Abstract
The assessment of spinal degenerative diseases with diagnostic imaging – as well as other fields of application – has seen remarkable development with technological progress, in particular regarding computed tomography (CT) and magnetic resonance imaging (MRI). Only 20 years ago, conventional radiography was considered the basis of degenerative spine diagnostic imaging and we proceeded to second-line investigations choosing between CT and MRI based on radiographic findings and clinical evidence. Today, the situation has changed radically thanks to the greater availability of CT and MRI, the relative cost reduction, and the greater scanning speed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Magnetic Resonance Image
- Contrast Agent
- Magnetic Resonance Image Study
- Compute Radiography
- Odontoid Process
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The assessment of spinal degenerative diseases with diagnostic imaging – as well as other fields of application – has seen remarkable development with technological progress, in particular regarding computed tomography (CT) and magnetic resonance imaging (MRI). Only 20 years ago, conventional radiography was considered the basis of degenerative spine diagnostic imaging and we proceeded to second-line investigations choosing between CT and MRI based on radiographic findings and clinical evidence. Today, the situation has changed radically thanks to the greater availability of CT and MRI, the relative cost reduction, and the greater scanning speed.
In practice today, faced with clinical situations indicative of degenerative spine disease, the first diagnostic imaging method is increasingly the MRI. This choice has the great advantage of avoiding exposure to ionizing radiation and of reducing the overall time required for diagnosis, thanks to the exploratory capacity of MRI as regards the extension of the field of view, its ability to demonstrate degenerative disease in the vertebrae, discs, joints, and ligaments, and its effects on the “content,” that is, the spinal cord, roots, and meningeal sheaths.
In light of the growing availability and accessibility of MRI, we can outline the main clinical and radiological scenarios. First, MRI is sufficient for diagnosis and covers clinical needs alone; no further investigation is needed. Second, MRI is diagnostic, but there is a clinical and radiological need for a complementary targeted CT on a specific area of interest or to define pre-surgical bone status. In selected cases, it will be possible to proceed further with a dynamic radiographic study, as the most simple, effective, and least expensive method of demonstration of any instabilities. Third, the MRI, CT, and X-ray refine the diagnosis, but – albeit exceptionally – there is a need for interventional procedures for diagnostic purposes or as a first step towards the choice of interventional procedures. In this context, there may also be a need to perform intrathecally contrast-enhanced studies (sacculo-radiculography/myelography-CT), discography, or biopsies. Fourth, the MRI is contraindicated (e.g., due to the presence of an incompatible pacemaker) and the CT replaces the MRI in the diagnostic algorithm. If there is a need to study the “content,” it becomes necessary to perform a CT-myelography. This is a schematization that moves from the superiority and acceptance to the MRI, sometimes not indicated, but auto-prescribed by the patient and offering the highest sensitivity and specificity.
This chapter, prior to those dedicated to degenerative diseases of the cervicodorsal spine and the lumbosacral spine, respectively, will briefly present the current status of diagnostic imaging techniques used in the assessment of degenerative spinal diseases. For historical reasons, we start with the section on X-rays, followed by those on CT and MRI, and thus the residual use of intrathecal contrast studies and other “invasive” methods. Finally, we present a few words on the – marginal – use of nuclear medicine techniques.
Radiography
The conventional X-ray examination represents the starting point in the study of the spine. Analogical techniques (which made use of direct exposure of film to X-rays) are now only still used by small peripheral radiology centers and were gradually or completely replaced by digital computed radiography (CR) or digital radiography (DR) systems [1]. Although digital systems are more functional and more cost-effective, from the point of view of quality, analogical images remain significantly better than digital ones. Analogical images are better in the study of subtle bone changes, while they have a marginal role, due to their limited contrast resolution, in the study of soft tissue (discs, ligaments).
CR systems are based on phosphor plates sensitive to X-rays, which replace cassettes and analogical films in all respects. After exposure, the cassette is transferred to a digitizer that reads the contained information and creates a digital image that, when saved in DICOM (Digital Imaging and Communication in Medicine) format, can be printed, saved on digital media (DVD, CD), or sent to the PACS (Picture Archiving and Communicating System) for reporting. Unlike CR, DR systems use detectors panels that are placed directly on the radiological table, on dedicated systems, or on portable devices. The high-resolution images are then directly processed by the computer and made available in a few seconds to be subsequently sent to the PACS system for reporting or other digital media, as described for CR systems. DR systems are much faster than CR systems in making the image available and, overall, both systems (CR and DR) are less sensitive to exposure errors than analogical systems. In addition, overall, digital systems allow reduced doses and number of patient exposures compared to analogical systems.
However, it must be emphasized that the role of conventional radiography in the study of spinal degenerative disease has undergone a critical reevaluation and is currently controversial [2, 3]. Its generalized and routine use was unjustified, dictated more by medico-legal reasons or by the anxiety that patients transmit to the doctor, rather than by legitimate clinical questions.
Given that the examination of basic orthogonal projections alone is often not diagnostic unless accompanied by additional projections (oblique, transbuccal, etc.) – with a significant increase of the dose to the patient – the use of conventional radiography should be reduced in favor of methods such as MRI and CT scans, which until a few years ago were considered “second line” tools. Herein, radiological study techniques are considered separately as regards their use for the cervical, thoracic, and lumbar spine.
