Abstract
Breast cancer is increasing 3.1 % annually. It is more deadly and more frequent in young women in developing countries compared to young women in the more developed countries. Important reasons for this increased incidence and lethality are poor nutrition (leading to decreased immunity to resist the advance of cancer), delayed access to health care, and poor quality of care when it is finally available. Early detection of breast cancer is the key to the control of its lethal effects. Increasing breast health awareness and clinical breast examination are key components of a screening program at the present time. Such a strategy is aimed at detecting Stage I and Stage II cancers and downstaging cancers from the now prevalent presentation at Stage III and Stage IV. For the future, however, a low cost methodology needs to be adopted in order to diagnose small node-negative cancers by screening the asymptomatic population. Organized screening mammography is not a feasible option for low and mid-resource countries, even in the future. A combination of low prevalence and the expensive infrastructure needed in terms of the equipment and trained health-care professionals makes this an unrealistic option and a potential drain and diversion of health-care funding resources in developing countries. The background of the situation that is currently in existence, problems thereof, and the potential for the use of whole breast ultrasound screening for breast cancer is discussed in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
A. Future Strategies for Breast Cancer Screening in Developing Countries
Abstract
Breast cancer is increasing 3.1 % annually. It is more deadly and more frequent in young women in developing countries compared to young women in the more developed countries. Important reasons for this increased incidence and lethality are poor nutrition (leading to decreased immunity to resist the advance of cancer), delayed access to health care, and poor quality of care when it is finally available. Early detection of breast cancer is the key to the control of its lethal effects. Increasing breast health awareness and clinical breast examination are key components of a screening program at the present time. Such a strategy is aimed at detecting Stage I and Stage II cancers and downstaging cancers from the now prevalent presentation at Stage III and Stage IV. For the future, however, a low cost methodology needs to be adopted in order to diagnose small node-negative cancers by screening the asymptomatic population. Organized screening mammography is not a feasible option for low and mid-resource countries, even in the future. A combination of low prevalence and the expensive infrastructure needed in terms of the equipment and trained health-care professionals makes this an unrealistic option and a potential drain and diversion of health-care funding resources in developing countries. The background of the situation that is currently in existence, problems thereof, and the potential for the use of whole breast ultrasound screening for breast cancer is discussed in this chapter.
Status of Breast Cancer in Low Resource (LR) Countries
Breast cancer is a worldwide epidemic that is increasing 3.1 % per year, almost twice as fast as the increase in world population. Although only about half of the breast cancer cases occur in low resource countries, almost two thirds (63.5 %) of these cases occur in women under the age of 50, and almost three quarters (72.1 %) of the deaths from breast cancer found in this younger group occur in these developing countries [1].
Disproportionate Incidence in Young Women
The reasons for the increased incidence of breast cancer in younger women in LR countries and the disproportionate increased death rate among these women require complex explanations because of multiple causative factors. The overall incidence of breast cancer in the LR countries is not greater, and often is considerably less, than the incidence in the high resource (HR) countries. However, the incidence in women under 50 years of age in the developing countries is disproportionately high, probably for reasons discussed in the following sections.
Nutrition
The limited caloric intake of low resource women may have differing effects on cancer rates and the severity of cancer once established. Pre-cancer (in situ) and probably very early invasive cancer do not immediately establish an independent blood supply. Until they do, these proto-cancers must compete with the adjacent cells for nutrition. In the environment of low nutrients found in these women, cancer cells are at a disadvantage due to their higher metabolic rate, necessitated by the requirement to reproduce quickly. They may be unable to sustain themselves in this environment and fail to survive to establish a blood supply.
Compared to women from LR countries, women from HR countries with surfeits of nutrients form cancers which may more easily establish themselves, gain blood supplies, and go on to become clinically recognized cancers. Because of the increased sugar absorption in cancer cells, a Westernized diet may be particularly advantageous for cancer development [2]. This scenario may be true in China where the breast cancer rate has climbed greatly in the major cities over the past two or three decades due to the improved nutrition of these urban populations, with a diet including more free sugar than the traditional Chinese diet [3]. The cancer rate in the more nutritionally challenged countryside has not undergone the same marked increase. The countryside cancer incidence is less than half that of Shanghai, with the rate of increase accelerating faster in Shanghai for the past 30 years. The incidence of breast cancer in the urban areas is expected to be almost quadruple that of the countryside in 20 years [3].
The breast cancer rate will probably increase in women in all LR countries as their average calorie consumption increases, especially if this increase is accompanied by a disproportionate increase of simple sugars in the diet. At present, although the incidence of breast cancer is lower in LR countries, the mortality rate of these cancers is greater than those found in HR countries. The reasons are multiple.
Delayed Access to Health care
Obviously, where education is minimal and medical resources are scarce, cancers will be larger at discovery. These cancers would also be expected to be more aggressive and therefore more lethal as they enlarge [4].
Lower Quality Treatment
The lack of radiation and chemotherapy denies LR women any increased chance of survival once the cancer reaches the lymph nodes.
Decreased Immunity
Another important cause of the increased lethality of breast cancer in women of LR countries is that the body conserves energy when the diet is insufficient. The body is a multitasking organism, which, during times of extreme stress, including insufficient calories and other nutrients, will decrease its immunological defenses against infectious agents and cancer. Although it is more difficult for a breast cancer to recruit a blood supply in an undernourished woman, if it does succeed, it will likely grow faster and more aggressively than expected because of a reduced immunological resistance from the host [5] compared to women with better nutrition.
Hereditable Factors
The etiology of the majority of breast cancers is not well understood. Some breast cancer is clearly related to hereditary genetic defects such as BRCA1, BRCA2, and tp53, among many others. These genes are responsible for repair of strands of DNA damaged by ionizing radiation, free radicals, and other causes. If repair is impossible, some of these genes are responsible for the death of these damaged cells, thereby blocking unregulated reproduction of cells—in other words, formation of cancer [6]. However, at all ages, only about 5–10 % of breast cancer is explained by genetic abnormalities. The percentage of breast cancer related to genetic abnormalities is greater in the young, but it is insufficient to explain the preponderance of the young breast cancer cases in LR counties. Also, there is no reason to assume that the rate of hereditable factors would be greater in LR than in HR women.
Environmental Factors
Various environmental factors have been put forward to explain the increasing occurrence of breast cancer, such as exogenous estrogen, obesity, smoking, second hand smoke, alcohol consumption, and exposure to pesticides, but these factors do not explain the marked disparity between breast cancer frequency in women under age 40 in the HR and some LR countries.
Contagion
In 1936, Bittner [7] described transmission of breast cancer to normal mice through nursing from a strain of mice with a strong propensity for developing breast cancers. Once the originally normal mice developed breast cancer from this breastfeeding, their subsequent descendants did also. Since viruses had not yet been described, the etiology of this phenomenon was uncertain until the discovery of Mouse Mammary Tumor Virus (MMTV) as the causative agent [8].
Although some controversy still exists, Human Papilloma Virus, especially types 16, 18, 31, and 33, almost certainly is the underlying cause of up to 30 % of breast cancer in some regions of the world [9]. HPV-induced breast cancer, in the experience of the authors and others, is more aggressive and occurs more often in younger women [10] than would be otherwise expected. In the United States as in other countries, HPV infection peaks at a young age, usually under 30 [11] (Fig. 16A.1).
Human papillomavirus—prevalence of high-risk and low-risk types among females aged 14–59 years, National Health and Nutrition Examination Survey, 2003–2006. HPV Human Papillomavirus. Note: Error bars indicate 95 % confidence interval. Both high-risk and low-risk types of HPV were detected in some females (reprinted with permission of Oxford University Press from Hariri S, Unger ER, Sternberg M, Dunne EF, Swan D, Patel S et al. Prevalence of genital HPV in the among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. J Infect Dis 2011;204(4):566–73)
In general, the nutritional state of women is poor in LR countries relative to women from HR countries. Access to daily bathing is also compromised. Since HPV may persist in the pelvic region for many years without cancer of the cervix, the viral load of infective virus in the pelvic area will be considerably greater in those women who are able to cleanse themselves only weekly, monthly, or less.
Since common skin warts and all other HPVs are transmitted by an inoculum of the virus on broken skin or a mucous membrane, once established, the spread of the warts is by self-inoculation [12]. The chance of further self-infection is likely to be closely related to the amount of inoculum delivered to the susceptible site. Unlike HPV-induced malignancy at other sites, including cervix, anus, mouth, and pharynx, where the HPV is delivered to the site by and from a sexual partner, HPV-induced breast cancer may result from auto-infection through the nipple. This may occur from transfer of the inoculum from a woman’s own perineum to her hands or the hands of a sexual partner and then to her nipple during bathing or other touching. Such auto-infection would be expected to be particularly increased in young women from LR countries who have a lowered resistance to infection and who, because of inability to maintain proper hygiene, would likely have more HPV available for transfer from their perinea. However, it is not certain if breast HPV infection may at times be secondary to blood-borne infection also. Pakistan has one of the highest rates in the world of both HPV infection and breast cancer in young women [13]. Further clinical research in this area is critically necessary in order to strengthen the logical argument that these findings are related.
