Abstract
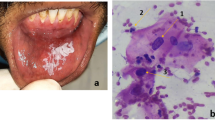
Squamous cell carcinomas of the oral cavity are among the ten most common cancers in the world, accounting for approximately 3–5 % of all malignancies. In Germany, approximately 4,100 new cases of oral cancer in males and 1,000 in females were encountered annually during the last decade. In spite of great surgical, chemo- and radiotherapeutic efforts the 5-year-survival-rate could not be decreased so far, being still less than 45 % in Europe. However oral cancer can be cured, if detected and treated early enough. One should, furthermore, emphasize the importance of an early diagnosis of oral cancers in order to reduce their disappointingly high morbidity and mortality. Until now, scalpel biopsy with histological assessment seemed to be the only accepted method to definitely evaluate suspicious oral lesions. However, literature shows insufficient inter- and intra-individual reproducibility of histological grading epithelial dysplasia and unequivocally identifying carcinoma in situ. Unfortunately, scalpel biopsies are not an ideal screening tool for the early identification of oral cancer because of their invasiveness; alternatively a useful diagnostic screening procedure could be easily obtained oral smears with subsequent cytological examination. Adjuvant methods e.g. image DNA cytometry or multimodal cell analysis may also help to increase the diagnostic accuracy and may lead to safe, quick and valid results of oral brush biopsies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Cytogenetic Backgrounds
All types of tumors, even benign ones, may show numerical and structural chromosomal aberrations, which are not present in healthy or reactive cells [1].
During progression of the tumor, early detectable and cancer specific primary aberrations are followed by secondary and tertiary chromosomal changes. Primary aberrations are the first cytogenetic structural or numeric changes, which are detectable by the conventional light microscope. Only one or a few chromosomes are hit specifically and mainly persistent during tumor progression. These changes are type specific for distinct malignancies like Philadelphia chromosomes in chronic myeloid leukemia. Solid tumors mostly present deletions of chromosomes, leukemia, however, is largely characterized by translocations. These early chromosomal changes are followed by secondary aberrations and affect specific chromosomes on a regular base; this leads to worsening the prognosis of the patient’s disease [2]. In contrast to the primary ones, secondary aberrations are detectable by quantification of the net effect of the cellular DNA content using image DNA cytometry [3]. Tertiary chromosomal aberrations are the result of genetic instability and may affect chromosomes at random.
In principle, the analysis of chromosomes is capable of qualifying cells to be malignant, independently by histological or cytological examination [2, 4]. Even earlier stages of malignancy without clinical symptoms and the malignant potential may be determined by chromosomal analysis. But these complex cytogenetic techniques are not available for all types of tissues due to the lack of sufficient cell culture capability to transfer the cells into the M-phase. Additionally they are elaborate and time consuming.
Feulgen Staining
The DNA content cannot be measured directly by cytometry. After quantitative DNA staining, the nuclear Integrated Optical Density (IOD) is the cytometric equivalent of its DNA content. Subsequently all specimens must be destained and additionally Feulgen stained in a temperature-controlled staining machine with Schiff’s reagent [5].
The Feulgen staining procedure is a well-established and frequently documented procedure for quantitative DNA staining [5]. The principle of this staining process is based on two steps: In the first step the double stranded DNA must be split off the purine bases, therefore it must be hydrolyzed by a strong acid, like 5 M HCl for 55 min. This results in an apurinic acid that shows aldehyde groups at the former positions of the purine base on the DNA strand. The destaining of prestained slides after Papanicolaou staining is made in this step as well.
Secondly, the Schiff base, like basic parafuchsin, binds stoichiometrically to the aldehyde groups of the DNA and this results in a reddish colored nucleus with an absorption maximum of 570 nm.
Studies have shown that the staining intensity depends strictly on the temperature of the DNA hydrolysis in 5 M HCl of the DNA; the optimum hydrolysis temperature is 27°C and even changes of 0.5°C affect the measurement of the IOD significantly [5–7]. For application in routine diagnostic procedures, the staining should be standardized to assure reliable and reproducible results.
