Abstract
The focus of this chapter is on visualization of QT data for thorough QT (TQT) study analysis and review. The use of graphics is particularly important for QT data due to the high variability and to explore the adequacy of heart rate QT correction, baseline adjustments, choice of positive control to establish assay sensitivity, and the relationship between exposure and QT prolongation. A QT knowledge management system implemented in the R package “QT” standardizes and automates the QT data analyses, graphical representation, and reporting. This allows for easier communication of the results because the analyses are consistent and enables pooled data analysis across TQT studies to address drug development related questions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The objective of a thorough QT (TQT) study is to determine whether a drug has a pharmacological effect on cardiac repolarization as detected by a QT prolongation on the surface electrocardiogram (ECG) as described in the guideline (ICH E14). Refer to Chap. 18 for more information about ECGs and the QT interval.
The ΔQTc (time-matched baseline adjusted QTc) and ΔΔQTc (time-matched change from placebo- and baseline-adjusted QTc) used for the central tendency and concentration–QTc analyses are calculated by
where the baseline QTc is calculated as the mean of the pre-dose ECG measurements for each treatment.
A key component for assessing the QT prolongation potential of a drug is to create informative graphs that are tailored to address the key questions to be answered. For that purpose, the R package “QT” (requires SAS™) was developed based on the accumulated review experience from the FDA’s interdisciplinary review team for QT (IRT-QT) (Tornoe et al. 2011). The purpose was to develop standardized graphics to increase the productivity, consistency, and quality-thereby ensuring faster and easier communication between the team of inter-disciplinary scientists.
While other papers focus on issues related to TQT study design, conduct, and analysis methods, the objective of this chapter is the visualization of QT data for TQT study analysis and review to make informed decisions through the following 10 steps:
-
1.
Data integrity
-
2.
QT correction method
-
3.
Adequacy of sampling times
-
4.
Baseline corrections
-
5.
Assay sensitivity
-
6.
Measure of central tendency
-
7.
Assessing delay between drug and QT effects
-
8.
Relationship between drug exposure and QT prolongation
-
9.
Prediction of QT prolongation at different exposure levels
-
10.
Benefit-risk assessment
2 Developing Standardized Graphics for QT Data
The high variability and low signal-to-noise ratio (trying to exclude a 10 ms QT prolongation) in QT measurements makes it difficult to spot trends and relationships based on individual data points. For this purpose, tailored quantile plots were developed.
The quantile plot is generated by binning the independent variable (e.g., RR or concentrations) into quantiles (bins with equal numbers of observations) and plotting the local median or midpoint of the observations in each of the independent variable bins against the corresponding local mean dependent variable (e.g., QT or ΔΔQT and associated 90% confidence interval). This is the binning method implemented in the R package.
A potential issue arises when using the local means across the dependent variable quantiles. The different bins can potentially be imbalanced in the number of individuals. Taking the mean of all observations in each bin and calculating the standard deviation for that mean ignores that some of the observations are correlated since they arise from the same subject. This is most likely to be an issue when pooling data from different studies with different variability in PK. One way to account for this imbalance is to use precision weighted averages in each bin by
where σ 2 is the variance of the measurements in the bin, N is the number of subjects in the bin, and n i is the number of measurements for the ith subject in the bin. M i is the mean of the ith subject’s measurements that fall into the bin.
Another way to avoid the complex calculations of the mean of the dependent variable is to calculate it for each sampling time thereby ensuring that only one measurement per subject is present in each of the bins. The disadvantage, however, is that the bins are not distributed evenly over the range of measurements.
3 QT Knowledge Management System
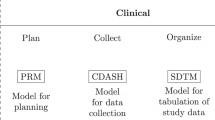
The QT knowledge management system developed for automatic QT data analyses and reporting is implemented in the R package “QT” (http://www.cran.r-project.org) that performs the data manipulation and graphical presentation of results, executes the linear mixed-effects analyses in SAS, and generates an analysis report with key results and figures.
The data template for the R package is shown in Table 16.1.
