Abstract
Although some basic concepts related to medicolegal aspects for the practicing physician have remained unchanged over several years, there is a rapid increase in case-law and new trends emerging in this field. Accordingly, this chapter is divided into three parts. First, a basic overview related to medico-legal civil liability for the practicing physician is discussed, including steps that physicians should consider to minimize this liability. Second, some of the unique legal issues in the practice of pediatric critical care are discussed. Third, several PICUs are in the midst of implementing electronic health records (EHR). The implementation of electronic health records and availability of electronic patient data creates unique challenges and legal issues previously unknown, and key concepts related to these new emerging areas are also discussed.
The information contained in this article is for educational purposes and is not intended to provide legal advice. You should consult an attorney for individual advice regarding your situation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
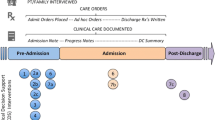
Given the high acuity and associated risks of patients treated in the pediatric intensive care unit (PICU), it is important that pediatric critical care physicians have a thorough understanding of the medicolegal aspects related to their practice (Fig. 2.1). Pediatric critical care physicians need to be aware of four distinct areas of civil liability (discussed below). This chapter primarily discusses the medico-legal concepts related to medical negligence, with a brief discussion of the False Claims Act. However, critical care physicians should also be aware of interactions between ethical and legal concepts related to withdrawal of care and brain death, and also issues related to obtaining informed consent particularly in elective situations in contrast to emergency situations in the PICU. These issues are discussed in greater detail in other chapters of this textbook.
Although some basic concepts related to medicolegal aspects for the practicing physician have remained unchanged over several years, there is a rapid increase in case-law and new trends emerging in this field. Accordingly, this chapter is divided into three parts from the perspective of the physicians in the U.S. First, a basic overview related to medico-legal civil liability for the practicing physician is discussed, including steps that physicians should consider to minimize this liability. Second, some of the unique legal issues in the practice of pediatric critical care are discussed. Third, several PICUs are in the midst of implementing electronic health records (EHR). The implementation of electronic health records and availability of electronic patient data creates unique challenges and legal issues previously unknown, and key concepts related to these new emerging areas are also discussed.
Medico-legal Civil Liability for Pediatric Critical Physicians
Typically, medico-legal civil liability for pediatric critical physicians relates to medical malpractice claims for negligence. The underlying premise is that there is no intent for the injury caused to the child. Such negligence claims require that the family of the injured child (plaintiff) affirmatively prove four key elements – duty, breach, causation, and harm (this is extensively discussed in many legal writings) [1]. The physician must have a duty to the patient. This is generally not an issue in the PICU where the physician is responsible for the children receiving medical care. Harm is also generally not a controversial issue with respect to proof because it typically forms a basis of initiating the claim. The two elements that become the subject of debate include breach and causation. Breach relates to the notation that a departure from the standard of care occurred. It is important to point out that this standard of care represents a national standard as highlighted in the case Hall vs. Hilbun [2]. In this particular case, the underlying issue was whether a surgeon breached the standard of care when he was at home and the patient suffered a complication after an exploratory laporatomy resulting in cardiorespiratory arrest. The surgeon argued that the care was consistent with the local practice (locality rule). However, the Supreme Court of Mississippi held that the surgeon be judged based upon a national standard of care. With respect to the application of this concept for the pediatric critical care physician, it is important to recognize that local practices within the PICU, although acceptable and popular locally, may be considered as departures from the standard of care if a national standard for that particular critical care condition exists.
The other element in an injury claim that is frequently subject to debate relates to the notion of causation. Causation implies that the physician’s actions resulted in the alleged harm. This can have unique implications in the pediatric critical care setting, where care is provided on a successive basis by multiple physicians during the course of care. Accordingly, it is generally not an acceptable defense that a physician did not cause harm if the underlying problem was precipitated by physician care provided earlier in the course of the care. A hypothetical example would be the situation in which a critical care physician inadvertently placed a central venous catheter in an artery and the care of the child is then taken over by a second physician. The second physician fails to detect this error and the patient suffers harm. In this case, it would generally not be a defense for the second physician that the procedure was performed by someone else. This concept relates to the legal theory of multiple defendants, where several physicians may work in series or tandem and be responsible for patient injury.