Cervical Spine
The routine study in two orthogonal projections has substantially lost value in the diagnosis of degenerative cervical spine diseases. Increasingly often, clinicians directly prescribe MRI and/or CT studies to patients with cervical brachialgia or neck pain, due to their ability to comprehensively display the bony structures and soft tissues (ligaments and discs, bone marrow) with marginal use of radiological examinations. The standard digital radiological examination of the degenerative spine (Fig. 2.1a, b) can still provide useful information on the bone spinal structures, such as on degenerative changes (i.e., spondylosis, osteophytes, irregular morphology of bodies, calcification of ligaments and discs) that are often not directly implicated as the cause of pain. However, X-rays provide more limited and indirect information on the disc (herniations) and possible stenosis of the spinal canal. Although the literature proposes the supine study position, it is useful to study the patient in upright position, at least in the lateral view, which can provide information concerning possible spinal instability (listhesis). The examination is performed in the two orthogonal planes (anteroposterior and latero-lateral), trying as much as possible, especially in the lateral view, to explore the bodies up to C7 (often masked by the shoulder girdle).
If properly performed, oblique views may be of some utility in evaluating the degenerative spine, for the study of the intervertebral foramina, the uncinate processes, and the facet joints, although all of this information can be provided more comprehensively by CT.
Given their complex implementation and their sometimes poor results, “swimmer’s” projections and the transbuccal projection for the study of the odontoid process are replaced by CT scan.
The “functional” radiological study of the cervical spine (Fig. 2.1c, d), still offers full diagnostic validity in evaluating instability, so as to propose the use of flexion-extension X-rays in upright standing in the routine study for the demonstration of instability [4]. In functional radiograms, the anterior atlantoaxial space (between the posterior margin of the anterior arch of the atlas and the anterior surface of the odontoid process) should never be more than 3 mm in adults and 4 mm in children; an enlarged distance, measured directly on the radiogram, implies the diagnosis of anterior atlantoaxial subluxation.
On the other hand, vertical atlantoaxial subluxations involve a cranial displacement of the odontoid process in relation to certain reference lines, such as, for example, that of Chamberlain, drawn from the posterior edge of the hard palate to the posterior margin of the foramen magnum. If the odontoid process exceeds it by more than 3 mm, we speak of a vertical atlantoaxial subluxation.
The occurrence of cervical instability in a degenerative spine, demonstrated in the functional radiological study, can alone be the cause – or contributing cause – of pain and must be supplemented, especially by MRI, in suspected ligament laxity/injury (Fig. 2.2).
Cervical spondylosis: MRI vs. functional X-ray study. MRI study performed in sagittal plane with T1 TSE (a) and T2 TSE (b) weighted images. Focal central disc protrusion at C5–C6 level, without cord compression. Plain radiographic functional study in flexion (c) and extension (d) lateral view, showing minimal hypermobility at C4–C5 level on flexion image
Thoracic Spine
The study of the thoracic spine is less commonly performed because of the limited involvement of this part of the spine in degenerative changes. It is usually prescribed by the clinician to obtain an overview of the spine and is performed in the supine position in two orthogonal projections (anteroposterior and lateral). As mentioned for the cervical tract, the information obtained has inherent limitations for the cervicodorsal junction (due to the superimposition of the shoulder girdle) and the dorsolumbar junction (because the X-ray beam is positioned at the level of the inter-nipple line, resulting in minimum projective deformations of the last thoracic and first lumbar vertebral bodies). No diagnostic information can be obtained about the width of the spinal canal, discs – if non-calcified – and of course the intraspinal content (spinal cord).
Dynamic radiological examinations are rarely carried out on thoracic spine, but are still applied (“lateral bending”) in the comprehensive thoracic/lumbar spine evaluation when bending instability is suspected [5].
Lumbar Spine
As stated above, the X-ray study of the lumbar spine is no longer routinely applied in degenerative diseases and is more commonly used selectively after an evaluation with an MRI and/or CT scan, often with functional issues [6]. It is traditionally performed in the supine position, with frontal and lateral projections, with an incident beam of about 2 cm from the iliac crests [7] (Fig. 2.3a, b). The use of complementary projections, such as oblique, no longer seems justified, as they are replaced by multiplanar CT reconstructions, which certainly provide better information. However, conventional radiology is still useful in evaluating lumbar instability.
Standard X-ray study of the lumbar spine. Antero-posterior (a) and lateral (b) radiograms, in standing position. Degenerative radiographic findings can be appreciated at L5–S1 level. “Functional” study performed on the same patient in extension (c) and flexion (d) lateral views shows no sign of instability
“Dynamic studies,” which are easy to perform and low cost [8], are performed primarily in an upright position, acquiring radiographs in full flexion and in full extension in the lateral projection [9, 10] (Fig. 2.3c, d).
Some authors [11] report a better evaluation of vertebral translation with the patient in the supine than in the upright position, probably related to the reduced spinal motion determined by the paraspinal and abdominal musculature in the upright position. In addition, the pain that often accompanies such maneuvers in the upright position is less than in the supine position.
Flexion-extension X-rays in the lateral projection allow the measurement of sagittal vertebral translation and of vertebral rotation in the sagittal plane (defined as the variation of the angle formed by the intersection of the lines drawn between the two opposite endplates in full flexion and extension). These measurements, however, may suffer overestimation errors, unless the criteria [12] of a rigorous and standardized measurement technique and high-quality radiographs are met. According to some authors, the estimation error generated could lead to unjustified surgical stabilization procedures. The “cut-off” data for the determination of instability are about 10° for sagittal rotation and 4 mm for sagittal translation [13]. It must nevertheless be taken into account that, in a small percentage of asymptomatic patients, the dynamic examination may find values higher than those of reference above. In these individuals, spinal hypermobility is fully compensated by the muscle and vertebral structures. Side bending or lateral bending can also be radiological indicators of instability [14].
