Abstract
Salmonella belong to the group of Enterobacteriaceae that are aerobic, gram-negative rods and approximately 1–3 μm × 0.5 μm in size [1, 2]. Currently there are approximately 2,400 pathogenic species of salmonella. Salmonella was first identified in 1880 by Eberth from the mesenteric nodes and spleen of a patient dying from typhoid fever [3, 4].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Salmonella belong to the group of Enterobacteriaceae that are aerobic, gram-negative rods and approximately 1–3 μm × 0.5 μm in size [1, 2]. Currently there are approximately 2,400 pathogenic species of salmonella. Salmonella was first identified in 1880 by Eberth from the mesenteric nodes and spleen of a patient dying from typhoid fever [3, 4]. Later in 1884 Gaffky was able to isolate the bacillus. A year later Salmon and Smith described a bacillus that is now known to be S. Choleraesuis, the first bacteria that affects both human and animals [5]. Salmonella possess a flagellar antigen (H), somatic (O), and a surface antigen Vi. Salmonella are divided into two subspecies of S. enterica and S. bongori. S. bongori contains 8 serovars and S. enterica contains the other approximately 2,300 serovars that are divided into 6 subspecies based on flagellar H antigen. Salmonella nomenclature has undergone many changes [6]. Serotypes of Salmonella are recognized using the technique recommended in the Kauffman–White scheme.
Only few Salmonella serovars have been identified to cause disease in animals [7]. Salmonella subspecies enterica serovar Typhi is the most common cause of infection in humans and serologically is placed in Salmonella group D due to O antigens 9 and 12 [8]. The genetic makeup of the organism has not shown variation geographically and is stable with a few exceptions of isolates from Indonesia that have slightly different flagellar antigens. S. Typhi expresses a polysaccharide capsule Vi (virulence antigen) on its surface and is highly stable serologically compared to other Salmonella serotypes [9]. Presence of Vi prevents the binding of O antigen to the O antibody and thus enables the pathogenesis of the organism. Clinical severity of typhoid fever is a result of the Vi antigen that increases the infectivity [10]. However, Vi-negative strains have also been identified; therefore, Vi presence is not essential for S. Typhi-related typhoid fever. In vitro studies have shown that the Vi antigen of S. Typhi has anti-opsonic and antiphagocytic characteristic that reduces the level of secretion of Salmonella serovar Typhi-induced tumor necrosis factor alpha (a marker of activation) by human macrophages and increases the level of resistance of the organism to oxidative killing [8].
2 Typhoid Fever Epidemiology
A recent analysis estimated that there are 21 million typhoid fever cases per year and 216,000 deaths [11]. An earlier WHO estimate of the global typhoid disease burden based on a study from 1984 indicated around 17 million cases and approximately 500,000–600,000 deaths per year [11, 12]. Recent analysis assumes an average case fatality rate (CFR) of only 1%, which is at the low end of most estimates in the literature. Typhoid fever is considered endemic in most of the developing world. An estimated 90% of typhoid-related deaths occur in Asia [11, 13].
The recent burden of disease analysis was based on data derived from selected studies in a total of only 10 developing countries that included only one from sub-Saharan Africa (South Africa). High incidence rates of typhoid have been documented for south and Southeast Asia, but arbitrary estimates were made for many regions of the developing world that lacked any data, especially Africa. The paucity of reliable incidence data from most developing countries reflects the fact that laboratories capable of bacteriologic confirmation are lacking in much of the developing world [13]. As well as typhoid fever being endemic, the disease has also appeared as epidemic forms in central Asia, Africa, and south Asia [14].
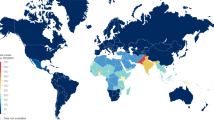
The incidence of typhoid fever may vary considerably not only between, but also within, countries [15] (Fig. 1). In some countries, evidence suggests that residents of poor urban areas are at considerably higher risk than rural dwellers. Until recently typhoid was considered as a disease of school-aged children. More recent systematic population-based studies from India, Bangladesh, and Pakistan have confirmed that the incidence is higher in young children [16–19].
Estimated distribution of typhoid fever burden in 2000 (a) and the geographic differences of typhoid fever incidence in Vietnam (b) [15]
Typhoid fever is a waterborne disease transmitted by the ingestion of food or water contaminated with excreta of patients and asymptomatic carriers and is therefore most common in areas with poor water and sanitation systems and practices. Common sources include polluted water and contaminated food (e.g., milk products), often eaten outside of the home and handled by infected persons. Other risk factors for increased transmission include recent typhoid fever in the household, a lack of toilet in the household, drinking unboiled water, not using soap for hand washing, and sharing food from the same plates as others [20, 21].
3 Typhoid Fever: Clinical Presentation and Outcome
Typhoid fever caused by Salmonella Typhi is an acute generalized infection of the reticuloendothelial system, intestinal lymphoid tissue, and gall bladder. The clinical presentation of the disease varies from high-grade fever to more systemic involvement of nervous system [22]. Typhoid is often confused with other acute febrile illnesses until it persists for more than 3 days and does not respond to symptomatic treatment or first-line antimicrobial therapy [23]. Typhoid was recognized as a distinct disease in the earlier quarter of nineteenth century and soon gained significance as a serious health problem due to its ability to spread quickly in populations, especially those living collectively such as army soldiers and in dormitories [2, 20, 24].
Presentation of typhoid fever varies ranging from mild fever to more severe forms such as toxic shock. Symptoms include sustained high-grade fever (~104°F), profuse sweating, altered bowel habits from constipation in adults to diarrhea in children, malaise, myalgia, a dry cough resembling bronchitis, anorexia, nausea, and in some cases non-bloody diarrhea. If fever lasts for more than 5 days, a rash of flat, rose-colored spot may appear. The incubation period for a non-complicated case of typhoid fever is 10–14 days. Malaise and lethargy can continue for a couple of months even when the disease may have resolved. If left untreated, typhoid fever progresses through the four stages, each lasting approximately 1 week. In the first week, there is a slowly rising temperature with relative bradycardia, malaise, headache, and cough. In some cases bleeding from nose (epistaxis) and abdominal pain may also occur. The number of circulating white blood cells decreases with eosinopenia and relative lymphocytosis; blood cultures are positive for Salmonella Typhi, while Widal is negative in the first week [25, 26].
