Abstract
This chapter aims to provide a pragmatic approach to the management of patients with CKD. First, we must correctly identify those with CKD, impart the information to the patient in an informative and appropriate way and then offer strategies to ameliorate the complications of CKD and prevent progression of the kidney disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic Kidney Disease
- Renal Replacement Therapy
- Acute Kidney Injury
- Serum Creatinine Concentration
- Blood Pressure Target
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
This chapter aims to provide a pragmatic approach to the management of patients with CKD. First, we must correctly identify those with CKD, impart the information to the patient in an informative and appropriate way and then offer strategies to ameliorate the complications of CKD and prevent progression of the kidney disease.
Ascertainment of CKD
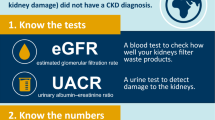
The diagnosis of CKD relies upon the accurate measurement of excretory kidney function and proteinuria, both of which have some pitfalls. Given that kidney disease is predominantly asymptomatic (in the early stages at least), healthcare providers must ensure that they correctly identify those with CKD in order to offer optimal care to those with CKD and reassure those who do not.
Measurement of Glomerular Filtration Rate in the Management of CKD
It is seldom necessary to measure glomerular filtration rate directly in routine clinical practice, but there are exceptions:
-
1.
To reassure patients with high muscle bulk, a high serum creatinine concentration and a low estimated GFR that excretory kidney function is normal
-
2.
When considering use of drug treatments using renally cleared drugs with a narrow therapeutic index, e.g. cytotoxic chemotherapy
-
3.
In assessing excretory kidney function prior to live kidney donation
Measurement of GFR can be performed using isotopic methods (such as 125I-iothalamate) or using contrast media (such as iohexol). Alternatively creatinine clearance may be measured using 24-h urine collection and a serum creatinine measurement taken during the collection period. However, creatinine clearance overestimates GFR as a result of tubular creatinine secretion (approximately 15 % in normal renal function, rising to 50 % in advanced CKD). This can be corrected by the concurrent administration of a drug that blocks tubular creatinine secretion such as 48 h pretreatment with full-dose cimetidine.
Quantification of Proteinuria
Proteinuria is the cardinal feature of renal disease; therefore, the accurate identification and quantification of proteinuria is paramount in the management of patients with CKD.
Proteinuria may be glomerular (predominantly albuminuria), tubular (as a result of the failure of tubular reabsorption of filtered low-molecular-weight proteins) or overflow (such as excess light chain excretion in myeloma which overwhelms the normal tubular reabsorptive capacity). Quantification of urinary protein using a total protein assay will take account of all of these varying proteins; however, measuring albuminuria will only give an indication of glomerular disease. The measurement of albumin is generally favoured in the biochemistry community as it is quantified using an immunoassay which has technical advantages over the less precise physicochemical assays used for total protein. It has also been said that albuminuria is the better test at low levels (<0.5 g/day total proteinuria equivalent) as the noise/signal ratio (with physiological proteins being the noise and the albuminuria being the signal) is superior. However, the early studies of diabetic nephropathy (from which this received wisdom emanated) did not measure total proteinuria, so no head-to-head comparison was made. This low-level albuminuria was previously known as ‘microalbuminuria’ which is a misleading term and should now be avoided.
Traditionally, proteinuria was measured using timed (usually 24-h) urine collections. However, these are cumbersome for the patient, doctor and laboratory and have generally been superseded by spot measurements of total protein/creatinine ratio (uPCR) or albumin/creatinine ratio (uACR). The urine creatinine is used as a surrogate for urine flow rate to allow comparison between samples. This gives reasonably reliable intraindividual comparisons; however, there is significant interindividual variation in urinary creatinine excretion which is not taken into consideration with this approach. This may or may not be an important issue [1]. Ratios from spot urine samples become unreliable at very high protein excretion rates (such as >6 g/day) and a timed urine collection may still be indicated in these circumstances [2]. Dipsticks are no longer recommended for the quantification of proteinuria (unless laboratory quantification is not available in a resource scarce healthcare environment), however still have utility to detect non-visible haematuria. The 2012 KDIGO guidelines recommend that every description of kidney disease includes a quantification of albuminuria (A1–A3 depending on severity) [3] (Table 48.1). The addition of proteinuria to the updated international CKD classification underlines the increasing appreciation of the importance of proteinuria in the diagnosis, management and prognostication in CKD.
Quantitation of urine protein excretion is important in several clinical situations (see also Chap. 2):
-
1.
In patients with suspected glomerular disease, including the nephrotic syndrome. Quantification of albumin excretion is the most logical test to do in this situation, as this gives the best estimate of the severity of glomerular damage. However, there is much less convincing evidence to support changes in management at lower levels of albuminuria in glomerular disease, and so quantitation of total protein (which is cheaper and still takes account of albumin loss) is still widely used.
-
2.
In patients with suspected tubular disease (either inherited, as in Dent’s disease, or acquired, such as tubulointerstitial nephritis) – in this situation, specific assays for low-molecular-weight proteins that appear in the urine as a result of failure of tubular reabsorption (endocytic mechanism via megalin and cubilin receptors on proximal tubular cells) may be required, the commonest test being for retinol-binding protein.
-
3.
Amongst patients with diabetes mellitus, albuminuria of 30–300 mg/day equivalent, when present on repeated tests, is diagnostic of early diabetic nephropathy and should prompt treatment to prevent progressive nephropathy.
The presence of low-level albuminuria (30–300 mg/day equivalent) is also associated with atherosclerosis and hypertensive vascular disease and has been shown to be a powerful predictor of cardiovascular disease (the risk extends into the ‘normal’ range) [4]. In this situation, low-level albuminuria probably reflects widespread endothelial dysfunction rather than indicating a specific kidney disease. It is unknown whether offering nondiabetic patients with low-level albuminuria additional treatment to prevent vascular disease improves prognosis, when it would not otherwise be indicated by traditional risk factors. However, many such patients do have existing vascular disease and will benefit from interventions to reduce risk such as advice on exercise, smoking, correction of obesity, salt restriction, blood-pressure-lowering drugs and lipid-lowering drugs. Whether or not ACEIs or ARBs confer additional prognostic benefit (in preventing cardiovascular disease) in this situation is not known.
Proteinuria that is caused by kidney disease, whether resulting from diabetes or from other disorders, is also strongly associated with an increased risk of cardiovascular disease. It is not known whether specific immunosuppressant treatment that reduces proteinuria caused by kidney disease results in a subsequent improvement in cardiovascular risk.
Finding Patients with CKD
The Role of Automated eGFR Reporting
The widespread implementation of eGFR reporting (since 2006 in the UK) has revolutionised how CKD is perceived, diagnosed and managed by non-nephrologists (but has not been without its share of critics). It has allowed increased recognition in primary care and was a major factor in the addition of CKD to the Quality Outcomes Framework in the UK. In this model, primary care physicians receive financial incentives for the identification, monitoring and some aspects of management of patients with CKD (predominantly blood pressure control). There has been an increase in the diagnosis of CKD, predominantly in the early stages (stage 3A, eGFR 45–59 ml/min/1.73 m2).
