Abstract
Purpose
We sought to clarify the electrocardiographic and electrophysiological characteristics of ventricular arrhythmias (VAs), including idiopathic ventricular tachycardia (VT) and premature ventricular contractions (PVCs), with acute successful radiofrequency catheter ablation (RFCA) at the left ventricular basal inferoseptum recess near the mitral annulus (LV-BIS-MA).
Methods
Twenty-five patients with acute successful RFCA at the LV-BIS-MA were included in this study.
Results
The S-wave amplitudes on lead III during VAs were 1.54 ± 0.38 mV, significantly larger than those on lead II (0.55 ± 0.19 mV) and aVF (1.04 ± 0.31 mV) (P < 0.01). Precordial R/S > 1 transition before lead V2 and S-waves in lead V6 was recorded in 100% and 48.0% of patients, respectively. The earliest bipolar activation preceded the QRS onset by 32.3 ± 11.5 ms. Pace mapping demonstrated perfect QRS morphology matching in only 56.0% of patients. The RFCA start-to-effect time was 10.2 ± 5.8 seconds (s) in 21 patients (84.0%). In the remaining 4 patients (16.0%), the mean duration of successful RFCA was not well determined due to the infrequent presence of clinical VAs during ablation. The trans-septal approach was utilized in all 25 cases. Intra-cardiac echocardiography (ICE) showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve via the reversed C-curve technique. Early (within 3 days) and late (1 year) recurrence rates were 4.0% (one patient) and 12.0% (three patients), respectively. No complications during RFCA or at the 1-year follow-up.
Conclusions
LV-BIS-MA VAs are a subgroup of idiopathic VAs with distinctive ECG and EP features. RFCA via a trans-septal approach using a reversed C-curve technique is effective for better identification and targeting of the areas of VAs origin, and ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Most idiopathic ventricular arrhythmias (VAs), including idiopathic ventricular tachycardia (VT) and premature ventricular contractions (PVCs), have a right ventricular outflow tract (RVOT) or left ventricular outflow tract (LVOT) origin; however, some may arise from other anatomical sites, including the right or left ventricular (LV) epicardial site, the aortic sinus cusps (ASCs), the aortomitral continuity (AMC), around the anterior portion of the mitral annulus, and other sites [1,2,3]. Radiofrequency catheter ablation (RFCA) has emerged as a treatment for these idiopathic VAs and has a fairly high success rate. Recently, several cases of VAs have been reported to be successfully ablated at the left ventricle basal inferoseptum recess near the mitral annulus (LV-BIS-MA) [4, 5]. However, little is known regarding the prevalence, electrocardiographic (ECG) and electrophysiological (EP) characteristics, efficacy of RFCA, and follow-up findings of LV-BIS-MA VAs. Therefore, this study was performed to clarify these points.
2 Methods
2.1 Patient selection
Among 543 consecutive patients who presented with VAs for RFCA, including idiopathic VT and PVC, between July 2014 and November 2019, 25 (4.6%) patients were found to have an acute successful RFCA of VAs at the LV-BIS-MA. None of these patients exhibited significant coronary artery disease by coronary angiography or CT coronary angiography or any structural heart disease. They failed beta-blocker or at least one anti-arrhythmic drug therapy. Monomorphic non-sustained VT (defined as three or more consecutive PVCs) was present in 2 patients, and monomorphic PVCs were seen in the remaining 23 patients. All patients were in normal sinus rhythm (SR) before RFCA. Twelve-lead ECGs and 24-h ambulatory Holter monitoring were carried out at least once before RFCA. The demographic and clinical data, including patient age, sex, height, weight, biochemical blood examination results, echocardiographic parameters, and clinical arrhythmias, were collected prior to the procedure. The study protocol was reviewed and approved by the hospital’s ethics committee, and all patients provided written informed consent before undergoing RFCA.
