Abstract
Cobalt–chrome (Co–Cr) is a metal alloy of cobalt and chromium with a very high specific strength. For as long as investment casting has been available as an industrial process, cobalt-based alloys have been used in demanding applications including dental and orthopedic implants [1]. The alloy composition used in orthopedic implants, described in industry standard ASTM-F75, is composed of cobalt with (1) chromium (27–30 %) and (2) molybdenum (5–7 %) and (3) limits on other important elements such as manganese and silicon (<1 %), iron (<0.75 %), nickel (<0.5 %), and carbon, nitrogen, tungsten, phosphorus, sulfur, boron, etc. [1]. Besides cobalt–chromium–molybdenum (Co–Cr–Mo), cobalt–nickel–chromium–molybdenum (Co–Ni–Cr–Mo) is also used for implants (Table 5.1) [2, 3].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Femoral Component
- Ultrahigh Molecular Weight Polyethylene
- Bone Ingrowth
- Porous Coating
- Orthopedic Implant
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Cobalt–Chrome Alloys
Cobalt–chrome (Co–Cr) is a metal alloy of cobalt and chromium with a very high specific strength. For as long as investment casting has been available as an industrial process, cobalt-based alloys have been used in demanding applications including dental and orthopedic implants [1]. The alloy composition used in orthopedic implants, described in industry standard ASTM-F75, is composed of cobalt with (1) chromium (27–30 %) and (2) molybdenum (5–7 %) and (3) limits on other important elements such as manganese and silicon (<1 %), iron (<0.75 %), nickel (<0.5 %), and carbon, nitrogen, tungsten, phosphorus, sulfur, boron, etc. [1]. Besides cobalt–chrome–molybdenum (Co–Cr–Mo), cobalt–nickel–chromium–molybdenum (Co–Ni–Cr–Mo) is also used for implants (Table 5.1) [2, 3].
The possible toxicity of released Ni ions from Co–Ni–Cr alloys and their limited frictional properties have been a matter of concern in using these alloys as articulating components. Thus, Co–Cr–Mo is usually the dominant alloy for total joint arthroplasty [3]. Co–Cr–Mo alloys can withstand high temperatures and have a high wear resistance. The alloy is especially used where high stiffness or a highly polished and extremely wear-resistant material is required. It can be used in gas turbines, valve seats, nuclear power plants, automotive engines, aerospace fuel nozzles, engine vanes, and other components, most importantly in a variety of medical prosthetic implant devices, such as knee implants, metal-to-metal hip joints, and dental prosthetics due to its high biocompatibility [1]. The increased stability and excellent material properties of Co–Cr alloys are advantageous for long-term durability and thus are a promising advance for younger patients in need of total joints.
Porous Metallic Coatings
For a number of years there has been increasing interest in surface treating orthopedic implants in an attempt to improve implant fixation. Various coatings have been manufactured. Porous metallic and ceramic coatings deposited on implants facilitate implant fixation and bone ingrowth. Implant surfaces modified by ion implantation or physical vapor deposition exhibit superior hardness and wear resistance. Polymeric coating formulations are used to enhance biocompatibility and biostability, thrombo-resistance, antimicrobial action, dielectric strength, and lubricity make medical devices used within the body more visible to ultrasound and for delivery of drugs [4]. It is well known in the medical arts for providing a metallic bone prosthesis with a porous metallic coating to enhance the fixation of the prosthesis to the patient’s bone. Such fixation is generally achieved by either cementation or bone tissue ingrowth. Bone cement or freshly grown bone tissue occupies pore volume in the porous coating and thereby serves to lock the prosthesis in place. Until the 1970s, polymethyl methacrylate bone cement was the predominant means to fix a joint replacement implant to bone. This fixation is primarily mechanical. Cement penetrates the cancellous bone and locks onto small surface irregularities on the implant. In contrast, fixation by bone ingrowth has been recommended by many orthopedic researchers as a means of eliminating or alleviating several disadvantages associated with fixation by bone cement (such as premature loosening of the prosthesis, tissue reaction with the bone cement, the need to remove a substantial amount of bone to provide space for the cement mantle). However, failure of a bone tissue ingrowth fixation of cementless implants, which would lead to premature loosening of the implant, remains a matter of concern. In a metallic prosthesis comprising a porous coating extending over a nonporous substrate, such failure can occur at the substrate–porous coating interface, within the porous coating or within the patient’s bone outside the coating.