The characteristic findings for determining lateral instability are represented by the misalignment of the spinous processes, laterolisthesis, loss of motility, and excessive widening of the vertebral interbody space during lateral flexion [8]. Some authors argue that lateral bending provides complementary information in flexion-extension studies and that it should be performed whenever there is a suspicion of instability, especially in the case of negative flexion-extension test.
We can conclude that the value of functional studies is still debated, but most surgeons require them, for integration of CT or MRI study, and believe in their usefulness as an indicator of instability (Fig. 2.4).
Lumbar instability: MRI vs. functional X-ray study. MRI study performed in sagittal plane with T1 TSE (a) and T2 TSE (b) weighted images. Multiple disc protrusions, more evident at L4–L5, with minimal deformity of the ventral surface of the thecal sac. No significant listhesis is seen on supine MRI study. Radiographic functional study (lateral view) in flexion (c) and extension (d) in standing position demonstrates a listhesis at L4–L5 level, increasing on flexion image
Computed Tomography (CT)
After its introduction, computed tomography became a gold standard in the study of the spine [15]. In the past decade, the introduction of multidetector CT scanners (MDCT) has completely changed the role of the MDCT in spinal studies. The outdated “single-layer” machines with long scan times, thick slices (3 mm), and a reduced exploratory capacity have given way to MDCT, which allows reduced acquisition times (in the order of seconds), submillimeter acquisition/reconstruction thicknesses (0.5–0.6 mm), and the possibility to include the entire spine in a single scan. Modern MDCT equipment can have up to 256 detectors, with an increase in spatial resolution, which reaches values much higher than those of MRI. An MDCT study of the spine provides for the acquisition of axial slices perpendicular to the longitudinal spinal axis, with slice thicknesses chosen according to different equipment and directions; thickness of 0.6–0.7 mm with reconstruction per 1 mm and increases of 0.5–0.6 are satisfactory parameters for most clinical questions. The obtained images, measured using soft tissue (Fig. 2.5a) and bone reconstruction algorithms (Fig. 2.5b), together with the use of convolution filters (high-resolution filters that provide a better spatial resolution but a worse imaging signal/noise ratio, or a standard filter that is a good compromise between spatial resolution and imaging signal/noise ratio), allow an optimal visualization of the bony structures of the vertebral body, such as cortical integrity, and a satisfactory visualization of the intervertebral discs, especially in the lumbar spine, thanks also to the richness of fat tissue in the epidural area, compared to the cervical and thoracic regions. On the other hand, they appear to be totally inadequate in the study of bone marrow and ligaments, which remains the exclusive prerogative of MRI. Axial MDCT acquisitions can be reconstructed and easily viewed in the sagittal and coronal planes, thanks to the new reconstruction algorithms and increased computing power of workstations, with a significant improvement in ease of interpretation (Fig. 2.5c, d).
Computed tomography (CT) of lumbar spine. CT axial images, with soft tissue (a) and bone (b) windows. In (a) a wide-based annular disc protrusion, associated to minimal facet changes (b). Reformatted coronal (c) and sagittal (d) images better visualize the bone structures. (e, f) 3D shaded surface display
Three-dimensional (3D) reconstructions appear to be of little diagnostic value, but may give the clinician a better overview, especially in surgery planning [16]. In this regard, the best 3D techniques are those reconstructed with the shaded surface display (SSD) that, while maintaining its inherent limitations (loss of spatial resolution and contrast), provide, however, a marked improvement in the quality of the images [17] (Fig. 2.5e, f). The use of contrast media, especially in the study of the degenerative spine, provides limited additional information and only in selected instances (such as post-surgical evaluations changes and infectious diseases). MDCT is the reference method in the study of the postoperative spine because of its multiplanarity, the scanning speed, and the reduced artifacts derived from orthopedic implants (compared to MRI). It is essential that the study be performed by a “dedicated radiologist,” able to distinguish normal surgical sequelae from complications (early or late).
A special use of CT is that of CT fluoroscopy [18], which allows obtaining real-time images during interventional procedures, such as those of nerve block, CT discography, and vertebral and soft tissue biopsies.
The so-called “twist test” is a functional study that is performed on CT to determine the presence of possible lumbar instability.
It consists of placing the patient in a supine position on the CT table, having him/her turn his back first to the right and then to the left, and performing a scan through the interapophyseal joints between two adjacent vertebrae. The test demonstrates an abnormal increase of motility and of the distance of the interapophyseal joints (exhibiting a vacuum phenomenon) during the rotation of the trunk, data that are not appreciable in the functional radiographic tests [19, 20]. Although this test can show the presence of a lumbar vertebral instability, it is not used routinely because of the significant exposure to ionizing radiation it entails.
With regard to CT studies performed using the so-called “axial loader,” we refer the reader to the chapter on MRI in which they are discussed.
The superiority of MDCT, however, involves a strong focus on radiation-protection problems, as the radiation dose delivered to the patient is not negligible. It is estimated that, on average, approximately 8.2 mSv are administered for a lumbar MDCT examination and about 3.4 mSv for an examination of the cervical spine. The radiologist must try to reduce the exposure dose (for example, by using automatic programs, reducing the milliamperage, etc.), and to suggest the use of alternative imaging tools (such as MRI) to the clinician.