Screening Programmes
The principles of a screening programme were first outlined by the World Health Organization in 1968. Kidney disease is amenable to screening as early CKD (the preclinical state) is usually asymptomatic and effective interventions exist (such as blood pressure control) to prevent progression of disease. There are two main questions to consider regarding screening for CKD; what should we measure and in whom should we measure it? The obvious measurement is serum creatinine (and eGFR) but studies (such as PREVEND in the Netherlands) have also assessed albuminuria screening and found even low levels to be highly predictive of subsequent renal decline [5]. Secondly, should we screen the whole adult population or select high-risk patients? The Alberta Kidney Disease Network, in Canada, reported that screening with eGFR was not cost-effective [6]. However, this analysis is extremely dependent on the provision of primary healthcare in the host country, what proportion of patients already underwent testing and therefore what proportion would require additional screening to ensure population coverage. A Scottish study found that 42 % of the adult population had had their serum creatinine checked in the preceding year – in the absence of a formal screening programme [7].
Several groups have now published on the potential benefits of systematic screening of laboratory databases to detect patients with progressive CKD and offer additional interventions. In the Kaiser Permanente system in Hawaii, for instance, the provision of unsolicited nephrology consultations based on the detection of high-risk patients, combined with triage of incoming nephrology consultations to prioritise patients at high risk of progressive CKD, reduced the rate of late referrals markedly, increased the proportion of patients starting haemodialysis with an arteriovenous fistula and increased the proportion of patients starting haemodialysis as an outpatient [8]. A similar programme in Birmingham, UK, in which a nephrologist screened all creatinine reports from patients with diabetes in a single laboratory database, identified those with low or deteriorating eGFR and wrote with unsolicited advice to the doctor who had requested the test, resulted in a fall in the number of patients with diabetes starting RRT [9]. Savings (both monetary and carbon) can be made by a system of electronic consultation, in which nephrologists are given full access to the primary care electronic record of patients with CKD [10].
In the UK at present, there is not a population screening programme for serum creatinine or urinary protein excretion, but regular estimation of kidney function is recommended in people at high risk of developing CKD [11], including those with:
-
Diabetes mellitus
-
Hypertension
-
Heart failure
-
Coronary, cerebral vascular or peripheral vascular disease
-
Chronic multisystem diseases with potential renal involvement – e.g. systemic lupus erythematosus, rheumatoid arthritis and chronic diarrhoeal illnesses
-
A family history of stage 5 CKD or hereditary kidney disease
-
Regular use of drugs that can cause CKD, including nonsteroidal anti-inflammatory drugs, lithium and 5-aminosalicylate derivatives
-
Proteinuria and/or otherwise unexplained haematuria
There is no evidence on which to base recommendations regarding the ideal interval between measurements. For most patients, an annual measurement seems most practicable, but more frequent monitoring will be required with increasing severity of kidney disease.
Detecting a potentially important change in kidney function requires comparison with previous measurements – ideally, all of them, even if generated in several different laboratories (using IDMS traceable values). Graphical display of estimated GFR over time is the easiest way to detect progressive deterioration or, conversely, to show that an apparent recent deterioration in renal function is within the limits of previous fluctuations.
Screening for albuminuria is recommended in specific conditions (most notably diabetes mellitus) and we are likely to see increasing use of proteinuria as a screening test (and for prognostication) in conditions such as hypertension in future.
How Do You Tell Your Patient that They Have CKD?
Although age-related reduction in GFR is common, it is not an inevitable consequence of ageing. Just as low bone density or high arterial blood pressure is common in older people, so is low GFR. Some commentators argue that ‘labelling’ older patients with a low GFR is an example of the medicalisation of normal old age. Given that older patients have higher absolute risks of cardiovascular disease and death, the finding that the relative risks of these events associated with a reduction in GFR is lower in older than in younger adults should not be seen as surprising nor as evidence that a low GFR is harmless. The association of anaemia, hypertension and hyperparathyroidism with reduced GFR is the same in older than in younger adults [12].
However, there is a legitimate concern that ‘labelling’ asymptomatic patients with the ‘diagnosis’ of CKD, based solely on the results of an estimate of GFR, could do harm. This partly depends on what is said to patients, how it is said and by whom.
Let us imagine a 76-year-old patient with a 15-year history of reasonably controlled hypertension, a 3-year history of type 2 diabetes, a urine albumin/creatinine ratio of 1.2 mg/mmol, no dipstick haematuria and an eGFR of 52 ml/min/1.73 m2. She is seen by a general practitioner for medication review. She is told ‘Your blood test shows that you have stage 3 chronic kidney disease. There are 5 stages, and if you reach stage 5 you will either die or need dialysis. I am going to refer you to a specialist, and they will probably send you an appointment’. One would expect that the patient will go home in a state of severe anxiety and spend the time while waiting for the appointment to come through worrying, writing her will, attributing every minor new symptom to kidney disease and ask for repeated checkups at the GP’s surgery. If the same patient were seen by a GP or practice nurse and told ‘As part of our routine checks to make sure that your high blood pressure and diabetes aren’t causing kidney damage, the practice nurse did a blood test the last time you saw her. The blood test gives a rough estimate of how efficiently the kidneys are working to clear waste products from the bloodstream. This estimate is called the ‘eGFR’. A healthy young person usually has an eGFR of around 100. Your eGFR was 52, so you have about 52 % of the kidney function of a young healthy person. This is most likely due to ‘wear and tear’ in the kidneys that has occurred over the years; we know that high blood pressure can make this type of wear and tear more likely. Luckily, there is a lot of reserve capacity in the kidneys, so you are unlikely to become unwell unless the kidney function gets a lot worse. I suggest that we repeat your blood test in 3 months’ time. If the next eGFR is also below 60, that will mean that you will be said to have ‘stage 3 chronic kidney disease’. When we use the word ‘chronic’, we don’t mean ‘bad’, we just mean that the condition has been the same for at least 3 months. So long as we keep your blood pressure and diabetes under control, it is very unlikely that your kidney function will get worse – but it’s worth us keeping an eye on this every 3 months or so. Do you have any questions?’ This patient may ask questions but is much less likely leave feeling anxious or ‘labelled’. This may look like a long explanation but takes less than 90 s to say. If backed up by a patient information leaflet or, even better, an individualised care plan (an example of this My Kidney Care Plan designed by Katy Gerald is given in the Appendix to this chapter), this investment of time is likely to improve the patient’s understanding of her condition and her adherence to recommended lifestyle and drug treatment and improve long-term outcomes.
Specialist Referral
Given the increasing ascertainment of CKD (and possibly a true increase in prevalence), the vast majority of patients with CKD are cared for in primary care. Most kidney units will have local guidelines for primary care providers regarding referral of patients with CKD which are tailored to local circumstances and we do not seek to replace these here. However, some fundamental principles apply. Most importantly, there should be ‘value added’ for the patient by their attendance at a hospital clinic. Practically this means that three broad groups of patients should be seen regularly in nephrology clinics: patients requiring specialist management of glomerular or tubular disease (e.g. immunosuppression for vasculitis); patients with evidence of complications, such as renal anaemia or secondary hyperparathyroidism requiring specialist management (which usually manifest in CKD stage 4 onwards and are certainly rare in stage 3A); or those with progressive kidney disease (requiring RRT planning). These groups will derive additional benefit from seeing the renal multidisciplinary team in a hospital setting. However, the person with stable CKD stage 3A without proteinuria and controlled blood pressure may find attendance at hospital clinics a stressful burden without any discernible improvement in outcome compared to the monitoring that can be provided in primary care.