The DNA cytometry is a quantitative measurement and thus all cells on the glass slide must be stained in a similar way; reference cells on the identical slide have to be taken as an internal standard. Differences of the staining intensity occurring within the same slide may lead to incorrect calibration and thus to false ploidy values. Therefore the application of an automated staining machine is strictly recommended. For example the commercially available Shandon Varistain 24 staining machine can be run automatically and (flow-through) cuvettes are 24 h temperature controlled, if necessary [5]. The storage must be in the dark to avoid fading effects of the slides. The Feulgen stained slides can be re-stained to PAP easily for conventional re-evaluation.
Preparation of Specimens
The slides of alcohol-fixed, Papanicolaou-stained, routine smears from mucosal brushings should be evaluated according to the published guidelines for extra genital cytology [8]. This is necessary to define normal, doubtful, suspicious or unequivocal tumor cells on the slide. The precondition for a proper DNA analysis is the marking/circling of these cells with a felt pen on the glass slide prior to Feulgen staining. This procedure is followed by photocopying the slides to assure the remarking after removal of the cover slip. Afterwards cover slips should be removed carefully after xylol treatment. The time depends on the time of archiving the specimens. Never use force for removal, you may dislodge cells from the slide. After staining the areas of interests must be re-marked on the slides using the photocopies.
After rehydration in decreasing ethanol concentrations and refixation in buffered 10% formalin, 5 N HCL for acid hydrolysis was applied at 27°C for 55 min, followed by staining in Schiff´s reagent (Merck, Darmstadt, Germany) for another hour, followed by rinsing in SO2-water to remove surplus dye from cell nuclei and cytoplasm. Dehydration at increasing ethanol concentrations is followed [9]. The slides must then be covered with Entellan (Merck, Darmstadt, Germany) and stored in the dark.
DNA-Image Cytometry/DNA-Measurements
The aim of diagnostic DNA cytometry is to identify DNA stem lines outside the euploid regions as abnormal (or aneuploid) at a defined statistic level of significance. The numerical and/or structural chromosomal aberrations are the biological basis for DNA-Image cytometry. The quantitation of nuclear DNA requires a rescaling of the measured Integrated Optical Density (IOD) values by comparison with those from cells with known DNA content. Therefore the DNA content is expressed in a “c” scale in which 1c is half the mean nuclear DNA content of cells from a normal (non-pathological) diploid population in G0/G1 cell cycle phase. A DNA-stem line was defined as a frequency peak in a histogram accompanied by values at its twofold DNA-content. It was defined interactively when the DNA-histograms were displayed on the screen by marking its minimum and maximum [9–11] (Fig. 8.1).
Top left: 2. DNA-histogram of a smear from a histologically proven hyperkeratosis without dysplasia, showing number of cells measured (n) and their corresponding DNA-content (c) and a (normal) diploid stem line at 2.0c. Top right: DNA-histogram of a smear from a Lichen planus (erosive), showing (euploid) polyploid stem lines at 2.0c and 4.0c. Bottom left: DNA-histogram of a smear from a squamous cell carcinoma of the tongue. An abnormal stem line at 1.7c and 3.5 can be detected as an aspect of DNA-aneuploidy. Bottom right: DNA-histogram of a smear from a squamous cell carcinoma of the alveolar ridge. Abnormal stem lines are shown, additionally, four cells with a DNA-content greater than 9c (9cEE) can be detected as another aspect of DNA-aneuploidy
The photometric analysis of the integrated optical density was performed by the QUIC-DNA system (TriPath, Burlington, NC, USA) in combination with a conventional light microscope Axioplan 2 (Zeiss, Jena, Germany) with the objectives 40/0,75; 20/0,40; 10/0,25 and 4/0,10. To reduce stray light, the Köhler measurement was performed and an interference filter 570 nm ± 10 nm was used. The TriPath system was interfaced with a 486 IBM-compatible personal computer with a frame grabber card (Matrox electronics, Munich, Germany) using a TV camera with 572 lines (VarioVam CCIR, PCO Computer Optics, Kehlheim, Germany) with a magnification of factor 1.6. Segmentation was performed automatically on individual nuclei by gray level thresholding, taking the local background into consideration for each nucleus. The glare- and diffraction errors were corrected by software as proposed by Kindermann and Hilgers [12]. The data were interpreted using the analysis software of the system.
