Abstract
Prion diseases are characterized by the deposition of PrPSc, an abnormal form of the normal cellular protein, PrPc in the brain. The unique nature of human prion diseases includes their pathogenesis, mode of transmission, and neuropathology. In humans, a long incubation time, rapid and dramatic evolution of the disease course, and always a lethal outcome are key features of the clinical syndrome. The clinical diagnosis in sCJD is supported by detection of periodic sharp and slow wave complexes (PSWCs) in the electroencephalogram, 14-3-3 proteins, the detection of the abnormal PrP of in the cerebrospinal fluid (CSF) via RT-QuIC, and hyperintense signal changes in the basal ganglia, thalamus and cortical areas on magnetic resonance imaging (MRI). These tests became part of the clinical diagnostic criteria for CJD. Elevated levels of brain-derived proteins in plasma such as neurofilaments or tau might contribute to the clinical diagnosis in the future. The sensitivity of diagnostic tests varies across molecular CJD subtypes. Alzheimer’s disease and Lewy body dementia are the most frequent differential diagnoses in elderly patients, while chronic inflammatory CNS disorders and autoimmune mediated encephalitis have to be considered in younger patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- 14-3-3 proteins
- PrPSc
- Cerebrospinal fluid
- Neurofilaments
- Tau
- Plasma
- Diagnosis
- Diagnostic criteria
- EEG
- Molecular disease subtype
- MRI
- PSWCs
1 Introduction
Human prion diseases share many common features—transmissibility in animal experiments, fatal progressive disease course, neuronal loss, astrogliosis, and PrPSc deposition in the brain. Despite this, several forms are distinguished depending on assumed pathophysiology: genetic, acquired, and sporadic disease forms. In addition, sporadic disease forms display clinicopathological diversity, which origins in codon 129 PRNP genotype and PrPSc type (see Molecular disease subtypes). In clinical terms, signs and symptoms of the disease are heterogeneous and comprise a wide spectrum of neurological and psychiatric abnormalities. Because of this and because of the fact that a definite early clinical test or biomarker is still lacking, several diagnostic investigations have to be taken into account and considered in the context of comprehensive clinical examination, thoughtful evaluation of the clinical history, and consideration of other differential, potentially curable diagnoses.
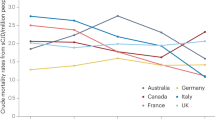
A definite and final diagnosis requires invasive procedures such as brain biopsy or analysis of brain material at autopsy. Early detection will become increasingly important once forthcoming effective therapies are available (Krammer et al. 2009). Clinical diagnostic criteria for sCJD were first suggested 40 years ago, using a combination of distinctive clinical features and best available investigations, which at that time was EEG (Masters et al. 1979). In recent years, substantial progress in developing other specialized investigations, including useful surrogate biomarkers in the cerebrospinal fluid, plasma and brain imaging, and clinical diagnostic criteria, have been amended (Collins et al. 2006; Zerr et al. 2000, 2009, 2022; Hermann et al. 2021) (Fig. 33.1). Blood-based biomarker are currently under investigations and might become important tools for monitoring disease progression and potentially even response to therapy once disease-modifying drugs become available (Vallabh et al. 2020).
Progress in the development of diagnostic techniques for Creutzfeldt–Jakob disease (CJD). (Zerr 2022)
2 Cerebrospinal Fluid
Cerebrospinal fluid (CSF) is the main component of the brain extracellular space and participates in the exchange of many biochemical products in the central nervous system (CNS). Consequently, CSF contains a dynamic and complex mixture of proteins, which reflects physiological or pathological state of the CNS. CSF analysis is an important part in clinical neurology and is used to diagnose various inflammatory and malignant disorders and recently also neurodegenerative disorders. The alterations in CSF composition are also discussed to reflect pathological changes in the brain and thus contribute to a better understanding of the pathophysiology of the underlying disorders affecting CNS.
For many years, CSF analysis in CJD has been used to exclude brain inflammation in patients with rapid progressive dementia. Since modern proteomic technologies allow us to identify proteins and protein patterns in human fluids, the CSF analysis in dementia disorders has become even more important. Historically, first CSF abnormalities in human prion diseases were reported by Harrington et al. (1986), who identified two proteins spots, named p130/131 in the CSF of CJD patients. Decades later, these proteins became known as 14-3-3 proteins and were the first CSF biomarker ever used in clinical criteria in patients with a neurodegenerative dementia.
2.1 Routine Tests
The routine examination of CSF from patients with CJD or GSS usually reveals normal results. An unspecific increase in total protein, the presence of oligoclonal IgG bands or raised cell count is an extremely rare finding (see Table 33.1). In the most comprehensive study on this subject, data from 450 patients with sporadic CJD and 47 patients with other TSEs were analyzed as part of an EC-supported multinational study. Raised white cell counts of >5 cells/ml were found in three out of 298 patients with sporadic CJD, in two with cell counts of 7 cells/ml and in one of 20 cells/ml. Total protein concentrations of >0.9 g/l were found in 5 of 438 patients with sporadic CJD, but none had a concentration of >1 g/l. CSF oligoclonal IgG was detected in 8 out of 182 sporadic CJD patients. Among patients with other TSEs, six had elevated cell counts ranging from 6 to 14 cells/ml, but none had total protein concentrations of >0.9 g/l and one patient had detectable oligoclonal IgG. None of the patients with sporadic CJD or other TSEs had abnormalities in all three tests (Green et al. 2007).
As a rule, inflammatory CSF findings exclude the diagnosis of a human prion disease.
2.2 14-3-3 Proteins
14-3-3 proteins were initially described as abundant, acidic brain proteins, and their names are derived from the combination of its fraction number on DEAE-cellulose chromatography and migration position in the subsequent starch gel electrophoresis (Hsich et al. 1996). Despite the fact that the pathology behind the elevated level of 14-3-3 in CJD is still a question of debate, the detection of 14-3-3 protein in CSF is part of clinical diagnostic criteria for probable sCJD because of its high sensitivity and, even more important, high predictive values in clinical setting. A large number of studies proved that in appropriate clinical circumstances, a positive 14-3-3 is highly sensitive and specific for sCJD diagnosis. A meta-analysis showed a sensitivity of 92% and a specificity of 80% of Western Blot 14-3-3 analyses (Muayqil et al. 2012). The recently developed γ14-3-3 ELISA was reported with 88% sensitivity and 96% specificity (Schmitz et al. 2016a, b) and showed superior diagnostic accuracy in a comparative evaluation (Leitão et al. 2016). However, the specificity may be substantially lower in the differentiation from acute non-neurodegenerative encephalopathies (Stoeck et al. 2012).
The sensitivity of 14-3-3 varies among TSE types. Whereas very high sensitivity was shown in gCJD and iatrogenic CJD, similar to sCJD, 14-3-3 positivity is substantially less frequent in GSS and rarely present in FFI (Llorens et al. 2020a, b, c; Schmitz et al. 2022). In variant CJD (vCJD), only about 49% of patients are positive (Green et al. 2001; Gmitterová et al. 2009; Green et al. 2002; Van Everbroeck et al. 2003; Castellani et al. 2004).
Biological parameters significantly influence the sensitivity of 14-3-3 test in patients with sCJD, that is, disease duration, codon 129 genotype, age at onset, and time of the lumbar puncture (Sanchez-Juan et al. 2007). In general, the 14-3-3 test displays best sensitivity in patients older than 40 years with short disease duration, homozygous at codon 129 genotype, and when lumbar puncture is performed at later disease stages (Sanchez-Juan et al. 2006). Differences in the sensitivity of 14-3-3 test are also observed between classical and nonclassical CJD types (see Molecular disease subtypes). In classical CJD (which basically fulfills the criteria of having the tendency to be older, homozygous for methionine at codon 129, short disease duration, and rapid progression), 14-3-3 test sensitivity is superior to nonclassical (or atypical) cases.
Although this test was often found to be positive at onset of the first neurological symptoms, higher sensitivity was reported in the middle or late stage of the disease. Moreover, in the terminal stage of disease, 14-3-3 level might decrease in CSF, but this observation is based on case reports and might reflect extremely long disease duration.
2.3 Tau/p-tau
Tau concentration in CSF of CJD patients is highly increased, and its quantitative analysis is a good diagnostic tool for CJD (Kovacs et al. 2017c). Determination of tau has shown to yield specificity and sensitivity comparable to those for 14-3-3 testing, and several studies revealed that the optimum cut-off point for CJD is at 1.300 pg/ml (Hermann et al. 2021). This cut-off is three times higher than levels reported for Alzheimer’s dementia. In the latter, extreme tau levels have been reported occasionally, especially in atypical or rapidly-progressive Alzheimer’s dementia. Therefore, a ratio of phosphorylated and total t-tau has been proposed to improve the diagnostic accuracy (Skillbäck et al. 2014, Hermann et al. 2022) Concerning the phosphorylated tau isoforms in CSF of CJD, tau phosphorylated at threonine 181 (p-tau) was significantly raised in sCJD as well as in vCJD. Interestingly, tau concentration was lower in vCJD when compared to sCJD, whereas p-tau concentration was much higher in vCJD than in sCJD.
