Abstract
Typhoid fever is a severe systemic infection caused by the human-adapted Salmonella enterica serovar Typhi (S. Typhi). Paratyphoid fever is indistinguishable from typhoid fever in its clinical presentation but is associated with other typhoidal Salmonella serovars, including the human-adapted S. enterica serovars Paratyphi A, Paratyphi B, Paratyphi C, or Sendai. Although eradicated in most developed countries, these illnesses continue to be a major contributor to morbidity and mortality worldwide, and the emergence of antibiotic resistance is beginning to limit treatment options. Sanitation of drinking water is effective in reducing transmission of typhoid and paratyphoid fever, but eradication of these diseases also requires management of human carriers. Typhoidal Salmonella serovars are closely related genetically to nontyphoidal Salmonella serovars, which are associated with a localized gastroenteritis in humans. Recent studies suggest that differences in the clinical presentation of typhoid fever and gastroenteritis can be attributed to virulence mechanisms that enable typhoidal Salmonella serovars to evade innate immunity but that are absent from nontyphoidal Salmonella serovars. One such factor is the virulence capsular polysaccharide (Vi antigen) of S. Typhi and S. Paratyphi C. Studies on immunity to typhoid fever have resulted in licensing of a killed whole-cell parenteral typhoid vaccine, a live-attenuated oral typhoid vaccine, and a parenteral vaccine consisting of purified Vi antigen. Our entry will review basic and applied research on this enigmatic human disease.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
History
Typhoid fever has been an important disease throughout history. A prominent typhoid fever victim in antiquity might have been Alexander the Great, who died from a febrile illness in Babylon on June 10, 323 BC (Oldach et al. 1998). Although the disease has likely contributed to morbidity and mortality for millennia, the nonspecific symptoms make it difficult to distinguish from other illnesses based on historic accounts. The term typhous (τυφωδηος) fever, meaning smoky or hazy fever, was applied broadly since the time of Hippocrates (460 BC–ca. 370 BC) to describe continued febrile illnesses associated with delirium or stupor which likely included, but were not limited to, typhoid fever.
The first accurate account of the symptoms associated with typhoid fever is that of “putrid fever” described by the British physician Thomas Willis in 1659 (Willis 1682). However, an influential treatise on classifying diseases published in 1763 by François Boissier de Sauvages de la Croix continued to apply the term typhus broadly to continued fevers (Sauvages de la Croix 1763). Pierre Charles Alexandre Louis was the first to define typhoid fever as a distinct disease entity in 1829. He used analytical methods to differentiate François Boissier de Sauvages de la Croix’s term typhus into two distinct diseases, typhus and typhoid fever, the latter being characterized by lesions in the Peyer’s patches and mesenteric lymph nodes (Louis 1836). Subsequent work in the 1830 s by William Wood Gerhard, a disciple of Pierre Charles Alexandre Louis, helped establish the concept that typhoid fever is an independent disease entity in the United States (US). It was not until 1849, through case reports published by Sir William Jenner, that the concept of typhoid fever being distinct from typhus became accepted in the United Kingdom (Jenner 1849).
In 1856, the British physician William Budd published a pioneering epidemiological study in which he demonstrated the communicable nature of typhoid fever and its spread through contagious dejecta (Budd 1856). William Budd’s contribution was remarkable as it preceded identification of the causative agent by decades and helped erect the modern discipline of epidemiology. Furthermore, the finding that typhoid fever spreads by fecal-oral transmission led William Budd to propose water chlorination as a preventive strategy. However, this idea was initially met with skepticism by those in the medical community, who remained convinced that typhoid fever spreads through the gases rising from putrid matter (miasma) rather than by contagion (germ theory). Eventually, William Budd’s recommendations were heeded with the passing of the British Public Health Act in 1875, and this resulted in improved sanitary practices.
In 1880, the German pathologist Carl Joseph Eberth provided direct support for the theory that contagious germs cause typhoid fever by visualizing the causative agent, termed typhoid bacillus, in histological sections (Eberth 1880). In 1884, the typhoid bacillus was isolated and grown in pure culture by the German physician Georg Theodor August Gaffky, who worked under Robert Koch at the Imperial Health Office (Kaiserliches Gesundheitsamt) in Berlin (Gaffky 1884). One year after Georg Theodor August Gaffky’s characterization of the typhoid bacillus, the bacteriologist Theobald Smith isolated Bacterium cholerae-suis from a pig while working under Daniel Elmer Salmon at the Veterinary Division of the United States Department of Agriculture (USDA) (Salmon and Smith 1885). In honor of Daniel Elmer Salmon, the genus Salmonella was erected in 1900 with Salmonella cholerae-suis as the type species (Salmonella-Subcommittee 1934). In 1904, the British physician Albert Sidney Grünbaum fulfilled the last Koch’s postulates by demonstrating that experimental oral infection of chimpanzees with the typhoid bacillus produces a typhoid-like disease with the characteristic intestinal lesions (Grunbaum 1904). In 1918, the typhoid bacillus was renamed Eberthella typhi to recognize Carl Joseph Eberth’s contribution to its discovery (Buchanan 1918). In 1933, the designation Eberthella typhi was changed to Salmonella typhi (Salmonella-Subcommittee 1934). At this time, each species within the genus Salmonella was defined based on its fermentative and serological characteristics and was referred to by a Latin binomial (Kelterborn 1967). This nomenclature was eventually abandoned when it became clear that members of the genus Salmonella are closely related genetically (Crosa et al. 1973). Current nomenclature distinguishes only two species within the genus, Salmonella enterica (Le Minor and Popoff 1987) and Salmonella bongori (Reeves et al. 1989). All other former Salmonella species are now considered to be serovars (also known as serotypes). For example, the causative agent of typhoid fever is now regarded as a serovar belonging to the species S. enterica, and it is correctly referred to as S. enterica serovar Typhi (S. Typhi) (Brenner et al. 2000).
The identification of the causative agent of typhoid fever by Carl Joseph Eberth and Georg Theodor August Gaffky in the 1880s (Eberth 1880; Gaffky 1884) not only helped to fortify the concept that typhoid fever spreads by contagious germs, but it also spawned important discoveries related to diagnosis and prevention. For example, the ability to grow the organism in pure culture enabled Georges-Fernand-Isidor Widal to demonstrate in 1896 that serum from typhoid fever patients could agglutinate S. Typhi (Widal 1896). This serological test for typhoid fever was termed the Widal test and is still in use today. In the same year, bacteria isolated from two individuals with symptoms of typhoid fever that tested negative in the Widal reaction were termed Bacille paratyphique (Achard and Bensaude 1896), a pathogen now known as S. enterica serovar Paratyphi B (S. Paratyphi B).
Cultivation of S. Typhi also paved the way in 1896 for the development of the first heat-killed parenteral vaccine (Groschel and Hornick 1981), a strategy pursued in parallel by the British pathologist Sir Almroth Edward Wright at the Army Medical College in Netley (Wright 1896) and the German bacteriologist Richard Pfeiffer, who worked under Robert Koch at the Imperial Health Office in Berlin (Pfeiffer and Kolle 1896). Identification of the virulence (Vi) antigen, a capsular polysaccharide of S. Typhi, in 1934 (Felix and Pitt 1934) set the stage for the development of a purified Vi polysaccharide parenteral vaccine (Robbins and Robbins 1984). Finally, René Germanier and Emil Fürer from the Swiss Serum and Vaccine Institute introduced a third immunization strategy in 1975 by developing the first live attenuated oral typhoid vaccine strain (Ty21a) (Germanier and Fuer 1975).
In 1903, Robert Koch gave a lecture at a conference in Kassel in which he proposed the new concept that typhoid fever spreads solely through human-to-human transmission and that healthy humans that chronically shed S. Typhi could serve as a reservoir. This presentation initiated measures to improve sanitary practices in Germany and launched public health measures to identify and isolate human carriers of the disease (Drigalski 1904). These public health measures for managing carriers proved essential for eradicating typhoid fever in North America and Europe. While it was established at the time that S. Typhi is regularly present in the gallbladder (Anton and Fütterer 1888), Robert Koch’s lecture sparked renewed interest, and soon persistence in the gallbladder was proposed as a mechanism for chronic human carriage (Kelly 1906; Porster 1906). In 1906, Heinrich Kayser, who worked under Robert Koch at the Imperial Health Office in Berlin, estimated that 13.5% of typhoid fever cases could be traced to apparently healthy human carriers (Kayser 1906). Perhaps the best-known case of chronic carriage was the one identified by the American sanitary engineer George Soper. In his 1907 report, he traced an outbreak of typhoid fever in the state of New York back to a cook named Mary Mallon, better known as typhoid Mary (Soper 1907).
Before improved sanitary practices were implemented, the annual incidence of typhoid fever remained as high as 500 cases per 100,000 people in the nineteenth century in Europe and North America. The discovery by William Budd that typhoid fever is transmissible led to improved sanitation of drinking water, while identification of the causative agent by Carl Joseph Eberth and Georg Theodor August Gaffky set the stage for vaccination and the identification and isolation of human carriers. Together, these public health measures reduced the incidence of typhoid fever in Europe and North America throughout the first half of the twentieth century to their current level of less than 1 case per 100,000 people.
Taxonomy
Salmonella Species
The genus Salmonella belongs to the phylum Proteobacteria, the class Gammaproteobacteria, the order Enterobacteriales, and the family Enterobacteriaceae. The genus consists of two species, Salmonella enterica (Le Minor and Popoff 1987) and Salmonella bongori (Reeves et al. 1989). The species S. enterica is further subdivided into six subspecies, which can be referred to either by roman numerals (subspecies I, II, IIIa, IIIb, IV, and VI) or by names (subspecies enterica, salamae, arizonae, diarizonae, houtenae, and indica, respectively) (Brenner et al. 2000; Tindall et al. 2005). All Salmonella serovars that are associated with typhoid fever or paratyphoid fever in humans belong to S. enterica subspecies enterica (S. enterica subspecies I). However, the subspecies designation is commonly omitted when referring to a serovar (e.g., S. enterica serovar Typhi instead of S. enterica subspecies enterica serovar Typhi), and, in order to shorten reports, this designation is often further abbreviated (e.g., S. Typhi).
Salmonella Serovars
Each Salmonella serovar is defined by an antigen formula, which lists O factors, H1 factors, and H2 factors separated by colons (Table 17.1 ). O factors (also known as O antigens or somatic antigens) correspond to antigenic determinants present in the oligosaccharide repeat units of lipopolysaccharide (LPS). Capsule expression is uncommon in the genus Salmonella but occurs in S. Typhi and S. enterica serovar Paratyphi C, which express the Vi antigen. Expression of the Vi antigen is indicated along with O factors before the first colon in the antigen formula. H factors (H antigens) represent antigenic determinants present in flagellin, the major protein subunit of flagella. The majority of S. enterica serovars express two flagellins, termed FliC (H1 factor) and FljB (H2 factor), respectively. Flagellin expression oscillates between states characterized by exclusive production of FliC (H1-phase flagellin) and exclusive production of FljB (H2-phase flagellin), a phenomenon known as flagellar phase variation (Andrews 1922). Sequence variants of FliC and FljB proteins can be distinguished serologically, and their reactivity with typing sera is indicated in the antigen formula of a serovar. Flagellar phase variation is mediated by a heritable molecular switching mechanism composed of an invertible promoter element controlling expression of the fljBA genes (Silverman and Simon 1980). If the invertible promoter element is oriented such that it drives expression of fljBA (phase H2 orientation), the cell produces FljB (H2-phase flagellin) and FljA. In turn, FljA prevents the production of H1-phase flagellin by binding to the 5′-untranslated region of the fliC transcripts (Bonifield and Hughes 2003), thereby blocking its translation (Yamamoto and Kutsukake 2006). Phase variation requires inversion of the controlling DNA element (phase H1 orientation), thereby silencing fljBA, which relieves the translational block of fliC mRNA and allows the cell to produce H1-phase flagellin (Silverman and Simon 1980).
S. Typhi has the O antigen formula 9, 12, [Vi] : d : -, which is a numeric representation of four antigenic epitopes: O factor 9, O factor 12, the Vi antigen, and H1 factor d (Table 17.1 ). O factor 9 corresponds to a tyvelose branch that is α-(1,3)-linked to d-mannose in the trisaccharide backbone of the O antigen and represents the immunodominant epitope in the LPS of S. Typhi. O factor 12 corresponds to the trisaccharide backbone of the O antigen repeat unit consisting of α-d-mannose-(1,4)-α-l-rhamnose-(1,3)-α-d-galactose (Fig. 17.1a ). The Vi antigen is a homopolymer composed of (1,4)-2-acetamido-3-O-acetyl-2-deoxy-α-d-galacturonic acid that forms a capsular polysaccharide on the bacterial surface (Heyns and Kiessling 1967) (Fig. 17.1b ). Expression of the Vi antigen prevents agglutination of S. Typhi with serum against O factors 9 and 12 (Felix et al. 1934; Felix and Pitt 1934). The parenthesis in the antigen formula indicates that the Vi antigen is encoded on a genetically unstable DNA region that can be lost upon laboratory passage of S. Typhi (Bueno et al. 2004; Nair et al. 2004). H1 factor d indicates that the FliC protein of S. Typhi reacts with H1 typing serum d. Finally, the absence of an H2 factor (-) indicates that S. Typhi is a monophasic serovar in which the fljBA genes have been lost by deletion. An exception to the monophasic phenotype of S. Typhi has been described for some Indonesian isolates which carry a fljBA-like operon on a linear plasmid that encodes the H : z66 antigen (Huang et al. 2004; Baker et al. 2007).
O antigen, Vi capsule, and complement deposition. (a) Chemical composition of the S. Typhi O antigen repeat unit (reproduced from (Wilson et al. 2011) with permission). Free hydroxyl groups available for complement deposition are indicated in bold font. (b) Chemical composition of the Vi antigen repeat unit (reproduced from (Wilson et al. 2011) with permission). Note the absence of free hydroxyl groups in the Vi antigen. (c) Mechanism of complement deposition (opsonization). An intramolecular thioester bond within C3b reacts with free hydroxyl groups in sugar moieties of the O antigen to form an ester bond that covalently attaches complement to the bacterial surface
Typhoid fever caused by S. Typhi is indistinguishable in its symptoms from paratyphoid fever, which can be caused by S. enterica serovar Paratyphi A (S. Paratyphi A), S. Paratyphi B, S. Paratyphi C, or S. enterica serovar Sendai (S. Sendai) (Kelterborn 1967). Pathogens causing typhoid fever or paratyphoid fever are collectively referred to as typhoidal Salmonella serovars (Table 17.1 ). S. Sendai expresses O factors 9 and 12 but lacks the Vi antigen. S. Paratyphi A and S. Paratyphi B possess the same trisaccharide repeating unit, O factor 12, but differ from S. Typhi and S. Sendai in their immunodominant branching carbohydrate moieties. S. Paratyphi A has paratose α-(1,3)-linked to d-mannose (O factor 2), while the branching carbohydrate moiety of S. Paratyphi B is abequose (O factor 4). In some isolates of S. Paratyphi B, the abequose branch can be acetylated, giving rise to O factor 5. O factor 12 serves as a receptor for P22 and related bacteriophages. Lysogenic conversion by these phages can result in expression of an additional epitope, O factor 1 (Zinder 1958), which represents a glucosyl branch linked to the galactose residue in the trisaccharide repeat unit. Finally, S. Paratyphi C (O antigen formula 6, 7, Vi) expresses the Vi antigen and an O antigen with pentasaccharide repeat units that are composed of β-d-mannose-(1,2)-α-d-mannose-(1,2)-α-d-mannose-(1,2)-β-d-mannose-(1,3)-β-N-acetyl-d-glucosamine (Lindberg et al. 1988). While S. Paratyphi B, S. Paratyphi C, and S. Sendai are biphasic (i.e., expressing H1 and H2 factors), S. Paratyphi A is a monophasic serovar due to mutations in the hin and fin genes (Kutsukake et al. 2006), which encode proteins that control inversion of the fljBA promoter element (Silverman and Simon 1980). As a result, the invertible fljBA promoter element is locked in the H1 orientation in S. Paratyphi A, resulting in exclusive expression of H1-phase flagellin (McClelland et al. 2004).
Salmonella Serogroups
Salmonella serovars that express identical immunodominant O factors can be further organized into serogroups (Table 17.1 ). For example, S. Typhi and S. Sendai both express the immunodominant O factor 9 and thus belong to the same serogroup, designated D1. The majority (95.7%) of Salmonella serovars isolated from humans or food animals belong to only five serogroups, including B (O factor 4), C1 (O factor 7), C2 (O factor 8), D1 (O factor 9), and E1 (O factor 10) (Kelterborn 1967).
S. Typhi Phage Types
Phage typing is a method to distinguish different isolates of the same serovar for epidemiological purposes. The method is based on differences in the susceptibility of isolates to a set of bacteriophages (typing phages). Phage typing schemes are available for two typhoidal Salmonella serovars, S. Typhi and S. Paratyphi B (Anderson and Williams 1956; Craigie and Felix 1947). S. Typhi typing phages are derived from a bacteriophage isolated by Craige and Yen in 1938, which is specific for the Vi antigen and is termed the type II Vi phage (CRAIGIE and YEN 1938). Derivatives of the type II Vi phage can be generated by sequential adaptation to growth on specific S. Typhi host strains. An adapted phage can yield progeny that forms more plaques on the parent strain than on genetically distinct S. Typhi isolates, and the respective phage stock can thus be used as a typing phage. Differences in the infectivity of these typing phages for different S. Typhi isolates are largely based on the restriction/modification systems encoded by the S. Typhi host strain used for sequential adaptation of the respective type II Vi phage stock (Pickard et al. 2008).
Isolation and Identification
Isolation
Salmonella serovars can be isolated from stool by streaking samples on low selective agar plates containing bile salts to inhibit growth of Gram-positive bacteria (e.g., MacConkey agar or deoxycholate agar) and on intermediate-selective agar plates containing bile salts, citrate, and a low concentration of Brilliant green (0.0003 g/l) to inhibit growth of Gram-positive bacteria and most coliform bacteria (e.g., Salmonella-Shigella agar). This method is commonly used for stool samples from febrile individuals with diarrhea because it screens for two possible causes, Shigella species and Salmonella serovars.
Isolation of S. Typhi from individuals with typhoid fever is best achieved using their bone marrow cultures, followed by duodenal content cultures, while blood cultures, stool cultures, or urine cultures are less reliable (Khourieh et al. 1989; Avendano et al. 1986; Gilman et al. 1975; Gilman and Hornick 1976; Benavente et al. 1984; Hoffman et al. 1984; Farooqui et al. 1991). A combination of these methods succeeds in isolating typhoidal Salmonella serovars from more than 90% of typhoid fever patients. However, due to the discomfort associated with bone marrow aspirate cultures and duodenal string-capsule cultures, isolation frequently relies on blood cultures, which reduces sensitivity to 40–70% (Hoffman et al. 1984; Benavente et al. 1984; Gilman et al. 1975; Farooqui et al. 1991).