In the second week, fever has a plateau of around 104°F and heart rate is slow with a thready pulse. Delirium is frequent and calm, but sometimes agitated. Rose spots appear on the lower chest and abdomen in around 30% of patients. Abdominal symptoms become more obvious with pain in the right lower quadrant. Diarrhea with a frequency of six to eight stools per day may occur during this time; however, constipation is also frequent. The spleen and liver become palpable and tender at this time. Elevation of transaminases can be seen on liver enzyme tests. Anti O and Anti H on Widal are strongly positive; blood culture may also be positive depending on the quantity of blood taken from the patient. In the third week of fever, complications appear including intestinal hemorrhage, encephalitis, metastatic abscess, cholecystitis, endocarditis, and osteitis. Overall 10–15% of typhoid fever cases develop complications. Intestinal perforation may occur in 1–3% of cases leading to peritonitis and ultimately to death if proper surgical intervention is not undertaken. In the fourth week fever is still high and oscillates very little. The patient has delirium due to dehydration. Other complications include disseminated intravascular coagulation that may lead to early death. Pneumonia is more common in children than in adults. Some of the rare outcomes reported are hepatic, splenic, and bone marrow granulomas; splenic and liver abscesses; pleural effusion; phagocytic syndrome; pseudotumor cerebri; hemolytic endocarditis and pericarditis. Arrhythmias or cardiogenic shock are manifestations of toxic myocarditis with fatty infiltration of the heart [1, 2, 24].
Hospitalization rates of typhoid fever cases vary from 10 to 40%, while the rest either self-medicate or are treated on an outpatient basis [16]. Population-based studies have reported variation in hospitalization rates. In settings where early treatment was provided due to extensive and systematic surveillance, it was possible to treat typhoid early. On the other hand patients who followed the regular health system mechanism had higher rates of hospitalization and complication. The average length of hospital stay ranges from 10 to 15 days.
Following recovery, convalescing patients may continue to excrete S. Typhi in the feces for almost 3 months. One to four percent of cases become long-term carriers, excreting the organism for more than 1 year. Most carriers are asymptomatic. The average case fatality rate is less than 1%, but this is variable among the endemic countries, with Pakistan and Vietnam having a case fatality rate of less than 2% and Indonesia and Papua New Guinea as high as 30–50%. Young children have been found to be at a higher risk of severe typhoid. Case fatality rates have been found to be 10 times higher in children younger than 4 years compared to older children. The most significant contributor to a poor outcome is a delay in the initiation of an effective antibiotic treatment. In untreated cases, fatality can go as high as 10–20%. The gall bladder carriage rate is 1–5% of the survivors of typhoid infection. Carrier status also increases the chances of hepatobiliary cancers [24, 27–30].
3.1 Diagnosis
Following ingestion of the Salmonella pathogen, there is an asymptomatic period. The incubation period for typhoid fever is 7–14 days and is influenced by the dose of the inoculum. Secondary bacteremia follows infection and coincides with the onset of symptoms such as high-grade fever and malaise. Other symptoms and signs that may help in the clinical diagnosis are loss of appetite, abdominal discomfort, headache, and severe myalgia. A coated tongue, tender abdomen, hepatomegaly, and splenomegaly are also common. Delirium, confusion, and convulsions may also occur in children less than 5 years. As a result of bacterial dissemination throughout the body, the patient may present with systemic involvement such as respiratory, neurological, and abdominal illnesses.
The diagnosis of typhoid fever in endemic settings is mostly clinical and relates to the clinical experience of the attending physician. There have been repeated and regular attempts to establish diagnostic criteria that combine clinical presentation and laboratory investigations. Such attempts have not resulted so far in the development of a diagnostic technique that will help overcome current diagnostic challenge. Despite reservations about the sensitivity, specificity, and predictive value of Widal, it is the most common laboratory method used for diagnosis of typhoid. Widal detects antibodies that are also cross-reactive with other Enterobacteriaceae. In typhoid patients, antibodies only appear in the second week; therefore, usefulness of the test is limited in the initial stages of the disease [31]. Other serological tests such as Tubex and Typhidot have not shown promising results. The gold standard for the diagnosis of typhoid is isolation of the bacteria from blood and/or bone marrow. Bone marrow cultures have higher sensitivity compared to blood culture. The bone marrow culture is positive for 80–95%. In cases where patients have been treated with antimicrobials, the bone marrow culture may still lead to S. typhi isolation. Blood culture is positive 60–80% of the time but the yield varies with the quantity of blood taken [23, 32–35].
3.2 Management
Lack of simple, accessible cost-effective tools for accurate diagnosis of typhoid fever results in delayed diagnosis and failure to adequately treat the disease. These factors in turn contribute to the high emergence of severe form of the disease in endemic settings. In initial stages, the disease is either treated at home or by informal health sector. Improper diagnosis leads to inappropriate management and resultant increase in severity of the disease ultimately leading to hospitalization and fatal outcomes. Careful assessment of fever cases is recommended. In cases where fever is more than 5 days, laboratory investigation such as blood culture is advised. However, clinical symptoms and signs should be correlated with laboratory findings. In cases where either the provisional diagnosis is typhoid fever or there is serological or bacteriological evidence of disease, first-line antimicrobial therapy should be initiated. Third-generation cephalosporins are the most effective treatment for typhoid fever with cure rates of 90–98% [27].
4 Control Strategies
Similar to other diseases spread by the fecal–oral route, typhoid fever predominates in areas with inadequate water and sanitation systems and/or poor hygienic practices. Typhoid was effectively eliminated in developed countries mainly through large-scale development of water treatment (e.g., chlorination), construction of deep wells, and piped water and sewerage systems. Impact of safe drinking water and adequate sanitation on diarrheal diseases has also been demonstrated in northeast Brazil where a 22% reduction in diarrheal diseases was evident after an expenditure of nearly 900 million dollars on infrastructure development. Infrastructure development for provision of safe water and proper sanitation is costly to build for many developing country government budgets. Considering most of the typhoid fever cases occur in urban slums of Asian cities, diversion of development budgets seems unrealistic in near future [36–38].
In lieu of the existing situations, alternative short-term interventions are recommended for the reduction of disease burden in these areas. These interventions include intensive hygiene education for hand washing using soap, discouraging open defecation especially by children, and the proper disposal of garbage and feces. There is evidence that such interventions have been effective in the control of enteropathogens at small scale. The practicality of such interventions at large scale has still not been answered systematically [39–42].
In the existing circumstances, a typhoid fever vaccination program may provide a short-term alternative strategy coupled with a continuous advocacy for development of infrastructure for safe water provision and clean and hygienic sanitation. There is evidence that immunization can virtually eliminate typhoid fever in a relatively short period of time, especially when targeted toward high-risk age groups and geographic areas. Due to the reduction in the price of the vaccine, it is now becoming more affordable to countries with high burden of typhoid fever. In order to make a typhoid fever vaccination program more effective, it must be introduced as a typhoid fever control program that should have other components such as hygiene education messages, sanitation improvements (e.g., latrines), and improved water supply and quality measures [19, 37, 43–47].