2.4 RT-QuIC
The Real-Time Quaking-induced conversion (RT-QuIC) is a new method to detect PrPSc in various tissues and body fluids. The method is described in detail in chapter 30. Since 2011, it has been evaluated in the context of the clinical diagnosis of sCJD in several retrospective and prospective studies. Because all studies reported good to excellent Sensitivity with outstanding specificity of 99%–100% (see a summary in Table 33.2), it was integrated as a new diagnostic criterion in recent consensus criteria. If available, the test should be performed in all patients with suspected prion disease (Hermann et al. 2021).
2.5 Other CSF Markers
Besides common TSE markers, several other proteins have been proposed as possibly useful in the diagnosis of the human TSE. So far, they were tested in small numbers of patients and need further rigorous testing and thoughtful validation of their potentials to be classified as biomarkers in human prion disorders (Table 33.3). Hermann et al. Lancet Neurol 2021.
2.6 Blood-Based Biomarkers
Blood-based biomarkers to detect disease or to monitor disease progression are highly desirable because they would replace CSF puncture or at least support the diagnostic process. In addition, blood samples can be taken regularly and repeatedly. Attempts to develop blood-based biomarkers have been carried out for many years (Otto et al. 1998; Völkel et al. 2001) and have experienced a renewed upswing in recent years. With the improvement of detection technology, some brain proteins can be detected in plasma with good reproducibility. These primarily include the proteins tau, NFL (Steinacker et al. 2016), and PrP (Villar-Piqué et al. 2019). Elevated levels may correlate with disease stage and progression but, unfortunately, the specificity of tau and NFL in the differential diagnosis from other rapidly progressive encephalopathic syndromes is not very high (Kovacs et al. 2017; Abu-Rumeileh et al. 2020a; Zerr et al. 2021). See Table 33.4 for a summary of recent studies. However, the sensible use may be to monitor the disease progression or as a surrogate marker to check the therapy effects in clinical trials (Thompson et al. 2021).
3 Magnetic Resonance Imaging
3.1 General Introduction
MRI has played an important role in the diagnosis of CJD (Tschampa et al. 2005; Urbach et al. 1998; Nozaki et al 2018; Young et al. 2005; Seror et al. 2010). In 1988, a hyperintense signal of the basal ganglia on T2-weighted images was first described as a characteristic finding in sCJD patients, followed by further case reports. Subsequently, systematic studies on the sensitivity and specificity of hyperintense signal changes in the striatum in sCJD were performed. Along with the availability of methods, the early MR studies mainly focused on T2-weighted, proton density weighted (Finkenstaedt et al. 1996; Schröter et al. 2000), and to a lesser extent on FLAIR (Choi et al. 2009) imaging, while current studies and criteria mainly rely on FLAIR and especially DWI MRI (Zerr et al. 2009; Vitali et al. 2011; Bizzi et al. 2020; Lee et al. 2010).
With the emergence of more sensitive MRI techniques, such as fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted image (DWI), cortical signal increase was additionally observed in sCJD patients and hyperintense basal ganglia were detected more frequently (Fig. 33.2). Using FLAIR- and DWI, signal increase in the cortex has been reported even more frequently than basal ganglia signal increase. Apart from the cortex and basal ganglia hyperintensity, signal increase has also been reported for the hippocampus, thalamus, and cerebellum and for the mesencephalon. In general, the most sensitive technique to date seems to be DWI, followed by FLAIR and T2 imaging.
3.2 Test Performance
With the introduction of diffusion-weighted imaging, MR changes are detected earlier in the disease (Collins et al. 2006; Heinemann et al. 2007b; Josephs et al. 2009) and interobserver reliability was improved (Demaerel et al. 1999, Zerr et al. 2009, Vitali et al. 2011). The diagnostic accuracy was reported by several studies with a sensitivity ranging from 80% to 98% and a specificity ranging from 74% to 98% (Hermann et al. 2021). However, discrepant reports of the test performance may be explained with the use of different criteria, different control groups, and, in particular, may be highly dependent on the image reader’s experience (Carswell et al. 2012).
3.3 Changes During the Disease
Data on serial MR examinations in CJD are limited in the literature. In early disease stages, characteristic basal ganglia lesions are not found in up to one-third of the patients (Meissner et al. 2008). According to Ukisu and colleagues (Ukisu et al. 2005), cortical DWI changes (9/9 cases) preceded the hyperintensities in the basal ganglia (5/9 cases at early stage). During the course of the disease, there is generally an expansion of the signal changes and progressive cerebral atrophy (Tribl et al. 2002; Eisenmenger et al. 2016), displaying lesion propagation from cortex to basal ganglia in MM1 and vice versa in VV2 (Pascuzzo et al. 2020). In the late stage of the disease, the diffusion changes may disappear (Arruda et al. 2004; Tribl et al. 2002). Some very interesting case studies reported very early and even preclinical MRI changes in genetic and sporadic CJD up to two years before disease onset (Alvarez et al. 2005; Zanusso et al. 2016; Novi et al. 2018; Koizumi et al. 2021).
4 EEG
For decades, periodic sharp wave complexes (PSWCs) in the EEG were reported to represent the most typical finding in the course of sCJD. The apparent advantages of the EEG are: This investigation is widely available, noninvasive, and can easily be repeated several times. At onset, the EEG might show only nonspecific changes such as background slowing of alpha activity and dysrhythmia. As the disease progresses, slow periodic complexes might appear occasionally; later, the typical periodic pattern is seen. In end stage of CJD, the EEG might show an isoelectric line. PSWCs might be provoked by acoustic or tactile stimulation. Typical periodic patterns (Fig. 33.3) are observed in 60%–70% of all cases after about 12 weeks (median) from disease onset but might occur as early as three weeks after onset. They may disappear at later disease stages. Since the term PSWCs has not been operationalized before, sensitivity of the detection of this abnormality varied among studies. EEG criteria have been suggested (Fig. 33.4). According to these criteria, PSWCs are detectable in two-thirds of CJD patients at mid and late disease stages (sensitivity 64%) with a specificity of 91% (Steinhoff et al. 2004). However, they are not able to differentiate CJD from nonconvulsive status epilepticus (Marquetand et al. 2017) and in addition, recent observations reported a lower sensitivity (around 40%) (Hermann et al. 2018), most likely due to the fact that modern diagnostics allow the identification of CJD in early disease stages when PSWCs are not present.
EEG criteria (according to Steinhoff et al. 2007)
5 Molecular Disease Subtype-Specific Diagnosis
Some years ago, a molecular basis has been defined, which might explain the clinical and pathological disease heterogeneity (Parchi et al. 1996). The polymorphism for methionine (M) or valine (V) at codon 129 of PRNP gene has been shown to influence the clinical features of sCJD. In 1996, two PrPSc subtypes in brain homogenates of sCJD patients were identified. The polymorphism at codon 129 and the prion protein types 1 and 2 were the basis for a new molecular classification of sCJD, which replaced the previous attempts (Parchi et al. 1999). Currently, patients with the MM1/MV1 subtype, who display a short disease duration, dementia, myoclonus, and typical EEG pattern, are frequently referred to as having “classical” or “common” CJD subtype. Other (“nonclassical” and “atypical”) subtypes are rare (Fig. 33.5).
The discovery of several distinct molecular CJD subtypes explains many features observed in sporadic CJD patients. The clinical presentation at early disease stage is peculiar in most disease subtypes, and the detailed investigation of the clinical syndrome often allows the assignment to the distinct CJD subtype. This observation is supported by EEG, CSF, and MRI results, which appear in subtype-distinctive pattern as described below. Table 33.5 gives an overview of the diagnostic investigations in distinct molecular CJD subtypes (Heinemann et al. 2007a).
EEG is abnormal in all disease subtypes, but the typical periodic sharp and slow wave pattern (PSWC) is observed in MM1/MV1 subtype only and is rare in MM2/ MV2/VV1-2 patients. Because CJD diagnosis was based on the triad: dementia, myoclonus, and PSWC in EEG for a long time, we might speculate that the frequency of so-called classical myoclonic CJD type was overestimated in earlier studies due to the selection bias. As mentioned above, results of various CSF tests vary considerably by disease subtype. 14-3-3 test sensitivity is best in MM1 and VV patients (>90%) and has the lowest sensitivity in MV2 (65%) and MM2 (78%) patients. Similar results were obtained for CSF tau protein (Sanchez-Juan et al. 2006) and for the detection of PrPSc via RT-QuIC (Franceschini et al. 2017; Rhoads et al. 2020).