A medium that is highly selective for Salmonella serovars is Brilliant green agar, which contains a high concentration of Brilliant green (12.5 g/l) to inhibit growth of Gram-positive bacteria and most Gram-negative bacilli (Kauffmann 1935). However, typhoidal Salmonella serovars do not adequately grow on Brilliant green agar. The medium of choice for isolating typhoidal Salmonella serovars is bismuth sulfite agar, which contains an intermediate concentration of Brilliant green (0.025 g/l) to inhibit growth of coliforms and Gram-positive bacteria (Wilson and Blair 1927, 1931). Bismuth sulfite agar contains ferrous sulfate (FeSO4), which can be reduced to hydrogen sulfide (H2S) by proteins encoded in the phsABC operon (Heinzinger et al. 1995) and the asrABC operon (Huang and Barrett 1991) of Salmonella serovars. Hydrogen sulfide (H2S) reacts with the bismuth sulfite indicator (Bi2[SO3]3) in the medium to produce bismuth sulfide (Bi2S3), a black insoluble precipitate that produces a characteristic black to brown coloration of colonies. H2S production in typhoidal Salmonella serovars is variable and can be absent (Table 17.1 ).
Enrichment can be performed for samples containing a low number of bacteria prior to streaking samples on selective agar plates. A common enrichment method for Salmonella serovars is static growth in tetrathionate broth (Muller 1923) or in derivatives of this medium. The ttrRS ttrBAC gene cluster (Hensel et al. 1995) enables Salmonella serovars to utilize tetrathionate (S4O 2-6 ) as a terminal respiratory electron acceptor (Barrett and Clark 1987), thereby promoting their outgrowth over competing microbes in tetrathionate broth under microaerophilic conditions.
Identification
Salmonella serovars are Gram-negative, rod-shaped, and commonly peritrichously flagellated bacteria. They can be distinguished based on their biochemical properties from closely related members of the Enterobacteriaceae that can grow on selective media used for isolation of Salmonella serovars. For instance, Escherichia coli and Citrobacter species utilize lactose, a property absent in Shigella species and most Salmonella serovars. However, some serovars of S. enterica subspecies arizonae and most serovars of S. enterica subspecies diarizonae can ferment lactose and therefore form pink colonies on MacConkey agar plates, which contain lactose and a pH indicator to visualize fermentation of this carbon source. Citrobacter species and most E. coli isolates can ferment sucrose, while Salmonella serovars are negative for this reaction. Citrobacter species and Salmonella serovars can reduce ferrous sulfate (FeSO4) to hydrogen sulfide (H2S), which distinguishes them from E. coli and Shigella species.
The above biochemical properties can be assessed, for example, by using triple sugar iron (TSI) agar slants, a medium containing lactose (1%), sucrose (1%), a small amount of glucose (0.1%), ferrous sulfate (FeSO4), and the pH indicator phenol red (Russell 1911). A TSI agar slant is inoculated by streaking a pure culture over the surface, followed by stabbing the inoculum deep into the agar. An organism that can ferment lactose and/or sucrose, such as E. coli or Citrobacter species, will turn the medium yellow after incubation for 24 h. Citrobacter species produce H2S, which forms a black ferrous sulfide (FeS) precipitate in TSI agar, with yellow-colored agar remaining visible at the top of the agar slant. No black precipitate is visible with slants inoculated with Escherichia coli and Shigella species. Since Salmonella serovars only ferment the small amount of glucose present in the medium, the top of the TSI agar slant remains red while H2S production turns the agar black. It should be mentioned that H2S production can be absent in typhoidal Salmonella serovars (Table 17.1 ).
A quick test of whether a colony isolated on selective media represents a Salmonella serovar is slide agglutination with polyvalent O antiserum, which allows a rapid detection of the most common Salmonella serogroups. Salmonella serovars can then be assigned to S. bongori or to one of the subspecies of S. enterica using biochemical criteria. Most isolates belonging to S. enterica subspecies enterica can utilize tartrate as a carbon source, a property absent from S. bongori and other S. enterica subspecies. However, tartrate utilization is commonly absent in typhoidal Salmonella serovars, which are all members of S. enterica subspecies enterica (Table 17.1 ).
Traditionally, the most common method for subdividing members of the genus Salmonella is serotyping. This is still the gold standard, but the procedure is time consuming and requires the availability of a collection of typing sera. A colony isolated on selective media can be immediately typed by slide-agglutination for its O factor and its H1 factor, but not for its H2 factor, because Salmonella serovars consist predominantly of bacteria in the H1-phase after in vitro passage (Stocker 1949). Isolation of H2-phase bacteria is performed by stabbing a culture into motility agar supplemented with antiserum against its H1 factor. Since H1-phase bacteria become entrapped in the agar by antibodies, halos formed after overnight incubation consist of H2-phase bacteria, which can then be isolated to type their H2 factor.
In some cases, biochemical characterization is performed to distinguish biotypes within a serovar. For example, S. Paratyphi B isolates from patients with paratyphoid fever are generally tartrate utilization-negative, while isolates from individuals with gastroenteritis are commonly tartrate utilization-positive, and the latter biotype is referred to as S. Paratyphi B variety Java (Table 17.1 ) (Kauffmann 1955; Ezquerra et al. 1993; Malorny et al. 2003). S. Sendai isolates associated with paratyphoid fever do not produce hydrogen sulfide (H2S) and/or cannot grow on citrate, which distinguishes them from gastroenteritis isolates that share the same antigen formula but represent a different biotype classified as S. Miami (Table 17.1 ) (Edwards and Moran 1945; Chau and Huang 1979).
Epidemiology
Habitat
Humans are the only known reservoir for S. Typhi, S. Paratyphi A, S. Paratyphi C, and for biotypes of S. Sendai and S. Paratyphi B that are associated with paratyphoid fever. Individuals with active typhoid fever commonly shed the organism with their feces or urine. During convalescence, at the time of hospital discharge, approximately 20% of individuals still excrete S. Typhi (Gould and Qualls 1912). This number declines to approximately 4% of individuals who develop chronic carriage in the gallbladder or, less frequently, in the urinary bladder (Stone 1912). Chronic carriage in the gallbladder leads to intermittent release of S. Typhi into the intestine, resulting in fecal shedding. In the absence of adequate treatment, this state can persist for the remainder of an individual’s life (Gregg 1908). Contact carriers represent another important reservoir for excretion of S. Typhi. Contact carriers have no history of typhoid fever but shed S. Typhi, presumably because they developed a subclinical infection, commonly through contact with a typhoid fever patient, a condition that can arise in hospital workers (Stone 1912).
Routes of Transmission
Typhoid fever spreads by means of water, milk, and food products that become contaminated by individuals excreting S. Typhi (Stone 1912). Carriers handling water, milk, or food can introduce the contamination directly into these products. Infections can also occur remotely, as S. Typhi can survive outside its host and contaminate water supplies or spread through products distributed by trade.
Observations made during the eradication of typhoid fever in the United States illustrate the relative importance of different routes of transmission. Typhoid fever was an important cause of death in major US cities when monitoring began. Typhoid fever death rates per 100,000 people were 65 for Boston in 1865, 73 for Chicago in 1867, 62 for Baltimore in 1875, 66 for Buffalo in 1882, 42 for Providence in 1884, and 43 for New Orleans in 1895 (Putnam 1927). A crucial initial step in the eradication of typhoid fever was improved sanitation of drinking water either by filtration or by chlorination (Howard 1920; Putnam 1927; Ferrie and Troesken 2008). The incidence of typhoid fever in the USA declined following the 1870s, but records during the initial period are sparse (Ausubel et al. 2001; Putnam 1927). Concurrently with the implementation of improved drinking water sanitation, the annual typhoid fever death rates in the USA dropped from an average of 31.3 per 100,000 people in 1900 to 3.8 per 100,000 people in 1925 (Putnam 1927). These data suggest that contaminated drinking water was the most important vehicle for typhoid fever transmission in the USA at the beginning of the twentieth century.
Given that 14.5% of typhoid fever cases had a fatal outcome in the USA during the first decades of the twentieth century (Graham 1916), a death rate of 3.8 per 100,000 people reported in 1925 (Putnam 1927) suggests an incidence of approximately 26 illnesses per 100,000 people, which is more than 100-fold higher than the current annual incidence of 0.2 illnesses per 100,000 people (Scallan et al. 2011). Thus, while sanitation of drinking water markedly reduced the incidence of typhoid fever, it did not result in an eradication of the disease (Leavitt 1992). This does not suggest that drinking water was not successfully treated because the measures taken were sufficient to eradicate the water-borne disease cholera in the USA by 1911 (Weber et al. 1994). The fact that typhoid fever remained endemic in the USA, even after the broad implementation of drinking water sanitation by 1925, has been attributed to healthy human carriers (Putnam 1927; Leavitt 1992). Chronic carriage of Vibrio cholerae does not develop in individuals that recover from an episode of cholera, which made it possible to eradicate the disease solely by providing access to safe drinking water. In contrast, the eradication of typhoid fever ultimately requires the identification and management of healthy human carriers in addition to improving water sanitation.
After drinking water in the USA became safe, the discovery and control of healthy typhoid carriers became an increasingly important goal in the effort to eradicate typhoid fever. For example, starting in the second and third decades of the twentieth century, confirmed chronic typhoid carriers in New York were placed under supervision by the local or state health department, which involved quarterly visits. Chronic typhoid carriers were not permitted to engage in any occupation involving the handling of food for other than members of their own household and were not permitted to reside on farms on which cows were kept. Furthermore, contacts of chronic carriers were advised to be vaccinated against typhoid fever. Chronic carriers remained under supervision by the local or state health department for the remainder of their lives, unless the carrier state was resolved by cholecystectomy, a procedure associated with 15% mortality in the 1920s and 1930s (Senftner and Coughlin 1933). Although chloramphenicol therapy did not succeed in clearing S. Typhi carriage (Woodward et al. 1950), the advent of antibiotic therapy in the 1940s made cholecystectomy a safe procedure to cure chronic carriers (Freitag 1964). Eventually, these public health measures led to an eradication of typhoid fever in the USA by the second half of the twentieth century (Armstrong et al. 1999).
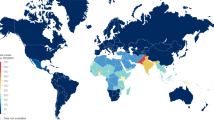
The Global Burden of Typhoid Fever
The most recent estimate suggests that 21,650,974 illnesses of typhoid fever occurred worldwide during the year 2000 (Crump et al. 2004). The incidence of typhoid fever is highest in south-central and Southeast Asia with more than 100 illnesses per 100,000 people each year. For comparison, the annual incidence in the USA at the beginning of the twentieth century was approximately 216 illnesses per 100,000 people (Putnam 1927). Typhoid fever is also endemic in the rest of Asia, Africa, Latin America, the Caribbean, and Oceania (with the exception of Australia and New Zealand) where it is responsible for between 10 and 100 illnesses per 100,000 people each year (Crump et al. 2004). For comparison, the incidence of typhoid fever in the USA was within this range in 1925, with 26 illnesses per 100,000 people, after improved sanitation of drinking water had been implemented, but before the problem of chronic carriage had been resolved (Putnam 1927). Currently, the disease is essentially eradicated in North America, Europe, and other developed countries. The Centers for Disease Control and Prevention (CDC) estimates 433 cases of typhoid fever occur each year in the USA (Scallan et al. 2011), and most of these cases can be traced back to foreign travel into endemic areas (Lynch et al. 2009).
Paratyphoid fever was responsible for an estimated 5,412,744 illnesses worldwide during the year 2000 (Crump et al. 2004). Globally, S. Paratyphi A is responsible for most episodes of paratyphoid fever. In southeast China, S. Paratyphi A has recently surpassed S. Typhi as the most common typhoidal serovar isolated from blood cultures (Ochiai et al. 2005). This might be due in part to successes in typhoid fever vaccination, which does not protect against S. Paratyphi A (Simanjuntak et al. 1991).
Using the conservative estimate of 1% for the case fatality derived from hospital-based studies and the estimate that 21,650,974 illnesses occurred worldwide in the year 2000, it has been approximated that typhoid fever was responsible for 216,510 deaths that year (Crump et al. 2004). A limitation of this estimate is that case fatality rate data from population-based studies in areas with a high incidence of the disease are lacking. A more recent meta-analysis of hospital-based studies conducted between 1984 and 2005 in Africa, Asia, Latin America, and Oceania suggests that 2% is a more realistic estimate for the current median case fatality rate of typhoid fever (Crump et al. 2008). When this more recent approximation for the case fatality rate is applied to predict the global death toll, it can be estimated that S. Typhi was responsible for 433,020 deaths in the year 2000.
Antibiotic Resistance
In 1948, chloramphenicol was identified as the first antibiotic to be effective in the treatment of typhoid fever (Woodward et al. 1948), revolutionizing management of the disease and quickly becoming the drug of choice in its treatment (Rosove et al. 1950). However, S. Typhi strains carrying plasmid-encoded resistance against chloramphenicol emerged in the early 1970s in Latin America and Asia (Anderson and Smith 1972), which led to a search for alternative drugs.
Amoxicillin/ampicillin and oral cotrimoxazole (trimethoprim/sulfamethoxazole) therapy surfaced as an effective alternative for treatment of typhoid fever in the 1960s and 1970s (Uwaydah and Shammaa 1964; Calderon 1974; Snyder et al. 1976). However, multidrug-resistant (MDR) S. Typhi strains carrying plasmid-encoded resistance to chloramphenicol, ampicillin, and trimethoprim-sulfamethoxazole appeared in the late 1980s in Asia (Anand et al. 1990). MDR S. Typhi currently comprises 7% of isolates from India, 22% of isolates from Vietnam, and 65% of isolates from Pakistan (Parry and Threlfall 2008).
In the 1980s and 1990s, new antibiotics for the treatment of MDR S. Typhi were introduced, which included extended spectrum cephalosporins (Soe and Overturf 1987; Islam et al. 1988) and fluoroquinolones (Wang et al. 1989; Dutta et al. 1993). Partial or full resistance to fluoroquinolones emerged in Vietnam in 1993 (decreased ciprofloxacin susceptible [DCS] S. Typhi), which has begun to limit treatment options (Wain et al. 1997; Chinh et al. 2000; Parry 2004). A recent survey suggests that 44% of typhoid fever isolates from Vietnam, 57% of isolates from India, and 59% of isolates from Pakistan represent DCS S. Typhi (Parry and Threlfall 2008). Current treatment recommendations for typhoid fever include the extended spectrum cephalosporin antibiotic ceftriaxone, the macrolide antibiotic azithromycin, the fluoroquinolone antibiotic gatifloxacin, and, in areas with low prevalence of plasmid-mediated resistance, chloramphenicol (Butler 2011).
Disease
Distribution of Bacteria
Typhoid fever is an infection characterized by systemic bacterial dissemination in immunocompetent individuals. Upon ingestion of contaminated food, milk, or water, S. Typhi enters the ileal mucosa at areas of Peyer’s patches. From here, the pathogen passes through the mesenteric lymph nodes and the efferent lymphatics into the blood stream, from which it disseminates to internal organs. Postmortem examination reveals S. Typhi to be present more commonly in the ileum and less frequently in the colon (Tonney et al. 1916). In the absence of antibiotic treatment, S. Typhi is isolated consistently from the Peyer’s patches, the mesenteric lymph nodes, the liver and the spleen, with great frequency from the bone marrow and the gallbladder, in about half of the cases from blood, and not commonly from the kidneys and the lungs (Horton-Smith 1900; Levy and Gaehtgens 1908). Bacteriuria occurs in approximately 22% of individuals toward the end of the disease or during convalescence, which is commonly associated with bacterial numbers high enough to turn the urine turbid (Richardson 1903; Horton-Smith 1900).
With the advent of antibiotic therapy, bacteriuria caused by S. Typhi has become rare (Mathai et al. 1995). However, S. Typhi can be isolated from rectal swab culture or stool culture in 26–37% of typhoid fever patients treated with antibiotics (Gilman et al. 1975; Hoffman et al. 1984; Benavente et al. 1984). Chronic gallbladder carriage develops in approximately 3% of patients despite antibiotic therapy (Huang and DuPont 2005; Gilman 1989).
Clinical Presentation
One striking feature of typhoid fever is that after ingestion of contaminated food, milk or water, the initial spread of S. Typhi through the Peyer’s patches and mesenteric lymph nodes into the circulation does not evoke overt host responses, as indicated by the fact that the average incubation period of the disease is 2 weeks (Olsen et al. 2003). After this incubation period, the disease presents with nonspecific symptoms, most commonly including fever and a relative slowing of the heart rate (bradycardia) (Nasrallah and Nassar 1978). Splenomegaly, hepatomegaly, or rose spots on the skin are encountered less frequently (Nasrallah and Nassar 1978). Less than half of typhoid patients present with neurological symptoms, cough, abdominal pain, or headache (Secmeer et al. 1995; Chow et al. 1989). Typhoid fever is not considered a diarrheal disease as this symptom develops in only a fraction (approximately one third) of typhoid fever patients, while the remaining individuals remain either diarrhea-free or become constipated (Chow et al. 1989; Yap and Puthucheary 1998). Paratyphoid fever is indistinguishable in its symptoms from typhoid fever but milder in its course.
Histopathology
The pathology of typhoid fever is characterized by the predominance of mononuclear phagocytes (macrophages and/or dendritic cells) and a paucity of neutrophils (Mallory 1898; Hornick et al. 1970). An exception is the accumulation of neutrophils that is occasionally seen in typhoidal meningitis, typhoidal osteomyelitis, or typhoidal pneumonia. However, neutrophils are typically scarce in typhoid fever lesions and the pathology consists of clusters of mononuclear phagocytes and lymphocytes, termed typhoid nodules, which are observed with variable frequency and size depending upon the severity of the condition (Nasrallah and Nassar 1978; Shin et al. 1994). These histopathological changes can be seen as early as 3 days after oral infection of volunteers in biopsies collected from the small intestinal mucosa, which exhibit granulomatous inflammatory lesions formed largely by mononuclear phagocytes (Sprinz et al. 1966). The characteristic swelling of the Peyer’s patches, the mesenteric lymph nodes, and the spleen during typhoid fever is due largely to the formation of mononuclear infiltrates (Mallory 1898). Mononuclear phagocytes can also be present in the urine (Pepper 1920) or in stool samples (Harris et al. 1972; Alvarado 1983).