Once the injured party (family) feels that the child has suffered an injury and obtains legal counsel, the first step relates to the concept of the Statute of Limitations. This is a predefined number of years established by state law during which time the medical malpractice claim can be initiated. This step typically is followed by a series of discovery during which interrogatories and depositions may be conducted and there is a thorough medical record review. The case can be settled by both parties anytime during the litigation period. A small number of cases proceed to a jury trial where both parties have the opportunity to provide legal arguments to the jury before making a final decision. As medical malpractice liability is based upon state laws which differ significantly across states, it is important for the pediatric critical physician to be fairly familiar with laws where they practice. Differences in state laws not only result in differences in liability but also in differences in the final payments to the injured party.
Steps to Minimize Medico-legal Liability for the Pediatric Critical Care Physician
In order to minimize the medico-legal liability, physicians must carefully keep the following considerations in mind. First, in the practice of pediatric critical care, it is important to be up-to-date on national recommendations for various clinical conditions. As mentioned earlier, it is generally not a defense that the standard of care being practiced was consistent with a local practice but inconsistent with a national standard. Second, physicians should maintain impeccable medical records and documentation of the care being provided. With the trend towards adoption of electronic health records, many of the issues related to legibility of handwriting will evaporate, but newer issues previously not addressed will emerge. Third, it is important to have open and honest communication with families. The emerging literature from patient safety supports that full disclosure of mistakes and patient safety related adverse events to the family in a timely manner in fact reduces the likelihood of subsequent lawsuits. Finally, it is important to approach the medico-legal litigation in professional manner. Typically when physicians are sued, many view this as a direct attack on their professional credibility. This is understandable. However, in order for successful resolution of the underlying lawsuit, it is important to fully cooperate with the investigation in a professional and truthful manner.
Figure 2.2 illustrates the progression of a hypothetical medico-legal case highlighting the change in approaches to medical errors and mistakes based upon the emerging quality and patient safety literature. In the past, the traditional approach to medical errors included avoiding any discussion with the family. The modern approach encourages early and full disclosure with an apology for the situation to the family. The physician should consult with their legal counsel as quickly as possible after learning of a patient safety event. Also, it is important to distinguish between an apology for a particular situation that a family is dealing with versus an admission of a mistake, and the physician should discuss this carefully with their legal counsel to ensure that the goals of full disclosure and transparency for patient safety are met without increasing the individual likelihood of incurring liability.
Legal Standards for Admissibility of Medical Evidence and Expert Testimony
A common issue emerging in medical malpractice related litigation surrounds the notion of determining the standard of care. Typically this standard of care would be established by expert testimony. There are two standards utilized in determining the admissibility of scientific evidence into legal evidence. First, the Frye standard which relates to the notion of general acceptance of the scientific evidence in the relevant field [3]. The role of the court is to prevent less than optimal science from being admitted into evidence. Many states have utilized the Frye standard for determining scientific admissibility. Subsequently, in the Daubert vs. Merrell Dow [4] case, the U.S. Supreme Court rejected the Frye test of general acceptance and established the Daubert standard, which relates to the notion that the scientific knowledge must be derived from scientifically sound methods for ensuring reliability and relevancy. Under the Daubert approach the court could use a broad range of criteria to establish the scientific reliability and relevance of the expert evidence. In order to determine the reliability factors using the Daubert standard, the court evaluates the totality of circumstances including considering factors whether the scientific theory being proposed has been empirically tested, whether there has been peer review and publication, determination of the potential error rate including the notion of Type 1 and Type 2 statistical error rates, and the need for the technique and results to be explained in simple terms. Although the Daubert standard typically emerged as a federal standard, it has increasingly been adopted by several states as their evidentiary standards. This has a unique application in the PICU where new research techniques are frequently leveraged in innovative new therapies and management techniques of care. Generally, the standard of care would be established by experts providing testimony for both parties. Recent decisions in the Kumho Tire [5] case highlighted that experts do not need to necessarily have a specific level of certification or education, and in fact, sufficient training and experience may be adequate to deem an individual an expert for establish credibility towards the expert testimony.