4.1 Antimicrobial Resistance
Increasing resistance to available antimicrobials is another challenge for typhoid fever control. Outbreaks of S. Typhi strains resistant to chloramphenicol first appeared in the 1970s in several parts of the world. As new drugs such as ampicillin and co-trimoxazole became available, resistance against these drugs also emerged. Outbreaks of multi-drug resistance (MDR), defined as resistance to first-line antibiotics, were first reported in the late 1980s in south Asia and the Middle East that later spread to east Asia and Africa. In Vietnam, 86% of all isolates were found to be multi-drug resistant. MDR typhoid has been associated with more severe illness and higher rates of complications and deaths, especially in children under 2 years of age. The emergence of multi-drug resistance S. Typhi strains has led to the widespread use of fluoroquinolones, such as ciprofloxacin and ofloxacin. However, outbreaks of nalidixic acid-resistant typhoid (called NARST) started to occur in Vietnam and Tajikistan in the early 1990s and then spread to Pakistan and India [32]. Nalidixic acid-resistant typhoid cases respond less well to fluoroquinolones, exhibiting more prolonged fever than sensitive cases, and, in one study, a 10-fold higher rate of post-treatment stool carriage was observed compared to sensitive cases (20% vs. 1.8%), increasing their potential to infect others. Cases of full-blown resistance to ciprofloxacin have also reported from Pakistan and India [33, 48–53].
More recent data from population-based studies confirm that multi-drug and nalidixic acid resistance is a serious problem in south and southeast Asia [14]. Sixty-seven percent of isolates tested in Karachi, 22% in Hue, and 7% in Kolkata were multi-drug resistant, and high rates of nalidixic acid resistance were found in all three sites – 59% in Karachi, 58% in Kolkata, and 44% in Hue. Two isolates in the India site (1.6%) were found to be ciprofloxacin resistant. On the other hand, no drug resistance was found in the Indonesian and Chinese sites (Table 1). The increase in the resistance to available antibiotics may result to increase in the fever duration, decrease in management options, and an economic burden on the families. The often non-specific symptoms of typhoid fever can make the clinical diagnosis difficult and it can be confused with malaria, dengue fever, influenza, and other febrile illnesses. Confirmed diagnosis requires isolating S. Typhi in the laboratory through blood cultures, bile-stained duodenal fluid culture, or occasionally through bone marrow culture. Unfortunately, such invasive tests are not conducted for the majority of patients in developing countries, especially those treated in non-hospital settings [14, 24, 54].
4.2 Vaccination
The use of new-generation antimicrobials to manage increasing resistance has increased the cost of treatment. The cost of illness, due to antimicrobial-resistant typhoid, is on average nearly four times greater than those who responded well to the first-line antimicrobial treatment (Table 2). Typhoid fever can have a devastating financial impact on families in several of these largely poor communities as the majority of costs of illness are private costs equivalent of 1.6 and 1.2 months of an average household income. These findings of disease burden from various parts of the world have important implications for typhoid fever immunization strategies at the country level, as they suggest that in many countries, vaccination in geographically targeted, high-risk populations, rather than universal immunization, will be potentially the most cost-effective means of controlling the disease [55].
Typhoid vaccine use for prevention of disease dates back to 1896 with the inoculation of heat-inactivated vaccine. This was the first bacterial vaccine to be widely used in humans. The vaccine was obtained by inactivating the virulent microorganisms with heat or chemicals. The associated adverse effects after administration of killed whole-cell vaccine restricted its wider public health use. The adverse events included fever (6–30%), malaise, local reaction (35%), and headache (10%). During the World Health Organization-sponsored trials, the efficacy of the vaccine was 51–66%, but it was highly reactogenic. Among vaccinees 25% had systemic and local reactions post-vaccination. It is believed that during the process of vaccine production, destruction of some heat-labile antigens resulted in the low efficacy and associated adverse effects. Irrespective of being highly reactogenic, the vaccine was widely used in the military in the early twentieth century due to high reporting of typhoid fever in the sick reports of the English and American armies. The vaccine was shown to reduce typhoid incidence by more than 90% from the time before vaccine introduction. Similarly the Belgian government conducted mass vaccination of the civilian population during the First World War in 1915. More recent examples of use of the killed WC vaccine are in schools and high-risk population in Thailand in the 1960s and early 1970s. A drop in the incidence of typhoid fever was noticed after the introduction of the vaccine. Similarly Cambodia used the vaccine during an outbreak; however, adverse events resulted in the dropping of the fourth dose [7, 56, 57].
In early twentieth century inactivated oral vaccines (acetone-inactivated vaccine and formalin-inactivated vaccine) were used to assess local immunity. These oral inactivated vaccines were evaluated in volunteers and field studies in the 1960s and 1970s. These vaccines could not make it to efficacy assessment and are no longer under consideration for production. The two new-generation typhoid vaccines that are currently internationally licensed and available are the injectable Vi polysaccharide vaccine and the oral, live-attenuated Ty21a vaccine [58–61].
4.2.1 Ty21a
Ty21a is an orally administered, live-attenuated Ty2 strain of S. Typhi in which multiple genes have been chemically mutated, including those responsible for the production of Vi. The vaccine was developed in the 1970s and first licensed in 1989, but initially used only in developed countries (Table 3). This lyophilized vaccine is currently available in two formulations. The enteric-coated capsules given in three to four doses and a liquid suspension consisting of the vaccine in one sachet and a buffer in another are combined with water before administration. The liquid formulation is given in three doses. For both formulations, the doses are administered every other day (e.g., over a 5-day period). The vaccine is licensed for use in persons 6 years and older. While the capsules are often used for travelers to developing countries, the liquid formulation is the one most likely to be used by public health programs in developing countries. The vaccine requires a cold chain (at 2–8°C) and survives for approximately 14 days at 25°C. Ty21a vaccine has been shown to be well tolerated and to have low rates of adverse events. In three double-blinded, randomized controlled efficacy trials in Chile and Indonesia involving approximately 550,000 school children, reactogenicity of the Ty21a vaccine was assessed through active surveillance. The rates of side effects (diarrhea, vomiting, fever, and rash) in the vaccinated groups were not found to be significantly greater than those in the control groups for both the enteric-coated capsule and liquid formulations. In large-scale field trials in children in Egypt, Chile, and Indonesia, Ty21a was found to have protective efficacy rates against blood culture-confirmed typhoid fever of 33–67% for the enteric-coated capsules and 53–96% for the liquid formulation (53–78% for the currently licensed liquid formulation) after 3 years of follow-up, when each was given in three doses every other day (except in Indonesia, where dosing occurred every 7 days). The vaccine appeared to be more efficacious in areas with lower incidence of typhoid (Egypt, Chile) than in hyper-endemic areas, such as Indonesia. Ty21a is therefore considered to provide protection for at least 5–7 years. Large-scale vaccination with Ty21a also appeared to confer herd protection in Chile. These data suggest that the systematic application of live oral typhoid vaccine can notably reduce the incidence of the disease in endemic areas [12, 62–65].