The normal 2c reference value was established by measuring 30 cytologically normal epithelial cells or lymphocytes on each slide as an internal reference (mean values of integrated optical densities (IOD)). CVs (=coefficient of variation) of reference cells must be below 5%. No correction factor was applied. If present, three hundred atypical epithelial or carcinoma cells per specimen were measured interactively at random. The performance of the system meets the standards of the European Society for Analytical Cellular Pathology (ESACP) task force on standardization of diagnostic DNA-image cytometry [9–11, 13].
Aspects of DNA-aneuploidy according to the Consensus reports of the European Society for Analytical and Cellular Pathology (1995, 1998, 2001) are as follows:
-
1.
In comparison to the normal proliferating cell population (G0/G1-phase-fraction) to the analyzing cell population show an abnormal stem line with the most frequent value, i.e. the mean value of the histogram class containing the highest number of nuclei, which differs at least at 10% from those of normal (resting, proliferating, or polyploidizing) cell populations. The DNA index of the stem line must be <0.90>1.10 or <1.80>2/20 or <3.60>4.40.
-
2.
Abnormal cells with a DNA content higher than 9c are present. Often called 9c exceeding events, are those cells having nuclear DNA content higher than the duplication or quadruplication region of a normal G0/G1 phase population, i.e. not belonging to G2/M phase fractions (cells >9c occurred (9c exceeding events [9cEE])) [14].
The quantity of nuclear DNA may be changed by the following mechanisms: replication, polyploidization, gain or deletion. Each affects the size or the number of chromatids. Furthermore viral infections may change the nuclear DNA content detectable by image cytometry. Among others, the unspecific effects of cytostatic or radiation therapy, vitamin B12 deficiency, apoptosis, autolysis and necrosis on nuclear DNA content play also a role [1, 15–19].
Clinical Impact of DNA-Image Cytometry for Oral Cancer Diagnosis
Primary Oral Squamous Cell Carcinomas
Our study group [20] has shown that specimens from healthy mucosa did not show any signs of aneuploidy according to the current Consensus reports of the ESACP. In a preliminary study, we have investigated 100 brush biopsies of benign, reactive or inflamed oral lesions and the modal value of the DNA stem line was nearly 2c (MV 2.01c; SD ±0.06). The correlation coefficient was 3.85%; 44 cases showed cells with cells >5c (Table 8.1). In a second step we investigated 100 brush biopsies from clinically unequivocal and histologically proven OSCCs: All hundred cases of cancer fulfilled the criteria for DNA aneuploidy. Thus all the cancer specimens showed one, two or both criteria of aneuploidy. Table 8.2 shows the incidence of the different criteria of aneuploidy. The presence of abnormal stemlines is seen in 9% of all aneuploid cases; 9c exceeding events (9cEE) were seen in 32% in aneuploid specimens. The occurrence of both, 9cEE and abnormal stemlines were seen in 59% of all cases.
The results of these pilot studies suggested strongly that aneuploidy detection may be a useful marker for discrimination of clinically doubtful lesions and may help to clarify their biological nature.
Additionally, we investigated 543 cases of brush biopsies from different doubtful lesions of the oral cavity in daily routine practice. In 53 cases, the DNA measurement was not possible due to technical limitations: (a) insufficient numbers of cells for proper analysis and (b) massive overlapping of cells and or nucleoli.
If present, 300 atypical epithelial or carcinoma cells per specimen were measured interactively, at random. Otherwise, only the available cells were measured: one (suspicious) case with 48 cells (=insufficient for DNA-cytometry); two cases with 51–100 measurable cells; four cases with 101–150 cells; six cases with 151–200 cells; seven cases with 201–250 cells; seven cases with 251–300 cells and all other cases with more than 300 cells. No stem line interpretation of DNA-aneuploidy was performed if less than 50 abnormal or atypical cells were contained. All inconspicuous cases (“tumor cell negative”) were measured using at least 30 reference cells and 300 analysis cells.