Mononuclear phagocytes containing erythrocytes are a common finding in typhoid lesions (Shin et al. 1994; Ponfick 1872). These so-called typhoid cells represent hemophagocytic macrophages that engulf neutrophils, red blood cells, and platelets (Mallouh and Sa'di 1987). A general increase in the phagocytic activity of macrophages in the reticuloendothelial system is suggested by an increased clearance of tagged albumen particles from the blood of typhoid fever patients (Greisman et al. 1964). Hemophagocytosis is thought to be a mechanism contributing to complete blood count changes that can accompany typhoid fever, including neutropenia, anemia, and thrombocytopenia (Serefhanoglu et al. 2003; Khosla et al. 1995; Abdool Gaffar et al. 1992; Butler et al. 1978; Houston 1901).
Complications
A relapse occurs in approximately 8–10% of patients receiving no antibiotic therapy and in 15–20% of patients treated with chloramphenicol (Hornick et al. 1970). Relapses in typhoid fever represent a complete renewal of the primary disease, producing the same symptoms but commonly being of shorter duration (Horton-Smith 1900).
Intestinal perforation develops in approximately 5% of typhoid fever patients (Butler et al. 1985). Typhoid intestinal perforation is a significant cause of mortality from typhoid fever affecting both children and adults (Uba et al. 2007; Bitar and Tarpley 1985). The mononuclear cell infiltrate in ileal lymphoid tissue can be associated with fibrin deposition in capillaries, resulting in capillary thrombosis and ulceration at areas of Peyer’s patches, usually observed in the second week of fever. Continuous ulceration can produce hemorrhage and intestinal perforation associated with peritonitis, which usually occurs in the third week of fever (Bitar and Tarpley 1985). Infiltrates observed in histological studies from perforated small intestines remain mononuclear while neutrophils are scarce (Mukawi 1978; Kraus et al. 1999).
Several complications of the hepatobiliary system have been described. Typhoid nodules may coalesce to form a liver abscess or hepatic necrosis or produce typhoid hepatitis with jaundice (Durrani 1995; Nasrallah and Nassar 1978). Jaundice can also be associated with cholecystitis, which develops in some individuals (Morison 1913). Spontaneous splenic rupture has also been reported (Huang and DuPont 2005). Finally, chronic gallbladder carriage is a risk factor for developing gallbladder cancer (Caygill et al. 1995; Caygill et al. 1994; Welton et al. 1979).
Approximately 1–6% of typhoid fever patients develop pneumonia, which is commonly associated with underlying abnormalities, such as immunosuppression (Dutta et al. 2001). Other atypical manifestations include osteomyelitis, arthritis, meningitis, and cardiac abnormalities (Huang and DuPont 2005).
Differences Between Typhoid Fever and Gastroenteritis
Typhoidal Salmonella serovars are closely related genetically to nontyphoidal Salmonella serovars (Selander et al. 1990) but cause strikingly different diseases in humans (Tsolis et al. 2008). Nontyphoidal Salmonella serovars are commonly associated with gastroenteritis in immunocompetent individuals (NTS gastroenteritis), with S. enterica serovars Typhimurium and Enteritidis being isolated most frequently (Rabsch et al. 2001). NTS gastroenteritis is a typical diarrheal disease that manifests as a localized infection of the terminal ileum, mesenteric lymph nodes, and less frequently the colon. Common symptoms include, in order of frequency, diarrhea, abdominal pain, fever, headache, muscle pains, chills, and vomiting. NTS gastroenteritis has a short incubation period, which is less than 1 day on an average (Glynn and Palmer 1992). The histopathological hallmark of NTS gastroenteritis is acute intestinal inflammation with infiltrates that are dominated by neutrophils (McGovern and Slavutin 1979; Murphy and Gorbach 1982). Similarly, fecal leukocytes from NTS gastroenteritis patients are dominated by neutrophils (Harris et al. 1972; Alvarado 1983). The disease is self-limited and symptoms subside within less than 10 days after onset (Glynn and Palmer 1992). Thus, the characteristics of NTS gastroenteritis differ markedly from the clinical features of typhoid fever (Table 17.2 ).
Infections with nontyphoidal Salmonella serovars can be complicated by bacteremia in immunocompromised individuals (NTS bacteremia) (Gordon 2008; Reddy et al. 2010), a condition accompanied by neutrophilia (Saballs et al. 1993; Fleisher 1991), an antibacterial response triggered by an interleukin (IL)-1β-mediated release of neutrophils from bone marrow stores (Tewari et al. 1990). In contrast, neutrophilia does not develop during S. Typhi bacteremia. Instead, 25% of individuals with typhoid fever develop neutropenia (Khosla et al. 1995; Abdool Gaffar et al. 1992). Leukocytes in the blood respond to NTS bacteremia by mounting a respiratory burst, and the resulting production of reactive oxygen intermediates can be visualized by an increased ability of blood samples to reduce nitroblue tetrazolium (NBT) (Miller et al. 1976). In contrast, typhoid fever is associated with a negative NBT blood test, indicating a markedly reduced oxidative response in the blood of patients infected with S. Typhi (Miller et al. 1976). Collectively, these observations suggest that nontyphoidal Salmonella serovars trigger some innate antibacterial responses in the human host, which are not observed in individuals with typhoid fever.
Phylogeny and Evolution
Evolutionary History of the Genus Salmonella
The genus Salmonella is a clonal lineage, which is closely related to E. coli, Shigella species, and Citrobacter species (Fig. 17.2 ) (Petty et al. 2010). It has been estimated that the point of divergence between the genus Salmonella and the genus Escherichia was approximately 100 Ma ago (Ochman and Wilson 1987). S. bongori and the different S. enterica subspecies form a hierarchical population structure (Fig. 17.3 ) (McQuiston et al. 2008). A low rate of recombination between these lineages is inferred from sequence data of housekeeping genes, which differ between 2.8% and 4.4% of nucleotides between species and subspecies (Nelson et al. 1991; Nelson and Selander 1992; Boyd et al. 1994). It has been estimated that S. enterica diverged from S. bongori during the Eocene period between 40 and 63 Ma ago, while S. enterica subspecies enterica emerged as a separate lineage 4 to 6 Ma ago (McQuiston et al. 2008). While other lineages within the genus Salmonella are largely reptile-associated, S. enterica subspecies enterica is commonly isolated from mammals and birds, contains the largest number of serovars (Fig. 17.3 ), and is responsible for more than 99% of human clinical isolates (Aleksic et al. 1996; Bäumler 1997). Recombination within S. enterica subspecies enterica is not uncommon (Lan et al. 2009; Didelot et al. 2007; Li et al. 1994; Smith et al. 1990).
Phylogenetic connection of S. enterica and S. bongori to related species within the Enterobacteriaceae. The tree is not drawn to scale. Phylogenetic relationships are based on genome analysis (Petty et al. 2010)
The genus Salmonella. The phylogenetic tree shown on the left is not drawn to scale and is based on sequence analysis of housekeeping genes (McQuiston et al. 2008). The number of serovars present in each species and subspecies has been reported recently (Grimont and Weill 2007). The classification into species and subspecies has been reviewed previously (Brenner et al. 2000)
Evolutionary History of Typhoidal Salmonella Serovars
The vast majority of S. enterica subspecies enterica serovars are associated with gastroenteritis in humans (Aleksic et al. 1996). Within this group, typhoidal Salmonella serovars developed in four phylogenetically unrelated clonal lineages, presumably from ancestral organisms that were originally associated with gastroenteritis (Selander et al. 1990). S. Typhi isolates, S. Paratyphi C isolates, and S. Paratyphi B isolates each form one of these distinct lineages. The fourth lineage is formed by isolates of S. Paratyphi A and S. Sendai. These observations suggest that S. Sendai evolved recently from S. Paratyphi A by acquiring an rfb biosynthesis gene cluster through horizontal gene transfer that encodes an O antigen of serogroup D1 (Table 17.1 ) (Selander et al. 1990).
S. Typhi represents a clonal lineage within S. enterica subspecies enterica that likely emerged after human migrations out of Africa but before the agricultural revolution of the Neolithic age (Roumagnac et al. 2006; Kidgell et al. 2002). This scenario is supported by sequence analysis of seven housekeeping genes from different S. Typhi isolates, which indicates that the lineage is between 15,000 and 150,000 years old (Kidgell et al. 2002). A more recent single-nucleotide polymorphism (SNP) analysis of 200 S. Typhi genes suggests a similar time of origin for the most recent common ancestor of the lineage, which lived an estimated 10,000–71,000 years ago (Roumagnac et al. 2006).
Although typhoidal Salmonella serovars form four phylogenetically distant lineages, evolution of the typhoidal lifestyle may have not occurred four times independently. For instance, the viaB region encoding production of the Vi antigen is present in S. Typhi and S. Paratyphi C, suggesting that convergence by horizontal transfer of this DNA region occurred in their evolutionary history (Selander et al. 1990). Furthermore, horizontal gene transfer between S. Typhi and S. Paratyphi A/S. Sendai lineage has occurred on a scale so massive (Didelot et al. 2007) that it blurs the evolutionary relationship of their lineages (Chan et al. 2003). This large-scale recombination between the lineages of S. Typhi and S. Paratyphi A/S. Sendai occurred before the common ancestors of their contemporary clinical isolates emerged. During this phase, both lineages exchanged an astonishing 23% of their genome by horizontal gene transfer, presumably during coexistence in a shared human reservoir (Didelot et al. 2007).
It has been speculated that extensive horizontal gene transfer between S. Typhi and S. Paratyphi A might have conferred new genetic traits required for causing disseminated infections (Holt et al. 2008), and this event could thus mark the origin of typhoid and paratyphoid fever. Large-scale recombination with S. Paratyphi A occurred after the S. Typhi lineage had already passed through much (approximately 75%) of its evolutionary history (Holt et al. 2008). The clock rate and age of the S. Typhi lineage estimated by Achtman and coworkers (Roumagnac et al. 2006) would suggest that this large-scale exchange took place between 1,500 and 10,700 years ago. Typhoid fever might thus have its origin somewhere between antiquity and the agricultural revolution of the Neolithic age.
Subsequent to the large-scale recombination between S. Typhi and S. Paratyphi A, both lineages became isolated again, which was accompanied by the formation of pseudogenes at an accelerated rate, a process that is still ongoing (Holt et al. 2008). Many pseudogenes of typhoidal Salmonella serovars encode functions required for the gastrointestinal lifestyle of nontyphoidal Salmonella serovars, suggesting that the phase of isolation and accelerated pseudogene formation might represent the transition to chronic gallbladder carriage, a route of transmission that became accessible to S. Typhi after it acquired the ability to cause disseminated infections. The transition to gallbladder carriage would have made functions obsolete that are required for transmission during gastroenteritis. Inactivation of such functions through pseudogene formation might have been accelerated because the lineage passed through bottlenecks as it became host-adapted (Holt et al. 2008). Finally, the lineage diversified to give rise to all contemporary S. Typhi isolates (Roumagnac et al. 2006).
Analysis of the contemporary population structure using SNP analysis suggests that extant S. Typhi lineages arose by clonal diversification from a monophasic, antibiotic-sensitive ancestral organism (Lan et al. 2009). A relatively recently emerged clonal lineage (Lan et al. 2009) acquired a linear plasmid (Baker et al. 2007) carrying a fljBA-like operon that encodes the H:z66 antigen (Roumagnac et al. 2006; Octavia and Lan 2007). Isolates from this clonal lineage are biphasic and currently circulate in Indonesia (Huang et al. 2004). Analysis of the variation within the contemporary S. Typhi population does not reveal evidence for adaptive selection (Holt et al. 2008), with the exception of mutations in gyrA, which confer resistance to ciprofloxacin (Wain et al. 1997). Separate clonal lineages emerged in response to antibiotic selection either by acquisition of plasmid-encoded antibiotic resistance determinants or by gaining ciprofloxacin resistance through mutations in the chromosomal gyrA gene (Holt et al. 2010; Kariuki et al. 2010; Octavia and Lan 2009; Lan et al. 2009; Baker et al. 2008; Octavia and Lan 2007; Wain et al. 1997; Roumagnac et al. 2006). The absence of adaptive selection, other than that imposed by antibiotic resistance, might be explained by small population size and genetic drift, a scenario consistent with the proposed key role of chronic S. Typhi carriers as the main reservoir of this pathogen during evolution (Holt et al. 2008). Furthermore, an absence of adaptive selection suggests that S. Typhi is not under strong selective pressure from the host immune system in the niche the pathogen occupies during chronic carriage (Holt et al. 2008).
Pathogenesis and Genetics
Animal Models for Typhoid Fever
Oral inoculation of chimpanzees with S. Typhi produces an illness that closely mimics typhoid fever in its clinical course and its pathological alterations (Engelhardt 1972; Gaines et al. 1968; Edsall et al. 1960; Grunbaum 1904). However, lower primates, such as rhesus macaques, are resistant to experimental S. Typhi infection (Gaines et al. 1968; Grunbaum 1904). Similarly, nonprimate vertebrate animals generally do not show signs of infection upon ingesting S Typhi. Historically, virulence of S. Typhi has been assessed by intraperitoneal or intravenous inoculation of mice, sometimes after administration of iron (Findlay 1951; Carter and Collins 1974; Powell et al. 1980; O'Brien 1982; Furman et al. 1994), but these models have fallen out of favor because they only poorly reproduce the course of infection and pathology characteristic of typhoid fever. More recently, S. Typhi has been shown to grow in the liver and spleen of humanized mice, which represents a promising new animal model for studying aspects of typhoid fever pathogenesis (Libby et al. 2010; Song et al. 2010; Firoz Mian et al. 2011).
Analysis of its phylogenetic history suggests that S. Typhi evolved from an ancestral nontyphoidal organism associated with gastroenteritis (Selander et al. 1990). Some virulence mechanisms inherited from this ancestral organism are likely shared with nontyphoidal Salmonella serovars, such as S. Typhimurium. This assumption provides the principle rationale for using S. Typhimurium infection in the mouse as an animal model for studying S. Typhi infection in humans. Mice ingesting S. Typhimurium develop a systemic illness characterized by bacterial multiplication in the liver, spleen, mesenteric lymph nodes, and Peyer’s patches (Loeffler 1892; Müller 1912; Ørskov and Moltke 1929). This animal model has been used extensively to study the pathogenesis of typhoid fever (mouse typhoid model) (reviewed in (Tsolis et al. 1999b; Santos et al. 2001)). Work using the mouse typhoid model provides important insights into the basic pathogenic strategies deployed by nontyphoidal Salmonella serovars and into the functions of major virulence factors shared by typhoidal and nontyphoidal Salmonella serovars.
Ancestral Virulence Mechanisms Shared by Typhoidal and Nontyphoidal Salmonella Serovars
One virulence strategy conserved among typhoidal and nontyphoidal Salmonella serovars is the ability to invade the intestinal epithelium. Flagella contribute to epithelial invasion by increasing bacterial contact with host cells. Flagella-mediated motility contributes markedly to the efficiency of epithelial invasion observed in vitro for S. Typhimurium (Jones et al. 1992; Khoramian-Falsafi et al. 1990) as well as S. Typhi (Winter et al. 2009b; Liu et al. 1988). A second virulence factor required for invasion is the invasion-associated type III secretion system (T3SS-1) of S. Typhi (Elsinghorst et al. 1989) and S. Typhimurium (Galán & Curtiss 1989). The T3SS-1 apparatus is encoded by Salmonella pathogenicity island 1 (SPI1) (Mills et al. 1995), a 40-kb DNA region conserved among isolates of S. bongori and S. enterica but absent from closely related bacterial species such as E. coli (Li et al. 1995). The T3SS-1 functions as a molecular syringe that injects proteins, termed effectors, into the host cell cytosol (Fu and Galan 1998). The T3SS-1 effector proteins SipA, SipC (SspC), SopA, SopB (SigD), SopD, SopE, and SopE2 cooperate in inducing actin rearrangements in the host cell cytosol, thereby promoting bacterial entry into the epithelium (Hong and Miller 1998; Hardt et al. 1998; Hayward and Koronakis 1999; Zhou et al. 1999; Friebel et al. 2001; Jepson et al. 2001; McGhie et al. 2001; Raffatellu et al. 2005b).
A second virulence strategy shared by typhoidal and nontyphoidal Salmonella serovars is the ability to survive in macrophages. Macrophage survival of S. Typhimurium (Ochman et al. 1996) and S. Typhi (Forest et al. 2010) requires the action of a second type III secretion system (T3SS-2) encoded by SPI2. SPI2 is a DNA region that is absent from S. bongori but highly conserved within S. enterica (Ochman and Groisman 1996; Hensel et al. 1997). Acting as a molecular syringe, the T3SS-2 injects the effector proteins SpiC, SseF, SseG, SlrP, SspH1, SspH2, SifA, SifB, SseI, SseJ, PipB, PipB2, SseK1, SseK2, GogB, and SopD2 into the macrophage cytosol (reviewed in (Abrahams and Hensel 2006)). One function of the T3SS-2 is to manipulate vesicular trafficking events in macrophages (Vazquez-Torres et al. 2000; Uchiya et al. 1999; Beuzon et al. 2000), but it remains unclear in most cases how individual effector proteins contribute to T3SS-2-mediated macrophage survival. Inactivation of T3SS-2 in S. Typhimurium attenuates virulence in the mouse typhoid model 10,000-fold (Hensel et al. 1995), suggesting that this virulence factor is important in the setting of a disseminated infection.
Induction of Innate Immunity During Gastroenteritis
To cause gastroenteritis in a calf model, S. Typhimurium uses flagella and T3SS-1 to invade the intestinal mucosa and T3SS-2 to survive in tissue (Tsolis et al. 1999a, c; Schmitt et al. 2001; Zhang et al. 2002; Winter et al. 2009a). The presence of S. Typhimurium in tissue is sensed by the innate immune system through a multitude of pathways, including the detection of cytosolic access by T3SS-1 through NLRC4 (NOD-like receptor [NLR] family caspase-associated recruitment domain [CARD]-containing protein 4) (Miao et al. 2006, 2010b; Franchi et al. 2006), the activation of NLRP3 (NLR family pyrin domain-containing protein 3) by an unknown mechanism (Broz et al. 2010), the detection of cell wall fragments by nucleotide-binding oligomerization domain (NOD)1 and NOD2 (Geddes et al. 2010, 2011; Le Bourhis et al. 2009), the detection of flagellin by TLR5 (Gewirtz et al. 2001), the detection of curli amyloid fibrils through TLR1/TLR2 (Tukel et al. 2005, 2009, 2010), and the detection of the lipid A moiety of LPS by TLR4 (Vazquez-Torres et al. 2004). Finally, the O antigen moiety of LPS is detected through complement, which results in the deposition of C3b, a cleavage product of complement component 3 (C3), on the bacterial surface (Joiner et al. 1989) through covalent attachment of C3b by an ester bond formed with free hydroxyl groups in LPS sugar moieties (Sahu et al. 1994) (Fig. 17.1c ).