Finding Patients with Treatable Causes
It is essential to pause (perhaps only briefly) to consider treatable causes before moving on to the next step in the management of a patient with CKD. The great majority of patients with CKD have nephrosclerosis in association with generalised vascular disease and hypertension. This is not associated with haematuria, and seldom with clinical proteinuria, although moderate increases in albumin excretion are common. Treatment requires control of cardiovascular risk factors and avoidance of further damage to the renal circulation, including avoidance of acute kidney injury and nephrotoxicity. However, it is dangerous to assume that CKD is due to nephrosclerosis without some effort to exclude causes that may require specific treatment – particularly because in some instances such treatment may be curative or at least prevent further deterioration. This aspect of management was not emphasised in the original 2002 classification of CKD and it became commonplace to see patients being described as having ‘CKD’ as the sole diagnosis with no effort to exclude treatable causes. This has been addressed to a certain extent in the new 2012 KDIGO guidelines with the introduction of the CGA classification (cause, GFR, albuminuria) which re-emphasises the importance of seeking the cause of the kidney disease [3]. Often this will be apparent on detailed history and examination, and the clinical findings can be augmented by (a relatively small number of) investigations.
If your patient has an active urinary sediment (i.e. blood and protein on dipstick urinalysis), this may be suggestive of a glomerular disorder and a number of serological markers can be measured. Testing for myeloma may also be undertaken, but the yield is low in the absence of any suggestive features (such as hypercalcaemia, bone pain). The finding of a paraprotein band in the absence of any clinical features of myeloma may represent a monoclonal gammopathy of uncertain significance (MGUS) and lead to further investigations and anxiety, so the testing should not be undertaken routinely without careful consideration. It is equally important in a patient with established CKD to exclude any superimposed causes of an unexpected decline in function (see Table 48.2). Commonly this may be an episode of hypotension or sepsis particularly in a patient receiving renin-angiotensin blockade, but sometimes important reversible causes intervene and it is the nephrologist’s job to identify these and postpone ESRD. Graphing reciprocal creatinine or log creatinine will highlight those that have deteriorated unexpectedly from their trajectory; this is not routine practice for most units but should be an absolute requirement of any new renal software.
Radiology
There is very little literature to guide a recommendation regarding who should undergo renal imaging in a cohort with CKD. A pragmatic recommendation would be that patients should have imaging performed if they have any of the following ‘high-risk’ features:
-
1.
History of urological disease
-
2.
Lower urinary tract symptoms
-
3.
Visible or non-visible haematuria (>trace on two occasions in the absence of confirmed UTI)
-
4.
Unexplained flank pain
-
5.
Recurrent UTIs (or single episode of pyelonephritis)
-
6.
Rapidly deteriorating renal function (>5 ml/min/1.73 m2 per annum)
-
7.
eGFR <30 ml/min/1.73 m2
-
8.
Family history of renal disease
-
9.
Suspicion of malignancy (e.g. to exclude pelvic mass or lymphadenopathy causing extrinsic compression)
-
10.
Abnormal physical examination
This is not intended to be an exhaustive list and clinical judgement will dictate other instances where a renal tract ultrasound is indicated. However, the salient point remains: the yield of structural abnormalities will be extremely poor in low-risk patients (e.g. those with stable CKD stage 3, negative urinalysis and no other history or symptoms suggestive of the causes listed above) and therefore they do not automatically require imaging of their renal tract. On the other hand, ultrasound scans are noninvasive, relatively cheap, give some idea of prognosis depending on kidney size and can also assess bladder emptying which may impact on subsequent progression or transplantation.
Ultrasound scanning remains the initial radiological investigation of choice; it is cheap, noninvasive and in skilled hands can be very helpful in diagnosing CKD and excluding obstruction. The quality of the scanning is critical however and ‘normal kidneys’ may well not be, and there is considerable interobserver variation in sizes which might prejudice management. Any degree of hydronephrosis indicates obstructive nephropathy until proved otherwise: if there is a history of previous long-standing obstruction or reflux nephropathy, additional investigations (e.g. dynamic isotope renography or even a trial of nephrostomy drainage) may be required. The degree of dilatation is not a reliable predictor of the severity of obstructive nephropathy, and case series exist of obstructive nephropathy without any detectable dilatation, caused by encasement of the kidneys and ureters by tumour or fibrosis. Although hydronephrosis usually resolves after relief of obstruction (e.g. by catheter drainage in patients with bladder outflow obstruction), this can take several days.
Renal size and echogenicity are also helpful. Using ultrasound, renal size is usually estimated from the length from upper to lower pole; these measurements can be unreliable, however, particularly in the presence of obesity, and are operator-dependent. Renal length should ideally be reported relative to body height (as taller patients have longer kidneys [13]), but this is seldom done in routine practice. Increased echogenicity is a feature of chronic kidney disease and correlates with interstitial fibrosis [14].
Renal asymmetry (often defined as a discrepancy of renal length of >1 cm) can occur for several reasons, including:
-
Renal artery stenosis
-
Reflux nephropathy
-
Renal parenchymal loss due to previous obstruction, e.g. due to stone disease
-
Artefacts caused by observer error (e.g. failure to image the long axis of the kidney; inclusion of renal cysts)
Increased renal size can occur as a result of infiltration, for instance, by lymphoma or amyloidosis.
CT scanning gives more accurate information about renal volume, which in health is closely related to body surface area and is a better predictor of measured GFR than creatinine-based estimating equations [15]. Contrast-enhanced CT is occasionally valuable, for instance, in suspected renal embolism and in IgG4-related tubulointerstitial nephritis.
Renal Biopsy
The role of renal biopsy in diagnosis of chronic kidney disease remains poorly defined [16]. When discussing whether to proceed to kidney biopsy with patients who have CKD, clinicians should ensure that the discussion takes into account the risks – mostly related to bleeding – and the potential benefits. The benefits can be hard to define. ‘Just having a diagnosis’ is not usually enough. A biopsy can usually be justified easily if it might result in a diagnosis that would alter management in such a way that may affect the outcome importantly – for instance, if there is a possibility of lupus nephritis, idiopathic membranous glomerulonephritis or interstitial nephritis. It can also be valuable to establish a diagnosis early in patients who might become candidates for kidney transplantation, particularly if there is a risk of disease recurrence in the graft.
Predicting Progression
Measuring Progression
In routine clinical practice, changes in excretory kidney function are monitored by serial measurement of serum creatinine concentration. Assuming that the patient’s creatinine generation rate has remained constant, a rise in serum creatinine concentration denotes a fall in GFR, and vice versa. However, this assumption does not always hold true. Creatinine generation rate falls in acute illness [17]. Even in chronic, stable disease, it is possible that some apparent alterations in GFR are in fact caused by alterations in tubular secretion of creatinine.
Risk Factors for Progression
Identifying, and correcting, modifiable risk factors for progressive loss of GFR in patients with CKD is the cornerstone of preventive management.
Proteinuria
The most well-established risk factor is proteinuria and there is a strong dose response relationship between the quantity of urinary protein and the rate of progression of renal decline. It is also very well established that low-level albuminuria is a risk marker for progressive kidney damage amongst patients with type 1 and type 2 diabetes, and the same holds true for people without diabetes [18].