4.2.2 Vi Capsular Polysaccharide
Vi is a subunit vaccine consisting of the purified Vi (“virulent”) polysaccharide outer capsule of the Ty2 strain of S. Typhi. The vaccine is administered subcutaneously or intramuscularly as a single dose of 25 μg. It was first developed in the 1970s and further developed for large-scale manufacture at the US NIH, in collaboration with Pasteur-Merieux-Connaught. First licensed in the USA in 1994, the vaccine is in the public domain and is now being produced by several multi-national and developing country manufacturers. Like other T-independent purified polysaccharide vaccines, Vi does not elicit adequate immune responses in children less than 2 years of age, and thus is licensed for use in persons 2 years and older. The vaccine is highly heat stable and is able to retain its physicochemical characteristics for 6 months at 37°C and for 2 years at 22°C (room temperature). Vi vaccines have been extensively tested in humans and demonstrate a strong safety profile (Table 4). No serious adverse events and minimum side effects were associated with Vi vaccination in large field trials. In a recent multi-center study of Vi effectiveness, the vaccine showed safe and with minimal side effects. There is no booster effect of Vi vaccine [8, 10, 66–72].
4.2.3 New Vaccines in Pipeline
The low-efficacy estimates, inability to confer lifelong immunity, and difficulties in administration through regular and routine public health programs have limited the use of available typhoid vaccines. Therefore, a search for new improved vaccine is on the agenda in the vaccine field. There have been attempts to produce conjugate typhoid vaccines in both oral and parenteral forms. The aim of a conjugate vaccine is the production of T-cell-dependent immunity where the serum antibody response can be boosted and results in long-term immunity. Tetanus and diphtheria toxoid, cholera toxin, cholera toxin B subunit of recombinant exotoxin A of Pseudomonas aeruginosa are being tested for conjugation to Vi. An earlier Vi conjugate vaccine did not produce significant results due to the high Vi volume. Recent advances in the conjugation of Vi to a carrier protein have led to significant antibody responses in adults and children in endemic settings. A similar approach has been adopted for oral vaccines using recombinant techniques. The aim is to have a vaccine that will be single dose and will induce sufficient immunity to protect the population for life. However, to have such a vaccine seems overambitious at this moment. Both Vi conjugate vaccines, designed to be effective in infants, and new oral live vaccines, designed to be highly immunogenic in a single dose, are currently in development. A prototype Vi conjugate vaccine was found to be highly efficacious (91%) in Vietnamese toddlers for at least 4 years and serum antibody responses suggest that it can protect for at least 10 years in persons 5 years and older. Several groups are now developing Vi-diphtheria toxoid (DT) conjugate vaccines, with the goal of transferring technology to appropriate developing country producers, so that low-cost typhoid conjugate vaccines can ultimately be incorporated into the infant EPI schedule for high-risk populations. A number of improved live oral vaccines are currently in clinical trials. However, all of these newer generation typhoid vaccines are still several years away from being licensed and available on the market. The future promise of these vaccines should not preclude the more immediate use of currently available new-generation vaccines in endemic populations.
4.3 Perceived Risk of Disease and Vaccination Acceptance
Research suggests that vaccine acceptance or demand can be influenced by the perceived prevalence of the disease in the community, as well as by beliefs regarding the severity of the disease, the risk of its striking one’s household, attitudes toward vaccination in general and perceived benefits and risks of specific vaccines. Among other factors, knowledge of and experience with the disease are also important factors. Communities also exhibit a strong understanding of how common the disease is in their communities. There is a strong correlation between actual incidence and perceptions of typhoid being a “common” or “very common” disease in their community. High-risk communities also tend to have good knowledge of how to prevent typhoid fever. There has been interest from high-risk population and demand for new-generation typhoid vaccines (Table 5). The findings from socio-behavioral studies also highlight the demand for typhoid vaccine in areas where incidence of typhoid fever was not high [47, 73, 74].
4.4 The Market (Vaccine Demand and Supply)
According to preliminary estimates, the potential demand for a typhoid vaccine was calculated for 30 countries in regions considered to have high typhoid incidence (>100/100,000/year). The estimated number of doses required each year was approximately 136 million. Given that there are several high-quality producers of Vi the issue of supply of Vi vaccine does not appear to be a problem with manufacturers being able to meet an increased demand for new-generation typhoid vaccines created by their introduction into public health program in endemic countries.
In the years since the WHO recommendation, several developing country manufacturers have acquired the technology to produce Vi. This proliferation of Vi producers has been facilitated by technology transfer from the US National Institutes of Health (NIH) to several companies, the lack of patent protection, as well as the relatively simple, low-cost production process involved. Two additional developing country producers are in the process of developing Vi vaccines, in collaboration with the International Vaccine Institute and the US NIH.
4.4.1 Vaccination Strategies
The typhoid fever burden estimates are available only from few countries globally. For countries where estimates are available, data come from small-scale population-based studies or conducted as part of surveillance for vaccine trials. Therefore, the introduction of typhoid vaccines for mass immunization is questioned. A more practical approach recommended by the WHO is to consider targeted introduction of the vaccine in national vaccination programs. The policy decision for typhoid vaccine uptake is largely dependent on the perception of typhoid endemicity in the country.
The estimates of clinical protection for typhoid fever have been consistent around 70% for at least 3 years across field trials. However, there has been little evidence on the effectiveness of the vaccine until recently. Results of the indirect protection in Kolkata suggest the actual impact of the vaccine is much higher than expected.
4.4.2 Determining Endemicity
The widespread use of antimicrobials has reduced complication rates of typhoid fever. However, population studies directed by hospital estimates have shown that high rates of typhoid incidence are captured once systemic surveillance is undertaken. Population-based studies are expensive and time-consuming. Therefore, in settings where typhoid fever is expected to be found, alternative methods can be adopted to assess disease burden. A rapid assessment of outpatient hospital visits, admissions, and outcome of fever episodes can provide approximate estimates about the most affected age group, geographic location, and socio-economic classes affected. Such data can then be used for typhoid fever advocacy, guiding control strategies and in determining the target population for vaccination. In endemic settings, focusing on the high-risk groups can be a cost-effective strategy. A vaccination campaign targeting high-risk populations such as school age children, food handlers will affect transmission of the pathogen and hence circulation in the environment. Such effects can reduce the burden of disease beyond controlled efficacy results for the vaccine.
A common source of typhoid spread in a high endemicity setting is food handlers. Unhygienic food is sold without control by street vendors. Considering the prevalence of typhoid fever, the chances that these food handlers will be carriers of typhoid qualify them as a priority group for vaccination. Typhoid incidence estimates from south Asia have shown that children of school age are at highest risk. Considering that 5% of cases become carriers after being infected, school-age children will have the highest rates of transmission and close interaction of children in school and sharing of food increases the risk of spread of S. Typhi infection from an infected child to other typhoid-susceptible children. Vaccinating school-aged children will also have a greater impact in disease reduction. School-based immunization in Thailand with the killed whole-cell vaccine in the 1980s provides lesson for countries with endemic typhoid [75].
5 Population Impact
Among the two vaccines available in the market, only Vi polysaccharide vaccine has been used at large scale in countries with a high burden of typhoid fever. The introduction of the vaccine resulted in a significant reduction of typhoid fever presenting to health clinics. However, a more scientific evaluation of the effect of the vaccine has not been done that could single out Vi vaccine use as the important factor in disease reduction.