Detection of S. Typhimurium through these pathways triggers a cytokine storm in the intestinal mucosa that helps to orchestrate antibacterial responses, including macrophage activation, neutrophil recruitment, and the epithelial release of antimicrobials (reviewed in (Winter et al. 2010a; Santos et al. 2009)). Orchestration of these innate immune responses occurs rapidly, which explains the short incubation period of gastroenteritis (Table 17.2 ). Infected macrophages sense T3SS-mediated cytosolic access and respond by releasing S. Typhimurium through pyroptosis, which renders the pathogen vulnerable to neutrophil attack (Miao et al. 2010a). Neutrophils are important for preventing spread of the pathogen beyond the mesenteric lymph node in humans (Noriega et al. 1994; Tumbarello et al. 1995) because C3-deposition on S. Typhimurium facilitates complement receptor 3 (CR3)-mediated phagocytosis (Joiner et al. 1989), an uptake mechanism that is linked to a respiratory burst in neutrophils (Joiner et al. 1989). Eventually, the pathogen is cleared from intestinal tissues through these mechanisms without transmitting to a susceptible host, which suggests that localization in tissue represents a dead end for S. Typhimurium.
However, growth of S. Typhimurium in the intestinal lumen is enhanced during intestinal inflammation (Stecher et al. 2007; Barman et al. 2008). Neutrophils migrate into the intestinal lumen, which gives rise to fecal leukocyte populations that are dominated by neutrophils, one of the characteristic clinical features of gastroenteritis (Table 17.2 ) (Harris et al. 1972; Alvarado 1983). Neutrophil transepithelial migration promotes luminal growth of S. Typhimurium (Sekirov et al. 2010) because a by-product of the phagocyte respiratory burst is the generation in the intestine of a new respiratory electron acceptor, tetrathionate (S4O 2-6 ) (Winter et al. 2010b). Tetrathionate is a chemical long used for the enrichment of Salmonella serovars in samples containing competing microbes (Muller 1923). Growth by tetrathionate respiration in the inflamed intestine enables S. Typhimurium to outgrow competing microbes (Winter et al. 2010b) by using nutrients, such as ethanolamine, that do not support growth by fermentation (Thiennimitr et al. 2011). The resulting outgrowth of S. Typhimurium in the intestinal lumen promotes transmission of the pathogen to the next susceptible host through the fecal oral route (Lawley et al. 2008).
In conclusion, the principal virulence strategy of nontyphoidal Salmonella serovars is to use their virulence factors, flagella, T3SS-1, and T3SS-2, to attract neutrophils into the intestinal lumen, thereby gaining a luminal growth advantage that ensures their transmission (reviewed in (Santos et al. 2009)).
Evasion of Innate Immunity During Typhoid Fever
While nontyphoidal and typhoidal Salmonella serovars share flagella, T3SS-1, and T3SS-2, the former group is associated with gastroenteritis in humans while the latter group causes typhoid and paratyphoid fever (Table 17.2 ). This clinical correlation suggests that some of the genes that enable S. Typhi to cause typhoid fever in humans are not present in S. Typhimurium. It follows that the virulence mechanisms responsible for the differences between gastroenteritis and typhoid fever (Table 17.2 ) cannot be interrogated by studying S. Typhimurium infection in mice (Tsolis et al. 2011). Since the vast majority of investigators studying typhoid fever pathogenesis rely on S. Typhimurium infection in the mouse as a model, the differences between gastroenteritis and typhoid fever remain less studied than the virulence mechanisms that are shared by nontyphoidal and typhoidal Salmonella serovars.
One striking difference between gastroenteritis and typhoid fever is that the latter has a very long incubation period (Table 17.2 ), which illustrates that flagella/T3SS-1-mediated epithelial invasion and T3SS-2-mediated survival in macrophages are not accompanied by host responses severe enough to elicit symptoms within the first 2 weeks of an S. Typhi infection. Since the acute onset of intestinal inflammation that produces symptoms of gastroenteritis within less than 1 day is triggered by innate immune recognition of S. Typhimurium, the long incubation period of typhoid fever suggests that S. Typhi evades or prevents detection by the innate immune surveillance system. A DNA region involved in this process is the viaB locus of S. Typhi (Hirose et al. 1997; Sharma and Qadri 2004; Raffatellu et al. 2005a, 2007).
In addition to genes for the biosynthesis (tviBCDE) and the export (vexABCDE) of the Vi antigen, the viaB locus contains tviA, which encodes a positive regulator of capsule expression (Virlogeux et al. 1995). Expression of tviA is induced at tissue osmolarity by the two-component system EnvZ/OmpR, while high osmolarity encountered in the intestinal lumen prevents tviA expression (Fig. 17.4 ) (Winter et al. 2009b, 2010c). TviA changes gene expression by forming heterodimers with the response regulator RcsB (Virlogeux et al. 1996), a repressor of the flhDC genes (Cano et al. 2002). In turn, FlhDC acts as a positive regulator for expression of flagella and T3SS-1 invasion genes (Frye et al. 2006). As a result, S. Typhi remains invasive, motile, and noncapsulated while it resides in the high-osmolarity environment of the intestinal lumen. However, expression of TviA is induced during the transit though the intestinal epithelium, resulting in a rapid repression of flagellin and T3SS-1 expression (Winter et al. 2010c), while expression of the Vi antigen, a capsular polysaccharide, is induced (Tran et al. 2010).
TviA-mediated evasion of innate immunity. The EnvZ/OmpR two-component system activates tviA expression in response to changes in osmolarity that S. Typhi encounters when it transits from the intestinal lumen into tissue. TviA forms heterodimers with RcsB, which in turn represses flhDC expression. Through this mechanism, TviA prevents innate immune recognition of flagella and T3SS-1 through TLR5 and NLRC4. Furthermore, TviA/RcsB activates genes in the viaB locus which are involved in the biosynthesis of the Vi antigen, a surface structure preventing complement activation and recognition through TLR4
TviA regulation has two important consequences. First, some of the signals that enable the innate immune system to detect S. Typhimurium in tissue, such as cytosolic access by the T3SS-1 sensed through NLRC4 (Miao et al. 2006, 2010b; Franchi et al. 2006) and the presence of flagellin sensed through TLR5 (Gewirtz et al. 2001), are rapidly turned off by TviA when S. Typhi enters the intestinal mucosa (Fig. 17.4 ). Second, the Vi antigen is expressed when S. Typhi transits through the intestinal epithelium (Tran et al. 2010), which ensures that the pathogen is encapsulated by the time it encounters complement. Expression of the Vi antigen inhibits complement deposition (Wilson et al. 2011; Looney and Steigbigel 1986) because this capsular polysaccharide does not contain free hydroxyl groups available for ester formation with C3b (Fig. 17.1b ). The complement fragments C3a and C5a generated during complement deposition are also known as the anaphylatoxins due to their potency in inducing inflammatory responses (reviewed in (Haas and van Strijp 2007)). C5a synergizes with TLR4 to generate responses against LPS (Li et al. 2005; Riedemann et al. 2003), which might explain why expression of the Vi antigen enables S. Typhi to evade detection through TLR4 (Hirose et al. 1997; Wilson et al. 2008; Jansen et al. 2011). Thus, TviA regulation enables S. Typhi to evade detection through multiple innate immune sensors by inducing Vi antigen expression and repressing motility and T3SS-1 (Fig. 17.4 ). These innate immune evasion mechanisms contribute to the scarcity of neutrophils in lesions of typhoid fever (Jansen et al. 2011; Haneda et al. 2009; Raffatellu et al. 2007) and might help explain the long incubation period of typhoid fever (Table 17.2 ).
Inhibition of complement deposition by the Vi antigen also has consequences for the interaction of S. Typhi with neutrophils. CR3-mediated phagocytosis by neutrophils is coupled to a respiratory burst (Joiner et al. 1989). Inhibition of complement deposition by the Vi antigen prevents CR3-mediated phagocytosis (Looney and Steigbigel 1986; Wilson et al. 2011) and the generation of a respiratory burst during the interaction of S. Typhi with neutrophils (Miller et al. 1972; Kossack et al. 1981). The inhibition of a respiratory burst in neutrophils helps explain why S. Typhi bacteremia is associated with a negative NBT blood test (Miller et al. 1976). Collectively, these properties might aid S. Typhi in overcoming a neutrophil barrier and spread beyond the mesenteric lymph node to cause a disseminated infection in humans (Table 17.2 ).
Importantly, the ability to disseminate throughout the host and take residence in internal organs is a prerequisite for transmission through gallbladder carriage. Similar to Mycobacterium tuberculosis, S. Typhi is able to persist in tissue in a state of dormancy, a property that is poorly studied but likely important for developing chronic carriage. Persistence in tissue may occur in hemophagocytic macrophages, or typhoid cells (Silva-Herzog and Detweiler 2010; Nix et al. 2007), that are commonly observed in typhoid lesions (Shin et al. 1994; Ponfick 1872). Finally, persistence in the gallbladder can be accompanied by the formation of S. Typhi biofilms on the surface of gallstones (Crawford et al. 2010). Formation of these biofilms requires an O antigen capsule that is distinct from the Vi antigen (Crawford et al. 2008).
In conclusion, the principal virulence strategy of S. Typhi is based on virulence mechanisms shared with nontyphoidal Salmonella serovars. These include flagella/T3SS-1-mediated epithelial invasion and T3SS-2-mediated macrophage survival. However, while nontyphoidal Salmonella serovars stimulate innate immunity to promote their growth in the intestinal lumen, S. Typhi evades innate immunity to disseminate systemically and ensure its transmission through chronic gallbladder carriage (reviewed in (Raffatellu et al. 2006; Tsolis et al. 2008)).
Genomic Rearrangements
The gene order on the chromosomes of E. coli and S. Typhimurium is highly conserved (Riley and Anilionis 1978) and very few inversions are observed between their sequenced genomes (Rocha 2004), although both lineages diverged approximately 100 Ma ago (Ochman and Wilson 1987). This high degree of conservation suggests that the gene order may be under selection. One effect commonly associated with genome rearrangements is a lower growth rate because inversions may alter gene dosage, gene strand bias, or chromosome symmetry (Rebollo et al. 1988; Hill and Gray 1988; Campo et al. 2004). It is therefore thought that any advantage gained by multiplying at a maximum growth rate places the gene order on the chromosome under selection. In the case of S. Typhimurium, selective pressure arises from the need to transmit from an infected host to a new susceptible host (Kingsley and Bäumler 2000). Transmission requires outgrowth of competing microbes in the gut (Lawley et al. 2008), which likely necessitates multiplication at a maximum growth rate. Thus, the maximum growth rate needed for transmission of Salmonella serovars associated with gastroenteritis likely imposes selective constraints that prevent chromosomal rearrangements.
In contrast to nontyphoidal Salmonella serovars, transmission of S. Typhi no longer depends on being able to multiply at a maximum growth rate to successfully compete with other microbes residing in the intestine. Instead, transmission is likely aided by a state of dormancy or low growth rate in tissue of chronic carriers. This would suggest that selective constraints that prevent chromosomal rearrangements no longer apply to S. Typhi. Consistent with this idea, major genomic rearrangements due to homologous recombination between the rrn operons, leading to inversions and translocations, are commonly detected in genomes of S. Typhi isolates (Kothapalli et al. 2005; Liu and Sanderson 1995, 1996). Similar genome rearrangements are also common in S. Paratyphi C (Liu and Sanderson 1998). Recombination between rrn operons occurs with equal frequency in S. Typhi and S. Typhimurium in the laboratory, but S. Typhimurium strains carrying rearrangements have never been isolated from nature (Kothapalli et al. 2005). In contrast, analysis of S. Typhi isolated from human carriers over multiple years shows that chromosome rearrangements occur within the host over time (Matthews et al. 2011). The finding that gene order on the S. Typhi chromosome is not under strong selective pressure in the niche the pathogen occupies during chronic carriage supports the concept that multiplication at a maximum growth rate is not needed for transmission of typhoid fever.
Pseudogene Formation in Typhoidal Salmonella Serovars
Typhoidal serovars contain substantially more pseudogenes (genes with inactivating mutations) than their nontyphoidal relatives (Fig. 17.5 ). Indeed, this accumulation of pseudogenes in typhoidal serovars is hypothesized to be both a cause and a consequence of their human host restriction, extraintestinal tissue residence and shift in disease manifestation. This process is not unique to human typhoidal isolates, however. Genome sequencing reveals substantial pseudogene accumulation has occurred independently in a variety of systemic, host-restricted pathogens (Chiu et al. 2004; Thomson et al. 2008; McClelland et al. 2004; Liu et al. 2009; Parkhill et al. 2001; Deng et al. 2003; Jarvik et al. 2010; Holt et al. 2009). Direct gene-for-gene comparisons between S. Typhi and S. Paratyphi A have revealed the two serovars share 25 independently evolved and 44 inherited or recombined pseudogenes (Holt et al. 2009). While understanding the initial changes that lead a Salmonella strain down the path of typhoidal evolution can provide insight into host specificity and disease, every alteration in this process can be informative for the pathogenesis of both typhoidal and nontyphoidal serovars: While genes that have been inactivated in typhoidal serovars can be seen as dispensable for an extraintestinal lifestyle, these genes likely persist in nontyphoidal serovars because they aid in intestinal growth and transmission during gastroenteritis.
Chromosome statistics and type III secretion system effector gene status. Chromosomal gene and pseudogene content for typhoidal and nontyphoidal serovars is provided (** Typhimurium strain LT2). Genes encoding effector proteins secreted by T3SS-1, T3SS-2, and by both systems are represented in the table as follows: black box, intact; white box, pseudogene; and dash, absent. Human typhoidal isolates are listed in white cells while nontyphoidal isolates are listed in gray cells for comparison. Differing results from multiple isolates of a serovar are presented in respective order separated by a forward slash. For more information on these effector proteins, please consult the review by Haraga et al. (2008)
For example, S. Typhi strain CT18 contains pseudogenes in 7 of its 11 fimbrial operons of the chaperone usher assembly class (Townsend et al. 2001), which encode intestinal colonization factors (Weening et al. 2005). The shdA and misL genes encode nonfimbrial adhesins that enhance intestinal colonization of S. Typhimurium (Dorsey et al. 2005; Kingsley et al. 2000, 2002). Pseudogene formation in typhoidal serotypes led to inactivation of both shdA (S. Typhi and S. Paratyphi A) and misL (S. Typhi) (Parkhill et al. 2001; McClelland et al. 2004). Another pseudogene in S. Typhi strain CT18 is ttrS (Parkhill et al. 2001), which is required by S. Typhimurium to outgrow competing microbes in the inflamed intestine by tetrathionate respiration (Winter et al. 2010b). Tetrathionate respiration supports growth of S. Typhimurium on ethanolamine as a carbon source in the lumen of the inflamed gut (Thiennimitr et al. 2011). Growth on ethanolamine under anaerobic conditions necessitates biosynthesis of vitamin B12 by the cob/cbi gene cluster (Roof and Roth 1988), which carries pseudogenes in S. Typhi (cbiM, cbiK, cbiJ, and cbiC) (Parkhill et al. 2001) and S. Paratyphi A (cbiA) (McClelland et al. 2004). Additional pathways with shared pseudogenes in S. Typhi and S. Paratyphi A include iron uptake and chemotaxis (Holt et al. 2009). Interestingly, iron acquisition and chemotaxis are both required by S. Typhimurium to edge out competing microbes in the gut lumen during gastroenteritis (Raffatellu et al. 2009; Stecher et al. 2008). In conclusion, many of the pseudogenes found in the genomes of typhoidal Salmonella serovars encode functions that aid intestinal colonization and competition with the microbiota during gastroenteritis, which in turn enhances transmission of nontyphoidal Salmonella serovars by the fecal oral route (Lawley et al. 2008). Thus, one driving force responsible for pseudogene formation in typhoidal Salmonella serovars might be that functions required for gaining an advantage during growth competition with the resident microbiota are no longer under selection, presumably because the main route of transmission changed to chronic gallbladder carriage during evolution of the typhoidal lifestyle.
One group of genes affected by pseudogene formation in S. Typhi and S. Paratyphi A are those encoding pathogenicity-associated T3SS effector proteins. While the stable of effectors in nontyphoidal serovars can be seen as relatively constant, with each serovar differing in status between four and five loci, the typhoidal effector repertoire appears to be more plastic, differing between nine and fifteen loci (Fig. 17.5 ). This observation suggests that some T3SS effectors play a greater role in the development of gastroenteritis than they do in enabling a typhoidal lifestyle.
Vaccination
Killed Parenteral Vaccines
The first killed parenteral typhoid vaccines were developed independently by Sir Almroth Edward Wright in England and Richard Pfeiffer in Germany (Wright 1896; Pfeiffer and Kolle 1896). Killed parenteral typhoid vaccines are effective against a low-dose challenge, which might result from a waterborne exposure, but offer little protection against high-dose challenge (Ashcroft et al. 1964; Hornick and Woodward 1967). Killed parenteral vaccines have a high reactogenicity, and their use has therefore been discontinued in most countries.
Live Attenuated Oral Vaccines
René Germanier and colleagues used the mouse typhoid model to develop the first live attenuated oral typhoid vaccine strain. S. Typhimurium mutants defective for the biosynthesis of uridine-5′-diphosphate galactose epimerase (GalE) are deficient in the biosynthesis of the outer core of LPS when grown in the absence of galactose and are avirulent and immunogenic for mice (Germanier 1970, 1972). Oral vaccination with a S. Typhimurium galE mutant confers better protection in the mouse typhoid model than parenteral vaccination with a killed S. Typhimurium vaccine (Germanier 1972). Using chemical mutagenesis, a galE mutant of S. Typhi strain Ty2 was derived (Ty21a) (Germanier and Fuer 1975) and shown to be protective as live attenuated oral vaccine in field trials (Wahdan et al. 1982; Black et al. 1983, 1990).
The galE mutation is likely not the sole reason for the attenuation of Ty21a because introduction of a defined mutation in galE does not render S. Typhi strain Ty2 avirulent for humans (Hone et al. 1988). Therefore, it remains unknown which chemically induced mutations contribute to the attenuation of the vaccine strain Ty21a. Subsequent studies have demonstrated that S. Typhi strains attenuated by defined mutations in cya crp (χ3927) (Tacket et al. 1992a), cya crp cdt (χ4073) (Tacket et al. 1992a), aroC aroD (CVD908) (Tacket et al. 1992b), aroC aroD htrA (CVD908-htrA) (Tacket et al. 1997, 2000), phoPQ (Ty800) (Hohmann et al. 1996), or aroC ssaV (ZH9) (Hindle et al. 2002) are immunogenic in humans. Nonetheless, Ty21a currently remains the only available live attenuated oral typhoid vaccine.