KDIGO have developed user-friendly ‘heat maps’ which stratify risk of developing progressive CKD and end-stage kidney disease according to eGFR and proteinuria. There is a powerful multiplicative relationship between reduced excretory function, proteinuria and risk (see Fig. 48.1). Interestingly the ‘heat maps’ are also very similar for the outcomes of all-cause mortality, cardiovascular mortality and AKI [3].
Relationship between proteinuria and risk of end stage kidney disease at moderately reduced eFGR (Data adapted from KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease (http://www.kdigo.org/clinical_practice_guidelines/pdf/CKD/KDIGO_2012_CKD_GL.pdf))
Hypertension
Hypertension is common in CKD and is associated with poorer outcomes. Experimental studies have shown that, in CKD, systemic hypertension is transmitted to the glomeruli: the resulting glomerular hypertension is damaging to the kidney, resulting in glomerulosclerosis and accelerated decline in kidney function. There is a strong relationship between hypertension and proteinuria: interventions for the former will impact on the latter.
Others
Other potentially important modifiable risk factors include:
-
Glycaemic control in diabetes
-
High dietary protein intake
-
Obesity
-
High fructose intake
-
Hyperuricaemia
-
Low fluid intake
-
Cigarette smoking
Non-modifiable risk factors include age, male gender and non-White ethnic origin.
Prediction Equations
There has been work over the past few years to produce models that can predict an individual’s risk of reaching end-stage kidney disease. A recent publication demonstrated the utility of a model with age, sex, eGFR, albuminuria, serum calcium, serum phosphate, serum bicarbonate and serum albumin. The authors highlight that these variables are routinely measured in clinical practice and, while the equation requires external validation prior to widespread use, could easily be incorporated in a laboratory reporting system [19].
Clinical Management of CKD: Prevention of Progression
Non-pharmacological Measures
Patient Activation
Patients with a chronic disease live with it 24 h a day, 365 days a year, and interact with health professionals for a tiny fraction of that time – four 15-min consultations per year for a patient with stable stage 4 CKD would probably be a generous estimate. There is a growing body of evidence that patients with chronic diseases who feel that they control their disease have better outcomes (e.g. adherence to drug treatment or dietary restrictions, lower consultation and hospitalisation rates) than those who feel that their disease controls them. Patient ‘activation’ or ‘empowerment’ are terms used to denote this sense of being in control. Sceptics might argue that both higher levels of patient activation and better outcomes might be caused by underlying factors such as educational attainment – and most would recognise the stereotype of the well-educated middle-class professional who attends an outpatient clinic armed with internet printouts about their disease. However, there is also good evidence that specific interventions – such as provision of personalised care plans, education sessions or coaching – can increase patient activation, irrespective of baseline health literacy. One specific example of such an intervention in the UK is the Renal PatientView website (www.renalpatientview.org.uk) which gives patients secure web-based access to their test results and clinic letters.
Co-operation with Primary Care and Other Secondary Care Disciplines
Many patients with CKD interact mainly with their primary care physician, with only intermittent input from a nephrologist. Many will also have intermittent input from other specialists, for example, cardiologists, diabetologists and vascular surgeons. This system, even in a single-payer system like the UK NHS, generates the potential for waste, duplication and confusion. For instance, a nephrologist may repeat tests (creatinine, glycated haemoglobin, full blood count) that may have been performed recently by the GP, subjecting the patient to unnecessary venipuncture and generating additional cost. Often this is done simply because the nephrologist and the GP are using different information systems – so one-off investment in computerised linkage between these systems is likely to generate major savings and improvements in clinical care. The introduction of joint hospital clinics can reduce duplication within secondary care, the most common example being a joint renal-diabetes clinic where patients can see physicians from both specialties and other members of the multidisciplinary team with crossover, such as dieticians. This can improve the management of joint targets, reduce waste and improve the patient pathway.
A situation of great concern is when a doctor is unaware that the patient has CKD and plans an intervention that carries significant risks – for instance, intravascular contrast administration for angiography, causing oliguric renal failure requiring dialysis, or the prescription of renally excreted drugs without dose adjustment. The most important intervention to reduce these risks is to ensure that the patient is ‘activated’ and has a clear understanding of their disease – preferably in the form of a written care plan.
Clear communication between professionals is also extremely important. It is commonplace, for instance, for recommendations to be made about changes in regular drug treatment when a patient attends a specialist clinic. Unless precise actions are specified, the GP may wait for the patient to request a new prescription, while the patient may be waiting to hear from the GP. The same is true of requests to monitor kidney function between visits; unless it is precisely specified who should arrange the blood test, and how the result should be brought to the attention of the right clinician, such arrangements can cause false reassurance. This is particularly true when test results need to be interpreted in the context of previous test results or recent changes in treatment – for instance, a GP may consider an Hb of 13.5 g/dl normal, but in a patient on treatment with ESAs, this result would usually trigger a dose reduction, depending on previous results and dose changes.
Salt Intake
There is overwhelming evidence in the general population that high dietary intake of salt (as sodium chloride) is associated with hypertension. Low dietary intake of potassium is also important, and the ratio of sodium to potassium intake is a better predictor of blood pressure.
The conventional wisdom, until recently, has been that high salt intake causes extracellular volume expansion and that hypertension results from this change in extracellular volume. Volume expansion, in turn, stimulates production of ouabain-like pressor hormones (e.g. marinobufagenin) that restore sodium balance at the expense of higher blood pressure. However, it has been known for many years that positive sodium balance does not result in the expected change in body weight or extracellular volume. It is now clear that retained sodium is largely stored in non-osmotically active form by binding to polyanionic glycosoaminoglycans, synthesised in response to positive sodium balance. The pathological consequences of non-osmotic salt storage are now being explored; they may include, for instance, changes in conduit artery function [20].
In patients with CKD, there is limited, observational evidence for the benefits of dietary salt restriction. Amongst patients with functioning kidney transplants, for instance, there was a positive association between 24 h urine sodium and blood pressure [21]. There is good evidence that dietary salt restriction amplifies the antiproteinuric effect of renin-angiotensin system inhibition [22]. Most studies reporting an association between unusually low sodium intake and adverse outcomes can be explained by inadequately rigorous assessment of sodium intake or excretion or are confounded by the association between ill health and low dietary intake of all nutrients, including salt. However, there may well be a lower limit for safe sodium intake [23]. In patients with diabetes mellitus, there is high-quality observational evidence that a low dietary salt intake may be associated with harm [24]. Enhanced proximal reabsorption of sodium, a feature of diabetic kidney disease, may be part of the explanation: a low salt intake, combined with avid proximal reabsorption, will result in decreased delivery of salt and water to the macula densa, increasing tubuloglomerular feedback and worsening glomerular hyperfiltration.
Exercise
Physical inactivity is associated with increased mortality amongst patients with CKD, just as it is amongst patients without CKD. A Cochrane review found that regular exercise has significant benefits for physical fitness, walking capacity, blood pressure, health-related quality of life and some nutritional parameters for patients with CKD [25].
Avoidance of Acute Kidney Injury Superimposed on CKD
‘Primum non nocere’.