The most characteristic MRI lesion patterns are found in MV2 and VV2, showing predominant involvement of thalamus and basal ganglia. Limited cortical signal increase was significantly related to PrPSc type 2. A further possible characteristic lesion pattern was found in VV1 showing widespread cortical hyperintensities and absence of basal ganglia signal alterations. In the other subtypes, there was a higher overlap between cortical and subcortical involvement. MV2 subtype was characterized by basal ganglia and thalamic involvement (Krasnianski et al. 2006). The pulvinar sign, according to current criteria, was identified in the MV2 subtype only (Collie et al. 2003). Due to the generally high frequency of thalamic hyperintensities in MV2, this subtype is the most likely to be mistaken for variant CJD (vCJD) on MRI. A multicenter international study evaluated MRI scans in 211 CJD patients with various sCJD disease subtypes (Meissner et al. 2009). Although basal ganglia hyperintensities on the MRI represented a consistent finding in all subtypes (except VV1), the frequency and location of cortex hyperintensities as well as the presence or absence of thalamus involvement varied between the subtypes. Across all molecular subtypes, VV2 patients showed the most frequent involvement of basal ganglia and thalamus. Cerebral cortical signal increase was usually restricted to less than three regions and most frequently found in the cingulate gyrus (Table 33.6 and Fig. 33.6). Recent studies validated these findings and reported that in the most common MM1 subtype, DWI abnormalities are predominantly present in cortical regions and caudate nucleus. VV2 and MV2 subtypes show primary involvement of the striatum and the thalamus, whereas in the rare MM2 and VV1 subtypes, often only cortical abnormalities can be detected (Pascuzzo et al. 2020). Based on these results, Bizzi et al. (2021) proposed an MRI-based prion subtype classification algorithm.
6 Genetic TSE
Patients with inherited forms of human prion diseases are diagnosed by genetic analysis of the PRNP gene. However, the family history of a prion disease might be absent in a considerable number of patients, thus it is important to know the outcomes of conventional tests such as EEG, CSF, and MRI. The most comprehensive studies have been carried out in genetic CJD with E200K and V210I mutations and in fatal familial insomnia (FFI), whereas only case reports or very small cohorts have been investigated in rare PRNP mutations.
Genetic transmissible spongiform encephalopathies (gTSE) represent 10%–15% of human TSEs. However, there is a special interest in studying biochemical and imaging markers in CSF to improve diagnosis and to monitor disease progression in genetic forms, especially when disease phenotype differs from that of typical sporadic CJD (Ladogana et al. 2009).
PSWCs are not recorded in Gerstmann–Sträussler–Scheinker (GSS) syndrome, fatal familial insomnia, and in transmitted forms of the disease such as Kuru, iCJD, and vCJD. In patients with genetic prion diseases, PSWCs are only occasionally seen, with exception of patients with the mutation at codon 200 and 210 (Ladogana et al. 2005). In these patients, the sensitivity of the EEG is almost the same as in sCJD (Zerr et al. 1998a).
Concerning CSF 14-3-3 testing, sensitivity varies across the spectrum of genetic mutations (Rosenmann et al. 1997). Apparently, the types of mutation significantly influence the biomarker concentration in the CSF and, thus, test sensitivity. According to current information from a large multicenter study, changes in the CSF of patients with familial genetic forms of CJD (gCJD) are comparable to those found in sCJD samples. Table 33.7 gives an overview. For example, 14-3-3 proteins are detectable in patients with an E200K and V210I mutation but only in rare cases in FFI and GSS (Schmitz et al. 2022). In an another study on biomarkers in CJD (Ladogana et al. 2009), the crude analyses of disease-modifying factors on 14-3-3 test in gCJD revealed that age at onset and PRNP codon 129 genotype influenced sensitivity. Age at onset correlated significantly with 14-3-3 test sensitivity in gCJD, being lower in those patients with disease onset before 40 years. These data parallel the results of the same analysis performed on sporadic CJD (Ladogana et al. 2009; Sanchez-Juan et al. 2006). Interestingly, the PRNP codon 129 genotype seemed to influence 14-3-3 sensitivity in gCJD in a different way as in sporadic CJD. Valine homozygous gCJD patients had a statistically significant lower sensitivity in 14-3-3 test than heterozygous patients, but sensitivity was not significantly lower when adjusted for the mutation. This might be due to the fact that the PRNP mutations coupled with valine alleles (P105T, R208H, D178N, and E196K) yielded lower sensitivity to 14-3-3 (Table 33.8).
In recent years, more and more data have become available concerning MRI changes in gCJD. Of special importance, thalamostriatal and cortical diffusion reductions have been shown to precede disease onset in E200K and other prion mutation carriers and might therefore serve as an early diagnostic marker (Lee et al. 2009; Cohen et al. 2015; Koizumi et al. 2021; Fulbright et al 2006; Fulbright et al. 2008; Tsuboi et al. 2005). Restricted diffusion seems to be observed less frequently in gTSE, especially in FFI GSS, than in sCJD (Krasnianski et al. 2016). A Japanese study that included 216 gTSE patients and reported an overall sensitivity of 79% (Nozaki et al. 2010). However, CJD-typical signal patterns are quite common in gTSE associated with typical gCJD mutations such as E200K (Gao et al. 2019).
An important point of interest for biomarkers in gTSEs is to analyze their potential use as surrogate parameter for disease progression in clinical trials. These data might be used for selection of homogenous patient groups when testing new drugs to obtain a more reliable assessment of their effects on the disease progression and to reduce the sample size needed in clinical trials. In addition, such biomarkers might be used to monitor the disease progression (Vallabh et al. 2020, Hermann et al. 2020, Thompson et al. 2021).
7 Differential Diagnosis
The differential diagnosis of sCJD includes a large number of neurological and psychiatric diseases (Van Everbroeck et al. 2004; Schmidt et al. 2010; Maat et al. 2015; Chitravas et al. 2011; Papageorgiu et al. 2009). In most cases, the diagnosis of CJD as the primary diagnosis is not taken into account when patients are admitted to hospital. Alzheimer’s disease is the most important differential diagnosis in older patients. Rapid disease courses, in particular, can rarely be discriminated from CJD, especially when myoclonus is present. Dementia with Lewy bodies is another neurodegenerative dementia that must be considered (Gaig et al. 2011). Because CJD typically presents as a rapidly evolving neurological disorder, the spectrum of differential diagnosis also comprises some treatable or reversible diseases or acute conditions. Figure 33.7 gives an overview on differential diagnoses of CJD in specialized centers. It indicates that potentially reversible conditions may be present in about 30% of suspected prion disease cases (Kelley et al. 2008). Moreover, studies from nonspecialized centers reported that immune-mediated and infectious encephalitides were the most frequent diagnosis among patients with rapidly progressive dementia (Zhang et al. 2017; Studart Neto et al. 2017; Anuja et al. 2018). Thus, a clinical suspicion of prion disease has to be validated through biomarker-based diagnostics and a thorough exclusion of potential mimics before a final diagnosis is made.
8 Criteria
The symptoms and signs of disease in patients with prion diseases are heterogeneous. This heterogeneity is the result of the involvement of various brain structures and still undefined biological determinants influencing disease course. The classification criteria are based on the etiology of the disease, which can be divided into four categories: sporadic, iatrogenic, familial/genetic, and variant CJD (WHO 2003; Will et al. 2000; Zerr et al. 2009; Hermann et al. 2021). Criteria for sporadic CJD have been amended by 14-3-3 CSF test, MRI, and more recently, detection of the PrPSc. They are displayed in Fig. 33.8.
Criteria for sporadic CJD. http://cjd-goettingen.de/en/for-doctors/criteria-of-sporadic-cjd
9 Conclusions
Creutzfeldt–Jakob disease is a frequent cause of rapid progressive dementia. Achieving a correct early diagnosis has important implications for (1) distinguishing prion disease from other, potentially treatable diseases, (2) preventing infectious material from being distributed via blood transfusions, surgery, or organ donations, and (3) selecting homogeneous population for upcoming drug trials. The clinical diagnosis of sCJD is supported by detection of biomarkers in blood or CSF, including the biomarkers such as 14-3-3 and tau/phosphorylated tau and recently detection of the abnormal PrP in the CSF. Clinical diagnostic criteria were amended and validated (Hermann et al. 2021, Watson et al. 2022). Advanced brain imaging techniques significantly contribute to the clinical diagnosis, on the one hand, but might also help in the early differentiation of molecular disease subtypes in sporadic CJD, on the other hand.