2.2 ECG analysis
All anti-arrhythmic drugs were discontinued at least 5 half-lives before the ECGs were recorded for analysis. Twelve-lead ECGs were recorded utilizing the Libang Electrical System (Libang ECG recording, Libang Medical, Shenzhen, China). The ECGs were analyzed at a paper speed of 25 mm/s, and the signals were amplified at 10 mm/mV. VAs were analyzed for the following parameters: (1) the QRS duration; (2) the QRS amplitude in the inferior leads; (3) the maximum deflection index (MDI), defined as the duration from the earliest activation to the peak of the largest amplitude deflection divided by the total QRS duration, measured in the precordial leads; and (4) the S-wave in lead V6. All parameters were measured with electronic calipers by 3 experienced investigators who were blinded to the site of origin. The mean values of these measurements were used for analysis. If the inter-observer difference was more than 5 ms, a final decision was made by a joint meeting of the three investigators.
2.3 Preparation and activation mapping
All anti-arrhythmic drugs were discontinued at least 5 half-lives before the EP study. Intra-cardiac tracings were recorded utilizing a Prucka CardioLabTM electrophysiology system (General Electric Health Care System, Inc., Milwaukee, WI, USA). If the clinical VAs did not occur spontaneously and were not induced at baseline, intravenous isoproterenol (0.5 to 2.0 μg/min) was administered to induce the clinical VAs. A 7.5-French, 3.5-mm tip, irrigated ablation catheter (F-curve, Smarttouch, Biosense Webster, Diamond Bar, CA, USA) was then introduced into the right ventricle (RV) via the right femoral vein. A quadripolar catheter (Synaptic Medical, Beijing, China) was placed in the His position via the left femoral vein. Mapping of the left ventricle (using a trans-septal approach) was initiated after mapping the RV (including the His area on both sides), and intravenous heparin was administered to maintain an activated clotting time (ACT) of 250–300 s. A steerable sheath (MobiCath, Biosense Webster, Diamond Bar, CA, USA) was advanced alternately only when the non-steerable sheath (8.5F SL1, St. Jude Medical, St. Paul, MN, USA) could not advance the ablation catheter to the LV-BIS-MA.
2.4 Electrogram (EGM) collection and analysis
During an episode of spontaneous clinical VAs, activation mapping was performed on at least three arrhythmic beats at a mapping site. The unipolar EGM was recorded from the distal (D) electrode of the mapping catheter and filtered at 0.5–100 Hz. The bipolar EGM was recorded from the distal (D-2) electrode pairs of the mapping catheter and filtered at 30–500 Hz. All EGM and twelve-lead ECG data were stored on the multichannel mapping system for offline analysis with a paper speed of 100 mm/s [6]. The V-QRS interval was calculated from the start of the bipolar ventricular EGM to the earliest start of the QRS complex from any lead (QRS from the surface leads and EGM from all intra-cardiac channels). All parameters were measured with electronic calipers by 3 experienced investigators who were blinded to the site of origin. We adopted the mean values of these measurements as the data. If the inter-observer difference was more than 5 ms, a final decision was made by a joint meeting of the three investigators.
2.5 Pace mapping
Pace mapping during SR was performed at the earliest activation site using the distal bipolar electrodes at a coupling interval of the VAs interval and a stimulus amplitude of 1 mA greater than the late diastolic threshold (up to a maximum output of 10 mA and pulse width of 2.0 ms). If present, a perfect pace-mapping match (12/12 leads) was indicative of the site at or in close proximity to the origin of VAs; otherwise, the activation mapping result was only used for guiding RFCA.
2.6 RFCA
RFCA was applied at the site where the earliest V-QRS interval or perfect pace-mapping match on ECG was recorded. The His catheter was withdrawn, and the ICE catheter was advanced into the RV via the left femoral vein to show the location of the RFCA catheter tip. RFCA was delivered using the power control mode at a maximum power of 35 to 40 W and a temperature of 43 °C with irrigation mode at a flow rate of 17 mL/min. If the VAs was not eliminated within 30 s after energy delivery, the energy application was terminated, and the RFCA site was tagged as an unsuccessful site on the map. If the VAs was abolished within 30 s, the energy application was continued for a total of 180–240 s at and around the target site, and the site was tagged as a successful site on the map.
2.7 Definition of acute successful RFCA
Acute successful RFCA was defined according to the following criteria: absence of spontaneous or induced clinical VAs, in both the absence and presence of isoproterenol infusion after RFCA with observation lasting 0.5 to 1 h.
