Abstract
Background
Obesity may be the most predominant risk factor for recurrence following ventral hernia repair. This is secondary to significantly increased intra-abdominal pressures, higher rates of wound complications, and the technical difficulties encountered due to obesity. Medically managed weight loss prior to surgery is difficult. One potential strategy is to provide a surgical means to correct patient weight prior to hernia repair.
Methods
After institutional review board approval, we reviewed the medical records of all patients who underwent gastric bypass surgery prior to the definitive repair of a complex ventral hernia at our medical center.
Results
Twenty-seven morbidly obese patients with an average of 3.7 (range 1–10) failed ventral hernia repairs underwent gastric bypass prior to definitive ventral hernia repair. Twenty-two of the gastric bypasses were open operations and five were laparoscopic. The patients’ average pre-bypass body mass index (BMI) was 51 kg/m2 (range 39–69 kg/m2), which decreased to an average of 33 kg/m2 (range 25–37 kg/m2) at the time of hernia repair at a mean of 1.3 years (range 0.9–3.1 years) after gastric bypass. Seven patients had hernia repair at the same time as their gastric bypass (four sutured, three biologic mesh), all of which recurred. Of the 27 patients, 19 had an open hernia repair and eight had a laparoscopic repair. Panniculectomy was performed concurrently in 15 patients who had an open repair. Prior to formal hernia repair, one patient required an urgent operation to repair a hernia incarceration and a small-bowel obstruction 11 months after gastric bypass. The average hernia and mesh size was 203 cm2 (range 24–1,350 cm2) and 1,040 cm2 (range 400–2,700 cm2), respectively. There have been no recurrences at an average follow-up of 20 months (range 2 months–5 years).
Conclusion
Gastric bypass prior to staged ventral hernia repair in morbidly obese patients with complex ventral hernias is a safe and definitive method to effect weight loss and facilitate a durable hernia repair with a possible reduced risk of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ventral hernias develop after laparotomy in up to 20% of patients in the United States each year. Reported hernia rates include 5–15% of patients undergoing open gastric band placement, 25% after other open bariatric procedures, and up to 40% after emergency midline laparotomy [1–5]. Ventral hernia repair has evolved from suture repair, with recurrence rates from 52% to more than 60%, to tension-free mesh repair using either an open or laparoscopic approach [6]. Mesh repair recurrence rates have decreased to less than 5% in some studies, and they have not changed significantly in recent years [7–10]. Obese patients are one of the highest risk groups for recurrence after ventral hernia repair [10, 11]. They often have associated independent risk factors for hernia recurrence, such as large defects, multiple previous repairs, and increased wound infections [10, 12, 13].
Medical comorbidities and perioperative complications, such as hypertension, diabetes, gastroesophageal reflux, obstructive sleep apnea, pulmonary embolism, stroke, cancer, and a shortened life span, are more common in obese patients. Calle et al. estimate that 90,000 cancer deaths per year could be avoided if the average adult body weights were reduced to the normal range (body mass index [BMI]<25) [14]. Weight loss, sustained weight loss, and the improvement of medical comorbidities with medical management is not as effective as with the surgical treatment of obesity [15]. The number of bariatric procedures in the United States has increased significantly with improvements in surgical technique and diminishing morbidity and mortality rates. The reduction or elimination of medical comorbidities after surgically induced weight loss has become an important consideration for surgeons when planning elective operations, such as ventral hernia repair. We hypothesized that performing a staged ventral herniorrhaphy in morbidly obese patients with complex hernias after a gastric bypass and significant weight loss would not only increase the quality of life, but also decrease both recurrence rates and perioperative complications.
Methods
Following institutional review board approval, we retrospectively reviewed the medical records of consecutive morbidly obese patients referred to our institution for the treatment of complex hernias who subsequently underwent a gastric bypass and delayed hernia repair. Morbid obesity was defined as having a BMI ≥40 kg/m2 or BMI ≥35 kg/m2 with at least one obesity-related comorbidity. Demographic, perioperative, and postoperative data were collected, including patient demographics, BMI (kg/m2) before and after gastric bypass, the number of previous abdominal operations and hernia repairs, operative and perioperative data, complications, hernia recurrences, and the duration of follow-up.