5.1 Guangxi Province, China
Typhoid fever has been endemic in many southern provinces of China. An annual incidence rate of 113/100,000 in the general population was reported in Jiangsu Province in 1988, and an average annual incidence of 53/100,000 between 1995 and 1999 in Hechi City in Guangxi Province. An immunization program using locally manufactured Vi vaccine was undertaken in these typhoid endemic areas in the 1980s. Initially the old- generation killed whole-cell vaccine and the new-generation oral live Ty21a vaccines were used. However, due to adverse events association with killed vaccine added with high cost and a difficult schedule of administration of Ty21a, the Ministry of Health switched to Vi polysaccharide vaccine in the program. Local production was a result of technology transfer to six institutes of biological products by the National Institute of Health United States.
Vi polysaccharide vaccine was introduced in the province of Guangxi in 1995; however, there are other provinces in China (provinces of Jiangsu, Hunan, Hubei, Yunnan, Guizhou, and Sichuan, and the cities of Beijing and Lanzhou) that have used Vi polysaccharide vaccine in a targeted program to reduce the burden of typhoid fever. Approximately 26 million doses of vaccine were given to school children and other high-risk groups such as food handlers. The most robust data on the impact of Vi polysaccharide vaccine on the incidence are available from the city of Guilin in Guangxi Province in southwest China from 1995 to 2006. Between 1995 and 2006, more than 1.3 million doses were administered to all target groups, peaking in 2000 and 2001. In all, 77% of the vaccine was given to students and 23% went to food handlers and residents of outbreak areas. Coverage rates have varied broadly from year to year, but have averaged 60–70% for students over the 11-year period and 80–85% for the other target groups [76].
The annual incidence of typhoid reported in the city averaged 57/100,000 in the student population and 42/100,000 in the non-student population from 1991 to 1994. Annual incidence rates of typhoid fever in Guilin from the National Notifiable Infectious Disease Reporting (NIDR) system showed the incidence declined to very low levels (0.2–4.5/100,000) in both the student and non-student population from 1995 to 2006 after vaccination [29]. Vaccine coverage ranged between 3 and 13% among the general population; between 15 and 74% among students. Approximately 3.5 million vaccines were provided to the target region in the specified period of time.
Typhoid vaccine is also recommended for use in outbreak settings in China. The recommendation is based on an effectiveness study of S. Typhi outbreak in China in 1999.
5.2 National Immunization Program, Vietnam
In 1997, the National Immunization Program (NIP), Vietnam, took the initiative of typhoid fever vaccination as a regular program. This decision was driven by the increase in the reporting of clinical typhoid fever and the rise in incidence of antibiotic resistance. Typhoid vaccination was limited to half of the 61 high incidence provinces. The vaccines were provided by the National Institute of Vaccines and Biological Substances (IVAC) to the NIP at price of approximately US $0.52 a dose. The typhoid vaccination program involved annual campaigns in which children 3–10 years of age were vaccinated with Vi polysaccharide in selected districts. Children as well as adults were vaccinated in districts with reported typhoid fever outbreaks. More than half a million doses of typhoid vaccine were given to 3- to 10-year-olds in the selected 30 provinces.
Review of the data from the NIP on the use of Vi polysaccharide vaccine in the northwestern region showed a clear decline in the incidence of typhoid fever from 97/100,000 persons per year in 1999 to less than 20/100,000 from 2006 after the introduction of Vi polysaccharide vaccine. Vaccine coverage in the general population ranged between 0.1 and 4%, but it was much higher among the targeted age group. A similar decline in the incidence of typhoid fever was seen not only from the southern Mekong delta region but also from other regions with medium typhoid incidences where Vi polysaccharide vaccine was introduced.
A meta-analysis of typhoid incidence data using prospective surveillance study results and the government’s routine disease reports suggests that a targeted immunization strategy is appropriate to reduce the number of cases. An impact and financial analysis further suggests that Vi polysaccharide vaccination in these provinces would need to be more intensive (e.g., covering all districts in a given province) and systematic than the current program in order to have a significant impact on disease incidence in the country as a whole.
5.3 Delhi State, India
The State Government of Delhi, India, funded a typhoid vaccination program for 2- to 5-year-old children with Vi polysaccharide vaccine. The program represented the first public sector typhoid vaccination program in India since 1987 when the old whole-cell vaccine was discontinued due to its reactogenicity and due to the perception that typhoid fever was not a major cause of mortality. The impetus for Vi polysaccharide vaccine introduction was the emergence of multi-drug-resistant typhoid fever among children coming to the city’s hospitals. The program targeted 2- to 5-year-old group children that are reported to be at a higher risk. The State Directorate of Family Welfare and the Delhi Municipal Corporation, which provides around 85% of the state’s government health services, ran the program. The vaccines are purchased for US $0.53 from a local producer. Since the start of the program, approximately 1 million children have been vaccinated at a rate of 300,000–325,000 children per year. A systematic evaluation of the program is not available, and it is therefore not possible to assess the impact of vaccination on the incidence of culture confirmed or clinical typhoid in the age group and on the general population [77].
5.4 Disease of Most Impoverished (DOMI) Studies in South and SouthEast Asia
Through the DOMI Program, the Vi polysaccharide vaccine was used for a series of effectiveness trials in Asia. Project sites were established in five Asian countries: Hechi, China; Kolkata, India; North Jakarta, Indonesia; Karachi, Pakistan; and Hue, Vietnam. Study sites were chosen in discussion with the local public health specialists on the basis of a high perceived burden of typhoid fever, absence of control programs against the disease, and willingness of the community to participate. The age groups selected were thought to be the likely targets for typhoid vaccination under a public health program. The projects were designed as a cluster randomized controlled effectiveness trial in all sites except for North Jakarta, which conducted a demonstration project to assess mass vaccination feasibility and safety. The project mimicked the way Vi polysaccharide vaccine might be delivered under public health conditions. In Indonesia and Vietnam, it was deemed most appropriate to target the school children at schools. In other sites, community-based vaccination was considered most appropriate. These decisions were made by the local public health experts and implemented for the projects.
Mass vaccinations were conducted in 2003 and 2004 in five sites, having more than 190,000 people vaccinated with Vi or a control agent. The program proved that very large mass vaccination campaigns are feasible and safe. The vaccination coverage in the target population was between 58 and 91%. The highest coverage rate (91%) was achieved in a school-based program in North Jakarta, Indonesia. The lowest coverage rate was observed in another school-based program in Hue, Vietnam. The community-based mass vaccination campaigns in China, India, and Pakistan had participation rates that ranged between 68 and 78%. Variations in the vaccination coverage might have been related to the different study designs [78–81].
A cluster randomized trial assessed the effectiveness of Vi polysaccharide vaccine through a cluster randomized effectiveness trial in Kolkata, India. 37,673 individuals of more than 2 years of age either received the Vi polysaccharide vaccine or the active control hepatitis A vaccine (Table 6). Protective effectiveness (PE) of Vi polysaccharide vaccine against typhoid fever was calculated to be 61% (95% CI: 41–75) 2 years after vaccination. The trial reported for the first time the Vi polysaccharide protection in children aged 2–5 years with a PE of 80% (95% CI: 53–91). The study reported no serious adverse event associated with the vaccine [82].