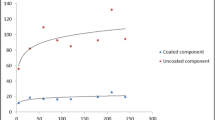
A variety of different porous metallic coatings have been proposed for enhancing the fixation of a metallic prosthesis by bone ingrowth. Three types of porous metallic coatings are currently available: (1) beaded, sintered Co–Cr coatings on a Co–Cr substrate (Fig. 5.1); (2) beaded, vacuum-sintered titanium coatings on a titanium substrate; and (3) vacuum-sintered titanium fiber mesh pads on a titanium substrate. Three items adequately characterize these types of porous coatings: (1) the materials used and any standards to which they conform; (2) the static shear strength of the coating to the substrate (ASTM F1044); and (3) the average bead and pore size, overall pore volume, the number of bead layers, and the thickness of the coating [4].
Forms and Fabrication Techniques
The porous coatings can take various forms and require different technologies. Co–Cr porous coatings can be produced from the following: (1) Spherical metal powders made by gas atomization. The tiny spheres, or beads as they are frequently referred to in the medical field, are 175–250 μm in diameter. Porous coatings produced from spherical powders are most frequently used on cobalt–chrome implant materials. (2) Wires or fibers that are formed into porous pads [4]. Sintering involves heating the implant to about one-half or more of the melting temperature of the alloy to enable diffusion mechanisms to form necks that join the beads to one another and to the surface of the implant. In the case of alloy beads, the manufacturer applies the coating material using binders over specific regions of the implant (Fig. 5.2) surface and then attaches the coating to the substrate by various high-temperature sintering stages. The porous coatings so formed (35–50 vol % porosity) are typically 500–1,000 μm thick and consist of a regular three-dimensional interconnected porous structure [5]. Tissue ingrowth into this three-dimensional porous coating results in resistance to shear, compressive, and tensile forces at the bone-implant interface (Fig. 5.3) [6].
Bond Failure of Sintered Porous Coatings
The metallurgical process for adhering the coating to the implant is a complex high-temperature process that requires a series of steps. The challenge is to provide strong bonds between each of the powder spheres (beads) and between the coating and the implant without significantly degrading the strength and corrosion resistance of the component. Proper processing prior to applying the porous coating is also critical for adequate bonding [4, 7].
Ion Implantation
Ion implantation is an approach for modifying the surface properties of materials. It is similar to a coating process, but it does not involve the addition of a layer on the surface. Ion implantation uses a highly energetic beam of ions (positively charged atoms) to modify the surface structure and the chemistry of materials at low temperature. The process does not adversely affect component dimensions or bulk material properties [4, 8]. The ion implantation process is conducted in a vacuum chamber at very low pressure (10−4 to 10−5 torr, or 0.13–0.013 Pa). Large numbers of ions (typically 1016–1017 ions/cm2) bombard and penetrate a surface interacting with the substrate atoms immediately beneath the surface. Typical depth of penetration is a fraction of a micrometer [4, 8]. Titanium and Co–Cr alloy orthopedic prostheses for hips and knees are among the most successful commercial applications of ion implanted components for wear resistance. In use, these components articulate against an ultrahigh molecular weight polyethylene mating surface (acetabular cup). Wear reduction may be further reduced by implantation of nitrogen ions into the alloy [8].
Hydroxyapatite-Coated Co–Cr Porous-Coated Implants
Friedman et al. compared hydroxyapatite (HA)-coated titanium and HA-coated Co–Cr implants in the distal femur of a rabbit model and evaluated bone apposition and interfacial shear strength [9]. The implants were press-fit into the metaphyseal cancellous bone of the lateral femoral condyle in a transverse fashion. The mechanical strength of the interface between HA and bone was measured using the push-out method. No differences were found in the shear strength and the amount of bone apposition between the titanium and Co–Cr implants. The HA-coated Co–Cr implants performed in a similar manner to the HA-coated titanium implants, both mechanically and histologically, suggesting that HA-coated Co–Cr implants deserve further study as a viable alternative to titanium for the biological fixation of total joint components in orthopedic surgery [9].
Biocompatibility of Co–Cr Porous-Coated Implants
The use of Co–Cr–Mo in orthopedic surgery is well tolerated [10]. Nevertheless, the alloy is still considered less biocompatible than titanium [11]. A recent study explored the biocompatibility of Co–Cr–Mo by investigating the biomechanical implant fixation and implant osseointegration of Co–Cr–Mo (ASTM F-75) porous bead-coated and titanium (ASTM F-136) porous bead-coated implants in an animal model. In ten dogs, the two implant types were inserted into the proximal part of the humerus. Implant sites were over drilled, leaving an empty 0.75-mm gap between implant and surrounding bone. The implants were observed for 6 weeks and were evaluated by the biomechanical push-out test and histomorphometry. The authors found a statistically significant 40 % decrease in the biomechanical fixation of Co–Cr–Mo porous bead-coated implants compared with titanium porous bead-coated implants that could be critical for long-term performance. Implant osseointegration was comparable between the two implants; however, a slight decrease in bone volume density around Co–Cr–Mo implants was observed [12].