Progress in development of blood-based biomarker is substantial and will further add to the development of monitoring strategies once powerful anti-prion drugs will appear on the horizon.
References
Abu-Rumeileh S, Baiardi S, Polischi B, et al. Diagnostic value of surrogate CSF biomarkers for Creutzfeldt-Jakob disease in the era of RT-QuIC. J Neurol. 2019;266:3136–43.
Abu-Rumeileh S, Baiardi S, Ladogana A, et al. Comparison between plasma and cerebrospinal fluid biomarkers for the early diagnosis and association with survival in prion disease. J Neurol Neurosurg Psychiatry. 2020a;91:1181–8. Published online ahead of print, 2020 Sep 14
Alberti C, Gonzalez J, Maldonado H, Medina F, Barriga A, Garcia L, Kettlun A, Collados L, Puente J, Cartier L, Valenzuela M. Comparative study of CSF neurofilaments in HTLV- 1-associated myelopathy/tropical spastic paraparesis and other neurological disorders. AIDS Res Hum Retroviruses. 2009;25:803–9.
Albrecht D, Garcia L, Cartier L, Kettlun AM, Vergara C, Collados L, Valenzuela MA. Trophic factors in cerebrospinal fluid and spinal cord of patients with tropical spastic paraparesis, HIV, and Creutzfeldt-Jakob disease. AIDS Res Hum Retroviruses. 2006;22:248–54.
Alvarez FJ, Bisbe J, Bisbe V, Dávalos A. Magnetic resonance imaging findings in pre-clinical Creutzfeldt-Jakob disease. Int J Neurosci. 2005;115(8):1219–25.
Anuja P, Venugopalan V, Darakhshan N, et al. Rapidly progressive dementia: An eight year (2008–2016) retrospective study. PLoS One. 2018; [cited 2018 Jul 5];[13 p]
Arruda WO, Bordignon KC, Milano JB, Ramina R. Creutzfeldt-Jakob disease, Heidenhain variant: case report with MRI (DWI) findings. Arq Neuropsiquiatr. 2004;2004(62):347–52.
Atarashi R, Satoh K, Sano K, et al. Ultrasensitive human prion detection in cerebrospinal fluid by real-time quaking-induced conversion. Nat Med. 2011;17:175–8.
Bizzi A, Pascuzzo R, Blevins J, et al. Evaluation of a new criterion for detecting prion disease with diffusion magnetic resonance imaging. JAMA Neurol. 2020;
Bizzi A, Pascuzzo R, Blevins J, et al. Subtype diagnosis of sporadic Creutzfeldt-Jakob disease with diffusion magnetic resonance imaging. Ann Neurol. 2021;89(3):560–72.
Blennow K, Diaz-Lucena D, Zetterberg H, et al. CSF neurogranin as a neuronal damage marker in CJD: a comparative study with AD. J Neurol Neurosurg Psychiatry. 2019;90:846–53.
Bongianni M, Orrú C, Groveman BR, et al. Diagnosis of Human Prion Disease Using Real-Time Quaking-Induced Conversion Testing of Olfactory Mucosa and Cerebrospinal Fluid Samples. JAMA Neurol. 2017;74:155–62.
Carswell C, Thompson A, Lukic A, Stevens J, Rudge P, Mead S, Collinge J, Hyare H. MRI findings are often missed in the diagnosis of Creutzfeldt-Jakob disease. BMC Neurol. 2012;12:153.
Cartier L, Garcia L, Kettlun AM, Castaneda P, Collados L, Vasquez F, Giraudon P, Belin MF, Valenzuela MA. Extracellular matrix protein expression in cerebrospinal fluid from patients with tropical spastic paraparesis associated with HTLV-I and Creutzfeldt-Jakob dis- ease. Scand J Clin Lab Invest. 2004;2004(64):101–7.
Castellani RJ, Colucci M, Xie Z, Zou W, Li C, Parchi P, Capellari S, Pastore M, Rahbar MH, Chen SG, Gambetti P. Sensitivity of 14-3-3 protein test varies in subtypes of sporadic Creutzfeldt-Jakob disease. Neurology. 2004;63:436–42.
Chitravas N, Jung RS, Kofskey DM, Blevins JE, Gambetti P, Leigh RJ, Cohen ML. Treatable neurological disorders misdiagnosed as Creutzfeldt-Jakob disease. Ann Neurol. 2011;70:437–44.
Choe LH, Green A, Knight RS, Thompson EJ, Lee KH. Apolipoprotein E and other cerebrospinal fluid proteins differentiate ante mortem variant Creutzfeldt-Jakob disease from antemortem sporadic Creutzfeldt-Jakob disease. Electrophoresis. 2002;23:2242–6.
Choi BY, Kim SY, Seo SY, An SS, Kim S, Park SE, Lee SH, Choi YJ, Kim SJ, Kim CK, Park JS, Ju YR. Mutations at codons 178, 200–129, and 232 contributed to the inherited prion diseases in Korean patients. BMC Infect Dis. 2009;9:132.
Cohen OS, Chapman J, Korczyn AD, Nitsan Z, Appel S, Hoffmann C, Rosenmann H, Kahana E, Lee H. Familial Creutzfeldt-Jakob disease with the E200K mutation: longitudinal neuroimaging from asymptomatic to symptomatic CJD. J Neurol. 2015;262(3):604–13.
Collie DA, Summers DM, Sellar RJ, Ironside JW, Cooper S, Zeidler M, Knight R, Will R. Diagnosing variant Creutzfeldt-Jakob disease with the pulvinar sign: MR imaging findings in 86 neuropathologically confirmed cases. Am J Neuroradiol. 2003;24:1560–9.
Collins SJ, Sanchez-Juan P, Masters CL, Klug GM, van Duijn C, Poleggi A, Pocchiari M, Almonti S, Cuadrado-Corrales N, de Pedro-Cuesta J, Budka H, Gelpi E, Glatzel M, Tolnay M, Hewer E, Zerr I, Heinemann U, Kretzschmar HA, Jansen GH, Olsen E, Mitrova E, Alpérovitsch A, Brandel JP, Mackenzie J, Murray K, Will RGRG. Determinants of diagnostic investigation sensitivities across the clinical spectrum of sporadic Creutzfeldt-Jakob disease. Brain. 2006;129:2278–87.
Cramm M, Schmitz M, Karch A, et al. Stability and reproducibility underscore utility of RT-QuIC for diagnosis of Creutzfeldt-Jakob disease. Mol Neurobiol. 2016;53:1896–904.
Demaerel P, Heiner L, Robberecht W, Sciot R, Wilms G. Diffusion-weighted MRI in spo- radic Creutzfeldt-Jakob disease. Neurology. 1999;52:205–8.
Diaz-Lucena D, Kruse N, Thüne K, Schmitz M, Villar-Piqué A, da Cunha JEG, Hermann P, López-Pérez Ó, Andrés-Benito P, Ladogana A, Calero M, Vidal E, Riggert J, Pineau H, Sim V, Zetterberg H, Blennow K, Del Río JA, Marín-Moreno A, Espinosa JC, Torres JM, Sánchez-Valle R, Mollenhauer B, Ferrer I, Zerr I, Llorens F. TREM2 expression in the brain and biological fluids in prion diseases. Acta Neuropathol. 2021;141(6):841–59.
Dorey A, Tholance Y, Vighetto A, et al. Association of cerebrospinal fluid prion protein levels and the distinction between Alzheimer disease and Creutzfeldt-Jakob disease. JAMA Neurol. 2015;72:267–75.
Eisenmenger L, Porter MC, Carswell CJ, et al. Evolution of diffusion-weighted magnetic resonance imaging signal abnormality in sporadic Creutzfeldt-Jakob disease, with histopathological correlation. JAMA Neurol. 2016;73(1):76–84.
Ermann N, Lewczuk P, Schmitz M, et al. CSF nonphosphorylated Tau as a biomarker for the discrimination of AD from CJD. Ann Clin Transl Neurol. 2018;5:883–7.
Finkenstaedt M, Szudra A, Zerr I, Poser S, Hise JH, Stoebner JM, Weber T. MR imaging of Creutzfeldt-Jakob disease. Radiology. 1996;199:793–8.
Fiorini M, Iselle G, Perra D, et al. High Diagnostic Accuracy of RT-QuIC Assay in a Prospective Study of Patients with Suspected sCJD. Int J Mol Sci. 2020;21:pii: E880.
Foutz A, Appleby BS, Hamlin C, et al. Diagnostic and prognostic value of human prion detection in cerebrospinal fluid. Ann Neurol. 2017;81:79–92.
Franceschini A, Baiardi S, Hughson AG, McKenzie N, Moda F, Rossi M, Capellari S, Green A, Giaccone G, Caughey B, Parchi P. High diagnostic value of second generation CSF RT-QuIC across the wide spectrum of CJD prions. Sci Rep. 2017;7(1):10655.