Patients with CKD are at higher risk of developing AKI than the general population, more likely to require RRT for AKI and less likely to recover renal function. Having responsive systems in place to rapidly identify any deterioration and act upon it may substantially delay the need for dialysis or death. It is critical to identify or exclude reversible causes in patients who have unexplained deterioration in their CKD. Common examples of this are superimposed obstructive uropathy (especially in elderly men), urinary tract infection, medication (TIN, direct toxic effect) and pre-renal causes including reduced intravascular volume and cardiac output. Avoiding or minimising any renal insult is paramount, especially those that are iatrogenic. The specifics of this are embedded in the appropriate sections (such as the recognition of risk associated with the administration of iodinated contrast [described above] and alterations of drug dosing [below]). However, the principle of non-maleficence, in this context, is so important it bears repeating.
Pharmacological Measures
Antiproteinuric Treatment
If a renal biopsy has revealed a specific glomerular lesion as the cause of proteinuria (such as minimal change disease), then targeted therapy such as corticosteroid is indicated. However, there are also nonspecific antiproteinuric treatments regardless of the underlying cause. There is a strong interaction between blood pressure and proteinuria. Lowering systemic blood pressure (using any antihypertensive agent) reduces intraglomerular hypertension and reduces proteinuria. However, blockade of the renin-angiotensin system has specific antiproteinuric effects, in excess of blood pressure lowering alone.
Inhibitors of the Renin-Angiotensin-Aldosterone System (RAAS)
A clear understanding of the effects of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) on kidney function in CKD is important. They are the first line of drug treatment in patients with proteinuric CKD, particularly in the presence of hypertension. Although this is an oversimplification (and ignores, for instance, antifibrotic actions via TGF-beta), it is useful to assume that the protection that these drugs provide against progressive loss of renal function is associated with their capacity to reduce intraglomerular pressure by causing preferential vasodilatation of the efferent arteriole. (We explain this to patients by saying that the excess protein in the urine is a sign that there is high pressure in the kidney filters, caused by kidney disease, making the filters work harder than normal: reducing the pressure on the filters allows them to last for longer, ‘giving the kidneys a rest’.) This haemodynamic action results in an acute fall in GFR. Post hoc analyses of trials amongst patients with diabetes show that the early fall in GFR, and the early fall in albumin excretion, are both predictive markers of long-term stability of kidney function [26]. However, it remains uncertain whether titrating antiproteinuric drug treatment against proteinuria results in better outcomes. Only one small trial has tested this strategy: titration of the dose of Benazepril or Losartan against proteinuria conferred greater benefit than standard doses, despite similar blood pressure control [27].
However, there are potential risks to maximising RAAS blockade: the RAAS plays an important part in autoregulation of renal blood flow and GFR, and acute hypotension and sepsis may be more likely to result in acute kidney injury in the presence of RAAS blockade.
In the presence of renal artery stenosis, or other conditions causing generalised renal under-perfusion, GFR is maintained solely by intense vasoconstriction of the efferent arteriole. In this setting, ACEIs and ARBs can cause acute kidney injury, which may be irreversible despite withdrawal of the drug. Therefore, a serum creatinine and potassium measurement is generally recommended 7–10 days following the introduction or dose titration of RAAS blockade and drug withdrawal if serum creatinine has risen >20 % or serum potassium >6.0 mmol/l. The large ONTARGET study of dual renin-angiotensin system blockade of patients at low renal risk (low prevalence of proteinuria in the cohort) found no improvement in renal outcomes in the dual blockage group but there was an excess of AKI requiring renal replacement therapy [28]. This finding has now been confirmed in a study of patients with type 2 diabetes mellitus and albuminuria. Patients were randomly allocated to receive losartan alone or losartan plus lisinopril; there was no difference in the primary end-point of fall in eGFR between treatment groups but the study was stopped due to safety concerns regarding hyperkalaemia and acute kidney injury in the dual blockade group [29].
Some clinicians have introduced ‘sick day rules’ for patients receiving RAAS blockade and counsel their patients to withhold these medicines if they have an acute intercurrent illness (the verbal warning may also be supported by written information). This intervention has biological plausibility but has not been tested in a randomised controlled trial and may have unintended consequences.
Non-dihydropyridine Calcium Channel Blockers
Non-dihydropyridine calcium channel blockers (such as diltiazem) may also have a beneficial effect on proteinuria when used in conjunction with an ACEi. They are effective antihypertensive agents in renal disease and have a superior antiproteinuric effect when compared to dihydropyridine calcium channel blockers (such as amlodipine) and some advocate their greater use in renal disease [30].
Antihypertensive Treatment
Blood pressure targets (and the agents used to achieve them) should be individualised to the patient according to their age, comorbidity, risk of progression of CKD, presence of pre-existent cardiovascular disease and diabetes. Excellent international guidelines written specifically for patients with CKD are available on this topic from the KDIGO website (www.kdigo.org). Particular recommendations of note: a lower blood pressure target (≤130 mmHg systolic and ≤80 mmHg diastolic) is recommended if urine albumin excretion exceeds 30 mg/day (or equivalent) regardless of a coexistent diagnosis of diabetes. However, if urine albumin is <30 mg/day (or equivalent), then a less stringent blood pressure target of ≤140 mmHg systolic and ≤90 mmHg diastolic is recommended, regardless of a coexistent diagnosis of diabetes.
Metabolic Acidosis
Metabolic acidosis is common in stage 4–5 CKD and is associated with multiple metabolic derangements including muscle wasting and loss of bone density and also with increased tubular ammoniagenesis, which may cause tubular damage and contribute to progressive loss of GFR. Several studies now support the hypothesis that correction of metabolic acidosis by sodium bicarbonate supplementation improves nutritional status and slows progression, and the KDIGO CKD guidelines suggest that patients with CKD and a serum bicarbonate concentration of <22 mmol/l should be treated to maintain serum bicarbonate within the normal range [3]. Larger studies are awaited.
There is good evidence that increased intake of sodium in the form of sodium bicarbonate does not result in volume expansion or worsening of hypertension amongst patients with CKD; these effects are only seen with increased sodium chloride intake. Although this has been known for more than 30 years [31, 32], the precise physiological explanation remains unclear but must relate in some way to renal chloride handling.
Hyperkalaemia
Hyperkalaemia is a common problem in CKD, particularly diabetics who may have an element of type 4 renal tubular acidosis (hyporeninaemic hypoaldosteronism) but also patients treated with RAAS blockade. Managed badly, this can result in multiple admissions with hyperkalaemia often with inappropriate doses of insulin and dextrose, stop-starting of important drugs and increased levels of anxiety. Careful, thorough culture-specific dietary advice is valuable in patients with persistent problems and patient information leaflets should be readily available for those with minor hyperkalaemia. Correction of chronic acidosis (see above) and addition of diuretics are often very helpful medium-term solutions. In type 4 RTA, the renin production is suppressed by real or apparent volume expansion, and the addition of a thiazide diuretic (in full dose) can combat this and concurrently improve the hyperkalaemia. In those with recurrent hyperkalaemia who are taking RAAS blockade, a careful review of the balance of risk and benefit is required, once other reversible causes have been dealt with. Clear guidelines on acceptable and not-acceptable hyperkalaemia need to be available for those encountering patients with CKD, and education on this front is an important task for nephrologists.