Approaches to Decreasing Breast Cancer Morbidity and Mortality
There are three levels of attack to decrease morbidity and mortality: (1) prevention, (2) early discovery, and (3) improved treatment. Prevention and early discovery have the added benefit of being sufficiently economical to be feasible in large populations.
Prevention
As discussed previously, it appears that Human Papilloma Viruses are contributing to the problem of aggressive breast cancers in young women in LR countries. This virus may explain most, if not all, of the disproportional occurrence in young women from these countries, compared to similar women in HR countries. This is equivalent to the disproportionate morbidity and mortality of cervical cancer in LR countries. An intensive worldwide campaign of vaccination against HPV in all children ages 9–12, particularly girls, would significantly reduce the death rate from breast cancer in those women as they mature, in addition to increasing the lives saved from prevention of cervical cancer. The present HPV vaccine is effective against types 16 and 18, which are the HPVs most often found in association with breast cancer, as well as types 6 and 11, which cause genital and anal warts [14]. However, other types are common in Asia and may account for a significant number of young women’s breast cancers in East and Southeast Asia [15].
Early Detection of Breast Cancer
Present Techniques for Detection of Breast Cancer
There are six possible methods for screening for breast cancer: physical examination and five imaging methods. Three of the imaging techniques can be dismissed immediately for widespread screening in LR countries because of complexity and expense. MRI has no portability and requires machinery costing many hundreds of thousands of dollars or more. Injection of gadolinium, an expensive rare-earth element, is necessary for each woman screened. The likelihood of performing contrast MRI for less than $200 in the near future is nil.
There are two nuclear imaging screening techniques, breast specific gamma imaging (BSGI) and positron emission tomography (PET), which use short-lived radioactive substances. The expense of the machinery and the unique rapid transportation requirements of the isotopes make these tests impossible in countries with poor technical infrastructures.
The three remaining breast screening methods need to be considered.
Physical Examination
The mean diameter of cancers discovered by non-imaging methods—including clinical breast examination (CBE), breast self-examination (BSE), and serendipity—is about 29 mm [16] in high resource countries. Recently, even in HR countries, BSE is considered not to decrease the average size of cancer discovered [17]. There is no study documenting the average size of breast cancers in asymptomatic LR women who are in a screening clinical examination program. Duffy and colleagues [18] predicted that screening for breast cancer with CBE alone in such a population would lead to a 13 % reduction in node-positive cases and a 12 % reduction in breast cancer deaths. The authors thought size reduction would probably occur only in cancers about 3 cm or larger because of the lack of well-trained examiners. As emphasized in Chap. 4 on screening for breast cancer, rigorous training in CBE is a key component of success. CBEs would miss most of the physically subtle, small cancers. Fine-needle aspiration (FNA) has been shown to be often over 90 % accurate in a meta-analysis [19], but many of the studies used image guidance, which would increase their accuracy over blind biopsy. Also, the FNAs were presumably more accurate due to the training and experience of the physicians performing the biopsies compared with the lower training of those doing biopsies in LR countries. Similarly, the accurate interpretation of FNA material is difficult, and only comes after proper training and long experience [20].
Screening Mammography
Dr. Lazlo Tabár [21] demonstrated about a 30 % reduction in mortality from breast cancer in the two-county Swedish study by discovering breast cancer two thirds smaller by volume at an average diameter of 1.8 cm compared with the 2.6 cm diameter average physical discovery without mammography. While this is a very significant decrease in mortality, it may be very difficult and expensive to replicate these results in LR countries. The two methods of recording mammographic images in wide use today are film-screen mammography (FSM) and digital mammography (DM), with both imaging technologies having significant base requirements. These two forms of mammography require a reliable source of high amperage and often high voltage electric current. FSM, the cheaper and easier form, also requires a source of clean water. DM requires a sophisticated computer installation, expensive viewing monitors, and many terabytes of data storage [22].
Mammography has some more pronounced disadvantages for women from low resource countries compared to women from higher resource backgrounds. LR women tend to be thinner and, therefore, more commonly have dense breasts with less fat to contrast with the fatless cancer (Fig. 16A.2). Up to 50 % of cancers in dense breasts will be visible by ultrasound before they are visible on annual screening mammography [23]. Since many of the cancers in LR women develop under the age of 40, not only is the percentage of women with dense breasts higher, but also routine screening mammography is not recommended in women younger than 40, partially because of the increased radiosensitivity of breast tissue below this age. For these reasons, the technical challenges of mammography and its expected poorer performance in the LR setting compared with the HR model make it not the first choice for screening.
Breast Cancer Screening by Ultrasound
Breast cancer incidence is expected to rise in low and mid-resource countries in the coming decades. While mammography is likely to remain the backbone of screening for early detection of breast cancer in the developed countries, it is not a viable, cost-effective option for widespread implementation in developing countries. Screening for breast cancer using sonography may be a viable alternative to mammography. A case for potential use of sonography for population-based or opportunistic screening is discussed. Unlike mammography, a mortality rate reduction from breast cancer through the use of screening breast ultrasound will probably never be proven. Existing data on the value of screening breast ultrasound are based on studies conducted on women at higher risk for breast cancer and almost always as a complement to mammography.
Evidence for the use of ultrasound in breast cancer screening. It is neither possible nor practical to attempt to prove a mortality rate reduction from the use of whole breast ultrasound screening. Proof of mortality rate reduction will require a randomized controlled clinical trial involving a large number of women receiving screening with the new modality, who will then have to be followed for at least 15 years and be matched with a control group of women who receive the current standard care [24]. The new modality being tested would have to show mortality rate reduction over and above what has been achieved with screening mammography; this is unlikely to be the case anytime in the near future [24]. The use of breast ultrasound as a supplemental modality for breast cancer screening has been studied in women with dense breast tissue and in those with an elevated risk for breast cancer [25, 26]. A systematic search and review of studies involving mammography and ultrasound performed for screening of breast cancer found six cohort studies, of which only two had follow-up on patients with negative or benign findings. Screening ultrasound performed in women with American College of Radiology breast density types 2–4 identified primarily invasive cancers in 0.32 % of women. The mean tumor size was 9.9 mm, and 90 % of the cancers were node negative. Biopsy rate was high at 2.3–4.7 %, with positive predictive value of 8.4–13.7 % for those biopsied because of an abnormal finding on the ultrasound examination. The added benefit of using ultrasound to screen for breast cancers in women with a negative mammogram might be lower in women aged 50–69 years [25]. The most notable and the largest clinical trial of screening ultrasound to date is the American College of Radiology Imaging Network trial35 (ACRIN 6666). This study was a prospective multicenter trial randomized to one group receiving ultrasound and mammographic screening and one group receiving mammographic screening alone to compare the diagnostic yield of performance of breast ultrasound and mammography vs. mammography alone in women with elevated risk of cancer [26]. The criteria used in this study to determine an elevated risk for breast cancer included a personal history of breast cancer, prior atypical biopsy, elevated risk based on the Gail or Claus model, or both. A standard protocol and interpretive criteria were used. Mammography and ultrasound were performed and read independently, allowing for reducing potential biases in patient recruitment and interpretation. Data were analyzed from 2,637 patients who underwent imaging. Thirty-one cancers were detected in the study group, 11.8 per 1,000 women; the increase in the cancer detection rate because of addition of ultrasound was 4.2 per 1,000 women. The diagnostic accuracy for mammography was 0.78, for ultrasound was 0.80, and for combined mammography and ultrasound was 0.91 [26]. Ultrasound hence proved a useful supplemental modality, identifying additional small node-negative invasive cancers in this cohort of women at an elevated risk for breast cancer [26].
Breast sonography has never been studied or been advocated to be used as the only modality to screen for breast cancer. There is, however, some data from a study conducted in Japan that demonstrated the value of sonography when used as the only modality for screening of breast cancer in women <40 years of age [27]. This study was undertaken in the Ibaraki prefecture of Japan where the breast cancer screening recommendations include performing annual screening ultrasound and CBE in women of ages 30 through 56 and biannual mammography in women of ages 40 through 65. There were 12,359 women in the age group of 30–39 years who received annual screening breast ultrasound and did not undergo mammographic screening. Of these, 4,501 women also received annual CBE in addition to whole breast screening ultrasound. In young women, i.e., younger than the age of 40 years, as expected, the cancer yield was low, with a cancer detection rate of 0.04–0.07 %. In those women between the ages of 40–56 years in whom both mammography and ultrasound were used, the cancer detection rate ranged from 0.13 to 0.16 % for sonography and 0.1–0.22 % for mammography. Overall, 41,653 women underwent mammography, and 48,294 women underwent CBE and breast ultrasound. The rate of detection of stage I cancers was 72 % by ultrasound, 66 % by mammography, and 42 % by CBE [27].