Magnetic Resonance Imaging (MRI)
Spinal MRIs in general – and those of the degenerative spine in particular – are based on the use of high-field equipments (equal to or greater than 1.5 T), powerful and efficient gradient systems, and phased-array receiving coils. The area to be explored can be the entire spine, but the examination is usually limited to only one region, based on the symptoms and/or previous diagnostic tests and/or other imaging techniques. As already mentioned for X-rays and CTs, with MRIs the study techniques are modified according to the area to be examined. However, both in the cases in which the entire spine study is indicated, and in the more common cases of “segmental” studies, a standard examination method can be indicated, forming the basis of the study.
An MRI of the spine for degenerative diseases (Figs. 2.6, 2.7, and 2.8) should include sagittal and axial T1- and T2-weighted images (T1WI and T2WI) as well as coronal (T1WI or T2WI) [21]. Depending on the imaging sequence, the repetition times (TR) and echo times (TE) to obtain T1 and T2 images may vary. In general, however, for T1, in Spin-Echo (SE) and Turbo Spin-Echo (TSE) sequences, they range between TR of 400–700 ms and TE of 15–30 ms, while the variability grows in the case of T2WI, almost constantly for TSE, with TR ranging between 1,500 and 3,000 ms and effective TE of 120–150 msec. The sagittal images must have an anatomical coverage sufficient to fully include the foramina on both sides, using a number of slices that depends on the slice thickness. In most cases, the sagittal sequences are obtained using a Spin-Echo (SE) technique or, more often, Turbo Spin Echo (TSE), with 2D acquisition and slice thicknesses between 3 and 4 mm.
MRI evaluation of the cervical spine in degenerative disease. TSE sagittal T1 (a), TSE sagittal T2 (b) weighted images; GRE axial T1 (c), GRE axial T2 3D with water selection (d). Degenerative disc disease with spondylosis are shown at C4–C5 and C5–C6 level. Note the evidence of central gray matter intensity on axial T2 3D image
MRI evaluation of the lumbar spine in degenerative disease. TSE sagittal T1 (a), TSE sagittal T2 (b), TSE axial T1 (c), BFE axial T2 (d), TSE coronal T2 (e), TSE (2D) coronal myelogram (f). There are diffuse degenerative disc and facet changes, especially at L4–L5 and L5–S1 levels. At L4–L5 spondylosis, disc protrusion and facet disease result in left L5 lateral recess stenosis with deformity of the thecal sac (white arrows)
For axial images, the choice of sequences is more complicated, because it is more related to the anatomical area (and, therefore, determined by the need to avoid pulse/movement artifacts), and because it is largely based on the clinically suspected pathology or visualized through sagittal images. In the case of axial images, especially of T2WI, 3D sequences are frequently used, both with TSE and with Gradient Echo (GRE) techniques. 3D sequences are preferred in particular when the area of interest is small, for example, in the case of two or at most three intersomatic levels (Fig. 2.9). Meanwhile, TSE and SE sequences are performed according to the rules previously defined for sagittal images. In the case of axial GRE sequences, T1 and T2 weighting depends mainly on the selection of the “flip angle,” with T2WI (T2*) based on the choice of short flip angles (<30 ms) and T1WI with large flip angles. Coronal images are (or should be) part of all MRI studies of the spine, as multiplanarity represents an inherent essential advantage of MRI, and because it enhances the exploratory potential of MRI, allowing, for example, the visualization of paravertebral changes/diseases that are otherwise missed. In the case of coronal images, both T1 or T2 images can be obtained.
C5–C6 disc herniation; different axial T2 image sequences. TSE sagittal T2 (a), GRE axial T2 3D with water selection (b), GRE axial T2 2D with water selection. Disc herniation is shown on sagittal T2 image; the soft tissue left postero-lateral herniated disc (white arrows) is better demonstrated on axial T2 2D (c) than on axial T2 3D (b), in which there is no significant contrast between spondylosis and herniated disc
The sagittal, axial, and coronal images should be considered the basis of all spinal MRIs, but can – and in some cases must – be supplemented by more specific scanning planes and sequences, selected to complete the study and optimize the diagnosis. For example, oblique scanning (or reconstruction if there are 3D acquisitions) planes can be added according to the axis of emergence of the cervical or lumbar roots and/or according to other structures of clinical interest (Fig. 2.10). In other cases, the angle of the axial images may have to be changed. These are typically obtained along the axis of the discs, but sometimes instead along the orientation of the lamina (for example, if we need to prove/exclude spondylolysis).