Outcome of Co–Cr Porous-Coated Implants
Metal-on-metal hip bearings made of Co–Cr–Mo alloy possess excellent wear properties and are a tempting choice for young and active patients [13, 14]. Previous experience suggested that cementless cobalt alloy porous-coated femoral components can achieve durable biological fixation by bone ingrowth for active patients less than 70 years old who have no metabolic bone disease (Fig. 5.4) [15]. Engh and Bobyn have shown that circumferential coating of more than half the femoral stem results in proximal bone atrophy [16]. Other authors reported the outcome of a porous-coated Co–Cr femoral component (Tri-lock; DePuy, Warsaw, IN) with a straight collarless stem of cast Co–Cr–Mo alloy (Muller type; DePuy, Warsaw, IN). The proximal five-eighths of the stem was coated circumferentially with sintered beads of average diameter 150 μm (100–250) to form an irregular porous surface with empty spaces ranging from 150 to 400 μm. The design allowed an interference fit with the medial and lateral endosteal cortices as viewed in the frontal plane. The thin flat lateral profile gave rotational stability and three-point fixation for the stem in the curved upper femur [15]. At 5- to 8-year follow-up, good or excellent results were recorded in 70 % by the Mayo Clinic hip evaluation and in 84 % by the Harris hip score. Revision for aseptic loosening of the femoral stem was necessary in only one hip. Thigh pain diminished with time and was present in only two hips at the last follow-up. Endosteal bone formation was seen at the junction of the smooth and the porous segments of the stem in 94 % of hips; in 60 % of them it continued after 3 years. No focal endosteal bone resorption was observed. In 90 % of hips, proximal femoral atrophy did not progress after 3 years. Discontinuous radiolucent lines were seen around 30 % of stems, most commonly in zones I, IV, and VII. They were not progressive in 94 % and their presence did not correlate with the clinical outcome [15]. Recently, encouraging long-term results have been reported for cylindrical and tapered cementless cobalt–chrome stems [17–23]. Extensively porous-coated cementless implants made from Co–Cr alloys have achieved good results. The most commonly used was the anatomical medullary locking stem (AML®, DePuy Orthopaedics, Inc., Warsaw, IN) (Fig. 5.5). Engh et al. followed up 196 of these stems implanted in patients with an average age of 55 years for 11 years and found a mechanical failure rate of only 2.6 % [17, 18]. Kronick et al. reported on 174 hips in 154 patients younger than 50 years of age using the AML® and Prodigy® (both DePuy Orthopaedics, Inc., Warsaw, IN) extensively porous-coated stems. At an average follow-up of 8.3 years, 99.4 % of the stems showed stable fixation, 96 % had bone ingrowth, 3.4 % were fibrous stable, and 1.1 % were revised. The rate of osteolysis in the femur was 14 % and was limited to zones 1 and 7 [24]. Engh and Hopper retrospectively reviewed the outcome of 3,314 total hip arthroplasties performed with AML®, Prodigy®, and Solution® stems (all DePuy Orthopaedics, Inc., Warsaw, IN) [25]. These hips included 460 proximally coated stems and 2,854 extensively coated stems. The survival rates for proximally and extensively coated stems were >95 % at 15 years, using revision for any reason as an endpoint. Slight differences in thigh pain, stress shielding, and patient satisfaction were not significant. The 2.8 % rate of component loosening among proximally coated stems was significantly higher than the 1.1 % rate observed with extensively coated stems [25]. Kim compared proximal porous-coated stems of identical shape, but with two types of stem materials (Ti alloy or Co–Cr alloy) to determine the differences in these stems in clinical and functional outcomes, prevalence of thigh pain, stem alignment and canal fill, cup position, degree of periprosthetic bone loss, prevalence of polyethylene liner wear and osteolysis, incidence of aseptic loosening of acetabular and femoral components, and complications. The clinical and radiographic results of this study were similar (no significant differences) between the titanium and Co–Cr alloy femoral components; however, the titanium alloy femoral component retained greater periprosthetic bone as compared with the Co–Cr alloy femoral component [26]. Yoon et al. reported long-term stability of the tapered fully porous-coated cobalt–chrome Autophor 900S stems (Osteo AG, Selzach, Switzerland). The survival rate of the stems at 17 years was 94.5 %. A stable stem with bone ingrowth was identified in all 120 hips, excluding femoral revision cases (seven hips). The causes of the seven femoral revisions were aseptic loosening in four, infection in two, and stem fracture in one. No surgical intervention was performed for osteolysis or stress shielding [23].