Dyslipidaemia
A meta-analysis of statins and albuminuria found that they may have a beneficial effect on pathological albuminuria, but the quality of the evidence was poor [33]. Treating dyslipidaemia in CKD, using an HMG Co-A reductase inhibitor (statin), with or without a selective cholesterol absorption inhibitor (e.g. ezetimibe), has not been shown to retard the progression of CKD in the study of heart and renal protection (SHARP) and the protection against nephropathy in diabetes with atorvastatin (PANDA) studies, respectively [34, 35]. The role of these drugs in cardiovascular risk reduction in CKD is discussed elsewhere.
Other Drug Therapy
It is important for prescribers to recognise impaired excretory renal function for two reasons; firstly, to avoid drug accumulation in renally cleared drugs (such as excess bleeding with low-molecular-weight heparins when eGFR <30 ml/min/1.73 m2) and to avoid renal toxicity at inappropriate doses (such as gentamicin). A calculated creatinine clearance is often preferred to eGFR for drug dosing purposes because it is not normalised to body surface area.
Fibrates
Most fibrates, with the possible exception of gemfibrozil, can cause a reversible increase in urea and creatinine concentration. In some patients, a progressive rise over time has also been demonstrated. Studies in people with normal kidney function have not demonstrated an effect of fibrates on isotopically measured GFR, but no such studies have been done in patients with CKD. Very few patients with CKD 3–5 were included in the FIELD and ACCORD studies. One study suggests that fibrates increase the rate of release of creatinine from muscle; this would explain a rise in creatinine, but not a progressive rise over time, nor a rise in serum urea concentration. In patients with CKD, it is probably safe to ignore a small, stepwise increase in serum creatinine concentration following the initiation of fibrate therapy, particularly if the serum urea concentration is unchanged; however, if there is a progressive rise in creatinine over time, particularly if accompanied by a rise in urea, the drug should be stopped.
Trimethoprim and Cimetidine
Trimethoprim and cimetidine inhibit the tubular secretion of creatinine. The use of trimethoprim in a patient with CKD can result in a marked rise (20–50 %) in serum creatinine concentration and fall in estimated GFR, without any change in true GFR. A clinician who does not understand what is happening may think that the patient has acute kidney injury and arrange unnecessary admission, invasive investigations, etc. Although no systematic studies have been reported, in our experience the serum creatinine can remain above baseline for at least 14 days after completion of a course of full-dose trimethoprim. Trimethoprim also reduces renal potassium excretion (through an amiloride-like action), and clinically apparent hyperkalaemia may be observed. This is of particular importance in patients with CKD and/or taking other drugs associated with hyperkalaemia (such as RAAS blockade) and the balance of risk versus benefit should be considered before prescribing trimethoprim in this context. The effect is dose-dependent: high doses used for treatment of Pneumocystis infection, for instance, are much more likely to cause hyperkalaemia.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs inhibit the action of vasodilator prostaglandins that play a major role in maintaining GFR, particularly in the presence of pre-existing CKD. Therefore, all NSAIDs can cause salt and water retention, a fall in GFR and hyperkalaemia. These effects are amplified amongst patients with effective or true hypovolaemia, those on RAAS blockade and in sepsis. These drugs must be used with great care in patients with CKD, who should be warned not to buy NSAIDs over the counter. However, an absolute ‘ban’ on prescription of these drugs in all patients with CKD is neither practicable nor justified. In some patients with severe osteoarthritis, for instance, in whom paracetamol is ineffective and opiate-based analgesics cause unacceptable adverse effects, it is reasonable to prescribe NSAIDs even in the presence of CKD4 so long as kidney function, blood pressure and fluid status are monitored carefully and regularly.
NSAIDs can also cause minimal change nephrotic syndrome and interstitial nephritis, but these are idiosyncratic reactions and may be drug-specific.
Aminoglycosides
As part of the drive to reduce hospital acquired infections, such as Clostridium difficile infection, there has been a switch from broad spectrum antibiotics to aminoglycoside antibiotics (especially gentamicin), with some hospitals seeing gentamicin prescribing doubling [36]. If monitored appropriately and dose alterations are made in light of changing renal function, gentamicin can be administered safely to patients with CKD. This requires multidisciplinary working between medical, nursing and pharmacy colleagues. Nephrotoxicity has not been shown to occur with single doses given as prophylaxis.
Clinical Management of CKD: Preparation for End-Stage Renal Failure
Multidisciplinary Education Programmes
Initiating renal replacement therapy (RRT) is a major life change, with practical, social, psychological and financial consequences as well as physical consequences. Physicians who focus solely on the physical consequences (e.g. treatment of anaemia, acidosis, hypertension and phosphate retention) are therefore missing the ‘bigger picture’ – and, when patients do not always adhere to complex drug treatments, may blame the patient for ‘poor compliance’ when in reality, the patient is struggling to cope with other aspects of their life and accords low priority to drug treatments that might affect their health some time into the future (think of Maslow’s hierarchy of needs – food is a basic need but a low-potassium, low-phosphate, fluid-restricted diabetic diet accompanied by the correct timing of insulin therapy before the meal and a phosphate binder afterwards is a need of a different magnitude. It requires a complex interplay of financial resources, strict dietary modification, memory, eyesight, manual dexterity, time, organisation and patient motivation).
While there is no reason in principle why doctors should not be trained, and given time, to address the ‘nonbiological’ aspects of coping with CKD and RRT, they are an expensive resource, and there is evidence that the most cost-effective way of preparing patients with CKD for major decisions about RRT is to provide a multidisciplinary clinic. Patients may meet other patients in small groups, including patients who have experienced various RRT modalities, nursing staff with expertise in patient education, psychologists, dietitians and others. Several observational studies have found that patients who have attended a multidisciplinary clinic are better informed and better prepared for RRT than similar patients attending conventional medical clinics. A nonrandomised comparison of a formal education programme (‘RightStart’) with standard care found improved morbidity and mortality over the first year after starting RRT [37]. A randomised trial in Canada amongst relatively low-risk patients with CKD not previously known to nephrologists found no clear evidence that multidisciplinary care slowed progression or improved management of complications compared to care by primary care physicians [38] but proved cost-effective largely due to a lower number of days in hospital; patients receiving multidisciplinary care reported a higher quality of life [39].
Identification and Workup of Patients Suitable for Transplantation
This is an important area and often delivered in an inconsistent manner. For most young patients, preemptive transplantation, ideally with a live donor transplant, is the treatment of choice when approaching ESRD. There are caveats and conditions around this but early assessment and education of appropriately selected patients is important. Strategies to avoid blood transfusion and advice on contraception in women of childbearing age are very important to avoid sensitisation.
Shared Decision-Making: Patient Decision Aids
Patients with CKD will be faced with numerous ‘medical’ decisions over the course of their life with CKD – some of which are listed in Table 48.3. For some decisions, the choice is straightforward, because of strong evidence that the outcomes are better with one choice than with the other. In guidelines using the GRADE classification, these options will be given as level 1 recommendations and will normally be supported by level A or B evidence. However, many other options are based on weaker evidence, will be given as level 2 suggestions, and will normally have level C or D evidence in support. The definition of a ‘suggestion’ for patients is ‘The majority of people in your situation would want the recommended course of action, but many would not’. For clinicians, the definition reads ‘Different choices will be appropriate for different patients. Each patient needs help to arrive at a management decision consistent with her or his values and preferences’.
Achieving high-quality shared decisions with patients about aspects of CKD care is morally the right thing to do, but there are also important pragmatic reasons. Patients who feel ‘ownership’ of the decision are more likely to implement it – improving adherence to treatment. Patients who are ‘activated’ to take control over their own treatment will require less support, in the medium term, than those who are the passive recipients of patriarchal, ‘doctor knows best’ care.
