Abstract
The traditional surgical technique for pelviureteric junction obstruction (PUJO) is the dismembered pyeloplasty which may be performed open, laparoscopic, or robotic assisted. In a select group of patients, aberrant lower pole crossing vessels may be responsible for an extrinsic compression of the pelviureteric junction. Relocation of the lower pole vessels can relieve the obstruction in such cases. This chapter focuses on the indications, contraindications, technical aspects, and postoperative management of the laparoscopic relocation of the lower pole vessels also known as the vascular hitch or pyelopexy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Laparoscopic transposition of the lower pole vessels is suitable in children in whom there is a high index of suspicion of lower pole vessels. Transposition of lower pole vessels was first described by Hellstrom in 1951 [1]. Suspicion of lower pole vessels is based on a normal antenatal history, intermittent episodes of flank pain with a predominantly extrarenal pelvic dilatation on ultrasound, worse during the time of the pain. Children tend to be older and in between episodes may even have a normal renal ultrasound with minimally dilated renal pelvis. Furosemide administration during an isotope renogram may precipitate the pain, and the renogram demonstrates an obstructive pattern with minimal washout with furosemide.
Indications for the Vascular Hitch
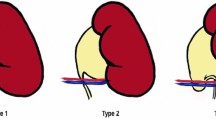
If as described above, there is a high index of suspicion of lower pole vessels, a vascular hitch may be considered. However, the surgeon must be prepared to perform a laparoscopic dismembered pyeloplasty if there are no lower pole vessels or if the vessels do not appear to be the causative factor of the PUJO. In a retrospective review of eight children undergoing the vascular hitch, three anatomical variations of the lower pole vessels were recognized: vessels in front of the pelvis, in front of the PUJ, and below the PUJ causing ureteric kinking [2]. The authors recommend performing the hitch for vessels below the PUJ.
Preoperative Investigations
As for PUJ obstruction, the preoperative investigations consist of:
-
1.
Renal ultrasound: with increasing resolution of the ultrasound scanners and experience of pediatric radiologists, lower pole vessels may be visualized on Doppler ultrasound.
-
2.
MAG 3 renogram.
All imaging MUST be available and on the screen in the OR at the time of the surgery.
All children should have a baseline renal biochemistry and full blood count. The author does not routinely group and save serum for this procedure or a laparoscopic pyeloplasty.
Instrumentation
-
Standard 5 mm laparoscopic set to include Kelly forceps, atraumatic graspers, scissors, diathermy hook, and needle holder.
-
The author prefers to have available bipolar diathermy forceps if required.
Anesthesia
General anesthesia with endotracheal intubation and full muscle relaxation
Patient Position
The patient is placed in a renal position with a sandbag under the lower costal margin to elevate the affected side. The patient should be well supported posteriorly. Anteriorly the patient is supported in the region of the chest but not in the region of the trunk as this can interfere with the working ports and instruments. The patient should be stabilized with broad tape over the pelvis and thorax. The position of the patient, surgeon, anesthetist, and equipment is shown in Fig. 9.1.
Port Position
One primary umbilical port and two working ports are required. The port positions are shown in Fig. 9.2. A trick to facilitate umbilical primary port access by the open technique is to tilt the table away from the surgeon to make the patient more supine. Once access is obtained, the table can be returned to its original position and the patient in the renal position.
Operative Technique
-
The ascending or descending colon is reflected medially to expose the perirenal fascia and quite often the bulging renal pelvis.
-
The perirenal fascia is incised and reflected medially and the adventitia over the pelvis cleared.
-
The pelvis is traced inferiorly to the PUJ, or the ureter is traced superiorly to expose the lower pole vessels (Fig. 9.3).
Fig. 9.3 Renal pelvis (P), ureter (U), and vessels (V) exposed (Reprinted from Godbole et al. [3]. Copyright© 2006, with permission from Elsevier)
-
If lower pole vessels are identified, with a combination of scissors/bipolar hook, the pelvis and ureter are fully mobilized so that they are completely free from the lower pole vessels (Fig. 9.4). This can be demonstrated by the “shoe shine” maneuver as seen in the accompanying video.
Fig. 9.4 Renal pelvis (P) fully mobilized (Reprinted from Godbole et al. [3]. Copyright© 2006, with permission from Elsevier)
-
A useful trick is to divide the fibrous strands towards the hilar end of the lower pole vessels to increase their mobility. A further tip to check the adequacy of dissection is to transpose the vessels superiorly over the pelvis where they should sit in a comfortable position on release of the pelvis.
-
Inspection of the PUJ and proximal ureter is now made and any kinks straightened out. If there are no vessels or they do not appear to be contributing to the obstruction, either a laparoscopic or open pyeloplasty can be performed depending on surgeon’s preference.
-
The vessels are fixed in position by suturing the renal pelvis on either side of the vessels with 2–3 absorbable 4.0 or 5.0 Vicryl sutures (Fig. 9.5) No drains or stents are required. The final appearance of the pexed vessels is seen in Fig. 9.6.
Fig. 9.5 Vessels pexed superiorly (Reprinted from Godbole et al. [3]. Copyright © 2006, with permission from Elsevier)
Fig. 9.6 Appearances at the end of the procedure (Reprinted from Godbole et al. [3]. Copyright© 2006, with permission from Elsevier)
Postoperative Care
The patient is allowed to eat and drink as tolerated soon after the procedure and is discharged when mobilizing usually the next day. The author routinely performs a US and MAG 3 renogram 6 weeks postoperatively.
Outcomes
Conclusion
The vascular hitch is a useful alternative to dismembered pyeloplasty in carefully selected cases where lower pole vessels are deemed to be the sole etiology. The procedure is simple to perform and relatively quick with a good success rate. Previous vascular hitch surgery does not seem to preclude a further open/laparoscopic pyeloplasty for recurrent PUJO [3, 5].
References
Hellstrom J, Giertz G, Lindblom K. Pathogenesis and treatment of hydronephrosis. J Belge Urol. 1951;20:1–6.
Schneider A, Ferreira CG, Delay C, Lacreuse I, Moog R, Becmeur F. Lower pole vessels in children with pelviureteric junction obstruction: vascular hitch or dismembered pyeloplasty? J Pediatr Urol. 2013;9(4):419–23.
Godbole P, Mushtaq I, Wilcox DT, Duffy PG. Laparoscopic transposition of lower pole vessels – the ‘vascular hitch’: an alternative to dismembered pyeloplasty for pelvi ureteric junction obstruction in children. J Pediatr Urol. 2006;2(4):285–9.
Gundeti MS, Reynolds WS, Duffy PG, Mushtaq I. Further experience with the vascular hitch (laparoscopic transposition of lower pole vessels): an alternate treatment for pediatric ureterovascular ureteropelvic junction obstruction. J Urol. 2008;180(4):1832–6.
Nerli RB, Jayanthi VR, Reddy M, Koura A. Pelvi ureteric junction obstruction with crossing renal vessels: a case report of failed laparoscopic vascular hitch. J Pediatr Urol. 2009;5(2):147–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Godbole, P.P. (2014). Transposition of Lower Pole Vessels: “The Vascular Hitch”. In: Godbole, P., Koyle, M., Wilcox, D. (eds) Pediatric Endourology Techniques. Springer, London. https://doi.org/10.1007/978-1-4471-5394-8_9
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5394-8_9
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5393-1
Online ISBN: 978-1-4471-5394-8
eBook Packages: MedicineMedicine (R0)