Recurrent L4–L5 left postero-lateral disc herniation; usefulness of coronal oblique acquisition. TSE sagittal T1 (a), TSE sagittal T2 (b), TSE axial T1 (c), BFE axial T2 (d), TSE oblique coronal T2 (e). The recurrent herniated disc (white arrows) is shown on all imaging planes; note the evidence of the lesion on oblique coronal T2 image (e)
Fat-suppression images are frequently used in degenerative spinal diseases. Fat signal suppression can be achieved with the short tau inversion recovery (STIR) technique or with a TSE sequence, using spectral suppression (SPIR, SPAIR). The main advantage of these sequences is in the optimal demonstration of bone edema and fluid components on T2WI in which the signal of the fat is cancelled. In this way, for example, we can recognize and characterize algodystrophic or Modic [22, 23] type “discogenic” changes, edema resulting in instability and/or typical of vertebral fractures. The choice of suppression on T2WI (STIR or SPIR/SPAIR) is largely dependent on the equipment used and the efficiency of suppression in different locations/areas, but in general the rule is that STIR is preferred for large fields of view and SPIR/SPAIR for small fields of view. This usually leads to favoring the STIR in sagittal and coronal images and the SPIR/SPAIR in axial images (Fig. 2.11). It must also be considered that the quality of suppression is usually better in the lumbar and cervical spine compared to the thoracic spine, because the presence of respiratory artifacts and abundant air (in the lungs) degrades the result in the thoracic spine. When faced with ligament changes/injuries, obtaining high-resolution proton density (PD) images with fat suppression has also proved useful. These sequences not only optimally display the longitudinal ligaments (anterior and posterior) but also the ligamenta flava, the interspinous ligaments, and the most complex ligaments in the craniocervical junction.
STIR sagittal images in spinal degenerative disease. Patient 1: TSE sagittal T1 (a), TSE sagittal T2 (b), STIR sagittal T2 (c). Degenerative C4–C5, C–5–C6, C6–C7 disc disease without vertebral signal changes. Patient 2: TSE sagittal T1 (d), TSE sagittal T2 (e), STIR sagittal T2 (f). Large L4–L5 extruded, cranially migrated, herniated disc. Modic 3 signal changes are seen at L5–S1, completely suppressed by STIR sequence (confirming fat-like signal). Note, in both patients, the optimal homogeneity of fat-suppressed images using STIR acquisitions
Fat-suppressed T1WI is instead almost always obtained using the spectral technique (SPIR) and its use is mostly combined with the intravenous administration of contrast agent (based on gadolinium). The use of intravenous contrast agent in extradural spinal diseases should necessarily lead to the use of SPIR sequences, because, without suppression, the evidence of contrast enhancement (CE) in fat-rich cancellous bone is very limited.
In addition to the need to suppress the fat, the study of the degenerative spine can greatly benefit from the use of sequences that optimize the contrast between the bony and the discal/ligamentous structures. These sequences are very useful in defining, for example, how much of a protrusion in cervical spondylosis is caused by osteophytes (“hard,” calcified) and how much by true disc herniation (“soft”). These are mainly GRE T2* sequences, which facilitate distinction by increasing the contrast between the hypointensity of the bone and the (hyper-) intensity of the disc (Fig. 2.12). According to the findings, the axial or the sagittal plane may be favored.
The use of T2* sequences with fat suppression in 3D high-resolution acquisition optimally marks out the body from the disc, enhances the demonstration ligaments, and, above all, allows an optimal quality of the study on the orientation/integrity of the fibers of the annulus fibrosus. With this technique, for example, we can directly see the interruption of the fibers of the ring that allows the expulsion of a herniated disc (Fig. 2.13).
Large L3–L4 cranially migrated/extruded disc herniation. TSE sagittal T1 (a), TSE axial T1 (b), GRE axial intermediate 3D with water selection (c). The large herniated disc is optimally demonstrated on all imaging sequences; note how on (c) water selection provides excellent evidence of the tear in the annulus fibrosus, allowing the extrusion of the disc material (white arrows)
MRI myelography represents a useful enrichment of the previously described morphological sequences. Its definition comes from a representation similar to that of myelography/saccoradiculography and is obtained using different sequences – 2D and 3D – mostly based on the TSE acquisition, which increase and enhance the CSF signal and decrease the signal of solid tissue (bone, disc, ligaments, spinal cord, spinal nerves). In this way, similar to other “fluid-enhanced” MRIs (MR-cisternography, MR-urography, MR-cholangiopancreatography), we obtain an enhancement of the CSF signal and see – in negative, as a filling defect – the intrathecal spinal nerves and the spinal cord with excellent demonstration of the radicular cervical, thoracic, and, mainly, lumbar root sleeves. MRI-myelography can be achieved with 3D volume study (Fig. 2.14a–c), or, especially in the lumbar and cervical spine, with multiple individual acquisitions according to different angles of view (Fig. 2.14d–f).
MR-myelography using 3D or 2D acquisition; two different patients. Patient 1: TSE sagittal T2 (a), TSE axial T2 (b), oblique sagittal myelogram extracted by 3D MR myelogram (c). Severe L3–L4 stenosis with facet subluxation and instability with complete effacement of the thecal sac; note the complete lack of CSF on axial image as well as the varicoid appearance of roots cranially to the stenosis. Patient 2: TSE sagittal T2 (d), oblique sagittal (e) and coronal (f) MR myelographic images obtained by multiple 2D acquisitions. The large L3–L4 herniated disc results in complete obliteration of CSF space in the compressed thecal sac
In the case of multiple 2D acquisitions, the so-called “single shot TSE” is often used, in which a single TR is used to completely fill the K-space (so that the entire set of images is obtained in just a few seconds). It is important to note that the MRI myelographic images, and more generally those strongly T2WI (with very high TR and TE), increase the fluids/solids contrast, but offer little or no intraparenchymal contrast, and thus are not suitable, for example, for detecting intramedullary lesions.