2.8 Definition of VAs near the LV-BIS-MA
We defined an LV-BIS-MA location as follows: (1) the catheter tip demonstrated the LV-BIS-MA location when viewed on the right and left anterior oblique fluoroscopic views at the successful RFCA site; (2) the ratio of atrial to ventricular EGMs at the RFCA site was < 1, and the amplitudes of the atrial and ventricular EGMs were > 0.08 mV and 0.5 mV at the RFCA site during sinus beats, respectively [3]; (3) acute successful VAs elimination was achieved by RFCA energy delivery at the LV-BIS-MA location; and (4) intra-cardiac echocardiography (ICE) showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve via the reversed C-curve technique using the trans-septal approach.
2.9 Observation after RFCA and at the 1-year follow-up
The patients were monitored for at least 3 days in the hospital after RFCA, and twelve-lead ECG and 24-h ambulatory Holter monitoring were carried out at least once during the 3-day hospitalization after RFCA. The patients were followed up in the outpatient arrhythmia clinic for 1 year, and twelve-lead ECG and 24-h ambulatory Holter monitoring were carried out at least once every 3 months. Clinical success was defined as the absence of clinical VAs (symptomatic or asymptomatic) that were targeted during RFCA at the follow-up visit, as well as at least an 80% reduction of VAs documented on post-RFCA 24-h Holter recording compared with the pre-RFCA VAs burden.
2.10 Statistical analysis
Continuous data are presented as the mean ± SD, and differences between groups were compared with one-way ANOVA. A p value < 0.05 was considered to indicate statistical significance.
3 Results
3.1 Location and frequency of VAs
Of the 543 patients referred for RFCA of idiopathic VAs, twenty-five (4.6%) patients had successful RFCA at the LV-BIS-MA location. The other origins were registered as follows: RVOT, 42.5%; ASC, 29.1%; AMC, 7.9%; tricuspid annulus (TA), 6.8%; papillary muscle, 3.1%; lateral and posterior portion of the MA, 5.7%; and possible right ventricular moderate band, 0.2%. The mean age of the 25 patients with LV-BIS-MA VAs was 67 ± 7 years, with 20 males and 5 females, and their clinical characteristics are summarized in Table 1.
3.2 ECG characteristics of LV-BIS-MA VAs
During the clinical VAs, the RII, SII, RIII, SIII, RaVF, and SaVF amplitudes were 0.17 ± 0.12 mV, 0.55 ± 0.19 mV, 0.05 ± 0.06 mV, 1.54 ± 0.38 mV, 0.09 ± 0.07 mV, and 1.04 ± 0.31 mV, respectively (Table 2). The QRS duration and MDI were 165.8 ± 27.9 ms and 0.54 ± 0.08, respectively. Precordial R/S > 1 transition before lead V2 and S-waves in lead V6 was recorded in 100% and 48.0% of patients, respectively. QRS morphology in lead V1 of QR, R, and the QS pattern was recorded in 44.0%, 40.0%, and 16.0% of patients, respectively. QRS notching in inferior leads was not seen in all 25 patients.
3.3 Activation mapping of clinical LV-BIS-MA VAs
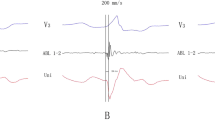
Detailed mappings of the middle cardiac vein, coronary sinus, and right and left basal ventricular septal regions were performed in all 25 patients. In all cases, the site of earliest activation was inferior and basal to the location of the His bundle electrogram on the LV septum. Furthermore, no areas of abnormal endocardial voltage were seen in either side of the basal ventricular septal regions. Acute successful RFCA at the LV-BIS-MA site was achieved in all 25 patients with a trans-septal approach. As shown in Table 3, the a/v amplitude ratio at the RFCA site during SR was 0.13 ± 0.10. The mean earliest V-QRS interval was 32.3 ± 11.5 ms, and initial unipolar QS-waves were recorded in 23 patients (92.0%). With bipolar mapping, isolated pre-potential, fragmented potential, and the earliest V-QRS interval without isolated pre-potential or fragmented potential preceding the QRS complexes were recorded in 3 (12.0%), 6 (24.0%), and 16 (64.0%) patients, respectively. ECGs from all these cases showed precordial R/S > 1 transition before lead V2 and the superior axis on the inferior leads (Figs. 1a, 2a, and 3a). Pace mapping and activation maps in Figs. 1b/d, 2b/d, and 3c/e at the successful ablation sites showed near-identical matches and V-QRS intervals of 57, 70, and 28 ms for bipolar recordings during PVC. The LV-BIS-MA PVC location is shown in Figs. 1e/f, 2e/f, and 3f/g (left and right anterior oblique fluoroscopic views). ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve using the trans-septal approach (Figs. 1g, 2g, and 3h).