6 Conclusion
Typhoid fever in childhood differs significantly from clinical presentation from adults and case fatality rates are higher in children under 5 although complication rates are almost similar. There are few community-based studies that have looked specifically for typhoid fever. The global estimates of typhoid fever grossly under-report rates of complications and have no data on severity of disease and outcome. There are regional differences in presentation which may reflect differences in care-seeking patterns, health systems, and co-morbidities. Case fatality rates from sub-Saharan and North Africa were higher than Asia and those from central Asia. This may have resulted due to reporting during an outbreak period. There is no evidence that MDR typhoid is associated with consistently higher rates of complications and mortality. Recent emergence of nalidixic acid-resistant strains poses enormous challenges for developing countries with few affordable options for treating typhoid in public health settings. There is an urgent need for expanding the antibiotic pipeline for typhoid and innovative approaches including combination therapies, antibiotic cycling, and reverting to first-line therapy in sensitive cases.
Vi-PS vaccine, unless used at scale for mass vaccination, may not provide protection against typhoid among young children (under 5) in endemic areas. The last Vi-conjugate vaccine efficacy trial (with 89% protection) was over 10 years ago. There is need for alternative strategy of fast tracking Vi-conjugate vaccines in endemic areas, potentially in combination with other antigens (e.g., paratyphoid A).
References
Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ. Typhoid fever. N Engl J Med. 2002 Nov 28;347(22):1770–82.
Bhan MK, Bahl R, Bhatnagar S. Typhoid and paratyphoid fever. Lancet. 2005 Aug 27–Sep 2;366(9487):749–62.
Eberth. Oranismen in den Organen bei. Typhus abdominalis. Virchows Arch Path Anal. 1880;81:16.
Skerman VBD, McGowan V, Sneath PHA. Approved lists of bacterial names. Int J Syst Bacteriol. 1980;30:195.
Gaffky. Aetiologie des Abdominaltyphus: Mittheilungen aus dem kaiserlichen Gesundheitsante. Feischsgesundheitsamt. 1884;48.
Edwards PR, Ewing WH. Identification of Enterobacteriaceae. Minneapolis, MN: Bugess Publishing Co; 1972.
Felix A, Pitt RM. A new antigen of B. typhosus. Lancet. 1934 July 28;224(5787):6.
Wong KH, Feeley JC, Northrup RS, Forlines ME. Vi antigen from Salmonella typhosa and immunity against typhoid fever. I. Isolation and immunologic properties in animals. Infect Immun. 1974 Feb;9(2):348–53.
Mehta G, Arya SC. Capsular Vi polysaccharide antigen in Salmonella enterica serovar typhi isolates. J Clin Microbiol. 2002 Mar;40(3):1127–8.
Robbins JD, Robbins JB. Reexamination of the protective role of the capsular polysaccharide (Vi antigen) of Salmonella typhi. J Infect Dis. 1984 Sep;150(3):436–49.
Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004 May;82(5):346–53.
Ivanoff B, Levine MM, Lambert PH. Vaccination against typhoid fever: present status. Bull World Health Organ. 1994;72(6):957–71.
Crump JA, Ram PK, Gupta SK, Miller MA, Mintz ED. Part I. Analysis of data gaps pertaining to Salmonella enterica serotype typhi infections in low and medium human development index countries, 1984–2005. Epidemiol Infect. 2008 Apr;136(4):436–48.
Ochiai RL, Acosta CJ, Danovaro-Holliday MC, Baiqing D, Bhattacharya SK, Agtini MD et al. A study of typhoid fever in five Asian countries: disease burden and implications for controls. Bull World Health Organ. 2008 Apr;86(4):260–8.
DeRoeck D, Jodar L, Clemens J. Putting typhoid vaccination on the global health agenda. N Engl J Med. 2007 Sep 13;357(11):1069–71.
Brooks WA, Hossain A, Goswami D, Nahar K, Alam K, Ahmed N et al. Bacteremic typhoid fever in children in an urban slum, Bangladesh. Emerg Infect Dis. 2005 Feb;11(2):326–9.
Sinha A, Sazawal S, Kumar R, Sood S, Reddaiah VP, Singh B et al. Typhoid fever in children aged less than 5 years. Lancet. 1999 Aug 28;354(9180):734–37.
Siddiqui FJ, Rabbani F, Hasan R, Nizami SQ, Bhutta ZA. Typhoid fever in children: some epidemiological considerations from Karachi, Pakistan. Int J Infect Dis. 2006 May;10(3):215–22.
Saha SK, Baqui AH, Hanif M, Darmstadt GL, Ruhulamin M, Nagatake T et al. Typhoid fever in Bangladesh: implications for vaccination policy. Pediatr Infect Dis J. 2001 May;20(5):521–4.
Vollaard AM, Ali S, van Asten HA, Widjaja S, Visser LG, Surjadi C et al. Risk factors for typhoid and paratyphoid fever in Jakarta, Indonesia. JAMA. 2004 June 2;291(21):2607–15.
Edelman R, Levine MM. Summary of an international workshop on typhoid fever. Rev Infect Dis. 1986 May–Jun;8(3):329–49.
Maskey AP, Basnyat B, Thwaites GE, Campbell JI, Farrar JJ, Zimmerman MD. Emerging trends in enteric fever in Nepal: 9124 cases confirmed by blood culture 1993-2003. Trans R Soc Trop Med Hyg. 2008 Jan;102(1):91–5.
Uneke CJ. Concurrent malaria and typhoid fever in the tropics: the diagnostic challenges and public health implications. J Vector Borne Dis. 2008 Jun;45(2):133–42.
Butler T, Islam A, Kabir I, Jones PK. Patterns of morbidity and mortality in typhoid fever dependent on age and gender: review of 552 hospitalized patients with diarrhea. Rev Infect Dis. 1991 Jan–Feb;13(1):85–90.
Chatterjee H, Jagdish S, Pai D, Satish N, Jayadev D, Reddy PS. Changing trends in outcome of typhoid ileal perforations over three decades in Pondicherry. Trop Gastroenterol. 2001 July–Sep;22(3):155–8.
Mweu E, English M. Typhoid fever in children in Africa. Trop Med Int Health. 2008 Apr;13(4):532–40.
Thaver D, Zaidi AK, Critchley JA, Azmatullah A, Madni SA, Bhutta ZA. Fluoroquinolones for treating typhoid and paratyphoid fever (enteric fever). Cochrane Database Syst Rev. 2008;4:CD004530.
Akpede GO, Akenzua GI. Management of children with prolonged fever of unknown origin and difficulties in the management of fever of unknown origin in children in developing countries. Paediatr Drugs. 2001;3(4):247–62.
Yang J. Enteric Fever in South China: Guangxi Province. J Infect Dev Ctries. 2008;2(4):6.