The use of magnetic resonance angiography (MRA) in degenerative diseases is limited and marginal. It is mostly used when we want to demonstrate the effect of spondylosis and unco-arthrosis on the course of the vertebral arteries in the transverse processes. For these requirements, we can use the so-called phase-contrast MRA (3D, velocity-encoding between 20 and 40 ms) or the so-called “contrast enhanced” technique, based on a bolus of paramagnetic contrast agent.
In degenerative diseases of the spine, the administration of a contrast agent during MRI is used only rarely, mostly in cases where there is a different suspicion (i.e., for exclusion of neoplastic and infectious diseases) or in postoperative studies. In fact, it is certainly true that the contrast agent modifies the diagnosis of degenerative diseases in a few selected cases. It is equally true that the use of contrast agent (combined with fat suppression) increases the evidence of degenerative vertebral, discal, and ligament changes. The contrast enhancement (CE) can better define herniated discs (and differentiate them from the adjacent venous congestion), confirms the diagnosis of infectious or “chemical” discitis, and strengthens the diagnosis of interapophyseal arthrosis/arthritis [24] (Fig. 2.15)
L3–L4 spinal stenosis and instability; the contribution of contrast-enhanced fat-suppressed (fs) T1 images. TSE sagittal T2 (a), T1 fs sagittal (b), T1 fs coronal (c) and T1 fs axial (d) images with contrast agent. Note how the contrast enhancement marks both the subchondral disc changes as well as the bilateral facet joint degenerative disease
To complete the brief presentation on the MRI study technique, it is worth recalling that “axial load” studies, performed with MRI and/or CT scans, have been introduced in clinical practice [25, 26]. These studies mainly use the so-called “axial loader,” that is, a mechanical system that aims to simulate the functional load on the spine (especially the lumbar) through the use of an apparatus that, with the patient supine, exerts scalable pressure on the shoulders, usually selected based on the body weight of the patient. The use of the axial loader has been supported by many authors and is supposed to serve the dual purpose of highlighting signs of instability under load and of increasing the sensitivity of MRI, revealing root/ganglion compressions that are not evident with the patient supine and that become manifest under load. The authors had the opportunity to use the axial loader in both CT and MRI scans, and consider the system unreliable. In fact, the loading conditions created by the axial loader do not bring into play the muscular dynamics and do not reproduce the situation of the upright position. This risks creating many false positives and highlighting discal protrusions/herniations that are not responsible for clinical symptoms or deserving of treatment (surgery). Think, for example, how many disc herniations are without corresponding clinical symptoms. The authors believe rather that, in the case of a symptomatic patient (without evidence of radicular compression and instability in the classic MRI), we can proceed to an MRI using the new reclining systems (intermediate field) that allow MRI studies in the upright position and have achieved a good level of image quality (although still lower than that of conventional high-field MRI). In the case of clinical or MRI suspicion of instability and unavailability of reclining MRI (the technology is not still currently accessible), the authors still prefer “dynamic” (flexion/extension) X-ray in the upright position, also because of the lower costs of such a choice.
Invasive Diagnostic Tools
Until the introduction of CT, myelography enjoyed a widespread use, especially in the diagnosis of lumbar radiculopathy and spondylotic myelopathy. With the advent and improvement of CT, the indication for intrathecal contrast-enhanced studies became limited and changed greatly, aiming mainly to demonstrate the effects of degenerative disease on the “content” and shifting the focus of imaging to CT-myelography. However, the impact of MRI has virtually eliminated the use of CT-myelography, which is limited primarily to patients with pacemakers or other absolute contraindications to MRI, for whom it is necessary to find the causes of spinal cord or radicular impairment. In fact, some authors continue to perform myelography and CT-myelography studies even in patients who can undergo an MRI, supporting the effectiveness and reliability of the technique and claiming the importance of the dynamic study (e.g., standing up, with dynamic flexion and extension tests).
Gas myelography has been completely abandoned and in cases in which we perform myelography/CT myelography, the introduction of contrast agents is almost exclusively via lumbar puncture, by administration of iodinated nonionic contrast agents of low osmolarity. When it is important to obtain dynamic myelographic studies, 10 cc of contrast agent are usually administered at a concentration of 300–350 mg I/ml and we proceed to radiography in two orthogonal and in oblique projections. After achieving the collection of the contrast agent in the areas of clinical interest, with an appropriate position and inclination of the patient table, and after the X-ray documentation, we proceed to the acquisition of CT myelography. In most common cases in which the indication is derived from the impossibility of use of MRI, an evaluation by CT myelography is instead sufficient. In these cases, the use of a smaller amount of contrast agent is preferred, and especially with lower iodine concentration. A lower contrast agent concentration is useful both to reduce side effects and to have a less increased density, as the opposite would disturb the detection of thinner intraspinal structures in the CT myelography. Indeed, it is essential to obtain a good contrast agent dilution in the CSF, to obtain a more homogeneous opacification, and this is achieved with multiple changes of position and rotations of the patient [27, 28].
Discography may provide valuable information in patients with unexplained chronic back pain regarding a possible discogenic origin of the pain. Discography is the only imaging procedure for the assessment of back pain that directly tries to correlate the patient’s pain response to internal disc morphology. It is more sensitive than MR in the detection of internal disc disruption. The technique consists of percutaneously placing a needle into a disc, injecting a low volume of iodinated contrast agent (1.5–3.0 ml) into the nucleus polposus, and then assessing the patient immediate pain response. The main value is in the clinical assessment of patient’s response to pain; the second value is in disc morphology assessment (discogram) by radiography and CT scans, based on the Modified Dallas Discogram Scale (Grade 0–5) [29].