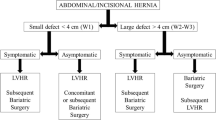
Standard open or laparoscopic Roux-en-Y gastric bypass was performed for each patient prior to definitive ventral hernia repair. At the time of gastric bypass, we attempted to leave the patient’s hernia undisturbed if possible, i.e., we did not reduce the contents of the hernia. Indeed, we believed that patients with large, fairly asymptomatic hernias would be safe from bowel obstruction if the small intestine did not need to “reorganize” within the hernia sac postoperatively. Small defects were sutured or a biologic mesh was used as a bridge when needed, with the understanding that these hernias would recur and require future intervention.
Our methods for ventral hernia repair have been previously described [10, 16]. Briefly, the open technique for ventral hernia repair was a modified Rives-Stoppa technique. Permanent mesh was placed in a retrofascial preperitoneal location with a large overlap of the hernia defect with a lightweight polypropylene mesh (Ultrapro™, Ethicon, Inc., Somerville, NJ). Transfascial fixation sutures were placed at 4–7-cm intervals around the periphery of the mesh. For laparoscopic repairs, access to the abdomen was obtained by a cut-down technique, followed by the creation of pneumoperitoneum. Three to five trocars were placed laterally. Adhesiolysis was performed immediately, and the hernia sac was left in situ after the contents of the hernia sac were reduced. Mesh was tailored to achieve a 4–7-cm overlap and was inserted into the abdomen. Titanium tacks were placed circumferentially at 1-cm intervals, and transfascial fixation sutures were placed every 4–7 cm around the periphery of the mesh. The 10-mm trocar sites were closed under direct vision using a suture passer.
Results
Twenty-seven morbidly obese patients were identified. Twenty-two had an open gastric bypass and five had laparoscopic operations. The average BMI prior to gastric bypass was 51 kg/m2 (range 39–69 kg/m2); the average BMI decreased to 33 kg/m2 (range 25–37 kg/m2) at the time of the staged ventral hernia repair. Elective ventral hernia repair occurred at a mean of 1.3 years (range 0.9–3.1 years) after gastric bypass. Patients undergoing staged repair had an average of 3.7 (range 1–10) previous failed ventral hernia repairs. Seven patients with small or very symptomatic defects had ventral hernia repairs at the time of gastric bypass (four sutured, three biologic mesh). One patient developed a major complication in the acute postoperative period, a dehiscence of his biologic mesh hernia repair on postoperative day 3, and required re-operation and closure. No anastomotic leaks occurred.
No patients with repair of small defects at the time of gastric bypass developed a bowel obstruction; however, all recurred, as expected, requiring staged, elective repair. One patient that had a large, unrepaired defect developed a small-bowel obstruction, requiring an urgent operation to reduce and repair an incarcerated ventral hernia 11 months after gastric bypass. Nineteen patients had an elective, open ventral hernia repair; eight were laparoscopic. The average hernia and mesh size was 203 cm2 (range 24–1,350 cm2) and 1,040 cm2 (range 400–2,700 cm2), respectively. Panniculectomy was concurrent with open ventral hernia repair in 15 patients. The average follow-up after ventral hernia repair was 20 months (range 2 months–5 years). Of the remaining 23 patients undergoing staged ventral hernia repair, no recurrences were identified.
Discussion
Obesity has reached epidemic proportions worldwide. The percentage of people with morbid obesity is climbing, even in countries that do not have a clear surplus of food.
Nearly 250 million people have a BMI ≥30 kg/m2. The World Health Organization (WHO) estimates that the number of obese people will increase by 20% to 300 million by 2025, with nearly half of Americans and one-third of Europeans having a BMI ≥30 kg/m2 [17, 18]. Surgically induced weight loss can provide a long-term solution for obese patients with the improvement or cure of obesity-related comorbidities [15].