Gil R, Alvarez JL, Gomez C, Alvaro A, Gil A. Epidemiology of typhoid and paratyphoid fever hospitalizations in Spain (1997-2005). Hum Vaccin. 2009 June;5(6):420–4.
Shukla S, Patel B, Chitnis DS. 100 years of Widal test & its reappraisal in an endemic area. Indian J Med Res. 1997 Feb;105:53–7.
Vallenas C, Hernandez H, Kay B, Black R, Gotuzzo E. Efficacy of bone marrow, blood, stool and duodenal contents cultures for bacteriologic confirmation of typhoid fever in children. Pediatr Infect Dis. 1985 Sep–Oct;4(5):496–8.
Bhutta ZA, Naqvi SH, Razzaq RA, Farooqui BJ. Multidrug-resistant typhoid in children: presentation and clinical features. Rev Infect Dis. 1991 Sep–Oct;13(5):832–6.
Naheed A, Ram PK, Brooks WA, Mintz ED, Hossain MA, Parsons MM et al. Clinical value of Tubex and Typhidot rapid diagnostic tests for typhoid fever in an urban community clinic in Bangladesh. Diagn Microbiol Infect Dis. 2008 Aug;61(4):381–6.
Chang JE, Hernandez H, Yi A, Chea E, Chaparro E, Matos E et al. [Hemoculture and bone marrow culture in children with typhoid fever]. Bol Med Hosp Infant Mex. 1982 Sep;39(9):614–16.
Whitaker JA, Franco-Paredes C, del Rio C, Edupuganti S. Rethinking typhoid fever vaccines: implications for travelers and people living in highly endemic areas. J Travel Med. 2009 Jan–Feb;16(1):46–52.
Tarr PE, Kuppens L, Jones TC, Ivanoff B, Aparin PG, Heymann DL. Considerations regarding mass vaccination against typhoid fever as an adjunct to sanitation and public health measures: potential use in an epidemic in Tajikistan. Am J Trop Med Hyg. 1999 Jul;61(1):163–70.
Levine MM, Lepage P. Prevention of typhoid fever. Adv Exp Med Biol. 2005;568:161–73.
Barreto ML, Genser B, Strina A, Teixeira MG, Assis AM, Rego RF et al. Effect of city-wide sanitation programme on reduction in rate of childhood diarrhoea in northeast Brazil: assessment by two cohort studies. Lancet. 2007 Nov 10;370(9599):1622–8.
Stanton BF, Clemens JD. An educational intervention for altering water-sanitation behaviors to reduce childhood diarrhea in urban Bangladesh. II. A randomized trial to assess the impact of the intervention on hygienic behaviors and rates of diarrhea. Am J Epidemiol. 1987 Feb;125(2):292–301.
Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A et al. Effect of handwashing on child health: a randomised controlled trial. Lancet. 2005 Jul 16–22;366(9481):225–33.
Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM Jr. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005 Jan;5(1):42–52.
Guzman CA, Borsutzky S, Griot-Wenk M, Metcalfe IC, Pearman J, Collioud A et al. Vaccines against typhoid fever. Vaccine. 2006 May 1;24(18):3804–11.
Griffin GE. Typhoid fever and childhood vaccine strategies. Lancet. 1999 Aug 28;354(9180):698–9.
Whittington D, Sur D, Cook J, Chatterjee S, Maskery B, Lahiri M et al. Rethinking cholera and typhoid vaccination policies for the poor: private demand in Kolkata, India. World Dev. 2009 Feb;37(2):399–409.
Do GC, Whittington D, Le TK, Utomo N, Nguyen TH, Poulos C et al. Household demand for typhoid fever vaccines in Hue, Vietnam. Health Policy Plan. 2006 May;21(3):241–55.
DeRoeck D, Clemens JD, Nyamete A, Mahoney RT. Policymakers’ views regarding the introduction of new-generation vaccines against typhoid fever, shigellosis and cholera in Asia. Vaccine. 2005 Apr 15;23(21):2762–74.
Hoffman SL, Punjabi NH, Kumala S, Moechtar MA, Pulungsih SP, Rivai AR et al. Reduction of mortality in chloramphenicol-treated severe typhoid fever by high-dose dexamethasone. N Engl J Med. 1984 Jan 12;310(2):82–8.
Gupta B, Kumar R, Khurana S. Multi drug resistant Salmonella typhi in Ludhiana (Punjab). Indian J Pathol Microbiol. 1993 Jan;36(1):5–7.
Mirza SH, Beeching NJ, Hart CA. Multi-drug resistant typhoid: a global problem. J Med Microbiol. 1996 May;44(5):317–19.
Kato Y, Fukayama M, Adachi T, Imamura A, Tsunoda T, Takayama N et al. Multidrug-resistant typhoid fever outbreak in travelers returning from Bangladesh. Emerg Infect Dis. 2007 Dec;13(12):1954–5.
Coovadia YM, Gathiram V, Bhamjee A, Garratt RM, Mlisana K, Pillay N et al. An outbreak of multiresistant Salmonella typhi in South Africa. Q J Med. 1992 Feb;82(298):91–100.
Woodward TE, Smadel JE et al. Preliminary report on the beneficial effect of chloromycetin in the treatment of typhoid fever. Ann Intern Med. 1948 Jul;29(1):131–4.
Olarte J, Galindo E. Salmonella typhi resistant to chloramphenicol, ampicillin, and other antimicrobial agents: strains isolated during an extensive typhoid fever epidemic in Mexico. Antimicrob Agents Chemother. 1973 Dec;4(6):597–601.
Bahl R, Sinha A, Poulos C, Whittington D, Sazawal S, Kumar R et al. Costs of illness due to typhoid fever in an Indian urban slum community: implications for vaccination policy. J Health Popul Nutr. 2004 Sep;22(3):304–10.
Wright AE, Leishman W. Remarks on the results which have been obtained by the antityphoid inoculations and on the methods which have been employed in the preparation of the vaccine. Br Med J. 1900;1:8.
Hawley PR, Simmons JS. The effectiveness of vaccines used for the prevention of typhoid fever in the United States army and navy. Am J Public Health Nations Health. 1934 Jul;24(7):689–709.
Frawley JM. The treatment of typhoid fever in children by means of lysed vaccine. Cal West Med. 1938 Jun;48(6):415–17.
Siler JF, Dunham GC. Duration of immunity conferred by typhoid vaccine: results of re-vaccination by intracutaneous injection of typhoid vaccine. Am J Public Health Nations Health. 1939 Feb;29(2):95–103.
Raettig H. [Indication for vaccination against typhoid fever.]. Dtsch Med Wochenschr. 1954 Jan 29;79(5):173–4.
Warren JW, Hornick RB. Immunization against typhoid fever. Ann Rev Med. 1979;30:457–72.
Levine MM, Ferreccio C, Cryz S, Ortiz E. Comparison of enteric-coated capsules and liquid formulation of Ty21a typhoid vaccine in randomised controlled field trial. Lancet. 1990 Oct 13;336(8720):891–4.