Metallic Ions Release from Co–Cr Porous-Coated Implants
Porous-coated technology has several inherent problems, one of which is the potential for the increased release of metallic ions due to more corrosion associated with the large surface area of the porous metal. The long-term effects of hyperphysiological concentrations of metallic ions are largely unknown, but many studies have indicated that the potential for toxicity or even carcinogenicity exists [27–30]. In addition to simple corrosion, there is the release of metal debris due to wear or fretting and fretting-corrosion mechanisms. Experience with metal-on-metal articulations showed that the rate or quantity of release of metal due to wear can be far more significant than that due to corrosion [30–32]. Material released by wear or fretting is more susceptible to corrosion because the protective effect of the passive oxide film is reduced. Furthermore, corrosion is enhanced in the presence of fretting and by differences in electrochemical potential between passivated and non-passivated regions on the surface of the metal [30–33].
Metallic ions release from metallic porous-coated prostheses raises important questions as to the fixation of porous-coated hip prostheses and the mechanical integrity of the metallic porous coating. While it has been occasionally observed that a few sintered particles become loose from a femoral prosthesis as it is impacted into the intramedullary canal, in the vast majority of patients the implant remains well fixed in the canal and no progressive loosening of particles is observed. If there is no motion at the bone-implant interface, constituents of the alloy are released primarily by corrosion (excluding wear debris from the ball-and-socket articulation). If on the other hand, the implant is not fixed or it becomes loose, cyclic motion at the bone-implant interface during loading and unloading can cause increased loosening of particles, fretting wear of particles, fretting corrosion, metallosis, and reactive changes in tissue. The metallic debris that is released in this manner resembles that observed with metal-on-metal joint replacements [30]. High local (tissue) levels of metal can develop and there may be problems related to sensitivity, inflammatory response, or systemic toxicity [31, 32]. When a cementless porous-coated femoral component is used, the stem is usually impacted with considerable force into a close-fitting channel. This may be the major cause of initial loosening of particles. Loosening of particles occurs in approximately 2 % of patients. Using sintering techniques and new methods for manufacturing textured or porous surfaces other than sintering, loosening of particles has been diminished [33]. It also seems reasonable to assume that loosening of particles would be most likely to develop after revision using a cementless porous-coated prosthesis [30].
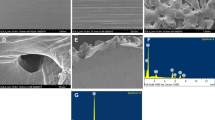
Corrosion Behavior of Co–Cr Porous Coatings
Particle release due to sloughing of the coating is a potential concern with Co–Cr alloys. The heightened release of particles can lead to severe wear and damage of the implant, enhanced inflammatory response, and decreased stability of the fixation [30, 34]. Clinical evidence suggests that bead sloughing can be attributed to either shear stresses at initial implantation or micromotion at the porous coating-bone interface [30, 35–39]. However, it has been hypothesized that this sloughing of beads from porous coatings may be due in part to corrosion at the fusion zones in the coatings, as opposed to a solely mechanical failure [34]. In addition, the tendency for the beads to slough may be related to the microstructure of the coating. The neck regions of the beads may have a different chemical composition from the rest of the surface due to melting and resolidification, and there are distinct compositional differences among the carbides in the fusion zones [40–43]. These local inhomogeneities can lead to preferential attack of the grain boundaries and regions of carbide precipitation as well as favoring galvanic corrosion [43]. According to Georgette and Davidson, the corrosion behavior of Co–Cr alloys depends on the microstructure [44]. A more stable, uniform oxide layer would be expected with a more homogeneous matrix (annealed alloy) than with a highly dendritic (as cast) structure [44]. Jacobs et al. stated that changes in the microstructure resulting from incipient melting of carbides during the porous coating sintering process may cause an increase in corrosion potential for porous-coated alloys as compared to conventional alloys [43]. In addition, this carbide melting may predispose these alloys to accelerated intergranular corrosion. Preferential or localized corrosion of the porous coating can lead to cracking and increase the susceptibility to failure [43]. Sintering heat treatments cause changes in the microstructure that result in changes in the corrosion behavior of the porous coatings. An in vitro study using SEM analysis examined the effects of microstructure on the corrosion of Co–Cr porous coatings [34]. The results showed a progressive generalized dissolution of the cobalt-rich matrix, with preferential attack of the grain boundaries and areas surrounding the carbides due to sensitization. This behavior was independent of microstructure; however, the severity of the attack was microstructure dependent. The degree and extent of sensitization is related to the alloy composition, porous coating procedures, and subsequent thermal treatments [34].
