Duijn CM, Will RG, Zerr I (2005) Mortality from Creutzfeldt-Jakob disease and related disorders in Europe, Australia, and Canada. Neurology 64:1586–91
Ladogana A, Sanchez-Juan P, Mitrova E, Green A, Cuadrado-Corrales N, Sanchez-Valle R, Koscova S, Aguzzi A, Sklaviadis T, Kulczycki J, Gawinecka J, Saiz A, Calero M, van Duijn CM, Pocchiari M, Knight R, Zerr I (2009) Cerebrospinal fluid biomarkers in human genetic transmissible spongiform encephalopathies. J Neurol 256:1620–8
Lee H, Rosenmann H, Chapman J, Kingsley PB, Hoffmann C, Cohen OS, Kahana E, Korczyn AD, Prohovnik I (2009) Thalamo-striatal diffusion reductions precede disease onset in prion mutation carriers. Brain 132:2680–7
Lemstra AW, van Meegen MT, Vreyling JP, Meijerink PH, Jansen GH, Bulk S, Baas F, van Gool WA (2000) 14-3-3 testing in diagnosing Creutzfeldt-Jakob disease: a prospective study in 112 patients. Neurology 55:514–6
Manaka H, Kato T, Kurita K, Katagiri T, Shikama Y, Kujirai K, Kawanami T, Suzuki Y, Nihei K, Sasaki H et al (1992) Marked increase in cerebrospinal fluid ubiquitin in Creutzfeldt-Jakob disease. Neurosci Lett 139:47–9
Mancuso M, Siciliano G, Capellari S, Orsucci D, Moretti P, Di Fede G, Suardi S, Strammiello R, Parchi P, Tagliavini F, Murri L (2009) Creutzfeldt-Jakob disease with E200K PRNP mutation: a case report and revision of the literature. Neurol Sci 30:417–20
Masters CL, Harris JO, Gajdusek DC, Gibbs CJJ, Bernoulli C, Asher DM (1979) Creutzfeldt-Jakob disease: patterns of worldwide occurrence and the significance of familial and sporadic clustering. Ann Neurol 5:177–88
Mastrianni JA, Capellari S, Telling GC, Han D, Bosque P, Prusiner SB, DeArmond SJ (2001) Inherited prion disease caused by the V210I mutation: transmission to transgenic mice. Neurology 57:2198–205
Masullo C, Bizzarro A, Guglielmi V, Iannaccone E, Minicuci G, Vita MG, Capellari S, Parchi P, Servidei S (2010) An atypical phenotype of CJD associated with the E200K mutation in the prion protein gene. Neurol Sci 31:837–9
Matoba M, Tonami H, Miyaji H, Yokota H, Yamamoto I (2001) Creutzfeldt-Jakob disease: serial changes on diffusion-weighted MRI. J Comput Assist Tomogr 25:274–7
Meissner B, Kallenberg K, Sanchez-Juan P, Krasnianski A, Heinemann U, Varges D, Knauth M, Zerr I (2008) Isolated cortical signal increase on MR imaging as a frequent lesion pattern in sporadic Creutzfeldt-Jakob disease. Am J Neuroradiol 29:1519–24
Minghetti L, Cardone F, Greco A, Puopolo M, Levi G, Green AJ, Knight R, Pocchiari P (2002) Increased CSF levels of prostaglandin E(2) in variant Creutzfeldt-Jakob disease. Neurology 58:127–9
Nitrini R, Mendonca RA, Huang N, LeBlanc A, Livramento JA, Marie SK (2001) Diffusion-weighted MRI in two cases of familial Creutzfeldt–Jakob disease. J Neurol Sci 184:163–7
Nozaki I, Hamaguchi T, Sanjo N, Noguchi-Shinohara M, Sakai K, Nakamura Y, Sato T, Kitamoto T, Mizusawa H, Moriwaka F, Shiga Y, Kuroiwa Y, Nishizawa M, Kuzuhara S, Inuzuka T, Takeda M, Kuroda S, Abe K, Murai H, Murayama S, Tateishi J, Takumi I, Shirabe S, Harada M, Sadakane A, Yamada M (2010) Prospective 10-year surveillance of human prion diseases in Japan. Brain 133:3043–57
Parazzini C, Mammi S, Comola M, Scotti G (2003) Magnetic resonance diffusion-weighted images in Creutzfeldt-Jakob disease: case report. Neuroradiology 45:50–2
Parchi P, Castellani R, Capellari S, Ghetti B, Young K, Chen SG, Farlow M, Dickson DW, Sima AAF, Trojanowski JQ, Petersen RB, Gambetti P (1996) Molecular basis of phenotypic variability in sporadic Creutzfeldt-Jakob disease. Ann Neurol 39:767–78