Vi Parenteral Vaccines
Antibodies against the Vi antigen are not elicited by immunization with the live attenuated oral typhoid vaccine because the vaccine strain Ty21a carries a mutation in the viaB locus (Germanier and Furer 1983). However, antibodies against the Vi antigen are present in the serum of typhoid fever patients (Felix et al. 1935). Early studies show that parenteral administration of purified Vi antigen confers protection in mouse models (Landy and Webster 1952; Landy 1954, 1957). Subsequent reports indicated variability in the efficacy by which purified Vi antigen conferred protection against S. Typhi (Gaines et al. 1961; Hornick et al. 1966). This variability in protection has been attributed to removal of O- and N-acetyl moieties from the Vi antigen during purification (Fig. 17.1b ), which alters antigenic properties of the polysaccharide (Robbins and Robbins 1984). Purification of the Vi antigen by methods that do not remove its O- and N-acetyl moieties yields capsular polysaccharide that confers protection in animals and humans (Wong et al. 1974; Levin et al. 1975; Robbins and Robbins 1984). Vi antigen prepared by this method proofed efficacious in clinical trials (Acharya et al. 1987; Klugman et al. 1987) and is now a licensed parenteral typhoid fever vaccine (Klugman et al. 1996; Hessel et al. 1999).
Antibodies elicited by immunization with purified Vi antigen are strictly T cell independent, and the vaccine therefore does not induce increased antibody titers to a recall injection (Landy 1954). Conjugation of the Vi antigen with a recombinant, nontoxic, exotoxin A from Pseudomonas aeruginosa (rEPA) yields a vaccine that elicits T cell–dependent responses and confers superior protection in children (Thiem et al. 2011; Canh et al. 2004; Lin et al. 2001; Szu et al. 1994). These data suggest that licensing of the Vi-rEPA vaccine could improve typhoid fever vaccination in children in the future.
References
Abdool Gaffar MS, Seedat YK, Coovadia YM, Khan Q (1992) The white cell count in typhoid fever. Trop Geogr Med 44:23–27
Abrahams GL, Hensel M (2006) Manipulating cellular transport and immune responses: dynamic interactions between intracellular Salmonella enterica and its host cells. Cell Microbiol 8:728–737
Achard C, Bensaude R (1896) Infections paratyphoidiques. Bulletin et Memoires de la Societe de Medicine des Hotitaux de Paris 13:820–833
Acharya IL, Lowe CU, Thapa R, Gurubacharya VL, Shrestha MB, Cadoz M, Schulz D, Armand J, Bryla DA, Trollfors B et al (1987) Prevention of typhoid fever in Nepal with the Vi capsular polysaccharide of Salmonella typhi. A preliminary report. N Engl J Med 317:1101–1104
Aleksic S, Heinzerling F, Bockemühl J (1996) Human infection caused by salmonellae of subspecies II to VI in Germany, 1977-1992. Zentralbl Bakteriol 283:391–398
Alvarado T (1983) Faecal leucocytes in patients with infectious diarrhoea. Trans R Soc Trop Med Hyg 77:316–320
Anand AC, Kataria VK, Singh W, Chatterjee SK (1990) Epidemic multiresistant enteric fever in eastern India. Lancet 335:352
Anderson ES, Smith HR (1972) Chloramphenicol resistance in the typhoid bacillus. Br Med J 3:329–331
Anderson ES, Williams RE (1956) Bacteriophage typing of enteric pathogens and staphylococci and its use in epidemiology. J Clin Pathol 9:94–127
Andrews FW (1922) Studies in group-agglutination. I. The Salmonella group and its antigenic structure. J Pathol Bacteriol 25:515–521
Anton B, Fütterer G (1888) Untersuchungen über Typhus abdominalis. Munch Med Wochenschr 35:315–318
Armstrong GL, Conn LA, Pinner RW (1999) Trends in infectious disease mortality in the United States during the 20th century. JAMA 281:61–66
Ashcroft MT, Ritchie JM, Nicholson CC (1964) Controlled field trial in British Guiana school children of heat-killed-phenolized and acetone-killed lyophilized typhoid vaccines. Am J Hyg 79:196–206
Ausubel JH, Meyer PS, Wernick IK (2001) Death and the human environment: The United States in the 20th century. Technol Soc 23:131–146
Avendano A, Herrera P, Horwitz I, Duarte E, Prenzel I, Lanata C, Levine ML (1986) Duodenal string cultures: practicality and sensitivity for diagnosing enteric fever in children. J Infect Dis 153:359–362
Baker S, Hardy J, Sanderson KE, Quail M, Goodhead I, Kingsley RA, Parkhill J, Stocker B, Dougan G (2007) A novel linear plasmid mediates flagellar variation in Salmonella Typhi. PLoS Pathog 3:e59
Baker S, Holt K, van de Vosse E, Roumagnac P, Whitehead S, King E, Ewels P, Keniry A, Weill FX, Lightfoot D, van Dissel JT, Sanderson KE, Farrar J, Achtman M, Deloukas P, Dougan G (2008) High-throughput genotyping of Salmonella enterica serovar Typhi allowing geographical assignment of haplotypes and pathotypes within an urban District of Jakarta, Indonesia. J Clin Microbiol 46:1741–1746
Barman M, Unold D, Shifley K, Amir E, Hung K, Bos N, Salzman N (2008) Enteric salmonellosis disrupts the microbial ecology of the murine gastrointestinal tract. Infect Immun 76:907–915
Barrett EL, Clark MA (1987) Tetrathionate reduction and production of hydrogen sulfide from thiosulfate. Microbiol Rev 51:192–205
Bäumler AJ (1997) The record of horizontal gene transfer in Salmonella. Trends Microbiol 5:318–322
Benavente L, Gotuzzo E, Guerra J, Grados O, Guerra H, Bravo N (1984) Diagnosis of typhoid fever using a string capsule device. Trans R Soc Trop Med Hyg 78:404–406
Beuzon CR, Meresse S, Unsworth KE, Ruiz-Albert J, Garvis S, Waterman SR, Ryder TA, Boucrot E, Holden DW (2000) Salmonella maintains the integrity of its intracellular vacuole through the action of SifA. EMBO J 19:3235–3249
Bitar R, Tarpley J (1985) Intestinal perforation in typhoid fever: a historical and state-of-the-art review. Rev Infect Dis 7:257–271
Black R, Levine MM, Young C, Rooney J, Levine S, Clements ML, O'Donnell S, Hugues T, Germanier R (1983) Immunogenicity of Ty21a attenuated “Salmonella typhi” given with sodium bicarbonate or in enteric-coated capsules. Dev Biol Stand 53:9–14
Black RE, Levine MM, Ferreccio C, Clements ML, Lanata C, Rooney J, Germanier R (1990) Efficacy of one or two doses of Ty21a Salmonella typhi vaccine in enteric-coated capsules in a controlled field trial. Chilean Typhoid Committee. Vaccine 8:81–84
Bonifield HR, Hughes KT (2003) Flagellar phase variation in Salmonella enterica is mediated by a posttranscriptional control mechanism. J Bacteriol 185:3567–3574
Boyd EF, Nelson K, Wang FS, Whittam TS, Selander RK (1994) Molecular genetic basis of allelic polymorphism in malate dehydrogenase (mdh) in natural populations of Escherichia coli and Salmonella enterica. Proc Natl Acad Sci USA 91:1280–1284
Brenner FW, Villar RG, Angulo FJ, Tauxe R, Swaminathan B (2000) Salmonella nomenclature. J Clin Microbiol 38:2465–2467
Broz P, Newton K, Lamkanfi M, Mariathasan S, Dixit VM, Monack DM (2010) Redundant roles for inflammasome receptors NLRP3 and NLRC4 in host defense against Salmonella. J Exp Med 207:1745–1755
Buchanan RE (1918) Studies in the nomenclature and classification of the bacteria: V. Subgroups and genera of the bacteriaceae. J Bacteriol 3:27–61
Budd W (1856) The fever at the clergy orphan asylum. Lancet 68:617–619
Bueno SM, Santiviago CA, Murillo AA, Fuentes JA, Trombert AN, Rodas PI, Youderian P, Mora GC (2004) Precise excision of the large pathogenicity island, SPI7, in Salmonella enterica serovar Typhi. J Bacteriol 186:3202–3213
Butler T (2011) Treatment of typhoid fever in the 21st century: promises and shortcomings. Clin Microbiol Infect 17:959–963
Butler T, Bell WR, Levin J, Linh NN, Arnold K (1978) Typhoid fever. Studies of blood coagulation, bacteremia, and endotoxemia. Arch Intern Med 138:407–410
Butler T, Knight J, Nath SK, Speelman P, Roy SK, Azad MA (1985) Typhoid fever complicated by intestinal perforation: a persisting fatal disease requiring surgical management. Rev Infect Dis 7:244–256
Calderon E (1974) Amoxicillin in the treatment of typhoid fever due to chloramphenicol-resistance Salmonella typhi. J Infect Dis 129(suppl):S219–S221
Campo N, Dias MJ, Daveran-Mingot ML, Ritzenthaler P, Le Bourgeois P (2004) Chromosomal constraints in Gram-positive bacteria revealed by artificial inversions. Mol Microbiol 51:511–522
Canh DG, Lin FY, Thiem VD, Trach DD, Trong ND, Mao ND, Hunt S, Schneerson R, Robbins JB, Chu C, Shiloach J, Bryla DA, Bonnet MC, Schulz D, Szu SC (2004) Effect of dosage on immunogenicity of a Vi conjugate vaccine injected twice into 2- to 5-year-old Vietnamese children. Infect Immun 72:6586–6588
Cano DA, Dominguez-Bernal G, Tierrez A, Garcia-Del Portillo F, Casadesus J (2002) Regulation of capsule synthesis and cell motility in Salmonella enterica by the essential gene igaA. Genetics 162:1513–1523
Carter PB, Collins FM (1974) Growth of typhoid and paratyphoid bacilli in intravenously infected mice. Infect Immun 10:816–822
Caygill CP, Braddick M, Hill MJ, Knowles RL, Sharp JC (1995) The association between typhoid carriage, typhoid infection and subsequent cancer at a number of sites. Eur J Cancer Prev 4:187–193
Caygill CP, Hill MJ, Braddick M, Sharp JC (1994) Cancer mortality in chronic typhoid and paratyphoid carriers. Lancet 343:83–84
Chan K, Baker S, Kim CC, Detweiler CS, Dougan G, Falkow S (2003) Genomic comparison of Salmonella enterica serovars and Salmonella bongori by use of an S. enterica serovar typhimurium DNA microarray. J Bacteriol 185:553–563
Chau PY, Huang CT (1979) Biochemical characterization of H2S-positive Salmonella sendai strains isolated in Hong Kong. Microbiol Immunol 23:125–129
Chinh NT, Parry CM, Ly NT, Ha HD, Thong MX, Diep TS, Wain J, White NJ, Farrar JJ (2000) A randomized controlled comparison of azithromycin and ofloxacin for treatment of multidrug-resistant or nalidixic acid-resistant enteric fever. Antimicrob Agents Chemother 44:1855–1859
Chiu CH, Su LH, Chu C (2004) Salmonella enterica serotype Choleraesuis: epidemiology, pathogenesis, clinical disease, and treatment. Clin Microbiol Rev 17:311–322
Chow CB, Wang PS, Leung NK (1989) Typhoid fever in Hong Kong children. Aust Paediatr J 25:147–150
Craigie J, Felix A (1947) Typing of typhoid bacilli with Vi bacteriophage; suggestions for its standardisation. Lancet 1:823–827
Craigie J, Yen CE (1938) The demonstration of types of B. typhosus by means of preparations of type II Vi-phage. Can Public Health J 29:484
Crawford RW, Gibson DL, Kay WW, Gunn JS (2008) Identification of a bile-induced exopolysaccharide required for Salmonella biofilm formation on gallstone surfaces. Infect Immun 76:5341–5349
Crawford RW, Rosales-Reyes R, Ramirez-Aguilar Mde L, Chapa-Azuela O, Alpuche-Aranda C, Gunn JS (2010) Gallstones play a significant role in Salmonella spp. gallbladder colonization and carriage. Proc Natl Acad Sci USA 107:4353–4358
Crosa JH, Brenner DJ, Ewing WH, Falkow S (1973) Molecular relationship among the salmonellae. J Bacteriol 115:307–315
Crump JA, Luby SP, Mintz ED (2004) The global burden of typhoid fever. Bull World Health Organ 82:346–353
Crump JA, Ram PK, Gupta SK, Miller MA, Mintz ED (2008) Part I. Analysis of data gaps pertaining to Salmonella enterica serotype Typhi infections in low and medium human development index countries, 1984-2005. Epidemiol Infect 136:436–448
Deng W, Liou SR, Plunkett G 3rd, Mayhew GF, Rose DJ, Burland V, Kodoyianni V, Schwartz DC, Blattner FR (2003) Comparative genomics of Salmonella enterica serovar Typhi strains Ty2 and CT18. J Bacteriol 185:2330–2337
Didelot X, Achtman M, Parkhill J, Thomson NR, Falush D (2007) A bimodal pattern of relatedness between the Salmonella Paratyphi A and Typhi genomes: convergence or divergence by homologous recombination? Genome Res 17:61–68
Dorsey CW, Laarakker MC, Humphries AD, Weening EH, Bäumler AJ (2005) Salmonella enterica serotype Typhimurium MisL is an intestinal colonization factor that binds fibronectin. Mol Microbiol 57:196–211
Drigalski V (1904) Ueber Ergebnisse bei der Bekämpfung des Typhus nach Robert Koch. Zentralblatt für Bakteriologie, Parasitenkunde und Infektionskrankheiten 35:776–798
Durrani AB (1995) Typhoid hepatitis. J Pak Med Assoc 45:317–318
Dutta P, Rasaily R, Saha MR, Mitra U, Bhattacharya SK, Bhattacharya MK, Lahiri M (1993) Ciprofloxacin for treatment of severe typhoid fever in children. Antimicrob Agents Chemother 37:1197–1199
Dutta TK, Beeresha, Ghotekar LH (2001) Atypical manifestations of typhoid fever. J Postgrad Med 47:248–251
Eberth KJ (1880) Die Organismen in den Organen bei Typhus abdominalis. Virchows Arch 81:58–74
Edsall G, Gaines S, Landy M, Tigertt WD, Sprinz H, Trapani RJ, Mandel AD, Benenson AS (1960) Studies on infection and immunity in experimental typhoid fever. I. Typhoid fever in chimpanzees orally infected with Salmonella typhosa. J Exp Med 112:143–166
Edwards PR, Moran AB (1945) Salmonella cultures which resemble the Sendai type. J Bacteriol 50:257–260
Elsinghorst EA, Baron LS, Kopecko DJ (1989) Penetration of human intestinal epithelial cells by Salmonella: molecular cloning and expression of Salmonella typhi invasion determinants in Escherichia coli. Proc Natl Acad Sci USA 86:5173–5177
Engelhardt H (1972) Study on chimpanzees on the efficacy of an oral typhoid immunization with an inactivated antigen. Ann Sclavo 14:626–631
Ezquerra E, Burnens A, Jones C, Stanley J (1993) Genotypic typing and phylogenetic analysis of Salmonella paratyphi B and S. java with IS200. J Gen Microbiol 139:2409–2414
Farooqui BJ, Khurshid M, Ashfaq MK, Khan MA (1991) Comparative yield of Salmonella typhi from blood and bone marrow cultures in patients with fever of unknown origin. J Clin Pathol 44:258–259
Felix A, Bhatnagar SS, Pitt RM (1934) Observations on the properties of the Vi antigen of B. typhosus. Br J Exp Pathol 15:346–354
Felix A, Krikorian KS, Reitler R (1935) The occurrence of typhoid bacilli containing Vi antigen in cases of typhoid fever and of Vi antibody in their Sera. J Hyg (Lond) 35:421–427
Felix A, Pitt RM (1934) A new antigen of B. typhosus. Lancet 227:186–191
Ferrie JP, Troesken W (2008) Water and Chicago’s mortality transition, 1850–1925. Explorations Econ Hist 45:1–16
Findlay HT (1951) Mouse-virulence of strains of Salmonella typhi from a mild and a severe outbreak of typhoid fever. J Hyg (Lond) 49:111–113
Firoz Mian M, Pek EA, Chenoweth MJ, Ashkar AA (2011) Humanized mice are susceptible to Salmonella typhi infection. Cell Mol Immunol 8:83–87
Fleisher GR (1991) Management of children with occult bacteremia who are treated in the emergency department. Rev Infect Dis 13(Suppl 2):S156–S159
Forest CG, Ferraro E, Sabbagh SC, Daigle F (2010) Intracellular survival of Salmonella enterica serovar Typhi in human macrophages is independent of Salmonella pathogenicity island (SPI)-2. Microbiology 156:3689–3698
Franchi L, Amer A, Body-Malapel M, Kanneganti TD, Ozoren N, Jagirdar R, Inohara N, Vandenabeele P, Bertin J, Coyle A, Grant EP, Nunez G (2006) Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1beta in salmonella-infected macrophages. Nat Immunol 7:576–582
Freitag JL (1964) Treatment of chronic typhoid carriers by cholecystectomy. Public Health Rep 79:567–570
Friebel A, Ilchmann H, Aepfelbacher M, Ehrbar K, Machleidt W, Hardt WD (2001) SopE and SopE2 from Salmonella typhimurium activate different sets of RhoGTPases of the host cell. J Biol Chem 276:34035–34040
Frye J, Karlinsey JE, Felise HR, Marzolf B, Dowidar N, McClelland M, Hughes KT (2006) Identification of new flagellar genes of Salmonella enterica serovar Typhimurium. J Bacteriol 188:2233–2243
Fu Y, Galan JE (1998) The Salmonella typhimurium tyrosine phosphatase SptP is translocated into host cells and disrupts the actin cytoskeleton. Mol Microbiol 27:359–368
Furman M, Fica A, Saxena M, Di Fabio JL, Cabello FC (1994) Salmonella typhi iron uptake mutants are attenuated in mice. Infect Immun 62:4091–4094
Gaffky G (1884) Zur Ätiologie des Abdominaltyphus. Mitteilungen aus dem Kaiserlichen Gesundheitsamt 2:372–420