Overall, 304 cases showed no criteria of DNA aneuploidy. However 184 cases showed DNA aneuploidy, three cancer cases showed none of the criteria and were evaluated as non-aneuploid. The combination of abnormal stem line and cells >9cEE was the major criteria of aneuploidy (60%), followed by 9cEE alone (29%) and abnormal stem lines with 11%. These data were in accordance with the pilot study mentioned above. The diagnostic accuracy is summarized as follows: The sensitivity was 98.4%, the specificity was 99.34%. The positive predictive value was 98.92% and the negative predictive value 99.01%. (For details see Table 8.3).
Lip Cancer
We investigated 27 cases of suspicious lesions of the lip, of which, 25 cases were technically sufficient for DNA analysis. All benign cases from lesions of the lip showed euploidy. In 16 cases of proven cancer, 11 cases fulfilled the aspects of aneuploidy, five patients showed normal euploid stem line. But the conventional cytological revaluation showed no evidence of cancer cells on these slides. Nevertheless the sensitivity of DNA-aneuploidy was 67% only; the specificity was 100%. The main criterion for aneuploidy was the presence of abnormal stem lines in 10% of all cases. Abnormal stem lines including 9c exceeding events were seen in 45% of the cases, followed by 9cEEs as a single marker in 45% of all measured cases (Table 8.4). Major limitations in these cases were the small number of cells, harvested with the nylon based cell collector. Even the maceration of the lips with physiologic salt solution prior to sampling did not increase the number of harvested cells significantly [20].
Reliability
To investigate the reliability of image DNA-cytometry, we calculated the intra-observer reliability; it is the variation in measurements taken by a single person on the same item and under the same conditions. In a second step, we determined the inter-observer reliability; this means the variation in measurements when taken by different persons but with the same method or instruments.
Therefore, we chose 137 specimens of oral brush biopsies out of 1,000 archived cases at random. The diagnoses were: 65 (47.45%) oral squamous cell carcinomas, thereof 55 (84.62%) primary carcinomas, 3 (4.62%) cases of recurrent cancer, 2 (3.08%) cases of secondary tumor and 5 (7.68%) cases of lip cancer. Out of 137 cases, 72 (52.55%) specimens came from clinically proven benign lesions.
All slides were independently analyzed by two observers to evaluate interobserver reliability of diagnosis of 137 cases; 2 month later identical specimens were re-evaluated by the same two observers to assess intraobserver reliability. The STATA program and Cohen’s Kappa statistics were used to assess reliability. The calculation showed an (almost) perfect inter- and intraobserver (k = 0.99) reliability according to Landis and Koch.
Laser Scanning Cytometry
The Laser scanning cytometry is a static cytometric DNA analysis that allows the measurement of fluorescent parameters of cells. It is a further development of the conventional flow cytometry, whereas the method combines the advantages of flow and static image cytometry. The detected cell features are enlarged on the screen and multiple screen shots are taken for documentation purposes [21–25].
We have adapted Gerstner’s assays [26, 27] for the fluorescent staining of different cytokeratins of oral keratinocytes with antibodies (Dako Cytomation, Hamburg, Germany) [20]. The clone MNF 116 for the cytokeratins 5, 6, 8, 17 and 19 was used. Due to the fact that not all squamous cells from carcinomas were stained; it seems likely that during carcinogenesis, epitopes were lost on the surface of the respective cells [27]. Therefore, we broadened the spectrum by using Clone beta E12, AE and AE3 (Dako Cytomation, Hamburg, Germany) to detect cytokeratin 1, 2, 3, 4, 5, 6, 8, 10, 14, 15, 16 and 19. The antibody was linked to streptavidin conjugated allophycocyanine (ACP). For details see Table 8.5.
The analysis was done by interpretation of the position of the stem line and the occurrence of 5cEE and 9cEE additionally [28].
We had evaluated 44 patients, including 22 oral squamous cell carcinomas. The sensitivity was 95.5%, the specificity 81.8%; the negative and positive predictive values were 84.0% and 94.7% respectively (Figs. 8.2–8.4). Gerstner and co-worker investigated 49 laryngeal lesions using cotton swabs and determined aneuploidy by stem line interpretation with the same laboratory setup: They achieved a sensitivity of 83% and a specificity of 93%, the negative predictive value was 67, the positive predictive value was around 88% [28].