Premature ventricular contraction (PVC) with acute successful ablation at the left ventricle basal inferoseptum recess near the mitral annulus (LV-BIS-MA). a Twelve-lead electrocardiographic (ECG) morphology of the QRS complex during sinus rhythm (SR) and PVC. b Pace-mapping QRS complex morphology. c CARTO3 mapping indicates an acute successful RFCA site at the LV-BIS-MA. d Earliest isolated pre-potential with a V-QRS interval of 57 ms for bipolar recording during PVC, delayed potential during SR (arrow), and an a/v amplitude ratio of 0.15 during SR (paper speed 100 mm/s). e and f Left and right anterior oblique fluoroscopic views indicate a reversed C-curve at the LV-BIS-MA. g ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve (arrow). See the text for further details (paper speed 25 mm/s unless otherwise indicated). CS, coronary sinus; ABL, ablation catheter; MAP 1–2, bipolar recording; MAP 1, unipolar recording; Stim, stimulation; ICE, intra-cardiac echocardiography; LA, left atrium; LV, left ventricle; IVS, intra-ventricular septum; MV, mitral valve. The same explanation as in Figs. 2 and 3 unless otherwise indicated
PVC with acute successful ablation at the LV-BIS-MA. a Twelve-lead ECG morphology of the QRS complex during SR and PVC. b Pace-mapping QRS complex morphology. c CARTO3 mapping indicates an acute successful RFCA site at the LV-BIS-MA. d Earliest fragmented bipolar potential with a V-QRS interval of 70 ms for bipolar recording during PVC and an a/v amplitude ratio of 0.05 during SR (paper speed 100 mm/s). e and f Left and right anterior oblique fluoroscopic views indicate a reversed C-curve at the LV-BIS-MA. g ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve (arrow)
PVC with acute successful ablation at the LV-BIS-MA. a Twelve-lead ECG morphology of the QRS complex during SR and PVC. b and c Clinical PVC and pace-mapping QRS complex morphology (paper speed 25 mm/s). d CARTO3 mapping indicates an acute successful RFCA site at the LV-BIS-MA. e Earliest V-QRS interval of 28 ms for bipolar recording during PVC and an a/v amplitude ratio of 0.05 during SR (paper speed 100 mm/s). e and f Left and right anterior oblique fluoroscopic views indicate a reversed C-curve at the LV-BIS-MA. h ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve (arrow). I: PVC was successfully ablated within 12.4-s ablation (paper speed 10 mm/s)
3.4 Pace mapping
Perfect (12/leads) or near-perfect (11/12 leads) pace maps of the QRS morphology of the clinical VAs were obtained in 14 patients (56.0%) at the successful RFCA site. A relatively large amount of myocardium could be captured around the pacing electrodes, which may have obscured subtle changes in the QRS morphology in 11 (44%) of these patients.
3.5 RFCA at the LV-BIS-MA location
Complete elimination of the VAs was achieved by RFCA at the site where the earliest V-QRS interval was recorded at the LV-BIS-MA location. The mean duration of successful RFCA was 10.2 ± 5.8 s in 21 patients (84.0%). In the remaining 4 patients (16.0%), the mean duration of successful RFCA was not well determined due to the infrequent nature of clinical VAs during ablation. The junctional rhythm was recorded in 1 patient (4.0%) after 21 s of RFCA, where the ablation was carried out only intermittently and was discontinued immediately when junctional rhythm occurred. No complications, including atrioventricular block or pericardial effusion, occurred during the RFCA procedure.
3.6 Observations after RFCA and at the 1-year follow-up
No complications occurred during at least 3 days of observation after RFCA or during the 1-year follow-up period. Clinical VAs were still recorded in 1 patient (4.0%) during the 3 days of in-hospital monitoring after RFCA. During the 1-year follow-up period, 3/25 (12.0%) patients had clinical VAs recurrence, and one patient underwent a re-do procedure. The final RFCA target was the same as the index procedure based on X-ray fluoroscopic views and CARTO3 mapping results.