Gaines S, Landy M, Edsall G, Mandel AD, Trapani RJ, Benenson AS (1961) Studies on infection and immunity in experimental typhoid fever. III. Effect of prophylactic immunization. J Exp Med 114:327–342
Gaines S, Sprinz H, Tully JG, Tigertt WD (1968) Studies on infection and immunity in experimental typhoid fever. VII. The distribution of Salmonella typhi in chimpanzee tissue following oral challenge, and the relationship between the numbers of bacilli and morphologic lesions. J Infect Dis 118:293–306
Galán JE, Curtiss R III (1989) Cloning and molecular characterization of genes whose products allow Salmonella typhimurium to penetrate tissue culture cells. Proc Natl Acad Sci USA 86:6383–6387
Geddes K, Rubino S, Streutker C, Cho JH, Magalhaes JG, Le Bourhis L, Selvanantham T, Girardin SE, Philpott DJ (2010) Nod1 and Nod2 regulation of inflammation in the Salmonella colitis model. Infect Immun 78:5107–5115
Geddes K, Rubino SJ, Magalhaes JG, Streutker C, Le Bourhis L, Cho JH, Robertson SJ, Kim CJ, Kaul R, Philpott DJ, Girardin SE (2011) Identification of an innate T helper type 17 response to intestinal bacterial pathogens. Nat Med 17(7):837–844
Germanier R (1970) Immunity in experimental Salmonellosis I. Protection induced by rough mutants of Salmonella typhimurium. Infect Immun 2:309–315
Germanier R (1972) Immunity in experimental salmonellosis. 3. Comparative immunization with viable and heat-inactivated cells of Salmonella typhimurium. Infect Immun 5:792–797
Germanier R, Fuer E (1975) Isolation and characterization of Gal E mutant Ty 21a of Salmonella typhi: a candidate strain for a live, oral typhoid vaccine. J Infect Dis 131:553–558
Germanier R, Furer E (1983) Characteristics of the attenuated oral vaccine strain “S. typhi” Ty 21a. Dev Biol Stand 53:3–7
Gewirtz AT, Navas TA, Lyons S, Godowski PJ, Madara JL (2001) Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J Immunol 167:1882–1885
Gilman RH (1989) General considerations in the management of typhoid fever and dysentery. Scand J Gastroenterol Suppl 169:11–18
Gilman RH, Hornick RB (1976) Duodenal isolation of Salmonella typhi by string capsule in acute typhoid fever. J Clin Microbiol 3:456–457
Gilman RH, Terminel M, Levine MM, Hernandez-Mendoza P, Hornick RB (1975) Relative efficacy of blood, urine, rectal swab, bone-marrow, and rose-spot cultures for recovery of Salmonella typhi in typhoid fever. Lancet 1:1211–1213
Glynn JR, Palmer SR (1992) Incubation period, severity of disease, and infecting dose: evidence from a Salmonella outbreak. Am J Epidemiol 136:1369–1377
Gordon MA (2008) Salmonella infections in immunocompromised adults. J Infect 56:413–422
Gould CW, Qualls GL (1912) A study of the convalescent carriers of typhoid. JAMA 58(8):542–546
Graham E (1916) Death rate in acute infections – A study of the mortality in philadelphia during 1911-1915 from measles, pertussis, diphtheria, scarlet fever and typhoid fever. J Am Med Assoc 67:1272–1275
Gregg D (1908) A typhoid carrier fifty-two years after recovery. Boston Med Surg J 158:80
Greisman SE, Wagner HN, Iio M, Hornick RB (1964) Mechanisms of Endotoxin Tolerance. II Relationship between endotoxin tolerance and reticuloendothelial system phagocytic activity in man. J Exp Med 119:241–264
Grimont PAD, Weill F-X (2007) Antigenic formulae of the Salmonella serovars. WHO Collaborating Centre for Reference and Research on Salmonella, Paris
Groschel DH, Hornick RB (1981) Who introduced typhoid vaccination: Almroth Write or Richard Pfeiffer? Rev Infect Dis 3:1251–1254
Grunbaum AS (1904) Report LXXXIII: some experiments on enterica, scarlet fever, and measles in the chimpanzee: [A preliminary communication]. Br Med J 1:817–819
Haas PJ, van Strijp J (2007) Anaphylatoxins: their role in bacterial infection and inflammation. Immunol Res 37:161–175
Haneda T, Winter SE, Butler BP, Wilson RP, Tukel C, Winter MG, Godinez I, Tsolis RM, Baumler AJ (2009) The capsule-encoding viaB locus reduces intestinal inflammation by a Salmonella pathogenicity island 1-independent mechanism. Infect Immun 77:2932–2942
Haraga A, Ohlson MB, Miller SI (2008) Salmonellae interplay with host cells. Nat Rev Microbiol 6:53–66
Hardt WD, Chen LM, Schuebel KE, Bustelo XR, Galan JE (1998) S. typhimurium encodes an activator of Rho GTPases that induces membrane ruffling and nuclear responses in host cells. Cell 93:815–826
Harris JC, Dupont HL, Hornick RB (1972) Fecal leukocytes in diarrheal illness. Ann Intern Med 76:697–703
Hayward RD, Koronakis V (1999) Direct nucleation and bundling of actin by the SipC protein of invasive Salmonella. EMBO J 18:4926–4934
Heinzinger NK, Fujimoto SY, Clark MA, Moreno MS, Barrett EL (1995) Sequence analysis of the phs operon in Salmonella typhimurium and the contribution of thiosulfate reduction to anaerobic energy metabolism. J Bacteriol 177:2813–2820
Hensel M, Shea JE, Bäumler AJ, Gleeson C, Blattner F, Holden DW (1997) Analysis of the boundaries of Salmonella pathogenicity island 2 and the corresponding chromosomal region of Escherichia coli K-12. J Bacteriol 179:1105–1111
Hensel M, Shea JE, Gleeson C, Jones MD, Dalton E, Holden DW (1995) Simultaneous identification of bacterial virulence genes by negative selection. Science 269:400–403
Hessel L, Debois H, Fletcher M, Dumas R (1999) Experience with Salmonella typhi Vi capsular polysaccharide vaccine. Eur J Clin Microbiol Infect Dis 18:609–620
Heyns K, Kiessling G (1967) Strukturaufklarung des Vi-antigens aus Citrobacter freundii (E. coli) 5396/38. Carbohydr Res 3:340–353
Hill CW, Gray JA (1988) Effects of chromosomal inversion on cell fitness in Escherichia coli K-12. Genetics 119:771–778
Hindle Z, Chatfield SN, Phillimore J, Bentley M, Johnson J, Cosgrove CA, Ghaem-Maghami M, Sexton A, Khan M, Brennan FR, Everest P, Wu T, Pickard D, Holden DW, Dougan G, Griffin GE, House D, Santangelo JD, Khan SA, Shea JE, Feldman RG, Lewis DJ (2002) Characterization of Salmonella enterica derivatives harboring defined aroC and Salmonella pathogenicity island 2 type III secretion system (ssaV) mutations by immunization of healthy volunteers. Infect Immun 70:3457–3467
Hirose K, Ezaki T, Miyake M, Li T, Khan AQ, Kawamura Y, Yokoyama H, Takami T (1997) Survival of Vi-capsulated and Vi-deleted Salmonella typhi strains in cultured macrophage expressing different levels of CD14 antigen. FEMS Microbiol Lett 147:259–265
Hoffman SL, Punjabi NH, Rockhill RC, Sutomo A, Rivai AR, Pulungsih SP (1984) Duodenal string-capsule culture compared with bone-marrow, blood, and rectal-swab cultures for diagnosing typhoid and paratyphoid fever. J Infect Dis 149:157–161
Hohmann EL, Oletta CA, Killeen KP, Miller SI (1996) phoP/phoQ-deleted Salmonella typhi (Ty800) is a safe and immunogenic single-dose typhoid fever vaccine in volunteers. J Infect Dis 173:1408–1414
Holt KE, Baker S, Dongol S, Basnyat B, Adhikari N, Thorson S, Pulickal AS, Song Y, Parkhill J, Farrar JJ, Murdoch DR, Kelly DF, Pollard AJ, Dougan G (2010) High-throughput bacterial SNP typing identifies distinct clusters of Salmonella Typhi causing typhoid in Nepalese children. BMC Infect Dis 10:144
Holt KE, Parkhill J, Mazzoni CJ, Roumagnac P, Weill FX, Goodhead I, Rance R, Baker S, Maskell DJ, Wain J, Dolecek C, Achtman M, Dougan G (2008) High-throughput sequencing provides insights into genome variation and evolution in Salmonella Typhi. Nat Genet 40:987–993
Holt KE, Thomson NR, Wain J, Langridge GC, Hasan R, Bhutta ZA, Quail MA, Norbertczak H, Walker D, Simmonds M, White B, Bason N, Mungall K, Dougan G, Parkhill J (2009) Pseudogene accumulation in the evolutionary histories of Salmonella enterica serovars Paratyphi A and Typhi. BMC Genomics 10:36
Hone DM, Attridge SR, Forrest B, Morona R, Daniels D, LaBrooy JT, Bartholomeusz RC, Shearman DJ, Hackett J (1988) A galE via (Vi antigen-negative) mutant of Salmonella typhi Ty2 retains virulence in humans. Infect Immun 56:1326–1333
Hong KH, Miller VL (1998) Identification of a novel Salmonella invasion locus homologous to Shigella ipgDE. J Bacteriol 180:1793–1802
Hornick RB, Greisman SE, Woodward TE, DuPont HL, Dawkins AT, Snyder MJ (1970) Typhoid fever: pathogenesis and immunologic control (second of two parts). N Engl J Med 283:739–746
Hornick RB, Woodward TE (1967) Appraisal of typhoid vaccine in experimentally infected human subjects. Trans Am Clin Climatol Assoc 78:70–78
Hornick RB, Woodward TE, McCrumb FR, Snyder MJ, Dawkins AT, Bulkeley JT, De la Macorra F, Corozza FA (1966) Study of induced typhoid fever in man. I. Evaluation of vaccine effectiveness. Trans Assoc Am Physicians 79:361–367
Horton-Smith P (1900) The Goulstonian Lectures on the typhoid bacillus and typhoid fever: delivered before the Royal College of Physicians of London. Br Med J 1:827–834
Houston T (1901) On anaemia in typhoid fever. Br Med J 1:1468–1470
Howard WT (1920) The natural history of typhoid fever in Baltimore, 1851-1919. Johns Hopkins Hospital Bulletin 354:276–286
Huang CJ, Barrett EL (1991) Sequence analysis and expression of the Salmonella typhimurium asr operon encoding production of hydrogen sulfide from sulfite. J Bacteriol 173:1544–1553
Huang DB, DuPont HL (2005) Problem pathogens: extra-intestinal complications of Salmonella enterica serotype Typhi infection. Lancet Infect Dis 5:341–348
Huang X, le Phung V, Dejsirilert S, Tishyadhigama P, Li Y, Liu H, Hirose K, Kawamura Y, Ezaki T (2004) Cloning and characterization of the gene encoding the z66 antigen of Salmonella enterica serovar Typhi. FEMS Microbiol Lett 234:239–246
Islam A, Butler T, Nath SK, Alam NH, Stoeckel K, Houser HB, Smith AL (1988) Randomized treatment of patients with typhoid fever by using ceftriaxone or chloramphenicol. J Infect Dis 158:742–747
Jansen AM, Hall LJ, Clare S, Goulding D, Holt KE, Grant AJ, Mastroeni P, Dougan G, Kingsley RA (2011) A Salmonella Typhimurium-Typhi genomic chimera: a model to study VI polysaccharide capsule function in vivo. PLoS Pathog 7:e1002131
Jarvik T, Smillie C, Groisman EA, Ochman H (2010) Short-term signatures of evolutionary change in the Salmonella enterica serovar typhimurium 14028 genome. J Bacteriol 192:560–567
Jenner W (1849) Typhus and typhoid: an attempt to determine the question of their identity or non-identity by an analysis of the symptoms, and of the appearances found after death in sixty-six fatal of continued fever, observed at the London fever hospital from January 1847 to February 1849. The Edinburgh Monthly Journal of Medical Sciences 3:663, 726, 816, 954, 1095, 1264
Jepson MA, Kenny B, Leard AD (2001) Role of sipA in the early stages of Salmonella typhimurium entry into epithelial cells. Cell Microbiol 3:417–426
Joiner KA, Ganz T, Albert J, Rotrosen D (1989) The opsonizing ligand on Salmonella typhimurium influences incorporation of specific, but not azurophil, granule constituents into neutrophil phagosomes. J Cell Biol 109:2771–2782
Jones BD, Lee CA, Falkow S (1992) Invasion of Salmonella typhimurium is affected by the direction of flagellar rotation. Infect Immun 60:2475–2480
Kariuki S, Revathi G, Kiiru J, Mengo DM, Mwituria J, Muyodi J, Munyalo A, Teo YY, Holt KE, Kingsley RA, Dougan G (2010) Typhoid in Kenya is associated with a dominant multidrug-resistant Salmonella enterica serovar Typhi haplotype that is also widespread in Southeast Asia. J Clin Microbiol 48:2171–2176
Kauffmann F (1935) Weitere Erfahrungen mit dem Kombinierten Anreicherungsverfahren für Salmonellabacillen. Z Hyg Infektionskr 117:26
Kauffmann F (1955) Differential diagnosis and pathogenicity of Salmonella java and Salmonella paratyphi B. Z Hyg Infektionskr 141:546–550
Kayser H (1906) Über die Gefährlichkeit von Typhusbazillenträgern. Arb a d Kais Gesundh 24:176–180
Kelly AOJ (1906) Infections of the biliary tract, with special reference to latent (or masked) and typhoid infections. Am J Med Sci 132:446–462
Kelterborn E (1967) Salmonella-species. First isolations, names and occurrence. S. Hirzel Verlag Leipzig, Karl-Marx-Stadt
Khoramian-Falsafi T, Harayama S, Kutsukake K, Pechere JC (1990) Effect of motility and chemotaxis on the invasion of Salmonella typhimurium into HeLa cells. Microb Pathog 9:47–53
Khosla SN, Anand A, Singh U, Khosla A (1995) Haematological profile in typhoid fever. Trop Doct 25:156–158
Khourieh M, Schlesinger M, Tabachnik E, Bibi H, Armoni M, Pollak S (1989) Typhoid fever diagnosed by isolation of S. typhi from gastric aspirate. Acta Paediatr Scand 78:653–655
Kidgell C, Reichard U, Wain J, Linz B, Torpdahl M, Dougan G, Achtman M (2002) Salmonella typhi, the causative agent of typhoid fever, is approximately 50,000 years old. Infect Genet Evol 2:39–45
Kingsley RA, Bäumler AJ (2000) Host adaptation and the emergence of infectious disease: the salmonella paradigm. Mol Microbiol 36:1006–1014
Kingsley RA, Santos RL, Keestra AM, Adams LG, Bäumler AJ (2002) Salmonella enterica serotype Typhimurium ShdA is an outer membrane fibronectin-binding protein that is expressed in the intestine. Mol Microbiol 43:895–905
Kingsley RA, van Amsterdam K, Kramer N, Baumler AJ (2000) The shdA gene is restricted to serotypes of Salmonella enterica subspecies I and contributes to efficient and prolonged fecal shedding. Infect Immun 68:2720–2727
Klugman KP, Gilbertson IT, Koornhof HJ, Robbins JB, Schneerson R, Schulz D, Cadoz M, Armand J (1987) Protective activity of Vi capsular polysaccharide vaccine against typhoid fever. Lancet 2:1165–1169
Klugman KP, Koornhof HJ, Robbins JB, Le Cam NN (1996) Immunogenicity, efficacy and serological correlate of protection of Salmonella typhi Vi capsular polysaccharide vaccine three years after immunization. Vaccine 14:435–438
Kossack RE, Guerrant RL, Densen P, Schadelin J, Mandell GL (1981) Diminished neutrophil oxidative metabolism after phagocytosis of virulent Salmonella typhi. Infect Immun 31:674–678
Kothapalli S, Nair S, Alokam S, Pang T, Khakhria R, Woodward D, Johnson W, Stocker BA, Sanderson KE, Liu SL (2005) Diversity of genome structure in Salmonella enterica serovar Typhi populations. J Bacteriol 187:2638–2650
Kraus MD, Amatya B, Kimula Y (1999) Histopathology of typhoid enteritis: morphologic and immunophenotypic findings. Mod Pathol 12:949–955
Kutsukake K, Nakashima H, Tominaga A, Abo T (2006) Two DNA invertases contribute to flagellar phase variation in Salmonella enterica serovar Typhimurium strain LT2. J Bacteriol 188:950–957
Lan R, Reeves PR, Octavia S (2009) Population structure, origins and evolution of major Salmonella enterica clones. Infect Genet Evol 9:996–1005
Landy M (1954) Studies on Vi antigen. VI. Immunization of human beings with purified Vi antigen. Am J Hyg 60:52–62
Landy M (1957) Studies on Vi antigen. VII. Characteristics of the immune response in the mouse. Am J Hyg 65:81–93
Landy M, Webster ME (1952) Studies on Vi antigen. III. Immunological properties of purified Vi antigen derived from Escherichia coli 5396/38. J Immunol 69:143–154
Lawley TD, Bouley DM, Hoy YE, Gerke C, Relman DA, Monack DM (2008) Host transmission of Salmonella enterica serovar Typhimurium is controlled by virulence factors and indigenous intestinal microbiota. Infect Immun 76:403–416
Le Bourhis L, Magalhaes JG, Selvanantham T, Travassos LH, Geddes K, Fritz JH, Viala J, Tedin K, Girardin SE, Philpott DJ (2009) Role of Nod1 in mucosal dendritic cells during Salmonella pathogenicity island 1-independent Salmonella enterica serovar Typhimurium infection. Infect Immun 77:4480–4486
Le Minor L, Popoff MY (1987) Designation of Salmonella enterica sp. nov., nom. rev., as the type and only species of the geneus Salmonella. Int J Syst Bacteriol 37:465–468
Leavitt JW (1992) “Typhoid Mary” strikes back. Bacteriological theory and practice in early twentieth-century public health. Isis 83:608–629
Levin DM, Wong KH, Reynolds HY, Sutton A, Northrup RS (1975) Vi antigen from Salmonella typhosa and immunity against typhoid fever. 11. Safety and antigenicity in humans. Infect Immun 12:1290–1294
