Abstract
Bariatric surgeons frequently encounter incisional or ventral hernias, and the management of these conditions remains controversial. This chapter will focus on available options to approach ventral hernias discovered preoperatively or incidentally at the time of bariatric surgery. New developments and experience with synthetic mesh may change the optimal approach to incisional hernias for these patients. Nonetheless, there is currently not enough definitive evidence to offer an unequivocal algorithm for the management of ventral hernia in bariatric surgical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bariatric surgery and hernia
- Hernia repair in the bariatric patient
- Ventral hernia in the bariatric patient
- Morbidly obese patients and hernia repair
The overall incidence and complexity of ventral and incisional hernias have increased. Patients live longer, accumulating comorbidities, and undergo more surgeries. Moreover, obesity is now a worldwide epidemic. Wound infections and incisional hernia formation more frequently complicate laparotomies on obese patients with a large abdominal girth. The management of hernias continues to evolve as we learn more about genetic predisposition and the pathophysiology of the disease. There are now multiple options for hernia repair. What historically began as the primary repair of simple ventral hernias has evolved to mesh repair of larger hernias and now encompasses complex procedures such as multiple layers of component separation complemented with synthetic and biologic mesh. With increasing numbers of bariatric procedures performed, hernias in these patients have now emerged as an important topic that needs to be addressed both preoperatively and postoperatively.
Morbidly obese patients are at an increased risk for primary as well as incisional hernias. Studies have shown that obese patients have increased intra-abdominal pressures (IAP) when compared to normal weight control patients [1, 2]. When comparing obese patients (mean BMI 55 ± 2 kg/m2) to controls, the mean IAP for the morbidly obese group was 12 ± 0.8 cm H2O, significantly increased when compared to controls with IAP = 0 ± 2 cm H2O. Obese patients consistently had elevated intra-abdominal pressures when compared to normal-weighed controls during the activities of daily living such as walking, climbing stairs, coughing, and lifting. Increased IAP puts added stress on the abdominal wall and tensile strength of the mesh. Obese patients are also more likely to be afflicted with weight-related comorbidities, which also predispose the development of hernias. A study looking at 62 patients with a mean BMI of 49 revealed that systemic hypertension, the American Society of Anesthesiologists (ASA) physical status score, and body mass index (BMI) were predictors of elevated IAP [3]. Risk factors for developing abdominal wall hernias include smoking, advanced age, wound infection, multiple surgeries, and chronic medical conditions such as chronic obstructive pulmonary disease, diabetes, and immunosuppression. Given these findings, it is not surprising that potential bariatric patients are more predisposed to primary ventral hernias as well as developing postoperative hernias. Open bariatric surgery is associated with an incidence of incisional hernias of ∼20% [4–6]. With laparoscopy now more customary, the number of large incisional hernias has decreased, but port-site hernias can still occur. The specific incidence of port hernias in the bariatric surgery population is not known, but in general, these hernias typically occur within 3–4 years after surgery at rates of 0.8–2.8% [7, 8].
The recurrence rates of incisional hernias have also been shown to be higher in the obese population. Many studies have shown a statistically significant higher incidence of incisional hernia in patients with BMI > 35 [9–12]. However, a retrospective study of 168 patients, specifically comparing morbidly obese to normal body weight patients, showed no difference in the complication or recurrence rates at 19-month follow-up after laparoscopic hernia repair [13]. Regardless, the morbidly obese patients tend to have larger fascial defects, and recurrence may occur up to 10 years postoperatively [14]. Thus, the timing of most durable ventral hernia repair may well be after significant weight loss which is usually accompanied by at least a partial resolution of medical comorbidities.