Obesity has long been considered to be a risk factor for the development of a ventral hernia and recurrence after definitive repair [11, 19–21]. Sugerman et al. [11] showed that obesity was a greater risk factor for incisional hernia formation and recurrence than chronic steroid use. Mingoli et al. [2] followed 138 patients for 2 years after emergency midline celiotomy and showed that incisional hernias occurred in 18.1%, with an increased incidence in morbidly obese patients (p<0.008). Recurrence after ventral hernia repair in morbidly obese patients has been reported to be as high as 50% [13]. Kaminski [22] stratified recurrence rates based on stabilized body weight after gastric restrictive procedures in 70 patients. The recurrence rate was 5% in patients who had a stabilized body weight less than 200 lbs, 19% if 200–250 lbs, and 33% if >250 lbs. Sauerland et al. [23] performed a meta-analysis including several series (two reached statistical significance and seven did not) and found that the pooled relative risk of recurrence in obese patients (BMI ≥30 kg/m2) was 1.60. It is believed that this risk is significantly higher in morbidly obese patients (BMI ≥40 kg/m2). Both open and laparoscopic ventral hernia repairs are associated with increased recurrence rates in morbidly obese patients. Vidović et al. [12] reviewed 297 patients undergoing open incisional hernia repair (109 with mesh, 188 without mesh) and showed that large hernias (10-cm diameter, p=0.0000) and obesity (p=0.0000) were associated with significant increases in hernia recurrence. We reported outcomes following 850 consecutive laparoscopic ventral hernia repairs and found that morbidly obese patients (BMI ≥40 kg/m2) were four times more likely to have a recurrence compared with normal-weight individuals (7.8 vs. 2.0%, p=0.05) [10].
An increased recurrence rate in obese patients after ventral hernia repair is associated with multiple independent risk factors, including large defects, increased wound infections, multiple previous repairs, intraoperative difficulties, and increased intra-abdominal pressure [12, 13, 24, 25]. Obese patients also have an increased rate of perioperative complications and defects in tissue structure and healing, which increase the risk of recurrence [26–33]. Obese diabetic patients develop wound complications secondary to glycosylated white blood cells and microangiopathy. The number of surgical-site infections is further increased without tight control of serum glucose in the perioperative period [34–36]. Greater extra-abdominal fat requires larger incisions for open surgery, which can increase infection rates. Increased intra-abdominal fat decreases the working space for laparoscopic procedures, which can contribute to an increased conversion rate [37–39]. Our group, along with Sugerman et al., have demonstrated that obese patients have higher intra-abdominal pressure compared with patients with normal weight and that the intra-abdominal pressure decreases after surgically induced weight loss [24, 25, 40, 41]. Data from our laboratory comparing bladder pressures in obese and non-obese patients show that obese patients have increased intra-abdominal pressures during every activity measured, which included Valsalva’s maneuver, lifting light weights, climbing stairs, coughing, and others [25]. Intra-abdominal pressures compared before and 1 year after gastric bypass (mean decrease in BMI from 44.52 to 29.09 kg/m2) show a statistical decrease for every activity measured [40].
One of the obvious benefits of staged ventral hernia repair in obese patients is a decrease in the recurrence rate. No patients in our series recurred after staged ventral hernia repair at a mean follow-up of 20 months, despite having very large hernias (average defect size 203 cm2). Eid et al. [42] reported no recurrences in 14 staged patients after gastric bypass at a mean follow-up of 20 months (average defect size of 14.5 cm2). Bonatti et al. [5] reported no recurrences in seven staged patients after the placement of an adjustable gastric band at a mean follow-up of approximately 34 months (two “giant” hernias and five with an average defect size of 7 cm2). Concurrent repairs at the time of bariatric surgery have higher recurrence rates. Schuster et al. reported one recurrence (9%) after 11 staged repairs at 14 months follow-up. Eid et al. reviewed 59 patients with concurrent repairs with permanent mesh at the time of gastric bypass and observed a 22% recurrence rate at 30 months follow-up [42].