Fulbright RK, Kingsley PB, Guo X, Hoffmann C, Kahana E, Chapman JC, Prohovnik I. The imaging appearance of Creutzfeldt-Jakob disease caused by the E200K mutation. Magn Reson Imaging. 2006;24:1121–9.
Fulbright RK, Hoffmann C, Lee H, Pozamantir A, Chapman J, Prohovnik I. MR imaging of familial Creutzfeldt-Jakob disease: a blinded and controlled study. AJNR Am J Neuroradiol. 2008;29:1638–43.
Gaig C, Valldeoriola F, Gelpi E, Ezquerra M, Llufriu S, Buongiorno M, Rey MJ, Marti MJ, Graus F, Tolosa E. Rapidly progressive diffuse Lewy body disease. Mov Disord. 2011;26:1316–23.
Gao LP, Shi Q, Xiao K, et al. The genetic Creutzfeldt-Jakob disease with E200K mutation: analysis of clinical, genetic and laboratory features of 30 Chinese patients. Sci Rep. 2019;9(1):1836. Published 2019 Feb 12
Gawinecka J, Ciesielczyk B, Sanchez-Juan P, Schmitz M, Heinemann U, Zerr I. Desmoplakin as a potential candidate for cerebrospinal fluid marker to rule out 14-3-3 false positive rates in sporadic Creutzfeldt–Jakob disease differential diagnosis. Neurodegener Dis. 2012;9:139–44.
Gmitterová K, Heinemann U, Bodemer M, Krasnianski A, Meissner B, Kretzschmar HA, Zerr I. 14-3-3 CSF levels in sporadic Creutzfeldt-Jakob disease differ across molecular sub- types. Neurobiol Aging. 2009;30(11):1842–50.
Green AJ, Thompson EJ, Stewart GE, Zeidler M, McKenzie JM, MacLeod MA, Ironside JW, Will RG, Knight RS. Use of 14-3-3 and other brain-specific proteins in CSF in the diagnosis of variant Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry. 2001;70(6):744–8.
Green AJ, Ramljak S, Muller WE, Knight RS, Schroder HC. 14-3-3 in the cerebrospinal fluid of patients with variant and sporadic Creutzfeldt-Jakob disease measured using capture assay able to detect low levels of 14-3-3 protein. Neurosci Lett. 2002;24:57–60.
Green A, Sanchez-Juan P, Ladogana A, Cuadrado-Corrales N, Sanchez-Valle R, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki J, Heinemann U, Hess K, Slivarichova D, Saiz A, Calero M, Mellina V, Knight R, van Dujin CM, Zerr I. CSF analysis in patients with sporadic CJD and other transmissible spongiform encephalopathies. Eur J Neurol. 2007;14:121–4.
Groveman BR, Orrú CD, Hughson AG, et al. Extended and direct evaluation of RT-QuIC assays for Creutzfeldt-Jakob disease diagnosis. Ann Clin Transl Neurol. 2017;4:139–44.
Guillaume E, Zimmermann C, Burkhard PR, Hochstrasser DF, Sanchez JC. A potential cerebrospinal fluid and plasmatic marker for the diagnosis of Creutzfeldt-Jakob disease. Proteomics. 2003;3:1495–9.
Halbgebauer S, Abu-Rumeileh S, Oeckl P, Steinacker P, Roselli F, Wiesner D, Mammana A, Beekes M, Kortazar-Zubizarreta I, Perez de Nanclares G, Capellari S, Giese A, Castilla J, Ludolph AC, Žáková D, Parchi P, Otto M. Blood β-synuclein and neurofilament light chain during the course of prion disease. Neurology. 2022;98(14):e1434–45.
Harrington MG, Merril CR, Asher DM, Gajdusek DC. Abnormal proteins in the cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. N Engl J Med. 1986;315:279–83.
Heinemann U, Krasnianski A, Meissner B, Gloeckner SF, Kretzschmar HA, Zerr I. Molecular subtype-specific clinical diagnosis of prion diseases. Vet Microbiol. 2007a;123:328–35.
Heinemann U, Krasnianski A, Meissner B, Varges D, Kallenberg K, Schulz-Schaeffer WJ, Steinhoff BJ, Grasbon-Frodl EM, Kretzschmar HA, Zerr I. Creutzfeldt-Jakob disease in Germany: a prospective 12-year surveillance. Brain. 2007b;130(Pt 5):1350–9.
Hermann P, Laux M, Glatzel M, et al. Validation and utilization of amended diagnostic criteria in Creutzfeldt-Jakob disease surveillance. Neurology. 2018;91:e331–8.
Hermann P, Koch JC, Zerr I. Genetic prion disease: opportunities for early therapeutic intervention with rigorous pre-symptomatic trials. Expert Opin Investig Drugs. 2020;29(12):1313–6.
Hermann P, Appleby B, Brandel JP, Caughey B, Collins S, Geschwind MD, Green A, Haïk S, Kovacs GG, Ladogana A, Llorens F, Mead S, Nishida N, Pal S, Parchi P, Pocchiari M, Satoh K, Zanusso G, Zerr I. Biomarkers and diagnostic guidelines for sporadic Creutzfeldt-Jakob disease. Lancet Neurol. 2021;20(3):235–46.
Hermann P, Haller P, Goebel S, Bunck T, Schmidt C, Wiltfang J, Zerr I. Total and phosphorylated cerebrospinal fluid tau in the differential diagnosis of sporadic Creutzfeldt-Jakob disease and rapidly progressive Alzheimer’s disease. Viruses. 2022;14(2):276.
Holsinger RM, Lee JS, Boyd A, Masters CL, Collins SJ. CSF BACE1 activity is increased in CJD and Alzheimer disease versus [corrected] other dementias. Neurology. 2006;67:710–2.
Hsich G, Kenney K, Gibbs CJ Jr, Lee KH, Harrington MG. The 14-3-3 brain protein in cerebrospinal fluid as a marker for transmissible spongifrom encephalopathies. N Engl J Med. 1996;335:924–30.
Jesse S, Steinacker P, Cepek L, von Arnim CA, Tumani H, Lehnert S, Kretzschmar HA, Baier M, Otto M. Glial fibrillary acidic protein and protein S-100B: different concentration pat- tern of glial proteins in cerebrospinal fluid of patients with Alzheimer’s disease and Creutzfeldt- Jakob disease. J Alzheimers Dis. 2009;17:541–51.
Josephs KA, Ahlskog JE, Parisi JE, Boeve BF, Crum BA, Giannini C, Petersen RC. Rapidly progressive neurodegenerative dementias. Arch Neurol. 2009;66:201–7.
Kasai T, Tokuda T, Ishii R, Ishigami N, Tsuboi Y, Nakagawa M, Mizuno T, El-Agnaf OM. Increased α-synuclein levels in the cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. J Neurol. 2014;261(6):1203–9.
Kelley BJ, Boeve BF, Josephs KA. Young-onset dementia: demographic and etiologic char- acteristics of 235 patients. Arch Neurol. 2008;65:1502–8.
Kettlun A, Collados L, Garcia L, Cartier LA, Wolf ME, Mosnaim AD, Valenzuela MA. Matrix metalloproteinase profile in patients with Creuztfeldt-Jakob disease. Int J Clin Pract. 2003;57:475–8.
Koizumi R, Ueda N, Mugita A, Kimura K, Kishida H, Tanaka F. Case report: Extremely early detection of preclinical magnetic resonance imaging abnormality in Creutzfeldt-Jakob disease with the V180I mutation. Front Neurol. 2021;12:751750.
Kovacs GG, Andreasson U, Liman V, et al. Plasma and cerebrospinal fluid tau and neurofilament concentrations in rapidly progressive neurological syndromes: a neuropathology-based cohort. Eur J Neurol. 2017;24:1326–e77.
Kovacs GG, Andreasson U, Liman V, Regelsberger G, Lutz MI, Danics K, Keller E, Zetterberg H, Blennow K. Plasma and cerebrospinal fluid tau and neurofilament concentrations in rapidly progressive neurological syndromes: a neuropathology-based cohort. Eur J Neurol. 2017c;24(11):1326–e77.
Krammer C, Vorberg I, Schätzl HM, Gilch S. Therapy in prion diseases: from molecular and cellular biology to therapeutic targets. Infect Disord Drug Targets. 2009;9:3–14.
Krasnianski A, Schulz-Schaeffer WJ, Kallenberg K, Meissner B, Collie DA, Roeber S, Bartl M, Heinemann U, Varges D, Kretzschmar HA, Zerr I. Clinical findings and diagnostic tests in the MV-2 subtype of sporadic CJD. Brain. 2006;129:2288–96.