Unique Issues in the Pediatric Intensive Care Unit Setting
The discussion in this chapter is largely limited to civil medico-legal situations. However, it is important for the critical care physician to recognize the breath of legal issues that surround decision making in the PICU setting. Several issues span underlying ethical principles, including research and policies on medical futility, end of life decisions, withdrawal of care, and determination of brain death. The full discussion of these topics is beyond the scope of this chapter. However, an emerging area of interest for the critical care physician related to qui tam litigation is briefly discussed below. The concepts of qui tam litigation (derived from the Latin phrase, qui tam pro domino rege quam pro se ipso in hac parte sequitur, meaning he who sues in this matter for the king as well as for himself, in which an individual who assists a prosecution can receive all or part of any penalty imposed) stem from the legal provisions of the False Claims Act [6]. The False Claims Act essentially prohibits falsification of billing to government (Centers for Medicare and Medicaid) for services provided. At the superficial level, this can be viewed in terms of obvious fraudulent actions such as billing for services or procedures that were not performed. However, the False Claims Act has recently been expanded to also cover gross breaches in the quality of care provided, which may be viewed as the absence of care. For example, case law from the nursing homes suggests that patients who developed pressure ulcers due to lack of appropriate nursing home staffing may be subject to liability under the False Claims Act [7]. Further, the False Claims Act provision includes protection and incentivization for whistleblowers. The application of the False Claims Act for combating healthcare fraud is an area of increasing interest in the U.S.
The potential implications for the PICU setting may be important. For example, recently the Centers for Medicare and Medicaid (CMS) adopted policies for nonpayment of “never” events. These complications will not be reimbursed by insurance because they should never occur if the hospital care is functioning appropriately. Examples of “never” events include wrong site surgery, hospital acquired conditions such as pressure ulcers, and more recently, hospital acquired catheter associated blood stream infections. This could create unique new problems from a billing perspective for critical care physicians and their institutions. Therefore, it is important for the pediatric critical care physician to be abreast of these new emerging rules and policies to avoid the unintentional liability that may arise because of compliance failure.
Emerging Medico-legal Issues Resulting from the Availability of Electronic Data from EHR
Most institutions in the U.S. healthcare system are in the midst of EHR implementation. Many PICUs have already adopted electronic health records. This is intended to improve the care quality of including patient safety. However, the increasing availability of electronic data can result in unintended consequences from a medico-legal standpoint. A case from the Wisconsin Supreme Court, Johnson vs. Kokemoor [8] highlights the potential implications. In this case, the plaintiff had an operation for a carotid aneurysm. Unfortunately, the plaintiff had a complication. The ensuing litigation was based on an argument of battery for the lack of obtaining informed consent utilizing available outcomes data. The plaintiff argued that the surgeon was aware of the comparative outcomes data for his performance compared to a renowned health system in the region which also had available outcomes data for the procedure. The surgeon failed to share these comparative outcomes data with the patient while obtaining informed consent for the surgical procedure. The Wisconsin State Supreme Court determined that this was material for the decision making by the patient and the failure of having this information was interpreted as failure of obtaining full informed consent. The Johnson vs. Kokemoor decision, although a landmark decision in this field, has gained limited acceptance in other jurisdictions over the past few years. This may be secondary to the lack of readily available outcomes data to perform meaningful statistical comparisons as was highlighted in this opinion. However, the availability of EHR in the future will result in this issue being magnified as physicians, hospitals, and insurance agencies rapidly acquire physician level performance data which can then be subjected to statistical comparisons with other providers [9].
The field of pediatric critical care medicine is particularly well-suited for comparative outcomes information to be used in the legal setting because of the availability of validated risk adjustment tools that have gained peer reviewed acceptance. An example of this is the Pediatric Risk of Mortality (PRISM) Score [10]. As most critical care physicians are familiar, risk adjustment tools such as the PRISM Score allows for comparison of standardized mortality that adjusts for severity of illness at the time of PICU admission. For example, mortality within PICUs can be risk adjusted to allow for comparisons across PICUs as well as over time within a PICU however, the algorithm requires periodic recalibration.