Whole breast ultrasound screening: pros and cons. The benefits of ultrasound as a screening modality are that it does not use ionizing radiation, is well tolerated, and is optimally amenable for percutaneous biopsy guidance. Ultrasound is able to identify small non-palpable masses while undeterred by presence of dense breast tissue, which is an inherent limitation of mammography. Compared to mammography, the initial capital expense and resources needed to maintain equipment are significantly lower; there is also no need for stringent quality assurance and control required at multiple stages of screen film mammography, for example, training of mammography technologists and ensuring consistency and reproducibility in the quality of mammographic images (dependent on a host of factors including machine calibration, patient positioning, tolerance of breast compression, and the process of film developing). Mammographic viewing requirements, mammogram films filing, and storage are additional costs to be factored in. Overall, the cost to set up screen film mammography for breast cancer screening is expected to be several multiples of the costs required for breast ultrasound. However, unlike mammography, the vast majority of cancers that are seen on ultrasound are invasive cancers; DCIS is not usually identified by sonography [26]. It is debatable whether a screening examination that identifies small node-negative cancers is adequate or whether detection of DCIS is a more critical requirement of a screening test. There are limitations for the use of ultrasound in screening for breast cancer. Ultrasound has never been proved to reduce mortality from breast cancer. Limitation of ultrasound is the high rate of false-positive studies; the positive predictive value in those cases in which biopsy was performed was 8.8–8.9 %, compared with 23 % with mammography [26]. In this context, it is worthwhile keeping in mind that a false-positive ultrasound might not have the same consequence as that of a false-positive mammogram. As Kuhl points out in an editorial, a suspicious finding on a mammogram requires a much more expensive and time-consuming biopsy procedure than an ultrasound-guided core biopsy or a fine-needle aspiration biopsy that can be performed often immediately after the ultrasound examination [28].
The positive predictive value of screening ultrasound is low. Of 233 women for whom biopsy was recommended based on a suspicious ultrasound finding, only 20 (8.6 %) were diagnosed with breast cancer. However, in the same cohort, mammography, which is the accepted standard of care for screening, had a positive predictive value of only 14.7 % (20 of 136) [26, 28]. Ultrasound has the added advantage of being able to stage cancers by examination of bilateral axilla in women who are diagnosed to have cancer.
Optimizing use of whole breast ultrasound screening for breast cancer. As stated previously, a basic prerequisite for implementation of screening for any cancer should be a high prevalence of the cancer being targeted. Such organized screening programs must therefore be put in place once credible disease prevalence statistics have been established in the region that is targeted. The success of such a program is very dependent on the expertise of those performing and interpreting the sonograms. In developing countries, a cost-effective approach would involve training technologists to perform breast ultrasound, and, depending on available local resources, direct or remote supervision of breast ultrasound exams may be performed by a physician. Use of ultrasound has the added advantage of being amenable to telemedicine consultation via web-based link to remote centers of excellence. Training of nurses to perform ultrasound-guided percutaneous fine needle or core needle biopsy is a very feasible option with opportunity for real time supervision from remote sites. A successful 2 day training module has been established by the Educational Committee of the Japan. Participants are tested for ability to detect lesions using videos and ability to characterize lesions using static images [29]. A study compared 422 physicians and 415 technologists. Ultrasound technologists performed as well as physicians in recognizing and interpreting cancers on these tests.
Using criteria described in the Chap. 4 on screening for breast cancer, it is possible to minimize the false-positive rate for biopsy of ultrasound screen detected non-palpable solid masses. Since ultrasound screening has never been studied extensively as a modality by itself to screen for breast cancer, it may very well be a learn-as-you-go approach. A high false-positive biopsy rate is to be expected when ultrasound is used for routine screening. There may be ways of mitigating this limitation. One way would be not to biopsy non-palpable masses smaller than 1 cm that exhibit no malignant features and instead follow them on a yearly basis for 2 years. Another way to minimize false positives would be to offer annual screening ultrasound to women 50–69 years of age and biannual screening for women 40–49 years of age, since incidental benign abnormalities are more commonly encountered in younger women. The proposed methodology of using whole breast ultrasound is a novel one and its efficacy can only be validated by conducting large-scale observational studies. The aim of screening breast ultrasound would be mainly to identify stage I breast cancers, i.e., an invasive breast cancer that is less than or equal to 2 cm (T1), with no regional (axillary) lymph node metastasis (N0) and no distant metastasis (M0).
Screening sonography (ultrasound): handheld ultrasound screening. Handheld ultrasound examinations are used in most of the world—including Asia, Australia, South America, and parts of Europe—as a tool for screening for breast cancer. Handheld ultrasound has the advantages of being portable and not requiring elaborate base requirements as with mammography. All that is needed is a 110 V or higher electrical supply. However, there are significant problems in this manner of screening. Because there is no permanent record of the entire procedure, the study must be done by a skilled reader, usually a physician, who interprets the study as she is doing it. A less educated technician cannot be used, since she would have to interpret the results with her insufficient knowledge of the appearance of cancer. Ultrasound machines were designed for diagnosis rather than detection. This design prevents optimum imaging during breast screening, which is a pure detection task.
The ultrasound-machine monitors display very enlarged images suitable for review one-at-a-time for diagnostic inspection. Since the goal of breast screening is, or at least should be, the discovery of 5 mm or larger cancers anywhere in either breast, the entire image on the monitor must fit in the eye of the reader-operator during the motion of the transducer, since a 5 mm cancer may be anywhere in the image. While unique images are being displayed continuously, if the images are too magnified, eye movement will be necessary because of the eyes’ inability to subtend the entire image. Inevitably, this will result in information being missed by the reader. Similarly, children who sit in the front row at the cinema think they will see better than everyone else, but in reality they cannot see the entirety of the images on the screen and are therefore sitting in the worst seats in the house.
Hand scanning is usually performed too rapidly to allow sufficient persistence of a 5 mm cancer for recognition on the monitor. The magnification of the lesion also decreases its contrast with the surrounding normal tissue. Typically, the contrast control on the ultrasound machine does not allow specifically for additional contrast in the grays between fat and cancer. If absolutely necessary in low resource countries, with insufficiently trained physicians or locations so remote that a fixed site with automated ultrasound for screening is not possible, then an alternative would be to simulate automated screening as much as possible by using a modified handheld technique. This possibility will be discussed in the recommendations that follow.
Automated whole breast ultrasound (AWBU). AWBU [24] is designed to find small cancers and to overcome the drawbacks of handheld screening. Although AWBU requires a fixed location for doing the examination, the advantages, described next, far outweigh this limitation.
The examination can be done by a minimally trained operator, since all the images are recorded for later review by a skilled reader, usually a physician who has been trained in breast ultrasound evaluation. The automated computer guidance is done by a machine (Fig. 16A.3) attached to the transducer of the ultrasound machine, which is detachable from the AWBU system, so that the ultrasound unit and the room can be used for diagnostic ultrasound of possible abnormalities found by AWBU and other tasks when breast screening is not being done.
The AWBU [30] system performs two of the four functions usually done by the operator of the ultrasound machine. The computer-driven arms (Fig. 16A.3) regulate the position and speed of the transducer as it passes over the breast. The angle of incidence of the transducer, and therefore the ultrasound beam, is controlled by the operator by means of a gimbal attached to the probe arm. The free-floating probe arm also allows the operator to apply the correct pressure on the breast to get optimum images.
Since the aim of AWBU is to record sufficient images for recognition of 5 mm invasive cancers anywhere in either breast, computer control of the gathering of the images is necessary to assure complete coverage of the both breasts. The speed of the transducer is synchronized to the generation of unique images, so that about 5 or 6 images will be recorded through a 5 mm cancer anywhere in the breasts. At the proper playback speed, the visual dwell time for a cancer this size will be about half a second, more than enough time for recognition of the abnormality (Fig. 16A.4). The images are gathered in linear rows with about 7 mm overlap of contiguous rows (Fig. 16A.5). Because this pattern results in the least redundancy in scanning compared with a radial or anti-radial pattern, it is the quickest method to obtain complete breast coverage.
Because the location of all points in a breast can be calculated precisely relative to the nipple, the position of any abnormality identified by AWBU can be easily found on a later handheld ultrasound for follow-up or biopsy. Since the complete AWBU is stored permanently, comparison of a newly recognized finding with any previous examination is possible.