4 Discussion
4.1 Main findings
The current study had four major findings. First, the frequency of LV-BIS-MA VAs confirmed by successful RFCA was 4.6% in 543 consecutive patients with idiopathic VAs in a single center. Second, precordial R/S > 1 transition before lead V2 was recorded in 100% of patients, and SIII amplitudes were significantly larger than SII and SaVF amplitudes without QRS notching in inferior leads in all 25 patients. Third, RFCA via a trans-septal approach using a reversed C-curve technique was effective for the acute elimination of these VAs. Fourth, ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve.
4.2 ECG characteristics of VAs from LV-BIS-MA
The origin of LV-BIS-MA VAs is located in the left inferior basal portion of the LV septum, distant from the precordial electrodes and lead III. The myocardium at the RFCA site is depolarized in a direction toward the precordial electrodes and backward the lead III. This could account for the early precordial transition and concordant positive QRS pattern in leads V1 to V5 and significantly larger SIII than SII and SaVF. The ventricular septum is oriented nearly horizontally to the electrode of lead V1. The myocardium during LV-BIS-MA VAs may be depolarized to or away from lead V1. This may account for the different QRS morphologies in lead V1 in different patients (Table 2). The ventricular septum and the rest of the myocardium were depolarized simultaneously during LV-BIS-MA VAs, which may explain the absence of notching in inferior leads or the absence of an s-wave in lead V6. An electric impulse from the LV-BIS-MA region takes more time to reach the Purkinje network to depolarize myocardium than that of an electric impulse from the Purkinje network, resulting in a wide QRS duration and maximum deflection index (MDI) during LV-BIS-MA VAs. Our results of LV-BIS-MA VAs are different from those of right side para-Hisian VAs reported by Sun et al. in 25 consecutive patients [7]. In para-Hisian VAs, the magnitude of the R wave in lead II was larger than that in lead III, and precordial R wave transition occurred between leads V2 and V3 in 17 of 25 (68%) patients. Liang et al. reported similar ECG characteristics of VAs from 25 patients who underwent successful ablation at the basal inferoseptal LV endocardium (BIS-LVe) with a wider QRS duration of 178.2 ± 22.4 ms and MDI of 0.49 ± 0.04 [8]. In contrast, among the patients with LV-BIS-MA VAs in our study, more than half had an MDI ≥ 0.55. Based on the QRS morphology on 12-lead electrocardiographic recordings of our 25 and 44 patients from the aforementioned 2 studies, we proposed a flowchart to differentiate LV-BIS-MA VAs from other VAs (Fig. 4). The new ECG criteria were investigated prospectively in 3 cases and were able to predict the site of LV-BIS-MA VAs origin with 100% accuracy.
4.3 Hypothetical mechanism of VAs genesis near the LV-BIS-MA
The isolated pre-potential or fragmented potential at successful RFCA targets suggest a focal mechanism of either automaticity or triggered activity with a slow conduction area between the VAs origin and the ventricle breakout point (Figs. 1 and 2). However, in 16 of 25 patients (64%), the earliest bipolar V-QRS interval without isolated pre-potential or fragmented potential was recorded at the successful RFCA sites. This suggests that the VAs origin may be right at the ventricular breakout point without conduction delay or it may be located at an intramyocardial or epicardial location too small to be recorded.