Pennington C, Chohan G, Mackenzie J, Andrews M, Will R, Knight R, Green A (2009) The role of cerebrospinal fluid proteins as early diagnostic markers for sporadic Creutzfeldt-Jakob disease. Neurosci Lett 455:56–9
Piubelli C, Fiorini M, Zanusso G, Milli A, Fasoli E, Monaco S, Righetti PG (2006) Searching for markers of Creutzfeldt-Jakob disease in cerebrospinal fluid by two-dimensional mapping. Proteomics 6(Suppl 1):256–261
Rosenmann H, Meiner Z, Kahana E, Halimi M, Lenetsky E, Abramsky O, Gabizon R (1997) Detection of 14-3-3 protein in the CSF of genetic Creutzfeldt-Jakob disease. Neurology 49:593–5
Sanchez JC, Guillaume E, Lescuyer P, Allard L, Carrette O, Scherl A, Burgess J, Corthals GL, Burkhard PR, Hochstrasser DF (2004) Cystatin C as a potential cerebrospinal fluid marker for the diagnosis of Creutzfeldt-Jakob disease. Proteomics 4:2229–33
Sanchez-Juan P, Green A, Ladogana A, Cuadrado-Corrales N, Sanchez-Valle R, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki J, Hess K, Bodemer M, Slivarichova D, Saiz A, Calero M, Ingrosso L, Knight R, Janssens C, Van Duijn C, Zerr I (2006) CSF tests in the differential diagnosis of Creutzfeldt-Jakob disease. Neurology 67:637–43
Sanchez-Juan P, Sanchez-Valle R, Green A, Ladogana A, Cuadrado-Corrales N, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki J, Hess K, Krasnianski A, Equestre M, Slivarichova D, Saiz A, Calero M, Pocchiari M, Knight R, van Dujin CM, Zerr I (2007) Influence of timing on CSF tests value for Creutzfeldt-Jakob disease diagnosis. J Neurol 254:901–6
Schmidt H, Otto M, Niedmann P, Cepek L, Schroter A, Kretzschmar HA, Poser S (2004) CSF lactate dehydrogenase activity in patients with Creutzfeldt-Jakob disease exceeds that in other dementias. Dement Geriatr Cogn Disord 17:204–6
Schmidt C, Redyk K, Meissner B, Krack L, von Ahsen N, Roeber S, Kretzschmar H, Zerr I (2010) Clinical features of rapidly progressive Alzheimer’s disease. Dement Geriatr Cogn Disord 29:371–8
Schröter A, Zerr I, Henkel K, Tschampa HJ, Finkenstaedt M, Poser S (2000) Magnetic resonance imaging (MRI) in the clinical diagnosis of Creutzfeldt-Jakob disease. Arch Neurol 57:1751–7
Seror I, Lee H, Cohen OS, Hoffmann C, Prohovnik I (2010) Putaminal volume and diffusion in early familial Creutzfeldt-Jakob disease. J Neurol Sci 288:129–34
Shyu WC, Hsu YD, Kao MC, Tsao WL (1996) Panencephalitic Creutzfeldt-Jakob disease in a Chinese family. Unusual presentation with PrP codon 210 mutation and identification by PCR-SSCP. J Neurol Sci 143:176–80
Silveyra MX, Garcia-Ayllon MS, Calero M, Saez-Valero J (2006) Altered glycosylation of acetylcholinesterase in the Creutzfeldt-Jakob cerebrospinal fluid. J Mol Neurosci 30:65–6
Stoeck K, Bodemer M, Ciesielczyk B, Meissner B, Bartl M, Heinemann U, Zerr I (2005) Interleukin 4 and interleukin 10 levels are elevated in the cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. Arch Neurol 62:1591–4
Stoeck K, Bodemer M, Zerr I (2006) Pro- and anti-inflammatory cytokines in the CSF of patients with Creutzfeldt-Jakob disease. J Neuroimmunol 172:175–81
Tomita I, Sato K, Shirabe S, Nagasato K, Satoh A, Tsujihata M (2004) Serial diffusion-weighted MRI (DWI) in a patient with sporadic Creutzfeldt-Jakob disease. Rinsho Shinkeigaku 44:182–6
Tribl GG, Strasser G, Zeitlhofer J, Asenbaum S, Jarius C, Wessely P, Prayer D (2002) Sequential MRI in a case of Creutzfeld-Jakob disease. Neuroradiology 44:223–6
Tschampa HJ, Neumann M, Zerr I, Henkel K, Schröter A, Schulz-Schaeffer WJ, Steinhoff BJ, Kretzschmar HA, Poser S (2001) Patients with Alzheimer’s disease and dementia with Lewy bodies mistaken for Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry 71:33–9