3D automated breast ultrasound (ABU). This type of automated ultrasound is performed with a single craniocaudad sweep from the subclavicular region to the inframammary fold with a 15 cm automated transducer. The patient examination is quicker to perform. 3D-ABU was not specifically designed to find 5 mm cancers. It is not a whole breast examination in that the axillary tail and lower axilla are not visualized completely. To obtain complete coverage, it depends on mammography to clear those areas [31].
The piezoelectric sensors (ultrasound recording elements) in a 3D-ABU 15 cm wide probe are further apart than in a typical 5 cm high frequency transducer. The 2D-ABU images, which are used for the 3D reconstructions, are almost three times further apart than AWBU images, 2.3 mm v 0.8 mm. Both of these factors reduce the sharpness and conspicuousness of small masses in the image stream or ciné. The ABU requires a sophisticated work station for 3D reconstructions. The file size of about 1 GB requires more expensive computer hardware to display and store these files. AWBU files are usually between 1/10 and 1/6 the size of the 3D-ABU files. At this time, there are no published, peer-reviewed, and multi-institutional studies of 3D-ABU. Consequently, the clinical results with this method are uncertain and are not comparable to AWBU.
Results of handheld and AWBU screening. There have been two large multi-institutional, published, peer-reviewed breast ultrasound screening studies performed, one handheld (ACRIN 6666) [26] and the other automated [23] (Table 16A.1). The handheld examinations were performed and read by academic radiologists specializing in breast imaging. The subjects in this study were all at high risk for breast cancer. Over half of these women had breast cancer previously. Of the cancers found, the authors did not state how many of the cancer recurrences were at or near the original surgery site. The cancers in the area of the previous cancer, although counted as screening discoveries, are, in another sense, not truly screening discoveries, since the locations of the scars are known and these areas will be explored more thoroughly as an area of great interest, as opposed to the rest of the breast tissue. The radiologists did well. They found 55 % more invasive breast cancers than mammography alone. The average diameter of the cancers was 1.2 mm. The average time to complete the scan was 19 min. Obviously, the radiologist must be available when the patient is present. A person of less training cannot do the scan because the detection of cancer occurs during scanning. If a technologist or a technician does not detect the cancer, it will not be in the images given to the radiologist. Also, the viewing at the bedside of a highly magnified image is not ideal for recognition of abnormalities. Interaction with the patient and the ultrasound machine are distracting. The proper transducer speed for identification of a 5 mm abnormality is about ½ cm per second. Handheld scanning is much faster and allows less than the ½ s necessary to recognize this size cancer. Unfortunately, the biopsy PPV for cancer was only 9 %, considerably less than what is customary in most major breast centers in the United States. Although not stated in the ACRIN article, there are probably two reasons for this low PPV.
All the women in the study were either at high risk for developing or already had had breast cancer, and they were understandably worried about developing another one. These women knew that the radiologists scanning them were the decision makers. It is my supposition that, during the scans, the radiologists might have stopped to look at difficult areas of breast tissue to clear them, and the women would notice and immediately ask “Can you biopsy this?” before the radiologist was even certain there was a true abnormality present. Once the biopsy question arises, it is hard to dissuade the nervous patient. These radiologists were not used to being put in this position, since they were not screening patients in their daily practice.
However, with screening mammography and diagnostic ultrasound, the radiologist has time to evaluate the imaging studies and formulate a plan before speaking to the patient. Consequently, with experience, the PPV of biopsy for screening ultrasound findings should be similar to the departmental PPV for diagnostic evaluation of breast abnormalities found mammographically or physically.
The AWBU study published in European Radiology in 2010 [23] found that the number of cancers doubled and the number of 1 cm or less invasive cancers tripled from 7 to 21 when AWBU was added to mammography. The cancers found by AWBU average 1.0 cm compared with handheld ultrasound’s average diameter of 1.2 cm, a three quarter larger volume (Table 16A.2). Duffy and colleagues [18] estimated that only about 10 % of women with breast cancers presenting up to 1.4 cm would die of their disease within 20 years (Fig. 16A.6). An advantage of AWBU is that the examinations, if done efficiently, can be conducted by lower trained personnel in about 15 min. Subsequent reading time by physicians trained in breast imaging is about 5–7 min [23].
Recommendations for Early Detection of Breast Cancer in LR Countries
Of the three possible methods of breast screening—clinical breast examination, screening mammography, and screening ultrasound—ultrasound will generally find cancers small enough that they may be cured by surgery alone, without radiation or chemotherapy, at a considerably less cost than screening mammography. This is an important consideration, since the LR countries have no practical way of obtaining significant amounts of these treatment modalities in the foreseeable future.
Mass Screening with Automated Whole Breast Ultrasound
In LR countries, maximum throughput will be important to minimize costs. AWBU will outperform handheld ultrasound, since the operator can be a lower skilled worker than the reader of the examination. The operator will be able to perform about four procedures an hour. A proficient reader can read about ten studies an hour, but will probably need to switch off about every 2 h to other less visually intensive tasks, such as diagnostic ultrasound or ultrasound-guided biopsies. If done efficiently, the AWBU procedure can be performed in about 15 min. Operating 6 days a week and 10 h a day, about 12,500 examinations could be performed annually per AWBU unit and ultrasound machine. If the prevalence of ultrasound-discoverable breast cancer were as high as the United States (6 per thousand) [23], as many as 60 cancers would be found the first year and probably 30 in the subsequent biannual rounds. In the United States, the annual incidence rate of breast cancer is about 0.3 % found at annual mammography. In China, the incidence rate appears to be about one-fourth that of the United States, but in the major cities the rate is rising and now may be nearly half the US rate. In that case, about 15 cancers would be found both in the first year and each succeeding biannual examination by each AWBU unit. The death rate from breast cancer over the next 20 years for women whose cancers were found at less than 1.5 cm would be about 10 %, compared to 40 % for cancers otherwise found. Although some uncertainty exists, probably beginning with the second round of screening 80 % of the cancers could be identified when they are less than 1.5 cm.
For a country with a high population density and a highly organized health-care system, the most efficient method for breast screening would be regional breast centers (Fig. 16A.7) distributed geographically throughout the country. Each regional center would be the diagnostic and treatment center for that geographic area. It would be staffed by radiologists reading the ABWUs done at multiple satellite screening centers throughout the geographic area as well as evaluating and needle-biopsing discovered abnormalities. The center’s surgeons would perform lumpectomies or mastectomies on the women with cancer. The staff at the satellite screening centers would perform the AWBU examinations and transmit the data electronically or physically to the regional breast center for interpretation. The operators of AWBU equipment would need only minimal training. If each satellite breast center had four AWBU units, it would examine about 100,000 women each year. If the women had examinations every other year, 200,000 eligible women would be screened. Given that half the population is male and about half the female population is not between the ages of 35 and 75, with a compliance rate of 80 %, each satellite screening center could serve a general population of 1,000,000.
If each regional center had ten satellite centers, the center would read about 1,000,000 AWBUs annually and serve a base population of 10,000,000. As an example, for China to screen the entire country in this manner, it would have to create 130 regional centers to serve a population of 1.3 billion, of which 260 million would receive an AWBU biannually. In 2008, the annual number of new breast cancers in China was about 169,500 [32]. The increase of population plus the increase of the breast cancer rate are estimated at about 4.5 %, which, compounded over 4 years to 2012, would suggest that the number of cancers found in 2012 will be 203,400.
The estimate of 52,800 deaths for this year will underestimate the 20-year cumulative deaths for cancers discovered this year because 52,800 deaths are from cancers that were found anywhere from 1 to 20 years before, when the annual numbers of cancers were considerably smaller. Truer estimated 20-year mortality would be based on the average diameter of the cancer at discovery, probably about 3.0 cm for China. Using Dr. Tabár’s 20-year longevity data (Fig. 16A.6), 40 % (81,360) of the 203,400 women learning they have breast cancer this year will die of this disease within 20 years if no effort at screening is made. Assuming 80 % biannual attendance of the eligible women at AWBU screening and that 80 % of the cancers are found at 1.4 cm diameter or less in these women, the death rate at 20 years would be reduced in those women from 40 to 10 %, since almost all these sonographically found cancers would be stage 1 with no lymph node involvement. Of the 130,176 women with cancers found at this size, 13,028 would be expected to die of breast cancer in 20 years. The other 20 % of attendees’ cancers (32,544) would be found smaller than without AWBU, at probably 1.5–3 cm in diameter, with 20 % mortality expected at 20 years instead of 40 % (6,509). Obviously, the 20 %, who were non-attendees (40,680) and did not have their biannual AWBU screens would ultimately have a 20-year mortality rate of about 40 % (16,272). The overall result would be that instead of 81,360 women dying of their breast cancers within 20 years, only 36,809 would die and 55 % (44,551 women) would be saved. If 100 % attendance were achievable, theoretically the 20-year mortality would drop under 25,000.