While the mechanism of LV-BIS-MA VAs could not be determined in our study, an appreciation of the particular anatomical-histological evaluation of this region potentially provides some insights. Yanni et al. reported histologically and histochemically different AV ring-specialized tissue at the MA and TA, which may lead to arrhythmia genesis [9]. Tawara first described the structure of the compact AV node and its left and right posterior extensions [10]. Inoue et al. reported that among 21 randomly selected and basically normal hearts obtained from autopsies, 13 showed posterior extensions of the AV node on both the right and left sides, 7 showed a rightward posterior extension only, and only 1 heart showed a single leftward extension [11]. The rightward extension ran close to the TA, and the leftward extension ran close to the MA. McGuire et al. reported that microelectrode recordings revealed cells with nodal-type action potentials were found within 1 to 2 mm of the tricuspid and mitral valve rings [12]. These nodal-type cells can respond to adenosine and lack connexin-43. Ashikaga et al. reported a VT case originating from the LV-BIS-MA, which could be induced by exercise or isoproterenol administration but not by pacing [13]. Frequent PVCs with the same QRS morphology as the VT were transiently suppressed by an adenosine triphosphate injection, suggesting that the mechanism was due to cyclic AMP-mediated triggered activity. We speculate that those nodal-type cells from the left posterior extension may represent the arrhythmogenic substrate for LV-BIS-MA VAs. Anisotropy of the conduction velocity and refractory period could exist between the so-called left posterior extension and its neighboring ventricular myocardium, which may potentially provide the arrhythmogenic substrates for micro-reentry, abnormal automaticity or triggered activity near the LV-BIS-MA area. It will be important to test this hypothesis in the future, both in the laboratory and in clinical studies, and this is an area that warrants further electrophysiological study.
4.4 Related studies
Several previous studies have reported the successful ablation of VAs at or near the LV-BIS-MA location; however, none has systemically determined the prevalence or ECG and EP characteristics of VAs originating from the LV-BIS-MA location and short- and long-term outcomes in as many patients as those included in the present study [2,3,4,5]. Li et al. reported that such VAs significantly increased with intravenous isoproterenol infusion or became more prominent during the washout phase after infusion termination, instead of being induced by programmed stimulation, suggesting triggered activity or automaticity as the potential mechanisms [14]. Kawamura et al. reported idiopathic VAs from the cardiac crux with similar electrocardiographic characteristics and demonstrated that ablation is effective in eliminating these VAs [15]. Ashikaga et al. reported a PVC case that was transiently suppressed by an adenosine triphosphate injection, supporting the hypothesis of cyclic AMP-mediated triggered activity (Table 4) [13]. Because VAs can originate from the LV/RV endocardial/epicardial aspect of the basal ventricle inferoseptum near the mitral/tricuspid annulus, determining whether ablation from the endocardial/epicardial aspect of the LV/RV will be successful or whether mapping and ablation from the CS or epicardium are likely to be required is important (Table 5).
4.5 Trans-septal approach vs the transaortic approach
Both activation map and pace map methods were useful for identifying target sites for LV-BIS-MA VAs in this study. We choose the trans-septal approach in all 25 cases. Ouyang et al. reported that the trans-septal approach using a reversed S-curve was effective for ablating ventricular arrhythmias arising from the LVOT below the aortic sinus cusps [16]. The advantage of the trans-septal approach over the transaortic approach is mainly the easier catheter manipulation; easier advancement to the VAs origin; avoiding obstacle of the aortic valve, chordae tendineae, and papillary muscle; and for avoiding passing catheters through the tortuous iliac or femoral artery. Venous access was also associated with a low risk of hematoma with short bed rest time.
4.6 Study limitations
There are several limitations of this retrospective study. First, while isolated pre-potential or fragmented potential preceding the QRS complexes was recorded at the RFCA site, its genesis and significance were not determined. Second, the majority of the VAs were successfully ablated despite the fact that isolated pre-potential or fragmented potentials during VAs were not recorded. The causes for the lack of recording for isolated pre-potential or fragmented potentials are only speculative. Third, this was a retrospective analysis, and the results need to be validated with a prospective study with a larger sample size.
5 Conclusion
LV-BIS-MA VAs are a subgroup of idiopathic VAs with distinctive ECG and EP features. RFCA via a trans-septal approach using a reversed C-curve is effective for the acute elimination of these VAs. ICE showed that the ablation catheter tip was underneath the anterior leaflet of the mitral valve. Advanced knowledge of the LV-BIS-MA anatomy and ECG and EP features may be useful in planning and facilitating the RFCA procedure.
References
Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias: Executive summary. Heart Rhythm. 2019;59:81–133.
Tada H, Ito S, Naito S, Kurosaki K, Kubota S, Sugiyasu A, et al. Idiopathic ventricular arrhythmia arising from the mitral annulus: a distinct subgroup of idiopathic ventricular arrhythmias. J Am Coll Cardiol. 2005;45:877–86.