Metallic Failures of Co–Cr Porous-Coated Implants
Although metallic failure is relatively uncommon with many of the high-strength alloys currently used in implant applications, there continues to be concern about the reduced fatigue strength associated with porous-coated Co–Cr–Mo alloys in weight-bearing applications [37, 45–52]. Failures were fatigue related; low ductility and low fatigue strength have been implicated [53, 54]. The mechanical properties of porous-coated Co–Cr implants may be compromised because of the sintering heat treatment [44, 55]. Metallurgical defects and poor microstructure, owing to suboptimal processing, have been associated with mechanical failures [45, 54, 56]. In total knee arthroplasty, many tibial tray fractures and femoral component fractures have been reported for Co–Cr–Mo alloy [37, 46–52].
Influence of Co–Cr Porous Coating on Infection
Porous-coated implants, particularly those made of Co–Cr alloys, may carry a higher risk of infection than do smooth-surfaced alternatives. An experimental study in a rabbit model showed that the Co–Cr implants were easier to infect compared to titanium [57]. The researchers implanted cylinders of Co–Cr or titanium, with smooth or porous surfaces, into rabbit bones which had been inoculated with suspensions of Staphylococcus aureus in various doses. Results showed that the bacterial concentration required to produce infection of porous-coated titanium implants was 2.5 times smaller than that necessary to infect implants with polished surfaces; probably, the bacteria colonize the porous surface faster than did the tissue cells. Moreover, porous-coated Co–Cr implants required bacterial concentrations that were 40 times smaller than those needed to infect implants with polished surfaces and 15 times smaller than those required to infect porous-coated titanium implants; this may reflect the better osseointegration of titanium compared to Co–Cr [57].
Titanium is one of the best materials for implantation in bone, because of its biocompatibility; once a glycoprotein film has formed on a titanium-oxide surface, osteoblasts rapidly colonize it and this may protect the surface against colonization by bacterial pathogens. Co–Cr alloy is less readily colonized by the cells of the host and is consequently colonized more easily by bacteria [58]. Therefore, the advantages and disadvantages of an implant, such as improved osseointegration, larger ion-release surfaces, surface wear, and relative stiffness, must be weighed against the higher infection rates in the porous-coated implants, and particularly in the Co–Cr porous-coated implants [57].
Influence of Sex and Estrogens on Co–Cr Porous Coating Ingrowth
Sex hormones are an established variable in the studies of bone density and mineral metabolism [59, 60]. The sex-related differences in bone physiology may correspond to differences in bone ingrowth into the porous surface. Many total hip or knee arthroplasties have been performed in aged patients. At least some of these patients are in osteoporotic status due to menopause and/or aging. Most orthopedists would use cemented prostheses for severely osteoporotic patients based on the belief that bone ingrowth into the porous surface of a cementless prosthesis may not be achievable in these patients [61]. High-dose estrogen has been shown to stimulate the differentiation and activity of osteoblasts in vitro and increase bone formation and bone mass in animal models as well as in postmenopausal women [62–66]. Shih et al. evaluated the effects of sex and estrogen therapy on bone ingrowth into porous-coated implant in an animal model [67]. Three months after implantation, histological examination showed significantly more bone ingrowth in areas with cortical bone contact than in areas with cancellous bone contact. Bone ingrowth was essentially the same in male and female control dogs. Ovariectomized dogs showed less overall bone ingrowth than male and female controls. Bone ingrowth in areas with cortical bone contact did not decrease significantly, whereas bone ingrowth in areas with cancellous bone contact was significantly impaired in ovariectomized dogs compared with female controls. Short-term high-dose estradiol treatment did not increase bone ingrowth volume fraction. Mechanical tests did not show any statistical differences among groups [67]. The authors concluded that the type of bone contact is the key factor affecting the amount and pattern of bone ingrowth into the porous surface and recommended extensively or full-coated porous prostheses to achieve enough cortical bone contact and ingrowth for postmenopausal patients.