Tschampa HJ, Kallenberg K, Urbach H, Meissner BCN, Kretzschmar HA, Knauth M, Zerr I (2005) MRI in the diagnosis of sporadic Creutzfeldt-Jakob disease: a study on inter-observer agreement. Brain 128:2026–33
Tsuboi Y, Baba Y, Doh-ura K, Imamura A, Fujioka S, Yamada T (2005) Diffusion-weighted MRI in familial Creutzfeldt-Jakob disease with the codon 200 mutation in the prion protein gene. J Neurol Sci 232:45–9
Urbach H, Klisch J, Wolf HK, Brechtelsbauer D, Gass S, Solymosi L (1998) MRI in sporadic Creutzfeldt-Jakob disease: correlation with clinical and neuropathological data. Neuroradiology 40:65–70
Van Everbroeck B, Quoilin S, Boons J, Martin JJ, Cras P (2003) A prospective study of CSF markers in 250 patients with possible Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry 74:1210–4
Van Everbroeck B, Dobbeleir I, De Waele M, De Deyn P, Martin J-J, Cras P (2004) Differential diagnosis of 201 possible Creutzfeldt-Jakob disease patients. J Neurol 251:298–304
WHO (2003) WHO manual for surveillance of human transmissible spongiform encephalopathies including variant Creutzfeldt-Jakob disease, WHO Library Cataloguing-in-Publication Data
Will RG, Zeidler M, Stewart GE, Macleod MA, Ironside JW, Cousens SN, Mackenzie J, Estibeiro K, Green AJ, Knight RS (2000) Diagnosis of new variant Creutzfeldt-Jakob disease. Ann Neurol 47:575–82
Young GS, Geschwind MD, Fischbein NJ, Martindale JL, Henry RG, Liu S, Lu Y, Wong S, Liu H, Miller BL, Dillon WP (2005) Diffusion-weighted and fluid-attenuated inversion recovery imaging in Creutzfeldt-Jakob disease: high sensitivity and specificity for diagnosis. Am J Neuroradiol 26:1551–62
Zerr I, Bodemer M, Gefeller O, Otto M, Poser S, Wiltfang J, Windl O, Kretzschmar HA, Weber T (1998a) Detection of 14-3-3 protein in the cerebrospinal fluid supports the diagnosis of Creutzfeldt-Jakob disease. Ann Neurol 43:32–40
Zerr I, Giese A, Windl O, Kropp S, Schulz-Schaeffer W, Riedemann C, Skworc K, Bodemer M, Kretzschmar HA, Poser S (1998b) Phenotypic variability in fatal familial insomnia (D178N-129 M) genotype. Neurology 51:1398–1405
Zerr I, Pocchiari M, Collins S, Brandel JP, de Pedro CJ, Knight RSG, Bernheimer H, Cardone F, Delasnerie-Lauprêtre N, Cuadrado Corrales N, Ladogana A, Fletcher A, Bodemer M, Awan T, Ruiz Bremón A, Budka H, Laplanche JL, Will RG, Poser S (2000) Analysis of EEG and CSF 14-3-3 proteins as aids to the diagnosis of Creutzfeldt-Jakob disease. Neurology 55:811–5
Zerr I, Bodemer M, Kaboth U, Kretzschmar H, Oellerich M, Armstrong VW (2004) Plasminogen activities and concentrations in patients with sporadic Creutzfeldt-Jakob disease. Neurosci Lett 371:163–6
Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Ladogana A, Schuur M, Haik S, Collins SJ, Jansen GH, Stokin GB, Pimentel J, Hewer E, Collie DA, Smith P, Varges D, Heinemann U, Meissner B, Roberts H, Brandel JP, Van Dujin CM, Pocchiari M, Begue P, Cras P, Will RG, Sanchez-Juan P (2009) Updated clinical diagnostic criteria for sporadic Creutzfeldt-Jakob disease. Brain 132:2659–68
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Zerr, I., Gawinecka, J., Stoeck, K., Breithaupt, M. (2013). Diagnosis of Prion Disease: Conventional Approaches. In: Zou, WQ., Gambetti, P. (eds) Prions and Diseases. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5338-3_13
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5338-3_13
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5337-6
Online ISBN: 978-1-4614-5338-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)