There are other spinal contrast agent injections. A very low volume of nonionic iodinated contrast agent (0.5–1 ml) is injected during fluoroscopy-guided percutaneous spinal procedures. These include selective nerve root block, in order to document the correct needle position into the nerve root sleeve before injection of the therapeutic agents, and facet or sacro-iliac joint injection, in order to document the correct intra-synovial position of the needle before injection of the therapeutic agents. A larger volume of diluted contrast agent (2–3 ml) is injected during epidural block procedures, in order to visualize (by a lateral-view fluoroscopic image) the correct position of the needle tip evidenced by spread of the agent within the epidural space, before injection of the therapeutic agents.
Nuclear Medicine
The role of nuclear medicine in the characterization of bone degenerative lesions, in particular in the spine, is definitely limited. In the great majority of cases, the detection of changes is an incidental finding in the course of bone scans with diphosphonates, performed for the identification of skeletal metastases in cancer patients or for the diagnosis of benign bone tumors. In such cases, we typically see a symmetrical uptake of the radiopharmaceutical in the interapophyseal facet joints of the lumbar vertebrae, especially L5 (Fig. 2.16), in patients with lumbar osteoarthritis associated with “lower back pain,” or “mid-cervical-lateral-focus” at the level of a cervical vertebral body in patients with neck pain [30].
However, bone scintigraphy retains an important role in the differential diagnosis between benign and malignant changes, especially in the case of single skeletal metastasis and/or in the few patients in whom the CT and MRI give equivocal results or do not allow a reliable disease characterization. The sensitivity of bone scintigraphy (greater than 70 % in different series) can be increased up to 90 % with the use of hybrid SPECT (single-photon emission tomography)/CT imaging. The hybrid method allows the integration of the functional information of bone scintigraphy with the morphological information of a MDCT. SPET/CT allows a better localization of the radiopharmaceutical uptake compared to the planar images of bone scintigraphy alone, especially in the spine. Indeed, uptakes localized in the vertebral pedicle have a higher likelihood of malignancy compared to the same finding in the facet joints or in the vertebral body (88 % vs. 21–57 %) [31].
Nuclear medicine functional imaging continues to be essential in differentiating degenerative changes from inflammatory changes, in particular as regards spondylodiscitis. The most frequently used methods are SPET/CT with 67Ga-citrate and, more recently, 18F-FDG (fluoro-deoxy-glucose) PET (positron emission tomography)/CT [32]. A recent review has shown that SPET/CT with 67Ga-citrate has a sensitivity equal to MRI (92 %) but higher specificity (92 vs. 77 %), especially in cases where the MRI proves not definitive (Fig. 2.17). 18F-FDG (fluoro-deoxy-glucose) PET (positron emission tomography)/CT has sensitivity, specificity, and accuracy of 100, 87, and 96 %, respectively, in spinal infections, and is used especially in mild spondylitis and discitis, particularly if associated with concurrent infection of the adjacent soft tissues [33].
Conclusion
Imaging has become the basis for the diagnosis and choice of treatment in degenerative spinal disease. The imaging assessment has rapidly changed over the past 20 years, with a drastic reduction in the role and appropriateness of radiographs and the predominant use of MRI. In practice, in most clinical situations of degenerative spinal diseases, the first imaging tool is now the MRI and it is only on the basis of the MRI findings that the indication for a targeted complement by CT or by radiographic study is proposed, which increasingly must include a functional/dynamic study (Fig. 2.18). It is essential that MRI allows us to obtain a certain diagnosis in order to reduce the time and cost of diagnosis, as well as to limit the use of imaging tools that require radiation exposure. It therefore becomes essential that, during the MRI study, the radiologist, starting from the standard images/sequences in multiple planes, integrates in the MRI procedure the specific sequences that will allow solving the clinical problems of the patient and, if appropriate, contribute to suggesting the subsequent diagnostic procedure.
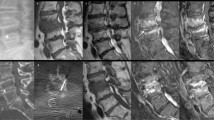
Exhaustive imaging assessment of lumbar spine instability. TSE mid-line sagittal T1 (a), parasagittal (b), BFE axial T2 (c), TSE axial fat-suppressed (SPAIR, d), sagittal (e), axial (f) and coronal (g) CT reconstructions, X-ray lateral projection, flexion study (h). Sagittal T1 images show longstanding disc L5–S1 degenerative disease, minimal L4–L5 listhesis, and obvious signal modification of articular pillars (arrow); on axial BFE image there are obvious irregularities of interpophyseal joint surfaces with some subluxation on the left side. The acquisition of T2 axial fat-suppressed SPAIR images increases the evidence of bone edema . On the basis of MRI findings, the patient’s evaluation has been completed by MDCT and functional/dynamic upright X-ray study. CT study optimally depicts the facet joint modifications with ankylosis and subchondral erosions. The upright flexion lateral X-ray demonstrates evident instability with L4–L5 degenerative spondylolisthesis
References
Boos N, Aebi M. Spinal disorders. Fundamentals of diagnosis and treatment. New York: Springer; 2008.
Fullenlove T, Williams AJ. Comparative roentgen findings in symptomatics and asymptomatics backs. Radiology. 1957;68:572–4.
Gehweiler JA, Daffner RH. Low back pain: the controversy of radiologic evaluation. AJR Am J Roentgenol. 1983;140:109–12.