Management
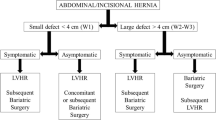
The management of concomitant ventral hernia at the time of primary bariatric surgery remains controversial. Datta et al. have shown that the incidence of ventral hernia at the time of gastric bypass was quite common. Of the 325 patients operated in their series, 26 had a ventral hernia, an incidence of 8% [15]. This rate is even higher when combined with those patients who also have known and symptomatic incisional or ventral hernias. The ultimate goal is to perform the primary bariatric surgery safely and avoid postoperative complications. However, there may be an increased risk of complications if these hernias are not addressed at the time of primary bariatric surgery.
Currently, there is no consensus regarding the best option for bariatric surgery patients with ventral hernias. There are essentially three surgical options when an unsuspected hernia is encountered during the performance of a gastric bypass, which is defined as a clean-contaminated case. The most straightforward option is to simply note the presence of the hernia in the operative report and “leave it alone.” This approach offers certain advantages including expediting the operative time and avoiding hernia repair complications. The downside is painful incarceration and/or bowel obstructions that are the well-documented possible sequelae of untreated hernias, and immediate postoperative gastric bypass patients have even greater risks. Incarceration and potential proximal bowel obstruction can stress fresh anastomoses, and disruption can cause leaks. Given that these patients are already considerably medically compromised due to their morbid obesity, this can be a potentially life-threatening complication.
Another option is primary closure, especially in smaller (<3–4 cm) hernias, a strategy which sidesteps the potential of mesh placement in a clean-contaminated field. This approach may not be appropriate as an oft-cited study suggests that more than one-third of patients who had deferred treatment of their hernias during laparoscopic Roux-en-Y gastric bypass experienced subsequent development of small bowel obstruction. 85 patients who had ventral hernias at the time of gastric bypass had either no treatment, primary repair, or repair with small intestinal submucosa (SIS). There was a 22% recurrence in the primary repair group, and 36% developed bowel obstruction due to incarceration in no treatment group [16].
Another smaller study examined 27 preoperative bariatric patients with complex recurrent ventral hernias. Seven patients underwent ventral hernia repair simultaneously (primary and biologic mesh), and all others were deferred. All seven of the repaired hernias recurred, and one patient in the deferred group needed an urgent operation for incarceration [17]. Clearly, there is a relatively high risk of complications if complex hernias are not treated at the time of gastric bypass.
For simple small defects that measure <3–4 cm and already have viable omentum in the hernia sac and are out of the operative field, the risk of incarceration still appears minimal, and these may be left in situ. The omentum in the sac may actually act like a “plug” and prevent bowel incarceration and obstruction. Then there are small hernias that are symptomatic or do not contain anything within the hernia sac. While all symptomatic hernias must be addressed at the time of bariatric surgery since clinical symptoms are likely secondary to intermittent bowel incarceration and obstruction, these small-necked hernias may be more likely to cause incarceration (or a partial Richter’s type hernia). Postoperative ileus and bowel distension is common after bariatric surgery, which may increase the risk of incarceration. Small defects <3–4 cm may be closed primarily with a suture passer at the time of bariatric surgery. Although, as mentioned, the recurrence may be as high as 25%, this may bridge the patients during the early, crucial postoperative period [16].
For larger symptomatic hernias and complex hernias, studies have shown that the rate of hernia recurrence is largely based on initial size of the defect, and these hernias cannot be closed primarily [13]. The best option may be repair with biologic or synthetic mesh. Recurrent hernias with multiple small defects or those with mesh from previous surgeries are also difficult to deal with. Since the likelihood of recurrence and bowel obstruction is high, these hernias must also be addressed, likely with mesh.