Simanjuntak CH, Paleologo FP, Punjabi NH, Darmowigoto R, Soeprawoto, Totosudirjo H et al. Oral immunisation against typhoid fever in Indonesia with Ty21a vaccine. Lancet. 1991 Oct 26;338(8774):1055–9.
Engels EA, Lau J. Vaccines for preventing typhoid fever. Cochrane Database Syst Rev. 2000;2:CD001261.
Fraser A, Paul M, Goldberg E, Acosta CJ, Leibovici L. Typhoid fever vaccines: systematic review and meta-analysis of randomised controlled trials. Vaccine. 2007 Nov 7;25(45):7848–57.
Wang JY, Noriega FR, Galen JE, Barry E, Levine MM. Constitutive expression of the Vi polysaccharide capsular antigen in attenuated Salmonella enterica serovar typhi oral vaccine strain CVD 909. Infect Immun. 2000 Aug;68(8):4647–52.
Tacket CO, Ferreccio C, Robbins JB, Tsai CM, Schulz D, Cadoz M et al. Safety and immunogenicity of two Salmonella typhi Vi capsular polysaccharide vaccines. J Infect Dis. 1986 Aug;154(2):342–5.
Acharya IL, Lowe CU, Thapa R, Gurubacharya VL, Shrestha MB, Cadoz M et al. Prevention of typhoid fever in Nepal with the Vi capsular polysaccharide of Salmonella typhi. A preliminary report. N Engl J Med. 1987 Oct 29;317(18):1101–4.
Klugman KP, Gilbertson IT, Koornhof HJ, Robbins JB, Schneerson R, Schulz D et al. Protective activity of Vi capsular polysaccharide vaccine against typhoid fever. Lancet. 1987 Nov 21;2(8569):1165–9.
Tacket CO, Levine MM, Robbins JB. Persistence of antibody titres three years after vaccination with Vi polysaccharide vaccine against typhoid fever. Vaccine. 1988 Aug;6(4):307–8.
Klugman KP, Koornhof HJ, Robbins JB, Le Cam NN. Immunogenicity, efficacy and serological correlate of protection of Salmonella typhi Vi capsular polysaccharide vaccine three years after immunization. Vaccine. 1996 Apr;14(5):435–8.
Arya SC. Efficacy of Salmonella typhi Vi capsular polysaccharide vaccine in South Africa. Vaccine. 1997 Feb;15(2):244.
Chen X, Stanton B, Pach A, Nyamete A, Ochiai RL, Kaljee L et al. Adults’ perceived prevalence of enteric fever predicts laboratory-validated incidence of typhoid fever in children. J Health Popul Nutr. 2007 Dec;25(4):469–78.
Kaljee LM, Pham V, Son ND, Hoa NT, Thiem VD, Canh do G et al. Trial participation and vaccine desirability for Vi polysaccharide typhoid fever vaccine in Hue City, Viet Nam. Trop Med Int Health. 2007 Jan;12(1):25–36.
Bodhidatta L, Taylor DN, Thisyakorn U, Echeverria P. Control of typhoid fever in Bangkok, Thailand, by annual immunization of schoolchildren with parenteral typhoid vaccine. Rev Infect Dis. 1987 Jul–Aug;9(4):841–5.
Yang HH Experience of school based vaccination in typhoid fever endemic area using Vi manufactured in China. Typhoid Fever, a Neglected Disease: Towards a Vaccine Introduction Policy, Annecy, 2–4 April 2007.
Acosta CJ, Galindo CM, Ochiai RL, Danovaro-Holliday MC, Page AL, Thiem VD et al. The role of epidemiology in the introduction of vi polysaccharide typhoid fever vaccines in Asia. J Health Popul Nutr. 2004 Sep;22(3):240–5.
Yang J, Acosta CJ, Si GA, Zeng J, Li CY, Liang DB et al. A mass vaccination campaign targeting adults and children to prevent typhoid fever in Hechi; expanding the use of Vi polysaccharide vaccine in southeast China: a cluster-randomized trial. BMC Publ Health. 2005 May;18(5):49.
Acosta CJ, Galindo CM, Ali M, Elyazeed RA, Ochiai RL, Danovaro-Holliday MC et al. A multi-country cluster randomized controlled effectiveness evaluation to accelerate the introduction of Vi polysaccharide typhoid vaccine in developing countries in Asia: rationale and design. Trop Med Int Health. 2005 Dec;10(12):1219–28.
Agtini MD, Ochiai RL, Soeharno R, Lee HJ, Sundoro J, Hadinegoro SR et al. Introducing Vi polysaccharide typhoid fever vaccine to primary school children in North Jakarta, Indonesia, via an existent school-based vaccination platform. Publ Health. 2006 Nov;120(11):1081–7.
Khan MI, Ochiai RL, Hamza HB, Sahito SM, Habib MA, Soofi SB et al. Lessons and implications from a mass immunization campaign in squatter settlements of Karachi, Pakistan: an experience from a cluster-randomized double-blinded vaccine trial [NCT00125047]. Trials. 2006;7:17.
Sur D, Ochiai RL, Bhattacharya SK, Ganguly NK, Ali M, Manna B et al. A cluster-randomized effectiveness trial of Vi typhoid vaccine in India. N Engl J Med. 2009 Jul 23;361(4):335–44.
Wahdan MH, Sérié C, Cerisier Y, Sallam S, Germanier R. A controlled field trial of live Salmonella typhi strain Ty 21a oral vaccine against typhoid: three-year results. J Infect Dis. 1982 Mar;145(3):292–5.
Levine MM, Ferreccio C, Black RE, Germanier R. Large-scale field trial of Ty21a live oral typhoid vaccine in enteric-coated capsule formulation. Lancet. 1987 May 9;1(8541):1049–52.
Black RE, Levine MM, Ferreccio C, Clements ML, Lanata C, Rooney J, Germanier R. Efficacy of one or two doses of Ty21a Salmonella typhi vaccine in enteric-coated capsules in a controlled field trial. Chilean Typhoid Committee. Vaccine. 1990 Feb;8(1):81–4.
Yang HH, Wu CG, Xie GZ, Gu QW, Wang BR, Wang LY, Wang HF, Ding ZS, Yang Y, Tan WS, Wang WY, Wang XC, Qin M, Wang JH, Tang HA, Jiang XM, Li YH, Wang ML, Zhang SL, Li GL. Efficacy trial of Vi polysaccharide vaccine against typhoid fever in south-western China. Bull World Health Organ. 2001;79(7):625–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Bhutta, Z.A., Khan, M.I., Soofi, S.B., Ochiai, R.L. (2011). New Advances in Typhoid Fever Vaccination Strategies. In: Curtis, N., Finn, A., Pollard, A. (eds) Hot Topics in Infection and Immunity in Children VII. Advances in Experimental Medicine and Biology, vol 697. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-7185-2_3
Download citation
DOI: https://doi.org/10.1007/978-1-4419-7185-2_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-7184-5
Online ISBN: 978-1-4419-7185-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)