Novel Techniques for Micro-structural Metal Surface Texture
Long-term success of porous-coated prostheses is often impaired by the loss of fixation between the prosthesis and bone. To overcome the potential disadvantages of porous-coated prostheses, including metal debris from porous coatings (third-body wear particles) and irregular micro-texture of metal surfaces, a recent study presented a precisely controllable porous texture technique based on material removal by the yttrium–aluminum–garnet (YAG) laser for controlling application of micro-structural metal surface texture (tartan check shape) [68]. Using this technique, free shapes can be applied to complex, three-dimensional hard metal surfaces such as Co–Cr. In this study, tartan check shapes made by crossing grooves and dot shapes made by forming holes were produced on titanium (Ti6A14V) or cobalt–chrome (Co–Cr) and evaluated with computer-assisted histological analysis and the measurement of bone-metal interface shear strength. The width of grooves or holes ranged from 100 to 800 μm (100, 200, 500, and 800 μm), with a depth of 500 μm. Results showed superior osteoconduction (especially in the 500-μm grooves) with the tartan check shape compared to commercial porous coating and superior shear strength between the bone and implant interface. Additionally, titanium provided faster osteoconduction than cobalt–chrome in tartan check shape samples [68].
References
ARCAM.ASTM F75 CoCr Alloy. Arcam EB system. Available at: http://www.arcam.com/CommonResources/Files/www.arcam.com/Documents/EBM%20Materials/Arcam-ASTM-F75-Cobalt-Chrome.pdf. Accessed on March 1, 2012.
Browne M, Gregson PJ. Metal ion release from wear particles produced by Ti-6Al4V and Co-Cr alloy surfaces articulating against bone. Mater Lett. 1995;24:1–6.
Nouri A, Hodgson PD, Wen CE. In: Biomimetic porous titanium scaffolds for orthopedic and dental applications, Mukherjee A. (Ed). Biomimetics, Learning from Nature, chapter 21, InTech Open Access Publisher, 2010:415-50
ASM International. Coatings. In: Davis JR, editor. Handbook of materials for medical devices. 03rd ed. Materials Park: ASM International; 2003. p. 179–95.
Pilliar RM. Porous biomaterials. In: Williams D, editor. Concise encyclopedia of medical & dental materials. Oxford/New York/Cambridge, MA: Pergamon Press and The MIT Press; 1990. p. 312–9.
Bobyn JD, Cameron HU, Abdulla D, Pilliar RM, Weatherly GC. Biologic fixation and bone modeling with an unconstrained canine total knee prosthesis. Clin Orthop. 1982;166:301–12.
Lisin M, Peterson RR. Failure of the bond between a cobalt alloy prosthetic casting and a sintered porous coating. In: Esaklul KA, editor. Handbook of case histories in failure analysis. 1st ed. Materials Park: ASM International; 1992. p. 449–51.
Hirvonen JK, Sartwell BD. Ion implantation. In: Surface engineering, ASM handbook. 5th ed. Materials Park: ASM International; 1994. p. 604–10.
Friedman RJ, Bauer TW, Garg K, Jiang M, An YH, Draughn RA. Histological and mechanical comparison of hydroxyapatite-coated cobalt-chrome and titanium implants in the rabbit femur. J Appl Biomater. 1995;6(4):231–5.
Jakobsen SS, Larsen A, Stoltenberg M, Bruun JM, Soballe K. Effects of as-cast and wrought cobalt-chrome-molybdenum and titanium-aluminium-vanadium alloys on cytokine gene expression and protein secretion in J774A.1 macrophages. Eur Cell Mater. 2007;14:45–54.
Baldwin L, Hunt JA. Host inflammatory response to NiCr, CoCr, and Ti in a soft tissue implantation model. J Biomed Mater Res A. 2006;79:574–81.
Jakobsen SS, Baas J, Jakobsen T, Soballe K. Biomechanical implant fixation of CoCrMo coating inferior to titanium coating in a canine implant model. J Biomed Mater Res A. 2010;94(1):180–6.
Firkins PJ, Tipper JL, Saadatzadeh MR, Ingham E, Stone MH, Farrar R, Fisher J. Quantitative analysis of wear and wear debris from metal-on-metal hip prostheses tested in a physiological hip joint simulator. Biomed Mater Eng. 2001;11:143–57.
Rieker C, Kottig P. In vivo tribological performance of 231 metal-on-metal hip articulations. Hip Int. 2002;12:73–6.
Pellegrini Jr VD, Hughes SS, Evarts CM. A collarless cobalt-chrome femoral component in uncemented total hip arthroplasty. Five- to eight-year follow-up. J Bone Joint Surg Br. 1992;74B:814–21.
Engh CA, Bobyn JD. The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop. 1998;231:7–28.
Sotereanos NG, Engh CA, Glassman AH, Macalino GE, Engh Jr CA. Cementless femoral components should be made from cobalt chrome. Clin Orthop. 1995;313:146–53.
Engh Jr CA, Culpepper 2nd WJ, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79A:177–84.