The “QT” R package consists of 5 main functions (the R and SAS code can be found at http://qttool.googlecode.com):
-
QTcorrections: This function performs the QT-RR analysis on off-drug treatment data and evaluates the ability of the different QT corrections to remove the heart rate effect on on-drug treatment data using PROC MIXED in SAS
-
DataCheck: The DataCheck function visualizes key data to check the integrity of the analysis dataset
-
MeanData: The MeanData function calculates and plots the mean profiles, and creates the dataset for the QTc-time and concentration–QTc analyses
-
QTtime: The central tendency analysis of QTc versus time is performed in SAS using PROC MIXED
-
QTconc: The concentration–QTc analysis is performed in SAS using PROC MIXED. Three models are estimated, i.e., (1) “with intercept,” (2) “no intercept,” and (3) “intercept fixed to zero with variability.” The results are summarized in tables and graphs
4 Visualization of QT Data in Ten Steps for TQT Study Analysis and Review
In the following, the 10 visual steps for TQT study analysis and review are illustrated using simulated data included in the R package “QT.” The simulated TQT study is a 4-way crossover design with placebo, moxifloxacin (active control), and therapeutic and supra-therapeutic doses of the drug candidate. The colors used for the different treatment arms are consistent in the following figures with black, orange, blue, and red representing placebo, moxifloxacin, therapeutic dose, and supra-therapeutic dose, respectively. Mean and 90% confidence interval are used throughout.
4.1 Data Integrity
Initially, the derived dataset containing QT-, RR-, and concentration–time profiles are inspected by visualizing the data to ensure the merging of data is performed correctly. In Fig. 16.1, the QT, RR, moxifloxacin, and drug X concentrations are plotted for the 4 treatments to assess whether there are outliers, unrealistic values, or unit differences in the measurements.
4.2 QT Correction Method
Before assessing the QT prolongation potential of a drug, the heart rate effect should be removed first since it is known to affect the QT interval. The relationship between QT interval length and heart rate (using the RR interval) is investigated using the available off-drug data only (Fig. 16.2 top). Given the high variability in QT measurements, it is difficult to assess the adequacy of the QT correction method when visualizing the individual data points and comparing it to the estimated regression line (Fig. 16.2 top). However, by using the previously described quantile plot a different intercept (at RR = 1,000 ms) and slope between males and females are clearly seen in Fig. 16.2 (bottom).
Placebo QT vs. RR relationship. (Top) Observed placebo QT-RR for males (gray squares) and females (black circles) together with the mean predictions (males = blue, females = red). (Bottom) Mean (90% confidence interval) predicted QT-RR curves. The dots represent the observed median RR quantiles and associated mean (90% confidence interval) QT. RR quantile ranges for males (blue) and females (red) are shown along the x-axis
In Fig. 16.3, the individual relationship between QT, QTcB (Bazzett’s), QTcF (Fridericia), and QTcI (Individual correction) and RR indicates that QTcB overcorrects for heart rate whereas QTcF and QTcI both seem to be appropriate correction methods.
The choice of the heart rate correction method to use for further analyses is further investigated by estimating a linear model using on-drug data to see whether the slope is significantly different from zero indicating whether there still is a relationship between QT and heart rate. The quantile plots in Fig. 16.4 show that the slopes for QTcF and QTcI are both significantly different from zero on a 0.05 α-level but QTcI appears to be the most appropriate QT correction methods.
Mean (90% confidence interval) predicted QTcF and QTcI versus RR relationship (solid line and shaded area) for male (blue) and female (red). The dots represent the observed median RR quantiles and associated mean (90% confidence interval) QT. RR quantile ranges for males (blue) and females (red) are shown along the x-axis
Furthermore, to ensure that it is not only a global trend shown between the different QT correction methods (QTc) and RR, the average sum of squared individual slopes are calculated and compared to the QTcI having the lowest average (see Table 16.2).
4.3 Adequacy of Sampling Times
The timing of ECG samples should be guided by the available information about the PK properties of the drug candidate and the QT effect should be characterized throughout the anticipated dosing interval (FDA 2005).
ECG and PK should be sampled frequently enough to ensure the peak drug concentration is captured and ECG recordings at time points around the maximum concentration time, tmax in case the peak effect on QT does not correspond to peak concentration. The sampling should be for at least 24 h post dose in case the cardiac repolarisation effect is delayed. The PK concentration–time profiles for therapeutic, supra-therapeutic doses and the positive control moxifloxacin are shown in Fig. 16.5 with a t max around 4 h for the test drug and around 2 h for moxifloxacin. The sampling is more frequent up until 5 h post dose to ensure the individual C max (maximum concentration) is captured. The time-matched ECGs are sampled just prior to the PK sample to ensure that the venipuncture does not affect the ECG sample.
4.4 Baseline Correction
Baseline corrections are necessary in TQT studies due to the large inter-individual variability. For a crossover study design, baseline measurements before each period are used with the diurnal variability in QTc accounted for by each subject receiving all 4 treatments at exactly the same time points. In Fig. 16.6, the mean QTcI and ΔQTcI (change from baseline) are illustrated showing a clear separation of moxifloxacin and supra-therapeutic dose from placebo and the therapeutic dose. The diurnal variation in all treatment arms is clearly visible with peaks around 4 and 18 h post dose and nadirs around 12 and 24 h post dose. This variability can be a result of many factors including activity level, postural changes, circadian patterns, and food intake. Finally, it is noticed that all treatment arms return to baseline 24 h post dosing where the exposure of the drug is negligible (see Fig. 16.6).