Staged ventral hernia repair after bariatric surgery has previously been criticized because of the increased incidence of bowel obstruction during the period of rapid, surgically induced weight loss [42]. One patient (3.7%) in our series required urgent surgery for small bowel obstruction secondary to hernia incarceration. Eid et al. [42] reported a bowel obstruction rate of 35.7% in 14 patients with staged repairs after gastric bypass. Bonatti et al. [5] reviewed seven patients with ventral hernia repairs after the placement of an adjustable gastric band and reported bowel obstructions in 29% of the cases. Our average defect size (203 cm2) was more than 14 times the highest reported average defect size (14.5 cm2, Eid et al.) for staged ventral hernia repairs after gastric bypass [42]. Obviously, the incidence of bowel obstruction after bariatric surgery is higher when smaller defect sizes are treated in a delayed fashion. We concurrently repaired hernias in patients with small defects at the time of gastric bypass, 100% of which recurred. This, however, allowed us to definitively repair the hernia later. Biologic meshes used for a concurrent repair at the time of bariatric surgery eventrated over time, requiring a definitive repair with a synthetic mesh following weight loss. The risk/benefit ratio with regard to recurrence and bowel obstruction appears to be in favor of concurrent repairs for small defects and staged repair for larger hernias. Large studies measuring defect size and location, hernia contents, weight loss, etc., are needed to define the risk of bowel obstruction during the period of rapid, surgically induced weight loss after bariatric surgery.
Successful laparoscopic ventral hernia repair in obese patients requires strict adherence to technical details. Cobb et al. [43] reviewed 277 patients at our institution and found that the recurrence rate in patients with BMI ≥40 kg/m2 was at least twice that of patients with BMI <40 kg/m2, but this was not statistically significant (9.4% for BMI ≥40 kg/m2 compared to 4.5% for BMI 30–40 kg/m2 and 3.5% for BMI <30 kg/m2). Novitsky et al. [44] reviewed 163 patients with BMI ≥30 kg/m2 who underwent laparoscopic ventral hernia repair and reported an overall recurrence rate of 5.5%, which is only slightly increased compared with the published recurrence rates for all patients undergoing laparoscopic ventral hernia repair [10]. These results suggest that a standardized laparoscopic technique is advantageous in obese patients. Technical detail is also important for successful outcome after open repair. Concurrent abdominoplasty and scar revision often necessitate an open approach for patients with giant hernias after surgically induced weight loss, as seen in 67% of patients in this study. Wide overlap of non-absorbable retrofascial preperitoneal mesh extending well beyond the edge of the hernia defect circumferentially with transfascial fixation sutures at close intervals resulted in no recurrences after staged ventral hernia repairs at 20 months of follow-up in this study. Twelve of our patients had a simultaneous panniculectomy. Shermak [45] reviewed 40 patients undergoing abdominoplasty at the time of ventral hernia repair. The only recurrence in Shermak’s series occurred 1 year after hernia repair in a patient with a BMI of 41.3. Hughes et al. [46] reported a recurrence rate after simultaneous ventral hernia repair and panniculectomy of 3.6% (two of 55 patients). Robertson et al. [47] reported a 10% recurrence rate in 82 patients undergoing simultaneous procedures. Concurrent abdominoplasty does not appear to diminish the durability of ventral hernia repair; however, larger series with longer follow-up are needed [44].
Conclusion
Gastric bypass followed by the staged repair of recurrent ventral hernia in morbidly obese patients appears to be safe and provide a durable repair. The benefits include a reduced recurrence rate and an improved overall quality of life due to weight loss. The risk of hernia incarceration and bowel obstruction during the period of rapid, surgically induced weight loss is present but rare in our study. All smaller defects repaired concurrently with gastric bypass have a high recurrence rate but no reported incidence of bowel obstruction. Herniorrhaphy performed after gastric bypass and significant weight loss results in a formidable hernia repair and a lack of recurrence at 20 months follow-up. It should be considered in any morbidly obese patient with a complex or recurrent hernia.