Grant P, Grøgaard B, Nordsletten L. Ultralok uncemented femoral prostheses: 12 to 15 year follow-up evaluation. J Arthroplasty. 2004;19(3):274–80.
Mallory TH, Lombardi Jr AV, Leith JR, Fujita H, Hartman JF, Capps SG, Kefauver CA, Adams JB, Vorys GC. Minimal 10-year results of a tapered cementless femoral component in total hip arthroplasty. J Arthroplasty. 2001;16(8 S1):49–54.
Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. J Arthroplasty. 2004;19(2):151–6.
Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (tri-lock) inserted without cement. J Bone Joint Surg Am. 2002;84A:2140–4.
Yoon TR, Rowe SM, Kim MS, Cho SG, Seon JK. Fifteen- to 20-year results of uncemented tapered fully porous-coated cobalt-chrome stems. Int Orthop. 2008;32(3):317–23.
Kronick JL, Barba ML, Paprosky WG. Extensively coated femoral components in young patients. Clin Orthop. 1997;344:263–74.
Engh CA, Hopper Jr RH. The odyssey of porous-coated fixation. J Arthroplasty. 2002;17(4 S1):102–7.
Kim YH. Titanium and cobalt-chrome cementless femoral stems of identical shape produce equal results. Clin Orthop. 2004;427:148–56.
Heath JC, Freeman MA, Swanson SA. Carcinogenic properties of wear particles from prostheses made in cobalt-chromium alloy. Lancet. 1971;1(7699):564–6.
Sunderman Jr FW. Metal carcinogenesis in experimental animals. Food Cosmet Toxicol. 1971;9(1):105–20.
Woodman JL, Black J, Jiminez SA. Isolation of serum protein organometallic corrosion products from 316LSS and HS-21 in vitro and in vivo. J Biomed Mater Res. 1984;18(1):99–114.
Buchert PK, Vaughn BK, Mallory TH, Engh CA, Bobyn JD. Excessive metal release due to loosening and fretting of sintered particles on porous-coated hip prostheses. Report of two cases. J Bone Joint Surg Am. 1986;68A:606–9.
Evans EM, Freeman MA, Miller AJ, Vernon-Roberts B. Metal sensitivity as a cause of bone necrosis and loosening of the prosthesis in total joint replacement. J Bone Joint Surg Br. 1974;56B:626–42.
Dobbs HS, Minski MJ. Metal ion release after total hip replacement. Biomaterials. 1980;1(4):193–8.
Cohen J, Lindenbaum B. Fretting corrosion in orthopedic implants. Clin Orthop. 1968;61:167–75.
Placko HE, Brown SA, Payer JH. Effects of microstructure on the corrosion behavior of CoCr porous coatings on orthopedic implants. J Biomed Mater Res. 1998;39(2):292–9.
Hamblen DL, Paul JP. The integrity of porous coatings for cementless implants. J Bone Joint Surg Br. 1988;70B:521–3.
Callaghan JJ, Dysart SH, Savory CG. The uncemented porous-coated anatomic total hip prosthesis. Two-year results of a prospective consecutive series. J Bone Joint Surg Am. 1988;70A:337–46.
Morrey BF, Chao EY. Fracture of the porous-coated metal tray of a biologically fixed knee prosthesis. Report of a case. Clin Orthop. 1988;228:182–9.
Davey JR, Harris WH. Loosening of cobalt chrome beads from a porous-coated acetabular component. A report of ten cases. Clin Orthop. 1988;231:97–102.
Cameron HU. Six-year results with a microporous-coated metal hip prosthesis. Clin Orthop. 1986;208:81–3.
Clemow AJ, Daniell BL. Solution treatment behavior of Co-Cr-Mo alloy. J Biomed Mater Res. 1979;13(2):265–79.
Kilner T, Pilliar RM, Weatherly GC, Allibert C. Phase identification and incipient melting in a cast Co–Cr surgical implant alloy. J Biomed Mater Res. 1982;16(1):63–79.
Pilliar RM. Powder metal-made orthopedic implants with porous surface for fixation by tissue ingrowth. Clin Orthop. 1983;176:42–51.
Jacobs JJ, Latanision RM, Rose RM, Veeck SJ. The effect of porous coating processing on the corrosion behavior of cast Co-Cr-Mo surgical implant alloys. J Orthop Res. 1990;8(6):874–82.
Georgette FS, Davidson JA. The effect of HIPing on the fatigue and tensile strength of a case, porous-coated Co-Cr-Mo alloy. J Biomed Mater Res. 1986;20(8):1229–48.
Kohn DH, Duchyene P, Cuckler JM, et al. Fractographic analysis of failed porous and surface-coated cobalt-chromium alloy total joint replacements. Med Prog Technol. 1994;20:169.