4.5 Assay Sensitivity
The purpose of including a positive control is to ensure confidence in the ability of the TQT study to detect changes in the mean QT prolongation of around 5 ms (FDA 2005). Moxifloxacin (a fluoroquinolone used for respiratory infections) is the most commonly used positive control in TQT studies because it reliably prolongs the QT interval with no significant effect on heart rate and is considered relatively benign.
Assay sensitivity is established if at least one time point excludes a 5 ms difference in the mean ΔΔQTc (baseline and placebo adjusted) with a one-sided 95% confidence interval thereby preserving at least 50% of the previously reported ΔΔQTc effect of 10–14 ms following 400 mg moxifloxacin (Bloomfield et al. 2008). The shape of the ΔΔQTcI-time profile is shown in Fig. 16.7 with peak effect excluding 5 ms around 2–4 h post dose and return to baseline at 24 h post dose as expected (Florian et al. 2011). Similarly, the slope of the moxifloxacin concentration–QTc relationship shown in Fig. 16.7 can be used to confirm assay sensitivity in cases with reduced moxifloxacin exposure, e.g., due to over-encapsulation (Florian et al. 2011).
(Top) Mean (90% confidence interval) ΔΔQTcI–time profile and (bottom) mean (90% confidence interval) moxifloxacin concentration–ΔΔQTcI observations (dots), and the estimated relationship (solid black line and shaded gray area) following 400 mg moxifloxacin with the moxifloxacin concentration quantile range is shown along the x-axis
4.6 Measure of Central Tendency
The FDA E14 guidance (FDA 2005) sets the threshold of regulatory concern for the drug candidate around 5 ms evidenced by an upper bound of the one-sided 95% confidence interval around the mean ΔΔQTc (time-matched difference in baseline and placebo adjusted QTc) excluding 10 ms. The TQT study is considered to be negative if the mean excludes 10 ms at all time points. In Fig. 16.8, the therapeutic treatment arm clearly excludes 10 ms at all time points whereas the upper 95% confidence interval includes 10 ms between 1.5 and 18 h post dose for the supra-therapeutic treatment arm.
4.7 Assessing Delay Between Drug and QT Effects
Before investigating the potential relationship between drug exposure and QT effect, it is important to assess whether there is a temporal delay between drug concentrations and ΔΔQTc. This could potentially indicate that an active metabolite is causing the QT prolongation, and it often requires more advanced modeling to account for the delay if the metabolite is not measured directly. Due to the inter-individual variability in PK and QT, the individual QTc versus drug concentration is expected to show very different slopes (positive and negative) and potentially also hysteresis (the effect on QT lags the change in concentration). Instead, the mean concentrations at each sampling time are plotted against the corresponding mean (90% confidence interval) ΔΔQTcI and connected in chronological order in Fig. 16.9. The slope for the therapeutic and supra-therapeutic treatment arms appear similar and there does not appear to be any clear sign of hysteresis except for the last 2 sampling times at 18 and 24 h post dose. A linear exposure-response model therefore seems adequate to assess the relationship between drug concentration and ΔΔQTcI.
4.8 Relationship Between Drug Exposure and QT Prolongation
An adequate TQT study should ensure that the dose- and exposure-response relationship for QT prolongation has been characterized at concentrations covering the worst case clinical exposure scenario in order to support regulatory review (Garnett et al. 2008).
It is important to understand the relationship between drug exposure and QT prolongation when (1) the primary E14 analysis is positive, (2) it is not possible to test doses high enough to cover the worst case clinical exposure scenario, or (3) when the TQT study is positive based on the E14 analysis but there is lack of dose- and exposure-response (Garnett et al. 2008, 2011).
The relationship between drug concentration and ΔΔQTcI is shown in Fig. 16.10 with a clear linear dependency, and the relationship appears similar for therapeutic and supra-therapeutic exposures.
ΔΔQTcI versus drug concentration. (Top) Observed data with population mean predictions (solid red line) and (bottom) observed concentration quantile–ΔΔQTcI plot with population mean and 90% confidence interval (solid black line with shaded gray area). The drug concentration quantiles following therapeutic (circles) and supra-therapeutic (squares) doses are shown as horizontal bars along the x-axis and the 10 ms threshold is shown as a dotted line
The individually estimated linear mixed-effects regression lines are furthermore shown in Fig. 16.11 (top) to assess whether the relationship between concentration and ΔΔQTcI is more or less pronounced compared to the population mean predictions. All subjects have a positive slope very similar to the estimated population slope while there is some variability in the intercept. The residuals are shown in Fig. 16.11 (bottom) to see whether there are outliers or subjects that are poorly fitted by the linear mixed-effects model.