Achieving shared decision-making in practice is culturally disruptive both for caregivers and for patients. Doctors, for instance, have more knowledge about the risks and benefits of the various options than patients can possibly have; patients used to conventional medical care may well reply ‘you’re the doctor, you should know what’s best for me’. Accepting these attitudes means that patients will probably spend more time researching their next holiday than they will researching their medical options. One way of facilitating shared decision-making is to encourage patients to participate in their own ‘kidney care plan’. An example of this is shown in the Appendix and can be modified for local bias and individual needs. The version shown is popular with patients and acts as prompt to ensure that the patient is encouraged to voice their wishes.
‘Crashlanding’
Despite all of the efforts, described above, to identify patients with deteriorating renal function, there are still a significant proportion of patients who commence RRT within 3 months of first nephrology consultation (known as ‘crashlanding’). This is particularly challenging for the patient, family and nephrologist. It may be as a result of an unavoidable acute irreversible deterioration (such as anti-GBM disease), or late presentation or late referral. Hospital haemodialysis often becomes the default option for this group of patients, but with appropriate multidisciplinary input, other forms of RRT can still be successfully adopted.
Increasingly patients are also referred with AKI on a background of CKD, often frail, elderly patients with only scant available information on patient preference and functional status. A decision about the benefits of providing acute renal replacement therapy must be made relatively promptly, frequently out-of-hours. These patients deserve careful and thoughtful assessment, and a decision to withhold or commence renal replacement therapy should be made at a senior level.
Conclusion
The recognition of CKD has changed dramatically over the past 15 years with the introduction of eGFR reporting and the introduction of schemes such as the UK Quality and Outcomes Framework. It is no longer a collection of rare diseases looked after by specialists in hospital clinics; it is a common condition predominantly managed in primary care with appropriate support and input from nephrologists. Our current management strategies reflect these changes with greater emphasis on risk stratification, avoidance of AKI and financial incentives to attain blood pressure targets. It is a rapidly evolving field with many exciting developments on the horizon for us and our patients.
References
Methven S, Macgregor MS, Traynor JP, O’Reilly DS, Deighan CJ. Reply to ‘improving the interpretation of protein: creatinine ratios. The impact of creatinine excretion’. Nephrol Dial Transplant. 2011;26(3):1109.
Methven S, Macgregor MS, Traynor JP, O’Reilly DS, Deighan CJ. Assessing proteinuria in chronic kidney disease: protein-creatinine ratio versus albumin-creatinine ratio. Nephrol Dial Transplant. 2010;25:2991–6.
KDIGO Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013;3(1):1.
CKD Prognosis Consortium. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073.
Halbesma N, Kuiken DS, Brantsma AH, Bakker SJ, Wetzels JF, De Zeeuw D, et al. Macroalbuminuria is a better risk marker than low estimated GFR to identify individuals at risk for accelerated GFR loss in population screening. J Am Soc Nephrol. 2006;17(9):2582–90.
Manns B, Hemmelgarn B, Tonelli M, Au F, Chiasson TC, Dong J, et al. Population based screening for chronic kidney disease: cost effectiveness study. BMJ. 2010;341:c5869.
Gifford FJ, Methven S, Boag DE, Spalding EM, Macgregor MS. Chronic kidney disease prevalence and secular trends in a UK population: the impact of MDRD and CKD-EPI formulae. QJM. 2011;104(12):1045–53.
Lee BJ, Forbes K. The role of specialists in managing the health of populations with chronic illness: the example of chronic kidney disease. BMJ. 2009;339:b2395.
Rayner HC, Hollingworth L, Higgins R, Dodds S. Systematic kidney disease management in a population with diabetes mellitus: turning the tide of kidney failure. BMJ Qual Saf. 2011;20(10):903–10.
Stoves J, Connolly J, Cheung CK, Grange A, Rhodes P, O’Donoghue D, et al. Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Qual Saf Health Care. 2010;19(5):e54.
National Collaborating Centre for Chronic Conditions. Chronic kidney disease: national clinical guideline for early identification and management in adults in primary and secondary care. London: Royal College of Physicians; 2008.
Bowling CB, Inker LA, Gutierrez OM, Allman RM, Warnock DG, McClellan W, et al. Age-specific associations of reduced estimated glomerular filtration rate with concurrent chronic kidney disease complications. Clin J Am Soc Nephrol. 2011;6(12):2822–8.
Emamian SA, Nielsen MB, Pedersen JF, Ytte L. Kidney dimensions at sonography: correlation with age, sex, and habitus in 665 adult volunteers. AJR Am J Roentgenol. 1993;160(1):83–6.
Moghazi S, Jones E, Schroepple J, Arya K, McClellan W, Hennigar RA, et al. Correlation of renal histopathology with sonographic findings. Kidney Int. 2005;67(4):1515–20.
Johnson S, Rishi R, Andone A, Khawandi W, Al-Said J, Gletsu-Miller N, et al. Determinants and functional significance of renal parenchymal volume in adults. Clin J Am Soc Nephrol. 2011;6(1):70–6.
Tomson CR. Indications for renal biopsy in chronic kidney disease. Clin Med. 2003;3(6):513–7.
Wilson FP, Sheehan JM, Mariani LH, Berns JS. Creatinine generation is reduced in patients requiring continuous venovenous hemodialysis and independently predicts mortality. Nephrol Dial Transplant. 2012;27(11):4088–94.
Lambers Heerspink HJ, de Zeeuw D. Debate: PRO position. Should microalbuminuria ever be considered as a renal endpoint in any clinical trial? Am J Nephrol. 2010;31(5):458,61.
Tangri N, Stevens LA, Griffith J, Tighiouart H, Djurdjev O, Naimark D, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA. 2011;305(15):1553–9.
Lambers Heerspink HJ, Navis G, Ritz E. Salt intake in kidney disease–a missed therapeutic opportunity? Nephrol Dial Transplant. 2012;27(9):3435–42.
van den Berg E, Geleijnse JM, Brink EJ, van Baak MA, Homan van der Heide JJ, Gans RO, et al. Sodium intake and blood pressure in renal transplant recipients. Nephrol Dial Transplant. 2012;27(8):3352–9.
Lambers Heerspink HJ, Holtkamp FA, Parving HH, Navis GJ, Lewis JB, Ritz E, et al. Moderation of dietary sodium potentiates the renal and cardiovascular protective effects of angiotensin receptor blockers. Kidney Int. 2012;82(3):330–7.
Heerspink HL, Ritz E. Sodium chloride intake: is lower always better? J Am Soc Nephrol. 2012;23(7):1136–9.
Vallon V, Thomson SC. Anomalous role for dietary salt in diabetes mellitus? Nat Rev Endocrinol. 2011;7(7):377–8.
Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011;(10):CD003236.
Holtkamp FA, de Zeeuw D, Thomas MC, Cooper ME, de Graeff PA, Hillege HJ, et al. An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int. 2011;80(3):282–7.
Hou FF, Xie D, Zhang X, Chen PY, Zhang WR, Liang M, et al. Renoprotection of optimal antiproteinuric doses (ROAD) study: a randomized controlled study of benazepril and losartan in chronic renal insufficiency. J Am Soc Nephrol. 2007;18(6):1889–98.