Krasnianski A, Heinemann U, Ponto C, Kortt J, Kallenberg K, Varges D, Schulz-Schaeffer WJ, Kretzschmar HA, Zerr I. Clinical findings and diagnosis in genetic prion diseases in Germany. Eur J Epidemiol. 2016;31(2):187–96.
Ladogana A, Puopolo M, Croes EA, Budka H, Jarius C, Collins S, Klug GM, Sutcliffe T, Giulivi A, Alperovitch A, Delasnerie-Laupretre N, Brandel J-P, Poser S, Kretzschmar H, Rietveld I, Mitrova E, de Pedro-Cuesta J, Martinez-Martin P, Glatzel M, Aguzzi A, Knight R, Ward H, Pocchiari M, van Duijn CM, Will RG, Zerr I. Mortality from Creutzfeldt-Jakob disease and related disorders in Europe, Australia, and Canada. Neurology. 2005;64:1586–91.
Ladogana A, Sanchez-Juan P, Mitrova E, Green A, Cuadrado-Corrales N, Sanchez-Valle R, Koscova S, Aguzzi A, Sklaviadis T, Kulczycki J, Gawinecka J, Saiz A, Calero M, van Duijn CM, Pocchiari M, Knight R, Zerr I. Cerebrospinal fluid biomarkers in human genetic transmissible spongiform encephalopathies. J Neurol. 2009;256:1620–8.
Lattanzio F, Abu-Rumeileh S, Franceschini A, et al. Prion-specific and surrogate CSF biomarkers in Creutzfeldt-Jakob disease: diagnostic accuracy in relation to molecular subtypes and analysis of neuropathological correlates of p-tau and Aβ42 levels. Acta Neuropathol. 2017;133:559–78.
Lee H, Rosenmann H, Chapman J, Kingsley PB, Hoffmann C, Cohen OS, Kahana E, Korczyn AD, Prohovnik I. Thalamo-striatal diffusion reductions precede disease onset in prion muta- tion carriers. Brain. 2009;132:2680–7.
Lee H, Cohen OS, Hoffmann C, Prohovnik I. Putaminal volume and diffusion in early familial Creutzfeldt-Jakob disease. J Neurol Sci. 2010;288:129–34.
Leitão MJ, Baldeiras I, Almeida MR, et al. Sporadic Creutzfeldt-Jakob disease diagnostic accuracy is improved by a new CSF ELISA 14-3-3γ assay. Neuroscience. 2016;322:398–407.
Li J, Duan Y, Zhao D, et al. Detection of Cell-Free Mitochondrial DNA in Cerebrospinal Fluid of Creutzfeldt-Jakob Patients. Front Neurol. 2019;10:645.
Llorens F, Thüne K, Tahir W, et al. YKL-40 in the brain and cerebrospinal fluid of neurodegenerative dementias. Mol Neurodegener. 2017;12:83.
Llorens F, Villar-Piqué A, Hermann P, et al. Cerebrospinal fluid non-phosphorylated tau in the differential diagnosis of Creutzfeldt-Jakob disease: a comparative prospective study with 14-3-3. J Neurol. 2020a;267:543–50.
Llorens F, Villar-Piqué A, Hermann P, Schmitz M, Calero O, Stehmann C, Sarros S, Moda F, Ferrer I, Poleggi A, Pocchiari M, Catania M, Klotz S, O’Regan C, Brett F, Heffernan J, Ladogana A, Collins SJ, Calero M, Kovacs GG, Zerr I. Diagnostic accuracy of prion disease biomarkers in Iatrogenic Creutzfeldt-Jakob disease. Biomolecules. 2020b;10(2):290.
Llorens F, Villar-Piqué A, Schmitz M, et al. Plasma total prion protein as a potential biomarker for neurodegenerative dementia: diagnostic accuracy in the spectrum of prion diseases. Neuropathol Appl Neurobiol. 2020c;46:240–54.
López-Pérez Ó, Bernal-Martín M, Hernaiz A, et al. BAMBI and CHGA in Prion Diseases: Neuropathological Assessment and Potential Role as Disease Biomarkers. Biomolecules. 2020;10:706.
Maat P, de Beukelaar JW, Jansen C, Schuur M, van Duijn CM, van Coevorden MH, et al. Pathologically confirmed autoimmune encephalitis in suspected Creutzfeldt-Jakob disease. Neurol Neuroimmunol Neuroinflamm. 2015;2:e178.
Mammana A, Baiardi S, Rossi M, et al. Detection of prions in skin punch biopsies of Creutzfeldt-Jakob disease patients. Ann Clin Transl Neurol. 2020;7:559–64.
Manaka H, Kato T, Kurita K, Katagiri T, Shikama Y, Kujirai K, Kawanami T, Suzuki Y, Nihei K, Sasaki H, et al. Marked increase in cerebrospinal fluid ubiquitin in Creutzfeldt-Jakob disease. Neurosci Lett. 1992;139:47–9.
Marquetand J, Knake S, Strzelczyk A, et al. Periodic EEG patterns in sporadic Creutzfeld-Jakob-Disease can be benzodiazepine-responsive and be difficult to distinguish from non-convulsive status epilepticus. Seizure. 2017;53:47–50.
Masters CL, Harris JO, Gajdusek DC, Gibbs CJJ, Bernoulli C, Asher DM. Creutzfeldt- Jakob disease: patterns of worldwide occurrence and the significance of familial and sporadic clustering. Ann Neurol. 1979;5:177–88.
McGuire LI, Peden AH, Orrú CD, et al. RT-QuIC analysis of cerebrospinal fluid in sporadic Creutzfeldt-Jakob disease. Ann Neurol. 2012;72:278–85.
Meissner B, Kallenberg K, Sanchez-Juan P, Krasnianski A, Heinemann U, Varges D, Knauth M, Zerr I. Isolated cortical signal increase on MR imaging as a frequent lesion pattern in sporadic Creutzfeldt-Jakob disease. Am J Neuroradiol. 2008;29:1519–24.
Meissner B, Kallenberg K, Sanchez-Juan P, Collie D, Summers DM, Almonti S, Collins SJ, Smith P, Cras P, Jansen GH, Brandel JP, Coulthart MB, Roberts H, Van Everbroeck B, Galanaud D, Mellina V, Will RG, Zerr I. MRI lesion profiles in sporadic Creutzfeldt-Jakob disease. Neurology. 2009;72(23):1994–2001.
Minghetti L, Cardone F, Greco A, Puopolo M, Levi G, Green AJ, Knight R, Pocchiari P. Increased CSF levels of prostaglandin E(2) in variant Creutzfeldt-Jakob disease. Neurology. 2002;58:127–9.
Muayqil T, Gronseth G, Camicioli R. Evidence-based guideline: diagnostic accuracy of CSF 14-3-3 protein in sporadic Creutzfeldt-Jakob disease: report of the guideline development subcommittee of the American Academy of Neurology. Neurology. 2012;79:1499–506.
Norsworthy PJ, Thompson AGB, Mok TH, et al. A blood miRNA signature associates with sporadic Creutzfeldt-Jakob disease diagnosis. Nat Commun. 2020;11:3960.
Nozaki I, Hamaguchi T, Sanjo N, Noguchi-Shinohara M, Sakai K, Nakamura Y, Sato T, Kitamoto T, Mizusawa H, Moriwaka F, Shiga Y, Kuroiwa Y, Nishizawa M, Kuzuhara S, Inuzuka T, Takeda M, Kuroda S, Abe K, Murai H, Murayama S, Tateishi J, Takumi I, Shirabe S, Harada M, Sadakane A, Yamada M. Prospective 10-year surveillance of human prion diseases in Japan. Brain. 2010;133(10):3043–57.
Nozaki I, Hamaguchi T, Sanjo N, Noguchi-Shinohara M, Sakai K, Nakamura Y, Sato T, Kitamoto Novi G, Canosa A, Nobili F, et al. Longitudinal brain magnetic resonance imaging and real-time quaking induced conversion analysis in presymptomatic Creutzfeldt-Jakob disease. Eur J Neurol. 2018;25(12):e127–8.
Oeckl P, Steinacker P, Lehnert S, Jesse S, Kretzschmar HA, Ludolph AC, Otto M, Ferger B. CSF concentrations of cAMP and cGMP are lower in patients with Creutzfeldt-Jakob disease but not Parkinson’s disease and amyotrophic lateral sclerosis. PLoS One. 2012;7(3):e32664.
Oeckl P, Metzger F, Nagl M, et al. Alpha-, Beta-, and Gamma-synuclein Quantification in Cerebrospinal Fluid by Multiple Reaction Monitoring Reveals Increased Concentrations in Alzheimer’s and Creutzfeldt-Jakob Disease but No Alteration in Synucleinopathies. Mol Cell Proteomics. 2016;15:3126–38.