Surgeons are justifiably concerned with mesh infection and recurrence of hernia when performing primary clean-contaminated bariatric surgery concomitantly with complex hernia repair. The previously cited study by Eid et al. showed no recurrence of hernia when mesh repair with SIS was performed. However, there were significant perioperative complications as wound infection occurred in 25% and seroma in 33% of these patients [16]. Biologic mesh is not an ideal solution. It is expensive, and significant rates of early and midterm recurrences, especially when this type of mesh is used to bridge fascial defects, have been reported [18]. Another, more recent, retrospective study of 325 gastric patients, 26 of whom had ventral hernia, underwent primary and prosthetic mesh repair. Surprisingly, 2 of the 8 patients who had primary repair had postoperative small bowel obstruction, while those with mesh repair had none [15]. This same study also showed no mesh infection when gastric bypass was performed simultaneously with synthetic mesh ventral hernia repair. Thus, it appears that complex hernias may be repaired with either synthetic or biologic mesh, depending on the surgeon’s comfort level.
Now that sleeve gastrectomy is an accepted part of the bariatric armamentarium [19], this may be the bariatric procedure of choice if a patient has a complex hernia. Sleeve gastrectomy allows for minimal manipulation of the bowel and does not dislocate the bowel that then may potentially incarcerate. The peritoneum is never appreciably exposed to enteric contents, and there is minimal risk of mesh infection. These patients are less likely to develop ileus or bowel distension since there are no anastomoses. For those with a large complex hernia or those with chronically incarcerated but nonobstructed bowel, sleeve gastrectomy may be a very safe option.
Occasionally, there are large, complex hernias that may preclude the surgeon from performing any intra-abdominal procedure prior to repairing the hernia. These hernias need to be repaired as a separate procedure prior to any elective bariatric surgery. Those patients with very large, chronic incisional hernias (>25–30 cm) will pose a problem for the surgeon in many aspects. Given the lack of fascia and chronically distended bowel, access into the peritoneum for insufflation to perform laparoscopy or adequate exposure for open surgery may be nearly impossible. The loss of domain with pneumoperitoneum will also be prohibitive for this type of patient, and ventilation, venous return, and tissue oxygenation will be compromised. This can lead to multiple complications including prolonged intubation, cardiac depression, and poor wound healing [20, 21]. Thus, the hernia must be dealt with first. In this scenario, the patient may need component separation and a staged ventral hernia repair prior to an elective bariatric surgery [22].
Another subset of patients with chronic fistulas or infected mesh from previous hernia repair will also require definitive hernia repair prior to bariatric surgery. The presence of an ongoing infection and further exposure of mesh will put the patient at risk for multiple postoperative complications. An attempt to remove the infected mesh in order to completely resolve the infection should be done before proceeding with (elective) bariatric surgery.
Conclusion
Whether an incisional hernia is simple or large and complex, the repair must be tailored to each individual bariatric patient. Clearly the lowest recurrence and complication rates will be realized if hernia repair is deferred until maximal weight loss is accomplished, with the added benefit that concurrent abdominoplasty can be performed. For some, small, incidentally discovered hernias, deferred management may be appropriate, but close follow-up is necessary. There appears to be good data at present however to make a case that primary repair is usually not sufficient as definitive therapy even for small, but clinically significant, defects, but it still may be applicable as a bridge repair during the immediate postoperative period. While infection rates are not common when prosthetics are used concomitantly with gastric bypass, mesh use in clean-contaminated cases remains debatable. If biologic mesh is used, substantial recurrence rates (and expense!) are important considerations. Despite some encouraging safety data that synthetic mesh should be considered in the repertoire of techniques to repair incisional hernia during gastric bypass, the use of this type of prosthetic material remains controversial.
References
Lambert DM, Marceau S, Forse RA. Intra-abdominal pressure in the morbidly obese. Obes Surg. 2005;15(9):1225–32.
Cobb WS, Burns JM, Kercher KW, Matthews BD, Norton JH, Heniford BT. Normal intraabdominal pressure in healthy adults. J Surg Res. 2005;129(2):231–5.
Varela JE, Hinojosa M, Nguyen N. Correlations between intra-abdominal pressure and obesity-related co-morbidities. Surg Obes Relat Dis. 2009;5(5):524–8.