Handheld Ultrasound Screening
In countries where there are not sufficient trained physicians for centralized reading of AWBUs or where transportation is not available to bring women to a screening facility or where there is inadequate governmental organization and/or funding to set up such facilities, handheld ultrasound screening remains a less efficient and less accurate option. To overcome the problems with handheld screening in the past, the technique had to be modified to mimic AWBU. The scanning must be done methodically and slowly so that sub-centimeter cancers can be seen. The rate of movement of the transducer must be approximately 1 cm per second. The operator should not interact with the woman during the scan so as not to be distracted. Any discussion should be done before or after the scan. The screening should be done in a fixed grid, radial, or anti-radial pattern (Fig. 16A.8) so that all the tissue is seen well once. Repetition only serves to increase the time of the scan and to put pressure on the operator to scan faster. With the least overlap, the grid pattern is the quickest and the easiest to learn. The retro-areolar areas and the axillae should be examined separately. Any area in question should be marked on the skin and examined as a diagnostic study at the end of the screening study so as to not interrupt the screening examination. Depending on breast size, the handheld screening examination will require between 10 and 20 min.
Grid; slightly overlapping craniocaudad rows from the infraclavicular line to the inframammary fold; circular: series of overlapping circles surrounding the nipple; radial: radial scans extending from the periphery of the breast to the nipple (modified with permission of Elsevier from Kelly KM, Richwald GA. Automated whole breast ultrasound: advancing the performance of breast cancer screening. Semin Ultrasound CT MRI 2011;32:273–80)
Clearly, the personnel performing the screening will need considerable training, which will take between 3 and 6 months. The personnel should be female, since the testing is being done away from a clinical setting. Because the operator is travelling to the women to be screened, any other testing necessary, such as Pap smears, should be done at the same time. These women also need to be able to recognize abnormal breast findings. This requires intensive instruction on how cancer appears sonographically. Fortunately, there are teaching cines that may be available from AWBU sites that simulate handheld scanning. Any country planning on implementation of such a program must be committed to the training and oversight that would be necessary.
Because of the difficulty of bringing women with any findings to a medical facility, the technician must be able to determine if the woman has cancer. Consequently, the technician will need to be able to do an ultrasound directed 14g needle biopsy or at least a FNA. In order to do either of these tests, the technicians need to learn basic sterile technique and limited local anatomy.
The advantage of a FNA is that it is safer and cheaper than a core needle biopsy, but it is more difficult to obtain a satisfactory specimen and to preserve the specimen correctly. The evaluation of the specimen requires an experienced cytologist, who may not be available in a very low resource setting. A 14 or a 16g biopsy delivers a better and more accurate specimen. It requires only immersion in formalin for preservation. It is more easily evaluated by a hospital pathologist, even in LR countries. However, the biopsy must be performed in a safe manner and is less forgiving of errors in technique. A disposable 14g needle is only a few dollars when used with a non-disposable spring-loaded gun.
Improved Therapy for Breast Cancer
Clearly, low resource countries are woefully lacking as regards the relatively recent advances in radiation and chemotherapy. Education of the medical providers and technical infrastructure is minimal in those countries. In the few places that they do exist to some degree, they are usually restricted to the influential and wealthy. What little capital is available is better spent on prevention and early detection.
Conclusion
Although in most developing countries there is minimal funding for programs to mitigate the effect of breast cancer, particularly in young women, early detection by sonographic discovery while the cancers are small enough that survival is highly probable even without radiation or chemotherapy is a feasible strategy for the future. Implementation of a HPV vaccination program would markedly lower the future incidence of cervical cancer in the young women who received their immunizations in their pre- and early teens. An unexpected bonus from a vaccination program may be a significant reduction of the disproportional incidence of breast cancers expected in these young women. Whole breast ultrasound may be a cost-effective alternative to organized screening mammography in view of lower prevalence of the target cancer and the massive investment in infrastructure and health-care personnel that would be required to implement a mammographic screening program. Unlike mammography, screening using sonography will aim to identify Stage I cancers; mortality rate reduction is unlikely to be ever proved with use of sonography. Use of sonography will need to be validated by undertaking observational studies in a large cohort of asymptomatic women. If the one drawback of the expected higher false positive rate with use of ultrasound can be overcome, sonography may very well prove to be a feasible low cost alternate to screening for breast cancer in developing countries.
B. Future Strategies for Cervical Cancer Prevention in Developing Countries: HPV Vaccine and Its Implementation Around the World
Abstract
Cervical cancer prevention is a feasible option to control cervical cancer in low resource countries. In this chapter, the etio-pathogenesis of cervical cancer is presented. The types and role of HPV vaccine in cervical cancer prevention are discussed. The future strategy in preventing cervical cancer screening utilizing HPV cervical cancer vaccine is outlined.
Introduction
The human papillomavirus (HPV) infection is the most common sexually transmitted disease [1, 2]. According to the World Health Organization, there are approximately 440 million people affected by genital HPV infection around the world [3]. Among all diseases that HPV may cause, the one that has the greatest impact to public health is cervical cancer. Almost half a million cases globally are recorded annually, and 85 % of all the cases occur in developing countries. The highest incidences of the disease are recorded in Latin America, the Caribbean, Sub-Saharan and South Africa, and Southeast Asia [4, 5]. The World Health Organization estimates that cervical cancer cases will increase significantly in the coming years if no additional measures are taken, estimating that in the year 2030 around 775,000 new cases and 440,000 deaths will be recorded as a result of such tumors [6].
High-risk HPVs are not only linked to cervical cancer, but also to other types of cancer such as vulva, vagina, penis, anal canal, mouth, and oropharynx [7, 8]. However, even viruses considered to be “low risk” have some carcinogenic potential, although it is less common to see cancer caused by such viruses [9].
The Papanicolaou test, introduced in the 1950s as a cervical cancer screening method, is traditionally considered an example of a successful strategy for secondary prevention of cancer. Several countries reported dramatic reductions in the incidence and mortality coefficients due to cervical cancer after its implementation. But this phenomenon was observed especially in developed countries. In developing countries, cervical cancer screening programs did not present good results due to the low coverage offered by the Pap smear exam, poor quality of the cytological exam, and difficulty in getting access to health services [10]. These data justify the need for the incorporation of new strategies in the fight against cervical cancer.
One such strategy would be the use of an HPV vaccine in the primary prevention of cervical cancer. According to a manifesto by the World Health Organization in 2009: “…routine HPV vaccination should be included in national immunization programs, provided that prevention of cervical cancer or other HPV-related diseases, or both, constitutes a public health priority; vaccine introduction is programmatically feasible; sustainable financing can be secured; and the cost effectiveness of vaccination strategies in the country or region is considered” [11].
However, critics argue that there is not enough evidence to conclude that the HPV vaccine will bring an effective reduction in the incidence of and mortality caused by cervical cancer. In order to achieve that, a period of 20–30 years would be necessary, since cervical cancer has a long natural history. Nevertheless, data from the Australian HPV vaccination program reinforce the idea that the HPV vaccine can be a tool for the primary prevention of cervical cancer. Brotherton and colleagues [12] showed a significant reduction in the incidence of high-grade cervical cytological abnormality in young Australian women. Since the natural history of cervical cancer is well known, one could infer that the reduction in the incidence of precursor lesions in cervical cancer will have a direct impact on the incidence of cervical cancer in the future. It is estimated that the HPV vaccine may reduce by 80 % the chance of cervical cancer developing during a woman’s lifetime [11].
HPV Vaccines
Currently, there are two versions of the HPV vaccine, both of them developed with recombinant technology. They do not carry a live or attenuated virus or genetic material; therefore, they are not able to induce infection. Vaccines are comprised of VLP (virus-like particle), a particle similar to the virus capsid from the structural point of view [8, 13]. The quadrivalent vaccine (Gardasil® or Silgard®, Merck & Co, Whitehouse Station, NJ) protects against viruses 6, 11, 16, and 18, and the bivalent vaccine (Cervarix®, GlaxoSmithKline, London, UK) protects against viruses 16 and 18. One should remember that 70 % of cervical carcinomas are caused by types 16 and 18, and 90 % of genital warts by types 6 and 11. Both vaccines must be administered intramuscularly in three doses during a period of 6 months. The recommendation for the quadrivalent vaccine is that the second dose should be administered 2 months after the first dose and the third dose be administered sixth months after the initial vaccination. For the bivalent vaccine, the second dose is recommended 1 month after the initial dose. The current indication on the use of bivalent and quadrivalent vaccines approved by the Food and Drug Administration (FDA) is shown on Table 16B.1 [14].
There are no doubts regarding the safety of the bivalent and quadrivalent vaccines or their effectiveness in the prevention of precursor lesions of cervical cancer [15–21]. The effectiveness of the vaccine is close to 100 % for the prevention of cervical intraepithelial lesions, and, in the case of quadrivalent vaccine, it also protects condyloma, vulvar, and vaginal intraepithelial lesions. The effectiveness of the quadrivalent vaccine decreases if women had a previous or have an infection by HPV at the time of vaccination [7]. Vaccines must be used only with a prophylactic intent, with no indication of treatment in cases of already established HPV-induced lesions [8]. Vaccines decrease the risk of precursor lesions, but they do not eliminate completely this risk since immunization does not cover all types of high-risk HPV. Thus, cervical cancer prevention by way of a Pap smear examination is still necessary even for those women that have been previously vaccinated for HPV [13].
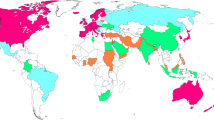
Bivalent and quadrivalent vaccines have already been approved for use in more than 100 countries. However, not all countries included them in their public immunization program. Besides having questions about the best method of implementation, the cost of the vaccines itself is a relevant barrier for several countries, especially for low-income countries. Table 16B.2 highlights countries with national funding programs through mid-2012.
Vaccination Strategy
One of the challenges to be overcome in HPV immunization programs is the age group that will receive the vaccine: teenagers. It is common knowledge that teenagers, especially the older ones, are less receptive and less adherent to vaccination programs. In the United States, for example, the overall coverage rate in 2009 among teenagers ranging from 13 to 17 was approximately 50 % for boys and 33 % for girls [22].
Currently, the discussion focuses on what would be the best strategy for the vaccination of teenagers: a school-based approach or one based on the health system. The European Centre for Disease Prevention and Control declared that school-based immunization: “…is likely to be the lowest cost option for the delivery of human papillomavirus (HPV) vaccines to preadolescent girls. However, local issues, such as whether school-based health services exist, funding arrangements for vaccine purchase and administration and obtaining parental consent may affect the feasibility of this approach” [23]. Regarding the immunization programs based on the health system, they considered that “a universally available additional or alternative option for HPV vaccine delivery. This may be more expensive than school-based immunization and monitoring of vaccine uptake may be more difficult here” [23].
It may be that no one single vaccination strategy is better than the other, but one strategy could be more adequate than the other according to each individual regional reality. The available literature provides examples of public HPV immunization programs that both succeeded and failed when each of the immunization strategies was applied.
Australia
The first country in the world to establish a national public HPV immunization program was Australia. In April 2007, they started the regular school-based vaccination program targeting girls aged 12–13. However, two other catch-up programs ran only up to December 2009, one of them being school-based and the other community-based. Women up to 17 years of age were vaccinated in schools, and older women or women who missed vaccination at school were vaccinated at community health agencies [24]. This particular program determined relatively high coverage rates for the school-based program [25]. The data presented by the Australian government may be seen on Table 16B.3. As of 2013, boys aged 12–13 will also be included in the school-based vaccination program.
Europe
Austria was one of the first countries in the world to have national immunization recommendation against HPV. Despite being the first country with regard to the recommendation, the country itself has never had a public policy for funding the vaccine. On the other hand, the majority of the European Community countries currently count on government funding for the HPV vaccine [26]. Different vaccination strategies were adopted in Europe, with considerable variation regarding targeted age groups, catch-up programs, and type of vaccine. There is also a considerable variation in relation to the vaccine delivery, where the majority of programs are based on the health system (public or private). Few European countries adopted the school-based strategy for their vaccination programs. Table 16B.4 displays a summary of several European HPV vaccination programs.
In most European countries where the vaccine is given on demand, the general vaccine coverage rates are invariably lower than 90 %. In some countries, such as Belgium, the Netherlands, Germany, France, Norway, and Luxemburg, coverage rates are near or lower than 50 % [14, 26]. A few of the nonschool-based programs, such as the one in Denmark, reached higher coverage rates; the rate reached 80 % for the first dose of the vaccine for 12-year-old girls.
The Americas
Although the HPV vaccine has largely been approved for use in the United States and in the Caribbean, very few countries within this region have adopted public funding policies as of mid-2012, namely, United States, Canada, Mexico, Panama, Argentina, Puerto Rico, and the Guyana.
In the United States, bivalent and quadrivalent vaccines were approved for use in 2006 and 2009, respectively [14]. Currently, the country does not present a public funding program for the immunization of uninsured woman aged 21 or older. It is worth mentioning that, in the United States, 13 % of women between ages 9 and 18 and 27 % of those aged 19–26 are uninsured [27]. Uninsured girls up to the age of 18 benefit from the Vaccines for Children (VFC) Program [28]. This is a federal program that finances vaccines approved by the ACIP (Advisory Committee on Immunization Practices). Through this program, the CDC (Centers for Disease Control and Prevention) buys the vaccine directly from the manufacturer and distributes them to state health departments and public health agencies, which transfer the vaccines, at no cost, to public health clinics and to physicians’ offices [29]. There are three additional public financing programs for women or girls who do not benefit from the VFC, namely, Immunization Grant Program, Medicaid, and State Children’s Health Insurance Program [28]. In spite of these public immunization funding programs, the HPV vaccine coverage rate for one or more doses is only 45 % among North American girls [22]. It is worth mentioning that none of the described programs has a school-based approach.
In Canada, the quadrivalent vaccine was approved in July 2006 for women aged 9–26. The approval for the bivalent vaccine occurred in February 2010, for women aged 10–25. In an unprecedented way, in April 2011, Canada approved the quadrivalent vaccine for women up to 45 years of age, and in May 2011, the use of the quadrivalent vaccine for men aged 9–26 was approved [7]. In 2007, the Canadian government expended about 300 million dollars to provinces and territories as an incentive for an HPV national immunization program [30]. All provinces and territories have introduced HPV vaccine programs for adolescent girls into their immunization schedules since 2008. Noteworthy is the fact that each province/territory has its own HPV immunization program, but, in all those programs, vaccines are provided free of charge to girls through school-based clinics administered by local public health units [7]. Table 16B.5 shows the summary of HPV immunization programs in Canada. During the first year of the immunization program, coverage rates were variable: Newfoundland (85 %), Ontario (53 %), and Quebec (84 % for grade 4 and 87 % for grade 9). The coverage rate for the Atlantic provinces was approximately 80 % [31].
In Latin America, information regarding HPV vaccination is still insufficient. As of mid-2012, only Mexico, Panama, and Argentina had implemented HPV public immunization programs. Of these countries, only Mexico showed data published about the HPV immunization program. The Mexican HPV vaccination program deserves mention because of the way it was implemented. In Mexico, the vaccine was approved for use in 2008. The HPV public immunization program did not cover the whole territory initially but only cities displaying the lowest human development index. This represented only 5 % of country’s population. This program achieved a coverage rate of 85 % for the first dose in girls aged 9–12 (2009). In 2011, the Mexican government expanded the vaccination program to the entire country and included a school-based vaccination strategy for 9-year-old girls [32].
Until mid-2012, Brazil, the largest country in Latin America, had not implemented a public immunization program. Although quadrivalent and bivalent vaccines have been approved in Brazil in 2006 and 2008, respectively, at that time, both vaccines were available only in the private sphere. Nevertheless, a few municipalities by local political decision decided to offer the HPV vaccine for free. This was the case in São Francisco do Conde (BA), Campos de Goitacazes (RJ), Araraquara (SP), and Itu (SP). The first two municipal districts followed a school-based strategy, while the latter two opted for a local public health system strategy. None of these programs have data published regarding the coverage rates.
Barretos, a small Brazilian municipal district located in the state of São Paulo (southeast region of Brazil), recently participated in a school-based HPV vaccination demonstrative study. The study was designed and carried out by the Barretos Cancer Hospital, and it included girls attending sixth and seventh grades (average age: 12) enrolled in public and private schools in the city. From a total of 1,513 candidates for the immunization program, parents or legal guardians of 1,389 kids accepted participation for their girls in the program (91.8 % acceptance rate). The main reason reported by parents or guardians for refusing to participate was the fear of adverse events caused by the vaccine. The study confirmed high coverage rates for the three doses: 87.5 % (first dose), 86.3 % (second dose), and 85.0 % (third dose) (author’s personal information). Peru also performed a demonstrative study involving a school-based vaccination strategy. This study involved approximately 8,000 girls attending the fifth grade and achieved a 88.9 % vaccination-coverage rate [33].
Funding for Vaccination Programs in Developing Countries
One of the main problems related to the HPV vaccine in developing countries is the cost of the vaccines. Mathematical models suggest that the HPV vaccine would be cost effective in low- and middle-income countries only if the three doses of the vaccine had a maximum cost of US$25 [11]. Considering that each dose of the vaccine has an average cost of U$120 [1], the magnitude of the problem can be appreciated. It is estimated that there are approximately 52 million 11-year-old girl candidates for HPV in developing countries and about seven million in developed countries [34]. Thus, low-income and many middle-income countries will have trouble implementing the HPV vaccine in the absence of a supporting funding program [29].
The main supporting funding programs currently available for the HPV vaccine are the ones described in the next sections.
GAVI Alliance (Global Alliance for Vaccines and Immunization)
Founded in 2000, this alliance is a public–private partnership with a global sphere of action whose main goal is to promote health through access to vaccines in countries that have low economic resources. Only countries with a gross national income lower than or equal to US$1,520 in 2009 (by the World Bank’s classification) are currently candidates for GAVI’s programs. According to such criteria, there are currently 57 GAVI-eligible countries (Table 16B.6). The alliance is comprised of members from the World Health Organization, UNICEF, the World Bank, pharmaceutical industries, research agencies, civil society, the Bill and Melinda Gates Foundation, the International Finance Facility for Immunization, in addition to developing country governments and donor governments. Today, the GAVI Alliance is the largest source of external funding for several immunization programs around the world [35]. In November 2011, complying with the demand of developing countries, the alliance included the HPV vaccine in their vaccine list. At this time, the quadrivalent vaccine manufacturer announced that they could supply the vaccine at a cost of US$5 per dose for the GAVI Alliance. In 2012, GAVI opened a round of applications for vaccine demonstration programs [36, 37].
Pan American Health Organization Revolving Fund
The Pan American Health Organization (PAHO) serves as the Regional Office of the World Health Organization in the Americas, and it provides a program for the acquisition of vaccines, syringes, and other immunization equipment for their 48 member countries. Countries pay for the vaccine, the cost of which is widely negotiated by PAHO with the manufacturers at a low price [36, 38]. In January 2010, the bivalent vaccine was offered to PAHO for a price of US$32. However, since then, there has been a significant reduction in vaccine prices. In 2012, the average prices for bivalent and quadrivalent vaccines offered to PAHO were US$13.48 and US$14.25, respectively [38]. The PAHO Revolving Fund is not truly a funding program, but it allows for a considerable price reduction for the cost of the vaccines for member countries.
Gardasil Access Program
The Axios Healthcare Development, a US nonprofit organization, manages the Gardasil Access Program (GAP). Through this program, Merck & CO has pledged to donate at least three million doses of the quadrivalent vaccine to organizations or institutions in developing countries. The guidances are provided by an independent advisory board comprised of public health experts. To date, more than a million doses of quadrivalent vaccine were donated to 22 participants in 20 countries (Bolivia, Kiribati, Honduras, Haiti, Guyana, Mali, Ghana, Cameroon, Lesotho, Tanzania, Kenya, Uganda, Georgia, Moldova, Uzbekistan, Nepal, Mongolia, Buthan, Cambodia, and Papua New Guinea). In this program, the doses of vaccines are donations, but, on the other hand, the costs related to the importation and to the whole cold chain are the responsibility of the participating organizations and institutions [39, 40].
Summary
The development of vaccines for HPV provides a new perspective on the primary prevention of diseases induced by the virus, especially cervical cancer. Although both versions of the vaccine currently available have been approved for use in more than 100 countries, the number of countries that implemented HPV public immunization programs is much lower. It is paradoxical to observe that the majority of countries that have an HPV immunization program already implemented are high-income countries with low cervical cancer incidence coefficients. Conversely, low- and middle-income countries, the ones with the greatest need for the vaccines, currently have limited access to the vaccines because of the high cost. Reduction of the vaccine cost is fundamental. Programs that provide financial support, such as GAVI Alliance and PAHO Revolving Fund, are essential for the implementation of HPV immunization programs in countries that have few economic resources. Additionally, the development of a second generation of HPV vaccines, created using new production technologies at a lower cost, will make it easier to incorporate the vaccine in low- and middle-income countries.
References
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozao R, Lopez AD, Murray CJ, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378(9801):1461–84.
Pavelic L, Pavelic K, Vuk-Pavelic S. Human mammary and bronchial carcinomas in vivo and in vitro secretion of substances immunologically cross-reactive with insulin. Cancer. 1984;53:2467–71.
Ziegler RG, Anderson WF, Gail MH. Increasing breast cancer incidence in China: the numbers add up. JNCI. 2008;100:1339–41.
Polyak K. Breast cancer: origins and evolution. J Clin Invest. 2007;117:3155–63.
Satyaraj E. Emerging paradigms in immunonutrition. Top Companion Anim Med. 2011;26(1):25–32.
Farmer H, McCabe N, Lord C, Tutt AN, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–21.
Bittner JJ. Some possible effects of nursing on the mammary gland tumor incidence in mice. Science. 1936;84:162.
Ross SR. Mouse mammary tumor virus molecular biology and oncogenesis. Viruses. 2010;2:2000–12.
Akil N, Yasmeen A, Kassab A, Ghabreau L, Darnel AD, Moustafa A-E. High-risk human papillomavirus infections in breast cancer in Syrian women and their association with Id-1 expression: a tissue microarray study. Br J Cancer. 2008;99:404–7.
Kroupis C, Markou A, Vourlidis N, Dionyssiou-Asteriou A, Lianidou ES. Presence of high-risk human papillomavirus sequences in breast cancer tissues and association with histopathological characteristics. Clin Biochem. 2006;39:727–31.
Hariri S, Unger ER, Sternberg M, Dunne EF, Swan D, Patel S, et al. Prevalence of genital HPV in the among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. J Infect Dis. 2011;204(4):566–73.
Shenefelt PD. Nongenital warts. Medscape Reference Drugs Disease & Procedures. 2012. http://emedicine.medscape.com/article/1133317-overview
Khan S, Jaffer NN, Khan MN, Rai MA, Shafiq M, Ali A, et al. Human papillomavirus subtype 16 is common in Pakistani women with cervical carcinoma. Int J Infect Dis. 2007;11(4):313–7.
Center for Communicable Diseases. Epidemiology and prevention of vaccine-preventable diseases: human papillomavirus. The pink book: course textbook, Ch 10, 12th ed. Washington, DC: Public Health Foundation; 2012. p. 139–49.
Clifford GM, Smith JS, Aguado T, Franceschi S. Comparison of HPV type distribution in high-grade cervical lesions and cervical cancer: a meta-analysis. Br J Cancer. 2003;89:101–5.
Barth AJ Jr, Gibson GR, Mott LA, Becher RD, Poplack SP. Detection of breast cancer on screening mammography allows patients to be treated with less-toxic therapy. AJR. 2005;184:325–9.
Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:727–37.
Duffy SW, Tabár L, Vitak B, Warwick J. Tumor Size and breast cancer detection: what might be the effect of a less sensitive screening tool than mammography? Breast J. 2006; 12 Suppl 1:S91–5.
Yu Y-H, Wei W, Liu J-L. Diagnostic value of fine-needle aspiration biopsy for breast mass: a systematic review and meta-analysis. BMC Cancer. 2012;12:41.
Ljung BM, Drejet A, Chiampi N, Jeffrey J, Goodson WH 3rd, Chew K, et al. Diagnostic accuracy of fine-needle aspiration biopsy is determined by physician training in sampling technique. Cancer. 2011;93(4):263–8.
Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011;260:658–63.
Keen C. SSPs take on larger role in digital mammography. Hefty data sets and multiple prior images threaten to put a strain on standard storage and network options. Diagnostic Imaging. 2005;27:S-23–31. http://www.diagnosticimaging.com/display/article/113619/1197582. Cited 17 Aug 2012.
Kelly KM, Dean J, Comulada WS, Lee S-J. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010;20:734–42.
Elmore JG, Armstrong K, Lehman CD, et al. Screening for breast cancer. JAMA. 2005;293:1245–56.
Nothacker M, Duda V, Hahn M, et al. Early detection of breast cancer: benefits and risks of supplemental breast ultrasound in asymptomatic women with mammographically dense breast tissue: a systematic review. BMC Cancer. 2009;9:1–9.
Berg WA, Blume JD, Cormack JB, et al. Combined screening with ultrasound and mammography vs. mammography alone in women with elevated risk of breast cancer. JAMA. 2008;299:2151–63.
Tohno E, Ueno E, Watanabe H. Ultrasound screening of breast cancer. Breast Cancer. 2009;16:18–22.
Kuhl CK. The “coming of age” of nonmammographic screening for breast cancer. JAMA. 2008;299:2203–5.
Tohno E, Takahashi H, Tamada T, Fujimoto Y, Yasuda H, Ohuchi N. Educational program and testing using images for the standardization of breast cancer screening by ultrasonography. Breast Cancer. 2012;19(2):138–46.
Kelly KM, Richwald GA. Automated whole-breast ultrasound: advancing the performance of breast cancer screening. Semin Ultrasound CT MRI. 2011;32:273–80.
Tabár L. Personal Communication. Santa Barbara, California. Summer 2011.
WHO International Agency for Research on Cancer. Breast cancer incidence and mortality worldwide in 2008 summary. 2008. http://globocan.iarc.fr/factsheets/cancers/breast.asp. Cited 17 Aug 2012.
References
Saslow D, Castle PE, Cox JT, Davey DD, Einstein MH, Ferris DG, et al. American Cancer Society Guideline for human papillomavirus (HPV) vaccine use to prevent cervical cancer and its precursors. CA Cancer J Clin. 2007;57(1):7–28.
Burchell AN, Winer RL, de Sanjose S, Franco EL. Chapter 6: Epidemiology and transmission dynamics of genital HPV infection. Vaccine. 2006;24 Suppl 3:S3/52–61.
WHO. Initiative for vaccine research (IVR)—viral cancer—HPV. World Health Organization. 2011. http://www.who.int/vaccine_research/diseases/viral_cancers/en/index3.html. Cited 30 Jun 2012.
Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001;2(9):533–43.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v1.2, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10. Lyon: International Agency for Research on Cancer; 2011. http://globocan.iarc.fr. Cited 30 Jun 2012.
Update on Human Papillomavirus (HPV) Vaccines. CCDR (Canada communicable disease report) 2012;38:1–62.
WHO. Human papillomavirus and HPV vaccines: technical information for policy-makers and health professionals. Geneva: WHO Press; 2007. p. 43.
WHO/ICO. Human papillomavirus and related cancers in world. Summary report update. October 9, 2009. WHO/ICO Information Centre on HPV and Cervical Cancer. 2009.
Parkin DM, Bray F. Chapter 2: The burden of HPV-related cancers. Vaccine. 2006;24 Suppl 3:S3/11–25.
WHO. Human papillomavirus vaccines. WHO position paper. Weekly Epidemiological Record 2009;15:118–31.
Brotherton JM, Fridman M, May CL, Chappell G, Saville AM, Gertig DM. Early effect of the HPV vaccination programme on cervical abnormalities in Victoria, Australia: an ecological study. Lancet. 2011;377(9783):2085–92.
Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56(RR-2):1–24.
FDA. Vaccines, blood & biologics. Vaccines. Approved products FDA; 2012. http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm172678.htm. Cited 2012 Jul 20, 2012.
Garland SM, Hernandez-Avila M, Wheeler CM, Perez G, Harper DM, Leodolter S, et al. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356(19):1928–43.
Villa LL, Costa RL, Petta CA, Andrade RP, Paavonen J, Iversen OE, et al. High sustained efficacy of a prophylactic quadrivalent human papillomavirus types 6/11/16/18 L1 virus-like particle vaccine through 5 years of follow-up. Br J Cancer. 2006;95(11):1459–66.
Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356(19):1915–27.
Paavonen J, Naud P, Salmeron J, Wheeler CM, Chow SN, Apter D, et al. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374(9686):301–14.
Lehtinen M, Paavonen J, Wheeler CM, Jaisamrarn U, Garland SM, Castellsague X, et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13(1):89–99.
Villa LL. HPV prophylactic vaccination: the first years and what to expect from now. Cancer Lett. 2011;305(2):106–12.
Villa LL, Costa RL, Petta CA, Andrade RP, Ault KA, Giuliano AR, et al. Prophylactic adrivalent human papillomavirus (types 6, 11, 16, and 18) L1 virus-like particle vaccine in young women: a randomised double-blind placebo-controlled multicentre phase II efficacy trial. Lancet Oncol. 2005;6(5):271–8.
Stokley S, Cohn A, Dorell C, Hariri S, Yankey D, Messonnier N, et al. Adolescent vaccination-coverage levels in the United States: 2006–2009. Pediatrics. 2011;128(6):1078–86.
Finn A. Strategy options for HPV vaccine delivery in EU countries. Guidance for the introduction of HPV vaccines in EU countries. Stockholm: European Centre for Disease Prevention and Control; 2008. p. 30–6.
Garland SM, Skinner SR, Brotherton JM. Adolescent and young adult HPV vaccination in Australia: achievements and challenges. Prev Med. 2011;53 Suppl 1:S29–35.
Immunise Australia Program. Human Papillomavirus (HPV). Information about the National Human Papillomavirus (HPV) Vaccination Program funded under the Immunise Australia Program.: Australian Government. Depatment of Health and Aging; 2011 [updated Apr 04, 2011]; http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/immunise-hpv#figure2. Cited 30 Jun 2012.
Dorleans F, Giambi C, Dematte L, Cotter S, Stefanoff P, Mereckiene J, et al. The current state of introduction of human papillomavirus vaccination into national immunisation schedules in Europe: first results of the VENICE2 2010 survey. Euro surveillance: bulletin europeen sur les maladies transmissibles = European communicable disease bulletin 2010;15(47).
HPV Vaccine: Implementation and Financing Policy. The Henry J. Kaiser Family Foundation. 2007. http://www.kff.org/womenshealth/upload/7602.pdf. Cited 2012.
The HPV Vaccine: Access and Use in the U.S.: The Henry J. Kaiser Family Foundation. 2011. http://www.kff.org/womenshealth/7602.cfm. Cited 2012.
IARC. Making cervical cancer vaccines widely available in developing countries: cost and financing issues. IARC. http://screening.iarc.fr/doc/IAVI_PATH_HPV_financing_brief.pdf. Cited 2012.
Smith LM, Brassard P, Kwong JC, Deeks SL, Ellis AK, Levesque LE. Factors associated with initiation and completion of the quadrivalent human papillomavirus vaccine series in an Ontario cohort of grade 8 girls. BMC Public Health. 2011;11:645.
Colucci R, Hryniuk W, Savage C. HPV vaccination programs in Canada: Are we hitting the mark? Report Card on Cancer in Canada [Internet]. 2010 Aug 11, 2012. Available from: http://www.canceradvocacy.ca/reportcard/2008/HPV%20Vaccination%20Programs%20in%20Canada.pdf.
Progress toward implementation of human papillomavirus vaccination--the Americas, 2006–2010. MMWR Morbidity and mortality weekly report 2011;60(40):1382–4.
LaMontagne DS, Barge S, Le NT, Mugisha E, Penny ME, Gandhi S, et al. Human papillomavirus vaccine delivery strategies that achieved high coverage in low- and middle-income countries. Bull World Health Organ. 2011;89(11):821–30B.
Saxenian H. HPV Vaccine Adoption in Developing Countries: Cost and Financing Issues: International AIDS Vaccine Initiative/Program for Appropriate Technology in Health (PATH). http://www.iavi.org/HPVreport. Cited 2007.
Garland SM. Human papillomavirus vaccination: where to now? Sex Transm Infect. 2011;87 Suppl 2:ii23–4.
GAVI Alliance. http://www.gavialliance.org/. Cited 2012.
GAVI. Human papillomavirus vaccine support. GAVI Alliance. http://www.gavialliance.org/support/nvs/human-papillomavirus-vaccine-support/. Cited 2012.
PAHO. PAHO Revolving Fund. Pan American Health Organization; Available from: http://new.paho.org/hq/index.php?option=com_content&task=view&id=1864&Itemid=2234&lang=en.
Bonanni P, Levi M, Latham NB, Bechini A, Tiscione E, Lai P, et al. An overview on the implementation of HPV vaccination in Europe. Hum Vaccin. 2011;7(Suppl):128–35.
Ladner J, Besson MH, Hampshire R, Tapert L, Chirenje M, Saba J. Assessment of eight HPV vaccination programs implemented in lowest income countries. BMC Public Health. 2012;12:370.
GAP. Gardasil Access Program. 2012. http://www.gardasilaccessprogram.org/section/141. Cited 4 Nov 2012.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Kelly, K.M., Shetty, M.K., Fregnani, J.H.T.G. (2013). Breast Cancer Screening and Cervical Cancer Prevention in Developing Countries: Strategies for the Future. In: Shetty, M. (eds) Breast and Gynecological Cancers. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-1876-4_16
Download citation
DOI: https://doi.org/10.1007/978-1-4614-1876-4_16
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-1875-7
Online ISBN: 978-1-4614-1876-4
eBook Packages: MedicineMedicine (R0)