Oeckl P, Halbgebauer S, Anderl-Straub S, et al. Targeted Mass Spectrometry Suggests Beta-Synuclein as Synaptic Blood Marker in Alzheimer’s Disease. J Proteome Res. 2020;19:1310–8.
Orrú CD, Bongianni M, Tonoli G, et al. A test for Creutzfeldt-Jakob disease using nasal brushings. N Engl J Med. 2014;371:519–29.
Orrú CD, Groveman BR, Hughson AG, Zanusso G, Coulthart MB, Caughey B. Rapid and sensitive RT-QuIC detection of human Creutzfeldt-Jakob disease using cerebrospinal fluid. MBio. 2015;6:e02451–14.
Otto M, Wiltfang J, Schütz E, Zerr I, Otto A, Pfahlberg A, Gefeller O, Uhr M, Giese A, Weber T, Kretzschmar HA, Poser S. Diagnosis of Creutzfeldt-Jakob disease by measurement of S100 protein in serum: prospective case-control study. BMJ. 1998;316(7131):577–82.
Papageorgiou SG, Kontaxis T, Bonakis A, et al. Rapidly progressive dementia: Causes found in a Greek tertiary referral center in Athens. Alzheimer Dis Assoc Disord. 2009;23:337–46.
Parchi P, Castellani R, Capellari S, Ghetti B, Young K, Chen SG, Farlow M, Dickson DW, Sima AAF, Trojanowski JQ, Petersen RB, Gambetti P. Molecular basis of phenotypic vari- ability in sporadic Creutzfeldt-Jakob disease. Ann Neurol. 1996;39:767–78.
Parchi P, Giese A, Capellari S, et al. Classification of sporadic Creutzfeldt-Jakob disease based on molecular and phenotypic analysis of 300 subjects. Ann Neurol. 1999;46:224–33.
Park JH, Choi YG, Lee YJ, et al. Real-Time Quaking-Induced Conversion Analysis for the Diagnosis of Sporadic Creutzfeldt-Jakob Disease in Korea. J Clin Neurol. 2016;12:101–6.
Pascuzzo R, Oxtoby NP, Young AL, et al. Prion propagation estimated from brain diffusion MRI is subtype dependent in sporadic Creutzfeldt-Jakob disease. Acta Neuropathol. 2020;140:169–81.
Piubelli C, Fiorini M, Zanusso G, Milli A, Fasoli E, Monaco S, Righetti PG. Searching for markers of Creutzfeldt-Jakob disease in cerebrospinal fluid by two-dimensional mapping. Proteomics. 2006;6(Suppl 1):256–61.
Rhoads DD, Wrona A, Foutz A, Blevins J, Glisic K, Person M, Maddox RA, Belay ED, Schonberger LB, Tatsuoka C, Cohen ML, Appleby BS. Diagnosis of prion diseases by RT-QuIC results in improved surveillance. Neurology. 2020;95(8):e1017–26.
Rosenmann H, Meiner Z, Kahana E, Halimi M, Lenetsky E, Abramsky O, Gabizon R. Detection of 14-3-3 protein in the CSF of genetic Creutzfeldt-Jakob disease. Neurology. 1997;49:593–5.
Rudge P, Hyare H, Green A, Collinge J, Mead S. Imaging and CSF analyses effectively distinguish CJD from its mimics. J Neurol Neurosurg Psychiatry. 2018;89:461–6.
Sanchez JC, Guillaume E, Lescuyer P, Allard L, Carrette O, Scherl A, Burgess J, Corthals GL, Burkhard PR, Hochstrasser DF. Cystatin C as a potential cerebrospinal fluid marker for the diagnosis of Creutzfeldt-Jakob disease. Proteomics. 2004;4:2229–33.
Sanchez-Juan P, Green A, Ladogana A, Cuadrado-Corrales N, Sanchez-Valle R, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki J, Hess K, Bodemer M, Slivarichova D, Saiz A, Calero M, Ingrosso L, Knight R, Janssens C, Van Duijn C, Zerr I. CSF tests in the differential diagnosis of Creutzfeldt-Jakob disease. Neurology. 2006;67:637–43.
Sanchez-Juan P, Sanchez-Valle R, Green A, Ladogana A, Cuadrado-Corrales N, Mitrova E, Stoeck K, Sklaviadis T, Kulczycki J, Hess K, Krasnianski A, Equestre M, Slivarichova D, Saiz A, Calero M, Pocchiari M, Knight R, van Dujin CM, Zerr I. Influence of timing on CSF tests value for Creutzfeldt-Jakob disease diagnosis. J Neurol. 2007;254:901–6.
Schmidt H, Otto M, Niedmann P, Cepek L, Schroter A, Kretzschmar HA, Poser S. CSF lactate dehydrogenase activity in patients with Creutzfeldt-Jakob disease exceeds that in other dementias. Dement Geriatr Cogn Disord. 2004;17:204–6.
Schmidt C, Redyk K, Meissner B, Krack L, von Ahsen N, Roeber S, Kretzschmar H, Zerr I. Clinical features of rapidly progressive Alzheimer’s disease. Dement Geriatr Cogn Disord. 2010;29:371–8.
Schmitz M, Ebert E, Stoeck K, et al. Validation of 14-3-3 Protein as a Marker in Sporadic Creutzfeldt-Jakob Disease Diagnostic. Mol Neurobiol. 2016a;53:2189–99.
Schmitz M, Llorens F, Pracht A, et al. Regulation of human cerebrospinal fluid malate dehydrogenase 1 in sporadic Creutzfeldt-Jakob disease patients. Aging (Albany NY). 2016b;8:2927–35.
Schmitz M, Villar-Piqué A, Hermann P, Escaramís G, Calero M, Chen C, Kruse N, Cramm M, Golanska E, Sikorska B, Liberski PP, Pocchiari M, Lange P, Stehmann C, Sarros S, Martí E, Baldeiras I, Santana I, Žáková D, Mitrová E, Dong XP, Collins S, Poleggi A, Ladogana A, Mollenhauer B, Kovacs GG, Geschwind MD, Sánchez-Valle R, Zerr I, Llorens F. Diagnostic accuracy of cerebrospinal fluid biomarkers in genetic prion diseases. Brain. 2022;145(2):700–12.
Schröter A, Zerr I, Henkel K, Tschampa HJ, Finkenstaedt M, Poser S. Magnetic resonance imaging (MRI) in the clinical diagnosis of Creutzfeldt-Jakob disease. Arch Neurol. 2000;57:1751–7.
Seror I, Lee H, Cohen OS, Hoffmann C, Prohovnik I. Putaminal volume and diffusion in early familial Creutzfeldt-Jakob disease. J Neurol Sci. 2010;288:129–34.
Silveyra MX, Garcia-Ayllon MS, Calero M, Saez-Valero J. Altered glycosylation of acetyl- cholinesterase in the Creutzfeldt-Jakob cerebrospinal fluid. J Mol Neurosci. 2006;30:65–6.
Singh A, Beveridge AJ, Singh N. Decreased CSF transferrin in sCJD: a potential pre-mortem diagnostic test for prion disorders. PLoS One. 2011;6(3):e16804.
Skillbäck T, Rosén C, Asztely F, Mattsson N, Blennow K, Zetterberg H. Diagnostic performance of cerebrospinal fluid total tau and phosphorylated tau in Creutzfeldt-Jakob disease: results from the Swedish Mortality Registry. JAMA Neurol. 2014;71:476–83.
Steinacker P, Blennow K, Halbgebauer S, et al. Neurofilaments in blood and CSF for diagnosis and prediction of onset in Creutzfeldt-Jakob disease. Sci Rep. 2016;6:38737.
Steinhoff BJ, Zerr I, Glatting M, et al. Diagnostic value of periodic complexes in Creutzfeldt-Jakob disease. Ann Neurol. 2004;56:702–8.
Steinhoff BJ, Grasbon-Frodl EM, Kretzschmar HA, Zerr I. Creutzfeldt-Jakob disease in Germany: a prospective 12-year surveillance. Brain. 2007;130:1350–9.
Stoeck K, Bodemer M, Ciesielczyk B, Meissner B, Bartl M, Heinemann U, Zerr I. Interleukin 4 and interleukin 10 levels are elevated in the cerebrospinal fluid of patients with Creutzfeldt- Jakob disease. Arch Neurol. 2005;62:1591–4.
Stoeck K, Bodemer M, Zerr I. Pro- and anti-inflammatory cytokines in the CSF of patients with Creutzfeldt-Jakob disease. J Neuroimmunol. 2006;172:175–81.