Left: Dot plots of measured cell features. DNA-content (x-axis, linear) is plotted vs. APC-fluorescence per area (y-axis, logarithmic) (5% cut-off is set in the control sample–not shown). Three populations were definable: regions 1 and 3 (cytokeratin positive) and 2 (no cytokeratin ≈ lymphocytes ≈ internal reference). Right: The cells of region 1 showed a stem line with a DNA Index (DI) 1,0 and in region 2 showed a stem line with a DNA Index of 2
A brush biopsy from a tongue carcinoma (pT3pN1cM0) was prepared according to the protocol (total cell count of the positive sample: 8,327). The set-up of the figure and acquisition of micrographs is equivalent to Fig. 8.1. The marked changes from normal cytokeratin-positive epithelium (DI = 1.09) to aneuploid carcinoma (DI = 1.64 and 3.27) are clearly visible. There are also cells with polyploid DNA content (DI > 5.0)
Interpretation of LSC data: Brush biopsy (benign) was analyzed by LSC: pseudocolored images were taken by rescanning single cells (upper lines). Then, slides were stained with PAP, identical cells were relocalized, and images were taken (lower lines). Analysis and imaging were performed with the ×20 objective. (Note: Because of different optical pathways, corresponding images are symmetrical to their center)
Comparison of DNA-Image Cytometry Versus Laser Scanning Cytometry
All samples described in the previous chapter were re-stained and investigated by LSC and ICM as well. Out of 44 samples, one sample was technically insufficient for image cytometry due to significant cell loss by rigid removal of the cover slip. All 21 histograms of histologically proven cancer show aneuploidy and but none of the benign lesions: the combination of abnormal stem line and cells >9c were shown in 48% of all cases, abnormal stem lines in 42% and 9cEE in 10%. Thus the sensitivity and specificity were 100%.
The regression analysis (Pearson product–moment correlation coefficient) revealed 0.87 in comparison of both techniques. The major problem for the validity of the LSC was the stringent re-localisation after re-staining according to PAP to verify 9cEEs to reduce false negative results. This procedure extended the evaluation time up to 2–3 h per case [20].
Multi-modal Cell Analysis
The aim of this clinical study was to apply a novel approach to improve diagnostic accuracy by sequential analysis of cellular characteristics in the same smear using Multimodal Cell Analysis (MMCA) [29, 30]. We applied the MMCA process to smears from oral brush biopsies, combining conventional cytology with the more quantifiable DNA content, followed by Argyrophilic Nucleolar Organizing Regions (AgNOR) count, to identify early malignant transformation [31]. Recent studies have shown that the number and/or size of AgNORs correlate with the ribosomal gene activity and therefore with cellular proliferation and consequent malignant potential [32–36].
DNA-Measurements
The performance of our system, that is based on a Leica DMLA automated microscope, meets the standards of the European Society for Analytical Cellular Pathology (ESACP) task force on standardization of diagnostic DNA-Image cytometry [9, 10, 37].
Details of software algorithms for precise scene matching, re-localization and registration have been described in detail elsewhere [29, 38, 39].
AgNOR-Analysis
Nucleolar Organising Regions (NORs) represent loops of DNA actively transcribing via ribosomal RNA to proteins. These NORs are associated with acidic, argyrophilic, non-histone proteins that are visualized using a silver staining technique. Recent studies show that the number and/or the size of the AgNORs correlate positively with the ribosomal gene activity and therefore with cellular proliferation [33, 40–44].
Silver staining was performed according to the one step method by Ploton et al. [35] and Crocker et al. [45] with modifications [46]. Manual AgNOR counting was performed on 100 normal cells and abnormal squamous cells for each cytological smear. The mean number of AgNORs per nucleus as clusters, satellites, clusters and satellites together were considered.
All information gathered from different stains and evaluated by different methods of analysis contribute to the identification and characterization of cancerous or even precancerous cells.