Levy E, Gaehtgens W (1908) Über die Verbreitung der Typhusbazillen in den Lymphdrüsen bei Typhusleichen. Arb Kaiserl Gesundh 28:168–171
Li J, Nelson K, McWhorter AC, Whittam TS, Selander RK (1994) Recombinational basis of serovar diversity in Salmonella enterica. Proc Natl Acad Sci USA 91:2552–2556
Li J, Ochman H, Groisman EA, Boyd EF, Solomon F, Nelson K, Selander RK (1995) Relationship between evolutionary rate and cellular location among the Inv/Spa invasion proteins of Salmonella enterica. Proc Natl Acad Sci USA 92:7252–7256
Li S, Boackle SA, Holers VM, Lambris JD, Blatteis CM (2005) Complement component c5a is integral to the febrile response of mice to lipopolysaccharide. Neuroimmunomodulation 12:67–80
Libby SJ, Brehm MA, Greiner DL, Shultz LD, McClelland M, Smith KD, Cookson BT, Karlinsey JE, Kinkel TL, Porwollik S, Canals R, Cummings LA, Fang FC (2010) Humanized nonobese diabetic-scid IL2rgammanull mice are susceptible to lethal Salmonella Typhi infection. Proc Natl Acad Sci USA 107:15589–15594
Lin FY, Ho VA, Khiem HB, Trach DD, Bay PV, Thanh TC, Kossaczka Z, Bryla DA, Shiloach J, Robbins JB, Schneerson R, Szu SC (2001) The efficacy of a Salmonella typhi Vi conjugate vaccine in two-to-five-year-old children. N Engl J Med 344:1263–1269
Lindberg B, Leontein K, Lindquist U, Svenson SB, Wrangsell G, Dell A, Rogers M (1988) Structural studies of the O-antigen polysaccharide of Salmonella thompson, serogroup C1 (6,7). Carbohydr Res 174:313–322
Liu SL, Ezaki T, Miura H, Matsui K, Yabuuchi E (1988) Intact motility as a Salmonella typhi invasion-related factor. Infect Immun 56:1967–1973
Liu SL, Sanderson KE (1995) Rearrangements in the genome of the bacterium Salmonella typhi. Proc Natl Acad Sci USA 92:1018–1022
Liu SL, Sanderson KE (1996) Highly plastic chromosomal organization in Salmonella typhi. Proc Natl Acad Sci USA 93:10303–10308
Liu SL, Sanderson KE (1998) Homologous recombination between rrn operons rearranges the chromosome in host-specialized species of Salmonella. FEMS Microbiol Lett 164:275–281
Liu WQ, Feng Y, Wang Y, Zou QH, Chen F, Guo JT, Peng YH, Jin Y, Li YG, Hu SN, Johnston RN, Liu GR, Liu SL (2009) Salmonella paratyphi C: genetic divergence from Salmonella choleraesuis and pathogenic convergence with Salmonella typhi. PLoS One 4:e4510
Loeffler F (1892) Ueber Epidemieen unter den im hygienishcen Institute zu Greifswald gehaltenen Mäusen und über die Bekämpfung der Feldmausplage. Zbl Bakt Parasitenkunde 11:129–141
Looney RJ, Steigbigel RT (1986) Role of the Vi antigen of Salmonella typhi in resistance to host defense in vitro. J Lab Clin Med 108:506–516
Louis PCA (1836) Anatomical, pathological and therapeutic researches upon the disease known under the name of gastro-enterite putrid, adynamic, ataxic, or typhoid fever, etc.; Compared with the most common acute diseases. Issac R. Butts, Boston
Lynch MF, Blanton EM, Bulens S, Polyak C, Vojdani J, Stevenson J, Medalla F, Barzilay E, Joyce K, Barrett T, Mintz ED (2009) Typhoid fever in the United States, 1999-2006. JAMA 302:859–865
Mallory FB (1898) A histological study of typhoid fever. J Exp Med 3:611–638
Mallouh AA, Sa'di AR (1987) White blood cells and bone marrow in typhoid fever. Pediatr Infect Dis J 6:527–529
Malorny B, Bunge C, Helmuth R (2003) Discrimination of d-tartrate-fermenting and -nonfermenting Salmonella enterica subsp. enterica isolates by genotypic and phenotypic methods. J Clin Microbiol 41:4292–4297
Mathai E, John TJ, Rani M, Mathai D, Chacko N, Nath V, Cherian AM (1995) Significance of Salmonella typhi bacteriuria. J Clin Microbiol 33:1791–1792
Matthews TD, Rabsch W, Maloy S (2011) Chromosomal rearrangements in Salmonella enterica Serovar Typhi Strains Isolated from Asymptomatic Human Carriers. MBio 2(3):e00060
McClelland M, Sanderson KE, Clifton SW, Latreille P, Porwollik S, Sabo A, Meyer R, Bieri T, Ozersky P, McLellan M, Harkins CR, Wang C, Nguyen C, Berghoff A, Elliott G, Kohlberg S, Strong C, Du F, Carter J, Kremizki C, Layman D, Leonard S, Sun H, Fulton L, Nash W, Miner T, Minx P, Delehaunty K, Fronick C, Magrini V, Nhan M, Warren W, Florea L, Spieth J, Wilson RK (2004) Comparison of genome degradation in Paratyphi A and Typhi, human-restricted serovars of Salmonella enterica that cause typhoid. Nat Genet 36:1268–1274
McGhie EJ, Hayward RD, Koronakis V (2001) Cooperation between actin-binding proteins of invasive Salmonella: SipA potentiates SipC nucleation and bundling of actin. EMBO J 20:2131–2139
McGovern VJ, Slavutin LJ (1979) Pathology of salmonella colitis. Am J Surg Pathol 3:483–490
McQuiston JR, Herrera-Leon S, Wertheim BC, Doyle J, Fields PI, Tauxe RV, Logsdon JM Jr (2008) Molecular phylogeny of the salmonellae: relationships among Salmonella species and subspecies determined from four housekeeping genes and evidence of lateral gene transfer events. J Bacteriol 190:7060–7067
Miao EA, Alpuche-Aranda CM, Dors M, Clark AE, Bader MW, Miller SI, Aderem A (2006) Cytoplasmic flagellin activates caspase-1 and secretion of interleukin 1beta via Ipaf. Nat Immunol 7:569–575
Miao EA, Leaf IA, Treuting PM, Mao DP, Dors M, Sarkar A, Warren SE, Wewers MD, Aderem A (2010a) Caspase-1-induced pyroptosis is an innate immune effector mechanism against intracellular bacteria. Nat Immunol 11(12):1136–1142
Miao EA, Mao DP, Yudkovsky N, Bonneau R, Lorang CG, Warren SE, Leaf IA, Aderem A (2010b) Innate immune detection of the type III secretion apparatus through the NLRC4 inflammasome. Proc Natl Acad Sci USA 107:3076–3080
Miller RM, Garbus J, Hornick RB (1972) Lack of enhanced oxygen consumption by polymorphonuclear leukocytes on phagocytosis of virulent Salmonella typhi. Science 175:1010–1011
Miller RM, Garbus J, Schwartz AR, DuPont HL, Levine MM, Clyde DF, Hornick RB (1976) A modified leukocyte nitroblue tetrazolium test in acute bacterial infection. Am J Clin Pathol 66:905–910
Mills DM, Bajaj V, Lee CA (1995) A 40 kb chromosomal fragment encoding Salmonella typhimurium invasion genes is absent from the corresponding region of the Escherichia coli K-12 chromosome. Mol Microbiol 15:749–759
Morison AE (1913) Typhoid cholecystitis. Br Med J 2:1578–1579
Mukawi TJ (1978) Histopathological study of typhoid perforation of the small intestines. Southeast Asian J Trop Med Public Health 9:252–255
Muller L (1923) Un nouveau milieu d'enrichissement pour la recherche du Bacille Typhique at Paratyphique. Comptes Rendus des Seances de la Societe de Biologie et de ses Filiales 89:434–437
Müller M (1912) Der Nachweis von Fleischvergiftungsbakterien in Fleisch und Organen von Schlachttieren auf Grund Systematischer Untersuchungen über den Verlauf und den Mechanismus der Infektion des Tierkörpers mit Bakterien der Enteritidis- und Paratyphusgruppe, sowie des Typhus. Zbl Bakt Hyg I Abt Orig 62:335–373
Murphy TF, Gorbach SL (1982) Salmonella colitis. N Y State J Med 82:1236–1238
Nair S, Alokam S, Kothapalli S, Porwollik S, Proctor E, Choy C, McClelland M, Liu SL, Sanderson KE (2004) Salmonella enterica serovar Typhi strains from which SPI7, a 134-kilobase island with genes for Vi exopolysaccharide and other functions, has been deleted. J Bacteriol 186:3214–3223
Nasrallah SM, Nassar VH (1978) Enteric fever: a clinicopathologic study of 104 cases. Am J Gastroenterol 69:63–69
Nelson K, Selander RK (1992) Evolutionary genetics of the proline permease gene (putP) and the control region of the proline utilization operon in populations of Salmonella and Escherichia coli. J Bacteriol 174:6886–6895
Nelson K, Whittam TS, Selander RK (1991) Nucleotide polymorphism and evolution in the glyceraldehyde-3-phosphate dehydrogenase gene (gapA) in natural populations of Salmonella and Escherichia coli. Proc Natl Acad Sci USA 88:6667–6671
Nix RN, Altschuler SE, Henson PM, Detweiler CS (2007) Hemophagocytic macrophages harbor Salmonella enterica during persistent infection. PLoS Pathog 3:e193
Noriega LM, Van der Auwera P, Daneau D, Meunier F, Aoun M (1994) Salmonella infections in a cancer center. Support Care Cancer 2:116–122
O'Brien AD (1982) Innate resistance of mice to Salmonella typhi infection. Infect Immun 38:948–952
Ochiai RL, Wang X, von Seidlein L, Yang J, Bhutta ZA, Bhattacharya SK, Agtini M, Deen JL, Wain J, Kim DR, Ali M, Acosta CJ, Jodar L, Clemens JD (2005) Salmonella paratyphi A rates, Asia. Emerg Infect Dis 11:1764–1766
Ochman H, Groisman EA (1996) Distribution of pathogenicity islands in Salmonella spp. Infect Immun 64:5410–5412
Ochman H, Soncini FC, Solomon F, Groisman EA (1996) Identification of a pathogenicity island for Salmonella survival in host cells. Proc Natl Acad Sci USA 93:7800–7804
Ochman H, Wilson AC (1987) Evolution in bacteria: evidence for a universal substitution rate in cellular genomes. J Mol Evol 26:74–86
Octavia S, Lan R (2007) Single-nucleotide-polymorphism typing and genetic relationships of Salmonella enterica serovar Typhi isolates. J Clin Microbiol 45:3795–3801
Octavia S, Lan R (2009) Multiple-locus variable-number tandem-repeat analysis of Salmonella enterica serovar Typhi. J Clin Microbiol 47:2369–2376
Oldach DW, Richard RE, Borza EN, Benitez RM (1998) A mysterious death. N Engl J Med 338:1764–1769
Olsen SJ, Bleasdale SC, Magnano AR, Landrigan C, Holland BH, Tauxe RV, Mintz ED, Luby S (2003) Outbreaks of typhoid fever in the United States, 1960-99. Epidemiol Infect 130:13–21
Ørskov J, Moltke O (1929) Studien über den Infektionsmechanismus bei verschiedenen Paratyphus-Infektionen in weißen Mäusen. Zeitschrift für Immunitätsforschung 59:357–405
Parkhill J, Dougan G, James KD, Thomson NR, Pickard D, Wain J, Churcher C, Mungall KL, Bentley SD, Holden MT, Sebaihia M, Baker S, Basham D, Brooks K, Chillingworth T, Connerton P, Cronin A, Davis P, Davies RM, Dowd L, White N, Farrar J, Feltwell T, Hamlin N, Haque A, Hien TT, Holroyd S, Jagels K, Krogh A, Larsen TS, Leather S, Moule S, O'Gaora P, Parry C, Quail M, Rutherford K, Simmonds M, Skelton J, Stevens K, Whitehead S, Barrell BG (2001) Complete genome sequence of a multiple drug resistant Salmonella enterica serovar Typhi CT18. Nature 413:848–852
Parry CM (2004) The treatment of multidrug-resistant and nalidixic acid-resistant typhoid fever in Viet Nam. Trans R Soc Trop Med Hyg 98:413–422
Parry CM, Threlfall EJ (2008) Antimicrobial resistance in typhoidal and nontyphoidal salmonellae. Curr Opin Infect Dis 21:531–538
Pepper OHP (1920) Endothelial leukocytes in the urine suggesting typhoid fever. Am J Med Sci 160:336–340
Petty NK, Bulgin R, Crepin VF, Cerdeno-Tarraga AM, Schroeder GN, Quail MA, Lennard N, Corton C, Barron A, Clark L, Toribio AL, Parkhill J, Dougan G, Frankel G, Thomson NR (2010) The Citrobacter rodentium genome sequence reveals convergent evolution with human pathogenic Escherichia coli. J Bacteriol 192:525–538
Pfeiffer R, Kolle W (1896) Experimentele Untersuchungen zur Frage der Schutzimpfungen des Menschen gegen den Typhus abdominalis. Dtsch Med Wochenschr 22:735–737
Pickard D, Thomson NR, Baker S, Wain J, Pardo M, Goulding D, Hamlin N, Choudhary J, Threfall J, Dougan G (2008) Molecular characterization of the Salmonella enterica serovar Typhi Vi-typing bacteriophage E1. J Bacteriol 190:2580–2587
Ponfick E (1872) Über die sympathischen Erkrankungen des Knochenmarks bei inneren Krankheiten. Virchow’s Archiv f path Anat 56:534–556
Porster J (1906) Bakteriologischer Befund bei der Autopsie enes Typhusbazillenträgers. Munch Med Wochenschr 50:2434
Powell CJ Jr, DeSett CR, Lowenthal JP, Berman S (1980) The effect of adding iron to mucin on the enhancement of virulence for mice of Salmonella typhi strain TY 2. J Biol Stand 8:79–85
Putnam P (1927) The trend of typhoid fever mortality in the United States. Am J Hyg 7:762–781
Rabsch W, Tschape H, Baumler AJ (2001) Non-typhoidal salmonellosis: emerging problems. Microbes Infect 3:237–247
Raffatellu M, Chessa D, Wilson RP, Dusold R, Rubino S, Baumler AJ (2005a) The Vi capsular antigen of Salmonella enterica serotype Typhi reduces Toll-like receptor-dependent interleukin-8 expression in the intestinal mucosa. Infect Immun 73:3367–3374
Raffatellu M, Chessa D, Wilson RP, Tukel C, Akcelik M, Baumler AJ (2006) Capsule-mediated immune evasion: a new hypothesis explaining aspects of typhoid fever pathogenesis. Infect Immun 74:19–27
Raffatellu M, George MD, Akiyama Y, Hornsby MJ, Nuccio SP, Paixao TA, Butler BP, Chu H, Santos RL, Berger T, Mak TW, Tsolis RM, Bevins CL, Solnick JV, Dandekar S, Baumler AJ (2009) Lipocalin-2 resistance confers an advantage to Salmonella enterica serotype Typhimurium for growth and survival in the inflamed intestine. Cell Host Microbe 5:476–486
Raffatellu M, Santos RL, Chessa D, Wilson RP, Winter SE, Rossetti CA, Lawhon SD, Chu H, Lau T, Bevins CL, Adams LG, Baumler AJ (2007) The capsule encoding the viaB locus reduces interleukin-17 expression and mucosal innate responses in the bovine intestinal mucosa during infection with Salmonella enterica serotype Typhi. Infect Immun 75:4342–4350
Raffatellu M, Wilson RP, Chessa D, Andrews-Polymenis H, Tran QT, Lawhon S, Khare S, Adams LG, Bäumler AJ (2005b) SipA, SopA, SopB, SopD and SopE2 contribute to Salmonella enterica serotype Typhimurium invasion of epithelial cells. Infect Immun 73:146–154
Rebollo JE, Francois V, Louarn JM (1988) Detection and possible role of two large nondivisible zones on the Escherichia coli chromosome. Proc Natl Acad Sci USA 85:9391–9395
Reddy EA, Shaw AV, Crump JA (2010) Community-acquired bloodstream infections in Africa: a systematic review and meta-analysis. Lancet Infect Dis 10:417–432
Reeves MW, Evins GM, Heiba AA, Plikaytis BD, Farmer JJ III (1989) Clonal nature of Salmonella typhi and its genetic realtedness to other salmonellae as shown by multilocus enzyme electrophoresis, and proposal of Salmonella bongori comb. nov. J Clin Microbiol 27:313–320
Richardson MW (1903) Upon the presence of the typhoid bacillus in the urine and sputum. Boston Med Surg J 148:152–153
Riedemann NC, Guo RF, Ward PA (2003) A key role of C5a/C5aR activation for the development of sepsis. J Leukoc Biol 74:966–970
Riley M, Anilionis A (1978) Evolution of the bacterial genome. Annu Rev Microbiol 32:519–560
Robbins JD, Robbins JB (1984) Reexamination of the protective role of the capsular polysaccharide (Vi antigen) of Salmonella typhi. J Infect Dis 150:436–449
Rocha EP (2004) Order and disorder in bacterial genomes. Curr Opin Microbiol 7:519–527
Roof DM, Roth JR (1988) Ethanolamine utilization in Salmonella typhimurium. J Bacteriol 170:3855–3863
Rosove L, Chudnoff JS, Bower AG (1950) Chloramphenicol in the treatment of typhoid fever. Calif Med 72:425–430
Roumagnac P, Weill FX, Dolecek C, Baker S, Brisse S, Chinh NT, Le TA, Acosta CJ, Farrar J, Dougan G, Achtman M (2006) Evolutionary history of Salmonella typhi. Science 314:1301–1304
Russell FF (1911) The isolation of typhoid bacilli from urine and feces with the description of a new double sugar tube medium. J Med Res 25:217–229
Saballs P, Aregall S, Pallares E, Tremoleda J, Gimeno JL, Drobnic L (1993) Salmonella typhimurium as the causal agent of pulmonary cavitations. Enferm Infecc Microbiol Clin 11:93–96
Sahu A, Kozel TR, Pangburn MK (1994) Specificity of the thioester-containing reactive site of human C3 and its significance to complement activation. Biochem J 302(Pt 2):429–436
Salmon DE, Smith T (1885) Report on swine plague. United States Department of Agriculture, Washington, DC, pp 184–246
Salmonella-Subcommittee (1934) The genus Salmonella lignieres, 1900. J Hyg 34:333–350
Santos RL, Raffatellu M, Bevins CL, Adams LG, Tukel C, Tsolis RM, Baumler AJ (2009) Life in the inflamed intestine, Salmonella style. Trends Microbiol 17:498–506
Santos RL, Zhang S, Tsolis RM, Kingsley RA, Adams LG, Bäumler AJ (2001) Animal models of Salmonella infections: enteritis vs typhoid fever. Mircrobes Infect 3:1335–1344
Sauvages de la Croix FB (1763) Nosologia methodican sistens morborum classes, genera, et species, juxta sydenhami mentem et botanicorum ordinem. de Tournes, Amsterdam
Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM (2011) Foodborne illness acquired in the United States–major pathogens. Emerg Infect Dis 17:7–15
Schmitt CK, Ikeda JS, Darnell SC, Watson PR, Bispham J, Wallis TS, Weinstein DL, Metcalf ES, O'Brien AD (2001) Absence of all components of the flagellar export and synthesis machinery differentially alters virulence of Salmonella enterica serovar Typhimurium in models of typhoid fever, survival in macrophages, tissue culture invasiveness, and calf enterocolitis. Infect Immun 69:5619–5625
Secmeer G, Kanra G, Cemeroglu AP, Ozen H, Ceyhan M, Ecevit Z (1995) Salmonella typhi infections. A 10-year retrospective study. Turk J Pediatr 37:339–341
Sekirov I, Gill N, Jogova M, Tam N, Robertson M, de Llanos R, Li Y, Finlay BB (2010) Salmonella SPI-1-mediated neutrophil recruitment during enteric colitis is associated with reduction and alteration in intestinal microbiota. Gut Microbes 1:30–41
Selander RK, Beltran P, Smith NH, Helmuth R, Rubin FA, Kopecko DJ, Ferris K, Tall BD, Cravioto A, Musser JM (1990) Evolutionary genetic relationships of clones of Salmonella serovars that cause human typhoid and other enteric fevers. Infect Immun 58:2262–2275
Senftner HF, Coughlin FE (1933) Typhoid carriers in New York state, with special reference to gall bladder operations. Am J Hyg 17:711–723
Serefhanoglu K, Kaya E, Sevinc A, Aydogdu I, Kuku I, Ersoy Y (2003) Isolated thrombocytopenia: the presenting finding of typhoid fever. Clin Lab Haematol 25:63–65
Sharma A, Qadri A (2004) Vi polysaccharide of Salmonella typhi targets the prohibitin family of molecules in intestinal epithelial cells and suppresses early inflammatory responses. Proc Natl Acad Sci USA 101:17492–17497
Shin BM, Paik IK, Cho HI (1994) Bone marrow pathology of culture proven typhoid fever. J Korean Med Sci 9:57–63
Silva-Herzog E, Detweiler CS (2010) Salmonella enterica replication in hemophagocytic macrophages requires two type three secretion systems. Infect Immun 78:3369–3377
Silverman M, Simon M (1980) Phase variation: genetic analysis of switching mutants. Cell 19:845–854
Simanjuntak CH, Paleologo FP, Punjabi NH, Darmowigoto R, Soeprawoto, Totosudirjo H, Haryanto P, Suprijanto E, Witham ND, Hoffman SL (1991) Oral immunisation against typhoid fever in Indonesia with Ty21a vaccine. Lancet 338:1055–1059
Smith NH, Beltran P, Selander RK (1990) Recombination of Salmonella phase 1 flagellin genes generates new serovars. J Bacteriol 172:2209–2216
Snyder MJ, Gonzalez O, Palomino C, Music SI, Hornick RB, Perroni J, Woodward WE, Gonzalez C, DuPont HL, Woodward TE (1976) Comparative efficacy of chloramphenicol, ampicillin, and co-trimoxazole in the treatment of typhoid fever. Lancet 2:1155–1157
Soe GB, Overturf GD (1987) Treatment of typhoid fever and other systemic salmonelloses with cefotaxime, ceftriaxone, cefoperazone, and other newer cephalosporins. Rev Infect Dis 9:719–736
Song J, Willinger T, Rongvaux A, Eynon EE, Stevens S, Manz MG, Flavell RA, Galan JE (2010) A mouse model for the human pathogen Salmonella typhi. Cell Host Microbe 8:369–376
Soper GA (1907) The work of a chronic typhoid germ distributor. J Am Med Assoc 48:2019–2022
Sprinz H, Gangarosa EJ, Williams M, Hornick RB, Woodward TE (1966) Histopathology of the upper small intestines in typhoid fever. Biopsy study of experimental disease in man. Am J Dig Dis 11:615–624
Stecher B, Barthel M, Schlumberger MC, Haberli L, Rabsch W, Kremer M, Hardt WD (2008) Motility allows S. Typhimurium to benefit from the mucosal defence. Cell Microbiol 10:1166–1180
Stecher B, Robbiani R, Walker AW, Westendorf AM, Barthel M, Kremer M, Chaffron S, Macpherson AJ, Buer J, Parkhill J, Dougan G, von Mering C, Hardt WD (2007) Salmonella enterica serovar typhimurium exploits inflammation to compete with the intestinal microbiota. PLoS Biol 5:2177–2189
Stocker BA (1949) Measurements of rate of mutation of flagellar antigenic phase in Salmonella typhi-murium. J Hyg (Lond) 47:398–413
Stone WS (1912) The medical of chronic typhoid infection (typhoid bacillus carriers). Am J Med Sci 143:544–557
Szu SC, Taylor DN, Trofa AC, Clements JD, Shiloach J, Sadoff JC, Bryla DA, Robbins JB (1994) Laboratory and preliminary clinical characterization of Vi capsular polysaccharide-protein conjugate vaccines. Infect Immun 62:4440–4444
Tacket CO, Hone DM, Curtiss R 3rd, Kelly SM, Losonsky G, Guers L, Harris AM, Edelman R, Levine MM (1992a) Comparison of the safety and immunogenicity of delta aroC delta aroD and delta cya delta crp Salmonella typhi strains in adult volunteers. Infect Immun 60:536–541
Tacket CO, Hone DM, Losonsky GA, Guers L, Edelman R, Levine MM (1992b) Clinical acceptability and immunogenicity of CVD 908 Salmonella typhi vaccine strain. Vaccine 10:443–446
Tacket CO, Sztein MB, Losonsky GA, Wasserman SS, Nataro JP, Edelman R, Pickard D, Dougan G, Chatfield SN, Levine MM (1997) Safety of live oral Salmonella typhi vaccine strains with deletions in htrA and aroC aroD and immune response in humans. Infect Immun 65:452–456
Tacket CO, Sztein MB, Wasserman SS, Losonsky G, Kotloff KL, Wyant TL, Nataro JP, Edelman R, Perry J, Bedford P, Brown D, Chatfield S, Dougan G, Levine MM (2000) Phase 2 clinical trial of attenuated Salmonella enterica serovar typhi oral live vector vaccine CVD 908-htrA in U.S. volunteers. Infect Immun 68:1196–1201
Tewari A, Buhles WC Jr, Starnes HF Jr (1990) Preliminary report: effects of interleukin-1 on platelet counts. Lancet 336:712–714
Thiem VD, Lin FY, do Canh G, Son NH, Anh DD, Mao ND, Chu C, Hunt SW, Robbins JB, Schneerson R, Szu SC (2011) The Vi conjugate typhoid vaccine is safe, elicits protective levels of IgG anti-Vi, and is compatible with routine infant vaccines. Clin Vaccine Immunol 18:730–735
Thiennimitr P, Winter SE, Winter MG, Xavier MN, Tolstikov V, Huseby DL, Sterzenbach T, Tsolis RM, Roth JR, Bäumler AJ (2011) Intestinal inflammation allows Salmonella to utilize ethanolamine to compete with the microbiota. Proc Natl Acad Sci USA 108:17480–17485
Thomson NR, Clayton DJ, Windhorst D, Vernikos G, Davidson S, Churcher C, Quail MA, Stevens M, Jones MA, Watson M, Barron A, Layton A, Pickard D, Kingsley RA, Bignell A, Clark L, Harris B, Ormond D, Abdellah Z, Brooks K, Cherevach I, Chillingworth T, Woodward J, Norberczak H, Lord A, Arrowsmith C, Jagels K, Moule S, Mungall K, Sanders M, Whitehead S, Chabalgoity JA, Maskell D, Humphrey T, Roberts M, Barrow PA, Dougan G, Parkhill J (2008) Comparative genome analysis of Salmonella Enteritidis PT4 and Salmonella Gallinarum 287/91 provides insights into evolutionary and host adaptation pathways. Genome Res 18:1624–1637
Tindall BJ, Grimont PA, Garrity GM, Euzeby JP (2005) Nomenclature and taxonomy of the genus Salmonella. Int J Syst Evol Microbiol 55:521–524
Tonney FO, Caldwell FC, Griffin PJ (1916) The examination of the urine and the feces of suspect typhoid-carriers with a report on elaterin catharsis. J Infect Dis 18:239–246
Townsend SM, Kramer NE, Edwards R, Baker S, Hamlin N, Simmonds M, Stevens K, Maloy S, Parkhill J, Dougan G, Bäumler AJ (2001) Salmonella enterica serotype Typhi possesses a unique repertoire of fimbrial gene sequences. Infect Immun 69:2894–2901
Tran QT, Gomez G, Khare S, Lawhon SD, Raffatellu M, Baumler AJ, Ajithdoss D, Dhavala S, Adams LG (2010) The Salmonella enterica serotype Typhi Vi capsular antigen is expressed after the bacterium enters the ileal mucosa. Infect Immun 78:527–535
Tsolis RM, Adams LG, Ficht TA, Baumler AJ (1999a) Contribution of Salmonella typhimurium virulence factors to diarrheal disease in calves. Infect Immun 67:4879–4885
Tsolis RM, Kingsley RA, Townsend SM, Ficht TA, Adams LG, Baumler AJ (1999b) Of mice, calves, and men. Comparison of the mouse typhoid model with other Salmonella infections. Adv Exp Med Biol 473:261–274
Tsolis RM, Townsend SM, Miao EA, Miller SI, Ficht TA, Adams LG, Baumler AJ (1999c) Identification of a putative Salmonella enterica serotype typhimurium host range factor with homology to IpaH and YopM by signature-tagged mutagenesis. Infect Immun 67:6385–6393
Tsolis RM, Xavier MN, Santos RL, Baumler AJ (2011) How to become a top model: impact of animal experimentation on human Salmonella disease research. Infect Immun 79:1806–1814
Tsolis RM, Young GM, Solnick JV, Baumler AJ (2008) From bench to bedside: stealth of enteroinvasive pathogens. Nat Rev Microbiol 6:883–892
Tukel C, Nishimori JH, Wilson RP, Winter MG, Keestra AM, van Putten JP, Baumler AJ (2010) Toll-like receptors 1 and 2 cooperatively mediate immune responses to curli, a common amyloid from enterobacterial biofilms. Cell Microbiol 12:1495–1505
Tukel C, Raffatellu M, Humphries AD, Wilson RP, Andrews-Polymenis HL, Gull T, Figueiredo JF, Wong MH, Michelsen KS, Akcelik M, Adams LG, Baumler AJ (2005) CsgA is a pathogen-associated molecular pattern of Salmonella enterica serotype Typhimurium that is recognized by Toll-like receptor 2. Mol Microbiol 58:289–304
Tukel C, Wilson RP, Nishimori JH, Pezeshki M, Chromy BA, Baumler AJ (2009) Responses to amyloids of microbial and host origin are mediated through Toll-like receptor 2. Cell Host Microbe 6(1):45–53
Tumbarello M, Tacconelli E, Caponera S, Cauda R, Ortona L (1995) The impact of bacteraemia on HIV infection. Nine years experience in a large Italian university hospital. J Infect 31:123–131
Uba AF, Chirdan LB, Ituen AM, Mohammed AM (2007) Typhoid intestinal perforation in children: a continuing scourge in a developing country. Pediatr Surg Int 23:33–39
Uchiya K, Barbieri MA, Funato K, Shah AH, Stahl PD, Groisman EA (1999) A Salmonella virulence protein that inhibits cellular trafficking. EMBO J 18:3924–3933
Uwaydah M, Shammaa M (1964) The treatment of typhoid fever with ampicillin. Lancet 1:1242–1243
Vazquez-Torres A, Vallance BA, Bergman MA, Finlay BB, Cookson BT, Jones-Carson J, Fang FC (2004) Toll-like receptor 4 dependence of innate and adaptive immunity to Salmonella: importance of the Kupffer cell network. J Immunol 172:6202–6208
Vazquez-Torres A, Xu Y, Jones-Carson J, Holden DW, Lucia SM, Dinauer MC, Mastroeni P, Fang FC (2000) Salmonella pathogenicity island 2-dependent evasion of the phagocyte NADPH oxidase. Science 287:1655–1658
Virlogeux I, Waxin H, Ecobichon C, Lee JO, Popoff MY (1996) Characterization of the rcsA and rcsB genes from Salmonella typhi: rcsB through tviA is involved in regulation of Vi antigen synthesis. J Bacteriol 178:1691–1698
Virlogeux I, Waxin H, Ecobichon C, Popoff MY (1995) Role of the viaB locus in synthesis, transport and expression of Salmonella typhi Vi antigen. Microbiology 141(Pt 12):3039–3047
Wahdan MH, Serie C, Cerisier Y, Sallam S, Germanier R (1982) A controlled field trial of live Salmonella typhi strain Ty 21a oral vaccine against typhoid: three-year results. J Infect Dis 145:292–295
Wain J, Hoa NT, Chinh NT, Vinh H, Everett MJ, Diep TS, Day NP, Solomon T, White NJ, Piddock LJ, Parry CM (1997) Quinolone-resistant Salmonella typhi in Viet Nam: molecular basis of resistance and clinical response to treatment. Clin Infect Dis 25:1404–1410
Wang F, Gu XJ, Zhang MF, Tai TY (1989) Treatment of typhoid fever with ofloxacin. J Antimicrob Chemother 23:785–788
Weber JT, Levine WC, Hopkins DP, Tauxe RV (1994) Cholera in the United States, 1965-1991. Risks at home and abroad. Arch Intern Med 154:551–556
Weening EH, Barker JD, Laarakker MC, Humphries AD, Tsolis RM, Baumler AJ (2005) The Salmonella enterica serotype Typhimurium lpf, bcf, stb, stc, std, and sth fimbrial operons are required for intestinal persistence in mice. Infect Immun 73:3358–3366
Welton JC, Marr JS, Friedman SM (1979) Association between hepatobiliary cancer and typhoid carrier state. Lancet 1:791–794
Widal F (1896) Serodiagnostic de la fievre typhoide. Bulletin et Memoires de la Societe de Medicine des Hotitaux de Paris 13:561–566
Willis T (1682) Opera omnia. De Febribus, Amstelaedami
Wilson RP, Raffatellu M, Chessa D, Winter SE, Tukel C, Baumler AJ (2008) The Vi-capsule prevents toll-like receptor 4 recognition of Salmonella. Cell Microbiol 10:876–890
Wilson RP, Winter SE, Spees AM, Winter MG, Nishimori JH, Sanchez JF, Nuccio SP, Crawford RW, Tukel C, Baumler AJ (2011) The Vi capsular polysaccharide prevents complement receptor 3-mediated clearance of Salmonella enterica serotype Typhi. Infect Immun 79:830–837
Wilson WJ, Blair EM (1927) Use of a glucose bismuth sulphite iron medium for the isolation of B. typhosus and B. proteus. J Hyg (Lond) 26:374–391
Wilson WJ, Blair EM (1931) Further experience of the bismuth sulphite media in the isolation of Bacillus typhosus and B. paratyphosus B from faeces, sewage and water. J Hyg (Lond) 31:138–161
Winter SE, Keestra AM, Tsolis RM, Bäumler AJ (2010a) The blessings and curses of intestinal inflammation. Cell Host Microbe 8:36–43
Winter SE, Thiennimitr P, Nuccio SP, Haneda T, Winter MG, Wilson RP, Russell JM, Henry T, Tran QT, Lawhon SD, Gomez G, Bevins CL, Russmann H, Monack DM, Adams LG, Baumler AJ (2009a) Contribution of flagellin pattern recognition to intestinal inflammation during Salmonella enterica serotype typhimurium infection. Infect Immun 77:1904–1916
Winter SE, Thiennimitr P, Winter MG, Butler BP, Huseby DL, Crawford RW, Russell JM, Bevins CL, Adams LG, Tsolis RM, Roth JR, Baumler AJ (2010b) Gut inflammation provides a respiratory electron acceptor for Salmonella. Nature 467:426–429
Winter SE, Winter MG, Godinez I, Yang H-J, Russmann H, Andrews-Polymenis HL, Bäumler AJ (2010c) A rapid change in virulence gene expression during the transition from the intestinal lumen into tissue promotes systemic dissemination of Salmonella. PLoS Pathog 6(8):e1001060
Winter SE, Winter MG, Thiennimitr P, Gerriets VA, Nuccio SP, Russmann H, Baumler AJ (2009b) The TviA auxiliary protein renders the Salmonella enterica serotype Typhi RcsB regulon responsive to changes in osmolarity. Mol Microbiol 74:175–193
Wong KH, Feeley JC, Northrup RS, Forlines ME (1974) Vi antigen from Salmonella typhosa and immunity against typhoid fever. I. Isolation and immunologic properties in animals. Infect Immun 9:348–353
Woodward TE, Smadel JE et al (1948) Preliminary report on the beneficial effect of chloromycetin in the treatment of typhoid fever. Ann Intern Med 29:131–134
Woodward TE, Smadel JE, Ley HL Jr (1950) Chloramphenicol and other antibiotics in the treatment of typhoid fever and typhoid carriers. J Clin Invest 29:87–99
Wright AE (1896) On the association of serous haemorrhages with conditions of defective blood-coagulability. Lancet 2:807–809
Yamamoto S, Kutsukake K (2006) FljA-mediated posttranscriptional control of phase 1 flagellin expression in flagellar phase variation of Salmonella enterica serovar Typhimurium. J Bacteriol 188:958–967
Yap YF, Puthucheary SD (1998) Typhoid fever in children–a retrospective study of 54 cases from Malaysia. Singapore Med J 39:260–262
Zhang S, Santos RL, Tsolis RM, Stender S, Hardt W-D, Bäumler AJ, Adams LG (2002) SipA, SopA, SopB, SopD and SopE2 act in concert to induce diarrhea in calves infected with Salmonella enterica serotype Typhimurium. Infect Immun 70:3843–3855
Zhou D, Mooseker MS, Galan JE (1999) Role of the S. typhimurium actin-binding protein SipA in bacterial internalization. Science 283:2092–2095
Zinder ND (1958) Lysogenization and superinfection immunity in Salmonella. Virology 5:291–326
Acknowledgments
Work in A.J.B.’s laboratory is supported by Public Health Service Grants AI040124, AI044170, AI076246, AI088122, and AI096528.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
Nuccio, SP., Wangdi, T., Winter, S.E., Bäumler, A.J. (2013). Typhoid. In: Rosenberg, E., DeLong, E.F., Lory, S., Stackebrandt, E., Thompson, F. (eds) The Prokaryotes. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-30144-5_105
Download citation
DOI: https://doi.org/10.1007/978-3-642-30144-5_105
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-30143-8
Online ISBN: 978-3-642-30144-5
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences