Abstract
In this chapter, some challenging and interesting Electrophysiology cases done in Rajaie Cardiovascular, Medical and Research Center were discussed. These cases include some interesting SVT and AFL, AF, PVC and accessory pathway cases. In each case, differentiating maneuvers were discussed. Some of them are simple arrhythmia cases but there was a challenge in ablation due to anatomical causes. The first case was a patient with prosthetic valves with SVT. The patient was a case of severe MS, severe AS, AI, and severe TR for whom AVR and MVR and TVR was done; 1 day after the operation she had revealed a regular narrow QRS tachycardia that was degenerated to AF; Amiodarone was administrated for her; about 3 h later, she had demonstrated torsade de point and with D/C shock had been converted to NSR and had revealed that QT was prolonged (about 500 ms) so sulfate magnesium was administrated and an epicardial pacemaker was programed in 70 VVI 85 bpm; then she had demonstrated three more episodes of narrow QRS tachycardia, mostly compatible with AVNRT (Fig. 12.1).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
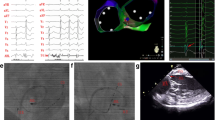
The patient was a case of rheumatic heart disease with severe MS, severe AS, AI, and severe TR for whom AVR and MVR and TVR was done; 1 day after the operation she had revealed a regular narrow QRS tachycardia degenerated to AF; Amiodarone was administrated for her; about 3 h later, she had demonstrated torsade de point and with D/C shock was converted to NSR and then revealed that QT was prolonged (about 500 ms) so sulfate magnesium was administrated and an epicardial pacemaker was programed in 70 VVI 85 bpm; then she had demonstrated three more episodes of narrow QRS tachycardia, mostly compatible with AVNRT (Fig. 12.1).
So we decided to ablate the arrhythmia, because we could not administer Beta-blocker or other antiarrhythmic drugs, due to long QT. EPS was done; we only used a decapolar catheter in CS, epicardial temporary pacemaker was programmed to VVI 60 bpm. With CS pacing a narrow QRS tachycardia infavor of AVNRT was induced and RFA in the posterosetpal area, between CS ostium and prosthetic tricuspid valve resulted in junctional rhythm and RFA continued for 1 min. Then Isuprel was administrated and arrhythmia was not inducible after ablation (Fig. 12.2a, b).
Discussion
AVNRT is the most common type of supraventricular arrhythmia and usually presents with no visible P wave in narrow QRS tachycardia [1,2,3].
In typical AVNRT there is a long AH interval (>180 ms) during tachycardia, and the earliest retrograde atrial activity is at the fast (Beta) pathway; at the superior part of Koch’s triangle, posterior to the Todaro tendon (Fig. 12.3) [4].
In most of the AVNRT patients, CS ostium is greater than normal subjects, and it may be a case of difference between slow and fast pathway conduction velocity and refractory periods and that could participate in the occurrence of AVNRT [5].
With HRA pacing prolongation of AH interval to more than 180 ms, is indicative of slow pathway conduction.
Some features of dual AV nodal physiology are as:
-
1.
More than 50 ms increase in AH interval with 10 ms decrease in A1–A2 interval with atrial extrastimulation (Fig. 12.4).
In addition to the more common type of the AVNRT (slow–fast) type, there are two another less common types as: slow–slow and fast–slow types, which include about 3% and 2% of all AVNRT cases respectively [6,7,8].
-
2.
Left-sided variant occur about 1.5% of all AVNRT cases who underwent ablation, and usually needs ablation from the left atrium (mostly via coronary sinuse). A short VA interval (<15 ms) and double response to atrial pacing are most frequent in this variant. The differential diagnosis of typical AVNRT is AT and orthodromic AVRT via the anteroseptal accessory pathway. There are frequent maneuvers for differentiation of them, such as Morady maneuver (ventricular entrainment and VAV response with PPI–TCL (Post-pacing interval—Tachycardia cycle length) difference more than 110 ms and SA-VA difference more than 85 ms (Fig. 12.5) [9, 10].
Atrial pacing at TCL and AH interval difference between atrial pacing and during tachycardia more than 40 ms is infavor of AVNRT; between 20 and 40 ms is infavor of AVRT and less than 20 ms suggests AT.
At the beginning of all maneuvers, His pacing for evaluation about the nodal or extranodal response is more effective; and is sinus rhythm, para-Hision pacing could be done by low and higher amplitude for myocardial capture and his capture; if VA interval was the same during myocardial capture and His capture; there is evidence of extranodal response and in nodal conduction VA during His capture should be shorter than during myocardial capture (Fig. 12.6) [10].
Junctional tachycardia (JT) is another arrhythmia that mostly occurs after ablation and should be differentiated from AVNRT for decision making about the termination of ablation. JT could be discriminated from AVNRT with early PAC that administered before His activation, and terminates the AVNRT, but could induce the JT [10].
Ablation of typical AVNRT is done by ablation of the slow pathway in CS ostium between CS and TV ring.
In this patient, we were very careful about prosthetic mechanical TV.
The atrial EGM in the ablation site should have multiple components and AV ratio should be about 1:3–1:10.
Ablation in the higher position and CS roof could result in AV block. The recommended power for initiation of ablation is 20–30 W with nonirrigated catheters, after 15 s the power could be gradually increased to 60 W with target temperature of 60 °C.
Junctional rhythm during ablation is a sensitive marker of success.
Cyoablation could be done with a lower risk of AV block but a higher rate of recurrence. No junctional rhythm is elucidated during cryoablation and it should be done during atrial pacing to demonstrate slow pathway conduction, and if eliminated, ablation should be continued 4 min at 60 °C.
It is recommended to give Isoproterenol after the ablation for all patients with AVNRT, regardless of the initial induction (with or without Isuprel).
References
Gonzalez M, Quiroga C, Fernandez P, Garro H, Chiale P. Different atrioventricular conduction times and cycle length alternans phenomenon of a typical AV nodal reentrant tachycardia. Arch Cardiol Mex. 2015;85:87–90.
Morady F. Catheter ablation of supraventricular arrhythmias: state of the art. Pacing Clin Electrophysiol. 2004;27:125–42.
Blomstrom-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias–executive summary. A report of the American college of cardiology/American Heart Association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493–531.
Gonzalez MD, Contreras LJ, Cardona F, et al. Demonstration of a left atrial input to the atrioventricular node in humans. Circulation. 2002;106:2930–4.
Kiedrowicz RM, Kazmierczak J, Wielusinski M. The effect of atrial pacing site on electrophysiological properties of the atrioventricular junction and induction of atrioventricular nodal reentry in patients with typical atrioventricular nodal reentrant t achycardia. Kardiol Pol. 2017;75:221–30.
Yu WC, Chen SA, Chiang CE, et al. Effects of isoproterenol in facilitating induction of slow-fast atrioventricular nodal reentrant tachycardia. Am J Cardiol. 1996;78:1299–302.
Miller JM, Rosenthal ME, Gottlieb CD, Vassallo JA, Josephson ME. Usefulness of the delta HA interval to accurately distinguish atrioventricular nodal reentry from orthodromic septal bypass tract tachycardias. Am J. 1991;68:1037–44.
Knight BP, Zivin A, Souza J, et al. A technique for the rapid diagnosis of atrial tachycardia in the electrophysiology laboratory. J Am Coll Cardiol. 1999;33:775–81.
Knight BP, Ebinger M, Oral H, et al. Diagnostic value of tachycardia features and pacing maneuvers during paroxysmal supraventricular tachycardia. J Am Coll Cardiol. 2000;36:574–82.
Gonzalez-Torrecilla E, Arenal A, Atienza F, et al. First postpacing interval after tachycardia entrainment with correction for atrioventricular node delay: a simple maneuver for differential diagnosis of atrioventricular nodal reentrant tachycardias versus orthodromic reciprocating tachycardias. Rhythm. 2006;3:674–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer-Verlag London Ltd., part of Springer Nature
About this chapter
Cite this chapter
Madadi, S. (2021). A 37-Year-Old Lady, Post-MVR, -AVR, -TVR and -AVNRT. In: Maleki, M., Alizadehasl, A. (eds) Case-Based Clinical Cardiology. Springer, London. https://doi.org/10.1007/978-1-4471-7496-7_12
Download citation
DOI: https://doi.org/10.1007/978-1-4471-7496-7_12
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-7495-0
Online ISBN: 978-1-4471-7496-7
eBook Packages: MedicineMedicine (R0)