References
Read RC, Yoder G (1989) Recent trends in the management of incisional herniation. Arch Surg 124:485–488
Mingoli A, Puggioni A, Sgarzini G, Luciani G, Corzani F, Ciccarone F, Baldassarre E, Modini C (1999) Incidence of incisional hernia following emergency abdominal surgery. Ital J Gastroenterol Hepatol 31:449–453
Higa KD, Boone KB, Ho T (2000) Complications of the laparoscopic Roux-en-Y gastric bypass: 1,040 patients—what have we learned? Obes Surg 10:509–513
Brolin RE (1996) Prospective, randomized evaluation of midline fascial closure in gastric bariatric operations. Am J Surg 172:328–331
Bonatti H, Hoeller E, Kirchmayr W, Muhlmann G, Zitt M, Aigner F, Weiss H, Klaus A (2004) Ventral hernia repair in bariatric surgery. Obes Surg 14:655–658
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583 (discussion 583–585)
Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, Rege RV, Turnage RH (2000) Factors affecting recurrence following incisional herniorrhaphy. World J Surg 24:95–100 (discussion 101)
Luijendijk RW, Lemmen MH, Hop WC, Wereldsma JC (1997) Incisional hernia recurrence following “vest-over-pants” or vertical Mayo repair of primary hernias of the midline. World J Surg 21:62–65 (discussion 66)
Stoppa RE (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238:391–399 (discussion 399–400)
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171:80–84
Vidović D, Jurisić D, Franjić BD, Glavan E, Ledinsky M, Bekavac-Beslin M (2006) Factors affecting recurrence after incisional hernia repair. Hernia 10:322–325
Hesselink VJ, Luijendijk RW, de Wilt JH, Heide R, Jeekel J (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr (1999) Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 341:1097–1105
Kushner RF, Noble CA (2006) Long-term outcome of bariatric surgery: an interim analysis. Mayo Clin Proc 81:S46–S51
Novitsky YW, Porter JR, Rucho ZC, Getz SB, Pratt BL, Kercher KW, Heniford BT (2006) Open preperitoneal retrofascial mesh repair for multiply recurrent ventral incisional hernias. J Am Coll Surg 203:283–289
Seidell JC (2000) Obesity, insulin resistance and diabetes—a worldwide epidemic. Br J Nutr 83(Suppl 1):S5–S8
Li Z, Bowerman S, Heber D (2005) Health ramifications of the obesity epidemic. Surg Clin North Am 85:681–701
Regnard JF, Hay JM, Rea S, Fingerhut A, Flamant Y, Maillard JN (1988) Ventral incisional hernias: incidence, date of recurrence, localization and risk factors. Ital J Surg Sci 18:259–265
Pitkin RM (1976) Abdominal hysterectomy in obese women. Surg Gynecol Obstet 142:532–536
Cleveland RD, Zitsch RP 3rd, Laws HL (1989) Incisional closure in morbidly obese patients. Am Surg 55:61–63
Kaminski DL (2000) The role of gastric restrictive procedures in treating ventral hernias in morbidly obese patients. Int J Surg Investig 2:159–164
Sauerland S, Korenkov M, Kleinen T, Arndt M, Paul A (2004) Obesity is a risk factor for recurrence after incisional hernia repair. Hernia 8:42–46
Sugerman HJ (2001) Effects of increased intra-abdominal pressure in severe obesity. Surg Clin North Am 81:1063–1075
Paton BL, Cristiano J, Head MC, Norton HJ, Kuwada TS, Kercher KW, Heniford BT (2006) Intra-abdominal pressure in normal, fit, and obese individuals. In: SAGES annual meeting
Choban PS, Heckler R, Burge JC, Flancbaum L (1995) Increased incidence of nosocomial infections in obese surgical patients. Am Surg 61:1001–1005
Blaszyk H, Wollan PC, Witkiewicz AK, Björnsson J (1999) Death from pulmonary thromboembolism in severe obesity: lack of association with established genetic and clinical risk factors. Virchows Arch 434:529–532
Wu EC, Barba CA (2000) Current practices in the prophylaxis of venous thromboembolism in bariatric surgery. Obes Surg 10:7–13 (discussion 14)