Stoeck K, Sanchez-Juan P, Gawinecka J, Green A, Ladogana A, Pocchiari M, Sanchez-Valle R, Mitrova E, Sklaviadis T, Kulczycki J, Slivarichova D, Saiz A, Calero M, Knight R, Aguzzi A, Laplanche JL, Peoc’h K, Schelzke G, Karch A, van Duijn CM, Zerr I. Cerebrospinal fluid biomarker supported diagnosis of Creutzfeldt-Jakob disease and rapid dementias: a longitudinal multicentre study over 10 years. Brain. 2012;135(Pt 10):3051–61.
Studart Neto A, Soares Neto HR, Simabukuro MM, et al. Rapidly progressive dementia: prevalence and causes in a neurologic unit of a tertiary hospital in Brazil. Alzheimer Dis Assoc Disord. 2017;31:239–43.
Thompson AGB, Luk C, Heslegrave AJ, et al. Neurofilament light chain and tau concentrations are markedly increased in the serum of patients with sporadic Creutzfeldt-Jakob disease, and tau correlates with rate of disease progression. J Neurol Neurosurg Psychiatry. 2018;89:955–61.
Thompson AGB, Anastasiadis P, Druyeh R, et al. Evaluation of plasma tau and neurofilament light chain biomarkers in a 12-year clinical cohort of human prion diseases. Mol Psychiatry. 2021;26(10):5955–66.
Tribl GG, Strasser G, Zeitlhofer J, Asenbaum S, Jarius C, Wessely P, Prayer D. Sequential MRI in a case of Creutzfeld-Jakob disease. Neuroradiology. 2002;44:223–6.
Tschampa HJ, Kallenberg K, Urbach H, Meissner BCN, Kretzschmar HA, Knauth M, Zerr I. MRI in the diagnosis of sporadic Creutzfeldt-Jakob disease: a study on inter-observer agree- ment. Brain. 2005;128:2026–33.
Tsuboi Y, Baba Y, Doh-ura K, Imamura A, Fujioka S, Yamada T. Diffusion-weighted MRI in familial Creutzfeldt-Jakob disease with the codon 200 mutation in the prion protein gene. J Neurol Sci. 2005;232:45–9.
Ukisu R, Kushihashi T, Kitanosono T, et al. Serial diffusion-weighted MRI of Creutzfeldt-Jakob disease. AJR Am J Roentgenol. 2005;184:560–6.
Urbach H, Klisch J, Wolf HK, Brechtelsbauer D, Gass S, Solymosi L. MRI in sporadic Creutzfeldt-Jakob disease: correlation with clinical and neuropathological data. Neuroradiology. 1998;40:65–70.
Vallabh SM, Minikel EV, Schreiber SL, Lander ES. Towards a treatment for genetic prion disease: trials and biomarkers. Lancet Neurol. 2020;19:361–8.
Van Everbroeck B, Quoilin S, Boons J, Martin JJ, Cras P. A prospective study of CSF mark- ers in 250 patients with possible Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry. 2003;74:1210–4.
Van Everbroeck B, Dobbeleir I, De Waele M, De Deyn P, Martin J-J, Cras P. Differential diagnosis of 201 possible Creutzfeldt-Jakob disease patients. J Neurol. 2004;251:298–304.
Villar-Piqué A, Schmitz M, Lachmann I, Karch A, Calero O, Stehmann C, Sarros S, Ladogana A, Poleggi A, Santana I, Ferrer I, Mitrova E, Žáková D, Pocchiari M, Baldeiras I, Calero M, Collins SJ, Geschwind MD, Sánchez-Valle R, Zerr I, Llorens F. Cerebrospinal Fluid Total Prion Protein in the Spectrum of Prion Diseases.Mol Neurobiol. 2019 Apr;56(4):2811-2821.
Villar-Piqué A, Schmitz M, Hermann P, et al. Plasma YKL-40 in the spectrum of neurodegenerative dementia. J Neuroinflammation. 2019;16:145.
Vitali P, Maccagnano E, Caverzasi E, et al. Diffusion-weighted MRI hyperintensity patterns differentiate CJD from other rapid dementias. Neurology. 2011;76:1711–9.
Völkel D, Zimmermann K, Zerr I, Bodemer M, Lindner T, Turecek PL, Poser S, Schwarz HP. Immunochemical determination of cellular prion protein in plasma from healthy subjects and patients with sporadic CJD or other neurologic diseases. Transfusion. 2001;41:441–8.
Watson N, Hermann P, Ladogana A, Denouel A, Baiardi S, Colaizzo E, Giaccone G, Glatzel M, Green AJE, Haïk S, Imperiale D, MacKenzie J, Moda F, Smith C, Summers D, Tiple D, Vaianella L, Zanusso G, Pocchiari M, Zerr I, Parchi P, Brandel JP, Pal S. Validation of revised international Creutzfeldt-Jakob disease surveillance network diagnostic criteria for Sporadic Creutzfeldt-Jakob Disease. JAMA Netw Open. 2022;5(1):e2146319.
WHO. WHO manual for surveillance of human transmissible spongiform encephalopathies including variant Creutzfeldt-Jakob disease. WHO Library Cataloguing-in-Publication Data; 2003.
Will RG, Zeidler M, Stewart GE, Macleod MA, Ironside JW, Cousens SN, Mackenzie J, Estibeiro K, Green AJ, Knight RS. Diagnosis of new variant Creutzfeldt-Jakob disease. Ann Neurol. 2000;47:575–82.
Young GS, Geschwind MD, Fischbein NJ, Martindale JL, Henry RG, Liu S, Lu Y, Wong S, Liu H, Miller BL, Dillon WP. Diffusion-weighted and fluid-attenuated inversion recovery imaging in Creutzfeldt-Jakob disease: high sensitivity and specificity for diagnosis. Am J Neuroradiol. 2005;26:1551–62.
Zanusso G, Camporese G, Ferrari S, et al. Long-term preclinical magnetic resonance imaging alterations in sporadic Creutzfeldt–Jakob disease. Ann Neurol. 2016;80:629–32.
Zerr I. Laboratory diagnosis of Creutzfeldt-Jakob disease. N Engl J Med. 2022;386:1345–50.
Zerr I, Hermann P. Diagnostic challenges in rapidly progressive dementia. Expert Rev Neurother. 2018;18(10):761–72.
Zerr I, Bodemer M, Gefeller O, Otto M, Poser S, Wiltfang J, Windl O, Kretzschmar HA, Weber T. Detection of 14-3-3 protein in the cerebrospinal fluid supports the diagnosis of Creutzfeldt-Jakob disease. Ann Neurol. 1998a;43:32–40.
Zerr I, Pocchiari M, Collins S, Brandel JP, de Pedro CJ, Knight RSG, Bernheimer H, Cardone F, Delasnerie-Lauprêtre N, Cuadrado Corrales N, Ladogana A, Fletcher A, Bodemer M, Awan T, Ruiz Bremón A, Budka H, Laplanche JL, Will RG, Poser S. Analysis of EEG and CSF 14-3-3 proteins as aids to the diagnosis of Creutzfeldt-Jakob disease. Neurology. 2000;55:811–5.
Zerr I, Bodemer M, Kaboth U, Kretzschmar H, Oellerich M, Armstrong VW. Plasminogen activities and concentrations in patients with sporadic Creutzfeldt-Jakob disease. Neurosci Lett. 2004;371:163–6.
Zerr I, Kallenberg K, Summers DM, Romero C, Taratuto A, Ladogana A, Schuur M, Haik S, Collins SJ, Jansen GH, Stokin GB, Pimentel J, Hewer E, Collie DA, Smith P, Varges D, Heinemann U, Meissner B, Roberts H, Brandel JP, Van Dujin CM, Pocchiari M, Begue P, Cras P, Will RG, Sanchez-Juan P. Updated clinical diagnostic criteria for sporadic Creutzfeldt- Jakob disease. Brain. 2009;132:2659–68.
Zerr I, Villar-Piqué A, Hermann P, et al. Diagnostic and prognostic value of plasma neurofilament light and total-tau in sporadic Creutzfeldt-Jakob disease. Alzheimers Res Ther. 2021;13(1):86. Published 2021 Apr 21
Zhang Y, Gao T, Tao QQ. Spectrum of noncerebrovascular rapidly progressive cognitive deterioration: a 2-year retrospective study. Clin Interv Aging. 2017;12:1655–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Zerr, I., Hermann, P. (2023). Diagnosis of Prion Disease: Conventional Approaches. In: Zou, WQ., Gambetti, P. (eds) Prions and Diseases. Springer, Cham. https://doi.org/10.1007/978-3-031-20565-1_33
Download citation
DOI: https://doi.org/10.1007/978-3-031-20565-1_33
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20564-4
Online ISBN: 978-3-031-20565-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)