Mann JF, Schmieder RE, McQueen M, Dyal L, Schumacher H, Pogue J, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372(9638):547–53.
Fried LF, Emanuele N, Zhang JH, Brophy M, Connor TA, Duckworth W, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369:1892–1903.
Bakris GL, Weir MR, DeQuattro V, McMahon FG. Effects of an ACE inhibitor/calcium antagonist combination on proteinuria in diabetic nephropathy. Kidney Int. 1998;54(4):1283–9.
Husted FC, Nolph KD, Maher JF. NaHCO3 and NaC1 tolerance in chronic renal failure. J Clin Invest. 1975;56(2):414–9.
Weinberger MH. Sodium chloride and blood pressure. N Engl J Med. 1987;317(17):1084–6.
Douglas K, O’Malley PG, Jackson JL. Meta-analysis: the effect of statins on albuminuria. Ann Intern Med. 2006;145(2):117–24.
Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (study of heart and renal protection): a randomised placebo-controlled trial. Lancet. 2011;377(9784):2181–92.
Rutter MK, Prais HR, Charlton-Menys V, Gittins M, Roberts C, Davies RR, et al. Protection against nephropathy in diabetes with atorvastatin (PANDA): a randomized double-blind placebo-controlled trial of high- vs. low-dose atorvastatin(1). Diabet Med. 2011;28(1):100–8.
Helps A, Deighan C, Gourlay Y, Seaton RA. Gentamicin and acute kidney injury requiring renal replacement therapy in the context of a restrictive antibiotic policy. J Antimicrob Chemother. 2011;66(8):1936–8.
Wingard RL, Pupim LB, Krishnan M, Shintani A, Ikizler TA, Hakim RM. Early intervention improves mortality and hospitalization rates in incident hemodialysis patients: RightStart program. Clin J Am Soc Nephrol. 2007;2(6):1170–5.
Barrett BJ, Garg AX, Goeree R, Levin A, Molzahn A, Rigatto C, et al. A nurse-coordinated model of care versus usual care for stage 3/4 chronic kidney disease in the community: a randomized controlled trial. Clin J Am Soc Nephrol. 2011;6(6):1241–7.
Hopkins RB, Garg AX, Levin A, Molzahn A, Rigatto C, Singer J, et al. Cost-effectiveness analysis of a randomized trial comparing care models for chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(6):1248–57.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix
Appendix
My Kidney Care Plan
Name ……………………………….
Hospital number …………………..
Welcome to the Chronic Kidney Disease (CKD) Service (designed by Katy Gerrard)
This is your care plan; it will help all members of your healthcare team (including your GP) to care for you. Hopefully it will also help you understand and get involved in your kidney problems and plans for treatment.
Please bring it with you to every appointment and also if you get admitted to hospital or go to your GP.
The chronic kidney disease team is a group of renal specialists who help manage people with kidney problems. As well as running clinics at the Royal Free Hospital, we also run clinics at Barnet Hospital, Mary Rankin (St. Pancras) and North Middlesex Hospital.
Your nurses are: ………………………………………………………..
Your consultant is: ………………………………………………………………………………………………….
The specialist nurses and doctors in this team work alongside dieticians, social workers, psychologists, your primary care team (GP surgery) and of course you and your family/carers to manage your kidney problems.
We can help with many aspects of kidney problems in our clinic, including:
-
Further monitoring and stabilisation of your kidney function
-
Management of any associated symptoms or complications you may have
-
Anaemia (blood count) management
-
General health and wellbeing promotion
-
Preparation for dialysis
-
Assessing whether you are physically fit enough for a kidney transplant
-
Conservative management if you choose not to have dialysis
We are happy to discuss any/all of the above issues with you and also any other matters you are concerned about. You will still continue to see a renal doctor (specialist) regularly.
All your other day-to-day health problems will still be managed by your general practitioner (GP). We recommend that you take this care plan with you when you attend your GP surgery.
If you need to contact us about any kidney-related problems then you can call us on ………… (office hours). We might not be able to answer your call straight away as we run clinics every day, but we will return your call as soon as we can. If the problem is urgent, then please contact your GP or go straight to your nearest Accident and Emergency.
Lifestyle
There are many things you can do to try and keep yourself healthy:
-
We recommend that you follow a balanced healthy diet and do not eat salty foods or add extra salt to your food.
-
Some patients need to follow specific diets like low potassium or low phosphate; we will advise you, if you are one of these patients – you can use this section of your folder to insert relevant diet sheets. We also have dieticians who you will be able to see. If you want to contact the dieticians, please call ext 31719.
-
It is beneficial to take regular exercise as your condition allows.
-
If you smoke, we strongly advise that you stop as it will damage your kidneys further. Your GP will be able to provide help for you to stop smoking.
-
We recommend that you do not drink too much alcohol; this is no more than 14 units for women and 21 for men per week.
-
It is advisable to be a healthy weight; we will recommend what weight is ideal for you.
-
High blood pressure (BP) damages kidneys further, so it is very important that you make sure your BP is well controlled. We will advise you what your BP should be.
-
If you are diabetic, it is vital that your diabetes is well controlled as high blood sugars will damage the kidneys further; your healthcare team can help you with this.
-
It is advisable that blood is taken from the veins in your hands; if this is not possible, then your dominant arm can be used; this is in case we need to make a fistula for dialysis.
My medication list | |||
|---|---|---|---|
Medication | Dose | Frequency | Function |
| |||
My Test Results
If you would like to know your blood test results, they can be included here.
Target range | __/__/__ | __/__/__ | __/__/__ | __/__/__ | __/__/__ | __/__/__ | |
|---|---|---|---|---|---|---|---|
eGFR | |||||||
Urea | |||||||
Creatinine | |||||||
Calcium | |||||||
Potassium | |||||||
Phosphate | |||||||
Haemoglobin | |||||||
Blood pressure | |||||||
Weight |
Results Key
eGFR | Roughly the percentage of normal kidney functionI have left (on average people need to consider dialysis treatment with a level below 15 %) |
Urea | Waste level |
Creatinine | Waste level |
Calcium | Important for bone strength |
Potassium | A mineral, which if high can cause heart rhythm problems |
Phosphate | Important for bone strength and can cause itching if high |
Haemoglobin | Blood count |
Treatment Options
When/if your kidney function deteriorates, we will need to discuss treatment options. This is in order for us to make plans for your future care. You will be very central to the decision-making process, and so we will need to explain to you in detail about the options. You may wish to make notes about all of the options here.
You can change your decision at any time, but please discuss this with your nurse as soon as possible.
We also suggest that you discuss this with you family/carers.
Peritoneal Dialysis
……………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………
Haemodialysis/Home Haemodialysis
……………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………
Kidney Transplant
……………………………………………………………………………………………………………………………………………………………………………………………………………………………………………
Conservative Management
……………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………
Dates These Options Were Discussed
……………………………………………………..
Decision on Preferred Treatment Option
……………………………………………………….
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Tomson, C.R.V., Methven, S. (2014). Chronic Kidney Disease: Management. In: Harber, M. (eds) Practical Nephrology. Springer, London. https://doi.org/10.1007/978-1-4471-5547-8_48
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5547-8_48
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5546-1
Online ISBN: 978-1-4471-5547-8
eBook Packages: MedicineMedicine (R0)