Wasmer K, Köbe J, Dechering DG, Bittner A, Pott C, Mönnig G, et al. Ventricular arrhythmias from the mitral annulus: patient characteristics, electrophysiological findings, ablation, and prognosis. Heart Rhythm. 2013;10:783–8.
Kawamura M, Arai S, Gokan T, Yoshikawa K, Ogawa K, Ochi A, et al. Idiopathic basal crux ventricular arrhythmias with left bundle branch block and superior axis: a comparison with inferior-septal valvular arrhythmias. J Cardiovasc Electrophysiol. 2019;30:1914–22.
Sato E, Yagi T, Ishida A, Mibiki Y, Yamashina Y, Sato H, et al. Idiopathic ventricular arrhythmias arising from the posterior septum of tricuspid and mitral annuli: comparison of electrocardiographic characteristics and outcomes of catheter ablation. J Interv Card Electrophysiol. 2019;54:125–34.
Mountantonakis SE, Vaishnav AS, Jacobson JD, Bernstein NE, Bhasin K, Coleman KM, et al. Conduction patterns of idiopathic arrhythmias from the endocardium and epicardium of outflow tracts: new insights with noninvasive electroanatomic mapping. Heart Rhythm. 2019;16:1582–9.
Sun J, Zhang PP, Wang QS, Xu QF, Wang ZQ, Yu Y, et al. Catheter ablation of ventricular arrhythmias originating from the para-Hisian region with reversed C-curve technique. J Cardiovasc Electrophysiol. 2019;30:2377–86.
Liang JJ, Shirai Y, Briceño DF, Muser D, Enriquez A, Lin A, et al. Electrocardiographic and electrophysiologic characteristics of idiopathic ventricular arrhythmias originating from the basal inferoseptal left ventricle. JACC Clin Electrophysiol. 2019;5:833–42.
Yanni J, Boyett MR, Anderson RH, Dobrzynski H. The extent of the specialized atrioventricular ring tissues. Heart Rhythm. 2009;6:672–80.
Tawara S. The Conduction System of the Mammalian Heart. An Anatomico-Histological Study of the Atrioventricular Bundle and the Purkinje Fibers. London: Imperial Collage Press; 2000.
Inoue S, Becker AE. Posterior extensions of the human compact atrioventricular node: a neglected anatomic feature of potential clinical significance. Circulation. 1998;97:188–93.
McGuire MA, de Bakker JM, Vermeulen JT, Moorman AF, Loh P, Thibault B, et al. Atrioventricular junctional tissue. Discrepancy between histological and electrophysiological characteristics. Circulation. 1996;94:571–7.
Ashikaga K, Tsuchiya T, Tashiro H, Yamamoto K. Idiopathic ventricular tachycardia originating from the posteroseptal mitral annulus: a case report. J Cardiovasc Electrophysiol. 2006;17:1375–7.
Li A, Zuberi Z, Bradfield JS, Zarif JK, Ward DE, Anderson RH, et al. Endocardial ablation of ventricular ectopic beats arising from the basal inferoseptal process of the left ventricle. Heart Rhythm. 2018;15:1356–62.
Kawamura M, Gerstenfeld EP, Vedantham V, Rodrigues DM, Burkhardt JD, Kobayashi Y, et al. Idiopathic ventricular arrhythmia originating from the cardiac crux or inferior septum: epicardial idiopathic ventricular arrhythmia. Circ Arrhythm Electrophysiol. 2014;7(6):1152–8.
Ouyang F, Mathew S, Wu S, Kamioka M, Metzner A, Xue Y, et al. Ventricular arrhythmias arising from the left ventricular outflow tract below the aortic sinus cusps: mapping and catheter ablation via trans-septal approach and electrocardiographic characteristics. Circ Arrhythm Electrophysiol. 2014;7:445–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the TEDA International Cardiovascular Hospital ethics committee for clinical research. All patients provided written informed consent.
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di, C., Gao, P., Wang, Q. et al. Electrocardiographic and electrophysiological characteristics of idiopathic ventricular arrhythmias with acute successful ablation at the left ventricular basal inferoseptum recess near the mitral annulus. J Interv Card Electrophysiol 66, 281–290 (2023). https://doi.org/10.1007/s10840-021-00983-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00983-3