Wood KB, Popp CA, Transfeldt EE, Geissele AE. Radiographic evaluation of instability in spondylolisthesis. Spine. 1994;19:1697–703.
Pitkanen M, Manninen HI. Sidebending versus flexion-extension radiographs in lumbar spinal instability. Clin Radiol. 1994;49:109–14.
Leone A, Costantini AM, Guglielmi G, Tancioni V, Moschini M. Degenerative disease of the lumbosacral spine: disk herniation and stenosis. Rays. 2000;25(1):35–48. Review.
Scavone JG, Latshaw RF, Weidner WA. Anteroposterior and lateral radiographs: an adequate lumbar spine examination. AJR Am J Roentgenol. 1981;136:715–7.
Dupuis PR, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH. Radiological diagnosis of degenerative lumbar spinal instability. Spine. 1985;10:262–6.
Dvorak J, Panjabi MM, Chang D, Theiler R, Grob D. Functional radiographic diagnosis of the lumbar spine: flexion-extension and lateral bending. Spine. 1991;16:562–71.
Hayes MA, Howard TC, Grue CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine. 1989;14:327–31.
Lowe RW, Hayes TD, Kaye J, Bagg RJ, Luekens CA. Standing roentgenograms in spondylolisthesis. Clin Orthop Relat Res. 1976;117:80–4.
Shaffer WO, Spratt KF, Weinstein J, Lehmann TR, Goel V. The consistency and accuracy of roentgenograms for measuring sagittal translation in the lumbar vertebral motion segment. Spine. 1990;15:741–50.
Boden SD, Wiesel SW. Lumbosacral segmental motion in normal individuals: have we been measuring instability properly? Spine. 1990;15:571–6.
Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res. 1982;165:110–23.
Cacayorin ED, Kieffer SA. Applications and limitations of computed tomography of the spine. Radiol Clin North Am. 1982;20(1):185–206.
Rothman SLG, Glenn WV. Multiplanar CT of the spine. Baltimore: University Park Press; 1985. Chapters 1–4, p. 1–112, chapters 16–17, p. 477–504.
Perrone L, Politi M, Foschi R, Masini V, Reale F, Costantini AM, Marano P. Post-processing of digital imaging. Rays. 2003;28(1):95–101. Review.
Fast A, Goldsher D. Navigating the adult spine: Bridging clinical practice and neuroradiology. New York: Demos; 2007.
Larde D, Mathieu D, Frija J, Gaston A, Vasile N. Spinal vacuum phenomenon: CT diagnosis and significance. J Comput Assist Tomogr. 1982;6:671–6.
Czervionke LF, Daniels DL. Degenerative disease of the spine. In: Atlas SW, editor. Magnetic resonance imaging of the brain and spine. New York: Raven; 1991.
Colosimo C, Gaudino S, Alexandre AM. Imaging in degenerative spine pathology. Acta Neurochir Suppl. 2011;108:9–15.
Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–86.
Modic MT, Ross JS. Lumbar degenerative disk disease. Radiology. 2007;245:43–61.
Colosimo C, Cianfoni A, Di Lella GM, Gaudino S. Contrast-enhanced MR imaging of the spine: when, why and how? How to optimize contrast protocols in MR imaging of the spine. Neuroradiology. 2006;48:18–33.
Saifuddin A, Blease S, MacSweeney E. Axial loaded MRI of the lumbar spine. Clin Radiol. 2003;58(9):661–71.
Kinder A, et al. Magnetic resonance imaging of the lumbar spine with axial loading: a review of 120 cases. Eur J Radiol. 2012;81(4):e561–4.
Fenton DS, Czervionke LF. Image-guided spine intervention. Philadelphia: Saunders (Elsevier); 2003.
Williams AL, Murtagh FR. Handbook of diagnostic and therapeutic spine procedures. St. Louis: Mosby (Elsevier); 2002.
Sachs BL, Vanharanta H, Spivey MA, et al. Dallas discogram description: a new classification of CT/discography in low back disorders. Spine. 1987;12:287.
Scharf S. SPECT/CT imaging in general orthopedic practice. Semin Nucl Med. 2009;39(5):293–307.
Reinartz P, Schaffeldt J, Sabri O, Zimny M, Nowak B, Ostwald E, Cremerius U, Buell U. Benign versus malignant osseous lesions in the lumbar vertebrae: differentiation by means of bone SPET. Eur J Nucl Med. 2000;27:721–6.
Treglia G, Focacci C, Caldarella C, Mattoli MV, Salsano M, Taralli S, Giordano A. The role of nuclear medicine in the diagnosis of spondylodiscitis. Eur Rev Med Pharmacol Sci. 2012;16 Suppl 2:20–5.
Rosen RS, Fayad L, Wahl RL. Increased 18F-FDG uptake in degenerative disease of the spine: characterization with 18F-FDG PET/CT. J Nucl Med. 2006;47:1274–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Colosimo, C., Pileggi, M., Pedicelli, A., Perotti, G., Costantini, A.M. (2014). Diagnostic Imaging of Degenerative Spine Diseases: The Technical Approach. In: Menchetti, P. (eds) Minimally Invasive Surgery of the Lumbar Spine. Springer, London. https://doi.org/10.1007/978-1-4471-5280-4_2
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5280-4_2
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5279-8
Online ISBN: 978-1-4471-5280-4
eBook Packages: MedicineMedicine (R0)