Sugarman HJ, Kellum JM, Reines HD, DeMaria EJ, Newsome HH, Lowry JW. Greater risk of incisional hernia with morbidly obese than steroid dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg. 2006;171:80–4.
Alper D, Ramadan D, Vishne T, et al. Silastic ring vertical gastroplasty—long-term results and complications. Obes Surg. 2000;10:250–4.
Paran H, Shargian L, Schwarz I, Gutman M. Long-term follow-up on the effect of Silastic ring vertical gastroplasty on weight and co-morbidities. Obes Surg. 2007;17:737–41.
Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M. Trochar site hernia. Arch Surg. 2004;139:1248–56.
Hussain A, Mahmood H, Singhal T, et al. Long-term study of port-site incisional hernias after laparoscopic procedure. JSLS. 2009;13:346–9.
Bageacu S, Blanc P, Breton C, Gonzalez M, Porcheron J, Chabert M, Balique JG. Laparoscopic repair of incisional hernia: a retrospective study of 159 patients. Surg Endosc. 2002;16:345–8.
Raftopoulos I, Vanuno D, Khorsand J, Ninos J, Kouraklis G, Lasky P. Outcome of laparoscopic ventral hernia repair in correlation with obesity, type of hernia, and hernia size. J Laparoendosc Adv Surg Tech. 2002;12:425–9.
Rosen M, Brody F, Ponsky J, Walsh RM, Rosenblatt S, Duperier F, Fanning A, Siperstein A. Recurrence after laparoscopic ventral hernia repair. Surg Endosc. 2003;17:123–8.
Novitsky YW, Cobb WS, Kercher KW, Matthews BD, Sing RF, Heniford BT. Laparoscopic ventral hernia repair in obese patients: a new standard of care. Arch Surg. 2006;141:57–61.
Ching SS, Sarela AI, Dexter SP, Hayden JD, McMahon MJ. Comparison of early outcomes for laparoscopic ventral hernia repair between nonobese and morbidly obese patient populations. Surg Endosc. 2008;22(10):2244–50.
Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg. 2003;238:391–4.
Datta T, Eid G, Nahmias N, Dallal RM. Management of ventral hernias during laparoscopic gastric bypass. Surg Obes Relat Dis. 2008;4(6):754–7.
Eid GM, Mattar SG, Hamad G, Cottam DR, Lord JL, Watson A, Dallal RM, Schauer PR. Repair of ventral hernias in morbidly obese patients undergoing laparoscopic gastric bypass should not be deferred. Surg Endosc. 2004;18:207–10.
Newcomb WL, Polhill JL, Chen AY, Kuwada TS, Gersin KS, Getz SB, Kercher KW, Heniford BT. Staged hernia repair preceded by gastric bypass for the treatment of morbidly obese patients with complex ventral hernias. Hernia. 2008;12(5):465–9.
Jin J, Rosen MJ, Blatnik J, et al. Use of acellular dermal matrix for complicated ventral hernia repair: does technique affect outcomes? J Am Coll Surg. 2007;205(5):654–60.
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 2009;5(4):469–75.
Paajanen H, Laine H. Operative treatment of massive ventral hernia using polypropylene mesh: a challenge for surgeon and anaesthesiologist. Hernia. 2005;9:62–7.
Molloy RG, Moran KT, Waldron RP, Brady MP, Kirwan WO. Massive incisional hernia: abdominal wall replacement with Marlex mesh. Br J Surg. 1991;78(2):242–4.
Rao RS, Gentileschi P, Kini SU. Management of ventral hernias in bariatric surgery. Surg Obes Relat Dis. 2011;7(1):110–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Choi, J.J., Pomp, A. (2013). The Bariatric Patient with a Complex Ventral Hernia. In: Jacob, B., Ramshaw, B. (eds) The SAGES Manual of Hernia Repair. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4824-2_41
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4824-2_41
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4823-5
Online ISBN: 978-1-4614-4824-2
eBook Packages: MedicineMedicine (R0)