In our oral cancer study the MMCA [31] process was operated as a stepwise process, as described previously. First, the operator selects representative regions on the stained slides containing atypical or abnormal cells. Images are immediately digitized and stored together with their coordinates. The slides are then de-stained and re-stained by the Feulgen method. The newly stained and covered slides are then placed back onto the microscope stage where the previously recorded coordinates stored in the database automatically reposition the slide to the regions of interest digitized before. Finally all cases received a third stain with silver nitrate to demonstrate AgNOR-dots. As before, a digital registration was performed on the digitized regions of interest. The results were appended to the feature set of the individual cells.
All 25 cytologically tumor negative specimens were DNA-non-euploid. 4/20 squamous cell carcinomas revealed an atypical DNA-stem line alone, 5/20 abnormal cells >9c alone and 9/20 both aspects of DNA-aneuploidy.
Sensitivity of DNA-aneuploidy on oral smears for the detection of cancer cells thus was 95%, specificity for the detection of benign lesions 100%, positive predictive value 100% and negative predictive value 96.4%.
AgNOR-analysis reached a sensitivity of 100% for the diagnosis of malignant cells, specificity of 100% for benign cells, whereas the cut-off level was determined by 5.09 AgNORs per nucleus, as described previously [46]. The negative predictive value reached 100% and the positive predictive value 100%.
The sequential application of different methods (e.g. DNA-cytometry, AgNOR-analysis) increased the sensitivity and specificity of our cytological diagnosis from 90% to 100%. Due to the hierarchical or cascaded approach of MMCA, a measurement of uncertain specimens is terminated at a certain stage, when a definitive cancer diagnosis is confirmed through additional information e.g. the presence of DNA-aneuploidy [31].
Conclusion
The prevalence of DNA aneuploidy is very high in oral cell carcinoma, on the contrary, in benign lesions it is nearly zero. Thus, as an independent marker, aneuploidy serves as a valid and reliable indicator for the identification of neoplasms of the oral cavity. The additional evaluation of conventional cytological specimens from brush biopsies by image cytometry improved the diagnostic accuracy of pathologist’s daily routine. DNA-Image cytometry is well established and current studies support our results for specimens of oral brush biopsies [47–50].
References
Sandberg A. The chromosomes in human cancer and leukemia. Amsterdam, New York: Oxford Elsevier; 1990.
Heim S, Mitelman F. Cancer cytogenetics. New York: Alan R Liss, Inc; 1987. p. 239–40.
Böcking A, Wied GL, Keebler CM, et al. DNA measurements. When and Why? Compendium on quality assurance, proficiency testing, and workload limitations. Chicago, IL; 1995. p. 170–88.
Hansteen IL, Hilt B, Lien JT, Skaug V, Haugen A. Karyotypic changes in the preclinical and subsequent stages of malignant mesothelioma: a case report. Cancer Genet Cytogenet. 1993;70(2):94–8.
Chatelain R, Willms A, Biesterfeld S, Auffermann W, Böcking A. Automated Feulgen staining with a temperature-controlled staining machine. Anal Quant Cytol Histol. 1989;11(3):211–7.
Böcking A, Striepecke E, Auer H, et al. Static DNA-cytometry. Biological background, technique and diagnostic interpretation. Tutorials of Cytology. Chicago, IL; 1994. p. 107–128.
Nguyen VQ, Grote HJ, Pomjanski N, Knops K, Böcking A. Interobserver reproducibility of DNA-image-cytometry in ASCUS or higher cervical cytology. Cell Oncol. 2004;26(3):143–50.
Böcking A, Freudenberg N. Standardisierte Befunderstellung in der extragenitalen Zytologie. Pathologe. 1998;19:235–6.
Haroske G, Baak JP, Danielsen H, et al. Fourth updated ESACP consensus report on diagnostic DNA image cytometry. Anal Cell Pathol. 2001;23(2):89–95.
Böcking A, Giroud F, Reith A. Consensus report of the ESACP task force on standardization of diagnostic DNA image cytometry. European Society for Analytical Cellular Pathology. AnalCell Pathol. 1995;8(1):67–74.
Giroud F, Haroske G, Reith A, Böcking A. 1997 ESACP consensus report on diagnostic DNA image cytometry. Part II: specific recommendations for quality assurance. European Society for Analytical Cellular Pathology. Anal Cell Pathol. 1998;17(4):201–8.