Ranawit CS, Johanson NA, Rimnac CM, et al. Retrieval analysis of porous-coated components of total knee arthroplasty. Clin Orthop. 1986;209:244.
Scott RD, Ewald FC, Walker PS. Fracture of the metallic tibial tray following total knee replacement. J Bone Joint Surg Am. 1984;66A:780.
Flivik G, Ljung P, Rydholm U. Fracture of the tibial tray of the PCA knee. Acta Orthop Scand. 1990;61:26.
Huang CH, Yang CY, Cheng CK. Fracture of the femoral component associated with polyethylene wear and osteolysis after total knee arthroplasty. J Arthroplasty. 1999;14:375.
Wada M, Imura S, Bo A, et al. Stress fracture of the femoral component in total knee replacement: a report of 3 cases. Int Orthop. 1997;21:54.
Whiteside LA, Fosco DR, Brooks JG. Fracture of the femoral component in cementless total knee arthroplasty. Clin Orthop. 1993;286:71.
Swarts E, Miller SJ, Keogh CV, Lim G, Beaver RJ. Fractured Whiteside Ortholoc II knee components. J Arthroplasty. 2001;16(7):927–34.
Ducheyne P, De Meester P, Aernoudt E. Fatigue fractures of the femoral component of Charnley and Charnley-Muller type total hip prostheses. J Biomed Mater Res. 1975;6:199.
Galante JO, Rostoker W, Doyle JM. Failed femoral stems in total hip prostheses. J Bone Joint Surg Am. 1975;57A:230.
Pilliar RM. Porous-surfaced metallic implants for orthopaedic applications. J Biomed Mater Res. 1987;21:1.
Rostoker W, Chao EYS, Galante JO. Defects in failed stems of hip prostheses. J Biomed Mater Res. 1978;12:635.
Cordero J, Munuera L, Folgueira MD. Influence of metal implants on infection. An experimental study in rabbits. J Bone Joint Surg Br. 1994;76B:717–20.
Gristina AG, Naylor PT, Myrvik QN. Mechanisms of musculoskeletal sepsis. Orthop Clin North Am. 1991;22:363–71.
Composton JE. Sex steroids and hone. Physiol Rev. 2001;81:419–77.
Raisz LG, Wiita B, Artis A, et al. Comparison of the effect of estrogen alone and estrogen plus androgen on biochemical markers of bone formation and resorption in postmenopausal women. J Clin Endocrinol Metab. 1996;81:3743.
Harris WH, Davies JP. Modern use of modern cement for total hip replacement. Orthop Clin North Am. 1988;19:581–9.
Ernst M, Schmid C, Froesch ER. Enhanced osteoblastic proliferation and collagen gene expression by estradiol. Proc Natl Acad Sci U S A. 1988;85:2307–20.
Tobias JH, Compstom JE. Does estrogen stimulate osteoblasts function in postmenopausal women? Bone. 1999;24:121–4.
Edwards MW, Bain SD, Bailey MC, et al. 17 p-estradiol stimulation of endosteal bone formation in the ovariectomized mouse: an animal model for the evaluation of bone-targeted estrogens. Bone. 1992;13:29–34.
Bord S, Beavan S, Ireland D, et al. Mechanisms by which high-dose estrogen therapy produces anabolic skeletal effects in postmenopausal women: role of locally produced growth factor. Bone. 2001;29:216–22.
Khastgir G, Studd J, Holland N, et al. Anabolic effect of long-term estrogen replacement on hone collagen in elderly postmenopausal women with osteoporosis. Osteop Int. 2001;12:465–70.
Shih LY, Shih HN, Chen TH. The effects of sex and estrogen therapy on bone ingrowth into porous coated implant. J Orthop Res. 2003;21(6):1033–40.
Hirao M, Sugamoto K, Tamai N, Oka K, Yoshikawa H, Mori Y, Sasaki T. Macro-structural effect of metal surfaces treated using computer-assisted yttrium-aluminum-garnet laser scanning on bone-implant fixation. J Biomed Mater Res A. 2005;73(2):213–22.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Babis, G.C., Mavrogenis, A.F. (2014). Cobalt–Chrome Porous-Coated Implant-Bone Interface in Total Joint Arthroplasty. In: Karachalios, T. (eds) Bone-Implant Interface in Orthopedic Surgery. Springer, London. https://doi.org/10.1007/978-1-4471-5409-9_5
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5409-9_5
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5408-2
Online ISBN: 978-1-4471-5409-9
eBook Packages: MedicineMedicine (R0)