However, risk of mortality scores such as the PRISM, allow for meaningful physiologic based clinical risk adjustment among groups of patients and was never intended to be used at the individual level to predict risk of death. Therefore, such systems should not be used for prognosis for an individual patient. With the availability of large granular data sets, resulting from the adoption of electronic health records, and with the increasing sophistication of statistical and analytical techniques, it will be likely that risk adjustment can be computed at the patient level in the future. Efforts to perform quality comparisons at the regional and national level have already been successfully implemented [11]. Although this methodology is still early in its development, the rapid growth of large data sets will likely allow the continued refinement of such methodologies. The legal implications of the possibility are presently unknown but would likely be used by the legal community.
Other electronic sources are also available (including the KIDS database, PHIS, Society for Thoracic Surgeons Congenital Heart Disease registry, etc.). Some data sets can be evaluated for changes in outcome or care over time to identify trends that may not otherwise be known. Data mining may allow the identification of unique trends related to quality of care for specific physicians. These approaches are still at the level medical outcomes research and have not yet been introduced into the courtroom. However, future mediolegal litigation will very likely attempt to expand the scope of evidence to include results from such analyses using large databases and patient registries.
There has already been a growing interest and movement within the legal profession to incorporate such information to enhance the scope of evidence and the various aspects of litigation [12]. Another application of these increasing electronic patient data sources are evaluation of quality of care and the potential introduction of such results into legal evidence remains unknown at present but it would be extremely important for the pediatric critical care physician to remain aware of the growing trends in this area which will likely impact their practice in the future.
The intersection of medicine and law continues to raise new issues and challenges as both of these fields continue to evolve. In the future, the intersection of medicine and law related to electronic data, discoverability, and admissibility into evidence will continue to be intensely debated in settings such as pediatric critical care which represent the forefront of advances in medicine.
References
Sachdeva RC, D’Andrea LA. Emerging medicolegal issues in the practice of pediatric sleep medicine. Child Adolesc Psychiatr Clin N Am. 2009;18:1017–25.
Hall v. Hilbun, 466 So.2d 856 (Sup. Ct. Miss., 1985).
Frye v. United States. 293 F. 1013 (D.C. Cir 1923).
Daubert v. Merrell Dow Pharmaceuticals, 509 U.S. 579. 1993.
Kumho Tire Co. v. Carmichael, 526 U.S. 137. 1999.
The False Claims Act (FCA). 31 U.S.C. §§ 3729–3733.
United States ex rel. Aranda v. Cmty. Psychiatric Ctrs. of Oklahoma, 945 F. Supp. 1485 (W.D. Okla. 1996).
Johnson v. Kokemoor, 199 Wis. 2d 615,545 N.W.2d 495. 1996.
Sachdeva RC. Electronic healthcare data collection and pay-for-performance: translating theory into practice. Ann Health Law. 2007;16:291–311.
Pollack MM, Ruttimann UE, Getson PR. The pediatric risk of mortality (PRISM) score. Crit Care Med. 1988;16:1110–6.
Slater A, Shann F, ANZICS Paediatric Study Group. The suitability of the Pediatric Index of Mortality (PIM), PIM2, the Pediatric Risk of Mortality (PRISM), and PRISM III for monitoring the quality of pediatric intensive care in Australia and New Zealand. Pediatr Crit Care Med. 2004;5:447–54.
Sachdeva RC, Blinka DD. Improving the odds of success: quantitative methodology in law practice. Wis Lawyer. 2005;78:12.
Acknowledgements
The author would like to thank Caroline Hackstein and Lisa Ciesielczyk for their assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Sachdeva, R.C. (2014). Pediatric Critical Care and the Law: Medical Malpractice. In: Wheeler, D., Wong, H., Shanley, T. (eds) Pediatric Critical Care Medicine. Springer, London. https://doi.org/10.1007/978-1-4471-6362-6_2
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6362-6_2
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6361-9
Online ISBN: 978-1-4471-6362-6
eBook Packages: MedicineMedicine (R0)