Kindermann D, Hilgers CH. Glare-correction in DNA image cytometry. Anal Cell Pathol. 1994;6(2):165–80.
Haroske G, Meyer W, Oberholzer M, Böcking A, Kunze KD. Competence on demand in DNA image cytometry. Pathol Res Pract. 2000;196(5):285–91.
Chatelain R, Schunck T, Schindler EM, Schindler AE, Böcking A. Diagnosis of prospective malignancy in koilocytic dysplasias of the cervix with DNA cytometry. J Reprod Med. 1989;34(8):505–10.
Biesterfeld S, Fuzesi L, Härle F, Böcking A. DNA-cytometric detection of euploid polyploidization in oral lichen ruber planus. Anal Quant Cytol Histol. 1991;13(1):7–10.
Biesterfeld S, Gerres K, Fischer-Wein G, Böcking A. Polyploidy in non-neoplastic tissues. J Clin Pathol. 1994;47(1):38–42.
Böhm N, Sprenger E, Schluter G, Sandritter W. Proportionalitätsfehler bei der Feulgen-Hydrolyse. Histochemie. 1968;15:194–203.
Stenkvist B, Strande G. Entropy as an algorithm for the statistical description of DNA cytometric data obtained by image analysis microscopy. Anal Cell Pathol. 1990;2(3):159–65.
Stenkvist B, Olding-Stenkvist E. Cytological and DNA characteristics of hyperplasia/inflammation and cancer of the prostate. Eur J Cancer. 1990;26(3):261–7.
Remmerbach: Evaluation der zytologischen Diagnostik und adjuvanter Methoden an Präparaten oraler Bürstenbiopsien zur Sekundärprävention von Lippen- und Oropharynxkarzinomen. Leipzig: Univ., Habil.-Schrift; 2006.
Kamentsky LA, Kamentsky LD. Microscope-based multiparameter laser scanning cytometer yielding data comparable to flow cytometry data. Cytometry. 1991;12(5):381–7.
Kamentsky LA, Gershman RJ, Kamentsky LD, Pomeroy BM, Weissman ML. CompuCyte Corporation. Pathfinder System: computerizing the microscope to improve cytology quality assurance. Acta Cytol. 1996;40(1):31–6.
Kamentsky LA, Burger DE, Gershman RJ, Kamentsky LD, Luther E. Slide-based laser scanning cytometry. Acta Cytol. 1997;41(1):123–43.
Kamentsky LA, Kamentsky LD, Fletcher JA, Kurose A, Sasaki K. Methods for automatic multiparameter analysis of fluorescence in situ hybridized specimens with a laser scanning cytometer. Cytometry. 1997;27(2):117–25.
Kamentsky LA. Laser scanning cytometry. Methods Cell Biol. 2001;63:51–87.
Tarnok A, Gerstner AO. Clinical applications of laser scanning cytometry. Cytometry. 2002;50(3):133–43.
Gerstner AO, Machlitt J, Welkoborsky HJ, Bootz F, Tarnok A. Analysis of ploidy in hypopharyngeal cancer by laser scanning cytometry on fine needle aspirate biopsies. Anal Cell Pathol. 2003;25(2):51–62.
Gerstner AO, Thiele A, Tarnok A, et al. Preoperative detection of laryngeal cancer in mucosal swabs by slide-based cytometry. Eur J Cancer. 2005;41(3):445–52.
Würflinger T, Stockhausen J, Meyer-Ebrecht D, Böcking A. Robust automatic coregistration, segmentation, and classification of cell nuclei in multimodal cytopathological microscopic images. Comput Med Imaging Graph. 2004;28(1–2):87–98.
Böcking A, Stockhausen J, Meyer-Ebrecht D. Towards a single cell cancer diagnosis. Multimodal and monocellular measurements of markers and morphology (5 M). Cell Oncol. 2006;26(1–2):73–9.
Remmerbach TW, Meyer-Ebrecht D, Aach T, et al. Toward a multimodal cell analysis of brush biopsies for the early detection of oral cancer. Cancer Cytopathol. 2009;117(3):228–35.