Luján JA, Frutos MD, Hernández Q, Liron R, Cuenca JR, Valero G, Parrilla P (2004) Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. Ann Surg 239:433–437
Flancbaum L, Choban PS (1998) Surgical implications of obesity. Annu Rev Med 49:215–234
Israelsson LA, Jonsson T (1997) Overweight and healing of midline incisions: the importance of suture technique. Eur J Surg 163:175–180
Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, Foley EF (2004) Wound infection after elective colorectal resection. Ann Surg 239:599–605 (discussion 605–607)
Memon MA (1997) Review. Laparoscopic appendicectomy: current status. Ann R Coll Surg Engl 79:393–402
Hu H, Li N, Yngen M, Ostenson CG, Wallén NH, Hjemdahl P (2004) Enhanced leukocyte-platelet cross-talk in Type 1 diabetes mellitus: relationship to microangiopathy. J Thromb Haemost 2:58–64
Krinsley JS (2004) Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc 79:992–1000
Latham R, Lancaster AD, Covington JF, Pirolo JS, Thomas CS (2001) The association of diabetes and glucose control with surgical-site infections among cardiothoracic surgery patients. Infect Control Hosp Epidemiol 22:607–612
Mendoza D, Newman RC, Albala D, Cohen MS, Tewari A, Lingeman J, Wong M, Kavoussi L, Adams J, Moore R, Winfield H, Glascock JM, Das S, Munch L, Grasso M, Dickinson M, Clayman R, Nakada S, McDougall EM, Wolf IS, Hulbert J, Leveillee RJ, Houshair A, Carson C (1996) Laparoscopic complications in markedly obese urologic patients (a multi-institutional review). Urology 48:562–567
Pikarsky AJ, Saida Y, Yamaguchi T, Martinez S, Chen W, Weiss EG, Nogueras JJ, Wexner SD (2002) Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc 16:855–858
Robinson SP, Hirtle M, Imbrie JZ, Moore MM (1998) The mechanics underlying laparoscopic intra-abdominal surgery for obese patients. J Laparoendosc Adv Surg Tech A 8:11–18
Thomas MS, Paton BL, Norton HJ, Newcomb WW, Hope WW, Kuwada TS, Gersin KS, Heniford BT (2007) Changes in bladder pressure in morbidly obese patients 1-year after gastric bypass surgery. In: SAGES annual meeting
Sugerman H, Windsor A, Bessos M, Kellum J, Reines H, DeMaria E (1998) Effects of surgically induced weight loss on urinary bladder pressure, sagittal abdominal diameter and obesity co-morbidity. Int J Obes Relat Metab Disord 22:230–235
Eid GM, Mattar SG, Hamad G, Cottam DR, Lord JL, Watson A, Dallal RM, Schauer PR (2004) Repair of ventral hernias in morbidly obese patients undergoing laparoscopic gastric bypass should not be deferred. Surg Endosc 18:207–210
Cobb WS, Kercher KW, Matthews BD, Burns JM, Tinkham NH, Sing RF, Heniford BT (2006) Laparoscopic ventral hernia repair: a single center experience. Hernia 10:236–242
Novitsky YW, Cobb WS, Kercher KW, Matthews BD, Sing RF, Heniford BT (2006) Laparoscopic ventral hernia repair in obese patients: a new standard of care. Arch Surg 141:57–61
Shermak MA (2006) Hernia repair and abdominoplasty in gastric bypass patients. Plast Reconstr Surg 117:1145–1150 (discussion 1151–1142)
Hughes KC, Weider L, Fischer J, Hopkins J, Antonetti A, Manders EK, Dunn E (1996) Ventral hernia repair with simultaneous panniculectomy. Am Surg 62:678–681
Robertson JD, de la Torre JI, Gardner PM, Grant JH 3rd, Fix RJ, Vásconez LO (2003) Abdominoplasty repair for abdominal wall hernias. Ann Plast Surg 51:10–16
Author information
Authors and Affiliations
Corresponding author
Additional information
No outside funding was received for this study.
Rights and permissions
About this article
Cite this article
Newcomb, W.L., Polhill, J.L., Chen, A.Y. et al. Staged hernia repair preceded by gastric bypass for the treatment of morbidly obese patients with complex ventral hernias. Hernia 12, 465–469 (2008). https://doi.org/10.1007/s10029-008-0381-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0381-1