4.9 Prediction of QT Prolongation at Different Exposure Levels
The ΔΔQTc predictions at the geometric mean peak concentration following therapeutic and supra-therapeutic doses are assessed and compared to the primary E14 analysis. Figure 16.11 (top) shows the mean (90% confidence interval) ΔΔQTcI of 0.00 (−2.50; 2.51) and 12.5 (9.49; 15.5) ms at geometric mean peak concentrations of 691 and 6,230 ng/mL, respectively. These predictions based on the concentration–ΔΔQTcI relationship are consistent with the primary E14 analysis mean (90% confidence interval) estimates of 4.39 (−0.86; 9.65) and 13.4 (9.62; 17.3) ms at 18 h and 3 h post therapeutic and supra-therapeutic doses, respectively.
4.10 Benefit-Risk Assessment
The concentration–QTc relationship is used to perform the benefit-risk assessment for drugs that prolong the QT interval. The first question to ask is whether the supra-therapeutic dose covers the highest expected clinical exposure scenario. This is done by adding the fold-change in C max and AUC for identified intrinsic and extrinsic factors (e.g., gender, race, organ impairment, drug–drug interactions, or food effects). This way the QT risk in subpopulations can be assessed and appropriate dose adjustments and ECG monitoring can be derived in order to write informative drug labels.
For the example shown in Fig. 16.12 (bottom), the geometric mean peak supra-therapeutic exposure shown in red is 9-fold higher than the therapeutic exposure shown in blue and clearly prolongs the mean QT interval by more than 10 ms. However, if the worst case clinical exposure scenario is between 2- and 4-fold, there does not appear a high risk of QT prolongation.
5 Concluding Remarks
The purpose of creating a QT knowledge management system was to automate QT data analyses and reporting for consistent and timely review of TQT studies. Furthermore, the developed graphics and reporting standards allow for easier communication (internally and externally) of results.
An important aspect of QT data analyses is to explore the adequacy of the model assumptions (e.g., heart rate QT correction, baseline adjustments, choice of positive control to establish assay sensitivity, linear or nonlinear concentration–QTc relationship, and direct or delayed effects) through model diagnostics and graphical analyses.
The system furthermore enables leveraging prior information to answer drug development related questions through pooled data analysis since the data and results are in a consistent format that easily can be combined. Contributions to improve the science include (1) the use of concentration–QT modeling for regulatory review of new drugs (Garnett et al. 2008) and (2) evaluating TQT study design features on moxifloxacin response (Florian et al. 2011).
References
Bloomfield D, Kost J, Ghosh K et al (2008) The effect of moxifloxacin on QTc and implications for the design of thorough QT studies. Clin Pharmacol Ther 84:475–480
Florian JA, Tornøe CW, Brundage R, Parekh A, Garnett CE (2011) Population pharmacokinetic and concentration–QTc models for moxifloxacin: pooled analysis of 20 thorough QT studies. J Clin Pharmacol 51(8):1152–1162
Food and Drug Administration (2005) Guidance for industry: E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs, U.S. Department of Health and Human Services, Food and Drug Administration. http://www.fda.gov/downloads/RegulatoryInformation/Guidances/ucm129357.pdf. Accessed 7 Aug 2011
Garnett CE, Beasley N, Bhattaram VA, Jadhav PR, Madabushi R, Stockbridge N, Tornøe CW, Wang Y, Zhu H, Gobburu JV (2008) Concentration–QT relationship play a key role in the evaluation of proarrhythmic risk during regulatory review. J Clin Pharmacol 48(1):13–18
Garnett CE, Lee JY, Gobburu JVS (2011) Contribution of modeling and simulation in the regulatory review and decision-making: U.S. FDA perspective in clinical trial simulations. AAPS Adv Pharmaceut Sci Ser 1:37–57
International Conference on Harmonisation (2005) Guidance on E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs; availability. Notice. Fed Regist 70:61134–61135
Tornoe CW, Garnett CE, Wang Y, Florian J, Li M, Gobburu JVS (2011) Creation of a knowledge management system for QT analyses. J Clin Pharmacol 51(7):1035–1042
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer Science+Business Media, New York
About this chapter
Cite this chapter
Tornøe, C.W. (2012). Visualization of QT Data for Thorough QT Study Analysis and Review. In: Krause, A., O'Connell, M. (eds) A Picture is Worth a Thousand Tables. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-5329-1_16
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5329-1_16
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-5328-4
Online ISBN: 978-1-4614-5329-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)