Rüschoff J, Plate K, Bittinger A, Thomas C. Nucleolar organizer regions (NORs). Basic concepts and practical application in tumor pathology. Pathol Res Pract. 1989;185(6):878–85.
Rüschoff J, Bittinger A, Neumann K, Schmitz-Moormann P. Prognostic significance of nucleolar organizing regions (NORs) in carcinomas of the sigmoid colon and rectum. Pathol Res Pract. 1990;186(1):85–91.
Rüschoff J. Nucleolus organizer regions in pathomorphologic tumor diagnosis. Veroff Pathol. 1992;139:1–144.
Aubele M, Biesterfeld S, Derenzini M, et al. Guidelines of AgNOR quantitation. Committee on AgNOR quantitation within the European Society of Pathology 1. Zentralbl Pathol. 1994;140(1):107–8.
Tuccari G, Giuffre G, Ofner D, Rüschoff J. Standardized use of the AgNOR method. J Oral Pathol Med. 2000;29(10):526–7.
Haroske G, Giroud F, Reith A, Böcking A. 1997 ESACP consensus report on diagnostic DNA image cytometry. Part I: basic considerations and recommendations for preparation, measurement and interpretation. European Society for Analytical Cellular Pathology. Anal Cell Pathol. 1998;17(4):189–200.
Würflinger T, Stockhausen J, Meyer-Ebrecht D, Böcking A. Automatic coregistration, segmentation and classification for multimodal cytopathology. Stud Health Technol Inform. 2003;95:218–23.
Bell A, Aach T, Ropers SO, Bocking A, Meyer-Ebrecht D, Wülflinger T. Towards fully automatic acquisition of multimodal cytopathological microscopy images with autofocus and scene managing. Methods Inf Med. 2007;46(3):314–23.
Rüschoff J. Nucleolus organizer regions in pathomorphologic tumor diagnosis. Veroff Pathol. 1992;139:1–144.
Crocker J, Boldy DA, Egan MJ. How should we count AgNORS? Proposals for a standardized approach. J Pathol. 1989;158(3):185–8.
Ploton D. Structure and molecular organization of the nucleolus. Zentralbl Pathol. 1994;140(1):3–6.
Ploton D, Bendayan M, Adnet JJ. Ultrastructural localization of Ag-NOR proteins and nucleic acids in reticulated nucleoli. Biol Cell. 1983;49(1):29–34.
Ploton D, Menager M, Jeannesson P, Himber G, Pigeon F, Adnet JJ. Improvement in the staining and in the visualization of the argyrophilic proteins of the nucleolar organizer region at the optical level. Histochem J. 1986;18(1):5–14.
Crocker J. Nucleolar organiser regions. Curr Top Pathol. 1990;82:91–149.
Remmerbach TW, Weidenbach H, Müller C, et al. Diagnostic value of nucleolar organizer regions (AgNORs) in brush biopsies of suspicious lesions of the oral cavity. Anal Cell Pathol. 2003;25(3):139–46.
Remmerbach TW, Hemprich A, Böcking A. Minimally invasive brush-biopsy: innovative method for early diagnosis of oral squamous cell carcinoma. Schweiz Monatsschr Zahnmed. 2007;117(9):926–40.
Maraki D, Becker J, Böcking A. Cytologic and DNA-cytometric very early diagnosis of oral cancer. J Oral Pathol Med. 2004;33(7):398–404.
Böcking A, Sproll C, Stocklein N, et al. Role of brush biopsy and DNA cytometry for prevention, diagnosis, therapy, and followup care of oral cancer. J Oncol. 2011;2011:875959.
Handschel J, Oz D, Pomjanski N, et al. Additional use of DNA-image cytometry improves the assessment of resection margins. J Oral Pathol Med. 2007;36(8):472–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Remmerbach, T.W. (2013). The Role of Ploidy Analysis in Oral Cytology. In: Mehrotra, R. (eds) Oral Cytology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5221-8_8
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5221-8_8
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-5220-1
Online ISBN: 978-1-4614-5221-8
eBook Packages: MedicineMedicine (R0)